Abstract
Background:
The COVID-19 pandemic alongside increased patient demand, enablement of scope, and government funding has accelerated the need and demand for pharmacist prescribing in Nova Scotia.
Methods:
A sequential explanatory mixed-methods study was undertaken to understand barriers and facilitators to pharmacist prescribing in Nova Scotia, Canada. This consisted of: 1) a cross-sectional survey and 2) semistructured, qualitative interviews with pharmacists practising in the community. The survey and interviews were designed using the Behaviour Change Wheel that encompasses the Capability Opportunity Motivation Model of Behaviour Change (COM-B) and Theoretical Domains Framework version 2 (TDFv2).
Results:
Of 190 survey respondents, the percentage who prescribed 15+ times/month increased from 49% before to 80% during the COVID-19 pandemic (P<0.001). Pharmacists identified knowledge, social norms/pressures, and rewards or consequences related to how and when to prescribe as facilitators (Knowledge, Social Influences, and Motivation TDFv2 domains, respectively). Barriers included the environmental context and fear of negative outcomes (Environmental Context and Resources and Beliefs about Consequences, respectively). Through the interviews, the presence of prescribing decision tools (Memory, Attention and Decision Processes) and a supportive organizational culture (Environmental Context and Resources) were facilitators. Worry was expressed about making mistakes (Beliefs about Consequences) and feeling significant pressure to meet patient demand (Social Influences) in a busy setting (Environmental Context and Resources).
Discussion:
Supports to better enable pharmacist prescribing are described, with key messages for pharmacists, pharmacy owners/managers, educators, advocacy bodies, regulators, and government identified.
Conclusion:
Pharmacist prescribing has increased significantly over a short period of time. Environmental supports (e.g., time, space, access to patient records), government funding, peer support, and public awareness are needed to optimize and fully implement these practice changes.
Knowledge into Practice.
Pharmacist prescribing positively impacts patients, including increasing access to care and improving medication adherence.
Enablers of prescribing include motivation to help patients, decision aids, supportive organizational cultures, and further integration of pharmacists into the health care system.
Significant barriers to pharmacist prescribing remain, including lack of time, unrealistic public expectations, fear of negative consequences, and difficulty or inability to access patient records.
Key areas of support for pharmacists, pharmacy owners/managers, educators, advocacy bodies, regulators, and government have been identified using behaviour change theory.
Introduction
Pharmacist prescribing has positive effects on patients and the health care system, including increased access to health care, more appropriate referrals, better medication adherence and cost savings.1-8 As health care providers with medication expertise, pharmacists are best positioned within the health care system to assess and prescribe for medication treatment. Although pharmacists have had the authority to prescribe for many conditions in Nova Scotia since 2011 (Table 1), previous research has shown that pharmacist uptake of prescribing has historically been less than anticipated. 9
Table 1.
Pharmacist prescribing categories with definitions in Nova Scotia as of December 2022 10
| Pharmacist prescribing categories | Definitions |
|---|---|
| Approved conditions | Prescribing for common ailments from an approved list of conditions, when a diagnosis is provided by a primary care provider or specialist, or a diagnosis supported by a protocol. |
| Prescribing in emergency | Prescribing when a patient has an immediate, urgent and high-risk medical requirement for medication. |
| Prescribing renewals | Prescribing to continue a current medication with a new prescription. The new prescription as written may include refills, but when a patient is dispensed a refill, it is not counted as a prescribing service. |
| Prescribing adaptions | Prescribing to modify the dose, formulation, regimen and/or duration of therapy when a diagnosis is known and an intended treatment requires modification for dispensing either related to medication supply issues or specific patient factors. |
| Prescribing therapeutic substitutions | Prescribing to substitute with a therapeutically equivalent medication due to medication supply issues or specific patient factors. |
| Prescribing drugs that do not require a prescription* | Prescribing any drugs that do not require a prescription as a condition of sale. This includes medications that may require pharmacist assessment prior to sale (Schedule II) or may be available for self-selection in the pharmacy (Schedule III). |
Health Canada determines whether a drug is prescription or nonprescription; Schedule II and III refer to nonprescription designations assigned by the National Association of Pharmacy Regulatory Authorities (NAPRA). 11
The COVID-19 pandemic rapidly accelerated change in the practice of pharmacy, with increased demand and use of pharmacies by the public to receive primary care, including vaccinations and increased enablement of full scope by pharmacy regulatory authorities.12-20
In Nova Scotia, the health care system has also increasingly recognized the role of pharmacists in the delivery of primary care. This has included public funding for pharmacist-led care and significant innovation in the pharmacy practice environment, including the recent opening of pharmacy primary care and walk-in clinics throughout the province.21,22 Given the pace and scale of pharmacist prescribing, there is a need for updated evidence on the uptake of prescribing and the pharmacist experience in this evolving practice environment.
The frequency of prescribing is known to be affected by a number of barriers, including limited training and lack of time in the pharmacy environment. 23 Conversely, patient care and increased job satisfaction have been identified as facilitators. 24 By using behaviour change theory to identify facilitators and barriers, targeted interventions and policies can then be developed to support pharmacist prescribing practices.25-27
Mise En Pratique Des Connaissances.
La prescription par les pharmaciens a un impact positif sur les patients, y compris en améliorant l’accès aux soins et l’observance thérapeutique.
Les facteurs habilitants de la prescription comprennent la motivation à aider les patients, les aides à la décision, les cultures organisationnelles favorables et l’intégration accrue des pharmaciens dans le système de soins de santé.
Les obstacles importants à la prescription par les pharmaciens demeurent, entre autres, le manque de temps, les attentes irréalistes du public, la crainte de conséquences négatives et la difficulté ou l’incapacité d’accéder aux dossiers des patients.
La théorie du changement de comportement a permis d’identifier les principaux domaines de soutien pour les pharmaciens, les propriétaires et gérants de pharmacies, les éducateurs, les organismes de défense des droits, les organismes de réglementation et le gouvernement.
This project aims to first describe barriers and facilitators to pharmacist prescribing and their impact on self-reported prescribing activity and then to identify potential behavioural change interventions based on the identified barriers and facilitators.
Methods
This sequential explanatory mixed-methods study took place in Nova Scotia and consisted of 2 components: (1) a cross-sectional survey of pharmacists practising in the community and (2) semistructured, qualitative interviews with pharmacists practising in the community.
Ethics approval was received from the Dalhousie Health Sciences Research Ethics Board, REB#2020-5083, on April 7, 2020. An amendment to support the qualitative interviews was approved on July 22, 2021. Renewals were approved annually.
Behaviour change theory
The cross-sectional survey and interviews were designed using the Behaviour Change Wheel that encompasses both the Capability Opportunity Motivation Model of Behaviour Change (COM-B) and Theoretical Domains Framework version 2 (TDFv2).27,28 The COM-B model consists of 3 constructs that are the antecedents of behaviour: Capability (C), Opportunity (O) and Motivation (M). The TDFv2 integrates 33 behaviour change theories and consists of 14 domains that map to Capability, Opportunity and Motivation. See Table 2 for the 14 domains of the TDFv2 with interpretations used in this study and corresponding COM-B constructs.
Table 2.
| COM-B | TDF domain (no. of survey questions per domain) | Interpretation for this study | |
|---|---|---|---|
| Capability | Psychological | Knowledge (2) | Knowledge of how and when to prescribe |
| Skills (9) | Skills and ability to prescribe attained through practice | ||
| Memory, Attention, Decision Processes (3) | Remembering information and making decisions related to prescribing | ||
| Behavioural Regulation (5) | Supports for changing prescribing behaviour Anything aimed at changing prescribing behaviours |
||
| Physical | Skills (repeat) | Skills and ability to prescribe attained through practice | |
| Opportunity | Social | Social Influences (4) | Social pressure or norms affecting prescribing |
| Physical | Environmental Context and Resources (9) | Influences in the environment that affect prescribing | |
| Motivation | Reflective | Social/Professional Role and Identity (3) | Seeing prescribing as part of pharmacist’s role |
| Beliefs about Capabilities (2) | Acceptance of ability to prescribe | ||
| Optimism (2) | Confidence that prescribing will lead to good outcomes | ||
| Beliefs about Consequences (13) | Beliefs about consequences of prescribing | ||
| Intentions (9) | Intentions to prescribe | ||
| Goals (2) | Aims of engaging in prescribing | ||
| Automatic | Social/Professional Role and Identity (repeat) | Seeing prescribing as part of pharmacist’s role | |
| Optimism (repeat) | Confidence that prescribing will lead to good outcomes | ||
| Reinforcement (4) | Rewards or incentives related to prescribing | ||
| Emotion (5) | Feelings associated with prescribing | ||
COM-B, Capability Opportunity Motivation Model of Behaviour Change; TDFv2, Theoretical Domains Framework version 2.
Cross-sectional survey: Questionnaire development and data collection
The cross-sectional survey, previously published, 9 used a mixed-methods design, collecting and analyzing both closed- and open-ended data. The questionnaire asked pharmacists about their prescribing activities, how often they were prescribing before and during the COVID-19 pandemic, perceptions of their prescribing role, perceptions of barriers and facilitators to prescribing using the TDFv2, 27 demographic information and a series of open-ended questions that allowed participants to provide additional comments about barriers to prescribing. Using 5-point Likert items, participants were asked the degree to which they agreed with a number of statements about their prescribing behaviour using the TDFv2. The questionnaire was e-mailed to 1338 licensed direct patient care pharmacists in Nova Scotia in July 2020.
Data analysis
Quantitative analysis
Likert-item responses were grouped into positive (agree, strongly agree), neutral or negative (strongly disagree, disagree). The number of positive and negative responses was summed across the survey questions and across respondents within each TDFv2 domain (see Table 2 for definitions and the number of questions per domain). More positive responses were indicative of facilitators, and more negative responses indicated a barrier to pharmacist prescribing. Each TDFv2 domain contained a variable number of questions based on the range of relevant topics identified that fell into each domain. All domains demonstrated acceptable reliability. Given this variability, the percentage of responses (which is equivalent to the percentage of respondents) within each domain was calculated to enable comparability across domains.
Definitions of high- and low-frequency prescribers were developed based on how often pharmacists reported prescribing across multiple categories. Low-frequency prescribers were defined as those who reported prescribing anywhere between 0 and 14 times per month, while high-frequency prescribers were those who reported prescribing 15 or more times per month. Differences in prescribing pre–COVID-19 versus during COVID-19 were compared using Wilcoxon signed-rank tests or McNemar’s tests, as appropriate. The relationship between prescribing behaviour using the TDFv2 domains and prescribing frequency (high- versus low-frequency prescribers) was examined using simple logistic regression. This analysis indicated how much more (if the odds ratio was greater than 1) or less (if the odds ratio was less than 1) likely an individual was to be a high- (versus low-) frequency prescriber based on their score on each TDFv2 domain.
Qualitative analysis
Responses to the 3 open-ended questions were analyzed with deductive content analysis using the 14 domains of the TDFv2 as the coding framework. 29 Four research team members (A.B., J.E.I., J.K., N.K.K.) comprised the qualitative analysis team. An agreed-upon codebook was developed prior to coding. Two team members (A.B., N.K.K.) independently coded the 3 open-ended questions, which were then reviewed by the 2 other team members. Discrepancies were resolved by group consensus. Inductive content analysis was then completed by 1 team member (J.K.) to identify themes within each of the domains using NVivo 12 qualitative software to organize and classify the data. 30 The full qualitative analysis team reviewed and agreed upon the themes. The analysis was then presented to the full research team for discussion and final interpretation.
Qualitative interviews
Recruitment
Maximum variation purposive sampling was used to recruit a cross section of prescribers across self-reported prescribing frequency (from infrequent to very frequent, see Figure 1). These interviews were designed to build off themes identified through the survey and to better understand the contextual factors that enable or hinder pharmacist prescribing. Recruitment was conducted through research team members and Facebook posts to a Nova Scotia community pharmacist group. Potential participants were instructed to contact the research manager directly to maintain the anonymity of participants.
Figure 1.
How would you characterize your activity as a prescriber?
Interview guide development
A semistructured interview guide was developed using the results of the cross-sectional survey. Areas covered included demographics (e.g., gender, years in practice), role (e.g., staff pharmacist, manager), pharmacy practice setting, characterization of prescribing activity, view and approach to prescribing, opportunities to prescribe in practice, how the decision to prescribe is made and supports and barriers to prescribing.
Interviews
One-on-one virtual interviews were completed by an experienced qualitative methods research assistant between September 2021 and January 2023 using Zoom video conferencing (Zoom Video Communications, Inc.). Interviews lasted between 20 and 40 minutes.
Data analysis
Interviews were recorded and transcribed verbatim using the speech-to-text dictation function on Microsoft Word (Microsoft Corporation) with identifying information removed. Transcribed interviews were uploaded into NVivo 12 30 and coded independently by 2 team members (A.B., N.K.K.), with consensus reached with a third team member (J.E.I.) when needed. The first round of coding was completed deductively using the 14 domains of the TDFv2 (Table 2). The TDFv2-coded data were categorized into the COM-B, and comparisons were made between interviewees and cross-sectional study results.
Results
Cross-sectional survey
Prescribing frequency
The complete results were previously published. 31 Briefly, 190 pharmacists participated, which represented 14.2% of the pharmacists licensed to practice in the community at the time the survey was completed. The demographics of those who responded were similar to Canadian Institute for Health Information workforce data for community pharmacists in Nova Scotia at the time. 32 Respondents were on average 46 years old, practising for an average of 20 years, with 51% of respondents identifying as female, and 37% working in a rural area.
Most pharmacists (98%) reported prescribing at least once per month, which was an increase from 77% in the 2014 survey. 9 In addition, pharmacists who prescribed 15+ times/month increased from 49% before to 80% after the COVID-19 pandemic began (P<0.001) (see Figure 2). Renewals (extension of a medication previously prescribed by another health care provider) were the most common prescribing activity, followed by diagnoses supported by protocol (e.g., shingles) and common ailments (e.g., allergic rhinitis, warts). During COVID-19, there was an increase in prescribing for common ailments, preventative medicine (e.g., contraception, vaccines), diagnosis supported by protocol and renewals (all P<0.05). There was a decrease in prescribing for emergencies compared with pre-COVID (P<0.01).
Figure 2.
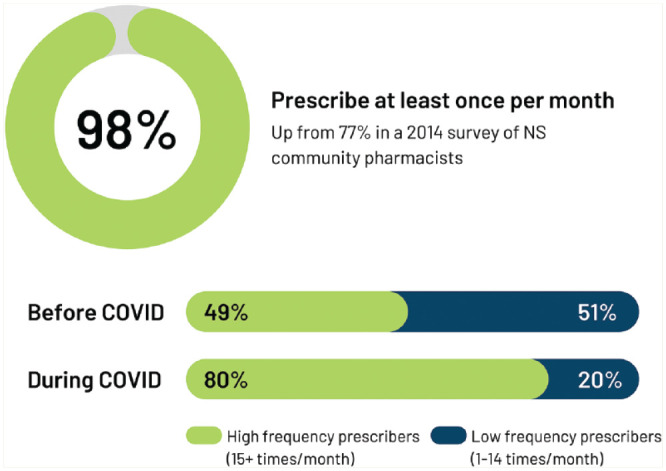
Frequency of pharmacist prescribing compared to 2014 survey, before and during COVID-19
The TDFv2 domains that had the highest percentage of positive responses (i.e., facilitators) and the highest percentage of negative responses (i.e., barriers) within each COM-B domain are summarized in Table 3. Within the Capability construct, positivity was highest for knowledge of how and when to prescribe (TDFv2 domain Knowledge; 85% of responses on this question were positive); within Opportunity, positivity was highest for social norms or pressures about when to prescribe (TDFv2 domain Social Influences, 73%); and within Motivation, positivity was highest for rewards or consequences related to prescribing (TDFv2 domain Reinforcement, 83%).
Table 3.
Barriers and facilitators to prescribing as identified in the cross-sectional survey of Nova Scotia pharmacists
| Likert-item responses | Open-ended responses | ||
|---|---|---|---|
| COM-B domain, TDFv2 domain | Top facilitators (most positive) | Top barriers (most negative) | Illustrative quotes |
| Number of responses (%)* | |||
| Capability | |||
| Knowledge | 321 (84.47) | “We were given very little notice . . . to do additional prescribing services (contraceptives, UTI, shingles) and were never offered any additional training . . . .” | |
| Behavioural Regulation | 248 (26.11) | “Crystal-clear training protocols, educational materials, CE [continuing education] events, etc., should have been put in place . . . .” | |
| Opportunity | |||
| Social Influences | 555 (73.03) | “. . . the media was blasted with ads that we could now provide these services; however, many patients did not meet the criteria or they did not want to make appointments . . . .” | |
| Environmental Context and Resources | 475 (27.78) | “. . . while we may be the most accessible health care professionals, we are probably LEAST on the amount of one-to-one time we can afford patients due to time constraints imposed by staffing . . . .” | |
| Motivation | |||
| Reinforcement | 631 (83.03) | “Lack of pharmacist reimbursement—that is the greatest barrier.” | |
| Beliefs about Consequences | 801 (32.43) | “I haven’t felt comfortable with prescribing in certain situations because I couldn’t access a patient’s lab values.” | |
The number of domains contained more than 1 question, and the number of questions varied between domains—thus, the number of responses is not directly reflective of the most positive or negative domain. COM-B, Capability Opportunity Motivation Model of Behaviour Change; TDFv2, Theoretical Domains Framework version 2; UTI, urinary tract infection. See Table 2 for TDFv2 and COM-B domain definitions.
In terms of barriers, within Capability, supports for changing prescribing behaviour was the top barrier (TDFv2 domain Behavioural Regulation, 26%). Within Opportunity, Environmental Context and Resources (28%) had the most negative responses identified. Lastly, within Motivation, potential negative consequences, such as being responsible for patient outcomes and the time it takes to prescribe (TDFv2 domain Beliefs about Consequences, 32%), was most negative.
Example quotes included in Table 3, solicited through open-ended survey responses, provide context around a pharmacist’s experience for each domain. All responses were coded as barriers to prescribing. Pharmacists most often cited issues around lack of staff and challenges integrating prescribing into overloaded workflows (Environmental Context and Resources), lack of appropriate reimbursement for both pharmacist and the pharmacies (Reinforcement) and discomfort asking patients to pay for prescribing services not covered by government funding (Social Influences).
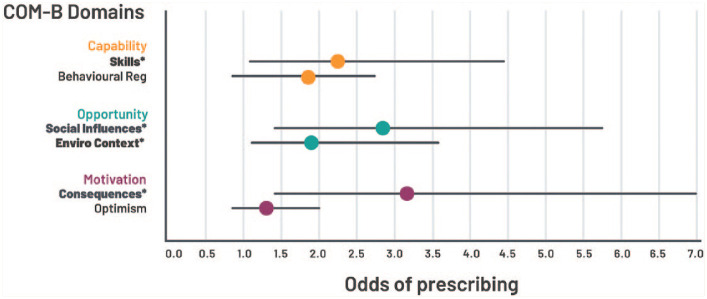
Prescribing behaviour
The TDFv2 domains with the most influence within each COM-B construct are presented in Figure 3. TDFv2 domains within the Opportunity and Motivation domains had the strongest relationship with prescribing frequency. For example, within the Motivation domain, increased positivity within Beliefs about Consequences (e.g., perceived positive benefits for patients) was related to higher odds of being classified as a high-frequency prescriber compared with a low-frequency prescriber (odds ratio [OR]=3.13, 95% confidence interval [CI] 1.41–6.97, P<0.01). This means that a 1-point increase in the TDFv2 score (e.g., an increase from agree [+1] to strongly agree [+2]) is related to 3.13 times higher odds of being classified as a high-frequency prescriber. Social Influences (e.g., having peers and colleagues supportive of prescribing) had the highest odds (OR=2.85, 95% CI 1.42–5.70, P<0.01) compared with other TDFv2 domains within the Opportunity domain of identifying high-frequency prescribers. Lastly, within Capability, Skills had a significant influence on prescribing activity (OR=2.32, 95% CI 1.19–4.49, P=0.01).
Figure 3.
Predictors of pharmacist prescribing activity based on positivity of response by TDFv2 and COM-B domains
*P<0.05. Simple logistic regression analyses results. Theoretical Domains Framework version 2 (TDFv2) within the Capability Opportunity Motivation Model of Behaviour Change (COM-B). TDFv2 abbreviations used in the figure: Consequences = Beliefs about Consequences; Enviro Context = Environmental Context and Resources; Behavioural Reg = Behavioural Regulation.
See the previously published full study for more details on these results. 31
Semistructured interviews
Five pharmacists practising in the community completed one-on-one interviews focused on their prescribing frequency, patterns and describing their pharmacy practice environment. See Table 4 for the demographics of the interview participants. Two pharmacists identified themselves as “active prescribers”, 1 as a “moderate prescriber”, and 2 as “infrequent prescribers”. All pharmacists described their practice location as being fairly busy, processing roughly 1500 prescriptions a week.
Table 4.
Demographic characteristics of interview participants
| n | |
|---|---|
| Pharmacy type | |
| Independent | 2 |
| Chain | 1 |
| Independent and chain | 1 |
| Grocery | 1 |
| Role | |
| Owner | 1 |
| Manager | 2 |
| Staff pharmacist | 2 |
| Location | |
| Urban | 2 |
| Rural | 2 |
| Both | 1 |
| Self-identified gender | |
| Woman | 4 |
| Man | 1 |
| Years in practice | |
| 0–5 | 1 |
| 5–10 | 1 |
| 10+ | 3 |
The qualitative interviews provided further explanation and evidence for the facilitators and barriers identified through the survey, with a significant number being associated with the TDFv2 domains of Memory, Attention and Decision Processes; Environmental Context and Resources; Social Influences; and Beliefs about Consequences. More specifically, the presence of prescribing decision tools (Memory, Attention and Decision Processes) and a supportive organizational culture (Environmental Context and Resources) were facilitators. However, pharmacists worried about making mistakes (Beliefs about Consequences) while also feeling significant pressure in the pharmacy environment to meet patient demand (Social Influences) in a very busy setting (Environmental Context and Resources).
A description of these domains and illustrative quotes are provided in Table 5.
Table 5.
Summary of facilitators and barriers identified in qualitative interviews organized by COM-B constructs and TDFv227,28
| COM-B | TDFv2 domain | Key findings | Facilitator illustrative quote | Barrier illustrative quote |
|---|---|---|---|---|
| Capability | Memory, Attention and Decision Processes | • Presence of prescribing decision algorithms and tools • Documentation requirements |
“Our organization has developed . . . some other tools for different conditions like skin conditions . . . where we have an assessment to go through; those tools are really helpful because you only have to look in 1 place to be able to ensure you're doing a full appropriate assessment going on the fly.” (#1 active prescriber) | “. . . I know I could do a better job at my documentation, but I just don't have the time to do that.” (#3 moderate prescriber) |
| Opportunity | Environmental Context and Resources | • Organizational culture • Time constraints |
“. . . support from ownership. We’ve had significant conversations from the ownership level and my boss is saying ‘hey, this is the future of pharmacy, this is what we have to be. What do you need from us to make this successful in your [pharmacy]?’” (#1 active prescriber) | “There is no free time in pharmacy when I'm staying late on my shifts to walk through these clinical scenarios with other pharmacists. I’m taking calls and talking to them on my off time and . . . I can see myself getting burnt out. Absolutely, I already have felt burnt out . . . .” (#2 active prescriber) |
| Social Influences | • Patient awareness/demand for services | “Renewals have kind of blown up, so that’s probably the most common thing. You can spend a morning, like a 9 to 1 shift, and do 2 or 3 renewals an hour no problem. . . . But then we also have a lot of people who are aware that we’re able to potentially prescribe for UTIs and for cold sores. . . . So minor ailments, some of them more so than others, but also birth control, have taken off in that area.” (#1 active prescriber) | “We have an issue in our profession with a culture of hyperaccessibility . . . we’re the only health care provider that provides absolutely free personalized medical advice at no cost. As soon as someone comes to the counter, at the drop of a hat, we rush over.” (#2 active prescriber) | |
| Motivation | Beliefs about Consequences | • Making a difference in patients’ lives and supporting other sectors in current health care crisis • Inability to access full patient records |
“If there are things that you can do to try to help the health care situation right now and the crisis that we’re in and take some of the workload off of the [emergency rooms] . . . I think that’s something that would be a positive . . . and would push you to want to help . . . .” (#5 infrequent prescriber) | “. . . some of the hesitancy is that I don’t have enough confidence in my skills or I worry . . . what I’m going to do is going to be the wrong thing . . . if I go into someone’s . . . [secure health access record] and look at their lab values and they haven’t had any blood work done in . . . 4 years then that kind of makes me anxious to prescribe.” (#5 infrequent prescriber) |
COM-B, Capability Opportunity Motivation Model of Behaviour Change; TDFv2, Theoretical Domains Framework version 2; UTI, urinary tract infection.
Discussion
This study explored pharmacist prescribing in Nova Scotia. Our findings showed an increase in self-reported prescribing frequency compared with a 2014 study and since the start of the COVID-19 pandemic. Almost all pharmacists reported prescribing at least once a month, up 21% since 2014. Moreover, almost 80% were prescribing more than 15 times a month, compared with only 23% of the respondents in 2014. This increase in frequency was likely partially driven by COVID-19, as prescribing for common ailments, preventative medicine and renewals was reported to increase after COVID-19 began. Initiation of government funding for prescribing for certain conditions in early 2020 (uncomplicated cystitis, shingles, contraception management and renewals) may also have driven some of the COVID-19–related increase in prescribing. This was likely also coupled with challenges in accessing other forms of primary care, such as family physicians, during the early stages of the pandemic. 33
Through the survey responses, we were able to identify facilitators and barriers to prescribing, which were further contextualized through the interviews. For example, pharmacists identified challenges related to Opportunity (within the COM-B), specifically referring to the pharmacy environment in the survey, and in the interviews identified that a supportive organizational culture was a facilitator, although the busy pharmacy setting is a barrier (Environmental Context and Resources). There was overlap in other results, with pharmacists expressing a fear of making mistakes (Beliefs about Consequences) through both data collection methods, which falls within the construct of Motivation. We also examined how these facilitators and barriers were related to prescribing behaviour (i.e., frequency in the current study). Through this analysis, we found further support of the impact of Beliefs about Consequences, Social Influences and Environmental Context and Resources as influencing the frequency of prescribing. Broadly, this reflects the particular importance of Motivation and Opportunity rather than Capability (e.g., Knowledge) (within the COM-B) in the pharmacy practice environment. These key areas identify important targets for interventions to support pharmacists, which are further described below.
Within Capability, respondents had positive perceptions of their Knowledge, but this was not found to be as important a predictor of prescribing as others (e.g., Skills). This may reflect that current education and training have been sufficient to support uptake of pharmacist prescribing or that education and training are not primary drivers of prescribing behaviour. This is further corroborated by Skills being identified as a key facilitator of prescribing. As pharmacists continue to practise to full scope, greater opportunities to prescribe have arisen, which may increase confidence and self-efficacy. Further support could be provided through the creation of additional decision aids and algorithms to increase confidence and self-efficacy (Behavioural Regulation) and to serve as environmental supports to prescribing (Memory, Attention and Decision Processes).
Focusing on Opportunity, patient demand for prescribing (Social Influences) is a driver but also a barrier to prescribing. Both the survey and interview findings identified time constraints in practice (Environmental Context and Resources) as a major barrier to prescribing. Interventional supports could be put in place related to environmental restructuring. This could include ensuring there is a separate clinical space available for prescribing, and time available for pharmacists to switch from dispensing to assessment may further enable this practice. In addition, restricting access through appointment-based care may be necessary to improve both pharmacist willingness to prescribe and also time to prescribe confidently. To enable these supports, adequate staffing and a shift in patient expectations regarding the accessibility and speed of care are needed. Interview participants who were active prescribers also cited that organizational culture and support were key facilitators to pharmacist prescribing.
When looking at Motivation, individuals who are more hesitant to prescribe, or who have less practice, may benefit from modelling by peers to build confidence and overcome fears associated with the negative outcomes of prescribing (Beliefs about Consequences). Enablement by pharmacy managers and by peers, through communities of practice or mentorship programs, may also help to further support prescribing. Also, access to complete patient records and processes to ensure access to patient history in pharmacy practice management systems may help to reduce hesitation in the prescribing process. Reinforcement of behaviour through additional financial incentives to practitioners for engaging in prescribing may also improve uptake. Changes in prescribing patterns identified in this study were likely influenced by expanding reimbursement for specific prescribing categories.
Supporting behaviour change in prescribing requires a multipronged approach—considering how different strategies (e.g., provision of an online appointment system alongside a communication campaign to shift patient mindset in speed of accessing care) might target multiple barriers and facilitators to enable change. By identifying these strategies, the goal is not to add more to a pharmacist’s plate but rather to shift how care is supported by the system (e.g., funding, organizational changes) and the public.
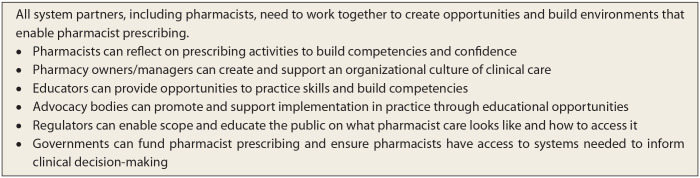
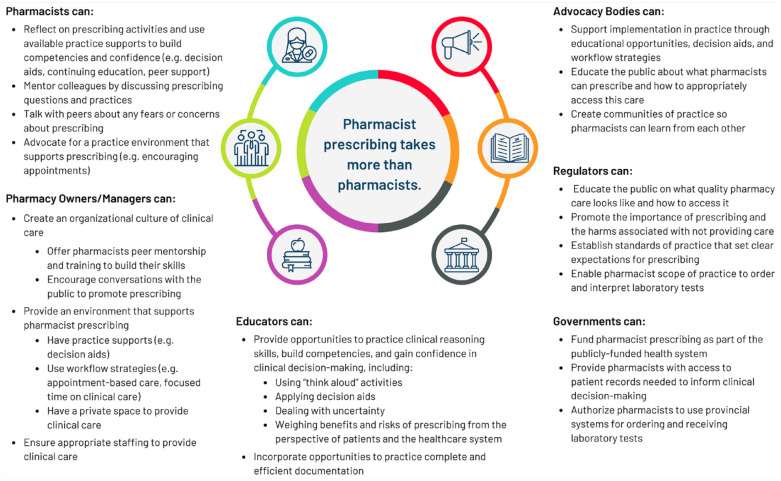
An overall summary of what health system partners, including pharmacists, need to change is shown in Figure 4. Proposed strategies for change, based on the COM-B, are broken down by key partner groups in Figure 5.
Figure 4.
What needs to change
Figure 5.
Ways to support pharmacist prescribing
Limitations
The survey was conducted in July 2020, followed by interviews in late 2021 to early 2023. Given that the interviews took place after the survey, the difference in identified barriers may reflect mounting pressures in the pharmacy environment. Although the results of this study should be considered transferrable to the current practice environment in Nova Scotia, they should be interpreted with some degree of caution, as changes in the pharmacy practice environment continue given increasing primary care access issues in the province over this period. However, the consistency between survey and interview findings is encouraging. Finally, this study focused on pharmacist prescribing in 1 province and may not be generalizable to pharmacist prescribing experiences in other provinces or territories. Nonetheless, it highlights important interventions grounded in behaviour change theory that may be necessary to improve the uptake and sustainability of pharmacist prescribing across jurisdictions.
Conclusions
This research provides valuable insights and proposes interventions crucial for enhancing pharmacist prescribing practices. This study found an increase in pharmacist prescribing compared to a 2014 study and from pre-COVID to during the COVID-19 pandemic. Using the COM-B and TDFv2 frameworks, the study identified Beliefs about Consequences, Social Influences and Environmental Context as pivotal factors influencing prescribing frequency, highlighting Motivation and Opportunity as critical drivers in the pharmacy environment. Potential strategies have been proposed to further enhance facilitators and mitigate barriers that influence pharmacist prescribing. ■
Acknowledgments
We would like to thank the other members of the Pharmacist Prescribing Survey Team who contributed to the conception, analysis and interpretation of our previously published study, of which some of the data contributed to and informed the current article. Thanks to Judith Fisher, Julia Kontak, Elizabeth Jeffers, Laura V. Minard, Bobbi Morrison, Juanna Ricketts, Glenn Rodrigues, Liam Rowe, Ingrid Sketris, Sam Stewart, Anne Marie Whelan and Lisa Woodill. Special thanks also to Alice Bruce and Julia Kontak for supporting the collection and/or analysis of qualitative interview data and to Rachel Giacomantonio for supporting graphic development and knowledge translation.
Footnotes
Author Contributions: All authors were involved in identifying the research questions and study methodology and contributed to the initial draft of the manuscript. A. Grant carried out the survey data analysis. A. Bishop, N. Kennie-Kaulbach and J. Isenor carried out the qualitative data analysis. All authors reviewed and approved the final draft of the manuscript.
The team has no declarations or conflicts of interest to declare in relation to this project.
Funding: The Maritime SPOR SUPPORT Unit (MSSU) receives financial support from the Canadian Institutes of Health Research (CIHR), the New Brunswick Department of Health, the Nova Scotia Department of Health and Wellness, the Prince Edward Island Department of Health and Wellness and Research. The opinions, results and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by the MSSU or the named funding partners is intended or should be inferred.
ORCID iD: Jennifer E. Isenor  https://orcid.org/0000-0003-1648-7362
https://orcid.org/0000-0003-1648-7362
Contributor Information
Amy Grant, Maritime SPOR SUPPORT Unit (MSSU), Halifax, Nova Scotia.
Natalie Kennie-Kaulbach, College of Pharmacy, Dalhousie University, Halifax, Nova Scotia.
Andrea Bishop, Nova Scotia College of Pharmacists, Halifax, Nova Scotia.
Jennifer E. Isenor, College of Pharmacy, Dalhousie University, Halifax, Nova Scotia.
References
- 1. Beahm NP, Smyth DJ, Tsuyuki RT. Outcomes of Urinary Tract Infection Management by Pharmacists (R(x)OUTMAP): a study of pharmacist prescribing and care in patients with uncomplicated urinary tract infections in the community. Can Pharm J (Ott). 2018;151(5):305-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Famiyeh IM, McCarthy L. Pharmacist prescribing: a scoping review about the views and experiences of patients and the public. Res Social Adm Pharm. 2017;13(1):1-16. [DOI] [PubMed] [Google Scholar]
- 3. Mansell K, Bootsman N, Kuntz A, Taylor J. Evaluating pharmacist prescribing for minor ailments. Int J Pharm Pract. 2015;23(2):95-101. [DOI] [PubMed] [Google Scholar]
- 4. Dineen-Griffin S, Benrimoj SI, Rogers K, Williams KA, Garcia-Cardenas V. Cluster randomised controlled trial evaluating the clinical and humanistic impact of a pharmacist-led minor ailment service. BMJ Qual Saf. 2020;29(11):921-31. [DOI] [PubMed] [Google Scholar]
- 5. Dineen-Griffin S, Vargas C, Williams KA, Benrimoj SI, Garcia-Cardenas V. Cost utility of a pharmacist-led minor ailment service compared with usual pharmacist care. Cost Eff Resour Alloc. 2020;18:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Al Hamarneh YN, Johnston K, Marra CA, Tsuyuki RT. Pharmacist prescribing and care improves cardiovascular risk, but is it cost-effective? A cost-effectiveness analysis of the R(x)EACH study. Can Pharm J (Ott). 2019;152(4):257-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rafferty E, Yaghoubi M, Taylor J, Farag M. Costs and savings associated with a pharmacists prescribing for minor ailments program in Saskatchewan. Cost Eff Resour Alloc. 2017;15:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kim JJ, Tian AH, Pham L, Nakhla N, Houle SKD, Wong WWL, et al. Economic evaluation of pharmacists prescribing for minor ailments in Ontario, Canada: a cost-minimization analysis. Int J Pharm Pract. 2021;29(3):228-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Isenor JE, Minard LV, Stewart SA, et al. Identification of the relationship between barriers and facilitators of pharmacist prescribing and self-reported prescribing activity using the theoretical domains framework. Res Social Adm Pharm. 2018;14(8):784-91. [DOI] [PubMed] [Google Scholar]
- 10. Nova Scotia College of Pharmacists. Standards of practice: prescribing drugs 2019 [updated 2021; cited Sep. 29, 2021]. Available: https://www.nspharmacists.ca/wp-content/uploads/2016/05/SOP_PrescribingDrugs.pdf. [Google Scholar]
- 11. National Association of Pharmacy Regulatory Authorities. Available: https://www.napra.ca/ (accessed Feb. 14, 2024).
- 12. Elbeddini A, Botross A, Gerochi R, Gazarin M, Elshahawi A. Pharmacy response to COVID-19: lessons learnt from Canada. J Pharm Policy Pract. 2020;13(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Elbeddini A, Hooda N, Yang L. Role of Canadian pharmacists in managing drug shortage concerns amid the COVID-19 pandemic. Can Pharm J (Ott). 2020;153(4):198-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Elbeddini A, Prabaharan T, Almasalkhi S, Tran C. Pharmacists and COVID-19. J Pharm Policy Pract. 2020;13:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Elbeddini A, Yeats A. Pharmacist intervention amid the coronavirus disease 2019 (COVID-19) pandemic: from direct patient care to telemedicine. J Pharm Policy Pract. 2020;13:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Goff DA, Ashiru-Oredope D, Cairns KA, et al. Global contributions of pharmacists during the COVID-19 pandemic. J Am Coll Clin Pharm. 2020;3(8):1480-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hedima EW, Adeyemi MS, Ikunaiye NY. Community pharmacists: on the frontline of health service against COVID-19 in LMICs. Res Social Adm Pharm. 2021;17(1):1964-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Watson KE, Schindel TJ, Barsoum ME, Kung JY. COVID the catalyst for evolving professional role identity? A scoping review of global pharmacists’ roles and services as a response to the COVID-19 pandemic. Pharmacy (Basel). 2021;9(2):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Strand MA, Bratberg J, Eukel H, Hardy M, Williams C. Community pharmacists’ contributions to disease management during the COVID-19 pandemic. Prev Chronic Dis. 2020;17:E69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Parajuli DR, Khanal S, Wechkunanukul KH, Ghimire S, Poudel A. Pharmacy practice in emergency response during the COVID-19 pandemic: lessons from Australia. Res Social Adm Pharm. 2022;18(8):3453-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pharmacy Association of Nova Scotia. Community pharmacy primary care clinics. Available: https://pans.ns.ca/cppc (accessed Feb. 14, 2024).
- 22. Nova Scotia Health. Available: https://www.nshealth.ca/primary-care-your-local-pharmacy (accessed Feb. 14, 2024).
- 23. Hussein R, Whaley CRJ, Lin ECJ, Grindrod K. Identifying barriers, facilitators and behaviour change techniques to the adoption of the full scope of pharmacy practice among pharmacy professionals: using the Theoretical Domains Framework. Res Social Adm Pharm. 2021;17(8):1396-406. [DOI] [PubMed] [Google Scholar]
- 24. Makowsky MJ, Guirguis LM, Hughes CA, Sadowski CA, Yuksel N. Factors influencing pharmacists’ adoption of prescribing: qualitative application of the diffusion of innovations theory. Implement Sci. 2013;8:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Phillips CJ, Marshall AP, Chaves NJ, et al. Experiences of using the Theoretical Domains Framework across diverse clinical environments: a qualitative study. J Multidiscip Healthc. 2015;8:139-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. French SD, Green SE, O’Connor DA, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci. 2012;7:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-88. [DOI] [PubMed] [Google Scholar]
- 30. NVivo. 12 ed. QSR International Pty Ltd; 2018. [Google Scholar]
- 31. Grant A, Rowe L, Kennie-Kaulbach N, et al. Increased self-reported pharmacist prescribing during the COVID-19 pandemic: using the Theoretical Domains Framework to identify barriers and facilitators to prescribing. Res Social Adm Pharm. 2023;19(1):133-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Canadian Institute for Health Information. Health workforce in Canada, 2020 - quick stats Ottawa, ON, 2021. Available: https://www.cihi.ca/en/pharmacists (accessed Feb. 14, 2024). [Google Scholar]
- 33. Kiran T, Wu F, Latifovic L, Glazier R, Frymire E. Did the COVID-19 pandemic cause family physicians to stop practice? Results from Ontario, Canada. Ann Fam Med. 2022;20(suppl 1):3018. [DOI] [PMC free article] [PubMed] [Google Scholar]