Abstract
Background
Intestinal parasitic (IP) infections caused by helminths are among the most significant public health concerns that mainly affect deprived people in Sub-Sahara African countries. The current study aimed to determine the prevalence and associated risk factors of intestinal parasitic helminths among patients attending Mekaneselam hospital.
Method
In this cross-sectional study conducted from August 2022 to February 2023, stool specimens were collected and examined microscopically to detect intestinal helminths using direct wet-mount and formal-ether concentration techniques. A structured questionnaire was employed to obtain information regarding the socio-demographic characteristics and associated risk factors. Data were analyzed via appropriate univariate and multivariable logistic regression methods using SPSS version 25.0.
Result
The overall prevalence of the parasitic helminths was 51 (12.6%) out of 404 patients attending in Mekaneselam town during the study period. In this study, seven species of intestinal helminths were detected, with Ascaris lumbricoides (5.7%) being the most prevalent followed by Trichuris trichiura (2.2%). Significant positive associations were observed between intestinal helminths infection and the socio-demographic characteristics including marital status (χ2 = 7.97, p = 0.047), educational level (χ2 = 9.34, p = 0.025) and residence (χ2 = 3.90, p = 0.048). The odds of being infected with IP were three times higher among divorced patients than married individuals (AOR = 3.21, CI = 1.15–8.96, p = 0.03). Illiterate individuals were three times (AOR = 2.61, CI = 1.24–5.49, p = 0.011) and those who attended primary school were two times (AOR = 2.3, CI = 1.029–5.143, p = 0.042), more likely to have helminthic infections. Participants who did not wash their hands after using the toilet were five times more likely to acquire IP helminths than those who did (AOR = 4.36, CI = 2.83–6.72, p = 0.000). In the case of the feeding habit, study subjects who ate unwashed vegetables were more likely to acquire helminths than those who did not eat unwashed vegetables (AOR = 5. 43, CI = 4.33–23.77, p = 0.000).
Conclusion
This study highlighted a substantial prevalence of intestinal helminths infections (12.6%) in the study area, warranting the urgent need for attention and interventions from relevant public health authorities.
Keywords: Ascaris lumbricoides, Mekaneselam town, Intestinal parasitic helminths, Prevalence, Risk factors
Introduction
Intestinal parasitic (IP) infections caused by helminths commonly known as neglected tropical diseases, are among the most significant socioeconomic and health problems affecting many people throughout the world [1]. They are the major health concerns responsible for high levels of morbidity and mortality, nutritional deficiency including iron deficiency, seizures, portal hypertension, chronic diarrhea, impaired physical and cognitive developments in children etc. [2]. The most predominant intestinal helminths includes the roundworms (Ascaris lumbricoides), whipworms (Trichuris trichiura), and hookworms (Necator americanus and Ancylostoma duodenale). Other species, such as Schistosoma mansoni, Hymenolepis nana, Enterobius vermicularis (E. vermicularis) and Strongyloides stercoralis, also present public health challenges [3]. More than 1.5 billion people worldwide, or 24% of the world’s population are infected by at least one of the most common intestinal helminths [4]. These infections affect the most deprived communities in low-income countries, with the highest prevalence reported from sub-Saharan Africa, China, South America, and Asia. People from resource-poor settings and children are the most affected population groups. The three intestinal helminths, commonly known as soil transmitted helminths (STH), are responsible for the most common parasitic infections. They are considered as neglected tropical diseases (NTDs). Thus, about 819 million people are infected with Ascaris lumbricoides (A. lumbricoides), 465 million with Trichuris trichiura (T. trichiura), and 439 million with hookworms. Besides, globally about 800 million individuals are at risk of intestinal schistosomiasis, and around 200 million people (of which 160 million live in Sub-Saharan Africa) are estimated to be infected with Schistosoma mansoni (S. manosoni) [5].
These intestinal helminthic infections are among the top ten public health problems in developing countries. Such infection are mostly common in the tropical and subtropical areas of Africa, where access to clean water, hygienic and sanitation facilities are poor [6]. The associated risk factors such as increasing population density, poverty, contaminated food, unhygienic environment, inadequate health services, inadequate health education on mechanisms of transmission, inadequate toilet facilities, low living standards, poor environmental sanitation, unsafe human waste disposal systems, incorrect finger nail trimming, inadequate and unsafe water supplies, low socio economic status and poor deworming practice result in high prevalence rates [7, 8].
To this end, Ethiopia is a country with the lowest quality of drinking water supply (34%) and latrine coverage (7.1%) in the world. More than half of the population in the country still uses open defecation, and most individuals in urban settings utilize unimproved sanitation facilities [9, 10]. Hence, the prevalence of IPs in Ethiopia is unacceptably high infecting more than half of the population. In Ethiopia around 81 million people live in endemic areas of STH infections, of which 25.3 million are school-age children [5]. For instance, based on the trend analysis of soil-transmitted helminths in Ethiopia (2000–2018), the pooled prevalence of intestinal parasites was 52.0%, where Amhara region with the highest in prevalence rate (60.3%). Among the helminthic infections reported in this study, Ascaris lumbricoides (11.2%) was the highest in pooled prevalence followed by hookworms (10.4%) and Trichuris trichiura (3.6%) [11]. However, a systematic review and meta-analysis conducted in 2022, on intestinal helminths parasitic infections in Ethiopia reported the pooled prevalence of intestinal helminthic infections in Ethiopia as 33.35%, with Ascaris lumbricoides the highest in prevalence rate (10.84%) [12]. Another study in 2022 reported the pooled prevalence of STH infections in Ethiopia as 36.78% where Ascaris lumbricoides had the highest pooled prevalence of 17.63%, followed by hook worm and Trichuris trichiura with a prevalence rate of 12.35% and 7.24% respectively [13]. These findings are against the national goal set by Federal Ministry of Health to eliminate the three STHs (ascariasis, hookworm infection, and trichuriasis) as public health problems by 2025 [14].
The predisposing factors associated with the high prevalence rate of intestinal parasitic infections in Ethiopia are similar to other Sub-Sahara African countries [15]. For instance, in a recent study conducted in northwest Ethiopia, the overall prevalence of intestinal parasite infection in schoolchildren was 58%, of these parasitic infections, prevalence of hookworm’s accounts (13.8%), S. mansoni (10.3%), Hymenolepis nana (H. nana) (4.2%), Taenia species 3% and A. lumbricoides 0.73% [16]. Another cross sectional study conducted in Shahura health center, northwest Ethiopia revealed the overall prevalence of intestinal parasite infection in patient was 56.9%; among the detected parasites, the prevalence of hookworm species was (11.8%), A. lumbricoides (2.2%), and S. mansoni 1.4% [17].
To address the burden of intestinal parasitic helminths, Ethiopia has implemented several control programs and interventions, focusing on both preventive measures and treatment strategies. The nation carries out mass drug administration (MDA) campaigns targeting at-risk populations, particularly school-age children. MDA campaigns have demonstrated success in reducing the prevalence and intensity of helminths infections in various regions of Ethiopia [18]. Besides, water, sanitation, and hygiene (WASH) interventions enhancing access to clean water, adequate sanitation facilities, and promoting good hygiene practices. WASH programs involve the construction of latrines, provision of safe drinking water sources, and hygiene education to promote hand washing and proper waste disposal. These interventions have shown positive results in improving sanitation and hygiene practices, although challenges in sustainability and coverage remain [19]. In this regard, the recent review (2020) specifically on the prevalence of STH infection in school age children reported that the pooled prevalence of STH reduced from 35.9% to 30.6% after the launch of the national STH control program in Ethiopia. However, more than one-third of the school age children in Ethiopia are still harbouring STH infections [20].
Although several studies have been conducted on the distribution and prevalence of intestinal helminths in Ethiopia, there are still several specific localities for which adequate epidemiological information is not available [21]. Therefore, studies on the prevalence of intestinal helminthic infections in various untouched geographic areas are vital for developing proper control policies. In this regard, the Amhara region is the second most populous region in Ethiopia, where intestinal helminthic infections are listed as the top reasons for people visiting the health centers in the region. Nevertheless, there are no sufficient studies conducted on the prevalence and associated risk factors of IP helminths in most parts of the districts in the region, of which Mekaneselam town is among those neglected areas. There is no sufficient data on the prevalence and associated risk factors of intestinal parasitic helminths infection in this unnoticed district.
Therefore, based on the gaps and needs, the current study aimed to determine the prevalence rate of intestinal helminths and their associated risk factors, among patients attending Mekaneselam hospital south Wollo, Amhara region, Ethiopia. The findings of the study provide information on the most vulnerable groups for intestinal parasitic helminths and on significant predictors of the infections. The outcome of this study can significantly support health officials to plan intervention programs in order to minimize the burden of the disease by identifying the risk factors. Additionally, it can guide public health officers on prevention and control strategies for intestinal helminthic infections in Mekaneselam town. Furthermore, it may serve as a stepping stone for other interested researchers to conduct more extensive studies on this topic in the stated specific localities.
Materials and methods
Study area
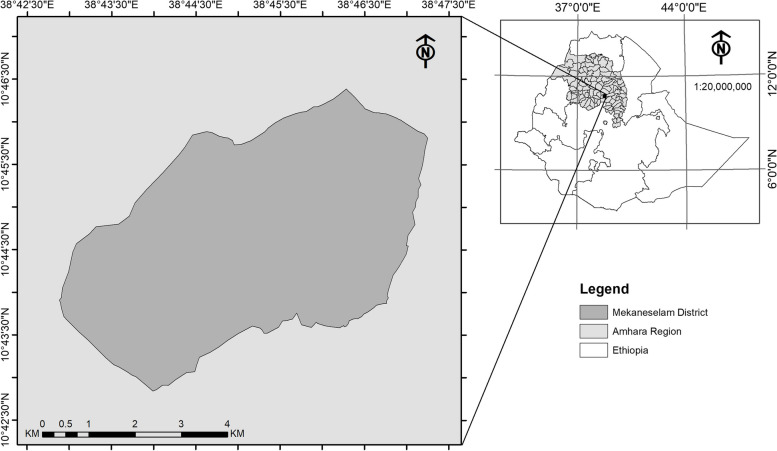
The study was conducted at Mekaneselam town, south Wollo, Ethiopia. It is located at the geographical coordinates of 10° 42′ 30′′-10o 46′ 30′′ N and 38° 42′ 30′′- 38° 47′ 30′′ E, northeast from Addis Ababa at about 580 kms (Fig. 1). Based on Mekaneselam town land administration (MTLA) office annual report in 2022, the elevation of the study area is around 1827 m above sea level [22]. The total population of the town is 101,592, of which 51,305 are males and 50,287 females [23]. The Borena Woreda Agricultural Bureau (BWAB) annual report indicated that climatic condition of Mekaneselam is sub-tropical (“woinadega”), with the average rain fall of 1270 mm in the main rainy season (June- August), and mean daily temperature of 23 °C [24].
Fig. 1.
Location map of the study area
Information about the elevation, climate, and rainfall is relevant to the study of intestinal parasitic helminths, because these factors can influence the prevalence and transmission of these parasites. For instance elevation can affect the distribution of helminths because different species of helminths have specific environmental requirements. For example, certain helminth species may thrive in low-lying areas or regions with high humidity, while others may prefer higher elevations or drier climates. Besides, climate can directly or indirectly affect the survival, development, and transmission of intestinal parasitic helminths. For instance, temperature can influence the development and viability of helminths eggs and larvae. Some helminths require specific temperature ranges for their eggs to hatch and larvae to survive. Furthermore, rainfall patterns are crucial for the survival and distribution of helminths, particularly those that rely on external environments outside the host. Adequate rainfall can create suitable conditions for helminths eggs and larvae to thrive in the environment. Heavy rainfall can increase soil moisture, creating favorable breeding grounds for certain helminths vectors, such as flies. These vectors can transmit helminths larvae to humans through contaminated food and water. Moreover, rainfall can impact the availability and quality of water sources, which can influence the transmission of waterborne helminths.
Study design and population
A cross-sectional study design was employed to determine the prevalence of intestinal parasitic helminths and associated risk factors among patients attending Mekaneselam primary hospital from August 2022 to February 2023. In this study, the source population were all residents living in Mekaneselam town; and the study population comprised patients visiting Mekaneselam primary hospital and requested for stool sample examination by a doctors during the study period.
Sample size determination and sampling technique
For this particular study, the sample size (n) was determined using the single population proportion formula for cross sectional study [25].
where; n = the required sample size;
z = standard value;
p = expected prevalence of intestinal parasite infection in the study area;
d = marginal error, at 95% confidence interval Z = 1.96 and d = 5%.
Since there was no similar study previously conducted in the study area, 50% prevalence rate of IPIs was assumed, assuming that IP helminths are significantly prevalent among patients attending Mekaneselam primary hospital. Therefore, by substituting the values in the formula, the required number of sample size (n) was calculated as, n = (1.96)2*0.5 (1–0.5)/ (0.05)2 = 384. To compensate for the non-respondents and to minimize errors arising from non-compliance, 5% of the sample size was added giving a final sample size of 404. Simple random sampling technique was employed to include all consented patients requesting stool examination until the achievement of the expected sample size was obtained in Mekaneselam primary hospital during the study period.
Data collection methods
Questionnaires
A structured questionnaire was developed to collect data on socio-demographic characteristics and potential risk factors associated with intestinal parasitic helminths. The questionnaire was initially drafted in English, translated into Amharic (the local language) by a language expert, and then back-translated into English to ensure consistency and clarity. This translated version was then pre-tested on a sample of 20 patients (5% of the study subjects) not included in the main study to assess its clarity, comprehensibility, and cultural appropriateness. Based on the pre-test feedback, minor modifications were made to the wording and sequencing of questions. The final questionnaire captured information on variables such as age, sex, residence, marital status, education level, occupation, income, latrine availability and usage, sources of drinking water, shoe-wearing habits, and hygiene practices. Hand washing habits were assessed by asking participants about the frequency of hand washing with soap and water before meals and after using the toilet. Similarly, consumption of unwashed vegetables was determined by asking participants about their frequency of consuming raw vegetables without washing them thoroughly.
Microscopic examination
Stool sample collection procedures
Fresh stool samples were collected from 404 study subjects by experienced laboratory technologists from Mekaneselam primary hospital. The participants were instructed properly and given clean labeled stool collection cups along with applicator sticks, and informed to bring sufficient stool enough for direct saline wet mount and formal-ether concentration technique. At the time of collection, the date of sampling, the participants name, age, and sex was recorded for each subject on a recording format.
Direct wet mount method
A small portion of the stool sample (about 2 mg equivalent to the size of a match head) was emulsified with normal saline (0.85% NaCl solution). Then, a drop of the emulsified sample was placed on a clean microscopic glass slide, a few drops of iodine solution were added to the stool sample, mixed with this reagent, then it was covered with a cover slip at an angle of 45° [26]. Finally, the samples were examined using light microscope under 10 × and 40 × objective lenses by experienced laboratory technologists from Mekaneselam primary hospital.
Formal-ether concentration method
A portion of the stool sample was processed by the formal-ether concentration technique. In brief, using an applicant stick, about 1–1.5 g of stool sample was placed in a clean 15 ml conical tube containing 10 ml of 10% formalin. The sample was suspended and mixed thoroughly with the applicant stick. The resulting suspension was filtered through mesh sieve (2 layers of wet surgical cotton gauze) into a beaker, and the filtrate was poured into the same tube. 10% of formalin was added to the suspension to bring the volume to 10 ml. Subsequently, 3 ml of ether was added to the mixture and hand shaken vigorously for 10 s; the content was centrifuged at 500 g for 3 min. The three upper layers were poured off in a single movement in five seconds. Iodine stain preparation was made from the sediments that have mixed with a drop of saline. Finally, the entire area under the cover slip was examined using 10 × and 40 × objective lenses under the microscope [26].
Methods of data analysis
Throughout the process of data collection, thorough checks were conducted to ensure the completeness, appropriateness, and precision of every answer while gathering data through the questionnaire and during putting it into MS Excel. The collected data was analyzed using SPSS Version 22. Descriptive statistics and Chi square statistical tests were used to assess presence and absence of association between risk factors and IP helminthic infections. Univariate logistic regression analysis was used for analyzing socio demographic factors and personal lifestyle associated with IP helminths. Furthermore, risk factors associated with IP helminths was analyzed by multivariate logistic regression. Then, COR was calculated as it is crucial in interpreting the magnitude and direction of relationships between variables, where COR represents the expected change in the dependent variable for each one-unit increase in the independent variable, while holding other variables constant. Furthermore, the Adjusted Odds Ratio (AOR) was used to measure the impact of predictor variables on the odds of a binary outcome. The AOR indicates the change in odds associated with a one-unit increase in the predictor variable, adjusted for the influence of other variables in the model. The p-value for all tests was set at p ≤ 0.05. Summary of statistical interpretation and percentage values are presented in Tables.
Results
Socio-demographic characteristics of the study participants
Among the 404 study subjects, 210 (52%) were males and 194 (48%) were females. Regarding their age categories, 72 (17.8%), 133 (32.9%) and 199 (49.3%) of the study participants were in the age groups 5–14 years, 15–24 years, and ≥ 25 years, respectively. In the case of residence area, 168 (41.6%) of the study subjects were urban and 236 (58.4%) were rural dwellers. The marital status of the study participants was 124 (30.7%) single, 243 (60.1%) married, 28 (6.9%) divorced and 9 (2.2%) were widowed. Out of the total 404 respondents, 204 (50.5%), 95 (23.5%), 57 (14.1%), 48 (11.9%) respondents were illiterate, attended primary school, secondary school, and diploma and above, respectively (Table 1).
Table 1.
Socio-demographic characteristics of study participants (n = 404)
| Characteristics | Categories | Frequency (n) | Percentage (%) | |
|---|---|---|---|---|
| Sex | Male | 210 | 52 | |
| Female | 194 | 48 | ||
| Age group | 5-14 | 72 | 17.8 | |
| 15-24 | 133 | 32.9 | ||
| Residence | ≥ 25 | 199 | 49.3 | |
| Urban | 168 | 41.6 | ||
| Rural | 236 | 58.4 | ||
| Marital status | Single | 124 | 30.7 | |
| Married | 243 | 60.1 | ||
| Divorced | 28 | 6.9 | ||
| Widowed | 9 | 2.2 | ||
| Education level | Illiterate | 204 | 50.5 | |
| Primary school | 95 | 23.5 | ||
| Secondary school | 57 | 14.1 | ||
| Diploma &above | 48 | 11.9 | ||
| Occupational status | Government employer | 80 | 19.8 | |
| Merchant | 28 | 6.9 | ||
| Farmer | 196 | 48.5 | ||
| House wife | 22 | 5.4 | ||
| Student | 78 | 19.3 | ||
| Family size | ≤ 3 | 162 | 40.1 | |
| 4-6 | 176 | 43.6 | ||
| 7-9 | 39 | 9.7 | ||
| >9 | 27 | 6.7 | ||
| Income level in ETB | Lower (<3000) | 216 | 53.5 | |
| Medium (3000-5000) | 96 | 23.8 | ||
| High (>5000) | 92 | 22.8 | ||
Prevalence of some identified intestinal parasitic helminths infections
Out of the 404 study subjects, 51 were positive for helminthic cases, and the overall prevalence rate of parasitic helminths infection was 12.6%. Based on the microscopic examination of stool specimens, seven intestinal parasitic helminths were identified. In this study A. lumbricoides accounted for 23 (5.7%), T. trichiura 9 (2.2%), E. vermicularis 7(1.7%), hookworm species 5(1.2%), H. nana 5(1.2%), S. mansoni 1(0.2%), and the cases for Taenia species was 1(0.2%) (Table 2). However, double and triple parasitic infections were not recorded. The overall intestinal helminths prevalence was higher among males 34 (8.4%) than females 17 (4.2%). On the other hand, the highest percentage of A. lumbricoides prevalence was found also in male participants (Table 2).
Table 2.
Socio-demographic characteristics (sex and age) of patients and the identified helminths (n = 404)
| Types of Intestinal Parasites | Sex | Age | |||||
|---|---|---|---|---|---|---|---|
| Male + ve (%) (%) |
Female + ve (%) |
Total + ve |
5–14 + ve (%) (%) |
15–24 + ve (%) |
> 25 + ve (%) | Total + ve |
|
| A.lumbricoides | 17(4.2) | 6(1.5) | 23(5.7) | 9(2.2) | 8(2.0) | 6(1.5) | 23(5.7) |
| E.vermicularis | 5(1.2) | 2(0.5) | 7(1.7) | 2(0.5) | 4(1.0) | 1(0.2) | 7(1.7) |
| T.trichiura | 5(1.2) | 4(1.0) | 9(2.2) | 2(0.5) | 4(1.0) | 3(0.8) | 9(2.2) |
| Hookworms | 3(0.8) | 2(0.5) | 5(1.2) | 0 | 1(0.2) | 4(1.0) | 5(1.2) |
| H.nana | 3(0.8) | 2(0.5) | 5(1.2) | 0 | 1(0.2) | 4(1.0) | 5(1.2) |
| Taenia species | 0 | 1(0.2) | 1(0.2) | 0 | 1(0.2) | 0 | 1(0.2) |
| S.mansoni | 1(0.2) | 0 | 1(0.2) | 0 | 1(0.2)) | 0 | 1(0.2) |
| Total | 34(8.4) | 17(4.2) | 51(12.6) | 13(3.2) | 21(5.2) | 17(4.2) | 51(12.6) |
Prevalence of intestinal helminths infections in relation to different socio-demographic characteristics
The findings revealed significant positive association between infection of intestinal helminths and some socio-demographic characteristics of the study participants. For instance, regarding the marital status divorced individuals had a significantly higher prevalence (χ2 = 7.97, p = 0.047). In the case of educational level illiterate individuals had a significant higher prevalence rate (χ2 = 9.34, p = 0.025) and residence (χ2 = 3.90, p = 0.048). However, with regard to sex, there was no statistically significant difference in the prevalence of intestinal helimnths infections between male and female (χ2 = 5.04, p = 0.16), age (χ2 = 0.63, p = 0.731). Similarly, occupation status (χ2 = 4.07, p = 0.396), family size (χ2 = 2.77, p = 0.429), and monthly income level χ2 = 3.57, p = 0.168) had no statistically significant association with intestinal helminths infections (Table 3).
Table 3.
Prevalence of intestinal parasitic helminths in relation to different socio demographic factors (n = 404)
| Risk factors | Categories | N (%) | Positive (%) | Negative (%) | χ2, p –value |
|---|---|---|---|---|---|
| Sex | Male | 210(52) | 34(16.2) | 176(83.8) | 5.04, 0.16 |
| Female | 194(48) | 17(8.8) | 177(91.2) | ||
| Age group | 5–14 | 72(17.8) | 13(18.1) | 59(81.9) | 0.63, 0.731 |
| 15–24 | 133(32.9) | 21(15.8) | 112(84.2) | ||
| ≥ 25 | 199(49.3) | 17(8.5) | 182(91.5) | ||
| Residence | Urban | 168(41.6) | 16(9.5) | 152(90.5) | 3.90, 0.048* |
| Rural | 236(58.4) | 35(14.8) | 201(85.2) | ||
| Marital status | Married | 243(60.1) | 22(9.1) | 221(90.9) | |
| Single | 124(30.7) | 18(14.5) | 106(85.5) | 7.97, 0.047* | |
| Divorced | 28( 6.9) | 9(32.1) | 19(67.9) | ||
| Widowed | 9(2.2) | 2(22.2) | 7(77.8) | ||
| Educational | Illiterate | 204(50.5) | 31(15.2) | 173(84.8) | |
| Level | Primary | 95(23.8) | 12(12.6) | 83(87.4) | 9.34, 0.025* |
| Secondary | 57(14.1) | 6(10.5) | 51(89.5) | ||
| Diploma and above | 48(11.9) | 2(4.2) | 46(95.8) | ||
| Income level | < 3000 | 216(53.5) | 36(16.7) | 180(83.3) | 3.57, 0.168 |
| 3000–3000 | 96(23.8) | 13(13.5) | 83(84.5) | ||
| > 5000 | 92(22.8) | 2(2.2) | 90(97.8) | ||
| Risk factors | Categories | N (%) | Positive (%) | Negative (%) | χ2, p –value |
| Family size | ≤ 3 | 162(40.1) | 17(10.5) | 145(89.5) | 2.77, 0.429 |
| 4–6 | 176(43.6 | 21(11.9) | 155(88.1) | ||
| 7–9 | 39(9.7) | 9(23.1) | 30(76.9) | ||
| > 9 | 27(6.7) | 4(14.8) | 23(85.2) | ||
| Occupation status | Government | 80(19.8) | 3(3.8) | 77(96.2) | 4.07, 0.396 |
| employers | |||||
| Merchants | 27(6.7) | 5(18.5) | 22(81.5) | ||
| Farmers | 196(48.5) | 22(11.2) | 174(88.8) | ||
| House wives | 22(5.4) | 5(22.7) | 17(77.3) | ||
| Students | 78(19.3) | 16(20.5) | 62(79.5) |
*Statistically significant association between socio-demographic factors (p < 0.05)
Risk factors associated with intestinal parasitic infection
Socio-demographic factors
Univariate analysis of the socio-demographic characteristics exhibited that patients coming from rural areas were two times more likely to be infected with IP helminths than patients coming from urban areas (COR = 6.70, CI = 4.49–9.98, p = 0.049). Regarding the marital status, divorced patients were three times more infected with IPIs than those who were married (COR = 2.73, CI = 1.03–7.19, p = 0.009); illiterate patients were four times more likely to be infected with IP helminths than patients who attended diploma and above (COR = 2.77, CI = 1.37–5.63, p = 0.005), patients who attended primary school were three times (COR = 2.37, CI = 1.10–5.13, p = 0.027), and patients who attended secondary school were two times more likely to have the helminthic infection than patients who were diploma and above (COR = 3.10, CI = 1.35–7.16, p = 0.008) respectively (Table 4).
Table 4.
Univariate logistic regression analysis for socio demographic factors associated with IP helminths
| Risk factors | Categories | N (%) | IPIs | COR, 95% CI, p-value | ||
|---|---|---|---|---|---|---|
| Positive | Negative | |||||
| (%) | (%) | |||||
| Sex | Male | 210(52) | 34(16.2) | 176(83.5) | , 0.68–1.49, 0.987 | |
| Female | 194(48) | 17(8.8) | 177(91.2) | 1 | ||
| Age group | 5–14 | 72(17.8) | 11(15.3) | 61(84.7) | 0.79, 0.45–1.41, 0.429 | |
| 15–24 | 133(32.9) | 17(12.3) | 116(87.2) | 0.86, 0.49–1.47, 0.571 | ||
| ≥ 25 | 199(49.3) | 23(11.6) | 176(88.4) | 1 | 0.731 | |
| Residence | Urban | 168(41.6) | 16(9.5) | 152(90.5) | 1 | |
| Rural | 236(58.4) | 35(14.8) | 201(85.2) | 6.70, 4.49–9.98, 0.049* | ||
| Marital | Married | 243(60.1) | 22(9.1) | 221(90.9) | 1 | 0.061 |
| Status | Single | 124(30.7) | 18(14.5) | 106(85.5) | 0.80, 0.52–1.23, 0.313 | |
| Divorced | 28(6.9) | 9(32.1) | 19(67.9) | 2.73,1.03–7.19, 0.009* | ||
| Widowed | 9(2.2) | 2(22.2) | 7(77.8) | 1.25, 0.32–4.88, 0.748 | ||
| Educational | Illiterate | 204(50.5) | 31(15.2) | 173(84.8) | 2.77, 1.37–5.63, 0.005* | |
| Primary | 95(23.8) | 12(12.6) | 83(87.4) | 2.37, 1.10–5.13, 0.027* | ||
| Secondary | 57(14.1) | 6(10.5) | 51(89.5) | 3.10, 1.35–7.16, 0.008* | ||
| Diploma and | 48(11.9) | 2(4.2) | 46(95.8) | 1 | 0.032 | |
| Above | ||||||
| Income level | < 3000 | 216(53.5) | 36(16.7) | 180(8.3) | 1.05, 0.64–1.73, 0.834 | |
| 3000–5000 | 96(23.8) | 13(13.5) | 83(86.5) | 1.61, 0.90–2.87, 0.105 | ||
| > 5000 | 92(22.8) | 2(2.2) | 90(97.8) | 1 | 0.170 | |
| Family size | ≤ 3 | 162(40.1) | 17(10.5) | 145(89.5) | 1 | 0.434 |
| 4–6 | 176(43.6) | 21(11.9) | 155(88.1) | 1.90, 0.81–4.49, 0.141 | ||
| 7–9 | 39(9.7) | 9(23.1) | 30(76.9) | 1.56, 0.66–3.65, 0.310 | ||
| > 9 | 27(6.7) | 4(14.8) | 23(85.2) | 1.39, 0.50–3.87, 0.527 | ||
| Occupation | Government | 80(19.8) | 3(3.7) | 77(96.3) | 1 | 0.401 |
| Status | Employers | |||||
| Merchants | 27(6.7) | 5(18.5) | 22(81.5) | 0.75, 0.32–1.77, 0.505 | ||
| Farmers | 196(48.5) | 22(11.2) | 174(88.7) | 0.59, 0.35–1.00, 0.051 | ||
| House wives | 22(5.4) | 5(22.7) | 17(77.3) | 0.59, 0.23–1.55, 0.289 | ||
| Students | 78(19.3) | 16(20.5) | 62(79.5) | 0.74, 0.39–1.38, 0.340 | ||
Frequency and percentage values are presented in parentheses
1 = reference value, * = statistically significant at p < 0.05, COR Crude odds ratio, N = Total. The p-value for the variable more than two categories in front of reference value for the comparison to entered for multivariate analysis
Personal life style
Life style related factors such as habit of eating unwashed vegetables and frequency of shoe wearing had statistically significant associations with intestinal helminths infections. The study subjects who ate unwashed vegetables were more likely to be infected with intestinal helminths than those who did not eat unwashed vegetables (COR = 4.90, CI = 3.28–7.32, p = 0.000). Similarly, study subjects who wear shoes sometimes were more likely to be infected with IP helminths than those who always wear shoes (COR = 5.73, CI = 3.72–8.83, p = 0.012) (Table 5).
Table 5.
Univariate logistic regression analysis for personal life style associated with intestinal parasitic helminths
| Risk factors | Categories | N (%) | IP helminths | COR, 95% CI, P-value | |
|---|---|---|---|---|---|
| Positive (%) | Negative (%) | ||||
| Hand washing | Yes | 393(97.3) | 42(10.7) | 351(89.3) | 1 |
| before food | No | 11(2.7) | 9(81.8) | 2(18.2) | 0.69, 0.20–2.42, 0.570 |
| Frequency of hand | Always | 223(55.2) | 31(13.9) | 192(86.1) | 1 |
| Washing before food | Sometimes | 170(42.1) | 20(11,8) | 150(88.2) | 0.67, 0.45–1.00, 0.51 |
| Shoe wearing habit | Yes | 394(97.5) | 45(11.4) | 349(88.6) | 1 |
| No | 10(2.5) | 6(60.0) | 4(40.0) | 0.30, 0.63–1.43, 0.131 | |
| Frequency of shoe | Always | 304(77.2) | 37(12.2) | 267(87.8) | 1 |
| Wearing | Sometimes | 90(22.8) | 14(15.6) | 76(84.4) | 5.73, 3.72–8.83, 0.012* |
| Habit of soil | Yes | 151(37.7) | 23(15.2) | 128(84.8) | 0.69, 0.465–1.03, 0.068 |
| Contact | No | 253(62.3) | 28(11.0) | 225(89.0) | 1 |
|
Habit of eating unwashed vegetable |
Yes | 184(45.5) | 29(15.7) | 155(84.2) | 4.90, 3.28–7.32, 0.000* |
| No | 220(54.5) | 22(10.0) | 198(90.0) | 1 | |
|
Habit of eating raw Meat |
Yes | 100(24.8) | 40(40.0) | 60(60.0) | 1.13, 0.72–1.77, 0.610 |
| No | 304(75.2) | 11(3.6) | 295(97.4) | 1 | |
| Habit of water | Yes | 257(63.6) | 43(16.7) | 214(83.3) | 0.64, 0.36–1.12, 0.118 |
| Contact | No | 147(36.4) | 8(5.4) | 139 (94.6) | 1 |
Frequency and percentage values are presented in parentheses
1 = reference value, * = statistically significant at p < 0.05, COR Crude odds ratio, N = Total
Personal hygiene
Hygiene related factors such as presence of finger trimming (decoration), presence of latrine at home, habit of hand washing after using toilet, and frequency of hand washing after visiting toilet were significantly associated with IP helminths (Table 6). Patients who had finger trimming were more likely to be infected with IP helminths than those who did not have finger trimming (COR = 5.17, CI = 3.43–7.78, p = 0.002); patients who did not have latrine at home were three times more likely to be infected with IP helminths than those who had latrine at home (COR = 5.46, CI = 3.66–8.17, p = 0.003); Similarly, those patients who did not wash their hands after toilets were five times more likely to acquire IP helminths than those who washed their hands after using toilet (COR = 4.63, CI = 3.11–6.90, p = 0.000) (Table 6).
Table 6.
Univariate logistic regression analysis for personal hygiene associated with intestinal parasitic helminths
| Variables | Categories | N (%) | IP helminths | COR, 95% CI,p-value | |
|---|---|---|---|---|---|
| Positive (%) | Negative (%) | ||||
| Presence of Finger trimming | Yes | 162(40.1) | 22(13.5) | 140(86.5) | 5.17, 3.43–7.78, 0.002* |
| No | 242(59.9) | 29(11.9) | 213(88.1) | 1 | |
|
Presence of latrine at Home |
Yes | 164(40.6) | 11(6.7) | 153(93.3) | 1 |
| No | 240(59.4) | 40(16.7) | 200(83) | 5.46, 3.66–8.17, 0.003* | |
|
Frequency of use latrine at home |
Always | 64(15.5) | 4(6.2) | 60(93.8) | 1 |
| Sometimes | 100(24.8) | 7(7.0) | 93(93.0) | 0.62, 0.33–1.17, 0.136 | |
| Personal hygiene | Good | 302(74.8) | 29(9.6) | 273(90.4) | 1 |
| Poor | 102(25.2) | 22(21.6) | 80(78.4) | 6.20, 4.17–9.20,0.018* | |
|
Habit of hand washing after using toilet |
Yes | 192(47.5) | 9(4.7) | 183(95.3) | 1 |
| No | 212(52.5) | 42(19.8) | 170(88.2) | 4.63, 3.11–6.90, 0.000* | |
|
Frequency hand washing after using toilet |
Always | 170(88.5) | 3(1.8) | 167(98.4) | 1 |
| Sometimes | 22(11.5) | 6(27.3) | 16(72.7) | 0.91, 0.36–2.26, 0.832 |
Frequency and percentage values are presented in parentheses
1 = reference value, * = statistically significant at p < 0.05, COR Crude odds ratio. N = Total
Multivariate logistic regression analysis of selected variables
Among the potential risk factors educational status, habit of hand washing after toilet, habit of eating unwashed vegetable, and presence of finger trimming were significantly associated with IP helminths infection (p < 0.05). The odds of being infected with IP helminths in those divorced patients were three times more than those who were married (AOR = 3.21, CL = 1.15–8.96, p = 0.03). Regarding the educational level illiterate patients were four times more likely to have parasite infection (AOR = 2.61, CI = 1.24–5.49, p = 0.011); but patients who attended primary school were three times (AOR = 2.3, CI = 1.029–5.143, p = 0.042), and those who completed secondary schools were three times (AOR = 3.44, CI = 1.43–8.30, p = 0.006) more likely to have IP helminths infection than patients who were diploma and above respectively. Those participants who did not wash their hands after toilet were five times more likely to acquire IP helminths than their counterparts (AOR = 4.36, CI = 2.83–6.72, p = 0.000). Regarding the feeding habit, study subjects who ate unwashed vegetables were more likely to acquire helminths than those who did not eat unwashed vegetables (AOR = 5. 43, CI = 4.33–23.77, p = 0.000). Similarly, patients who have finger trimming (decoration) were more likely infected with helminths than those have no finger trimming (AOR = 5.63, CI = 2.60–11.32, p = 0.001). Moreover, participants who had poor personal hygiene were more likely to acquire IP helminths than those who had good personal hygiene (AOR = 7.01, CI = 4.35–8.95, p = 0.015) (Table 7).
Table 7.
Multivariate logistics regression analysis of selected risk factors associated with IP helminths
| Risk factors | Categories | N (%) | IP helminths | AOR, 95%CI,P -value | |
|---|---|---|---|---|---|
| Positive (%) | Negative (%) | ||||
| Marital status | Married | 243(60.1) | 22(9.1) | 221(90.9) | 1 |
| Single | 124(30.7) | 18(14.5) | 106(85.5) | 0.92, 0.57–1.49, 0.739 | |
| Divorced | 28(6.9) | 9(32.5) | 19(67.5) | 3.21, 1.15–8.96, 0.030* | |
| Widowed | 9(2.2) | 2(22.2) | 7(77.8) | 1.47, 0.35–6.20, 0.602 | |
|
Educational Level |
Illiterate | 204(50.5) | 31(15.9) | 173(84.8) | 2.61, 1.24–5.49, 0.011* |
| Primary | 95(23.8) | 12(12.6) | 83(87.3) | 2.30,1.03–5.14, 0.042* | |
| Secondary | 57(14.1) | 6(10.5) | 51(89.5) | 3.44, 1.43–8.30, 0.006* | |
| Diploma and | 48(11.9) | 2(4,2) | 46(95.8) | 1 | |
| Above | |||||
| Income level | < 3000 | 216(53.5) | 36(9.0) | 180(45.5) | 0.834, 0.485–1.432 0.510 |
| 3000–5000 | 96(23.8) | 13(3.2) | 83(20.5) | 1.470, 0.780–2.769, 0.233 | |
| > 5000 | 92(22.8) | 2(0.5) | 90(22.3) | 1 | |
|
Habit of hand washing after toilet |
Yes | 192(47.5) | 9(4.7) | 183(95.3) | 1 |
| No | 212(52.5) | 42(19.8) | 170(88.2) | 4.36,2.83–6.72, 0.000* | |
|
Habit of eating Unwashed vegetable |
Yes | 184(45.5) | 29(15.7) | 155(84.2) | 5.43, 4.33–23.77, 0.000* |
| No | 220(54.5) | 22(10.0) | 198(90.0) | 1 | |
|
Presence of finger Trimming |
Yes | 162(40.1) | 22(13.5) | 140(86.5) | 5.63,2.60–11.32, 0.001* |
| No | 242(59.9) | 29(11.9) | 213(88.1) | 1 | |
|
Reason of water Contact |
Swimming | 66(16.3) | 9(13.6) | 57(86.4) | 1 |
| Washing cloth | 118(29.2) | 10(8.5) | 108(91.5) | 0.912, 0.470–1.769, 0.784 | |
| Irrigation | 36(8.9) | 4(11.1) | 32(88.9) | 0.428, 0.19–0.94, 0.035* | |
| Washing body | 127(31.4) | 20(15.7) | 107(84.3) | 0.499, 0.26–0.98, 0.042* | |
| Personal hygiene | Good | 302(74.8) | 29(9.6) | 273(90.4) | 1 |
| Poor | 102(25.5) | 22(21.6) | 80(78.4) | 7.01, 4.35–8.95, 0.0145* |
Frequency and percentage values are presented in parentheses
1 = reference value,*= statistically significant at p < 0.05,
AOR adjusted odds ratio (multivariate regression model), N = Total
Discussion
Understanding the epidemiological status of IP helminths and identifying their risk factors in a given local community found to be a prerequisite for planning intervention programs. In line with this perspective, the present study attempted to assess the prevalence of different intestinal parasitic helminths and the associated risk factors among patients attending Mekaneselam hospital. In this study, the overall prevalence of IP helminths in the given locality was 12.6%. However, the current finding found much lower than previous studies conducted in different parts of Ethiopia. For instance, it was (20.1%) from Shahura Health Center, Northwest Ethiopia [17], (74.5%) north Gonder [27], (32%) Jawi town, northwest Ethiopia [16] and (71.2%) Debre Elias, East Gojjam zone [8]. Furthermore, higher prevalence of intestinal parasitic helminths has been reported in Axum town (44.6%) [28], in Jimma town (48.2%) [29], in South Eastern Ethiopia (26.2%) [30], in Benishangul-Gumuz Regional State, Western Ethiopia (35.4%) [31], in Adigrat town (27%) [32]. Nevertheless, the current finding closely aligns with the previous report from the University of Gondar Hospital [33], reported a prevalence rate of 17.3%. These variations may be due to differences in the survey season, living and hygiene conditions of the study participants, differences in personal hygienic conditions, level of environmental sanitation, drinking water sources, and geographical factors in the various study areas. Additionally, the variation in IP helminths infection among patients in Mkanselam town compared to the mentioned studies above could be attributed to several factors. These include the variability in the habit of eating raw meat and unwashed vegetables, as well as the presence or absence of a latrine per home. Furthermore, the habit of hand washing after using the toilet and other socioeconomic factors may also contribute to the observed variations.
The first most prevalent parasitic helminth in the current study area was A. lumbricoides (5.6%). Nevertheless, its prevalence rate was much lower than the prevalence rate reported in Jimma town [29], and Adigrat town (19.1%) [32]. This difference might be attributed to the differences in drinking water sources, sanitation conditions, hand washing habit before eating food etc. in the various localities. However, the current finding was much closer to the prevalence rate of A. lumbricoides reported in Lake Langano area (6.2%) [34], Axum town, northern Ethiopia (9%) [28]. On the other hand, the prevalence rate of A. lumbricoides in the present study found higher than the findings reported in south eastern Ethiopia (4.7%) [35], northwest Ethiopia (2.2%) [17], and in Delo-Mena, south eastern Ethiopia (4.7%) [30]. This might be due to the variability in personal hygiene, consumptions of contaminated food and access to clean water among others. The second intestinal helminthic infection identified in this study was T. trichiura, with the prevalence rates of 2.2%. The finding exceeded the reported prevalence rate of T. trichiura (1.1%) in Addis Ababa [36]. However, compared to the present finding higher prevalence rate of T. trichiura reported previously in Shahura health center, northwest Ethiopia (4.7%) [17]. The third encountered intestinal parasite was E. vermicularis with a prevalence rates of 1.7%. This result revealed a higher prevalence rate than the reported 0.69% for E. vermicularis at Axum St. Mary Hospital in Axum town [37]. However, the current finding was lower than the reports in Bereka medical center southeast Ethiopia (5.6%) [38]. These differences in the prevalence rate of IP helminths infections might be due to the level of sanitary conditions, latrine ownership, latrine coverage in the household surroundings, degree of environmental contamination, and level of awareness about parasitic infections and mechanism of parasite transmission among the various local communities and other socio-economic factors.
In this study, hookworm species (1.2%) and H. nana (1.2%) found the fourth prevalent parasitic helminths identified. This finding was lower than the previous reports in Teda health center northeast Ethiopia [39], who reported a prevalence rate of 6.6% for hookworm species and that of 1.5 for H. nana. Similarly the study conducted in Axum town, northern Ethiopia [28] reported higher prevalence rates [(hookworm species (2.7%) and H. nana (6.2%)] than the current findings. On the other hand, the current findings was higher than that of the previous study conducted in Bereka medical center southeast Ethiopia who reported a prevalence rate of hookworm species (0.9%) [26]. Likewise a study conducted at Chelaleki health center around east Wollega zone reported lower prevalent rate 0.3% for H. nana [40]. The other prevalent parasites detected in the current study were S. mansoni (0.2%) and Tania species (0.2%). Compared to this findings higher prevalence rate of these two intestinal parasitic helminths were reported in different parts of Ethiopia, like Jawi town, northwest Ethiopia, where the prevalence rate for S.mansoni was 0.3% and 3% for Tania species [16]. Similarly a study from Shahura health center, northwest Ethiopia reported a prevalence rate of 1.4% for S. mansoni [7]. These variations in prevalence rates of S. mansoni and Tania species might be due to the difference in socio-economical, demographical, geographical, and other differences including climate conditions.
The interpretation of the findings clearly demonstrated that the predisposing factors for IP helminths infections among the study subjects were residence area, marital status, education level, habit of eating unwashed vegetables, presence of dirt matter under nails, lack of latrine at home, and habit of hand washing after toilet visit. In this study IP helminths were significantly associated with residence, and the likelihood of acquiring IP helminths among patients coming from rural areas was two times higher than patients coming from urban areas. This might be due to poor personal and environmental hygiene, the frequent contamination of water bodies, and close contact with animals and soil etc. in the rural areas than urban community. The other observed significant factor associated with IP helminths infection in the study area was hand washing practices after toilet. Those participants who did not wash their hands after defecation were five times more likely to acquire IPIs than those who washed their hands after defecation (Table 7). This was in consistent with previous reports from a study conducted in Teda health center, northwestern Ethiopia [39]. This might be attributed to the habit of washing hands with water without soap and inappropriate handling of readymade foods and drinks.
With regard to the feeding habit, study subjects who ate unwashed vegetable were more likely to acquire IPIs than those who did not eat unwashed vegetables (Table 7). This agrees with the report in Benishangul-Gumuz, western Ethiopia [31]. This might be due to contamination of vegetables with fecal materials in the farm and contamination of the vegetables at home. Presence of finger trimming was another significant factor associated with IPIs in the present study. Participants who have finger trimming were more likely to be infected with intestinal parasites than those who have finger trimming (Table 7). Similar association of IP helminths infection with the presence of finger trimming was reported in a study conducted in northwest Ethiopia [40]. This could be due to the fact that individuals who have finger trimming might get their nails contaminated easily with soil. The soil can contain cysts and eggs of parasitic organisms, which can lead to intestinal helminths infections.
Educational status also found important factor that exposed patients for IP helminths infection in this study area. Illiterate patients were four times more likely to have parasite infection than patients who were diploma and above (Table 7). This finding disagreed with the previous study conducted in Teda health center, northwestern Ethiopia [39], where they reported that the prevalence of IP helminths were not significantly associated with educational status. However, it could be argued with the fact that higher level of education is usually associated with higher level of awareness and better hygienic practices, which might reduce the vulnerability for IP helminths infection. Surprisingly, in the present study, no significant differences in IP helminths infections among those study subjects who have hand washing practices than those didn’t before food (p > 0.05). This might be related with the immunity level of individuals and a matter of probability. This was in agreement with a study conducted in Delgi, northern Gondar [27]. Regarding gender, the proportions of IP helminths infection in males (28.7%) found higher than that of females (26.5%). Similar result was reported in Jimma town Ethiopia [29]. The higher prevalence in males might be due to their everyday work habits in outdoor activities or frequent contact with soils and less hygienic practices than females which makes them more vulnerable for parasitic infections.
Limitation of the study
The study has limitations because of unavailability of previous study on prevalence of intestinal infection in the study area. Besides, it was cross-sectional; thus, it may not truly reflect the dynamic nature of socio-behavioral factors. Moreover, due to resource, financial and time constraints, we did not perform molecular techniques to identify the helminths. Only microscopy technique was used to determine the prevalence intestinal parasitic helminths infection in this study.
Conclusions and future perspectives
The overall prevalence of intestinal parasitic helminths infection among patients attending Mekanselam hospital was significant (12.6%) and deserves to implement intervention measures as public health concern. The most important prevalent intestinal parasitic helminths infection in this study area were A. lumbricoides T. trichiuria and E.vermicularis. In this study, presence of finger trimming, hand washing habit after toilet, the habit of eating unwashed vegetables, marital status, personal hygiene and educational level were important predictors variables significantly associated with the occurrence of intestinal helminthic infections among patients in the study area. The finding in this study showed that intestinal helminths infections are important public health problems in Mekaneselam town. The high prevalence rate of intestinal infection in men may be related to the habit of soil contact, the lack of hand washing practice before meal during field work in the farm etc. Important hygienic practices such as washing of hands after toilet, personal hygiene, using latrine and protecting water supply from contamination could reduce the intestinal parasite infection burden in the study area.
To reduce the risk of helminths infection around Mekaneselam town, stakeholders such as, public health officers, education institutions and the town administrators etc. have to create awareness and implement health education programs on the transmission and effective prevention methods including environmental and personal hygiene, sanitation, avoiding eating unwashed vegetable. There should be a provision of safe water for drinking and cooking, and other household activities. Besides, integrated control programs including provision of personal and environmental hygiene facilities are vital. Furthermore, to determine the burden of intestinal parasitic helminths infection further detailed studies must be conducted by considering extensive samples and wider area coverage.
Acknowledgements
Authors would like to thank K.S. Goudar for the preparation of the study area map, and all laboratory technicians at Mekaneselam hospital for their contribution in laboratory activities. All volunteered study participants deserve acknowledgment.
Abbreviations
- IP
Intestinal parasite
- IPIs
Intestinal parasite infections
- AOR
Adjusted odd ratio
- COR
Crude odd ratio
- CI
Confidence interval
- N (%)
Number and percentage
Authors’ contributions
Moges Kibret Wondimagegn and Lulit Tegegne Hailu conceived the research idea, formulated the design and interpret the findings, and eventually wrote the paper. Lulit Tegegne Hailu, wrote the proposal, conducted the field and lab work, collected data, analyzed the data, and wrote the draft results. Moges Kibret Wondimagegn and Lulit Tegegne Hailu reviewed and approved the manuscript.
Funding
The research fund was obtained through a local scholarship fund by Wollo University, Dessie, Ethiopia. Writing of this paper was the responsibility of the authors, and the funder was not involved.
Data availability
Data are available from the corresponding author upon request.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. The participants of the study were verbally informed about the purpose of the study, type of information to be sought during the interview, risks and benefits, confidentiality, the right to withdraw from the study, and additional study-related information. Written informed consent was obtained from all participants (adults and legal guardians/parents in the case of minors) before the interview. Participation was based on their willingness to participate, and participants could stop at any time without any obligation during the discussion or interview if they felt uncomfortable. The study was conducted after the receipt of ethics approval letter Ref No. WU3161/E-01/22 dated on July 21/2022 from the Institutional Review Board at Wollo University in Dessie, Ethiopia.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hotez PJ, Fenwick A, Savioli L, Molyneux DH. Rescuing the bottom billion through control of neglected tropical diseases. Lancet. 2009; 373(9674):1570–1575. https:// 10.1016/S0140-6736(09)60233-6. [DOI] [PubMed] [Google Scholar]
- 2.Patel MM, Patel PR, Gamit B, Modi J, Padsala S. Prevalence of intestinal parasites infection in Surat city of south Gujarat, a hospital based study. Nat J Comm Med. 2014; 5(03): 273–275. www.njcmindia.org pISSN 0976 3325│eISSN 2229 6816.
- 3.WHO, Soil-transmitted helminth infections: eliminating as public health problem soil transmitted helminthiases in children: progress report 2001–2010 and strategic plan 2011–2020. WHO Press. Geneva: Switzerland; 2016.
- 4.World Health Organization, Soil transmitted helminthes infection. 2023; available at: https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections.
- 5.WHO. World health statistics 2021: monitoring health for the SDGs, sustainable development goals. Geneva: WHO; 2021. Licence: CC BY-NC-SA 3.0 IGO. https://www.who.int/publications/i/item/9789240027053.
- 6.Haile A, Abera T, Dana D. The prevalence of intestinal parasitic infection and associated factors among primary school children in Gurage zone, south Ethiopia. J of Pharma & Alter Med. 2017; 15: SSN 2222–4807 (online).
- 7.Tigabu T, Taye S, Aynalem M, Adane K. Prevalence and associated factors of intestinal parasitic infections among patients attending Shahura health center, northwest Ethiopia. BMC Res Notes. 2019; 12(333): 10.1186/s13104-019-4377-y. [DOI] [PMC free article] [PubMed]
- 8.Workneh T, Esmael A, Ayichiluhm M. Prevalence of intestinal parasitic infections and associated factors among Debre Elias primary school children, east Gojjam zone, Amhara region, north west Ethiopia. J. Bacteriol. and Parasitol. 2014; 5(181): 10.4172/21559597.1000181.
- 9.Federal Democratic Republic of Ethiopia Ministry of Health. second edition of national neglected tropical diseases master plan. Addis Ababa, Ethiopia: Federal Democratic Republic of Ethiopia Ministry of Health; 2016. [Google Scholar]
- 10.TSEDU-Ethiopia, National ODF Campaign,. Campaign framework document (2019/20–2023/24). Addis Ababa, Ethiopia: Federal Democratic Republic of Ethiopia; 2024. p. 2019. [Google Scholar]
- 11.Alemu G, Mekonnen F, Nega M, Muluneh C. Trend of soil-transmitted helminths in Ethiopian children: A systematic review and meta-analysis (2000–2018). J of Parasitol Res. 2021. 10.1155/2021/5638836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liyih M, Damtie D, Tegen D. Prevalence and associated risk factors of human intestinal helminths parasitic infections in Ethiopia: A systematic review and meta-analysis. The Sci Worl J. 2022. 10.1155/2022/3905963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aemiro A, Menkir S, Tegen D, Tola G. Prevalence of soil-transmitted helminthes and associated risk factors among people of Ethiopia: A systematic review and meta-analysis. Infect Dis: Res and Treat.15:1–20, 10.1177/117863372110554 [DOI] [PMC free article] [PubMed]
- 14.Tegen, D, and Damtie, D. Prevalence and risk factors associated with intestinal parasitic infection among primary school children in Dera district, northwest Ethiopia. Canadian J of Infect Dis and Med Microbiol, Hindawi, 2021; 10.1155/2021/5517564. [DOI] [PMC free article] [PubMed]
- 15.Gehad E, Mustafa M. Risk factors associated with intestinal parasite infections among children. J of Egyptian Soci of Parasitol. 2013;43(1):287–94. 10.12816/0006385. [DOI] [PubMed] [Google Scholar]
- 16.Sitotaw B, Mekuriaw H, Damtie D. Prevalence of intestinal parasitic infections and associated risk factors among Jawi primary school children, Jawi town, northwest Ethiopia. BMC Infect Dis. 2019; 19 (341): 10.1186/s12879-019-3971-x. [DOI] [PMC free article] [PubMed]
- 17.Tigabu T, Taye T, Aynalem M, Adane K. Prevalence and associated factors of intestinal parasitic infections among patients attending Shahura Health Center, Northwest Ethiopia,” BMC Res Notes. 2019; 12 (3): 10.1186/s13104-019-4377-y. [DOI] [PMC free article] [PubMed]
- 18.WHO. Ending the neglect to attain the sustainable development goals. A road map for neglected tropical diseases 2021–2030. Geneva: WHO; 2020.
- 19.Gizaw Z, Addisu A, Dagne H. Effects of water, sanitation and hygiene (WASH) education on childhood intestinal parasitic infections in rural Dembiya, northwest Ethiopia: an uncontrolled before- and-after intervention study. Environ Hlth and Prev Med. 2019;24:16. 10.1186/s12199-019-0774-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hailegebriel T, Nibret E, Munshea A. Prevalence of soil-transmitted helminth infection among school-aged children of Ethiopia: A systematic review and meta-analysis. Infect Dis: Res and Treat. 2020;13:1–14. 10.1177/1178633720962812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abera A, Nibret E. Prevalence of gastrointestinal helminthic infection and associated risk factors among schoolchildren in Tilili town, northwest Ethiopia. Asian Pac J Trop Med. 2014;7(7):525–30. 10.1016/S1995-7645(14)60088-2. [DOI] [PubMed] [Google Scholar]
- 22.Mekaneselam town land administration office (MTLA) annual report. MTLA; 2022. Unpublished report.
- 23.CSA. Central Statistics Authority, Population and housing census of Ethiopia. Addis Ababa: CSA; 2007.
- 24.Borena Woreda Agricultural Bureau (BWAB) annual report. BWAB; 2022. Unpublished report.
- 25.Naing L, Winn T, Rusil BN. Practical issues in calculating sample size for prevalence studies. Archi of Orofacial Sci. 2006;1:9–14. [Google Scholar]
- 26.WHO. Bench Aids for the Diagnosis of Intestinal Parasites. Geneva: WHO; 1994.
- 27.Ayalew A, Debebe T, Worku A. Prevalence and risk factors of intestinal parasites among Delgi school children, North Gondar, Ethiopia. J Parasitol Vector Biology. 2011;3(5):75–81.
- 28.Gebreslassie M, Dejenie T, Tomass Z. Prevalence of intestinal parasite and associated risk factors in school children of Aksum town, northern Ethiopia. Acta Parasitologica Globalis. 2015;6(1):42–8. 10.5829/idosi.apg.2015.6.1.9268. [Google Scholar]
- 29.Jejaw A, Zeynudin A, Zemene E, Belay T. Status of intestinal parasitic infections among residents of Jimma Town, Ethiopia. BMC Research Notes. 2014; 7(502): 10.1186/1756-0500-7-502. [DOI] [PMC free article] [PubMed]
- 30.Tulu B, Taye S, Amsalu E. Prevalence and its associated risk factors of intestinal parasitsic infections among Yadot primary school children of south eastern Ethiopia: a cross-sectional study. BMC Research Notes.2014; 7(848): http://www.biomedcentral.com/1756-0500/7/848 [DOI] [PMC free article] [PubMed]
- 31.Gebretsadik G. Prevalence of intestinal parasites and associated risk factors among school children of homesha district (Woreda) in Benishangul-Gumuz regional state, western Ethiopia. J of Family Med and Hlth Care. 2016; 2 (4): 57–64. 10.11648/j.j.fmhc.20160204.16.
- 32.Senbeta D. Prevalence of intestinal parasitic infections and associated risk factors among school children in Adigrat town, northern Ethiopia.International,” J of Emerging Trends in Sci and Technol. 2017; 4(1): 4943–4948. 10.18535/ijetst/v4i1.03.
- 33.Aleka Y, G/egziabher S, Tamir W, Birhane M, Alemu A. Prevalence and associated risk factors of intestinal parasitic infection among under five children in university of Gondar hospital, Gondar, northwest Ethiopia. Biomed Res and Therapy. 2015; 2(8): 347–353, 2015. 10.7603/s40730-015-0020-2.
- 34.Legesse M, Erko B. Prevalence of intestinal parasites among schoolchildren in a rural area close to the southeast of lake Langano. Ethiopia Ethiop J Hlth Dev. 2004;18(2):116–20. 10.4172/2329-891X.1000132. [Google Scholar]
- 35.Tulu B, Taye S, Amsalu E. Prevalence and its associated risk factors of intestinal parasitsic infections among Yadot primary school children of south eastern Ethiopia: a cross-sectional study. BMC Res Notes. 2014; 7 (848): 10.1186/1756-0500-7-848. [DOI] [PMC free article] [PubMed]
- 36.Akililu A, Kahase D, Dessalegn M, Tarekegn N, Gebremichael S, Zenebe S, Desta K, Mulugeta G, Mamuye Y, Mama M. Prevalence of intestinal parasites, Salmonella and shigella among apparently health food handlers of Addis Ababa university student’s cafeteria, Addis Ababa, Ethiopia. BMC. 2015; 8 (17): doi.10.1186/s13104-014-0967-x. [DOI] [PMC free article] [PubMed]
- 37.Feleke DG, Tarko S, Hadush H, Gebretsadik D, Zenebe Y, Seid A. Prevalence of intestinal parasitic infections in St. Marry hospital, Axum, northern Ethiopia: A retrospective study. J Trop Dis. 2017; 5(235): 10.4172/2329-891X.1000235.
- 38.Taye S, Abdulkerim A. Prevalence of intestinal parasitic infections among patients with diarrhea at Bereka medical center, southeast Ethiopia: A retrospective study. Fam Med Med Sci Res. 2014; 3(3): 10.4172/2327-4972.1000131 [DOI] [PMC free article] [PubMed]
- 39.Abate A, Kibret B, Bekalu E, Abera S, Teklu T, Yalew A, Endris M, Worku L, Tekeste Z. Cross-Sectional Study on the Prevalence of Intestinal Parasites and Associated Risk Factors in Teda Health Centre, Northwest Ethiopia. ISRN Parasitol. 2013:757451. 10.5402/2013/757451. [DOI] [PMC free article] [PubMed]
- 40.Alemu M, Anley A, Tedla K. Magnitude of Intestinal Parasitosis and Associated Factors in Rural School Children, Northwest Ethiopia. Ethiop J Health Sci. 2019;29(1):923–8. 10.4314/ejhs.v29i1.14. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author upon request.