Case Presentation
A 7-year-old girl was referred for a 1-year history of dermatitis restricted to the distal pulp of the left fourth finger. She denied sucking the finger and had no history of atopic dermatitis. Previous patch tests had ruled out allergic contact dermatitis to the most important contact allergens. The clinical examination revealed eczematous changes restricted to the tip of the fourth finger, characterized by mild erythema, scales, and fissures. The nail plate was raised due to mild subungual hyperkeratosis and onycholysis. A diagnosis of parakeratosis pustulosa was suspected, and the treatment with potent topical corticosteroids led to clinical improvement, with almost complete resolution of skin signs observed within one month. No recurrences were seen at the 6-month follow-up visit.
Teaching Point
Parakeratosis pustulosa is a typical and exclusive pediatric condition, more commonly seen in girls aged 5 to 7 years. It frequently affects a single finger, typically the thumb or index finger, and manifests with mild eczematous changes of the pulp along with psoriasiform nail changes [1]. It is considered a possible clinical presentation of eczema or psoriasis [1]. The condition usually begins with pustules or vesicles, followed by eczematous changes, and may progress to pulpitis, though rarely. Nail alterations develop after the skin inflammatory changes and include mild subungual hyper-keratosis and onycholysis, often more pronounced on one side of the nail. Differential diagnosis includes onychomycosis, nail sucking, chronic paronychia, and eczema. Patch test helps to exclude allergic contact dermatitis. The course of parakeratosis pustulosa is chronic with spontaneous remission over time. In some patients it can evolve into nail psoriasis, typically mild [2].
Figure 1.
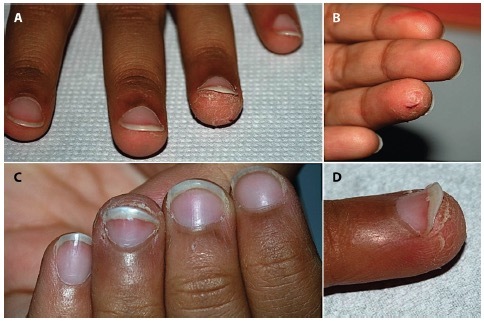
(A, B) Eczematous changes of the distal pulp of the left fourth finger, (B, C) associated with subungual hyperkeratosis and (C, D) onycholysis.
Footnotes
Funding: None.
Competing Interests: None.
Authorship: All authors have contributed significantly to this publication. Piraccini BM and Neri I contributed equally to this work and share senior authorship.
References
- 1.Tosti A, Peluso AM, Zucchelli V. Clinical features and long-term follow-up of 20 cases of parakeratosis pustulosa. Pediatr Dermatol. 1998;15(4):259–63. doi: 10.1046/j.1525-1470.1998.1998015259.x. [DOI] [PubMed] [Google Scholar]
- 2.Richert B, André J. Nail disorders in children: diagnosis and management. Am J Clin Dermatol. 2011 Apr 1;12(2):101–12. doi: 10.2165/11537110-000000000-00000. [DOI] [PubMed] [Google Scholar]


