Abstract
Bereavement carries consequences for the health and socioeconomic well-being of surviving family members. Using data from the National Longitudinal Study of Adolescent to Adult Health, the current study investigates whether formerly incarcerated individuals experience the death of a family member at higher rates than the general population. We find that relative to those without a history of incarceration, formerly incarcerated individuals are more likely to experience the death of an immediate family member by young adulthood. Subsequent analyses demonstrate that deaths occurring during or after a respondent was incarcerated were relevant for health and well-being.
Introduction
The death of a family member, including a parent, sibling, or child, carries deleterious consequences for the health and economic well-being of surviving family members. Indeed, the loss of a family member is considered among the most stressful life experiences, and the resulting stress can endure for years (Sanders, 1980; Stroebe, Hansson, Schut, & Stroebe, 2008; Stroebe, Schut, & Stroebe, 2007; Umberson et al., 2017). Previous research finds that bereavement is associated with a host of physical ailments, including disability and illness (Stroebe et al., 2007) and weight loss (Shahar, Schultz, Shahar, & Wing, 2001), as well as adverse psychological symptoms, such as depression and anxiety (Clayton, 1990; Clayton & Darvish, 1979; Kreicbergs, Valdimarsdóttir, Onelöv, Henter, & Steineck, 2004), insomnia (Hardison, Neimeyer, & Lichstein, 2005), and suicidal ideation (Segal & Roy, 2001; Stroebe & Schut, 2005). Moreover, bereavement is found to increase the risk of mortality among surviving family members (Bowling, 1994; Li, Laursen, Precht, Olsen, & Mortensen, 2003; Stroebe et al., 2007). The loss of a family member can also generate financial strain among surviving kin due to increased healthcare expenditures and reductions in labor force participation (Corden & Hirst, 2013; Fox, Cacciatore, & Lacasse, 2014; Stephen et al., 2015).
While a sizeable literature has documented the consequences related to bereavement, less research has documented disparities in familial mortality across subsets of the population. Notably, recent research by Umberson et al. (2017) revealed that as a result of differences in life expectancy and associated rates of premature mortality, black Americans lose family members at higher rates than white Americans over the life-course. Consequently, the adverse effects of bereavement serve as a unique and disproportionate source of adversity in the lives of black Americans. While these novel findings suggest that certain groups may be at an elevated risk for experiencing the death of a family member, prior research has not examined disparities in family mortality among other segments of the population beyond racial minorities. Drawing upon this prior research, the current study proposes that familial mortality may be a previously unexplored source of disadvantage among formerly incarcerated individuals.
There are currently 2.2. million individuals incarcerated in prison or jail on any given day in the United States (Kaeble & Cowhig, 2018). The size and scope of the U.S. penal population is so vast that mass incarceration may contribute to population health inequalities (Wildeman & Wang, 2017). Those who come into contact with the criminal justice system typically come from disadvantaged backgrounds (Massoglia et al., 2013), and these markers of disadvantage are often exacerbated by a period of incarceration as a result of social stigma and various legal restrictions placed on former inmates (Wildeman & Muller, 2012). A growing body of literature indicates that serving time behind bars worsens both physical and mental health conditions, while also elevating the likelihood of post release mortality relative to the general population (Binswanger et al., 2007; Massoglia & Pridemore, 2015; Massoglia et al., 2014; Patterson, 2013; Rosen, Schoenbach, & Wohl, 2008; Rosen, Wohl, & Schoenbach, 2011; Testa, Porter, & Nakamura, 2018). Incarceration also carries vicarious health consequences for kin, including diminished physical and psychological well-being for family members and offspring (Jackson & Vaughn, 2017; Lee, Wildeman, Wang, Matusko, & Jackson, 2014; Turney, 2014; Wildeman, Schnittker, & Turney, 2012), as well as an elevated risk of premature mortality for children of an incarcerated parent in both the short- and long-term (Wildeman, 2012; Wildeman et al., 2014; van de Weijer et al., 2018).
Although research has established a link between incarceration and premature mortality, previous work has not investigated whether persons with a history of incarceration experience the death of family members at higher rates than the non-incarcerated population. Given the elevated risk for premature mortality among formerly incarcerated persons themselves, as well as the adverse consequences of incarceration for the health of their family members, the current study proposes that persons with a history of incarceration may experience the death of family members at disproportionate rates. If so, disparities in familial mortality may be a previously unexplored form of disadvantage among this population. To be sure, considering death of family members among the carceral population is important as several factors that are consequences of incarceration are also consequences of bereavement, including depression (Porter & Noisky, 2017; Turney, Wildeman, & Schnittker, 2012), diminished physical health (Massoglia & Pridemore, 2015), socioeconomic hardship (Harding, Wyse, Dobson, & Morenoff, 2014), and weakened social support networks (Hochstetler, DeLisi, & Pratt, 2010; Naser & La Vigne, 2006). Likewise, experiencing familial death can diminish the capacity of family members to provide social support and may serve as an added stressor that makes both coping while in prison and community reintegration following release from prison more challenging. Finally, because of racial disparities in life expectancy in the United States (Shiels et al., 2017), the loss of family members (Umberson et al., 2017), and the composition of the penal population (Travis, Western, & Redburn, 2014), this study also explores whether the pattern of family mortality experienced among formerly incarcerated persons varies across black, white, and Hispanic persons.
Current study
The goal of the current study is to understand whether formerly incarcerated individuals experience the death of a family member at a higher rate than those who have not been previously incarcerated, and whether this relationship varies by race/ethnicity. We begin by assessing the direct association between prior incarceration and family mortality. Next, interaction terms are used to assess whether the influence of incarceration on familial mortality is moderated by race/ethnicity. After investigating the link between incarceration history and familial mortality, we then turn to an investigation of the timing of experiencing death, and the consequences of experiencing the death of a family member among formerly incarcerated individuals. In this second stage of the analysis, we classify when the most proximate death occurred based on respondent reports of the year each family member died, and the age at which they were first incarcerated. Using this information, deaths are classified into categories of experiencing no death, experiencing a death prior to incarceration, or experiencing a death during or after incarceration. After establishing the timing of a death, we investigate the consequences of experiencing mortality among formerly incarcerated persons. Specifically, we explore whether experiencing the death of a family member among formerly incarcerated persons (either prior to or during/after incarceration) is related to psychological health outcomes (depression symptoms, anxiety symptoms, and insomnia symptoms), self-reported physical health, and personal income.
Data
Data for this study are from the National Longitudinal Study of Adolescent to Adult Health (Add Health), an ongoing nationally representative longitudinal study of adolescents enrolled in grades 7–12 in the United States during the 1994–1995 academic year. The cohort has been followed from adolescents through the transition to young adulthood with four in-home interviews—Wave I (1994–1995), Wave II (1996), Wave III (2001–2002), and Wave IV (2008). Each interview lasted between 1 and 2 h and covered a variety of topics related to respondents’ social, economic, psychological, and physical well-being, as well as characteristics regarding their families. The current study draws on data from waves I and IV. At wave IV respondents were between ages 24 and 34. The analytic sample for the current study includes 12,813 respondents. The second stage of the analysis, which focuses on the consequence of experiencing the death of a family member, uses an analytic sample of 1739–1866 formerly incarcerated individuals.1
Dependent variables
Family mortality
The outcome variable measures whether or not a respondent experienced family mortality. At wave IV, respondents are asked to report if they have experienced the death of a biological parent, sibling, or child. Family mortality is coded as a binary variable, differentiating those who lost a family member from those who have not.2
Respondent health and well-being
Next, for analyses that assess the consequences of familial mortality among formerly incarcerated persons, we include a series of variables that capture psychological well-being, self-reported physical health, and socioeconomic status measured at wave IV. Depression symptoms are measured using items from the Centers for Epidemiological Studies-Depression Scale. Respondents were asked a series of questions at wave IV, regarding how often in the prior seven days they experienced 10 symptoms, including: being bothered by things, could not shake off the blues, felt as good as others (reverse coded), had trouble concentrating, felt depressed, felt too tired, felt happy (reverse coded), enjoyed life (reverse coded), felt sad, and felt disliked. Responses were coded on a scale including, never/rarely, sometimes, a lot of time, most/all of the time. Responses were summed to create a single scale ranging from 0 to 30 (alpha = .839) (Porter & Novisky, 2017). Anxiety symptoms are measured using a scale constructed from four items indicating in the past 30 days how often an individual respondent felt: unable to control the important things in life, confidence in the ability to handle personal problems (reverse coded), things were going your way (reverse coded), and difficulties were piling up so high they could not be overcome. Responses to each item were coded on a scale including, never, almost never, sometimes, fairly often, and very often. Responses to the four questions were combined into a scale ranging from 0 to 16 (alpha = .722) (Porter, 2014). Insomnia symptoms are measured using a scale that combines responses to two questions: “how often do you have trouble falling asleep” and “how often do you have trouble staying asleep.” Each response was coded on a scale ranging from 0 to 4 (never, less than once a week, 1–2 times a week, 3–4 times a week, 5 or more times a week). Responses to these items were combined into a scale ranging from 0 to 8 (alpha = .679) (Testa & Porter, 2017). Self-reported physical health is measured using responses to a question asking respondents how their general physical health is, where higher responses equate to poorer subjective health (excellent, very good, good, fair, or poor). Personal income is measured using a question that asks respondents in the past year “how much income did you receive from personal earnings before taxes, that is, wages or salaries, including tips, bonuses, and overtime pay, and income from self-employment.” Responses are reported in U.S. dollar value, and were transformed using the natural logarithm to reduce positive skew.
Independent variable
Prior incarceration
The focal predictor variable measures whether or not a respondent reported being previously incarcerated. At wave IV, respondents were asked if they have ever spent time in a jail, prison, or other correctional facility. Prior incarceration is coded as a binary variable, where 1 indicates a respondent has been previously incarcerated, and 0 represents respondents without a history of incarceration.
Timing of death
In order to perform a subset of analyses among previously incarcerated individuals, a follow-up question determined the age at which they were first incarcerated. Using information on the age of first incarceration and year a given family member died, a variable was constructed capturing whether the most proximate death of a family member occurred before incarceration or after the age of first incarceration.3
Control variables
Demographic control variables include the respondent’s age at Wave IV, race/ethnicity (white, black, Hispanic, other race), and sex (1 = male; 0 = female). Controls for background characteristics are measured at wave I and include a scale of concentrated disadvantage of the census tract of residence (proportion of residents who are on welfare, living at or below the poverty line, unemployed, and the proportion of female headed households), whether a respondent was born in the United States (1 = yes; 0 = no), whether a respondent had a low birth weight of <5 pounds, 8 ounces (1 = yes, 0 = no), whether a respondent reported feeling safe in the neighborhood they lived in during adolescents (1 = yes; 0 = no), the highest level of education either parent obtained (less than high school, high school graduate, post high school, or education information missing), and a five-point scale of the degree to which respondent reported they feel their parents care about them (not at all, very little, somewhat, quite a bit, very much). To account for differences in family size, models include controls for the total number of siblings and the total number of children—both living or deceased—reported by a respondent at wave IV.
Method
The association between prior incarceration and family mortality is estimated using a series of logistic regression models. Model 1 regresses prior incarceration on family mortality, adjusting for family size (number of siblings and children). Model 2 incorporates control variables for demographic and background characteristics. Next, interaction terms were included to assess whether the association between prior incarceration and family mortality is moderated by race/ethnicity. In models assessing the consequences of familial mortality among formerly incarcerated persons, negative binomial regression is used to assess depression symptoms, anxiety symptoms, and insomnia symptoms since each are overdispersed and positively skewed with a high rate of zero values. Ordinary least squares regression is used to assess the association between timing of a death and self-reported health and logged personal income. All models are estimated using Stata 15.1 and survey weights are applied using the SVY command to account for the complex survey design of the Add Health study.
Results
Table 1 provides the summary statistics for the analytic sample. Overall, 21.4% of the sample experienced the death of a parent, sibling, or child by young adulthood and 14.6% of the sample had experienced incarceration by wave IV. The majority of the sample is white (69.7%), about 14% of the sample is black, and 11.6% is Hispanic. By wave IV, the sample was on average 28 years old.
Table 1.
Summary statistics from wave I (1993–1994) and wave IV (2008) of the National Longitudinal Study of Adolescent to Adult Health (N = 12,813).
| Variables | Mean/Percentage | SE | Range |
|---|---|---|---|
| Dependent Variable | |||
| Family Death | 21.4% | 0–1 | |
| Independent Variable | |||
| Incarceration | 14.6% | 0–1 | |
| Control Variables | |||
| White | 69.7% | 0–1 | |
| Black | 14% | 0–1 | |
| Hispanic | 11.6% | 0–1 | |
| Other Race | 4.6% | 0–1 | |
| Male | 50.1% | 0–1 | |
| Age | 28.4 | .12 | 24–34 |
| Number of Siblings | 2.6 | .03 | 1–5 |
| Number of Children | .92 | .03 | 0–8 |
| Concentrated Disadvantage (W1) | −.03 | .03 | −10.29–2.66 |
| US Born | 74.7% | 0–1 | |
| Low Birthweight | 1.1% | 0–1 | |
| Feel Safe in Neighborhood (W1) | 90.2% | 0–1 | |
| Parent Education: Less than HS | 10.9% | 0–1 | |
| Parent Education: High School | 30.2% | 0–1 | |
| Parent Education: Post High School | 53.3% | 0–1 | |
| Parent Education: Missing | 5.7% | 0–1 | |
| Parent Cared | 4.80 | .01 | 1–5 |
Figure 1 illustrates that when the sampled is stratified by prior incarceration status, 27.8% of formerly incarcerated individuals experienced the death of a family member compared to 20.4% of those without a history of incarceration. Figure 2 presents the percentage of respondents who experienced family mortality across race/ethnicity. Black respondents experienced the death of an immediate family member at the highest rate (34.7%) compared to 23.1% of Hispanics and 18.5% of white respondents.
Figure 1.
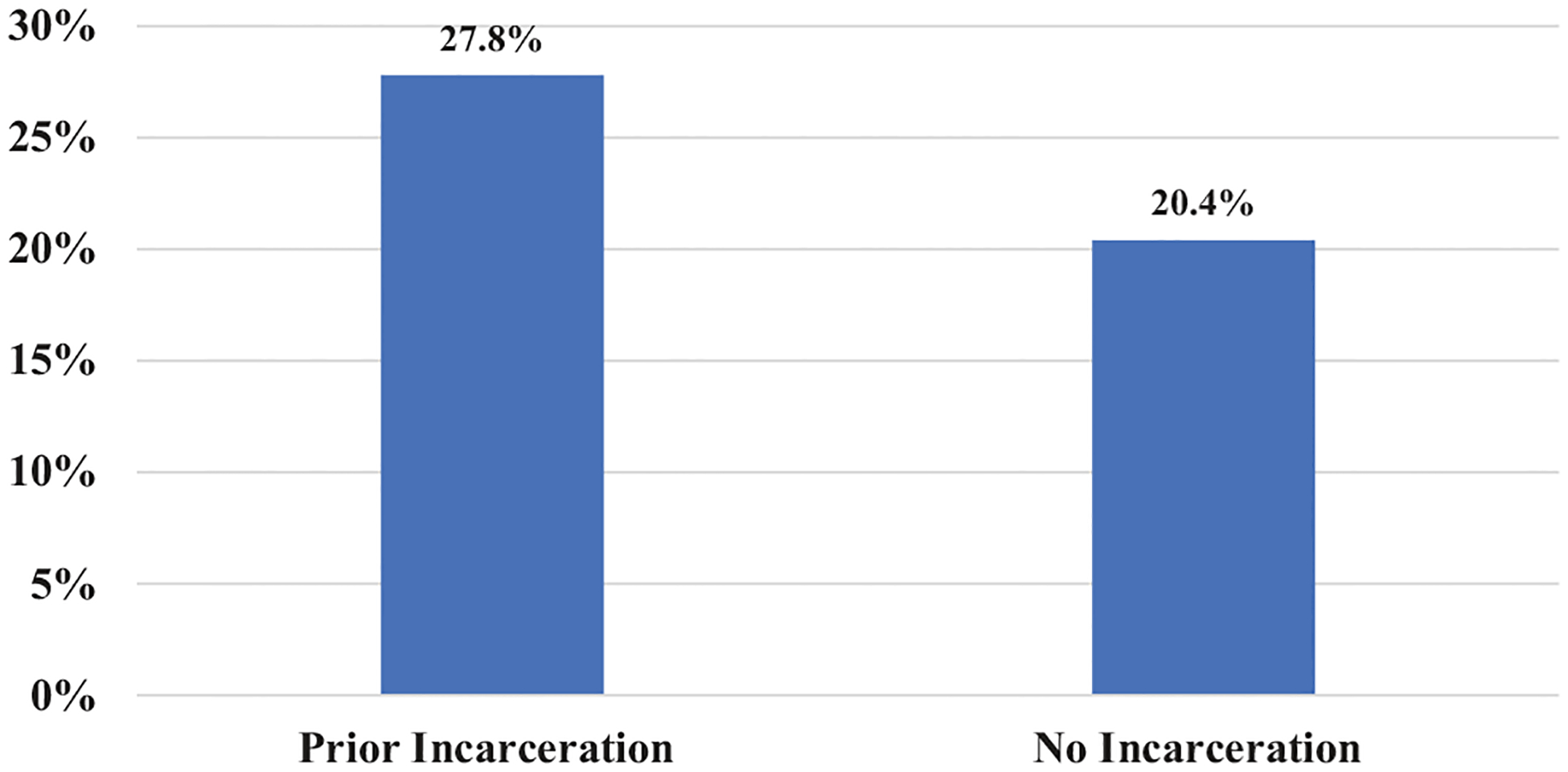
Death of a family member by incarceration status.
Figure 2.
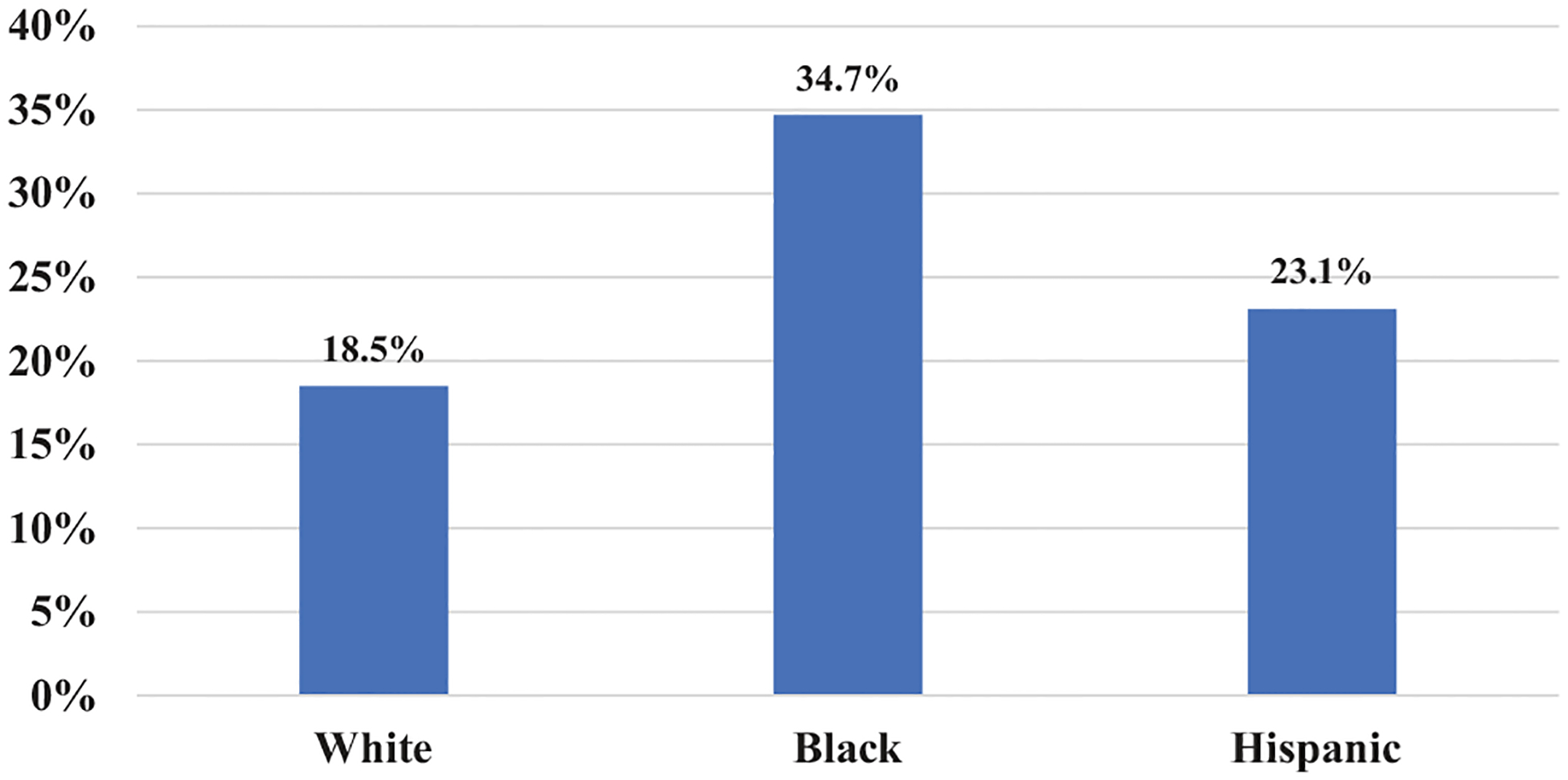
Death of a family member by race.
Table 2 presents the results of family mortality regressed on incarceration status and other covariates. The results in Model 1, which adjusts for family size, demonstrates that respondents with a history of incarceration are 30% more likely to experience family mortality than respondents without any incarceration history (OR = 1.30; 95% CI = 1.12, 1.52). After including control variables for demographic and background characteristics, the results in Model 2 remain similar as a history of incarceration is associated with higher odds of experiencing the death of an immediate family member (OR = 1.28; 95% CI = 1.08, 1.52).
Table 2.
Logistic regression of family mortality on incarceration and other covariates.
| Variables | OR | 95% CI | OR | 95% CI |
|---|---|---|---|---|
| Incarceration | 1.30*** | (1.12, 1.52) | 1.28** | (1.08, 1.52) |
| Number of Siblings | 1.38*** | (1.32, 1.45) | 1.31*** | (1.25, 1.38) |
| Number of Children | 1.18*** | (1.11, 1.25) | 1.09** | (1.03, 1.15) |
| Hispanic | 0.93 | (0.70, 1.24) | ||
| Black | 1.63*** | (1.30, 2.04) | ||
| Other Race | 1.14 | (0.87, 1.48) | ||
| Male | 0.86* | (0.76, 0.98) | ||
| Age | 1.07** | (1.03, 1.12) | ||
| Concentrated Disadvantage (W1) | 0.98 | (0.93, 1.04) | ||
| U.S. Born | 1.01 | (0.86, 1.17) | ||
| Low Birth Weight | 1.44 | (0.75, 2.77) | ||
| Feels Safe in Neighborhood | 0.87 | (0.68, 1.10) | ||
| Parented Education: HS Grad | 0.78* | (0.62, 0.99) | ||
| Parented Education: Post HS | 0.53*** | (0.43, 0.65) | ||
| Parented Education: Missing | 0.82 | (0.62, 1.09) | ||
| Parent Caring | 0.87** | (0.78, 0.96) | ||
| Constant | 0.09*** | (0.08, 0.11) | 0.05*** | (0.01, 0.20) |
| Observations | 12,813 | 12,813 |
p < .05;
p < .01;
p < .001.
The results of the interaction between incarceration history and race are displayed in Figure 3. A few patterns are notable. First, white respondents with a history of incarceration exhibited a particularly high likelihood of family mortality, relative to white respondents without a history of incarceration. Expressed as predicted probabilities, 25.3% of white respondents who have been previously incarcerated experienced the death of a family member, compared to 19.2% without a history of incarceration. The results also illuminate the vast racial disparities in family mortality. Specifically, 29.3% black respondents who have never been incarcerated had experienced the death of a family member compared to ~25% of white respondents who reported prior incarceration. This finding suggests that family mortality is such a common life event among black young adults, that black respondents without a history of incarceration remain more likely to experience the death of a family member than white respondents with a history of incarceration.
Figure 3.
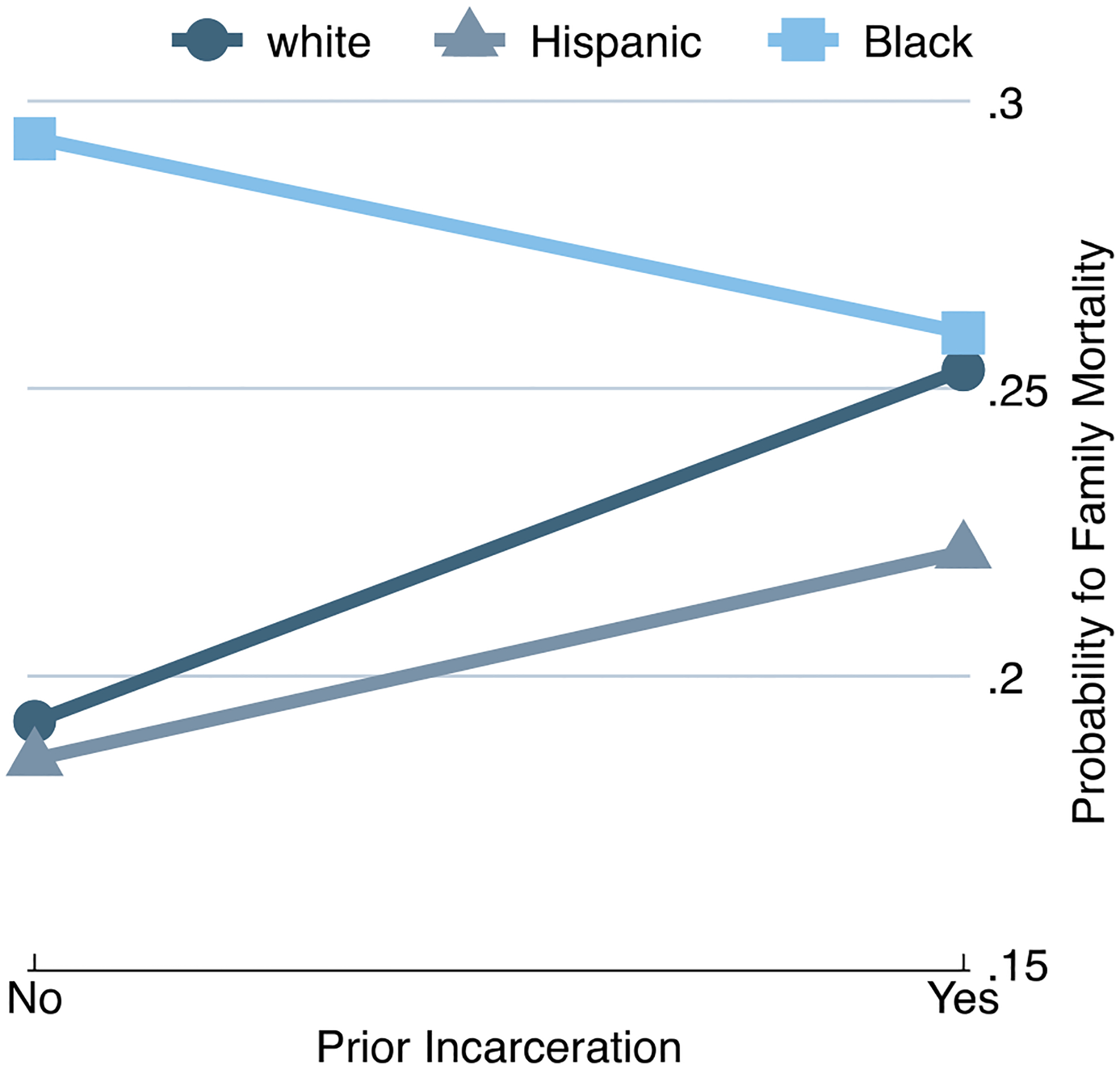
Logistic regression of family mortality on incarceration * race and other covariates.
Next, we turn to an analysis of the timing of death in relation to incarceration. Approximately 72% of former inmates had experienced no family member death, 12.9% experienced a death only before their first incarceration, and 15% experienced a family member death during or after being incarcerated.4 We use these three categories on timing of death to assess whether formerly incarcerated persons who experienced a death of a family member (either before or during/after incarceration) experience diminished psychological and physical well-being and reduced personal income at rates different than formerly incarcerated persons who did not experience death. The summary statistics for these measures across the three groups of formerly incarcerated persons (no death, death before incarceration, death during/after incarceration) are reported in Table 3. The general pattern suggests that relative to those who experienced no family member death, former inmates who experienced a death tend have worse psychological and physical health, and lower personal income, and that these outcomes are poorest for those who experienced a death during or after their first incarceration.5 To further explore this association, we regress our health and well-being measures on the timing of family member death (in reference to no family member death) among formerly incarcerated individuals. Results in Table 4 indicate that compared to formerly incarcerated persons who have not experienced a death, respondents who experienced the death of a family member during or after incarceration are significantly more likely to experience symptoms of depression (IRR = 1.20, CI = 1.07, 1.35), anxiety (IRR = 1.10, CI = .99, 1.21), and insomnia (IRR = 1.20, CI = .98, 1.46). They are also more likely to have poorer general health (b = .18, CI = .01, .35), and lower personal income (b = −.21, CI = −.38, −.05).6
Table 3.
Summary statistics of psychological well-being, physical health, and personal income among formerly incarcerated persons.
| Variables | No death | Death before incarceration | Death during or after incarceration | |||
|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | |
| Depression Symptoms | 6.67 | .16 | 7.53 | .46 | 8.35 | .58 |
| Anxiety Symptoms | 5.32 | .10 | 5.87 | .29 | 6.09 | .31 |
| Insomnia Symptoms | 2.63 | .08 | 3.06 | .23 | 3.16 | .27 |
| Physical Health | 2.50 | .03 | 2.61 | .07 | 2.72 | .08 |
| Personal Income (Ln) | 9.37 | .10 | 9.13 | .27 | 8.22 | .36 |
Table 4.
Regression of timing of family mortality on psychological well-being, physical health, and personal income among formerly incarcerated persons.
| Depression symptoms (n = 1862) | Anxiety symptoms (n = 1863) | Insomnia symptoms (n = 1832) | Physical health (n = 1866) | Personal income (Ln) (n = 1739) | |
|---|---|---|---|---|---|
| Variables | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | b (95% CI) | b (95% CI) |
| No Death (Reference) | – | – | – | – | – |
| Death Before Incarceration | 1.04 (.92, 1.19) | 1.03 (.94, 1.14) | 1.13 (.96, 1.32) | .06 (−.09, .22) | .04 (−.40, .48) |
| Death During or After incarceration | 1.20 (1.06, 1.36)** | 1.10 (.99, 1.21)† | 1.18 (.99, 1.39)† | .18 (.01, .35)* | −.98 (−1.63, −.32)**a |
p<.10;
p < .05;
p < .01
= death after incarceration significantly differs from death before incarceration category at p < .05.
All models include controls for race number of siblings, number of children, race/ethnicity, sex, age, concentrated disadvantage (w1), U.S. born, low birth weight, feels safe in neighborhood, parental education, and parent caring.
Discussion
This study provides the first assessment of whether (1) formerly incarcerated individuals experience the loss of family members at higher rates than their non-incarcerated counterparts and (2) the timing of family member death relative to incarceration impacts the health and well-being of formerly incarcerated persons who have experienced family member death. Our findings indicate that by young adulthood, Americans who have a history of incarceration are more likely to experience the death of a parent, sibling, or child than those who have not been previously incarcerated. Because bereavement carries several consequences for individuals’ socioeconomic status, mental and physical health, and risk of mortality (Stroebe et al., 2007, 2008; Umberson et al., 2017), investigating exposure to the death of family members among formerly incarcerated individuals is important, as these consequences may affect community reintegration and the mental and physical well-being of former inmates. On this point, our supplemental analyses show that relative to formerly incarcerated persons who did not experience family member death, former inmates who had a family member die during or after their first incarceration had poorer psychological and physical health, and lower levels of personal income. Ancillary analyses, moreover, indicated that such results are not simply a function of the recency of family member death, as recency of family member death was not associated with significant decreases in health and well-being among the formerly incarcerated.
While our findings do not definitively establish a causal link between family member death and reductions in respondent health and well-being among the formerly incarcerated, the correlational findings suggest that losing a family member may be an especially potent stressor when experienced through the lens of incarceration, and that, under such circumstances, it may harm the health and well-being of formerly incarcerated persons. Accordingly, it may be a beneficial strategy for correctional institutions to gather information about the loss of family members among incarcerated individuals and provide services, such as grief therapy, for both currently and formerly incarcerated persons.
These findings also carry implications for understanding how the death of a family member can influence coping during incarceration, as well as the effect of bereavement on post-release outcomes. During a period of incarceration, inmates may struggle to cope with a variety of stressors including the loss of liberty, overcrowding, and experiencing and witnessing violent victimization (Goffman, 1963; Toch, Adams, & Grant, 1989). As Haney (2003, p. 79) notes “incarcerated persons often suffer long-term consequences from having been subjected to pain, deprivation, and extremely atypical patterns and norms of living and interacting with others.” In addition to these immediate sources of deprivation, inmates are often socially isolated and have limited contact with friends and family members who can provide emotional support which can be instrumental in reducing stress and anxiety felt during incarceration (Comfort, 2008). Importantly, having lost a family member can diminish social support networks and decrease visitations by reducing the size of a person’s family. Moreover, because both the death of a family member and being incarcerated are each independently stressful experiences, inmates who experience the death of a family member may incur a proliferation of the stress related to coping with incarceration (Pearlin, 1989).
Furthermore, prior research on prisoner reentry suggests that formerly incarcerated individuals often rely on family members for emotional and tangible support following release from incarceration (Harding et al., 2014; Naser & La Vigne, 2006; Western, Braga, Davis, & Sirois, 2015). For instance, in their study of hardships faced by former prisoners, Harding et al. (2014, p. 454) find “family support provides not just an immediate place to live and meals to eat, but transportation, emotional sustenance, and a stable base from which to develop longer-term strategies for securing shelter and employment.” The findings of the current study have implications for understanding hardships encountered during reentry as experiencing family mortality will reduce the size of potentially useful social support networks, thereby potentially exacerbating the challenges associated with community reintegration. Relatedly, alongside diminished social support, the loss of a family member often represents the removal of a positively valued stimulus, which in turn can exacerbate feelings of strain. Consistent with general strain theory (Agnew, 1992), experiencing family member death may result in emotional upheaval and potentially manifest in difficulties coping and an increase in externalizing behaviors such as crime.7 While the current study is unable to explore the influence of family mortality on outcomes such as social support and coping with stressors both during and after incarceration, future research should explore these issues in order to further understand the intersection between incarceration, bereavement, and various post-release outcomes.
Next, because of racial differences in rates of bereavement and the likelihood of experiencing incarceration, we also explored whether the relationship between incarceration and familial mortality was moderated by race/ethnicity. Consistent with earlier research (Umberson et al., 2017), the findings demonstrated that black Americans are at a heightened risk of losing a family member by young adulthood. These findings suggest that black Americans may endure a disproportionate number of deleterious consequences related to bereavement. On this point, more attention should be devoted to reducing disparities in life expectancy in the United States in order to reduce racial disparities in loss of family members. Regarding the interaction between race and incarceration, our findings yielded novel results, as a history of incarceration elevated the risk of experiencing the death of a family member among whites but not blacks. This result is consistent with prior research that finds a history of incarceration is related to a higher mortality risk among white than black former inmates (Rosen et al., 2008; Spaulding et al., 2011; Testa et al., 2018). This finding may reflect a saturation effect wherein the disadvantage among blacks relative to whites conceals the link between incarceration and family mortality among blacks. In other words, because the criminal justice system tends to be more punitive toward minority defendants (Spohn, 2015), whites who are sentenced to a period of incarceration on average come from more disadvantaged backgrounds that leave them at a higher risk for experiencing family mortality. Such a finding is consistent with suggestions that the relationship between incarceration and poor health may be “weaker among African Americans than whites simply because prison is less selective of high risk among the former than the latter” (Schnittker, Massoglia, & Uggen, 2011, p. 137). Because data used in this study do not permit a complete examination of the process that explains this interaction, future research should further investigate the mechanisms underlying this finding.
Limitations and future research
There are several limitations of the present study upon which future research can expand. First, the Add Health data lack information concerning the specific causes of death of family members. It is possible that potential consequences of family member death for surviving family members may be contingent on how the deceased family member died. Second, the respondents in this study were young adults. The results found in the current study may be different among samples examined at a different stage of the life-course, as individuals generally experience more familial mortality as they grow older. Third, the data used in the current study were self-reports of both incarceration and familial mortality. Future studies would benefit from the use of official records, including administrative records of incarceration and death certificates. Finally, the structure of Add Health data used in this study are limited for understanding whether experiencing a death of a family member exacerbate stressors and other consequences related to incarceration. A beneficial area of future research would be to assess this relationship using alternative sources of longitudinal data, which collect information in monthly or yearly intervals. Doing so would provide more detailed insights into the complex interplay of stressors such as incarceration and familial death on an individual’s physical and psychological well-being.
Conclusion
In summary, we examined whether persons with a history of incarceration in the United States were at an elevated risk of losing a family member by young adulthood and whether this association differed by race/ethnicity. The findings suggest that relative to the never-incarcerated population, young adults in the United States who have been previously incarcerated exhibit a higher rate of family member death. Across race/ethnicity, study results indicate that black Americans experience familial mortality at the highest rates, with over one-third of black Americans in the sample experiencing the death of a family member by young adulthood. Moreover, we also found a Race × Incarceration interaction effect on family member mortality, such that a history of incarceration among white Americans appears to be particularly relevant to the risk of having a family member die. Finally, experiencing the death of a family member during or after incarceration was associated with worse health and economic outcomes. Taken together, the findings uncover bereavement as a potential source of disadvantage among formerly incarcerated individuals. Future research should continue to investigate this relationship and determine how the death of family members may exacerbate socioeconomic hardships and health problems among formerly incarcerated persons.
Acknowledgments
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Funding
This research was funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. No direct support was recieved from these grants for this analysis.
Footnotes
Sample size varies across the outcomes as a result of different patterns of non-response to the survey items.
Less than 4% of the sample had lost more than 1 family member by Wave IV. Subsequent analyses were conducted analyzing the total number of family members who died as the dependent variable. The results of these models were substantively similar substantively similar to the results reported using a binary measure of family mortality.
It may be relevant to consider whether a respondent experienced the death of a family member during a period of incarceration. Unfortunately, the structure of the Add Health data does not enable an accurate calculation of the exact length of the period of incarceration and therefore we could not confidently estimate deaths that occurred during the time an individual was incarcerated.
In total, 32 respondents experienced a death of a family member only prior to birth. Due to the small sample size these respondents were combined with those who experienced death prior to incarceration. Subsequent analyses were conducted that includes death prior to birth as a separate category. Results of these models remain substantively similar to those reported in the main analysis and are available upon request.
For those who reported being previously incarcerated, a follow up question is asked inquiring if the individual had been incarcerated once or more than once. In total, 1,042 respondents in the analytic sample reported having been incarcerated once and 851 respondents reported being incarcerated more than once.
It is possible that the differences found are a result of the recency of death, rather than the death happening during/after incarceration. To further investigate this possibility, we created measures of the recency of the most proximate death in years prior to the wave IV interview. Results indicate that relative to those who experienced no death, there were no clear patterns whereby the proximity of experiencing a family member death was related to psychological well-being, physical health, or personal income.
We thank an anonymous reviewer for making this useful suggestion. Because the Add Health data do not contain detailed information about when an individual is released from prison and their subsequent criminal offending, we could not assess whether bereavement influences the likelihood of recidivism.
References
- Agnew R (1992). Foundations for a general strain theory of crime and delinquency. Criminology, 30, 47–88. doi: 10.1111/j.1745-9125.1992.tb01093.x [DOI] [Google Scholar]
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, & Koepsell TD (2007). Release from prison-a high risk of death for former inmates. The New England Journal of Medicine, 356, 157–165. doi: 10.1056/NEJMsa064115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A (1994). Mortality after bereavement: An analysis of mortality rates and associations with mortality 13 years after bereavement. International Journal of Geriatric Psychiatry, 9, 445–459. doi: 10.1002/gps.930090603 [DOI] [Google Scholar]
- Clayton PJ (1990). Bereavement and depression. The Journal of Clinical Psychiatry, 51, 34–40. [PubMed] [Google Scholar]
- Clayton PJ, & Darvish HS (1979). Course of depressive symptoms following the stress of bereavement. In Barrett JE et al. (Eds.), Stress and mental disorder (pp. 121–136). New York: Raven. [Google Scholar]
- Comfort M (2008). Doing time together: Love and family in the shadow of the prison. Chicago, IL: University of Chicago. [Google Scholar]
- Corden A, & Hirst M (2013). Economic components of grief. Death Studies, 37, 725–749. doi: 10.1080/07481187.2012.692456 [DOI] [PubMed] [Google Scholar]
- Fox M, Cacciatore J, & Lacasse JR (2014). Child death in the United States: Productivity and the economic burden of parental grief. Death Studies, 38, 597–602. doi: 10.1080/07481187.2013.820230 [DOI] [PubMed] [Google Scholar]
- Goffman E (1963). Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Haney C (2003). The psychological impact of incarceration: Implications for post-prison adjustment. Washington, DC: Urban Institute. [Google Scholar]
- Harding DJ, Wyse JJ, Dobson C, & Morenoff JD (2014). Making ends meet after prison. Journal of Policy Analysis and Management: [The Journal of the Association for Public Policy Analysis and Management], 33, 440–470. doi: 10.1002/pam.21741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardison HG, Neimeyer RA, & Lichstein KL (2005). Insomnia and complicated grief symptoms in bereaved college students. Behavioral Sleep Medicine, 3, 99–111. doi: 10.1207/s15402010bsm0302_4 [DOI] [PubMed] [Google Scholar]
- Hochstetler A, DeLisi M, & Pratt TC (2010). Social support and feelings of hostility among released inmates. Crime & Delinquency, 56, 588–607. doi: 10.1177/0011128708319926 [DOI] [Google Scholar]
- Jackson DB, & Vaughn MG (2017). Parental incarceration and child sleep and eating behaviors. The Journal of Pediatrics, 185, 211–217. doi: 10.1016/j.jpeds.2017.03.026 [DOI] [PubMed] [Google Scholar]
- Kaeble D, & Cowhig M (2018). Correctional populations in the United States, 2016. Washington, DC: US Department of Justice. [Google Scholar]
- Kreicbergs U, Valdimarsdóttir U, Onelöv E, Henter JI, & Steineck G (2004). Anxiety and depression in parents 4–9 years after the loss of a child owing to a malignancy: A population-based follow-up. Psychological Medicine, 34, 1431–1441. doi: 10.1017/S0033291704002740 [DOI] [PubMed] [Google Scholar]
- Lee H, Wildeman C, Wang EA, Matusko N, & Jackson JS (2014). A heavy burden: the cardiovascular health consequences of having a family member incarcerated. American Journal of Public Health, 104, 421–427. doi: 10.2105/AJPH.2013.301504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Laursen TM, Precht DH, Olsen J, & Mortensen PB (2005). Hospitalization for mental illness among parents after the death of a child. New England Journal of Medicine, 352, 1190–1196. doi: 10.1056/NEJMoa033160 [DOI] [PubMed] [Google Scholar]
- Massoglia M, Firebaugh G, & Warner C (2013). Racial variation in the effect of incarceration on neighborhood attainment. American Sociological Review, 78, 142–165. doi: 10.1177/0003122412471669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massoglia M, Pare PP, Schnittker J, & Gagnon A (2014). The relationship between incarceration and premature adult mortality: Gender specific evidence. Social Science Research, 46, 142–154. doi: 10.1016/j.ssresearch.2014.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massoglia M, & Pridemore WA (2015). Incarceration and health. Annual Review of Sociology, 41, 291–310. doi: 10.1146/annurev-soc-073014-112326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naser RL, & La Vigne NG (2006). Family support in the prisoner reentry process: Expectations and realities. Journal of Offender Rehabilitation, 43, 93–106. doi: 10.1300/J076v43n01_05 [DOI] [Google Scholar]
- Patterson EJ (2013). The dose-response of time served in prison on mortality: New York State, 1989–2003. American Journal of Public Health, 103, 523–528. doi: 10.2105/AJPH.2012.301148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI (1989). The sociological study of stress. Journal of Health and Social Behavior, 30, 241–256. [PubMed] [Google Scholar]
- Porter LC (2014). Incarceration and post-release health behavior. Journal of Health and Social Behavior, 55, 234–249. doi: 10.1177/0022146514531438 [DOI] [PubMed] [Google Scholar]
- Porter LC, & Novisky MA (2017). Pathways to depressive symptoms among former inmates. Justice Quarterly, 34, 847–872. doi: 10.1080/07418825.2016.1226938 [DOI] [Google Scholar]
- Rosen DL, Schoenbach VJ, & Wohl DA (2008). All-cause and cause-specific mortality among men released from state prison, 1980–2005. American Journal of Public Health, 98, 2278–2284. doi: 10.2105/AJPH.2007.121855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen DL, Wohl DA, & Schoenbach VJ (2011). All-cause and cause-specific mortality among black and white North Carolina state prisoners, 1995–2005. Annals of Epidemiology, 21, 719–726. doi: 10.1016/j.annepidem.2011.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders CM (1980). A comparison of adult bereavement in the death of a spouse, child, and parent. Omega - Journal of Death and Dying, 10, 303–322. doi: 10.2190/X565-HW49-CHR0-FYB4 [DOI] [Google Scholar]
- Schnittker J, Massoglia M, & Uggen C (2011). Incarceration and the health of the African American community. Du Bois Review: Social Science Research on Race, 8, 133–141. doi: 10.1017/S1742058X11000026 [DOI] [Google Scholar]
- Segal NL, & Roy A (2001). Suicidal attempts and ideation in twins whose co-twins’ deaths were non-suicides: Replication and elaboration. Personality and Individual Differences, 31, 445–452. doi: 10.1016/S0191-8869(00)00149-5 [DOI] [Google Scholar]
- Shahar DR, Schultz R, Shahar A, & Wing RR (2001). The effect of widowhood on weight change, dietary intake, and eating behavior in the elderly population. Journal of Aging and Health, 13, 186–199. doi: 10.1177/089826430101300202 [DOI] [PubMed] [Google Scholar]
- Spaulding AC, Seals RM, McCallum VA, Perez SD, Brzozowski AK, & Steenland NK (2011). Prisoner survival inside and outside of the institution: implications for health-care planning. American Journal of Epidemiology, 173, 479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spohn C (2015). Race, crime, and punishment in the twentieth and twenty-first centuries. Crime and Justice, 44, 49–97. doi: 10.1086/681550 [DOI] [Google Scholar]
- Stephen AI, Macduff C, Petrie DJ, Tseng FM, Schut H, Skår S, … Wilson S (2015). The economic cost of bereavement in Scotland. Death Studies, 39, 151–157. doi: 10.1080/07481187.2014.920435 [DOI] [PubMed] [Google Scholar]
- Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA, Hartge P, … de Gonzalez AB (2017). Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. The Lancet, 389, 1043–1054. doi: 10.1016/S0140-6736(17)30187-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe M, & Schut H (2005). To continue or relinquish bonds: A review of consequences for the bereaved. Death Studies, 29, 477–494. doi: 10.1080/07481180590962659 [DOI] [PubMed] [Google Scholar]
- Stroebe M, Schut H, & Stroebe W (2007). Health outcomes of bereavement. Lancet (London, England), 370, 1960–1973. doi: 10.1016/S0140-6736(07)61816-9 [DOI] [PubMed] [Google Scholar]
- Stroebe MS, Hansson RO, Schut H, & Stroebe W (2008). Bereavement research: Contemporary perspectives. Handbook of Bereavement Research and Practice: Advances in Theory and Intervention, 3–25. [Google Scholar]
- Testa A, & Porter LC (2017). No rest for the wicked? The consequences of incarceration for sleep problems. Society and Mental Health, 7, 196–208. doi: 10.1177/2156869317707002 [DOI] [Google Scholar]
- Testa A, Porter LC, & Nakamura K (2018). Examining all-cause and cause-specific mortality among former prisoners in Pennsylvania. Justice Quarterly, 35, 782–815. doi: 10.1080/07418825.2017.1341541 [DOI] [Google Scholar]
- Toch H, Adams K, & Grant JD (1989). Coping: Maladaptation in prisons. New Jersey, NY: Transaction Publishers. [Google Scholar]
- Travis J, Western B, & Redburn FS (2014). The growth of incarceration in the United States: Exploring causes and consequences. Washington, DC: National Academies Press. [Google Scholar]
- Turney K (2014). Stress proliferation across generations? Examining the relationship between parental incarceration and childhood health. Journal of Health and Social Behavior, 55, 302–319. doi: 10.1177/0022146514544173 [DOI] [PubMed] [Google Scholar]
- Turney K, Wildeman C, & Schnittker J (2012). As fathers and felons: Explaining the effects. Journal of Health and Social Behavior, 53, 465–481. doi: 10.1177/0022146512462400 [DOI] [PubMed] [Google Scholar]
- Umberson D, Olson JS, Crosnoe R, Liu H, Pudrovska T, & Donnelly R (2017). Death of family members as an overlooked source of racial disadvantage in the United States. Proceedings of the National Academy of Sciences, 114, 915–920. doi: 10.1073/pnas.1605599114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Weijer SG, Smallbone HS, & Bouwman V (2018). Parental Imprisonment and Premature Mortality in Adulthood. Journal of Developmental and Life-Course Criminology, 4, 148–161. doi: 10.1007/s40865-017-0078-1 [DOI] [Google Scholar]
- Western B, Braga AA, Davis J, & Sirois C (2015). Stress and hardship after prison. American Journal of Sociology, 120, 1512–1547. [DOI] [PubMed] [Google Scholar]
- Wildeman C (2012). Imprisonment and infant mortality. Social Problems, 59, 228–257. [Google Scholar]
- Wildeman C, & Muller C (2012). Mass imprisonment and inequality in health and family life. Annual Review of Law and Social Science, 8, 11–30. doi: 10.1146/annurev-lawsocsci-102510-105459 [DOI] [Google Scholar]
- Wildeman C, & Wang EA (2017). Mass incarceration, public health, and widening inequality in the USA. Lancet (London, England), 389, 1464–1474. doi: 10.1016/S0140-6736(17)30259-3 [DOI] [PubMed] [Google Scholar]
- Wildeman C, Andersen SH, Lee H, & Karlson KB (2014). Parental incarceration and child mortality in Denmark. American Journal of Public Health, 104, 428–433. doi: 10.2105/AJPH.2013.301590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildeman C, Schnittker J, & Turney K (2012). Despair by association? The mental health of mothers with children by recently incarcerated fathers. American Sociological Review, 77, 216–243. doi: 10.1177/0003122411436234 [DOI] [Google Scholar]


