Abstract
The Centers for Disease Control and Prevention’s (CDC’s) Global Rapid Response Team (GRRT) was created in 2015 to efficiently deploy multidisciplinary CDC experts outside the United States for public health emergencies. The COVID-19 pandemic dramatically increased the need for domestic public health responders. This study aimed to follow up on previously published data to describe the GRRT surge staffing model during the height of the COVID-19 response. We conducted descriptive analyses to assess GRRT deployment characteristics during April 1, 2019–March 31, 2022, and characteristics of responders rostered in 2021 and 2022. We analyzed data on response events, remote versus in-person work, and international versus domestic deployment location. We also examined the number of responders on call per month, language proficiency, and technical skills. During the study period, 1725 deployments were registered, accounting for 82 058 person-days deployed. Of all person-days deployed during the study period, 82% were related to COVID-19. Eighty-seven percent of all person-days deployed were domestic. Virtual deployments that were not in person accounted for 51% of deployments registered, yet these resulted in 67% of person-days deployed. The median deployment duration was 31 days. We found a median of 79 surge responders on call each month. Among 608 responders rostered in 2021 and 2022, 35% self-reported proficiency in a second language. Epidemiology was the most common technical skill (38%). GRRT transitioned to primarily remote, domestic deployments to support the COVID-19 pandemic response. The GRRT model demonstrates how response structure shifted to address the global health threat of a pandemic.
Keywords: emergency response, emergency preparedness, global health, pandemic, outbreak response
The Centers for Disease Control and Prevention’s (CDC’s) Global Rapid Response Team (GRRT) deploys public health professionals employed at CDC to respond to emergencies worldwide. GRRT was created after the 2014-2016 Ebola virus disease (EVD) epidemic in West Africa to support international deployments addressing public health emergencies. A previous review documented that 74% of GRRT person-days deployed occurred outside the United States from October 1, 2018, through March 31, 2019. 1 Although CDC’s Emergency Operations Center has served as a communications, decision-making, and operations hub since 2003, 2 before the 2014-2016 West Africa EVD epidemic, CDC had no large-scale systematic response framework that registered volunteers from across the agency who could mobilize quickly in the event of an emergency.
GRRT maintains an up-to-date roster of skilled CDC responders who can mobilize quickly for an emergency response. Team members include “core” and “surge” responders. Core responders are full-time deployable GRRT staff who spend most of their time deployed. Between deployments, GRRT core responders debrief the agency on deployments, design training for GRRT surge responders, and serve as mentors for future responders. Surge responders are CDC staff working across the agency and are registered for 2 years. Surge responders select 2 on-call months each year during which they volunteer to respond to emergencies when deployment needs surpass the personnel capacity of CDC subject matter experts. Participation is contingent upon meeting annual readiness requirements to deploy, such as having an official passport, medical clearance, security training, and periodic technical skill training. Training is conducted by and for GRRT and non-GRRT members and covers a range of topics such as laboratory safety and the epidemiology of epidemic-prone diseases.
Purpose
Our study assessed the GRRT surge staffing model through descriptive analysis of GRRT deployment and responder characteristics to inform future emergency preparedness efforts. A previous report on this topic covered the 6-month period of October 2018 through March 2019. 1 Our study period encompasses the 3-year period of April 1, 2019, through March 31, 2022. We chose a longer study period (3 years vs 6 months) so that we could include data captured during the height of the COVID-19 response.
Methods
We conducted 2 descriptive analyses. We obtained data from the GRRT operational database maintained in Microsoft SharePoint and used R Studio version 4.2.1 (RStudio Team) to analyze data. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy (eg, 45 CFR part 46.102[l][2], 21 CFR part 56; 42 USC §241[d]; 5 USC §552a; 44 USC §3501 et seq).
The first analysis assessed GRRT deployment characteristics. Deployments include travel to field sites or virtual roles supporting the Emergency Operations Center or field partners. Deployments must have been approved by the GRRT Surge Coordination unit after another entity had requested GRRT’s assistance in recruiting temporary responders to address a public health issue. Deployments may be classified as training, nonemergency technical support, capacity building, or emergency response; we evaluated only deployments associated with emergency responses. We reviewed the database for duplicates. We examined data in the following categories: emergency type (disease related, conflict related, or natural disaster related), event (COVID-19, EVD, poliomyelitis, or other), remote versus in-person deployment, international versus domestic deployment, World Health Organization region (Africa, Americas, Europe, South-East Asia, and Western Pacific), 3 and role (border health, epidemiology and science, health communications and policy, laboratory and clinical skills, logistics, management and operations, or other). We calculated the number of person-days deployed. A person-day is defined as 1 day spent working on a deployment, not including travel days for deployments that require travel. We compared the total number of deployments during the study period with the total number of deployments since GRRT was founded in 2015.
The second analysis assessed GRRT responder characteristics from cohorts registered in 2021 and 2022. These cohorts included core and surge responders regardless of whether they deployed for a response. We examined the number of responders on call per month and the language proficiency and technical skills of responders. Responders self-reported language proficiency and technical skills; these data were requested of all responders, but responses were not mandatory. Responders were asked to categorize their skill set into 1 of the 6 GRRT technical pillars: border health, epidemiology and science, management and operations, health communications and policy, laboratory and clinical skills, and logistics.
Outcomes
During April 1, 2019–March 31, 2022, 1725 deployments were registered, accounting for 74.8% of all GRRT deployments (2305 deployments) since GRRT was founded in 2015. The total number of person-days deployed was 82 058 (Table). The median deployment duration was 31 days (range, 3-644 days).
Table.
Characteristics of deployments, by person-days deployed, in the Centers for Disease Control and Prevention’s Global Rapid Response Team, April 1, 2019–March 31, 2022 a
| Characteristic | Overall | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|
| Overall | 82 058 (100.0) | 6493 (7.9) | 35 034 (42.7) | 34 338 (41.8) | 6193 (7.5) |
| Emergency type | |||||
| Disease related | 80 694 (97.6) | 6384 (98.3) | 35 034 (100.0) | 33 475 (97.5) | 5801 (93.7) |
| Conflict related | 977 (1.2) | 0 | 0 | 693 (2.0) | 284 (4.6) |
| Natural disaster related | 387 (0.5) | 109 (1.7) | 0 | 170 (0.5) | 108 (1.7) |
| Event | |||||
| COVID-19 | 66 602 (81.2) | 0 | 29 055 (82.9) | 32 075 (93.4) | 5472 (88.4) |
| Ebola virus disease | 11 473 (14.0) | 5491 (84.6) | 4941 (14.1) | 1041 (3.0) | 0 |
| Poliomyelitis | 2036 (2.5) | 653 (10.1) | 924 (2.6) | 158 (0.5) | 301 (4.9) |
| Other | 1947 (2.4) | 349 (5.4) | 114 (0.3) | 1064 (3.1) | 420 (6.8) |
| International person-days deployed | 10 928 (13.3) | 5134 (79.1) | 4009 (11.4) | 1181 (3.4) | 604 (9.8) |
| Remote deployments | 54 811 (66.8) | 1318 (20.3) | 21 802 (62.2) | 27 279 (79.4) | 4412 (71.2) |
| World Health Organization region | |||||
| Africa | 9182 (11.2) | 4492 (69.2) | 3270 (9.3) | 889 (2.6) | 531 (8.6) |
| Americas | 71 248 (86.8) | 1397 (21.5) | 31 025 (88.6) | 33 237 (96.8) | 5589 (90.2) |
| Europe | 1156 (1.4) | 548 (8.4) | 608 (1.7) | 0 | 0 |
| Southeast Asia | 57 (<0.1) | 0 | 25 (<0.1) | 32 (<0.1) | 0 |
| Western Pacific | 415 (0.5) | 56 (0.9) | 106 (0.3) | 180 (0.5) | 73 (1.2) |
| Role | |||||
| Border health | 2317 (2.8) | 72 (1.1) | 1546 (4.4) | 252 (0.7) | 447 (7.2) |
| Epidemiology and science | 35 724 (43.5) | 2774 (42.7) | 16 106 (46.0) | 13 844 (40.3) | 3000 (48.4) |
| Health communications and policy | 10 554 (12.9) | 380 (5.9) | 4379 (12.5) | 4929 (14.4) | 866 (14.0) |
| Laboratory and clinical skills | 6627 (8.1) | 427 (6.6) | 2683 (7.7) | 2973 (8.7) | 544 (8.8) |
| Logistics | 3163 (3.9) | 491 (7.6) | 1540 (4.4) | 1042 (3.0) | 90 (1.5) |
| Management and operations | 21 250 (25.9) | 2236 (34.4) | 8524 (24.3) | 9541 (27.8) | 949 (15.3) |
| Other | 2423 (3.0) | 113 (1.7) | 256 (0.7) | 1757 (5.1) | 297 (4.8) |
Data source: Centers for Disease Control and Prevention’s Global Rapid Response Team database. All values are number (percentage).
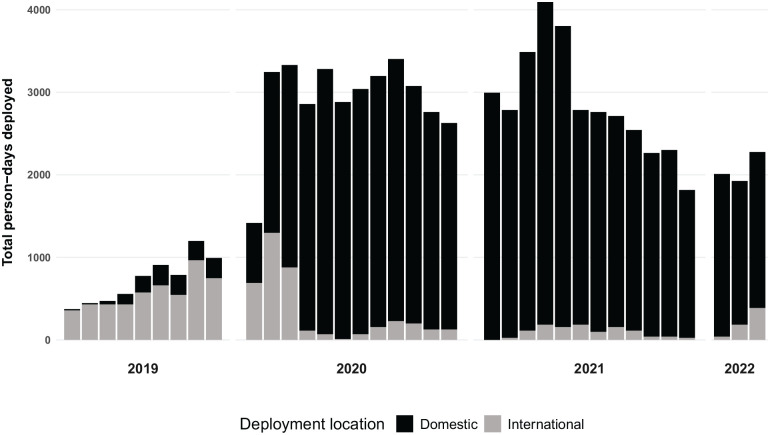
Deployments occurred across 5 World Health Organization regions; however, 86.7% of person-days deployed (71 130 person-days) were domestic. Thirteen percent of person-days deployed (10 928 person-days) were international (Figure 1). After the United States, Africa was the location for the next most person-days deployed (9182 person-days; 11.2%).
Figure 1.
Trends in deployment locations (domestic vs international) of the Global Rapid Response Team, Centers for Disease Control and Prevention, by month, April 1, 2019–March 31, 2022. Data source: Centers for Disease Control and Prevention’s Global Rapid Response Team database.
The number of deployments registered was approximately equally divided between in person (876 deployments; 50.8%) and remote (849 deployments; 49.2%). However, more person-days deployed (54 811 person-days; 66.8%) occurred remotely than in person (27 247 days; 33.2%). The median duration of remote deployments was 44 days, while the median duration of in-person deployments was 29 days. Of domestic person-days deployed, 76.5% (54 448 person-days) took place remotely. In contrast, of international person-days deployed, 96.7% (10 565 person-days) occurred in person.
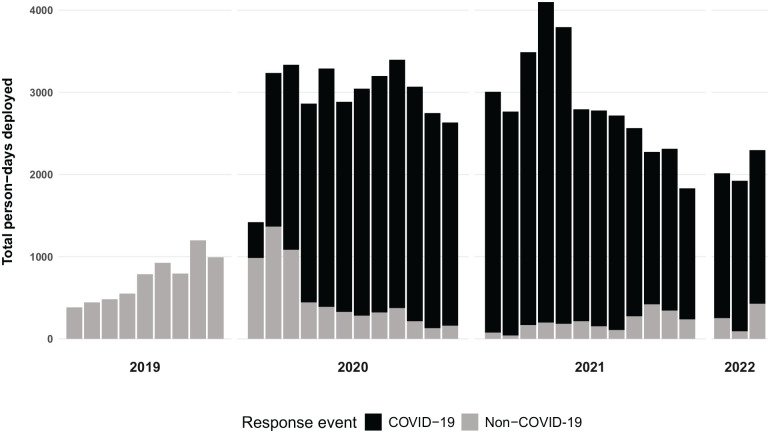
Eighty-two percent of person-days deployed (66 602 person-days) were associated with COVID-19 (Figure 2), 17.2% (14 092 person-days) were associated with other diseases, and 1.7% (1364 person-days) were associated with conflicts and natural disasters. After COVID-19, the next most common diseases addressed during deployments were EVD (11 473 person-days; 14.0%) and poliomyelitis (2036 person-days; 2.5%). Of 10 928 international person-days deployed, 65.7% (7176 person-days) were associated with EVD.
Figure 2.
Trends in deployment events (COVID-19 vs. non–COVID-19) of the Global Rapid Response Team, Centers for Disease Control and Prevention, by month, April 1, 2019–March 31, 2022. Data source: Centers for Disease Control and Prevention’s Global Rapid Response Team database.
Of the 608 responders in the 2021 and 2022 cohorts, 321 were surge responders in 2021, 240 were surge responders in 2022, and 47 were core responders. While these cohorts were active, a median of 79 (range, 71-88) surge responders were on call each month. Thirty-five percent (n = 215) of responders self-reported intermediate to advanced language skills in at least 1 of 6 languages (Spanish, French, Portuguese, Mandarin, Arabic, and Russian). Of the 608 responders, the most reported language proficiency was Spanish (n = 143; 23.5%) and the most reported technical skill was epidemiology (n = 232; 38.2%), followed by management and operations (n = 170; 28.0%). Fifteen percent of responders (n = 91) did not document self-reported technical skills in the system.
Lessons Learned
Despite fewer deployments during the final 3 months of our study in comparison with the first 3 months, the total number of GRRT deployments increased due to the COVID-19 response. Responders were needed for domestic and international deployments on an extraordinary scale. During the study period, 1725 deployments were registered, accounting for 75% of all GRRT deployments since GRRT was founded in 2015. Most of these deployments were domestic. GRRT was able to respond to CDC’s public health emergency needs because of its up-to-date roster of CDC employees with multidisciplinary skills and its adaptable data management tools. GRRT adjusted to the new virtual response environment by processing and managing remote deployments. During the study period, GRRT supported the CDC public health emergency response with skilled responders for more than 82 000 person-days.
Many deployments were remote. Telework was required for most CDC employees from late March 2020 through early 2022, including employees deployed to the COVID-19 response. This approach was entirely new for GRRT. Approximately half of the deployments registered during the study period were remote, and half were in person. However, the number of person-days deployed revealed that most time spent on deployments was remote. Remote work was associated with longer deployments. US Department of State medical clearance is required for in-person international travel scheduled for 29 days or more. This requirement could have been related to the lower median number of days deployed for in-person deployments than for remote deployments (29 vs 44) because most international deployments were in person.
The magnitude of domestic deployments—nearly 90%—is likely a reflection of several factors. First, emergency responders were needed domestically on a scale never seen before to address COVID-19. Second, all nonessential travel, especially nonessential international travel, was discouraged early in the pandemic. This factor likely led to a decrease in international deployments and led to much pandemic response work taking place virtually. Lastly, it is also likely that some countries where deployments might have otherwise taken place enforced restrictions on external staffing and international travel.
GRRT responders are well-positioned to protect the health of people in the United States. Operationally, GRRT readiness requirements ensure that responders are ready to deploy anywhere on short notice. Pivoting from international to domestic and remote deployments did not create additional challenges in coordinating deployment. The team continued to fulfill deployment requests and provide training.
The new response environment did lead to challenges in managing response metrics such as deployment location, remote versus in-person work, and response events. The ease with which responders could transition between responses in the virtual environment created some difficulties in tracking who was responding to which deployment at a given time. However, this challenge also led to improvements in the management system. For example, the system now tracks responders when they work remotely. The data system is now continuously updated to meet changing reporting requirements.
Our analysis was subject to several limitations. First, the database used for the analysis is dynamic. It was developed to capture operational data and is continuously updated to reflect deployment needs and responder availability. The data system was not originally designed to capture data on deployment characteristics such as remote work. Second, some self-reported data fields, such as technical skills, were not mandatory during the study period, which resulted in missing and incomplete data. The lack of mandatory reporting made the technical skills section easy to skip; adding to this problem, some responders were unclear on how to narrow down their skill set to 1 of the 6 GRRT pillars. Because of challenges in tracking the skills of responders, it was difficult to compare skills required for deployments with responder characteristics. Different sets of metrics were collected for responders and deployments, complicating any attempt to directly compare the two (eg, languages required for deployments were not captured in the operational database). Emergencies are often complex and involve overlaid response elements. Disease-related, natural disaster–related, and conflict-related emergencies are not mutually exclusive. Some response leadership roles encompass more than 1 emergency response. Finally, this study did not assess the effectiveness of GRRT deployments, which limits the usefulness of these descriptive data. Efforts are underway to incorporate impact-related metrics into GRRT’s operational data collection, including surveys of GRRT responders and surveys of those who request GRRT assistance. Mixed-methods projects are also underway that aim to assess effectiveness. In the future, process indicators could also be used to calculate some effect-related measures, such as timeliness of responder deployments. 4
GRRT is not the only emergency response mechanism at CDC. A response could be driven by subject matter experts from within a CDC branch or division, or a center- or agency-wide response could be staffed directly by CDC’s Emergency Operations Center. Often, a response does not need large-scale resources or agency-wide staff provided through a response structure such as GRRT. A branch or division may already have all the expertise and resources needed to staff a particular public health response or may have additional specialized staffing needs.
This study highlights how GRRT deployment characteristics shifted in response to evolving agency-wide needs during the COVID-19 pandemic and how nimble data management and operating systems captured these changing needs. CDC Moving Forward, an agency review commissioned by CDC’s director, underscored the need for a workforce prepared to respond to future public health emergencies. 5 The findings explicitly recommended the use of a rapid response team to quickly respond to public health emergencies, resulting in a new program, CDCReady Responder, designed to prepare all CDC staff for emergency response and to ensure rapid establishment and sustained response activities when emergencies occur.6,7 Data management that quickly incorporates new response elements, such as remote deployment requests, into response database platforms is essential. 8 While, as previously discussed, future analyses are needed to determine the effectiveness of GRRT, its surge staffing model could be replicated by other public health agencies with sufficient resources.
Acknowledgments
André van Zyl, MPH, provided technical assistance with R coding and analysis support. Amen Ben Hamida, MD, MPH, provided insight on methods used for the previously published 2018-2019 report: Trends and Characteristics of CDC Global Rapid Response Team Deployments—A 6-Month Report, October 2018–March 2019. At the time this research was done, Mwoddah Habib, MPH, was an Oak Ridge Institute for Science and Education (ORISE) Fellow.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Centers for Disease Control and Prevention.
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
ORCID iD: Christina Watson, DrPH  https://orcid.org/0000-0001-7590-757X
https://orcid.org/0000-0001-7590-757X
References
- 1. Ben Hamida A, Bugli D, Hoffman A, et al. Trends and characteristics of CDC Global Rapid Response Team deployments—a 6-month report, October 2018–March 2019. Public Health Rep. 2020;135(3):310-312. doi: 10.1177/0033354920914662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Redd SC, Frieden TR. CDC’s evolving approach to emergency response. Health Secur. 2017;15(1):41-52. doi: 10.1089/hs.2017.0006 [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization. Regional offices. 2024. Accessed May 10, 2023. https://www.who.int/about/who-we-are/regional-offices
- 4. Frieden TR, Lee CT, Bochner AF, Buissonnière M, McClelland A. 7-1-7: an organising principle, target, and accountability metric to make the world safer from pandemics. Lancet. 2021;398(10300):638-640. doi: 10.1016/S0140-6736(21)01250-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. CDC moving forward summary report. Updated 2022. Accessed June 5, 2023. https://www.cdc.gov/about/organization/cdc-moving-forward-summary-report.html; https://www.cdc.gov/about/cdc-moving-forward/index.html
- 6. Preparing for the next public health emergency: reauthorizing the Pandemic and All-Hazards Preparedness Act. Hearing before the US Senate Committee on Health, Education, Labor, and Pensions, 118th Cong, 1st Sess (2023) (testimony of Rochelle P. Walensky, MD, MPH, director, Centers for Disease Control and Prevention). 2023. Accessed August 21, 2023. https://www.help.senate.gov/hearings/preparing-for-the-next-public-health-emergency-reauthorizing-the-pandemic-and-all-hazards-preparedness-act
- 7. Centers for Disease Control and Prevention, Office of Readiness and Response. Readiness report 2023. 2023. Accessed December 17, 2023. https://www.cdc.gov/orr/pubs-links/2023/ORR_2023_Readiness_Report_508.pdf
- 8. World Health Organization. Strengthening health emergency prevention, preparedness, response and resilience. 2023. Accessed December 17, 2023. https://cdn.who.int/media/docs/default-source/emergency-preparedness/who_hepr_wha2023-21051248b.pdf