Abstract
Background:
The skyline or dorsal tangential view (DTV) and the carpal shoot-through (CST) have been developed to enhance the intraoperative examination of the distal radius’s dorsal cortex during open reduction and internal fixation with volar plates. This study aimed to assess the lateral view (LV), DTV, and CST’s effectiveness in showcasing screws that penetrate the dorsal cortex.
Methods:
Eighty patients, comprised of 42 women and 38 men with an average age of 53 years, underwent volar locking plate fixation for displaced distal radius fractures. The procedures incorporated the use of intraoperative LV, DTV, and CST views. Every view was meticulously examined to record the presence of screws that breached the dorsal cortex of the fractured region.
Results:
Only 2 screws were found to protrude the dorsal cortex in the LV, demonstrating 100% specificity and 18.8% sensitivity. On the DTV, 9 screws were detected with the same specificity but increased sensitivity (75%). On the CST, all 12 screws were identified, making for 100% specificity and sensitivity. Of 501 distal screws, 13 (2.54%) penetrated the dorsal cortex, with an average length of 1.34 mm (range, 0.5–2 mm). These screws were subsequently replaced with shorter screws in 12 of 80 patients.
Conclusions:
The findings show that the CST and DTV are more precise and accurate than LV in identifying dorsal screw protrusion during distal radius volar plating. To minimize the likelihood of subsequent complications, it is highly advisable to implement these views in all procedures.
Takeaways
Question: How to reduce the risk of dorsal screw protrusions in distal radius fractures?
Findings: Dorsal tangential view (DTV) and carpal shoot-through (CST) view were compared with the lateral view (LV) to evaluate the intraoperative detection of screws that penetrate the dorsal cortex in 80 patients with distal volar radius fracture. DTV and CST view detected more screws than the LV.
Meaning: DTV and CST are more sensitive than an LV when demonstrating dorsal screw protrusion in distal radius volar plating. The authors strongly recommend performing these views in every procedure to reduce the risk of secondary complications.
INTRODUCTION
Open reduction and internal fixation with volar plates is recognized as the standard surgical procedure for treating distal radius fractures.1–3 Although volar plates decrease the likelihood of postoperative extensor tendon injuries more than dorsal plating,4 they are still associated with some tendon-related issues.5 The increased usage of volar locking plates has seen reports of conditions such as tenosynovitis and extensor tendon ruptures, often a result of the distal screws penetrating the dorsal cortex of the distal radius.6–9
With these issues, the overall complication rate associated with extensor tendon rupture or tenosynovitis is approximately 6%.10,11 Due to the irregular contour of the dorsal cortex of the distal radius, detecting screw penetration on standard radiographic views is challenging.12 The lateral view (LV), obtained by a 20-degree elevation of the elbow (equivalent to the radial inclination to optimally visualize the radiocarpal joint), is primarily used to finalize the check-in volar plating for distal radius fractures. However, standard fluoroscopic views have low sensitivity, making it difficult to detect dorsal cortical penetration, even when the screws protrude 2 mm.12 New radiographic views have been described to detect dorsal screw penetration and avoid preventable iatrogenic pitfalls.13,14
Multiple studies suggest the intraoperative use of the fluoroscopic dorsal tangential view (DTV), also referred to as skyline view, for the precise detection of dorsal screw penetration following volar plating.15–17 Experimental research confirms this view’s accuracy.18–20 Similar to an axial scan using computed tomography (CT), the DTV aids in observing the dorsal topography of the distal radius and enables the identification of screw penetration in dorsal compartments.12 The carpal shoot-through (CST) view is a rarely used yet informative, fluoroscopic view.21,22 It offers insights into the dorsal radial cortex and the distal radial ulnar joint. The purpose of this study was to evaluate the effectiveness of LV, DTV, and CST in identifying screws that have penetrated the dorsal cortex.
MATERIALS AND METHODS
Eighty patients (mean age, 53 y; range, 24–89 y) were enrolled in a prospective study from January 2018 to March 2020. The cohort included 42 women and 38 men. These patients underwent volar locking plate fixation for intra- or extra-articular displaced distal radius fractures. Those with prior distal radius fractures, malunion, or prior osteosynthesis were excluded from our study. Every surgical procedure was performed by the same senior hand surgeon, classified as type IV according to the Tang classification.23 Any decisions regarding screw changes were made in the operating room. All procedures adhered to the ethical standards of the committee responsible for human experimentation in accordance with the revised Declaration of Helsinki of 1975, which was updated in 2008.
Surgical Technique
The Henry or modified Henry surgical approach was utilized for all patients. Locking compression VA-LCP two-column distal radius plate 2.4 mm (De Puy Synthes Companies, IN), with either 6 or 7 holes, were used in a volar position. Screw holes were labeled as illustrated in Figure 1. All plates were deployed according to the manufacturer’s instructions. Depth gauges were used to ascertain the correct screw length, with the standard practice of reducing the measured gauge length by 1–2 mm to determine the exact screw size. The surgeon recorded the lengths of both initial and revised screws based on direct observations or surgeon reports. The study kept records of the screw quantity protruding from the dorsal cortex of the distal fracture fragment, and the number of screws that needed replacement.
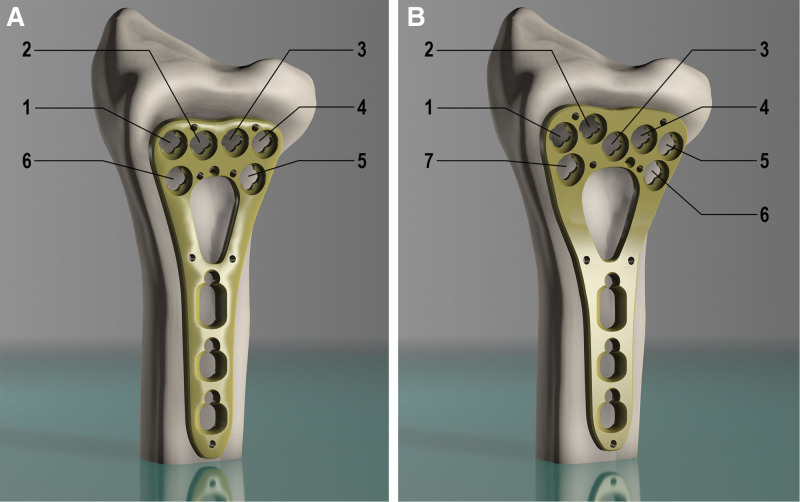
Fig. 1.
Locking compression VA-LCP two-column distal radius volar plate 2.4 (De Puy Synthes Companies) with (A) 6 or (B) 7 distal holes were used. The screw holes have been numbered progressively starting with the most radial and distal one.
Imaging Technique
During each operation, we obtained fluoroscopic images that included LV, DTV, and CST view. To acquire the DTV, the forearm was placed at a 70-degree angle relative to the horizontal arm table, whereas the wrist was flexed to the maximum. The dorsal cortex of the distal radius was adjusted to create a 20-degree angle with the vertical x-ray beam of the fluoroscope (Fig. 2A).
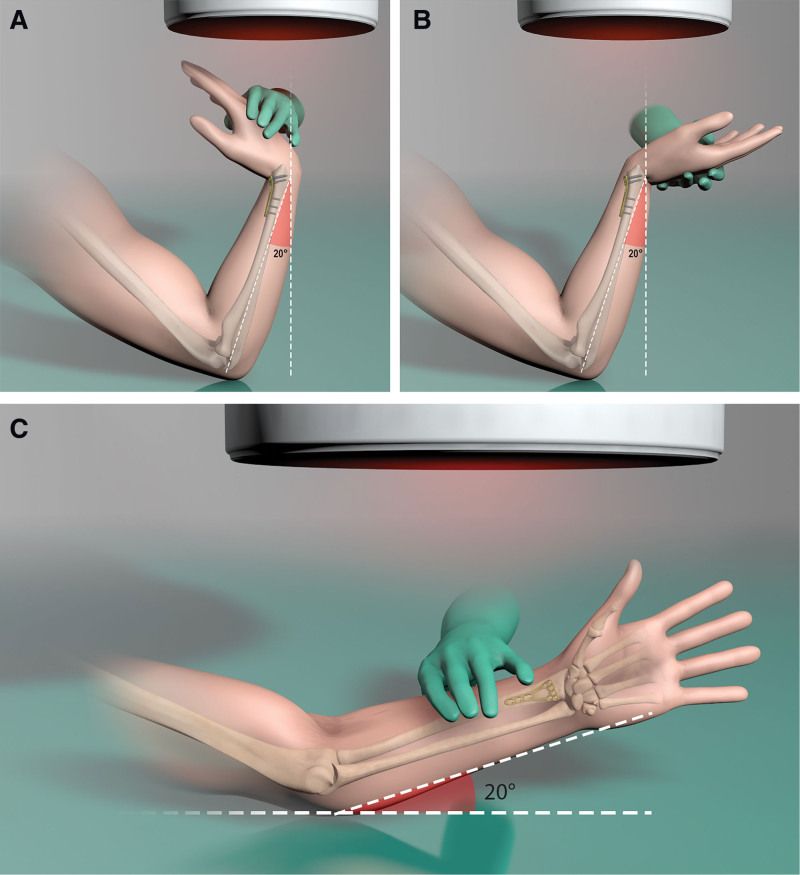
Fig. 2.
Position to be maintained for each view: A, DTV. B, CST view. C, LV.
To capture the CST view, the arm was positioned in supination with the elbow bent roughly 70 degrees, a 20-degree tilt from vertical. The wrist was also extended 70 degrees (Fig. 2B).
The dorsal cortex of the distal radius overlies the carpal bones. To obtain an LV, the patient’s wrist was elevated off the table by approximately 20 degrees, enhancing the visibility of the radiocarpal intra-articular space (Fig. 2C). It has been reported that standard x-ray examination of the forearm and wrist may not suffice for every patient.24 Therefore, the most convenient method to obtain a proper DTV or CST view is to utilize short bursts of continuous fluoroscopy (Figs. 3, 4).
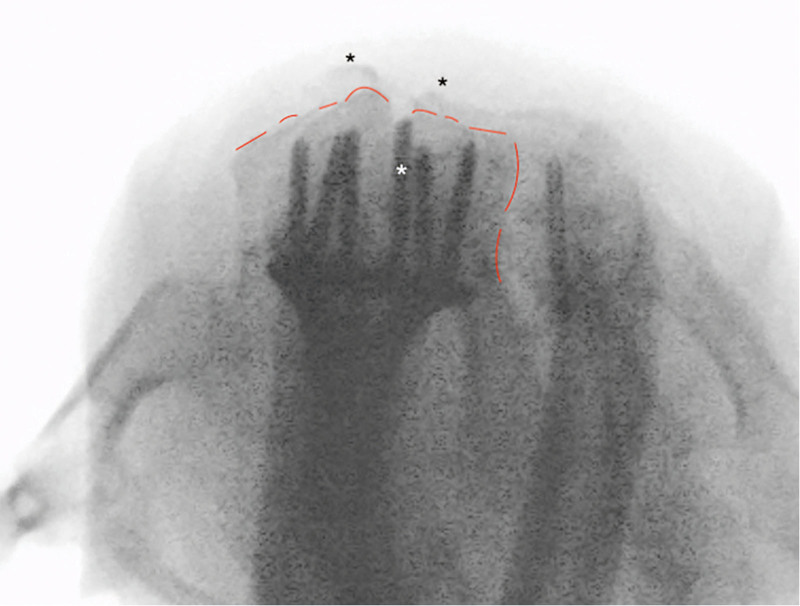
Fig. 3.
Skyline view (DTV). Black asterisk: comminution of dorsal fracture. Red dashed line: dorsal margin of radius and sigmoid notch. White asterisk: screw at position 3 changed for protrusion beyond the dorsal cortex of the radius.
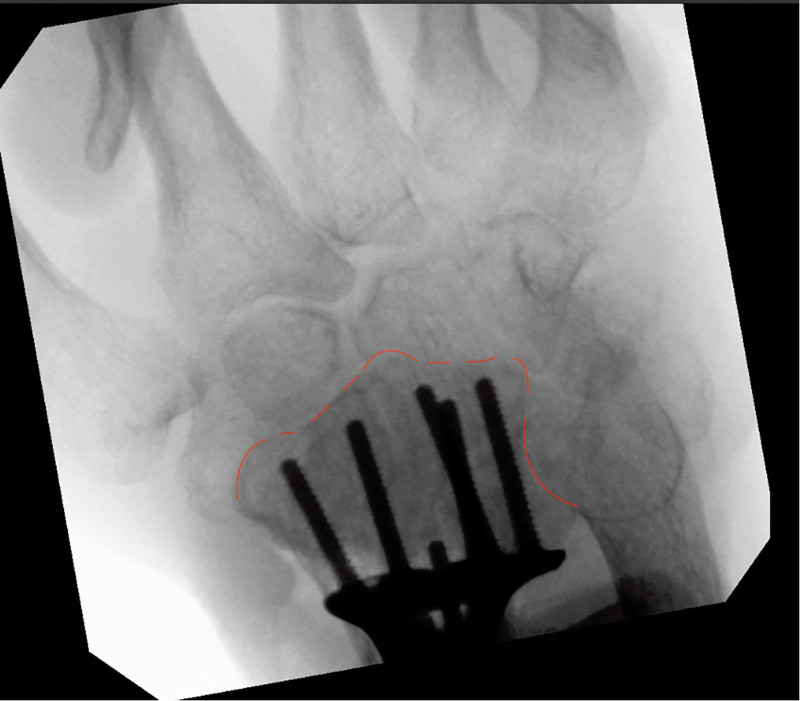
Fig. 4.
CST. Red dashed line: dorsal margin of radius and sigmoid notch. All screws have the correct length and do not protrude beyond the dorsal cortex of the distal radius.
Statistical Analysis
Continuous data were represented as the mean (SD) and median (25–75th percentile), whereas categorical data were shown as a count (%). We utilized the Friedman paired test to examine the variance in the number of screws across different views. For further analysis and pairwise comparison, corrections were made using the Bonferroni adjustment with the Wilcoxon paired test. The length of screws in various positions was compared using the Kruskal–Wallis test. We considered a P value less than 0.05 to be statistically significant. All statistical computations were executed with STATA v16.
RESULTS
Plates with 6 distal holes were used in 64 cases, whereas plates with 7 distal holes were used in 16 cases. The operation was performed on the left wrist in 45 cases and the right wrist in 35 cases. Twelve patients required at least 1 screw replacement, and 13 (2.6%) distal protruding screws were detected and replaced. Among these, 8 screws belonged to the VA-LCP 7 cases, whereas 5 belonged to VA-LCP 6 cases; the difference was not statistically significant (P > 0.05). The average excess length was 1.27 ± 0.63 mm, ranging from 0.5 to 2 mm.
On the LV, only 2 screws were found to protrude from the dorsal cortex (specificity 100% and sensitivity 18.8%), whereas 9 screws on the DTV (specificity 100% and sensitivity 75%) and 12 on the CST view (specificity 100% and sensitivity 100%) were detected (Table 1). The CST identified protruding screws in all cases that the DTV and LV had already detected. In addition, 3 cases in which neither DTV nor LV detected any protruding screws were identified by the CST (Table 2).
Table 1.
Total Number of Screw Protrusion Detected for Every Single View
| Total | VA-LCP 6 | VA-LCP 7 | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| N | 80 | 64 | 16 | |||
| LV | 2 | 2.5 | 1 | 1.6 | 1 | 6.3 |
| DTV | 9 | 11.3 | 4 | 6.3 | 5 | 31.3 |
| CST | 12 | 15.0 | 5 | 7.8 | 7 | 43.8 |
Table 2.
Protruded Screws Detected for Single View
| Protruded Screw | LV | DTV | CST | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| 0 | 78 | 97.5 | 71 | 88.75 | 68 | 85 |
| 1 | 2 | 2.5 | 9 | 11.25 | 11 | 13.75 |
| 2 | 0 | 0 | 0 | 0 | 1 | 1.25 |
The Friedman test revealed a significant difference among 3 projections (P < 0.001). When comparing the groups pairwise (using the Bonferroni correction), the LV significantly differed from the DTV (P = 0.025) and the CST view (P = 0.003). However, no statistically significant difference was found between the CST view and DTV (P = 0.137).
The screws requiring revision were in positions 1, 2, and 3, with the majority located in position 3 (46%) (Table 3). No significant difference was found in the excess length of the 3 types of screws.
Table 3.
Position of the Protruded Screw on the Plate
| Total | VA-LCP 6 | VA-LCP 7 | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| N | 13 | 5 | 8 | |||
| Position 1 | 3 | 23.1 | 0 | 0.0 | 3 | 37.5 |
| Position 2 | 4 | 30.8 | 3 | 60.0 | 1 | 12.5 |
| Position 3 | 6 | 46.2 | 2 | 40.0 | 4 | 50.0 |
DISCUSSION
Volar locking plates are commonly used as a treatment for displaced fractures in the distal radius. Surgeons select and verify the correct screw length through intraoperative depth gauges, ultrasound, or fluoroscopy.14,25,26 Recently, these plates have gained popularity among hand and trauma surgeons. However, the most common and preventable complications are tendinitis or belated ruptures of the extensor or flexor tendons due to volar locking compression.10,27
The anatomy of the distal radius is complex and irregular, posing challenges to achieving a complete and accurate intraoperative view.12,13 This study evaluated fluoroscopy options to address these anatomical complexities, yielding several significant findings. Notably, screws protruding from the dorsal cortex could be overlooked with an LV.14 We found that the majority of dorsally protruding screws were missed in standard LVs. (See table, Supplemental Digital Content 1, which displays demographics of the patients with the type of fracture, used plate, and detected screws for a single view, http://links.lww.com/PRSGO/D630.) The height of the Lister tubercle and the depth of the groove of the extensor pollicis longus vary between 4 and 10 mm, complicating the detection of screw protrusion, particularly in the third extensor compartment.28 Some studies have indicated that the height of the Lister tubercle ranges from 1.4 to 6.6 mm when assessed using CT scans.29 Although fluoroscopic views in pronation and supination aid in detecting protruding screws, standardization poses challenges.14
Through DTV, in the present study, the authors identified 69.2% of all protruding screws. Jacob et al30 suggested the DTV for a clearer visualization of the dorsal cortex of the distal radius. However, this view contrasts with the carpal tunnel view, which emphasizes the volar aspect of the distal radius.31,32 The DTV provides important data about dorsal screw penetration that is often unavailable in the conventional intraoperative fluoroscopic LV.13
Marsland et al21 introduced the CST in 2014. However, despite its introduction, there have been only a few studies that further explore this concept, and its application in clinical practice remains limited.22,33 In the present study, the authors identified 12 osteosyntheses in protruding hardware using both the DTV and CST view. Among DTV, LV, and CST, the latter proved to be the most sensitive in detecting protruding screws, thereby exemplifying its value in the open reduction and internal fixation of distal radius fractures (Fig. 5).
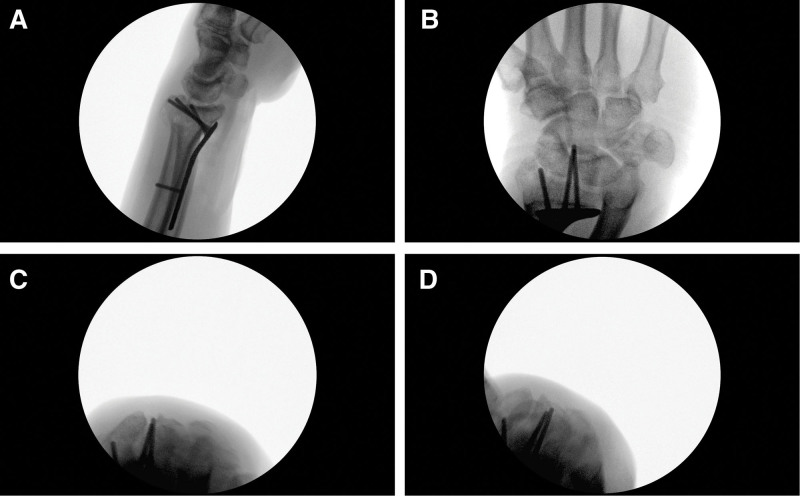
Fig. 5.
Clinical case report with intraoperative fluoroscopy. A, LV fails to detect a screw that is too long in the third compartment (black asterisk). The protruding screw is clearly visible in (B) with a CST view (white asterisk) and in (C) with DTV (black asterisk). D, The intraoperative control after the screw change.
The screw holes identified as most hazardous are numbers 1, 2, and 3. These have the potential to harm the tendons of the third and fourth extensor compartments.33 Currently, no proof establishes that a 1-mm dorsal screw protrusion has a significant impact on tendon damage. Yet, a cadaveric report noted an extensor tendon injury with a 2-mm dorsal screw protrusion.34 Soong et al35 revealed that extensor injuries, although rare in modern volar plating outputs, can induce considerable patient morbidity. Such harm can be easily prevented through detailed intraoperative views. Therefore, the preference for slightly shorter screws in plate fixation is strongly recommended to help avoid these issues. Wall et al36 confirmed that locked unicortical distal screws with 75% length can offer stiffness akin to bicortical-screw fixation. However, this solution does not apply to intra-articular, multifragmentary, and osteoporotic distal radius fractures that demand the application of longer locking screws.
This study has a few limitations, such as a small sample size, mixed cohorts, and the inability to visually inspect screw protrusion directly. Moreover, we lacked intraobserver or interobserver calculations because the screws were adjusted intraoperatively based on the surgeon’s judgment. The study might have been underpowered to detect a difference between DTV and CTV. The absence of intraoperative sonography or a postoperative CT scan could mean that some penetrating screws might have been overlooked, or replacements may not have been necessary. The radiocarpal intra-articular screws are typically evaluated using LV, which thus has different diagnostic features than DTV and CST. This study underscores that reliance solely on LV to detect protruding dorsal screws is inadequate.
CONCLUSIONS
The DTV and CST view seems particularly effective for accurately measuring screw length in distal radius fractures. The authors suggest routinely implementing this surgical procedure to assess the interface between the screw and the dorsal cortex. They also recommend reducing each depth gauge measurement by at least 2 mm and up to 4 mm to lessen the risk of screw protrusion.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
DECLARATION OF HELSINKI
Patients provided informed consent in accordance with the Declaration of Helsinki.
Supplementary Material
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Downing ND, Karantana A. A revolution in the management of fractures of the distal radius? J Bone Joint Surg Br. 2008;90:1271–1275. [DOI] [PubMed] [Google Scholar]
- 2.Sügün TS, Gürbüz Y, Ozaksar K, et al. Results of volar locking plating for unstable distal radius fractures. Acta Orthop Traumatol Turc. 2012;46:22–25. [PubMed] [Google Scholar]
- 3.Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000;5:103–112. [DOI] [PubMed] [Google Scholar]
- 4.Lutsky K, Boyer M, Goldfarb C. Dorsal locked plate fixation of distal radius fractures. J Hand Surg Am. 2013;38:1414–1422. [DOI] [PubMed] [Google Scholar]
- 5.Bergsma M, Doornberg JN, Duit R, et al. ; Lleyton Hewitt Study Group. Volar plating in distal radius fractures: a prospective clinical study on efficacy of dorsal tangential views to avoid screw penetration. Injury. 2018;49:1810–1815. [DOI] [PubMed] [Google Scholar]
- 6.Sügün TS, Karabay N, Gürbüz Y, et al. Screw prominences related to palmar locking plating of distal radius. J Hand Surg Eur Vol. 2011;36:320–324. [DOI] [PubMed] [Google Scholar]
- 7.Toros T, Sügün TS, Özaksar K. Complications of distal radius locking plates. Injury. 2013;44:336–339. [DOI] [PubMed] [Google Scholar]
- 8.Al-Rashid M, Theivendran K, Craigen MA. Delayed ruptures of the extensor tendon secondary to the use of volar locking compression plates for distal radial fractures. J Bone Joint Surg Br. 2006;88:1610–1612. [DOI] [PubMed] [Google Scholar]
- 9.Benson EC, DeCarvalho A, Mikola EA, et al. Two potential causes of EPL rupture after distal radius volar plate fixation. Clin Orthop Relat Res. 2006;451:218–222. [DOI] [PubMed] [Google Scholar]
- 10.Arora R, Lutz M, Hennerbichler A, et al. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316–322. [DOI] [PubMed] [Google Scholar]
- 11.Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003;27:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas AD, Greenberg JA. Use of fluoroscopy in determining screw overshoot in the dorsal distal radius: a cadaveric study. J Hand Surg Am. 2009;34:258–261. [DOI] [PubMed] [Google Scholar]
- 13.Ozer K, Toker S. Dorsal tangential view of the wrist to detect screw penetration to the dorsal cortex of the distal radius after volar fixed-angle plating. Hand (N Y). 2011;6:190–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maschke SD, Evans PJ, Schub D, et al. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand (N Y). 2007;2:144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hill BW, Shakir I, Cannada LK. Dorsal screw penetration with the use of volar plating of distal radius fractures: how can you best detect? J Orthop Trauma. 2015;29:e408–e413. [DOI] [PubMed] [Google Scholar]
- 16.Rausch S, Marintschev I, Graul I, et al. Tangential view and intraoperative three-dimensional fluoroscopy for the detection of screw-misplacements in volar plating of distal radius fractures. Arch Trauma Res. 2015;4:e24622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brunner A, Siebert C, Stieger C, et al. The dorsal tangential x-ray view to determine dorsal screw penetration during volar plating of distal radius fractures. J Hand Surg Am. 2015;40:27–33. [DOI] [PubMed] [Google Scholar]
- 18.Vaiss L, Ichihara S, Ramirez DG, et al. A comparative study about ionizing radiation emitted during radiological “skyline” view of the wrist in pronation versus supination. Eur J Orthop Surg Traumatol. 2015;25:309–311. [DOI] [PubMed] [Google Scholar]
- 19.Riddick AP, Hickey B, White SP. Accuracy of the skyline view for detecting dorsal cortical penetration during volar distal radius fixation. J Hand Surg Eur Vol. 2012;37:407–411. [DOI] [PubMed] [Google Scholar]
- 20.Joseph SJ, Harvey JN. The dorsal horizon view: detecting screw protrusion at the distal radius. J Hand Surg Am. 2011;36:1691–1693. [DOI] [PubMed] [Google Scholar]
- 21.Marsland D, Hobbs CM, Sauvé PS. Volar locking plate fixation of distal radius fractures: use of an intra-operative “carpal shoot through” view to identify dorsal compartment and distal radioulnar joint screw penetration. Hand (N Y). 2014;9:516–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stoops TK, Santoni BG, Clark NM, et al. Sensitivity and specificity of skyline and carpal shoot-through fluoroscopic views of volar plate fixation of the distal radius: a cadaveric investigation of dorsal cortex screw penetration. Hand (N Y). 2017;12:551–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tang JB, Giddins G. Why and how to report surgeons’ levels of expertise. J Hand Surg Eur Vol. 2016;41:365–366. [DOI] [PubMed] [Google Scholar]
- 24.Kiyak G. In vivo confirmation of the reliability of the dorsal tangential view of the wrist. Hand Surg Rehabil. 2018;37:56–59. [DOI] [PubMed] [Google Scholar]
- 25.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002;27:205–215. [DOI] [PubMed] [Google Scholar]
- 26.Watchmaker JD, Daley RA, Watchmaker GP, et al. Ultrasound imaging improves identification of prominent hardware in the surgical treatment of distal radius fractures: a cadaveric and prospective clinical study. J Wrist Surg. 2016;5:36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lucchina S, Fusetti C. Is early hardware removal compulsory after retention of angled drill guides in palmar locking plates? The role of pronator quadratus reconstruction. Chin J Traumatol. 2010;13:123–125. [PubMed] [Google Scholar]
- 28.Clement H, Pichler W, Nelson D, et al. Morphometric analysis of Lister’s tubercle and its consequences on volar plate fixation of distal radius fractures. J Hand Surg Am. 2008;33:1716–1719. [DOI] [PubMed] [Google Scholar]
- 29.Pichler W, Windisch G, Schaffler G, et al. Computer tomography aided 3D analysis of the distal dorsal radius surface and the effects on volar plate osteosynthesis. J Hand Surg Eur Vol. 2009;34:598–602. [DOI] [PubMed] [Google Scholar]
- 30.Jacob J, Clay NR. Re: Pichler et al. Computer tomography aided 3D analysis of the distal dorsal radius surface and the effects on volar plate osteosynthesis. J Hand Surg Eur. 2009, 34: 598-602. J Hand Surg Eur Vol. 2010;35:335–336. [DOI] [PubMed] [Google Scholar]
- 31.Wilson JN. Profiles of the carpal canal. J Bone Joint Surg Am. 1954;36:127–132. [PubMed] [Google Scholar]
- 32.Carroll RE, Lakin JF. Fracture of the hook of the hamate: radiographic visualization. Iowa Orthop J. 1993;13:178–182. [PMC free article] [PubMed] [Google Scholar]
- 33.Bergsma M, Denk K, Doornberg JN, et al. Volar plating: imaging modalities for the detection of screw penetration. J Wrist Surg. 2019;8:520–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Austin A, Green S, Ahsan S, et al. Cadaveric study of appropriate screw length for distal radius stabilization using volar plate fixation. Am J Orthop (Belle Mead NJ). 2015;44:369–372. [PubMed] [Google Scholar]
- 35.Soong M, van Leerdam R, Guitton TG, et al. Fracture of the distal radius: risk factors for complications after locked volar plate fixation. J Hand Surg Am. 2011;36:3–9. [DOI] [PubMed] [Google Scholar]
- 36.Wall LB, Brodt MD, Silva MJ, et al. The effects of screw length on stability of simulated osteoporotic distal radius fractures fixed with volar locking plates. J Hand Surg Am. 2012;37:446–453. [DOI] [PMC free article] [PubMed] [Google Scholar]