Abstract
The diagnosis of death by neurological criteria (DNC) requires the exclusion of any clinical effect attributable to xenobiotics. We undertook a retrospective analysis of enquiries to the National Poisons Information Service (NPIS) relating to DNC over a 10-year period. Enquiries were categorised as toxicological, where exposure to a non-therapeutically administered xenobiotic was implicated in the clinical presentation and non-toxicological where exposure to the xenobiotic was not the primary cause of the clinical state. The frequency of enquiry to the NPIS regarding xenobiotics and DNC demonstrates that it remains a valuable source of expert advice.
Keywords: Diagnosis of death by neurological criteria, poisoning
Introduction
The diagnosis of death has important medical, legal and societal implications, that necessitates its determination is accurate, reliable and certain. The Academy of the Medical Royal Colleges (AoMRC) Code of Practice for the Diagnosis of Death requires that when verifying death by neurological criteria (DNC), reversible causes and confounding factors contributing to the clinical state of the patient must have been excluded prior to the undertaking of clinical testing. 1 Specifically, there must be certainty that xenobiotics are not contributing to the state of unconsciousness, apnoea and absence of brainstem reflexes as multiple xenobiotics can mimic brainstem reflex loss. 2
The United Kingdom (UK) NPIS is a 24-h service led by consultant clinical toxicologists, offering advice and guidance to healthcare professionals on the management of poisoning including access to the poisons information database, TOXBASE. 3
We evaluated the reasons as to why the NPIS was contacted for guidance where DNC testing was being planned, what xenobiotics were involved and how often the NPIS was being contacted. This builds on previously published data. 4
Methods
A retrospective analysis of the NPIS database was undertaken using the search terms “brain dead,” “brain death,” “brain stem,” “brainstem” or “stem testing” between 01/01/2013 and 31/12/2022. Duplications or incongruous cases were deleted from the data set.
Toxicological injury was defined as a case where exposure to a non-therapeutically administered xenobiotic was implicated in the clinical presentation and considered to be contributing to the clinical state including direct effects of the xenobiotic and sequelae of poisoning. Non-toxicological injury was defined as a case where the primary cause was not due to exposure to a xenobiotic.
Results
We identified 136 enquiries, of which 95 were deemed relevant; 84 related to toxicological injury and 11 to non-toxicological injury. Reasons for contacting the NPIS are shown in Table 1 (multiple reasons in 21 enquiries):
Table 1.
Reason for enquiry to the NPIS and Class of xenobiotic.
| Reason for enquiry to the NPIS | Toxicological | Non-toxicological | Total |
|---|---|---|---|
| Presence of agents affecting brainstem testing | 60 | 8 | 68 |
| Kinetics and metabolism of xenobiotic | 29 | 0 | 29 |
| Requests for laboratory analysis - Xenobiotic (n) |
8 Zonisamide (1) Midazolam (1) Tramadol (1) Flunitrazepam (1) Cyanide (2) Cannabis (1) Phenobarbital (1) |
3 Thiopentone (2) Midazolam (1) |
11 |
| Interpretation of quantitative analytical results - Advice regarding significance of levels - Xenobiotic (n) - Interpreting results without units - Xenobiotic (n) - Level to enable testing for DNC - Xenobiotic (n) |
6 3 Amitriptyline and Nortriptyline (1) Lead (1) Carbon monoxide (1) 1 Benzodiazepine and Methadone (1) 2 Ethylene Glycol (2) |
2 2 Thiopentone (2) |
8 |
| Class of xenobiotic (n) | Frequently discussed xenobiotic (n) | ||
| Mixed prescription drugs (20) | Amitriptyline (11) Benzodiazepines (10) Barbiturates (6) Gabapentin (5) Baclofen (4) |
||
| Single prescribed drugs (18) | |||
| Toxic alcohol (13) | Ethylene Glycol (8) | ||
| Multiple drugs of abuse (8) | Cocaine (10) Benzodiazepines (10) Barbiturates (6) Cannabinoids (6) Heroin (5) |
||
| Single drug of abuse (12) | |||
| Combination of prescription drugs and drugs of abuse (6) | See above prescribed/drugs of abuse | ||
| Other (7) | Cyanide/Carbon monoxide (4) Bleach (1) Bleach/Myrrh/Frankincense (1) Lead (1) |
||
The median age of the toxicological group was 36 years (IQR 24-45); 51% were male. All agents requested for laboratory analysis in the toxicological group were the xenobiotic implicated in the original poisoning.
The median age of the non-toxicological group was 41 years IQR (25-61); 55% were male. The causes of non-toxicological injury were: trauma (n = 5), stroke (n = 1), subarachnoid haemorrhage (n = 1), status epilepticus (n = 1), hypoxic ischaemic encephalopathy (out of hospital cardiac arrest and hanging) (n = 2), and meningitis (n = 1). Enquiries related to therapeutic xenobiotics included thiopentone (n = 2) and midazolam (n = 1), specifically in reference to duration of infusion, agent levels and altered metabolism in renal or hepatic failure. All other enquiries (n = 8) related to concurrent use of xenobiotic in the patient history (use of heroin, methadone, amphetamine, cocaine, and cannabinoids) which were subsequently not found to be contributory to the clinical state.
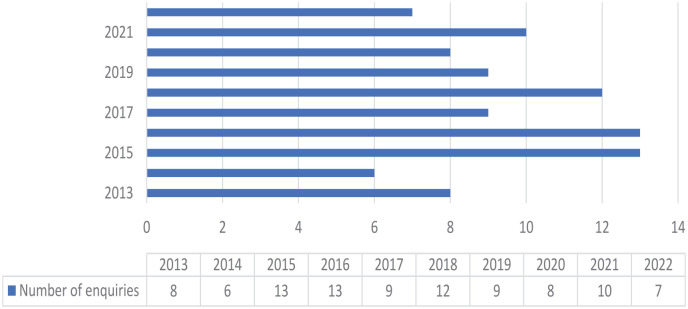
The frequency of enquiries to the NPIS relating to DNC over the 10-year period varied with a range of 6 to 13 per year (Figure 1).
Figure 1.
Yearly enquiries to NPIS relating to DNC.
Discussion
Of the 11 enquiries requesting laboratory analysis, just under half of those discussions led to advice relating to how the presence of agents affects brainstem tests. The enquiries requesting laboratory testing related to availability of quantitative analysis, for example out of hours testing and geographical location. In the majority of cases (n = 9) the agent was able to be tested following advice given by NPIS. In the remaining cases, testing was not available out of hours or not available in the UK (baclofen assays). Twenty-six enquiries requesting advice regarding the kinetics and metabolism of xenobiotics included common themes such as the half live of agents, how long to wait for neurological death testing, drug interactions, and clearance of agent in the context of multi-organ failure.
Given the requirement for certainty in excluding the confounding effects of xenobiotics prior to undertaking clinical testing when verifying DNC, the NPIS has been an important source of expert advice in the management of patients with both toxicological and non-toxicological injury. 4 The demand for access to this service has remained consistent over a 10-year period although whether this will be affected by recent published guidance regarding the use of ancillary testing when verifying DNC, 5 remains to be seen.
We recognise the limitations of this data set; in particular the lack of data in limited follow up and inability to comment on clinical decision making following NPIS advice. In a minority of cases we were unable to differentiate between recreational versus prescribed xenobiotics (specifically benzodiazepines and barbiturates), and the terms “death by neurological criteria” or “DNC” were not included in the search criteria.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Jeanie Worthington  https://orcid.org/0000-0001-9199-4562
https://orcid.org/0000-0001-9199-4562
Emma Moyns  https://orcid.org/0000-0003-2618-1973
https://orcid.org/0000-0003-2618-1973
References
- 1. Academy of Medical Royal Colleges. A code of practice for the diagnosis and confirmation of death. Academy of Medical Royal Colleges. www.aomrc.org.uk/reports-guidance/ukdec-reports-and-guidance/code-practice-diagnosis-confirmation-death (2008, accessed 16 April 2023).
- 2. Murphy L, Wolfer H, Hendrickson R. Toxicologic confounders of brain death determination: a narrative review. Neurocrit Care 2021; 34: 1072–1089. DOI: 10.1007/s12028-020-01114-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. The National Poisons Information Service. https://www.npis.org (accessed 13 April 2023).
- 4. Moyns E, Williams H, Pucci M, et al. M. The role of the UK National Poisons Information Service (NPIS) in the diagnosis of death in poisoned and non-poisoned patients. In: 38th International congress of the European association of poisons centres and clinical toxicologists (EAPCCT) 22-25 May 2018, Bucharest, Romania, Clinical Toxicology, vol. 56, no. 6, pp. 453–608. DOI: 10.1080/15563650.2018.1457818. [DOI] [PubMed] [Google Scholar]
- 5. Thomas EO, Manara A, Dineen RA, et al. The use of cerebral computed tomographic angiography as an ancillary investigation to support a clinical diagnosis of death using neurological criteria: a consensus guideline. Anaesthesia 2023; 78: 330–336. DOI: 10.1111/anae.15950. [DOI] [PubMed] [Google Scholar]