Abstract
Background
Pericapsular nerve group (PENG) block has emerged as a reliable analgesia technique for hip arthroplasty (HA). However, the effects of PENG block on perioperative neurocognitive disorder (PND) after HA has not yet been assessed. The present study aimed to investigate the effects of PENG block on early postoperative cognitive function in older people undergoing hip arthroplasty.
Methods
Sixty older patients undergoing HA under spinal anesthesia were randomly assigned to group P (n = 30) receiving PENG block with ropivacaine and patient-controlled intravenous analgesia (PCIA) pump with sufentanil after surgery or group C (n = 30) only receiving PCIA pump with sufentanil after surgery. The primary outcome was the Mini-Mental State Examination (MMSE) score at 7 days postoperatively. Secondary outcomes consisted of the incidence of PND 7 days postoperatively, the static VAS pain scores at 6, 12, 24, and 48 h postoperatively; cumulative sufentanil consumption and the requirement of rescue analgesia during the 0–24 h period after surgery; quality of recovery-15 (QoR-15) scale scores at 24 h postoperatively; and the plasma levels of high mobility group box protein 1 (HMGB1) preoperatively and 1 day after surgery, and adverse events.
Results
After surgery, the PENG block group had higher MMSE score than the control group at 7 days postoperatively (27.0 ± 1.8 vs. 26.1 ± 1.7, P = 0.048), with a mean difference of 0.9 (95%CI, 0.1–0.9). The incidence of PND at 7 days postoperatively was 6.7% in group P, lower than that of 30% in group C (P = 0.044). In group P, the static VAS scores at 6, 12, and 24 h postoperatively were significantly lower than those in group C (all P < 0.05). Compared with group C, the cumulative sufentanil consumption and the number of patients required rescue analgesia during the 0–24 h period after surgery were significantly lower in group P (all P < 0.05). The scores of QoR-15 scale were higher in group P at 24 h postoperatively than those in group C (P < 0.05). Patients in group P showed lower plasma levels of HMGB1 than group C at 1 day after surgery (P < 0.05), and the rate of complications didn’t differ between both groups.
Conclusions
Older people undergoing HA receiving a PENG block for perioperative analgesia experience improved early postoperative cognitive function, reduced postoperative pain, higher quality of recovery, and less postoperative inflammatory response.
Trial registration
Chictr.org.cn identifier ChiCTR2200061055 (Date of registry: 15/06/2022, prospectively registered).
Keywords: Pericapsular nerve group block, Postoperative cognitive function, Hip arthroplasty, Older people
Background
The annual number of hip fractures worldwide is expected to rise to more than 6 million by 2050 [1]. Hip arthroplasty (HA) is among the most commonly performed surgical procedures for hip fractures at present and can provide reliable outcomes. However, surgical stimulation, severe perioperative pain and inflammatory reaction can lead to various postoperative complications, which is not conducive to the recovery of patients [2]. Perioperative neurocognitive disorder (PND) are common complications following HA, which is mainly manifested as attention deficit, intellectual and memory impairment, and decreased social activity ability [3]. Factors including older age, the presence of comorbid diseases, perioperative pain, and inflammatory response, have been reported to affect PND incidence [4]. The incidence of PND in older patients after HA can be as high as 75%, resulting in delayed mobilization and prolonged hospital stay [5]. Therefore, it is urgent to explore a more reasonable approach to reduce the occurrence of PND.
It has been reported that effective postoperative analgesia by fascia iliaca compartment block can lower the incidence of PND, and lower serum cytokines in patients undergoing HA [6]. Peripheral inflammatory response induced by surgical and the release of systemic inflammatory mediators have been shown to affect inflammatory processes in the central nervous system [7]. Increased release of inflammatory cytokines after surgery, such as high mobility group box protein 1 (HMGB1), is associated with the risk of PND [8].
Pericapsular nerve group (PENG) block, first described by Girón-Arangoin in 2018, can selectively block the articular branches of the femoral, obturator and accessory obturator nerves, thereby providing analgesia for HA [9]. Some studies have shown that PENG block can provide good analgesic effect and result in better preservation of motor function for patients undergoing HA [10, 11]. Adequate postoperative analgesia is essential to reduce surgical stress, and PND, which is conducive to postoperative recovery [12]. However, there is rarely evidence investigating the influence of PENG block on cognitive function among older people undergoing HA. In this study, we aimed to explore the effect of PENG block on early postoperative cognitive function and analgesia effect in older people after HA.
Methods
This randomized controlled clinical trial was carried out in a single-center and was approved by the Medical Ethics Committee of the Affiliated LiHuiLi Hospital of Ningbo University (identifier: KY2022PJ126). The current trial was registered at www.chictr.org.cn (ChiCTR2200061055) before the participant’s enrollment. Written informed consent was signed by all subjects or legal representatives. The subjects were recruited over a period of 12 months (7/4/2022 to 7/28/2023). Inclusion criteria: age between 65 and 85 years; American Society of Anesthesiologists (ASA) II or III; body mass index (BMI) between 18 and 28 kg/m2, received primary school education or above; Mini-Mental State Examination (MMSE) score ≥ 24 before surgery; scheduled for HA. Exclusion criteria: serious cardiopulmonary or other vital organ disease; history of neurological and psychiatric disorders; coagulopathy; long-term use of drugs; severe impairment of visual, hearing or speech functions; and allergic to local anesthetics.
All subjects were randomly divided into two groups according to a computer-generated random number table and an opaque envelope technique: the PENG block group (group P, n = 30) and the control group (group C, n = 30). Postoperative outcome evaluators and statistical analysts were both blinded.
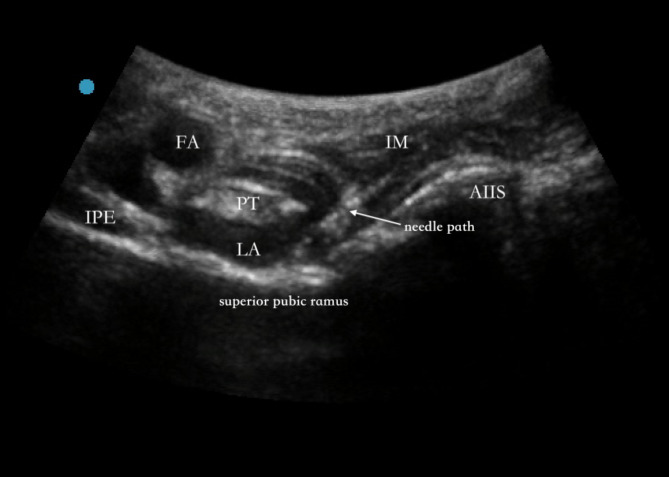
All patients with standard monitoring including 5-lead electrocardiogram, pulse oxygen saturation, and invasive arterial blood pressure were performed in the operating room. An intravenous cannula pathway was established. All patients were ultrasonically scanned in a supine position 20 min prior to spinal anesthesia. A curvilinear transducer (2–5 HZ, Edge, Sonosite, Seattle, USA) was positioned in a transverse plane, medial and caudal to the anterior superior iliac spine and adjusted until the anterior inferior iliac spine, iliopubic eminence, iliopsoas muscle and tendon were identified. Then patients in group P received a PENG block. Using an in-plane technique, a 21 gauge×100 mm SonoPlex Stim needle (Pajunk, Geisingen, Germany) was advanced in a lateral-to-medial direction until its tip was between the psoas tendon and periosteum dorsal (Fig. 1). Following negative aspiration, 20 mL of 0.375% ropivacaine (Naropin, AstraZeneca AB Company, Södertälje, Sweden) was slowly injected and the diffusion of local anesthetic (LA) was observed. Patients in group C didn’t receive sham PENG block. All PENG blocks were performed by an experienced anesthesiologist.
Fig. 1.
Ultrasound image of PENG block. AIIS, anterior inferior iliac spine; FA, femoral artery; IM, iliac muscle; IPE, iliopubic eminence; LA, local anesthetic, PT, psoas muscle tendon, arrow shows the needle path
After 20 min, all patients received spinal anesthesia in a lateral position. L2–L3 or L3–L4 intervertebral space was selected for puncture. A spinal needle was inserted into the subarachnoid space and 10–15 mg ropivacaine was slowly administered. All surgical procedures were performed by the same team of surgeons with the same procedure. All subjects received intravenous parecoxib sodium (40 mg) at the end of the surgery and underwent patient-controlled intravenous analgesia pump (PCIA) immediately. The PCIA comprised 2 µg/kg sufentanil, 0.15 mg/kg tropisetron and 100 mL normal saline. The background doses were 2 mL/h and 0.5 mL of intravenous bolus on demand with a 15 min lockout. Imrecoxib was administered orally once a day (100 mg). Another 100 mg tramadol was administered intravenously for rescue analgesia if patients couldn’t tolerate pain [the visual analog scale (VAS) scores ≥ 4].
An independent evaluator, who was not aware of the grouping, conducted visits and followed up the patients both before surgery and after HA up to 7 d.
Primary outcome
Our primary outcome was the MMSE score at 7 days postoperatively. The patients in both groups received the neurocognitive function test in a quiet room by an experienced anesthesiologist 1 day preoperatively and 7 days postoperatively. MMSE [13] is one of the most widely used screening tools of cognitive function in clinical practice that has high sensitivity and specificity. It’s a 30-point scale based on orientation, attention and calculation, registration, language, recall, and praxis (a total of 30 questions, 1 point for each correct answer, 0 points for the wrong answer or do not know). The scale ranges from 0 to 30 points.
Secondary outcomes
The incidence of PND was examined 7 days postoperatively. As mentioned in previous studies, PND was defined as a decline ≥ 1 standard deviation (SD) in the postoperative MMSE score compared with the preoperative MMSE score [14].
The secondary outcomes also included the static VAS (VAS scores ranged from 0 to 10, 0 is painless and 10 is excruciating pain) pain scores at 6, 12, 24, and 48 h postoperatively; cumulative sufentanil consumption and the requirement of rescue analgesia during the 0–24 h period after surgery; quality of recovery-15 (QoR-15) scale scores at 24 h postoperatively (QoR-15 scale includes five dimensions: physical comfort, emotional state, physical independence, psychological support and pain, with a total score of 0-150 points. The higher the score was, the better the recovery quality would be [15].); the plasma levels of high mobility group box protein 1 (HMGB1) preoperatively and 1 day after surgery; and adverse events (i.e., vascular puncture, LA systemic toxicity [LAST], postoperative nausea/vomiting [PONV], deep vein thrombosis, respiratory depression).
5 mL of venous blood samples were collected from all subjects 1 h before and 1 d after surgery and centrifuged at 1000 × g for 15 min at 4 °C. The plasma was collected and stored at − 80 °C for subsequent detection. The enzyme-linked immunosorbent assay (ELISA) method was used to detect the concentrations of HMGB1.
Statistical analyses
The sample size of this study was calculated using IBM SPSS Sample Power version 3.0 (IBM Corp., Armonk, New York, USA) based on the results of the pilot study, which showed a mean MMSE score (7 days postoperatively) of 27.4 with SD of 2.14 in group P and 25.3 with SD of 2.91 in group C. A calculated sample size of 25 participants per group was required to achieve a statistical power of 0.8 with a significance level alpha of 0.05. A total of 30 subjects in each group were recruited to account for possible 20% drop-out rate.
Statistical analysis was performed using SPSS V.24.0 (IBM Corp., Armonk, New York, USA). The Kolmogorov-Smirnov test was used to evaluate normality. Normally distributed continuous data were expressed as mean with SD and categorical data as frequency with percentages. Normally distributed continuous data were analyzed with the Student’s t-test. A repeated-measures analysis of variance was used to compare the two groups at different time points. For categorical data, the chi-square (χ2) test or Fisher’s exact test was used. Ranked data were compared by Mann-Whitney U test. A 95% confidence interval (CI) for differences in means (for continuous data) or relative risk (RR) (for categorical data) were calculated. A P-value of < 0.05 was considered statistically significant.
Results
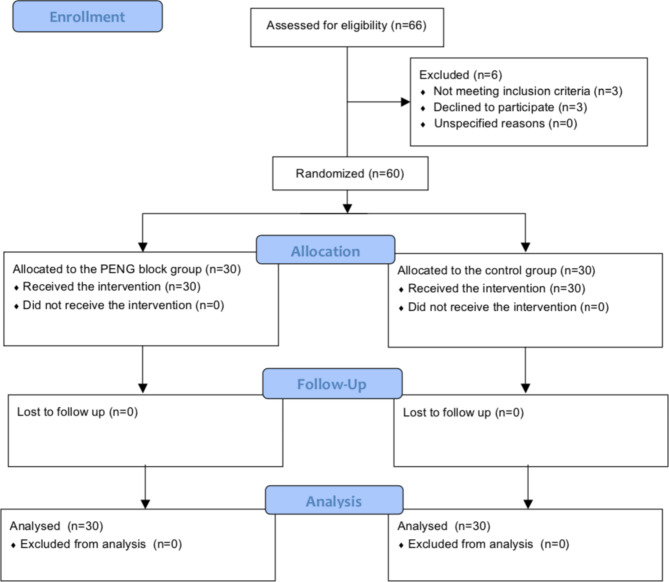
During the study period, a total of 66 patients were screened for eligibility. Three patients didn’t meet the inclusion criteria: 1 patient had a BMI of more than 28, 1 patient was illiterate, and 1 had cognitive impairments. Three patients didn’t wish to participate. Sixty patients were randomized equally to group P or group C. All patients completed the study and were included in the final analysis (Fig. 2). Clinical baseline characteristics such as age, gender, and BMI, were similar between both groups (Table 1). At the same time, surgical time and surgical fixation methods between the two groups were comparable (Table 1).
Fig. 2.
CONSORT diagram. PENG = pericapsular nerve group block
Table 1.
Clinical baseline characteristics of the patients
| group P (n = 30) | group C (n = 30) | P-value | ||
|---|---|---|---|---|
| Age (years) | 73.9 ± 5.7 | 75.2 ± 6.6 | 0.418 | |
|
Gender [n (%)] male female |
13 (43.3) 17 (56.7) |
16 (53.3) 14 (46.7) |
0.438 | |
| BMI (kg/m2) | 23.0 ± 2.8 | 22.3 ± 3.4 | 0.388 | |
| Education (years) | 7.6 ± 2.3 | 7.2 ± 2.0 | 0.475 | |
|
ASA score [n (%)] II III |
18 (60) 12 (40) |
14 (46.7) 16 (53.3) |
0.301 | |
|
Surgery side [n (%)] left right preoperative pain score (VAS) |
11 (36.7) 19 (63.3) 5.1 ± 1.7 |
15 (50) 15 (50) 5.2 ± 1.4 |
0.297 0.805 |
|
| surgical time (min) | 73.4 ± 20.6 | 79.8 ± 15.6 | 0.787 | |
| Surgical fixation method | 0.582 | |||
| cemented [n (%)] | 6 (20) | 8 (26.7) | ||
| cementless [n (%)] | 16 (53.3) | 15 (50) | ||
| hybride [n (%)] | 8 (26.7) | 7 (23.3) |
The data are represented as the mean ± SD or number (%)
BMI = body mass index; ASA = American Society of Anesthesiologists; VAS = visual analog scale
Continuous data were compared by Student’s t-test; categorical data were compared by chi-square (χ2) test; ranked data were compared by Mann-Whitney U test
Primary outcome
There were no differences in MMSE scores at 1 day preoperatively between both groups. Compared with group C, the MMSE scores were significantly higher in group P at 7 days postoperatively (P < 0.05). The MMSE scores were significantly lower in group C at 7 days postoperatively than that at 1 day preoperatively (P < 0.05; Table 2).
Table 2.
The Mini-mental State Examination (MMSE) scores of the patients
| time point | group P (n = 30) | group C (n = 30) | Difference in means (95% CI) | P-value | |
|---|---|---|---|---|---|
| MMSE | 1 day preoperatively | 27.7 ± 2. 1 | 27.5 ± 2.2 | 0.2 (-0.9 to 1.3) | 0.719 |
| 7 days postoperatively | 27.0 ± 1.8# | 26.1 ± 1.7* | 0.9 (0.1 to 1.9) | 0.034 |
The data are represented as the mean ± SD
MMSE = Mini-Mental State Examination
Compared with group C, #P < 0.05; compared with 1 day preoperatively, *P < 0.05
Data were compared by repeated-measures analysis of variance
Secondary outcomes
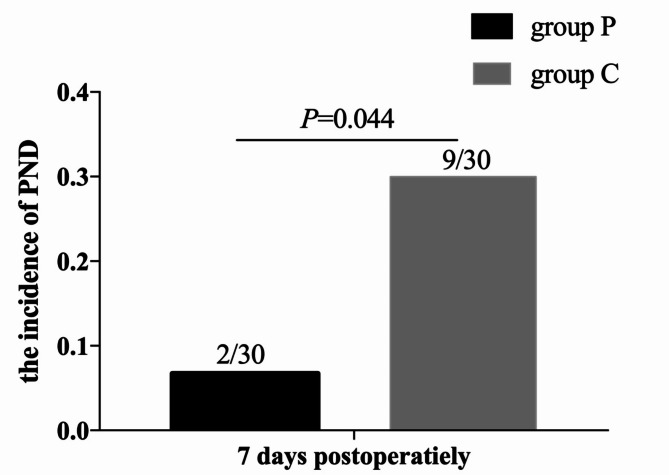
There were 2 patients in group P and 9 patients in group C who developed PND at 7 days postoperatively. The incidence of PND in group P at 7 days postoperatively was significantly lower than that in group C [6.7% vs. 30%, RR (95% CI): 0.2 (0.1, 0.9), P = 0.044; Fig. 3].
Fig. 3.
The incidence of perioperative neurocognitive disorder (PND) at 7 days postoperatively between the two groups. Data were compared by Fisher’s exact test
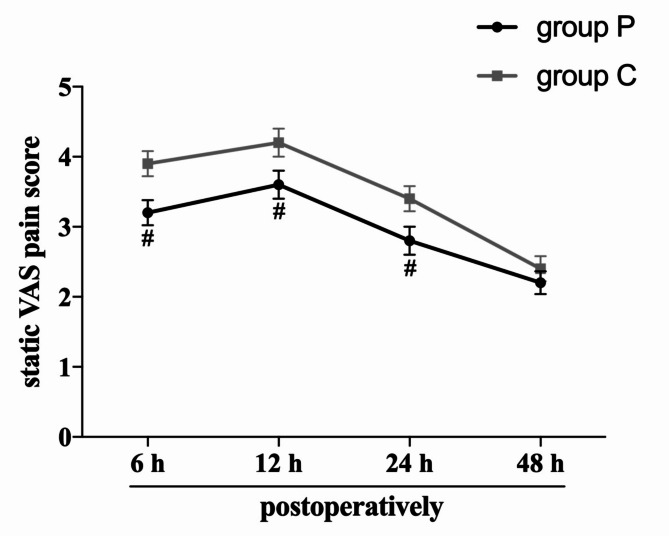
In group P, the static VAS scores at 6, 12, and 24 h postoperatively were significantly lower than those in group C (P < 0.05), but no intergroup difference was observed at 48 h postoperatively (P > 0.05, Fig. 4). Compared with group C, the cumulative sufentanil requirements and the number of patients required rescue analgesia during the 0–24 h period after surgery were significantly lower in group P (P < 0.05). The QoR-15 scores at 24 h postoperatively were higher among group P than compared with those in group C (P < 0.05, Table 3).
Fig. 4.
The postoperative static VAS pain scores between the two groups. The error bars indicate the standard error of the mean. VAS = visual analog scale. Compared with group C, #P < 0.05. Data were compared by repeated-measures analysis of variance
Table 3.
Sufentanil consumption, rescue analgesia requirements and QoR-15 score of the patients
| group P (n = 30) | group C (n = 30) | Difference in means (95% CI) | P-value | ||
|---|---|---|---|---|---|
| Static VAS scores | |||||
| 6 h postoperatively | 3.2 ± 1.0# | 3.9 ± 1.0 | -0.7 (-1.2 to -0.2) | 0.011 | |
| 12 h postoperatively | 3.6 ± 1.1 # | 4.2 ± 1.1 | -0.6 (-1.2 to -0.1) | 0.030 | |
| 24 h postoperatively | 2.8 ± 1.1# | 3.4 ± 1.0 | -0.6 (-1.2 to -0.0) | 0.034 | |
| 48 h postoperatively | 2.2 ± 0.9 | 2.4 ± 1.0 | -0.2 (-0.7 to 0.3) | 0.367 | |
| Sufentanil consumption (µg) | |||||
| 0–24 h after surgery | 53.3 ± 7.0# | 58.2 ± 9.8 | -4.9 (-9.2 to -0.5) | 0.029 | |
| Patients requiring rescue analgesia [n (%)] | RR (95% CI) | ||||
| 0–24 h after surgery | 6 (20) # | 14 (46.7) | 0.4 (0.2, 1.0) | 0.028 | |
|
QoR-15 score 24 h postoperatively |
119.7 ± 13.9# | 107.1 ± 20.1 |
Difference in means (95% CI) 12.6 (3.6 to 21.5) |
0.007 | |
The data are represented as the mean ± SD or number (%)
QoR = quality of recovery
Compared with group C, #P < 0.05
Continuous data were compared by Student’s t-test; categorical data were compared by chi-square (χ2) test
No intergroup differences were found in terms of preoperative HMGB1 levels (P > 0.05). HMGB1 levels in both groups increased dramatically at 1 day after surgery as compared to those preoperatively (P < 0.05). Compared with group C, group P resulted in lower HMGB1 levels at 1 day after surgery (P < 0.05; Table 4).
Table 4.
The plasma levels (pg/mL) of HMGB1 of the patients
| time point | group P (n = 30) | group C (n = 30) | Difference in means (95% CI) | P-value | |
|---|---|---|---|---|---|
| HMGB1 | preoperatively | 614.6 ± 164.5 | 629.7 ± 146.0 | -15.1 (-95.5 to 65.3) | 0.709 |
| 1 day after surgery | 756.5 ± 184.0#* | 845.4 ± 132.7* | -88.9 (-171.8 to -6.0) | 0.036 |
The data are represented as the mean ± SD
Compared with the control group, #P < 0.05; compared with baseline, *P < 0.05
Data were compared by repeated-measures analysis of variance
No serious adverse events, such as vascular puncture, LAST, deep vein thrombosis and respiratory depression, occurred in either group. No intergroup differences were observed in terms of the incidence of PONV (P > 0.05, Table 5).
Table 5.
Postoperative complications of the patients
| group P (n = 30) | group C (n = 30) | RR (95% CI) | P-value | |
|---|---|---|---|---|
| Vascular puncture [n (%)] | 0 | 0 | ||
| LAST [n (%)] | 0 | 0 | ||
| PONV [n (%)] | 11(36.7) | 13 (43.3) | 0.8 (0.5, 1.6) | 0.598 |
| Deep vein thrombosis [n (%)] | 0 | 0 | ||
| Respiratory depression [n (%)] | 0 | 0 |
The data are represented as number (%)
PONV = postoperative nausea and vomiting; LAST = local anesthetic systemic toxicity
Categorical data were compared by chi-square (χ2) test
Discussion
In this randomized trial, we studied the effects of on early postoperative cognitive function in older people undergoing HA. The present study showed that PENG block could effectively improve postoperative MMSE scores, reduce the incidence of PND, reduce pain intensity, as well as the plasma levels of HMGB1 in older people after HA.
The MMSE is a widely used and well-accepted screening tool of cognitive function. Due to its advantages of little training and easy to administer, it is the most popular cognitive test both in clinical practice and in research, and is regarded as an important tool for perioperative cognitive screening [13]. In our study, the MMSE scores in group P were higher at 7 days postoperatively compared with group C; the declined MMSE scores in group P were reduced than those in group C between 1 day preoperatively and 7 days postoperatively. The results suggested that preoperative implementation of PENG block could reduce the impairment of postoperative cognitive function in older people undergoing HA. Shang et al. [16]. found that paravertebral nerve block before radical gastrectomy can improve patients’ postoperative cognitive function, which is similar to our findings. However, the difference in MMSE scores at 7 days postoperatively between the two groups (0.9) did not reach the minimal clinically important difference (MCID) for MMSE, which was reported to be 1.5 [17].
It was reported that PND following elective HA has a median incidence of 19.3% at 7 days postoperatively, ranging from 6.7 to 75% [5]. The incidence of PND increases with age. Zha et al. [18] found that the incidence of PND after hip surgery was 30% in the general anesthesia group and 5% in the iliac fascia block group, which was roughly similar to the results in this study. In the current study, the incidence of PND at 7 days postoperatively in group C and group P was 30% and 6.7%, respectively, indicating that preoperative PENG block could result in lower rate of early PND. The rate of PND in group P of the current study (6.7%) is slightly higher than the reported incidence in patients receiving iliac fascia block (5%) [18]. The difference could be attributable to different study population, anesthesia method, and peripheral nerve block type.
Hip fractures and surgery can lead to moderate-to-severe perioperative pain [19]. Inadequate perioperative analgesia, advanced age, and opioid use are risk factors for PND after HA [20]. Severe postoperative pain has been shown to compromises the mental health of older patients and increase complications, which are detrimental to their postoperative mobilization and recovery [21]. Ultrasound-guided PENG block can be used in hip surgery to purely block the sensory nerve and without motor impairment [9]. The results of this randomized trial showed better early postoperative analgesia with the PENG block for HA resulting in lower pain scores and fewer patients requiring rescue analgesia. This study also showed opioid-sparing of the PENG block for HA as indicated by the lower consumption of sufentanil 24 h after surgery in group P when compared with group C. Our results were similar to the study by Lin et al. [22]. , who reported that patients receiving PENG block during hip surgery experienced less pain, PENG block could provide improved short-term analgesia in hip surgery. Adequate postoperative analgesia and reduced opioid use may be one of the reasons for improved postoperative cognitive function in patients receiving the PENG block.
The QoR-15 scale is a valid, easy-to use tool, and an important index to measure postoperative quality of recovery. The scores obtained from the QoR-15 in patients with PENG block were lower than those reported by Kukreja et al. [23]. However, the study was conducted in younger patients. When the score difference is greater than 8, the intervention is clinically significant [24]. Our results showed that QoR-15 scores at 24 h postoperatively were higher in group P than those in the group C. The difference between the two groups was more than 8, indicating that PENG block can enhance the quality of recovery after HA.
It has been recognized that PND is caused by surgical trauma and postoperative pain, which leads to an inflammatory response, a large number of inflammatory factors cross the blood-brain barrier (BBB) and trigger neuroinflammation. As an initiator of neuroinflammation, the nuclear HMGB1 is responsible for the progression of cognitive impairments by disrupting the BBB [25]. A previous study showed that the serum level of HMGB1 was increased significantly after surgery, associated with the development of postoperative short-term cognitive dysfunction [26]. In the present study, the outcome showed that the levels of HMGB1 increased in both groups after surgery, but rising trend in group P was lower than that in group C, indicating that postoperative inflammatory response was lower in patients receiving PENG block and subsequently reduced cognitive dysfunction.
There are still some limitations in this study. Firstly, the follow-up period of the study was short, only 7 days after surgery, extended follow-up is needed in future studies to assess long-term effects of patients after surgery. Secondly, the study was conducted in a small number of subjects, the findings of this study need to be further validated by high-quality studies with large sample sizes. Thirdly, only MMSE scale was used to assess cognitive function in this study. Because of its certain limitations, such as ceiling effect, performance influenced by education and age, multiple tests should be adopted in future researches. Finally, we didn’t perform a sham block in the control group due to ethical approval issues, which may potentially exacerbate bias in the follow-up results.
Conclusions
PENG block can effectively improve early postoperative cognitive function and recovery in older people undergoing HA, which may be related to more effective analgesia and lower plasma HMGB1 levels.
Acknowledgements
The study was supported by the Department of Anesthesiology, Department of Orthopaedics, The Affiliated LiHuiLi Hospital of Ningbo University, Ningbo, China, and Department of Anesthesiology, Ningbo Beilun People’s Hospital. The authors would like to appreciate the efforts of all medical staff and the patients for their participation in this study.
Abbreviations
- ASA
America Society of Anesthesiologist
- BBB
Blood-brain barrier
- BMI
Body mass index
- CI
Confidence interval
- ELISA
Enzyme-linked immunosorbent assay
- HA
Hip arthroplasty
- HMGB1
High mobility group box protein 1
- LA
Local anesthetic
- LAST
Local anesthetic systemic toxicity
- MMSE
Mini-Mental State Examination
- PCIA
Patient-controlled intravenous analgesia
- PENG
Pericapsular nerve group
- PND
Perioperative neurocognitive disorder
- PONV
Postoperative nausea and vomiting
- QoR-15
Quality of recovery-15
- RR
Relative risk, SD: standard deviation
- VAS
Visual analogue scale
Author contributions
Conception and design: MHZ; Data collection: QLY, RFZ; Data analysis: YLM, LZW; Drafting the manuscript: MHZ, QLY; Revision of the manuscript after critical review: MHZ. All authors read and approved the final manuscript.
Funding
This study was supported by Medical Health Science and Technology Project of Zhejiang Provincial Health Commission (2020KY866). The funding had no role in study design, data collection, analysis, and preparation of the manuscript.
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of the Affiliated LiHuiLi Hospital of Ningbo University, China (KY2022PJ126), and the protocol was registered at the Chinese Clinical Trial Registry (ChiCTR2200061055) (prospectively registered). The initial registration date was 15/06/2022. All procedures performed in this study involving human participants were in accordance with the Ethical Standards of the Institutional Ethics Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All patients signed written informed consent before surgery.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dhanwal DK, Dennison EM, Harvey NC, et al. Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop. 2011;45(1):15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yucuma D, Riquelme I, Avellanal M. Painful total hip arthroplasty: a systematic review and proposal for an algorithmic management approach. Pain Physician. 2021;24(3):193–201. [PubMed] [Google Scholar]
- 3.Ehsani R, Djalali MS, Zaman B, et al. Effect of general versus spinal anesthesia on postoperative delirium and early cognitive dysfunction in elderly patients. Anesth Pain Med. 2020;10(4):e101815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xiao QX, Liu Q, Deng R, et al. Postoperative cognitive dysfunction in elderly patients undergoing hip arthroplasty. Psychogeriatrics. 2020;20(4):501–9. [DOI] [PubMed] [Google Scholar]
- 5.Kitsis P, Zisimou T, Gkiatas I, et al. Postoperative delirium and postoperative cognitive dysfunction in patients with elective hip or knee arthroplasty: a narrative review of the literature. Life(Basel). 2022;12(2):314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feng TC, Zhao J, Wang JY, et al. Anesthetic effect of the fascia iliaca compartment block with different approaches on total hip arthroplasty and its effect on postoperative cognitive dysfunction and inflammation. Front Surg. 2022;9:898243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vacas S, Degos V, Feng X, et al. The neuroinflammatory response of postoperative cognitive decline. Br Med Bull. 2013;106(1):161–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu MH, Qi Y, He HJ, et al. Effect of quadratus lumborum block on postoperative cognitive function in elderly patients undergoing laparoscopic radical gastrectomy: a randomized controlled trial. BMC Geriatr. 2021;21(1):238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Girón-Arango L, Peng PWH, Chin KJ, et al. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43(8):859–63. [DOI] [PubMed] [Google Scholar]
- 10.Julián A, Sebastián L, Bravo D, et al. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total hip arthroplasty. Reg Anesth Pain Med. 2021;46(10):874–8. [DOI] [PubMed] [Google Scholar]
- 11.Bravo D, Aliste J, Layera S, et al. Randomized clinical trial comparing pericapsular nerve group (PENG) block and periarticular local anesthetic infiltration for total hip arthroplasty. Reg Anesth Pain Med. 2023;48(10):520–1. [DOI] [PubMed] [Google Scholar]
- 12.Baeriswyl M, Kirkham R, Kern C, et al. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015;121(6):1640–54. [DOI] [PubMed] [Google Scholar]
- 13.Velayudhan L, Ryu SH, Raczek M, et al. Review of brief cognitive tests for patients with suspected dementia. Int Psychogeriatr. 2014;26:1247–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lakshminarayanan S, Aboobacker M, Brar A, et al. Advancing Perioperative Neurocognitive Health: a critical review of Predictive Tools, Diagnostic methods, and interventional strategies. Cureus. 2024;16(5):e59436. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Stark PA, Myles PS, Burke JA. Development and psychometric evaluation of a postoperative quality of recovery score: the QoR-15. Anesthesiology. 2013;118(6):1332–40. [DOI] [PubMed] [Google Scholar]
- 16.Shang YH, Qi FW, Zheng Z, et al. Effect of bilateral paravertebral nerve block on cognitive function in elderly patients undergoing radical gastrectomy for gastric cancer: a prospective randomized double-blind controlled trial. BMC Anesthesiol. 2022;22(1):224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borland E, Edgar C, Stomrud E, et al. Clinically relevant Changes for Cognitive outcomes in Preclinical and Prodromal Cognitive stages. Neurology. 2022;99(11):e1142–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zha J, Ni JP, Chen S et al. Ultrasound Radiomics-Guided Iliac Fascia Block on Postoperative Cognitive Dysfunction in Elderly Patients Undergoing Hip Surgery. Comput Math Methods Med. 2022; 2022:2492667. [DOI] [PMC free article] [PubMed]
- 19.Kukreja P, MacBeth L, Sturdivant A, et al. Anterior quadratus lumborum block analgesia for total hip arthroplasty: a randomized, controlled study. Reg Anesth Pain Med. 2019;25:ramp–2019. [DOI] [PubMed] [Google Scholar]
- 20.Jia B, Tang YY, Wei CP, et al. Peripheral nerve Block and Peri-operative Neurocognitive disorders in older patients with hip fractures: a systematic review with Meta-analysis. Geriatr Orthop Surg Rehabil. 2023;14:21514593231186722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morrison RS, Magaziner J, Gilbert M, et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol Biol Sci Med Sci. 2003;58:M76–81. [DOI] [PubMed] [Google Scholar]
- 22.Lin DY, Morrison C, Brown B, et al. Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: a single-center double-blinded randomized comparative trial. Reg Anesth Pain Med. 2021;46:398–403. [DOI] [PubMed] [Google Scholar]
- 23.Kukreja P, Uppal V, Kofskey AM, et al. Quality of recovery after pericapsular nerve group (PENG) block for primary total hip arthroplasty under spinal anaesthesia: a randomised controlled observer-blinded trial. Br J Anaesth. 2023;130(6):773–9. [DOI] [PubMed] [Google Scholar]
- 24.Demumieux F, Ludes PO, Diemunsch P, et al. Validation of the translated quality of Recovery-15 questionnaire in a french-speaking population. Br J Anaesth. 2020;124(6):761–7. [DOI] [PubMed] [Google Scholar]
- 25.Paudel YN, Shaikh MF, Chakraborti A, et al. HMGB1: a common biomarker and potential target for TBI, Neuroinflammation, Epilepsy, and cognitive dysfunction. Front Neurosci. 2018;12:628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu H, Dong R, Lu YY et al. Short-Term Postoperative Cognitive Dysfunction and Inflammatory Response in Patients Undergoing Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy: A Pilot Study. Mediators Inflamm. 2017; 2017:3605350. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the current study are available from the corresponding author on reasonable request.