Abstract
Background:
Anatomical and developmental variations of ureters and renal pelvis have been observed frequently during routine human cadaveric dissection and surgical practice; however, their coexistence with accessory or aberrant renal arteries is exceptionally rare. Accordingly, this study was designed to evaluate the prevalence of anatomical and developmental abnormalities of ureters and renal pelvis existing with accessory renal arteries in human cadavers.
Materials and Methods:
This study was carried out on 50 human cadavers including dissected specimens (25 males and 25 females) the kidneys, renal pelvis, and ureters along with their arteries were exposed and the anomalous abnormalities of the renal pelvis and ureters existing with accessory renal arteries were observed. Photographs of the anomalous and developmental variations were taken for proper documentation.
Results:
Among the 50 cadavers studied, unilateral double ureters were found in 5 cadavers (10%), rare bilateral “S-”shaped loop of ureter with quadruple uretic constrictors in the abdominal segment of the ureter was observed in one female cadaver (2%), accessory or aberrant renal arteries were found in 15 cadavers (30%), hydronephrosis involving the renal pelvis and ureters was observed in 9 cadavers (18%). Interestingly, this prevalence was higher among males (28%) compared to females (8%). Moreover, the occurrence of bilateral hydronephrosis of the kidneys, renal pelvis, and ureters was identified in a single male cadaver, representing 2% of the sample. Notably, the prevalence of double ureter, hydronephrosis accompanied by congenital double and triple accessory renal arteries was documented in nine cadavers, accounting for 18% of the cohort.
Conclusion:
Anatomical and developmental variations of the ureters, renal pelvis, and renal vasculature, as well as their relationships to surrounding structures, hold clinical significance due to their impact on various surgical procedures, including kidney transplantation, abdominal aorta reconstruction, interventional radiology, and urologic operations. Therefore, identifying these potential developmental variations is essential for effective surgical management to preserve renal function and ensure optimal patient outcomes.
Keywords: Accessory renal arteries, duplex ureters, hydronephrosis, hydroureter, ureteral obstruction, Wolffian duct
Résumé
Contexte:
Des variations anatomiques et développementales des uretères et du bassinet du rein ont été fréquemment observées au cours de routines d’examens cadavériques humains. dissection et pratique chirurgicale; cependant, leur coexistence avec des artères rénales accessoires ou aberrantes est exceptionnellement rare. En conséquence, cette étude a été conçu pour évaluer la prévalence des anomalies anatomiques et du développement des uretères et du bassinet du rein existant avec des anomalies rénales accessoires. artères dans les cadavres humains.
Matériels et méthodes:
Cette étude a été réalisée sur 50 cadavres humains dont des spécimens disséqués (25 mâles et 25 femmes), les reins, le bassinet et les uretères ainsi que leurs artères ont été exposés et les anomalies anormales du système rénal un bassin et des uretères existant avec des artères rénales accessoires ont été observés. Des photographies des variations anormales et développementales ont été prises pour une documentation appropriée.
Résultats:
Parmi les 50 cadavres étudiés, des doubles uretères unilatéraux ont été retrouvés dans 5 cadavres (10 %), de rares cas bilatéraux. Une anse de l’uretère en forme de « S » avec des quadruples constricteurs urétiques dans le segment abdominal de l’uretère a été observée chez un cadavre féminin (2 %). des artères rénales accessoires ou aberrantes ont été retrouvées chez 15 cadavres (30 %), une hydronéphrose impliquant le bassinet et les uretères rénaux a été observée chez 9 cadavres (18 %). Il est intéressant de noter que cette prévalence était plus élevée chez les hommes (28 %) que chez les femmes (8 %). De plus, la survenue de conflits bilatéraux une hydronéphrose des reins, du bassinet du rein et des uretères a été identifiée sur un seul cadavre masculin, représentant 2 % de l’échantillon. Notamment, le La prévalence du double uretère et de l’hydronéphrose accompagnée d’artères rénales accessoires doubles et triples congénitales a été documentée dans neuf cas. cadavres, représentant 18% de la cohorte.
Conclusion:
Variations anatomiques et développementales des uretères, du bassinet et du rein le système vasculaire, ainsi que leurs relations avec les structures environnantes, revêtent une importance clinique en raison de leur impact sur diverses procédures chirurgicales, y compris la transplantation rénale, la reconstruction de l’aorte abdominale, la radiologie interventionnelle et les opérations urologiques. Par conséquent, identifier ces les variations potentielles du développement sont essentielles à une prise en charge chirurgicale efficace afin de préserver la fonction rénale et de garantir des résultats optimaux pour les patients.
Mots-clés: Artères rénales accessoires, uretères duplex, hydronéphrose, hydrouretère, obstruction urétérale, canal de Wolff
INTRODUCTION
The human ureters are paired muscular tubes that serve a vital role in the urinary system by transporting urine from the kidneys to the bladder. Each ureter originates from the renal pelvis of each kidney. The renal pelvis is a funnel-shaped structure in the kidney that collects urine from the major calyces and channels it into the ureter. Any obstruction or infection in the renal pelvis can lead to significant health issues, such as hydronephrosis or pyelonephritis. Each ureter is approximately 25–30 cm long and 3–4 mm wide and is divided anatomically into several distinct parts along its course from the renal pelvis to the bladder. Starting with the renal pelvis, where urine collects from the kidney’s collecting ducts, the ureter extends downward and narrows at the ureteropelvic junction. From the ureteropelvic junction, it continues as the abdominal ureter, descending along the posterior abdominal wall. As it reaches the pelvic cavity, it becomes the pelvic ureter, passing over the pelvic brim and traveling posterior to the internal iliac vessels in males (and posterior to the uterine artery and anterior to the vagina in females). The ureter then enters the bladder wall obliquely at the ureterovesical junction, forming a valve-like mechanism that prevents the backflow of urine into the ureter. This anatomical division is crucial for understanding the ureter’s function in transporting urine from the kidneys to the bladder, as well as for diagnosing and managing conditions such as ureteral stones, strictures, and reflux. Understanding the anatomy and function of ureters is crucial for diagnosing and managing conditions such as kidney stones, ureteral strictures, and vesicoureteral reflux, thereby preserving optimal urinary system function and health. The ureters feature three natural constrictions along their length, strategically positioned to regulate urine flow and prevent backflow. The first constriction is at the ureteropelvic junction, where the renal pelvis narrows to become the ureter. This area helps maintain pressure differentials to facilitate urine passage into the ureter while preventing reflux into the kidney. The second constriction occurs as the ureter crosses the pelvic brim over the common iliac vessels. This site’s anatomical relationship with the vessels creates a narrowing that enhances the peristaltic propulsion of urine through the ureter. The third and final constriction is at the ureterovesical junction, where the ureter enters the bladder wall obliquely. Here, the oblique insertion creates a functional valve that prevents urine from backing up into the ureter during bladder filling and emptying. These constrictions play a critical role in maintaining urinary flow dynamics and preventing complications such as hydronephrosis, kidney stone formation, and vesicoureteral reflux. Understanding their positions and functions is essential for diagnosing and managing ureteral disorders effectively.
Double ureters, aberrant or accessory renal arteries, abnormal ureteric constrictions, hydronephrosis, and hydroureters are developmental and anatomical variations observed in the genitourinary tract. Double ureters result from embryological anomalies where the ureteric bud bifurcates early, leading to two ureters draining a single kidney. Aberrant renal arteries involve variations in the number, position, or branching pattern of arteries supplying the kidneys. Abnormal ureteric constrictions can restrict urinary flow, potentially causing obstruction. Hydronephrosis refers to the distension of the renal pelvis due to urine accumulation secondary to obstruction, whereas hydroureters indicate dilation of the ureters. Clinically, these variations pose challenges in surgical procedures such as kidney transplantation and necessitate precise anatomical knowledge for successful outcomes. They can predispose individuals to urinary tract infections, renal impairment, and if untreated, complications such as renal damage and hypertension, underscoring the importance of early detection and management in clinical practice. According, this study was designed to evaluate the prevalence of anatomical and developmental variations of the renal pelvis, ureter, existing with accessory or aberrant renal arteries. Understanding these abnormalities helps in early identification and intervention, which can prevent long-term kidney damage and preserve renal function.
MATERIALS AND METHODS
This study was carried out on routine human cadaveric dissection of the abdomen (including dissected cadaveric specimens) conducted for medical undergraduates teaching purpose at respective anatomy departments. This study was reviewed and approved by the Institutional Ethics Committee (reference number: IECVAMC-ANT005 DEC 023). The kidneys, ureters, and along with their arteries were exposed and the anatomical and developmental variations of the renal pelvis and ureters were observed. Photographs of the anatomical and developmental variations were taken for proper documentation.
RESULTS
Out of 50 human cadavers (including dissected cadaveric specimens), the following anatomical and congenital abnormalities of the renal pelvis and ureters coexisting with accessory renal arteries were noted [Table 1].
Table 1.
Anatomical and developmental abnormalities of ureters and renal pelvis existing with accessory renal arteries
| Anomalies/abnormalities | Total number of cadavers studied (25 males, 25 females) | Prevalence (%) - unilateral | Prevalence (%) - bilateral |
|---|---|---|---|
| Double ureters | 50 | 10% (5 male cadavers) | - |
| “S-”shaped ureters | 50 | - | 2% (1 female cadaver) |
| Hydronephrosis of renal pelvis and ureters | 50 | 8% (4 male cadavers) | 10% (4 male and 1 female cadavers) |
| Hydronephrosis of kidneys, renal pelvis and ureters | 50 | - | 2% (1 male cadaver) |
| Accessory renal arteries | 50 | 10% (3 male and 2 female cadavers) | 20% (8 male and 2 female cadavers) |
DISCUSSION
Double or duplex ureters
Double or duplex ureters arise from the bifurcation of the ureteric bud during embryonic development, resulting in two ureters that may either partially or completely drain a single kidney. In the 5th week of embryonic development, the dorsomedial aspect of the caudal mesonephric duct gives rise to a structure called the ureteric bud. This bud extends cranially and forms a dilation, which is subsequently encased by a cap-like structure known as the metanephric blastema. The ureteric bud undergoes multiple divisions, leading to the formation of the major and minor calyces, as well as the collecting tubules of the kidney. The stalk of the ureteric bud develops into the ureter, whereas its dilated end remains as the renal pelvis. Double or duplex ureters result from the early splitting of the ureteric bud during embryogenesis, leading to two ureters draining a single kidney. Duplicated ureter occurs approximately 1% of the population, Siomou et al., reported the duplex collecting.[1] Chakravarthi et al. reported a case of unilateral double ureters descended from the separate renal pelvis (double pelvis) originated from the upper and lower renal poles of the right kidney joined at the middle in a Y-shaped manner.[2] Deka and Saikia observed double ureters in 1.67% of 60 specimens, all of which were on the left side.[3] In a study by Choudhary et al. involving 32 specimens, two kidneys (6.25%) exhibited unilateral incomplete duplication.[4] Arumugam et al. reported double ureters in 6% of 50 specimens.[5] Another study by Roy et al. found double ureters in 0.64% of 156 kidney specimens.[6] In the present study, we observed unilateral complete and incomplete double ureters in 5 male cadavers (10%) [Figures 1-3]. Such developmental variations were probably due to double ureteric buds arising from the caudal part of the mesonephric duct. These anomalies can be linked to congenital genitourinary tract defects such as ectopic ureters and an elevated risk of urinary tract infections, pain, hydronephrosis, and nephrolithiasis. Dalzell et al. reported a case where a duplex ureter was damaged during a laparoscopic hysterectomy and was diagnosed postoperatively.[7] Therefore, understanding the embryological and anatomical variations of the ureter is essential for recognizing and managing various congenital and acquired disorders of the urinary system.
Figure 1.

Posterior view of the right kidney showing congenital unilateral incomplete double ureter. Black arrow = Right renal artery, Yellow arrow = Superior polar artery, Red arrow = Incomplete double ureter
Figure 3.

Anterior view of the left kidney showing congenital unilateral complete double ureter. Black arrow = Right renal artery; Red arrows = Unilateral Complete double ureters
Figure 2.

Anterior view of the right kidney showing congenital unilateral complete double ureter. Black arrow = Right renal artery, Red arrow = Unilateral Complete double ureters
Abnormal loop of the ureter with abnormal constrictions
The ureter has three primary anatomical constrictions where the lumen is naturally narrower than the rest of the ureter. These constrictions are important clinically because they are common sites where kidney stones can become lodged. The transition from the wide renal pelvis to the narrower ureter forms the ureteropelvic junction constrictor. As the kidneys ascend from the pelvic region to their final position in the abdomen during development, the ureters elongate and course over the iliac vessels. The anatomical relationship and the pressure from these vessels create a natural narrowing (constriction). The ureterovesical junction forms the third constriction, as the distal end of the ureteric bud incorporates into the developing bladder. The oblique passage of the ureter through the bladder wall is essential for forming a functional valve that prevents backflow. Understanding these anatomical constrictions is crucial for diagnosing and treating various conditions related to the urinary system. The bilateral quadruple abnormal constrictions in the double “S-”shaped loop of the abdominal segment of the ureter below the ureteropelvic junction observed in our study likely result from disruptions during embryonic development [Figure 4]. To the best of our knowledge, such developmental variations observed in this study have not been cited in modern literature. Normally, the ureteric bud, an outgrowth from the mesonephric duct, elongates, branches, and differentiates to form the ureter. This process is tightly regulated by a series of genetic and molecular signals, including growth factors and transcription factors. Any genetic mutations or variations in key developmental genes (Such as GDNF (Glial Cell Line-Derived Neurotrophic Factor), RET (Rearranged during Transfection), and BMP4 (Bone Morphogenetic Protein 4)) can disrupt these signaling pathways, leading to improper ureteral formation. For instance, if the signaling that directs the elongation and positioning of the ureter is abnormal, it can result in atypical shapes, such as a double “S-”shaped loop with multiple constrictions. In addition, environmental and mechanical factors during fetal development can contribute to these anomalies. The presence of accessory or aberrant renal arteries can exert extrinsic pressure on the developing ureter, causing it to kink and form abnormal loops. Mechanical constraints within the intrauterine environment, such as oligohydramnios (reduced amniotic fluid), can also physically distort the growing ureter, leading to multiple constrictions. Furthermore, exposure to teratogens (substances that can cause congenital malformations) during critical periods of renal and ureteric development may result in structural anomalies. These factors, acting alone or in combination, can disrupt normal ureteric development, resulting in the complex and rare anatomical variations observed in this study. Understanding the developmental processes of the ureter is crucial in clinical practice for diagnosing and managing congenital and acquired urinary tract conditions. This knowledge aids in identifying congenital anomalies such as renal agenesis, ureteropelvic junction obstruction, and duplicated or ectopic ureters, which can lead to complications such as hydronephrosis, recurrent infections, and urinary incontinence. Early detection through prenatal ultrasounds and appropriate surgical interventions, such as correcting obstructions or reimplanting ureters, rely on a thorough grasp of ureteral development. In addition, recognizing the natural constriction points where kidney stones commonly lodge helps in effective diagnosis and treatment. Thus, developmental insights into the ureter’s formation are essential for optimizing patient outcomes in urological health.
Figure 4.

Showing congenial bilateral double “S” shaped loop of the ureter with quadruple abnormal ureteric constrictions existing with bilateral accessory renal arteries. Blue arrows = Quadruple abnormal constrictions of abdominal segment of ureter, Red arrows = Accessory renal arteries (lower polar arteries)
Hydroureter and hydronephrosis
Hydronephrosis and hydroureter are prevalent conditions managed by urologists, emergency medicine specialists, and primary care physicians. Hydronephrosis is a condition characterized by the dilatation of the urinary collecting system of the kidney. It occurs when there is an obstruction or blockage in the urinary tract, preventing urine from draining properly from the kidney to the bladder. The blockage can be located anywhere along the urinary tract, including the ureters, bladder, or urethra. This condition can vary in severity, from mild swelling to significant enlargement that can cause kidney damage. Common causes of hydronephrosis include kidney stones, congenital anomalies, tumors, and conditions such as benign prostatic hyperplasia. Pathologically, the obstruction leads to increased pressure within the urinary system, causing the renal pelvis and calyces to dilate. Symptoms can include pain in the side and back (flank pain), nausea, vomiting, frequent urination, and urinary tract infections. Over time, this pressure can impair renal function, leading to decreased glomerular filtration rate and, eventually, renal atrophy and fibrosis if left untreated. Nephrolithiasis (kidney stones) stands as the primary etiology for hydroureteronephrosis among young adults, with an estimated 600,000 cases of kidney stones occurring annually in the United States, affecting nearly 1 in 11 individuals. Hansen et al. reported that calculi were the most common cause of hydronephrosis in adults.[8] In a study conducted by Riddell et al., bedside ultrasound demonstrated a sensitivity ranging from 72% to 83% in detecting unilateral hydronephrosis.[9] Another investigation by Moş et al. found that transabdominal ultrasound identified hydronephrosis in 88.94% of cases and detected ureteric calculi in approximately 73% of patients.[10] Sternberg et al. reported that ultrasound findings of hydronephrosis had a positive predictive value of 77% and a negative predictive value of 71% for diagnosing ureteric calculi.[11] In our study, the prevalence of hydronephrosis and hydroureter was observed in 10 cadavers (20%) [Figures 5-8]. Chakravarthi et al. documented bilateral hydronephrosis involving the kidneys and pelvis of the ureters, in our study, we similarly observed bilateral hydronephrosis affecting the kidneys, pelvis of the ureters, and the ureters.[12] Thus, anatomical knowledge of hydronephrosis and hydroureter is crucial in diagnosing, managing, and treating urinary tract disorders. This expertise enables clinicians to accurately identify the cause and location of obstructions, such as ureteropelvic junction obstruction, vesicoureteral reflux, or ureterovesical junction obstruction, through advanced imaging techniques.
Figure 5.

Anterior view of kidneys showing bilateral hydronephrosis of the renal pelvis and ureters existing with bilateral accessory renal arteries. Red arrows = Bilateral hydronephrosis of renal pelvis, Blue arrows = Bilateral hydroureter, Black arrows = Renal arteries, Yellow arrows = Bilateral accessory renal arteries
Figure 8.

Anterior view of left kidney showing Unilateral hydronephrosis of renal pelvis existing with unilateral accessory renal arteries. Red arrows = Hydronephrosis of renal pelvis, Black arrow = Accessory renal arteries
Figure 6.

Anterior view of the right kidney showing unilateral hydronephrosis of the renal pelvis and ureters existing. Red arrow = Unilateral hydronephrosis of renal pelvis, Blue arrow = Unilateral hydroureter, Black arrow = Right renal arteries
Figure 7.
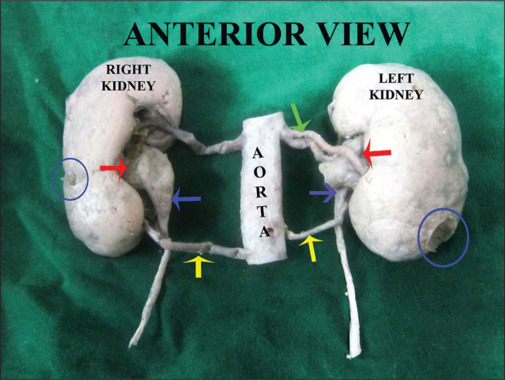
Anterior view of kidneys showing bilateral hydronephrosis of the renal pelvis and ureters existing with bilateral accessory renal arteries. Red arrows = Bilateral hydronephrosis of renal pelvis, Blue arrows = Bilateral hydroureter, Yellow arrows = bilateral accessory renal arteries, Green arrow = accessory renal arteries, Blue circles: Hydronephrosis of kidneys
Anomalous renal arteries in relation to abnormal ureters and renal pelvis
Variations in renal vessels are frequently observed during routine dissection and surgical practice; however, their coexistence with congenital anomalies or abnormalities of the kidneys or ureters is exceptionally rare. Normally, each kidney is supplied by a single renal artery, typically originate from the abdominal aorta, just below the superior mesenteric artery, at the level of the L1 and L2 vertebrae, run posterior to the renal veins and anterior to the renal pelvis and proximal ureters as they enter the kidney hilum. Accessory renal arteries are extra arteries that supply blood to the kidneys, usually originating from the abdominal aorta. They can lead to various complications. These arteries are usually common anatomical variant present in approximately 25%–30% of individuals. When abnormal ureters and renal pelvis are accompanied by anomalous renal arteries, the clinical implications can be more complex. These accessory renal arteries can complicate surgical interventions, renal transplants, and imaging studies and may be associated with hypertension and other vascular conditions. Accessory renal arteries, commonly arising from the abdominal aorta either above or below the main renal artery, are considered persistent embryonic lateral splanchnic arteries. Unilateral or bilateral double and triple renal arteries are reported by many authors.[13,14,15,16,17] The incidence of accessory renal arteries has been reported at various rates: 50% by Helstrom, 25% by Edsman, and 30% by Henry Gray.[18,19,20] In a cadaver study, Pollak et al. found 23% had double renal arteries, 4% had triple arteries, and 1% had quadruple arteries.[21] An angiographic study by Ozkan et al. reported multiple renal arteries in 24% of cases, bilateral multiple arteries in 5%, early arterial division in 8%, and bilateral aberrant renal arteries in 13%–16% of cases.[22] Adult polycystic kidney disease, an autosomal dominant disorder with high penetrance, occurs in 1 out of 400–1000 individuals and accounts for 5%–10% of chronic renal failure cases.[23] In our study, accessory or aberrant renal arteries were observed in 15 cadavers (30%). Unilateral and bilateral accessory renal arteries associated with bilateral hydronephrosis of the renal pelvis noted in this study are very rare [Figures 1-8]. Accessory renal arteries to the lower pole of the kidney noted in our study can increase the risk of bleeding during renal surgeries, such as nephrectomy or kidney transplantation, due to their unexpected presence and variability in location. Such congenital anomalies of renal arteries or pathological conditions affecting the renal vessels, such as vascular compression or aneurysms, can compress or distort adjacent ureters, leading to ureteral obstruction or hydronephrosis ureter or renal pelvis. This proximity is critical during surgical procedures involving the kidneys, as inadvertent injury to the ureters can occur, leading to complications such as urine leakage or strictures. In addition, the anatomical relationship aids in diagnostic imaging, where identifying potential compressions or abnormalities of the ureters by adjacent vascular structures helps in diagnosing and managing conditions such as ureteral obstruction or vascular anomalies affecting renal function. Understanding these relationships is essential for surgical planning, ensuring safe interventions, and optimizing outcomes in renal and urological care.
CONCLUSION
The observation of congenital anomalous double ureters, hydroureters, hydronephrosis, and accessory renal arteries as documented in this study is of substantial anatomical, developmental, and clinical significance. Anatomically, the presence of double ureters and accessory renal arteries indicates a deviation from typical renal vascular and urinary tract anatomy, which may complicate surgical interventions and diagnostic imaging. Developmentally, these anomalies suggest disruptions during embryogenesis, specifically in the processes of ureteric bud branching and renal arterial formation, which may provide insights into the mechanisms of renal and urinary tract malformations. Clinically, the coexistence of these anomalies can predispose patients to complications such as recurrent urinary tract infections, obstructive uropathy, and progressive renal damage due to hydronephrosis. Recognizing and understanding these anomalies are crucial for accurate diagnosis, effective management, and improving patient outcomes in individuals with complex renal and urinary tract abnormalities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Siomou E, Papadopoulou F, Kollios KD, Photopoulos A, Evagelidou E, Androulakakis P, et al. Duplex collecting system diagnosed during the first 6 years of life after a first urinary tract infection: A study of 63 children. J Urol. 2006;175:678–81. doi: 10.1016/S0022-5347(05)00184-9. [DOI] [PubMed] [Google Scholar]
- 2.Chakravarthi KK, Karuneswari DP, Uma MN. Congenital unilateral double renal pelvis and double ureters associated with triple renal veins and left retro aortic renal vein. Int J Chem Life Sci. 2013;2:1159–62. [Google Scholar]
- 3.Deka B, Saikia R. A study of human cadaveric ureter by simple dissection method. Int J Anat Res. 2016;4:3005–8. [Google Scholar]
- 4.Choudhary U, Kumar S, Jee K, Singh A, Bharti P. A cadaveric study on anatomical variations of kidney and ureter in India. Int J Res Med Sci. 2017;5:2358. [Google Scholar]
- 5.Arumugam S, Subbiah NK, Mariappan Senthiappan A. Double ureter: Incidence, types, and its applied significance-a cadaveric study. Cureus. 2020;12:e7760. doi: 10.7759/cureus.7760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roy M, Singh BR, Gajbe UL, Thute PJ. Anatomical variations of ureter in central India: A cadaveric study. Datta Meghe Inst Med Sci Univ. 2017;12:277–9. [Google Scholar]
- 7.Dalzell AP, Robinson RG, Crooke KM. Duplex ureter damaged during laparoscopic hysterectomy. Pelviperineology. 2010;29:88. [Google Scholar]
- 8.Hansen KL, Nielsen MB, Ewertsen C. Ultrasonography of the kidney: A pictorial review. Diagnostics (Basel) 2015;6:2. doi: 10.3390/diagnostics6010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riddell J, Case A, Wopat R, Beckham S, Lucas M, McClung CD, et al. Sensitivity of emergency bedside ultrasound to detect hydronephrosis in patients with computed tomography-proven stones. West J Emerg Med. 2014;15:96–100. doi: 10.5811/westjem.2013.9.15874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moş C, Holt G, Iuhasz S, Moş D, Teodor I, Hălbac M. The sensitivity of transabdominal ultrasound in the diagnosis of ureterolithiasis. Med Ultrason. 2010;12:188–97. [PubMed] [Google Scholar]
- 11.Sternberg KM, Pais VM, Jr., Larson T, Han J, Hernandez N, Eisner B. Is hydronephrosis on ultrasound predictive of ureterolithiasis in patients with renal colic? J Urol. 2016;196:1149–52. doi: 10.1016/j.juro.2016.04.076. [DOI] [PubMed] [Google Scholar]
- 12.Chakravarthi KK, Siddaraju KS, Venumadhav N. Anomalous renal vasculature existing with congenital anomalies of kidneys, ureters and suprarenal glands: A cadaveric study. Ital J Anat Embryol. 2020;124:517–26. [Google Scholar]
- 13.Saldarriaga B, Pérez AF, Ballesteros LE. A direct anatomical study of additional renal arteries in a Colombian mestizo population. Folia Morphol (Warsz) 2008;67:129–34. [PubMed] [Google Scholar]
- 14.Tuteja SY, Forgacs B. Multiple renal arteries. N Engl J Med. 2019;381:862. doi: 10.1056/NEJMicm1902894. [DOI] [PubMed] [Google Scholar]
- 15.Gulas E, Wysiadecki G, Cecot T, Majos A, Stefańczyk L, Topol M, et al. Accessory (multiple) renal arteries – Differences in frequency according to population, visualizing techniques and stage of morphological development. Vascular. 2016;24:531–7. doi: 10.1177/1708538116631223. [DOI] [PubMed] [Google Scholar]
- 16.Bayazit M, Göl MK, Zorlutuna Y, Tasdemir O, Bayazit K. Bilateral triple renal arteries in a patient with iliac artery occlusion: A case report. Surg Radiol Anat. 1992;14:81–3. doi: 10.1007/BF01628048. [DOI] [PubMed] [Google Scholar]
- 17.Chakravarthi KK. Unilateral multiple variations of renal, phrenic, suprarenal, inferior mesenteric and gonadal arteries. J Nat Sci Biol Med. 2014;5:173–5. doi: 10.4103/0976-9668.127320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Helstrom J. A contribution to the knowledge of the relation of abnormally running renal vessels to hydronephrosis, and an investigation of the arterial conditions in fifty kidneys. Acta Chirurgica Scandinavica. 1927;61:289–330. [Google Scholar]
- 19.Edsman G. Accessory vessels of the kidney and their diagnosis in hydronephrosis. Acta radiol. 1954;42:26–32. doi: 10.3109/00016925409175092. [DOI] [PubMed] [Google Scholar]
- 20.Standring S. ed . 39th. Edinburgh: Elsevier Churchill Livingstone; 2005. Gray’s Anatomy: The Anatomical Basis of Clinical Practice; p. 1274. [Google Scholar]
- 21.Pollak R, Prusak BF, Mozes MF. Anatomic abnormalities of cadaver kidneys procured for purposes of transplantation. Am Surg. 1986;52:233–5. [PubMed] [Google Scholar]
- 22.Ozkan U, Oğuzkurt L, Tercan F, Kizilkiliç O, Koç Z, Koca N. Renal artery origins and variations: Angiographic evaluation of 855 consecutive patients. Diagn Interv Radiol. 2006;12:183–6. [PubMed] [Google Scholar]
- 23.Sujatha K, Rao S. A human cadaveric study on incidence, prevalence and morphology of cystic kidneys-with emphasis on its embryological, pathological and clinical significance. Int J Anat Res. 2017;5:4437–40. [Google Scholar]


