Abstract
Background:
Head injury rates in lacrosse may be higher among women compared with men. Understanding these trends can guide appropriate injury prevention for female athletes.
Hypotheses:
Injuries most commonly involve the head, with no significant decline over the study period; contact with other players would be the most common injury mechanism.
Study Design:
Descriptive epidemiological.
Level of Evidence:
Level 3.
Methods:
The National Electronic Injury Surveillance System (NEISS) was queried (January 1, 2008 to December 31, 2022) for women’s lacrosse injuries presenting to United States (US) emergency departments (EDs). Patient demographics, injury diagnosis, body part injured, disposition, and clinical narrative were extracted. The provided narrative identified the mechanism of injury. Linear regression analysis assessed trends over time.
Results:
An estimated 57,635 women’s lacrosse injuries occurred during the study period extrapolated from 1899 evaluated NEISS cases. The mean age was 15.81 ± 5.35 years, with 68.3% of injuries sustained by high school (14- to 18-year-old) players. Over one-third of all injuries were to the head (national estimate [NE], 19,358; 33.6%), followed by the ankle (NE, 10,475; 18.2%), then the knee (NE, 6969; 12.1%). Strain/sprains were most common (NE, 19,402; 33.7%) followed by closed head injury (CHI)/sports-related concussion (SRC) (NE, 11,794; 20.5%) and contusion/abrasion (NE, 10,605; 18.4%). ED presentations of CHIs/SRCs and fractures remained elevated with no significant decline over the study period (P > 0.05), despite a significant decrease in strains/sprains and contusions/abrasions (P < 0.01 and P = 0.01, respectively). The most common injury mechanism was collision/contact with another player (NE, 10,664; 18.5%).
Conclusion:
An estimated one-third of women’s lacrosse players in the study sample had a head injury. CHIs and SRCs accounted for 20.5% of all injuries.
Clinical Relevance:
Given the high proportion of contact-related head injuries, headgear mandates and improved player safety protocols may be warranted.
Keywords: concussions, head injuries, lacrosse, women
Although women’s lacrosse is considered a noncontact sport, recent literature has suggested that head injuries may occur at high rates compared with men.1,2,10,22 Current national regulations require that women’s lacrosse players wear only eye protection, while men’s lacrosse requires full helmet protection and gloves.1,2,17 Women’s lacrosse players may thus face an increased risk of head injuries, resulting in repetitive concussions and prolonged recovery times.1,9,19
The potential elevated risk of head injuries among female athletes has become an important topic of discussion. In a recent study, Pirruccio et al 19 examined 1,176,092 national weighted estimates of sports-related concussions (SRCs) or closed head injuries (CHIs) in female patients (age 14 to 18 years) and reported a 3-fold increase within the last 20 years. Moreover, there is a significant underrepresentation of women in SRC research. 11 Nearly half of the 171 studies included in a 2022 meta-analysis of concussion research did not include female participants, and those that did relied on samples that were, on average, 80.1% male. 11
The purpose of this study was to evaluate the frequency and distribution of women’s lacrosse injuries presenting to emergency departments (EDs) in the United States (US) and identify major contributing mechanisms in a nationally representative cohort. Conducting research on the etiology of SRC among female athletes will guide appropriate prevention protocols and awareness initiatives, especially considering the sex-based differences in head injury rates. 9 We hypothesized that the overall number of SRC/CHI would not show a significant decline over the study period, and that contact injuries with other players or with the ball/stick would contribute most toward SRC/CHI.
Methods
Database
The National Electronic Injury Surveillance System (NEISS) is a public, deidentified database that collects data from approximately 100 EDs across the US. The database is maintained by the US Consumer Product Safety Commission, and the 100 EDs are statistically selected to serve as a representative probability sample of >5000 EDs across the country. The representative probability sample allows for national estimates (NEs) to be calculated using the statistical sample weight assigned to each patient case at a given hospital.
Data Extraction
The NEISS database was queried retrospectively for all women’s lacrosse injuries from January 1, 2008 to December 31, 2022. The NEISS product code 1215 was used to identify lacrosse-related injuries. After filtering for women’s lacrosse injuries, there were 2050 NEISS eligible cases.
Patient demographic information provided in the dataset including the age, sex, and race of the patient were extracted. The ED visit date was recorded, along with the primary injury location/body part, diagnosis, and disposition. SRCs were identified with NEISS diagnosis code 52 for concussions. Internal head injuries (NEISS body part code 75; NEISS diagnosis code 62) were categorized as CHIs. We used the available narrative reported by the ED clinician to identify the primary mechanism of injury. Mechanisms of injury included a collision/contact with another player, contact with lacrosse stick, a twisting motion (defined as rotation/rolling/inversion/eversion of a joint), being struck by the lacrosse ball, and falls. “Other” injuries did not fit into any categories outlined (eg, impact with a rock, running into a pole, getting foot stuck in the net, etc). Injuries where no mechanism was indicated were categorized as “not specified.” The cases narratives were reviewed by 2 reviewers, and any disagreements were resolved by a third reviewer.
Exclusion Criteria
Injuries that were not directly while playing lacrosse were excluded (eg, an allergic reaction during lacrosse practice, a spectator getting hit by the ball, etc). Injuries involving multiple sports were excluded (eg, injured while playing basketball and aggravated injury while playing lacrosse). Cases were excluded during review of the clinical narrative associated with each patient.
Statistical Analysis
Data were analyzed using IBM SPSS Statistics Version 28.0 (IBM Corp LLC). The distribution of injuries by age, sex, diagnosis, body part/region, and primary mechanism of injury were analyzed using descriptive statistics. Linear regression analysis assessed injury trends over time with reporting of associatedP value, regression coefficient (β), and 95% CI. Injury frequency was the outcome of interest, and the year of injury was used as the independent variable for simple linear regression analysis of trends over time.
Results
Our retrospective query of the NEISS database produced 2050 women’s lacrosse injuries from January 1, 2008 to December 31, 2022. A total of 151 NEISS cases that did not involve injuries sustained directly while playing lacrosse were excluded, resulting in 1899 ultimately included for analysis. There were 57,635 nationally estimated (1899 NEISS cases) women’s lacrosse head and musculoskeletal injuries that presented to US EDs during the study period. The mean age was 15.8 ± 5.4 years, with 68.3% of all injuries sustained among high school-aged players (14 to 18 years) (Table 1).
Table 1.
Injury incidence characterized by demographics, body part, and diagnosis
| Category | NE | % | |
|---|---|---|---|
| Age, y | <14 | 12,469 | 21.6% |
| 14-18 | 39,366 | 68.3% | |
| >18 | 5800 | 10.1% | |
| Race | White | 35,964 | 62.4% |
| Black/African American | 2145 | 3.7% | |
| Other | 1446 | 2.5% | |
| Asian | 495 | 0.9% | |
| American Indian/Alaska Native | 80 | 0.1% | |
| Native Hawaiian/Pacific Islander | 10 | 0.0% | |
| Not specified | 17,495 | 30.4% | |
| Body part | Head | 19,358 | 33.6% |
| Ankle | 10,475 | 18.2% | |
| Knee | 6969 | 12.1% | |
| Finger | 3259 | 5.7% | |
| Wrist | 2722 | 4.7% | |
| Shoulder | 2387 | 4.1% | |
| Foot | 1820 | 3.2% | |
| Other | 10,645 | 18.5% | |
| Diagnosis | Strains/sprains | 19,402 | 33.7% |
| CHI/SRC | 11,794 | 20.5% | |
| Contusions/abrasions | 10,605 | 18.4% | |
| Fracture | 5629 | 9.8% | |
| Other | 10,205 | 17.7% |
CHI, closed head injury; NE, national estimate; SRC, sports-related concussion.
Injuries overall decreased during the study period (2008 to 2022; P = 0.01; β = -157.9; 95% CI, -274.05 to -41.76) (Figure 1); however, there was no significant decrease (P = 0.25) appreciated before the COVID-19 pandemic (2008 to 2019) with a 80.2% decrease in injuries from 2019 to 2020.
Figure 1.
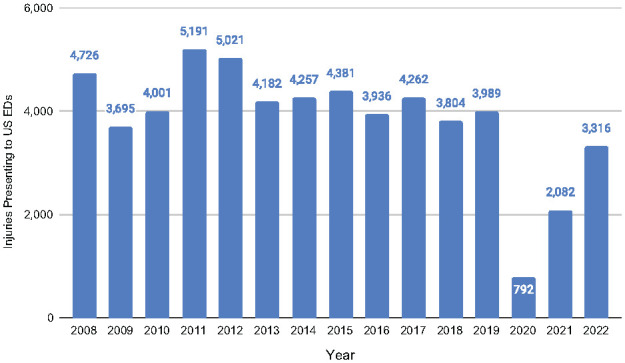
NEs of women’s lacrosse injuries presenting to US EDs. ED, emergency department; NE, national estimate; US, United States.
One-third of all women’s lacrosse injuries were sustained to the head (NE, 19,358; 33.6%) (Table 1). The ankle was the next most commonly injured body part (NE, 10,475; 18.2%), followed by the knee (NE, 6969; 12.1%). Strains/sprains (NE, 19,402; 33.7%) was the most common diagnosis, followed by CHI/SRC (NE, 11,794; 20.5%), contusion/abrasion (NE, 10,605; 18.4%), and fractures (NE, 5629; 9.8%).
Injuries sustained to the head remained prevalent, with no significant decline during the study period (P = 0.06) (Table 2 and Figure 2). Knee injuries similarly showed no significant decline during the study period (P = 0.93), while ankle injuries decreased significantly (P = 0.01).
Table 2.
Injury trends by body part and diagnosis from 2008 to 2022 using linear regression
| Category | Coefficient | 95% CI | PValue | |
|---|---|---|---|---|
| Body part | Head | -46.89 | -95.24 to 1.47 | 0.06 |
| Ankle | -46.46 | -79.05 to -13.88 | 0.01 | |
| Knee | -1.18 | -27.81 to 25.45 | 0.93 | |
| Diagnosis | Strains/sprains | -84.24 | -130.75 to -37.74 | <0.01 |
| CHI/SRC | -28.97 | -63.01 to 5.07 | 0.09 | |
| Contusions/abrasions | -44.82 | -77.13 to -12.52 | 0.01 | |
| Fracture | -17.62 | -35.76 to 0.52 | 0.06 |
CHI, closed head injury; SRC, sports-related concussion.
Figure 2.
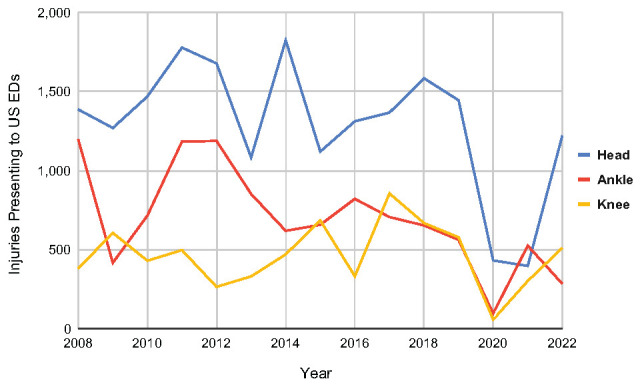
NEs of women’s lacrosse injuries presenting to US EDs for top 3 body parts. ED, emergency department; NE, national estimate; US, United States.
Assessment of injury trends by diagnosis revealed that ED presentations of CHI/SRC remained prevalent, with no significant decline over the study period (P = 0.09) (Table 2 and Figure 3). Moreover, strains/sprains (P < 0.01) and contusions/abrasions (P = 0.01) decreased significantly during the study period, whereas fractures showed no significant decrease (P = 0.06).
Figure 3.
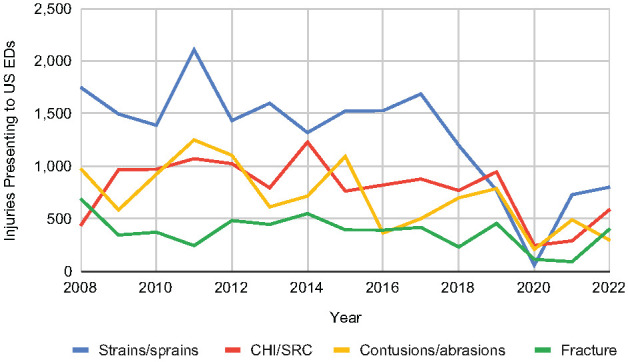
NEs of women’s lacrosse injuries presenting to US EDs for top 5 diagnoses. CHI, closed head injury; ED, emergency department; NE, national estimate; SRC, sports-related concussion; US, United States.
The most common injury mechanism was a collision/contact with another player, accounting for 18.5% of all injuries (NE, 10,664) (Table 3); 37.1% of all injuries involving a collision/contact with another player were sustained to the head. Contact with the lacrosse stick resulted in 17.2% of all injuries (NE, 9893) and involved head injury 59.4% of the time; 17.1% of all injuries were sustained due to a twisting motion (NE, 9828) and most often involved an ankle injury (62.4%). Being struck by the ball was the next most common mechanism of injury (NE, 9499; 16.5%), with a majority involving a head injury (71.4%). Finally, falls led to 10.53% (NE, 6068) of all injuries.
Table 3.
Stratification of injuries by mechanism and associated most frequently injured body parts
| Mechanism | NE | % | Most Frequently Injured Body Part |
|---|---|---|---|
| Collision/contact with player | 10,664 | 18.50% | Head |
| Contact with stick | 9893 | 17.16% | Head |
| Twist | 9828 | 17.05% | Ankle |
| Contact with ball | 9499 | 16.48% | Head |
| Fall | 6068 | 10.53% | Wrist |
| Other | 2421 | 4.20% | Lower trunk |
| Not specified | 9262 | 16.07% | Ankle |
NE, national estimate.
Injury trends stratified by age revealed a significant decrease in injuries presenting to US EDs among high school-age players during the study period (P = 0.03; β = -27.3; 95% CI, -51.57 to -3.04) (Figure 4). However, no significant decrease was identified before the COVID-19 pandemic (2008 to 2019; P = 0.60; β = -7.48; 95% CI, -38.39 to 23.43), and a drop in injuries of 62.5% was seen from 2019 to 2020 among high school-age women’s lacrosse players. No significant decreases were identified for those <14 years old (P = 0.70) or for those >18 (P = 0.78).
Figure 4.
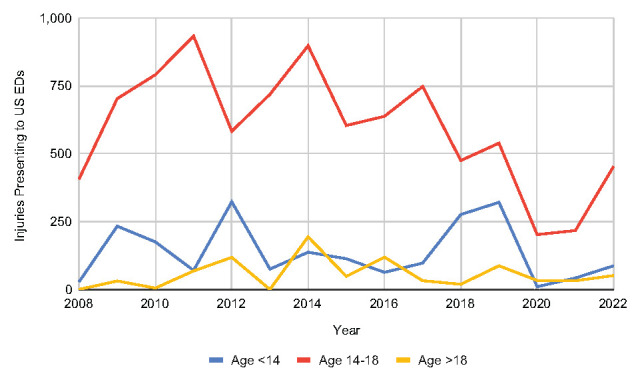
NEs of CHIs/SRCs stratified by age group from 2008 to 2022 using linear regression. CHI, closed head injury; ED, emergency department; NE, national estimate; SRC, sports-related concussion; US, United States.
Discussion
The number of head injuries in women’s lacrosse injuries presenting to US EDs in recent years has not demonstrated a significant decline, as one-third of injuries are sustained to the head and 1 in 5 injuries are diagnosed as SRC/CHI. Importantly, collisions with another player were found to be the major contributing mechanism despite women’s lacrosse being widely considered a noncontact sport. Furthermore, while injuries overall significantly decreased from 2008 to 2022, injuries of the head and knee as well as diagnoses of SRC/CHI and fracture remained elevated. Current efforts at injury prevention may be insufficient in mitigating head trauma in women’s lacrosse.
Previous literature has suggested a high proportion of women’s lacrosse injuries are sustained to the head.6,8,10,12 In 2021, Pirruccio et al 19 analyzed and ranked the most common sports or activities that led to head injuries and found that there were a total of 9742 SRC/CHI cases from high school women’s lacrosse between 2000 and 2019. In our study, we found one-third of all injuries localized to the head, and approximately 21% of injuries were diagnosed as a SRC/CHI. Despite the high incidence of concussions and head injuries, regulations surrounding helmets in women’s lacrosse remain controversial. Arguments against mandated headgear include the fact that the sport is noncontact, with rules prohibiting illegal contact with the head, helmets have not been proven to prevent concussions, and the “gladiator effect” phenomenon (where players would exhibit increased aggressive play under the notion that helmets would protect them). 13 Other advocates for game play without helmets argue that the traditional style of play should be maintained and more focus should be placed instead on rule enforcement by referees and adherence by coaches and players.14,15
In a recent study, however, Herman et al 13 showed that a statewide headgear mandate in Florida for high school girls’ lacrosse was associated with a lower concussion rate compared with girls playing in a state without a mandate. The study identified that players in states without a headgear mandate had a 59% greater incidence of sustaining concussions during practice than players required to wear headgear; during games, the incidence was higher, at 74%. 13 Other studies have similarly demonstrated that mandated headgear is effective at lowering the rate of head injuries in women’s lacrosse.4,7
Evidence-based decisions pertaining to rules, regulations, and protocols in sports are critical to minimize injury risk and ensure player safety. 3 Yet, there have been no national mandates on headgear use to date. One reason for this is the fact that the rules of women’s lacrosse explicitly prohibit illegal contact that could precipitate a head injury, which is why only eyewear and a mouthguard are required. However, our study demonstrates that a collision/contact with another player contributed to nearly 1 in 5 of all injuries. Furthermore, contact with the stick/ball resulted in one-third of all injuries. The high incidence of lacrosse stick-to-head injuries and lacrosse ball-to-head injuries among women’s lacrosse players has been supported by several studies in the sports medicine literature.1,10,16 Increased awareness of the injury burden associated with lacrosse may promote new regulations regarding protective equipment and precautions.1,10,16 The current regulations in girls’ high school lacrosse dictate all stick contact and body contact is illegal and warrants a penalty. Yet Caswell et al 7 found that 24% of all impacts resulted from foul play, which provides evidence that officials did not issue a penalty for approximately three-quarters of illegal contact. Our findings support the current literature that player contact in women’s lacrosse contributes to injuries and substantiates that adequate rule enforcement and regulations inclusive of mandated headgear are paramount.
The argument against headgear based on the “gladiator effect” was contradicted by Caswell’s study, which showed headgear did not change the rate of stick-to-head contact and lacrosse ball-to-head impacts or how they occur. 7 On the contrary, headgear reduced the magnitude of head accelerations associated with these impacts. 7 The data in our study reinforce previous findings that, while illegal contact will persist, headgear in women’s lacrosse may aid in reducing injury magnitude and severity, especially those arising from player-contact, stick-to-head injuries, and lacrosse ball-to-head injuries. 7
The COVID-19 pandemic significantly impacted the trend analysis of this study. Although overall injuries presenting to US EDs did decrease between 2008 and 2022, there was no significant decrease before 2019. In our present study, a 80.2% decrease in injuries presenting to US EDs was identified from 2019 to 2020. Interestingly, this decrease was higher than the 53.9% decrease in visits for injuries incurred during organized team sports in 2020 reported by Sabbagh et al. 20 This discrepancy may be a result of the closure of schools during the pandemic in 2020 and the associated reduction in organized high school team sports. 21 However, the finding that there was no change in injuries of the head or SRC/CHI diagnoses across the study period is especially concerning in the context of these reductions in overall injuries identified between 2008 and 2022.
This retrospective study is, to our knowledge, the first to assess long-term trends in ED visits for women’s lacrosse injuries and to identify the frequency, distribution, and trends of injury by mechanism, body part, diagnoses, and age group. By focusing our analysis of female athletes exclusively, this addresses a significant gap in the literature on the clinical management of head injuries in women’s sports, which have been historically underrepresented in the relevant literature. 11 Disparities in concussion diagnoses have significant clinical implications in the subsequent treatment and on long-term health and thus need to be addressed. 18
These findings highlight the importance of targeted prevention measures, concussion education initiatives, and evidence-based headgear mandates to address the alarming burden of head injuries, especially among high school-age women’s lacrosse players. Mandated protective headgear may aid in mitigating future head injuries and ensure women’s lacrosse is played as safely as possible.
Limitations
This study has major limitations. The NEISS dataset is only a cross-sectional probability sample and thus may not represent all national cases that presented to US EDs over the study period. These are only estimates. Whereas the database aims to serve as a representative sample of US EDs, it relies on cases collected from just 100 hospitals and thus is only an estimate of national injuries. Furthermore, the dataset only assesses injuries severe enough for patients to report to the ED for diagnosis and management, potentially omitting patients who may have presented to urgent care clinics or orthopaedic/pediatric offices for more minor injuries. SRC may also have been underdiagnosed depending on clinician variability in the ED. 5 In characterizing injury mechanism, a limitation was the brevity of the available narratives describing the injuries, which led to 16.1% of all injuries being categorized as “not specified.” Furthermore, the NEISS dataset does not include data on the specific injury sustained beyond the ED diagnosis and the body part.
Conclusion
This database study based on a representative sample of 100 US EDs demonstrated that one-third of women’s lacrosse injuries were sustained to the head, with CHIs and SRCs accounting for 20.5% of all injuries. Although overall injuries have declined over time, head injuries have not. At present, there are no national mandates on headgear in women’s lacrosse. To address the number of collision and contact-related head injuries, regulations may be warranted. The significant burden of injury among high school-age female lacrosse players suggests the importance of targeted prevention measures, education initiatives, and headgear protocols to ensure player safety.
Footnotes
The following author declared potential conflicts of interest: R.L.P. has received educational support from Gotham Surgical Solutions and Devices.
Contributor Information
Avanish Yendluri, Department of Orthopaedic Surgery, Icahn School of Medicine at Mount Sinai, New York, NY.
Katrina S. Nietsch, Department of Orthopaedic Surgery, Icahn School of Medicine at Mount Sinai, New York, NY.
Nikan K. Namiri, Department of Orthopaedic Surgery, Icahn School of Medicine at Mount Sinai, New York, NY.
Grant Gonsalves, Department of Orthopaedic Surgery, Icahn School of Medicine at Mount Sinai, New York, NY.
John J. Corvi, Department of Orthopaedic Surgery, Icahn School of Medicine at Mount Sinai, New York, NY.
Joseph Herrera, Department of Rehabilitation and Human Performance, Icahn School of Medicine at Mount Sinai, New York, NY.
Christopher J. Nowinski, Concussion Legacy Foundation, Boston, MA.
Robert L. Parisien, Department of Orthopaedic Surgery, Icahn School of Medicine at Mount Sinai, New York, NY.
References
- 1. Acabchuk RL, Johnson BT. Helmets in women’s lacrosse: what the evidence shows. Concussion. 2017;2(2):CNC39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barber Foss KD, Le Cara E, McCambridge T, Hinton RY, Kushner A, Myer GD. Epidemiology of injuries in women’s lacrosse: implications for sport-, level-, and sex-specific injury prevention strategies. Clin J Sport Med. 2018;28(4):406-413. [DOI] [PubMed] [Google Scholar]
- 3. Baroni BM, Oliveira Pena Costa L. Evidence-based prevention of sports injuries: is the sports medicine community on the right track? J Orthop Sports Phys Ther. 2021;51(3):91-93. [DOI] [PubMed] [Google Scholar]
- 4. Baron SL, Veasley SJ, Kingery MT, Nguyen MV, Alaia MJ, Cardone DA. Decreased injury rate following mandated headgear use in women’s lacrosse. Bull Hosp Jt Dis. 2020;78(4):260-265. [PubMed] [Google Scholar]
- 5. Boutis K, Weerdenburg K, Koo E, Schneeweiss S, Zemek R. The diagnosis of concussion in a pediatric emergency department. J Pediatr. 2015;166:1214-1220.e1. [DOI] [PubMed] [Google Scholar]
- 6. Bretzin AC, D’Alonzo BA, Chandran A, et al. Epidemiology of injuries in National Collegiate Athletic Association women’s lacrosse: 2014-2015 through 2018-2019. J Athl Train. 2021;56(7):750-757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Caswell SV, Kelshaw PM, Lincoln AE, et al. The effects of headgear in high school girls’ lacrosse. Orthop J Sports Med. 2020;8(12):2325967120969685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Comstock RD, Arakkal AT, Pierpoint LA, Fields SK. Are high school girls’ lacrosse players at increased risk of concussion because they are not allowed to wear the same helmet boys’ lacrosse players are required to wear? Inj Epidemiol. 2020;7(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Covassin T, Savage JL, Bretzin AC, Fox ME. Sex differences in sport-related concussion long-term outcomes. Int J Psychophysiol. 2018;132(Pt A):9-13. [DOI] [PubMed] [Google Scholar]
- 10. Diamond PT, Gale SD. Head injuries in men’s and women's lacrosse: a 10 year analysis of the NEISS database. National Electronic Injury Surveillance System. Brain Inj. 2001;15(6):537-544. [DOI] [PubMed] [Google Scholar]
- 11. D’Lauro C, Jones ER, Swope LM, Anderson MN, Broglio S, Schmidt JD. Under-representation of female athletes in research informing influential concussion consensus and position statements: an evidence review and synthesis. Br J Sports Med. 2022;56(17):981-987. [DOI] [PubMed] [Google Scholar]
- 12. Goldenberg MS, Hossler PH. Head and facial injuries in interscholastic women’s lacrosse. J Athl Train. 1995;30(1):37-41. [PMC free article] [PubMed] [Google Scholar]
- 13. Herman DC, Caswell SV, Kelshaw PM, Vincent HK, Lincoln AE. Association of headgear mandate and concussion injury rates in girls’ high school lacrosse. Br J Sports Med. 2022;56(17):970-974. [DOI] [PubMed] [Google Scholar]
- 14. Kelshaw PM, Eyerly DR, Herman DC, et al. Pilot study to explore girls’ lacrosse players’ attitudes toward headgear. Res Sports Med. 2023;31(6):873-880. [DOI] [PubMed] [Google Scholar]
- 15. Lacrosse Fanatic. An overview of helmets in women’s lacrosse. https://lacrossefanatic.com/blogs/news/an-overview-of-helmets-in-women-s-lacrosse. Accessed September 16, 2023.
- 16. Le RK, Saunders TD, Breedlove KM, Bradney DA, Lucas JM, Bowman TG. Differences in the mechanism of head impacts measured between men’s and women's intercollegiate lacrosse athletes. Orthop J Sports Med. 2018;6(11):2325967118807678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lincoln AE, Hinton RY, Almquist JL, Lager SL, Dick RW. Head, face, and eye injuries in scholastic and collegiate lacrosse: a 4-year prospective study. Am J Sports Med. 2007;35(2):207-215. [DOI] [PubMed] [Google Scholar]
- 18. Loftin MC, Zynda AJ, Pollard-McGrandy A, Eke R, Covassin T, Wallace J. Racial differences in concussion diagnosis and mechanism of injury among adults presenting to emergency departments across the United States. Brain Inj. 2023;37(12-14):1326-1333. [DOI] [PubMed] [Google Scholar]
- 19. Pirruccio K, Parisien RL, Kelly JD. Sports-related concussions in high school females: an epidemiologic analysis of twenty-year national trends. Res Sports Med. 2021;29(6):526-535. [DOI] [PubMed] [Google Scholar]
- 20. Sabbagh RS, Shah NS, Kanhere AP, Hoge CG, Thomson CG, Grawe BM. Effect of the COVID-19 pandemic on sports-related injuries evaluated in US emergency departments. Orthop J Sports Med. 2022;10(2):23259671221075373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shepherd HA, Evans T, Gupta S, et al. The impact of COVID-19 on high school student-athlete experiences with physical activity, mental health, and social connection. Int J Environ Res Public Health. 2021;18(7):3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vincent HK, Zdziarski LA, Vincent KR. Review of lacrosse-related musculoskeletal injuries in high school and collegiate players. Sports Health. 2015;7(5):448-451. [DOI] [PMC free article] [PubMed] [Google Scholar]


