Abstract
Background
The growing number of vulnerable migrants and refugees (VMRs) in the European Union presents challenges to healthcare systems, emphasizing the need for enhanced intercultural competence training for healthcare professionals. Educational escape rooms, using gamification-based principles, may offer an innovative solution to improve these competencies.
Objective
This pilot study evaluates the acceptability and preliminary effectiveness of an educational escape room aimed at improving intercultural competence, self-efficacy, and knowledge among healthcare students and professionals caring for VMRs.
Methods
A pre-post, single-group pilot study was conducted with 101 healthcare students and professionals, recruited through convenience sampling. Participants engaged in an educational escape room simulating a migratory crisis, designed to foster collaborative problem-solving under pressure. A newly validated questionnaire was administered before and after the intervention to measure changes in intercultural competence, self-efficacy, and knowledge. Paired t-tests were used to analyze pre-post differences, and thematic analysis explored participant feedback on the learning experience and the acceptability of the intervention.
Results
Significant improvements were observed in intercultural competence (d = 1.13, p < 0.001), self-efficacy (d = 0.38, p = 0.001), and knowledge (d = 1.19, p < 0.001). Participants reported high engagement, satisfaction, and an enhanced understanding of healthcare challenges related to VMRs. The escape room was deemed acceptable.
Conclusions
This pilot study provides evidence of the acceptability and effectiveness of an educational escape room in enhancing intercultural competence, self-efficacy, and knowledge. Further research with larger, more rigorous studies is recommended to confirm these findings and explore scalability.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12939-024-02304-2.
Keywords: Intercultural competence, Self-efficacy, Educational escape room, Vulnerable migrants and refugees, Healthcare education
Background
Since the beginning of the early 2000s, the number of migrants and mobile European Union (EU) citizens living in the EU has gone from 34 million (or 6.9% of the total EU population) in the early 2000s to over 90 million (or 10%) in recent years [1]. Asylum applications submitted in EU Member States has been following a similar upward trend, with 648,000 applications registered in 2021 and a 25.7% increase compared to 2020 [2]. Worldwide, with millions of Ukrainians displaced, the total forced displacement by violence, conflict, persecution, food insecurity, and human rights violations, now exceeds 100 million people. That is, 1 out of every 78 people on earth has been forced to flee their home [3].
The growing segment of vulnerable migrants and refugees (VMRs) across Europe represents a significant challenge to the healthcare systems of receiving countries. An essential problem in facing such challenges is the scarcity of intercultural competence (ICC) training offered within healthcare education at large [4]. Consequently, healthcare professionals often lack the necessary ICC skills, that is, the capability to deliver effective, respectful, and understandable care to VMRs seeking medical attention in a manner fitting the patient’s health beliefs, practices, and language [5, 6]. In turn, low ICC in the clinical encounter has consistently been shown to impact health service utilization and quality of care of the most vulnerable patients [7, 8].
Despite numerous calls to action to include ICC training in public health education across the globe [9], only a limited number of programs have truly implemented the necessary educational opportunities to meet such goals [5, 10]. In Spain alone, very few official programs offer a focused training curriculum about the unique health realities and barriers experienced by VMR [11, 12]. Results from several Spanish studies on the perceptions of healthcare providers caring for VMRs suggest that low levels of ICC are similarly perceived by professionals themselves as an important contributor to health-access disparities [13–15].
The rapid development of novel gamification-based initiatives such as educational Escape Rooms (ERs) may offer a promising solution to the ICC training gap. Educational ERs have been defined as a teaching method requiring learners to participate in collaborative “gamified” activities explicitly designed for knowledge acquisition or skill development to accomplish a specific goal (e.g. escape from a physical room) by solving time-limited puzzles related to prespecified educational goals [16]. More importantly, the data suggest that educational ESs are particularly successful at engaging participants in the learning process while providing an excellent framework for effective competency building [17].
Several examples of published educational ERs in healthcare are worth mentioning. For example, researchers developed an ER aimed at Nurse Practitioners to teach bedside nursing skills [18]. The authors argued that the ERs provided a unique opportunity to diversify learning strategies, as each puzzle required a varied set of skills to successfully solve (kinesthetic, knowledge, visual cues). Other authors created an escape-room-inspired game as part of a genetics course curriculum [19], with the objective to consolidate course materials. Overall, designers of ER educational activities report high levels of engagement, satisfaction, and knowledge retention.
Efforts are also being made to design educational ERs that tackle more complex, societally relevant topics. For instance, researchers developed an ER focusing on the topic of elder abuse [20]. The game, titled Sandra’s Keys, encouraged players to engage with the story of an imaginary older woman struggling with abuse through a series of puzzles. The goal of the ER is to bring participants into a dialogue about the different forms of elder abuse, deepening the understanding of the bystander’s role.
Despite the potential of educational ER to promote competency-building, none of the educational ERs found in the literature have focused on VMRs nor targeted ICC training. Furthermore, the majority of published educational ERs have important methodological problems such as the overutilization of poorly validated instruments; small sample sizes, and, overall, a lack of methodological rigor [18, 21, 22].
To bridge the identified research gap, we introduce the preliminary evidence-base of a novel educational ER, titled “Refugee Escape Room” (RER). This innovative ER was conceptualized and initially developed through a collaborative effort between authors NDC and LW during an academic exchange between Spain and Canada in 2017 as part of a Master of Public Health course focusing on gamification-based teaching methodologies. The RER, initially trialed with public health and health sciences students, draws upon the authors’ extensive research on the health ramifications of migration and VMR’s interactions with the healthcare system. Our main objective is to showcase a novel educational ER that aims to train ICC, improve Self-Efficacy (SE) and increase the Knowledge (Kw) of healthcare students and professionals caring for VMRs. Additionally, we aim to gain a deeper insight into the acceptability and the learning process of the RER experience.
Methods
Study design
We conducted a pre-post, single-group intervention study to assess the acceptability and preliminary effectiveness of our educational escape room on ICC, SE, and Kw among healthcare students and professionals.
Ethics statement
The study was conducted in accordance with the Harmonized Tripartite Standards for Good Clinical Practice and adhered to national regulations (Law 14/2007 of Biomedical Research) and the ethical principles outlined in the Declaration of Helsinki. Participant confidentiality was maintained following the Spanish Organic Law 15/1999 on the Protection of Personal Data. The Clinical Research Ethics Committee of the Vall d’Hebron Hospital in Barcelona approved the study protocol.
Procedure
A total of 101 participants were recruited through convenience sampling from health and social science fields, including both students and professionals aged 18 and older. Recruitment involved two student groups: 26 students from the MSc in International Health program at the Autonomous University of Barcelona and 50 students from the IES Abroad international education program. Both student groups had a 100% response rate, with all invited students voluntarily enrolling and providing signed consent forms. Additionally, 25 healthcare professionals were recruited from a pool of 197 individuals contacted via email through a local international-health mailing list, resulting in a 12.7% response rate. All participants provided informed consent to take part in the study.
The RER intervention was conducted in four sessions (two in English and two in Spanish) at three institutions in Barcelona, Spain: the Universitat Autònoma de Barcelona (UAB) on June 17, 2019; the Catalan Health Institute Auditorium on June 18, 2019; and the IES Abroad campus on June 19 and 20, 2019. Each session lasted two hours, with an additional 30 min allocated for consent forms and pre- and post-intervention questionnaires.
Before each session, assistants were assigned specific roles—corrupt official, passport officer, educational officer, health officer, and ticket officer—and given detailed instructions to ensure consistent role-playing. One team member was designated as a facilitator to assist participants during the intervention.
Data collection involved administering the pre- and post-intervention questionnaires on paper, which were later digitized using Google Forms and exported to SPSS for analysis.
Intervention description
The RER1 is a three-stage, two-hour, face-to-face activity set in the year 2084 during a global crisis caused by overpopulation, climate change, wars, and shifting infectious disease patterns. In this scenario, participants are divided into teams, each representing a family unit intentionally composed of diverse ethnic, geographical, and socioeconomic backgrounds to avoid replicating current real-world demographics. The teams collaborate to solve complex puzzles and compete for a spot on an interplanetary spaceship bound for Mars—portrayed as a safer haven than a deteriorating Earth.
Stage 1 provides a 30-minute classroom session where an expert discusses key aspects of health and migration. This section includes a Q&A session to equip participants with the knowledge necessary for solving puzzles in the later stages.
Stage 2 simulates a Border Control environment, presenting participants with bureaucratic challenges across four fictional Offices. Participants face language-based puzzles (using a fictional “Martian” language) and are evaluated on their education, language skills, and health status. They encounter various penalties, such as mandatory quarantine due to disease outbreaks or detention based on their country of origin. Corrupt officials also appear, demanding bribes, disproportionately targeting poorer family units. These challenges reflect the complexities of modern migration and highlight the role of socioeconomic status. The experience culminates in some teams reaching Mars, while others face a harsher reality, mirroring the unpredictable outcomes of real-world migration.
Stage 3 consists of a 30-minute semi-structured debriefing session during which participants discuss the challenges they encountered during the escape room activity, their emotional reactions, and the interpersonal skills they utilized. This session encourages participants to reflect on the insights gained from the experience, assess the acceptability of the intervention, and identify areas for improvement. Facilitators guide the discussion to help participants connect their experiences to real-world scenarios involving VMRs, reinforcing the activity’s learning objectives.
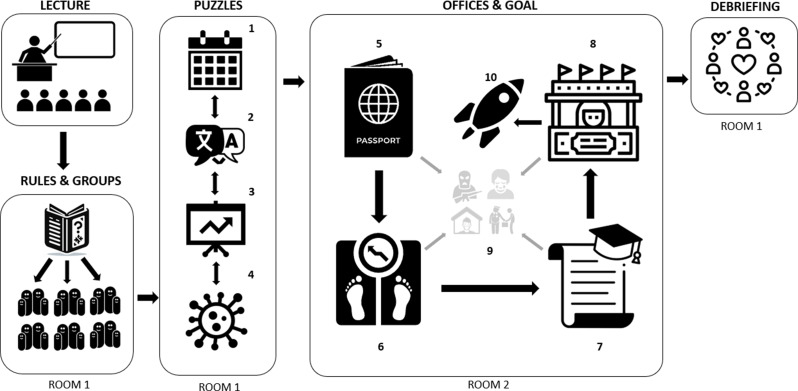
For a detailed summary of materials, time allocation, and resources required for the RER, see Table 1. The process flowchart and puzzle definitions are provided in Fig. 1.
Table 1.
Overview of the refugee escape room game - objectives, structure, and required materials
| Objectives | |||
| Increase knowledge about epidemiological, chronological and health aspects in relation to people that recently arrived because of the migration crisis. To better intercultural competency and self-efficacy of healthcare professionals that work directly or indirectly with migrants recently arrived in Europe. | |||
| General Aspects of the RER | |||
| Age: +18 years. Number of participants: 15–40 (5 to 7 groups of 3 to 6 participants). Duration: approximately 120 min. Format: session in classroom. Subject area: Refugees and migration process. Keywords: refugees, cultural competence, migration, health, refugee. | |||
| Overview and context | |||
| Earth is dying and must migrate to Mars to survive. Participants will be divided by groups (families) and must survive multiple challenges related to the migration process. Their goal is to reach the end of the game to discover a new land of opportunities. | |||
| Materials and Human Resources | |||
| 1 coordinator/teacher and 4 teacher assistants. Classroom 1: computer, screen, internet connection, audio, 4 tables, 15–40 chairs. Classroom 2: computer, 4 tables, 12 chairs. 4 boxes with coded lock. 5–7 envelops with groups information (family profile, passport, savings, pen). Border control documents (forms, flight tickets, poster signs pointing different offices) | |||
| Game structure | Description | Human Resource | Duration |
| Theoretical Framework | Introduction of basic aspects of health and immigration (room 1) | 1 coordinator/teacher | 30 min |
| Escape Room activity | Context of the game, rules, and familiar groups (room 1) | 1 coordinator/teacher | 10 min |
| First phase: knowledge puzzles (room 1) | 2 teacher assistants | 25 min | |
| Second phase: fictitious border (room 2) | 4 teacher assistants | 25 min | |
| Debriefing | Signifying the experience: lessons learned (room 1) | 1 coordinator/teacher | 30 min |
Fig. 1.
RER intervention flowchart. Note: This flowchart illustrates the progression through the escape room game, detailing each phase from the initial lecture to the final stage of reaching Mars. After the lecture participants are given instructions and form ‘family units,’ undergo a series of puzzles and challenges related to migration, and interact with various themed offices such as Passport, Health, Education, and Ticket offices. Description of the puzzles and offices: 1 Chronological Cards Puzzle: Participants arrange migration fact cards in chronological order to obtain a code. 2 Migration Terminology Puzzle: A crossword puzzle with migrant term definitions reveals a code. 3 Migratory Trends Puzzle: An alphabet soup puzzle about migration trends; unused letters form a code. 4 Migration & Health Literacy Puzzle: Filling gaps in a text about migration health aspects on a computer generates a code. 5 Passport Office: Presenting a family passport with previous codes, participants fill out an application in Martian and pay for translation. Outcomes depend on origin and suspected terrorist links. 6 Health Office: Families undergo medical checks, facing potential treatment costs, quarantine, or rejection. 7 Education Office: Validation of diplomas and demonstrating the relevance of professions for life on Mars. 8 Ticket Office: Families must buy tickets to Mars; inability to pay means returning to their country. 9 Penalties & Random Encounters: Participants face various obstacles like detention for epidemiological/geopolitical risks or corrupt officials demanding bribes. 10 Reaching the Rocket: This immersive experience reaches its climax as participants either successfully reach the rocket to Mars or, more commonly, confront a much harsher reality. The experience concludes with a debriefing session, aimed at consolidating the key learning outcomes and the insights participants have gained throughout their journey
Outcomes
The primary outcomes measured were ICC, SE, Kw, and the acceptability of the RER intervention.
Measurement instruments
Questionnaire development and validation
To measure ICC, SE, and Kw effectively while considering practical constraints, we adapted a shortened version of the Clinical Cultural Competency Questionnaire (CCCQ) [26] and introduced newly crafted items for SE and Kw. This approach allowed us to focus on obtaining accurate and relevant results specific to our study objectives without the need to develop a new, widely applicable psychometric instrument.
We began by conducting a brief literature review to identify existing ICC questionnaires that met the following criteria: published in peer-reviewed journals, targeted at healthcare professionals, easily accessible, and aligned with our RER learning objectives. Although we found several frequently cited questionnaires [23–25], most focused on North-American population dynamics, had different target groups, or were too lengthy to administer. After careful review, the CCCQ [26], a validated 86-item self-assessment tool measuring four ICC dimensions—Knowledge, Skills, Attitudes, and Awareness—was selected for adaptation due to its consistency with established ICC models [27, 28].
For item reduction, two researchers independently evaluated each item on a scale of 1 to 10 based on its relevance to our RER goals. Items with high inter-rater agreement were retained, resulting in a condensed questionnaire of 13 items. Additionally, three modified items from the Scale of Ethno-Cultural Empathy [24] were included following a similar evaluation process. Wording adjustments were made to focus on the target population of VMRs entering Europe, and a forward and backward translation to Spanish was performed.
An exploratory factor analysis with Promax rotation and the Kaiser criterion supported a model with 16 items across five dimensions, explaining over 70% of the variance with Eigenvalues greater than 1. The factor structure aligned with the original questionnaire (see Supplemental Digital Appendix 2). All items were scored on a 1–5 point Likert scale.
For SE and Kw, we created new items due to the lack of suitable validated questionnaires. Objective knowledge was assessed using multiple-choice questions on VMR-related topics. Internal consistency was confirmed using Cronbach’s alpha, which showed acceptable levels (α > 0.7) for all subscales with more than one item and for overall ICC and SE scores (see Supplemental Digital Appendix 3 for the reliability analysis).
The pre-test questionnaire included 24 items covering sociodemographic information and baseline outcomes, while the post-test added two open-ended qualitative questions and a 10-point Likert scale assessing activity satisfaction, totaling 27 items (see Supplemental Digital Appendix 4 for the questionnaires).
Qualitative analysis: participant reflections
Participant satisfaction ratings and qualitative feedback were collected via two open-ended questions in the post-intervention survey, focusing on the acceptability of the intervention, the learning experiences and suggestions for improvement. Thematic content analysis was performed on the responses, with two independent researchers coding the data into key themes to ensure reliability through triangulation.
Statistical analysis
Descriptive statistics were calculated to assess the distribution, central tendency, and dispersion of the main outcomes and sociodemographic variables. Paired-sample t-tests were used to compare pre- and post-test scores, with effect sizes determined using Cohen’s d. Correlation analyses explored relationships between scores and subsample variables. Missing data, accounting for less than 5%, were addressed using multiple imputation. All statistical analyses were conducted using SPSS version 25.
Results
Baseline measures and sociodemographic analysis
The total sample consisted of 101 participants (see Table 2), with a mean age of 25.76 years (sd 7.94). The majority identified as female (76%). Approximately half of our sample were health science students (51%), followed by healthcare workers (44%), evenly split between 50% nurses and 50% physicians. The remaining participants were professionals from other backgrounds (5%). Participants primarily originated from Europe (46%) and the United States (43%), with 91% of Europeans hailing from Spain. Most participants had previous work experience (69%), while only 28% reported experience working with migrants.
Table 2.
Sociodemographic characteristics of participants
| Characteristic | Value | n (%) |
|---|---|---|
| Sex | Female | 76 (76%) |
| Male | 23 (23%) | |
| Other | 1 (1%) | |
| Age | - | 25.76 (sd = 7.9) |
| Professional occupation | Nurse | 22 (22%) |
| Physician | 22 (22%) | |
| Student | 51 (51%) | |
| Other | 5 (5%) | |
| Activity Location | MSc | 26 (26%) |
| ICS | 24 (24%) | |
| IES | 50 (50%) | |
| Worked with migrants? | Yes | 28 (28%) |
| No | 72 (72%) | |
| Has work experience? | Yes | 69 (69%) |
| No | 31 (31%) |
Note: he table represents a comprehensive breakdown of the sociodemographic data of participants in the study. Percentages were calculated based on the total sample size of 101 participants. The mean age is provided with the standard deviation (SD)
Intercultural competence
At baseline, the overall mean score for ICC was 10.57 (SD = 1.54). Baseline scores for the subscales were as follows: Knowledge on Health Disparities (M = 2.02, SD = 0.67), Attitudes Toward Factors Contributing to Health Disparities (M = 4.61, SD = 0.85), Awareness of Racial, Ethnic, or Cultural Stereotypes (M = 0.79, SD = 0.18), Importance of ICC Training for Healthcare Professionals (M = 0.94, SD = 0.12), and Empathy (M = 2.22, SD = 0.54) (see Table 3).
Table 3.
Comparative analysis of pre and post-intervention scores in intercultural competence, self-efficacy, and knowledge related to health disparities and VMR
| Scale | Subscale | Description | Mean (SD) | Cohen’s d | Coefficient of variation (CV = SD/Mean) | t | Sig. (bilateral) | ||
|---|---|---|---|---|---|---|---|---|---|
| PRE | Post | PRE | Post | ||||||
| Intercultural Competence | Knowledge | Self-reported knowledge on health disparities | 2.02 (0.67) | 2.94 (0.59) | 1.57 | 0.33 | 0.20 | -14.28 | < 0.001 |
| Attitudes | Attitudes towards factors contributing to health disparities | 4.61 (0.85) | 4.98 (0.86) | 0.43 | 0.18 | 0.17 | -4.80 | < 0.001 | |
| Awareness | Awareness of racial, ethnic, or cultural stereotypes | 0.79 (0.18) | 0.82 (0.17) | 0.21 | 0.24 | 0.20 | -2.62 | 0.01 | |
| Importance | Importance of cultural competency training for health professionals | 0.94 (0.12) | 0.97 (0.09) | 0.40 | 0.12 | 0.09 | -2.99 | < 0.01 | |
| Empathy | Empathic perspective taking & empathic awareness | 2.22 (0.54) | 2.52 (0.45) | 0.67 | 0.24 | 0.18 | -6.92 | < 0.001 | |
| TOTAL | 10.57 (1.54) | 12.23 (1.47) | 1.13 | 0.15 | 0.12 | -12.64 | < 0.001 | ||
| Self-efficacy | Awareness on the personal capacity to assess factors related VMR | 3.08 (0.62) | 3.29 (0.54) | 0.38 | 0.20 | 0.16 | -3.56 | 0.001 | |
| Knowledge | General knowledge on VMR | 3.03 (1.13) | 4.08 (0.88) | 1.19 | 0.37 | 0.22 | -8.40 | < 0.001 | |
Note: This table displays the results of a bivariate analysis comparing pre- and post-intervention scores of the intercultural competence, self-efficacy and knowledge scales. The mean (M) and standard deviation (SD) are reported for each subscale for both the pre- and post-intervention groups. The effect size is measured using Cohen’s d, and the coefficient of variation (CV) is also provided. The t-value and bilateral significance level are reported for each subscale, indicating whether there was a significant difference between pre- and post-intervention scores
Coefficient of variation (CV) was calculated using the formula: CV = SD / Mean
Significance level (Sig.) was set at p < 0.05
Baseline ICC scores did not significantly differ between genders, age and previous working experience. However, participants with prior experience working with migrants had higher overall ICC scores compared to those without such experience (M = 11.28 vs. 10.29; p < 0.05). The largest difference was observed in the Knowledge subscale (M = 2.41 vs. 1.86; p < 0.05). healthcare professionals also scored higher in overall ICC than students (M = 11.07 vs. 10.01; p < 0.05), particularly in the Knowledge (M = 2.25 vs. 1.76; p < 0.05) and Empathy subscales (M = 2.48 vs. 1.94; p < 0.05). For more, refer to Table 4.
Table 4.
Analysis of baseline scores in relation to sociodemographic factors
| Intercultural Competency | Self Efficacy | Knowledge | Pre-Post Differences | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall Score | Subjective Knowledge | Attitudes | Awareness | Importance | Empathy | - | - | ICC | SE | Kw | ||
| Previous work experience? | Yes | 10.74a (1.49) | 2.08a (0.66) | 4.4a (0.85) | .78a (0.17) | .94a (0.11) | 2.31a (0.50) | 3.2a (0.63) | 3.03a (1.19) | 1.61a | .16a | 1.14a |
| No | 10.17a (1.61) | 1.88a (0.68) | 4.55a (0.87) | .81a (0.21) | .93a (0.13) | 2.01b (0.58) | 3.00a (0.62) | 3.03a (1.02) | 1.79a | .31a | .84a | |
| Worked with migrants? | Yes | 11.28a (1.66) | 2.41a (0.66) | 4.74a (0.78) | .84a (0.15) | .93a (0.14) | 2.36a (0.60) | 3.19a (0.63) | 2.96a (1.00) | 1.42a | .26a | 1.11a |
| No | 10.29b (1.42) | 1.86b (0.62) | 4.56a (0.88) | .77a (0.19) | .94a (0.11) | 2.16a (0.51) | 3.04a (0.62) | 3.06a (1.19) | 1.76a | .18a | 1.03a | |
| Professional vs. Student | Prof. | 11.07a (1.24) | 2.25a (0.49) | 4.65a (0.84) | .74a (0.16) | .95a (0.10) | 2.48a (0.33) | 3.17a (0.53) | 3.07a (1.19) | 1.27a | .14a | 1.36a |
| Student | 10.01b (1.60) | 1.76b (0.71) | 4.57a (0.89) | .82a (0.20) | .92a (0.13) | 1.94b (0.55) | 2.98a (0.70) | 3.02a (1.12) | 2.04b | .25a | .69b | |
| Sex | Male | 10.13a (1.66) | 1.89a (0.63) | 4.47a (0.86) | .79a (0.19) | .91a (0.13) | 2.07a (0.67) | 2.78a (0.66) | 3.17a (1.40) | 1.64a | .34a | .83a |
| Female | 10.66a (1.47) | 2.04a (0,67) | 4.65a (0.85) | .78a (0.19) | .94a (0.11) | 2.25a (0.49) | 3.17b (0.59) | 2.99a (1.05) | 1.68a | .16a | 1.11a | |
| Regional Differences | Europe | 11.08a (1.23) | 2.27a (0.51) | 4.61a (0.82) | .76a (0.17) | .97a (0.08) | 2.47a (0.33) | 3.21a (0.55) | 3.20a (1.05) | 1.30a | .13a | 1.28a |
| North America | 9.92b (1.55) | 1.73b (0.73) | 4.8a (0.86) | .79a (0.21) | .91b (0.14) | 1.90b (0.55) | 3.00a (0.69) | 3.09a (1.11) | 2.22b | .24a | .67a | |
Note: Values in the same row and subtable not sharing the same subscript are significantly different at p<0.05 in the two-sided test of equality for column means. Cells with no subscript are not included in the test. Tests assume equal variances.2
1. This category is not used in comparisons because the sum of case weights is less than two
2. Tests are adjusted for all pairwise comparisons within a row of each innermost subtable using the Bonferroni correction
Self-efficacy
Overall, the mean baseline SE score for participants was 3.08 (sd 0.62). While a trend of higher scores was observed for participants with previous work experience (M = 3.12 vs. 3), those having worked with migrants (M = 3.19 vs. 3.04), and healthcare professionals compared to students (M = 3.17 vs. 2.98), only gender differences in SE baseline scores were statistically significant. Females scored higher than their male counterparts, with a mean baseline score of 3.17 versus 2.78 (p < 0.05). See Tables 3 and 4 for more detailed information.
Knowledge
The baseline mean scores on the knowledge-based multiple-choice test were 3.03 (SD = 1.13). No statistically significant differences were observed at baseline for any of the sociodemographic categories (see Tables 3 and 4).
Pre- and post-intervention analysis
Pre-post analysis using paired t-tests revealed a significant increase in ICC scores compared to baseline (t=-12.64, p < 0.001), with a large observed effect size (Cohen’s d = 1.13). Similarly, all subscale scores exhibited higher averages after the RER intervention, with the largest effect size observed in the Knowledge on Health Disparities subscale (d = 1.57, t=-14.28; p < 0.001), followed by Empathy (d = 0.67 t=-6.92; p < 0.001), Attitudes Toward Factors Contributing to Health Disparities (d = 0.43, t=-4.80; p < 0.001), Importance of ICC Training (0.40, t=-2.99; p < 0.01) and Awareness of Stereotypes (d = 0.21, t=-2.63; p < = 0.05) subscales.
Significant increases were also observed in SE (t=-3.56; p = 0.001) with a moderate effect size (Cohen’s d = 0.38), and in the Knowledge scores (t=-8.40; p < 0.001, respectively) with a large effect size (Cohen’s d = 1.19). See Table 4 for more.
When examining specific sociodemographic groups, students demonstrated greater gains in ICC scores compared to professionals (M = 2.04 vs. 1.27; p < 0.05).
Participant reflections
Acceptability, learning experience and suggestions for improvement of the RER intervention was evaluated through responses to two open-ended questions. The first question, “What did you learn new from this activity?” received a 91% response rate. Responses were grouped into three primary themes: knowledge (65.9%), attitudes (25.3%), and skills (6.6%).
Within the knowledge theme, two key sub-themes emerged: migrant stressors and migration demographics. A significant portion of participants (36.3%) mentioned gaining new insights into the various stressors faced by migrants, including “language barriers” and “factors increasing inequality.” Another 29.7% of respondents highlighted learning about migration demographics, such as the “number of migrants worldwide” and the “magnitude of migratory movements.”
Regarding attitudes, empathy and self-awareness were central. A quarter of participants reflected on the emotional challenges that migrants face. One participant shared:
“It put me in the skin of immigrants and made me feel their sensations although it’s just a game” (Female, Spanish, nurse, 28 years old).
Similarly, another participant noted:
“I learned to be more empathetic towards the immigration process” (Female, North American, undergraduate student, 21 years old).
Several respondents also commented on an increased sense of self-awareness, with one participant stating:
“I was more ignorant than I thought; I was more unknowing about what I thought” (Male, Spanish, nurse, 26 years old).
Another added:
“With a simple game I felt stress, anxiety, frustration, and it’s interesting to be able to translate that to reality” (Female, Spanish, nurse, 23 years old).
A smaller group (6.6%) described how this newly acquired knowledge led to a shift in perspective. One respondent remarked:
“I learned that the immigration crisis is not specific to the US… It changed my perspective on how hard it is to get into another country” (Female, North American, undergraduate student, 21 years old).
The second question, “What aspects of the activity could be improved?” had a 58% response rate. Suggestions were categorized into four themes: Facilitation (22.4%), Content (22.4%), Space (13.8%), and Organization (6.9%). Participants recommended clearer instructions and stronger facilitation to enhance role-playing and a more comprehensive debriefing. Some felt the room was too small, though others acknowledged this may have been intentional to simulate stress. Adjustments to group organization were also suggested.
Overall, the RER intervention was successfully implemented across all sessions, adhering to time constraints and logistical requirements. Participants reported high levels of satisfaction with the immersive and interactive aspects of the experience. The mean satisfaction score was 8.29 (SD = 1.64) out of 10, indicating high levels of satisfaction and acceptability in this educational context.
Discussion
This study contributes to the growing literature [20] on the application of educational escape rooms in healthcare training by demonstrating their effectiveness in addressing critical, real-world issues such as intercultural competence, self-efficacy, and knowledge development among healthcare students and professionals working with VMRs. Consistent with previous research [21, 22, 29], our findings reveal that the immersive and interactive nature of ERs fosters significant learning outcomes by promoting problem-solving, teamwork, and engagement among participants. This study shows that the ER format, specifically tailored to simulate migration-related challenges, offers a novel way to bridge educational gaps in ICC.
Participants reported enhanced knowledge of the health stressors and challenges faced by VMRs, and they demonstrated attitudinal shifts characterized by increased empathy and awareness. The immersive nature of the ER enabled participants to engage deeply with the scenarios, leading to personal insights and a more contextualized understanding of migration-related healthcare challenges.
Previous ICC training initiatives in healthcare have largely focused on traditional workshop formats [5, 6, 30–33], which may lack the engagement and practical application provided by ERs. Our study is one of the first to explore the use of an ER specifically for ICC training, demonstrating significant improvements in participants’ competence, especially among students who started with lower baseline ICC scores. This suggests that ERs can be particularly valuable in helping learners with limited exposure to diverse populations develop crucial cultural competencies.
Notably, participants with prior experience working with migrants displayed higher baseline ICC scores, reinforcing existing literature that links exposure to diverse patient populations with greater cultural sensitivity and awareness [34, 35]. Given that ICC is closely associated with improved healthcare delivery and outcomes for vulnerable populations, the inclusion of ERs in training programs could be a valuable step toward addressing healthcare inequities [7, 8].
However, the concept of ICC remains somewhat ambiguous, and there have been ongoing debates about how best to conceptualize and teach it [34]. As some scholars argue [36], effective ICC training should incorporate a broader understanding of cultural complexity and the social determinants of health. Future iterations of the ER should consider embedding these broader concepts to create a more comprehensive learning experience.
While prior research on educational ERs has often relied on self-reported measures of knowledge retention [37, 38], few studies have objectively tested knowledge acquisition [39]. Our study adds to the evidence base by demonstrating significant improvements in participants’ knowledge scores on a multiple-choice test following the intervention. Although the long-term retention of this knowledge remains to be determined, some reports suggest that such gains may persist over time [40]. Interestingly, there was a discrepancy between participants’ self-assessed knowledge and their actual test performance, particularly among those with prior work experience. This suggests that ERs, through hands-on experience and reflection, can foster more accurate self-assessments, helping participants recognize gaps [41] in their knowledge that may not have been apparent through traditional learning methods [42].
Similar to other experiential-based learning interventions [32, 43, 44], our results show that educational ERs can enhance self-efficacy among participants. The observed increases in SE scores across all sociodemographic groups suggest that the ER experience may strengthen individuals’ beliefs in their abilities to provide culturally sensitive care to VMRs. Given that self-efficacy has been shown to be a predictor of actual behavior change [45], these findings have positive implications for improving healthcare delivery to vulnerable populations [45, 46].
Our sample included a diverse range of participants, including both students and healthcare professionals, which highlights the broad applicability of ERs across different educational and professional contexts. Non-student participants, often overlooked in previous studies [22], showed similar improvements, suggesting that ERs can be valuable tools for professional development as well as student learning.
A critical component of our intervention was the debriefing session following the ER. This reflective practice, led by trained facilitators, provided participants with the opportunity to process their experiences, consolidate learning, and address emotional responses. Debriefing, widely recommended in simulation-based learning [47], is essential for ensuring that participants derive meaningful insights from their ER experience.
Limitations & future research
While our methodology improves upon many published ER interventions [21, 22, 47], we acknowledge significant limitations.
First, the pre-post single-group design without randomization or a control group increases the risk of biases—such as measurement, confounding, and attrition—which limits causal inferences. The absence of long-term follow-up prevents assessing sustained knowledge retention, despite existing literature [40] indicating notable long-term retention through experiential learning.
Second, the lack of a power analysis and the use of convenience sampling likely introduced selection bias. Our sample predominantly consisted of self-selected physicians and students in global health programs, who may have an inherent sensitivity toward migration and health issues. This homogeneity limits the generalizability of our findings to more diverse populations.
Third, although our adapted measurement tool demonstrated acceptable internal validity and reliability, it lacked comprehensive validation. We did not obtain normative data from a representative sample or perform confirmatory factor analysis and concurrent validity assessments. Nonetheless, the tool served our purpose within the study’s scope.
Fourth, intervention-level challenges were identified, including excessive competition that may have intimidated some participants, the need for clearer instructions and stronger facilitation, language barriers in certain sessions, and logistical issues such as planning time and resource costs. These challenges, also noted in other studies, may be intrinsic to the ER format [22].
Recognizing the exploratory nature of this pilot study, future research should adopt more robust designs, such as randomized controlled trials with control groups, to strengthen causal inferences. Incorporating long-term follow-up assessments would enable evaluation of the ICC and SE score gains, aswell as knowledge retention, over time. Expanding sample sizes and employing random sampling methods could improve generalizability. Economic evaluations would help assess cost-effectiveness and inform scalability. Enhancing the qualitative component through methods like focus groups could provide deeper insights into participants’ experiences.
Conclusions
Health professionals have a professional and ethical obligation to provide adequate care for VMRs. Teaching healthcare professionals and students to be more culturally competent may help them become better healthcare providers and, in turn, tackle healthcare access and quality of care barriers affecting the most vulnerable.
While in the last years there has been a notable rise in educational ERs with promising results regarding teamwork, engagement, satisfaction, and communication [29, 47], research on the actual educational significance is still limited. In this paper, we presented an innovative educational ER that effectively expands the significance and utility of ER by exploring its potential impact on the ICC, SE, and Knowledge of healthcare students and professionals that care for VMRs.
There exist ample opportunities to foster synergies between global health, ICC training, and gamification initiatives within the curriculum of healthcare education [10]. Failing to meet the challenges of an increasingly diverse population through intercultural training may continue to broaden health disparities and limit access to health care resources for the most vulnerable patients. While there is a need for more structured research and superior methodological rigor, we hope that the RER intervention here presented is a small albeit important step to building the evidence base for a more effective curriculum that trains healthcare providers about the health challenges faced by VMRs worldwide.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors extend sincere gratitude to all volunteer participants and actors whose invaluable contributions were crucial to the success of the Refugee Escape Room research project. Their dedication and enthusiasm significantly enhanced the project’s outcomes.
Author contributions
NSD, LW: conception of the RER activity. NSD: RER intervention coordination. RM NSD: protocol and survey development. RM, AM: database creation, data monitoring, quantitative analysis. SE: qualitative analysis. NSD, RM, AM, SE: verified results and analytic methods. NSD: Study resources. RM, NSD, AM, SE: wrote the first draft of the manuscript. RM, NSD, SE, AM, LW: writing-review and editing. All authors contributed to the article and approved the submitted version.
Funding
Research reported in this publication was supported by co-funding from the Third EU Health Program (2014–2020) Project Grants (HP-PJ-2016) under Grant Agreement 738091 (MyHealth Consortium).
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approval
This research was evaluated and approved by the Clinical Research Ethics Committee (CEIC) of the Vall d’Hebron Hospital in Barcelona and adhered to the best clinical practices on the 7th of June of 2019.
Consent to participate
All participants gave their consent to participate in this study.
Consent for publication
not applicable.
Authors information
The content of this article is the sole responsibility of the authors and does not necessarily represent the views of any of the sponsoring organizations, institutes, or the European Commission.
Competing interests
The authors declare no competing interests.
Footnotes
Details on the context of the game can be seen at the video which all participants see prior to starting the game: https://www.youtube.com/watch?v=wzq6tc7H46c
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Global Trends to 2030. The future of Migration and Integration. European Strategy and Policy Analysis System; 2018.
- 2.Migration Outlook 2022 Twelve Migration Issues to Look out for in 2022 Origins, Key Events and Priorities for Europe. International Centre for Migration Policy Development; 2022.
- 3.More than 100 million now forcibly displaced: UNHCR report. UN News Global perspective. 2022. Accessed July 10, 2022. https://news.un.org/en/story/2022/06/1120542
- 4.Fleckman JM, Dal Corso M, Ramirez S, Begalieva M, Johnson CC. Intercultural Competency in Public Health: a call for action to Incorporate Training into Public Health Education. Front Public Health. 2015;3. 10.3389/fpubh.2015.00210. [DOI] [PMC free article] [PubMed]
- 5.Asgary R. Graduate public health training in healthcare of refugee asylum seekers and clinical human rights: evaluation of an innovative curriculum. Int J Public Health. 2016;61(3):279–87. 10.1007/s00038-015-0754-z. [DOI] [PubMed] [Google Scholar]
- 6.Crosson JC, Deng W, Chan Tal Brazeau, Boyd L, Soto-Greene M. Evaluating the Effect of Cultural Competency Training on Medical Student attitudes. Acad Med 36(3):515–7. [PubMed]
- 7.Betancourt JR. Cross-cultural medical education: conceptual approaches and frameworks for evaluation. Acad Med. 2003;78(6):560–9. 10.1097/00001888-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Kleinman A, Benson P. Anthropology in the clinic: the Problem of Cultural Competency and how to fix it. PLOS Med. 2006;3(10):e294. 10.1371/journal.pmed.0030294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Migration. and health: enhancing intercultural competence and diversity sensitivity. Published online 2020. Accessed July 10, 2022. https://apps.who.int/iris/bitstream/handle/10665/332186/9789289056632-eng.pdf
- 10.Asgary R, Saenger P, Jophlin L, Burnett DC. Domestic Global Health: a curriculum Teaching Medical students to Evaluate Refugee Asylum seekers and torture survivors. Teach Learn Med. 2013;25(4):348–57. 10.1080/10401334.2013.827980. [DOI] [PubMed] [Google Scholar]
- 11.Ruiz Moral R, García de Leonardo C, Cerro Pérez A, Caballero Martínez F, Monge Martín D. Barriers to teaching communication skills in Spanish medical schools: a qualitative study with academic leaders. BMC Med Educ. 2020;20(1):41. 10.1186/s12909-020-1944-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Escarbajal Frutos A, Leiva Olivencia JJ. La Necesidad De formar en competencias interculturales como fundamento pedagógico: Un estudio en la región de Murcia (España). Profr Rev Currículum Form Profr. 2017;21(1):281–93. 10.30827/profesorado.v21i1.10363. [Google Scholar]
- 13.Vázquez Navarrete ML, Terraza Núñez R, Vargas Lorenzo I, Lizana Alcazo T. Necesidades De Los profesionales de salud en la atención a la población inmigrante. Gac Sanit. 2009;23(5):396–402. 10.1016/j.gaceta.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 14.Terraza-Núñez R, Vázquez LM, Vargas I, Lizana T. Health professional perceptions regarding healthcare provision to immigrants in Catalonia. Int J Public Health. 2011;56(5):549–57. 10.1007/s00038-010-0223-7. [DOI] [PubMed] [Google Scholar]
- 15.Serre-Delcor N, Oliveira I, Moreno R, et al. A cross-sectional survey on professionals to Assess Health needs of newly arrived migrants in Spain. Front Public Health. 2021;9:667251. 10.3389/fpubh.2021.667251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lopez-Pernas S, Gordillo A, Barra E, Quemada J. Examining the Use of an Educational escape room for Teaching Programming in a higher education setting. IEEE Access. 2019;7:31723–37. 10.1109/ACCESS.2019.2902976. [Google Scholar]
- 17.Ahmed M, Sherwani Y, Al-Jibury O, Najim M, Rabee R, Ashraf M. Gamification in medical education. Med Educ Online. 2015;2029536. 10.3402/meo.v20.29536. [DOI] [PMC free article] [PubMed]
- 18.Adams V, Burger S, Crawford K, Setter R. Can you escape? Creating an escape room to facilitate active learning. J Nurses Prof Dev. 2018;34(2):E1–5. [DOI] [PubMed] [Google Scholar]
- 19.Brady SC, Andersen EC. An escape-room inspired game for genetics review. J Biol Educ Published Online 2019:1–12.
- 20.Lafontaine C, Sawchuk K, DeJong S. Social Justice games: building an escape room on elder abuse through Participatory Action Research. Comput Games J. 2020;9(2):189–205. 10.1007/s40869-020-00105-5. [Google Scholar]
- 21.Taraldsen LH, Haara FO, Lysne MS, Jensen PR, Jenssen ES. A review on use of escape rooms in education – touching the void. Educ Inq. 2022;13(2):169–84. 10.1080/20004508.2020.1860284. [Google Scholar]
- 22.Fotaris P, Mastoras T. Escape Rooms for Learning: A Systematic Review. In: Proceedings of the 13th European Conference on Game-Based Learning ECGBL. 2019; 2019:9.
- 23.Harris-Haywood S, Goode T, Gao Y, et al. Psychometric evaluation of a cultural competency assessment instrument for health professionals. Med Care. 2014;52(2):e7–15. 10.1097/MLR.0b013e31824df149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang YW, Davidson MM, Yakushko OF, Savoy HB, Tan JA, Bleier JK. The scale of Ethnocultural Empathy: Development, Validation, and reliability. J Couns Psychol. 2003;50(2):221–34. 10.1037/0022-0167.50.2.221. [Google Scholar]
- 25.Bernhard G, Knibbe RA, von Wolff A, Dingoyan D, Schulz H, Mösko M. Development and psychometric evaluation of an instrument to assess cross-cultural competence of Healthcare professionals (CCCHP). PLoS ONE. 2015;10(12). 10.1371/journal.pone.0144049. [DOI] [PMC free article] [PubMed]
- 26.Wetzel Angela P. Critical Synthesis Package: Clinical Cultural Competency Questionnaire (CCCQ). MedEdPORTAL. 9:9390. 10.15766/mep_2374-8265.9390
- 27.Campinha-Bacote J. The process of Cultural competence in the Delivery of Healthcare Services: a model of care. J Transcult Nurs off J Transcult Nurs Soc. 2002;13(3):181–4. 10.1177/10459602013003003. discussion 200–201. [DOI] [PubMed] [Google Scholar]
- 28.Sue DW. Multidimensional facets of Cultural competence. Couns Psychol. 2001;29(6):790–821. 10.1177/0011000001296002. [Google Scholar]
- 29.Veldkamp A, Knippels MCPJ, van Joolingen WR. Beyond the early adopters: escape rooms in Science Education. Front Educ. 2021;6:622860. 10.3389/feduc.2021.622860. [Google Scholar]
- 30.Carter MM, Lewis EL, Sbrocco T, et al. Cultural Competency Training for Third-Year Clerkship Students: effects of an interactive workshop on Student attitudes. Acad Psychiatry. 2006;30(6):498–505. 10.1176/appi.ap.30.6.498. [PMC free article] [PubMed] [Google Scholar]
- 31.Assessing Change: Evaluating Cultural Competence Education and Training Assessing Change: Evaluating Cultural Competence Education and Training. Association of American Medical Colleges. 2015. Accessed May 13, 2019. www.aamc.org.
- 32.Jin Jhyun, Cleofas JV. A proposed cultural competence training program for nurses based on their transcultural self-efficacy. Int J Adv Cult Technol. 2018;6(2):86–99. 10.17703/IJACT.2018.6.2.86. [Google Scholar]
- 33.Beach MC, Price EG, Gary TL, et al. Cultural competence: a systematic review of health care provider educational interventions. Med Care. 2005;43(4):356–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thackrah RD, Thompson SC. Refining the concept of cultural competence: building on decades of progress. Med J Aust. 2013;199(1):35–8. 10.5694/mja13.10499. [DOI] [PubMed] [Google Scholar]
- 35.Boyer CJ, Rice MJ, Sorrell TR, Spurling AM. Advancing Racial/Ethnic and cultural sensitivity among PMHNP students through Education, Practice, and experience. J Am Psychiatr Nurses Assoc. 2019;25(6):487–95. 10.1177/1078390318824651. [DOI] [PubMed] [Google Scholar]
- 36.Sakamoto I. An anti-oppressive approach to cultural competence. Can Soc Work Rev. 2007;24(1):105–14. [Google Scholar]
- 37.Bartlett KA, Anderson JL. Using an escape room to support the learning of Science Content. Sci Teach 86(7):36–41.
- 38.Dimova G, Videnovik M, Trajkovik V. Using Educational Escape Room to Increase Students’ Engagement in Learning Computer Science. In: 9th Mediterranean Conference on Embedded Computing (MECO). 2020:1–4. 10.1109/MECO49872.2020.9134170
- 39.Fusco NM, Foltz-Ramos K, Ohtake PJ. Interprofessional escape room improves knowledge and collaboration among nursing, pharmacy and physical therapy students. Am J Pharm Educ Published Online Dec. 2021;15:8823. 10.5688/ajpe8823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu C, Patel R, Ogunjinmi B, et al. Feasibility of a paediatric radiology escape room for undergraduate education. Insights Imaging. 2020;11(1):50. 10.1186/s13244-020-00856-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khanna A, Ravindran A, Ewing B, et al. Escape MD: using an escape room as a Gamified Educational and Skill-Building Teaching Tool for Internal Medicine residents. Cureus. 2021;13(9). 10.7759/cureus.18314. [DOI] [PMC free article] [PubMed]
- 42.Kolb A, Kolb D. Learning styles and learning spaces: a review of the multidisciplinary application of experiential learning theory in higher education. Learn Styles Learn Published Online January. 2006;1:45–91. [Google Scholar]
- 43.Mathieson A, Duca E. STEM escape rooms for public engagement. Res all. 2021;5(2). 10.14324/RFA.05.2.10.
- 44.Asurakkody TA. Predictors for transcultural self-efficacy of nursing students: application of ecological model. Health Sci J Published Online 2018:7.
- 45.Bandura A, Adams NE. Analysis of self-efficacy theory of behavioral change. Cogn Ther Res. 1977;1(4):287–310. 10.1007/BF01663995. [Google Scholar]
- 46.Sharifirad G, Azadbakht L, Feizi A, Kargar M, Mohebi S. Review the key role of self-efficacy in diabetes care. J Educ Health Promot. 2013;2(1):36. 10.4103/2277-9531.115827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Veldkamp A, van de Grint L, Knippels MCPJ, van Joolingen WR. Escape education: a systematic review on escape rooms in education. Educ Res Rev. 2020;31:100364. 10.1016/j.edurev.2020.100364. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.