Abstract
Background:
Inadequate physical activity (PA) is increasingly common among stroke patients, we aim to comprehensively analyze the experience of stroke patients delivering physical activity, understand the obstacles and promoting factors of physical activity, and summarize clinical management strategies.
Methods:
An electronic search of PubMed, Web of Science, Cochrane Library, ProQuest, SinoMed, CNKI, and WanFang Database was conducted for qualitative studies on the experience of PA in stroke patients. The review was appraised using the Joanna Briggs Institute methodology, the subsequent findings were synthesized via the Thomas and Harden approach and the credibility of the research results was evaluated by the CERqual tool.
Results:
Six thousand five hundred forty-nine findings were yielded through the search, ultimately 11 studies were included through screening, a total of 194 stroke patients participated in the study, and 3 synthesized themes that emerged were identified: barriers to PA, facilitators to PA, and strategies to improve compliance with physical activity in stroke patients. All selected articles were of medium quality and all themes were of medium or high quality.
Conclusion:
The experience of PA among stroke patients should be given more attention. Healthcare professionals should provide physical activity-related knowledge education, social support, personalized care, improved environments, and create more opportunities for PA. In the future, more tailored interventions should be carried out to develop PA habits and improve compliance.
Keywords: experience, meta-synthesis, physical activity, qualitative research, stroke
1. Introduction
The global prevalence of strokes is on the rise, with the disease having a high morbidity and mortality rate.[1] At present, the recurrence rate of stroke is 11% to 28.3%,[2] which seriously affects patients’ quality of life. There is evidence to suggest, however, that over 90% of strokes are contributed to physical activity (PA) inactivity, which belongs to modifiable risk factors.[3] PA refers to any physical activity that results in skeletal muscle contractions, which lead to energy expenditure.[4] In recent years, guidelines on PA of stroke have also emerged, but mainly in developed countries, such as the United States,[5–7] the United Kingdom,[8] Spain,[9] Canada,[10] and Australia.[11] We can see that the medical and social support for stroke patients varies among different countries, such as emotion, information, self-management, and tool support. Increasing PA can decrease the risk of cardiovascular disease, delay the decline of cognitive function, and reduce relapses.[12] Additionally, an individual’s mental health can also be improved.[13–15] Despite the known benefits, PA implementation among stroke patients remains insufficient in many countries. A study by American scholar Rand[16] concluded that 58% of stroke patients spent <30 minutes a day participating in PA in their recovery from the disease. West[17] pointed out that stroke patients spent only 12.8% and 22.7% of their day performing moderate and high-intensity PA, respectively. Belgian scholar Vanroy[18] and American scholar Tudor-Locke[19] investigated the daily steps of stroke patients, Vanroy found that 54% of stroke patients took <5500 steps per day, Tudor-Locke agreed with his results and expressed in the research that their sedentary time exceeded 8 to 9 hours per day. It can be seen that the PA of stroke patients is seriously insufficient.
Insufficient PA is influenced by various factors. Hendrickx W et al[20] included 4 cross-sectional and 5 intervention studies in a meta-analysis that identified behavioral and environmental factors associated with excessive sedentary time in community-dwelling stroke patients. In addition, English C et al[21] provided a systematic review of PA and sedentary levels in stroke patients which was limited to a cross-sectional survey of elderly stroke patients in the community. To continuously increase the compliance of stroke patients with PA, it is necessary to understand their true thoughts and feelings. Currently, qualitative studies on the experience of PA in stroke patients have emerged, no literature yet synthesizes these studies. Therefore, in our study, the meta-integration method was adopted to interpret stroke patients’ experience on PA and summarize clinical management strategies, to serve as a recommendation for the construction and development of PA programs for stroke patients.
2. Methods
2.1. Design
This study was conducted following the thematic approach of Thomas and Harden.[22] The protocol was registered with PROSPERO (CRD42023409107). The findings are reported per the guidelines of Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ).[23]
2.2. Search strategy
The search for resources was conducted in PubMed, Web of Science, Cochrane Library, ProQuest, SinoMed, CNKI, and WanFang Database. Based on the PICoS framework, the following key concepts were used: physical activity, stroke, and qualitative research. MeSH terms and free terms were combined to make a full search. In addition, the snowballing technique was used to screen reference lists of eligible articles. The articles on qualitative studies of stroke patients’ experiences with PA were collected from inception until December 31, 2022. The full PubMed search strategy can be seen in Appendix 1, Supplemental Digital Content, http://links.lww.com/MD/N883.
Initially, citations retrieved were exported into EndNote20 and managed. After removing duplicated citations, the title and abstract of the remaining articles were independently reviewed by 2 reviewers to determine whether they met the standards, and then read the full text in detail to select the literature again. To minimize the potential bias, the whole process was supervised by the research team. In case of disagreement between 2 reviewers, it is handed over to a third party.
2.3. Inclusion and exclusion criteria
An overview of the inclusion and exclusion criteria that were used for this study is in Table 1.
Table 1.
Inclusion and exclusion criteria for the studies.
| PICOS criteria | Eligibility criteria |
|---|---|
| Population | Adult patients diagnosed with stroke. |
| Phenomenon of interest | Experience of physical activity in patients with stroke. |
| Context | Any country, hospital, or place. |
| Study design | Research published in English and Chinese including qualitative or mixed methods with qualitative components. |
| Exclusion criteria | Duplicate publication and incomplete information; full text not available; poor-quality methodology. |
2.4. Quality assessment
Based on the appraisal tool developed by the Joanna Briggs Institute for Qualitative Research, the quality of the literature was assessed. There are 10 items in the evaluation. A rating of “yes,” “no,” “unclear” or “not applicable” is given to each item. The literature quality is divided into 3 grades.[24] Grades A and B indicate that the quality of the literature fully and partially meets the criteria, respectively. Grade C indicates that the literature quality does not meet the criteria at all. Discuss and decide with the third reviewer when the literature quality evaluation results of the 2 researchers are inconsistent. Ultimately, the literature which quality of A and B were included. Documents with quality levels A and B were included.
2.5. Data extraction and synthesis
Country, first author, participants, aim, method, and themes were separately acquired by 2 reviewers. A Thomas and Harden-based thematic approach was used to synthesize the findings.[25] Firstly, 2 reviewers independently extracted line-by-line text, including participant quotations and author interpretations, and coded it in an Excel spreadsheet. Secondly, the same reviewers individually established descriptive themes via initial code grouping with shared meaning. These descriptive themes were then discussed and upgraded to new analytical themes that represented the stroke patients’ PA perspectives. The CERqual tool was used to evaluate the credibility of the research results.[26] Throughout, disagreements would be handed over to a third party for decision, ultimately resulting in a new, comprehensive outcome. To reduce bias, the entire process is carried out under the supervision of the team.
3. Results
3.1. Screening process
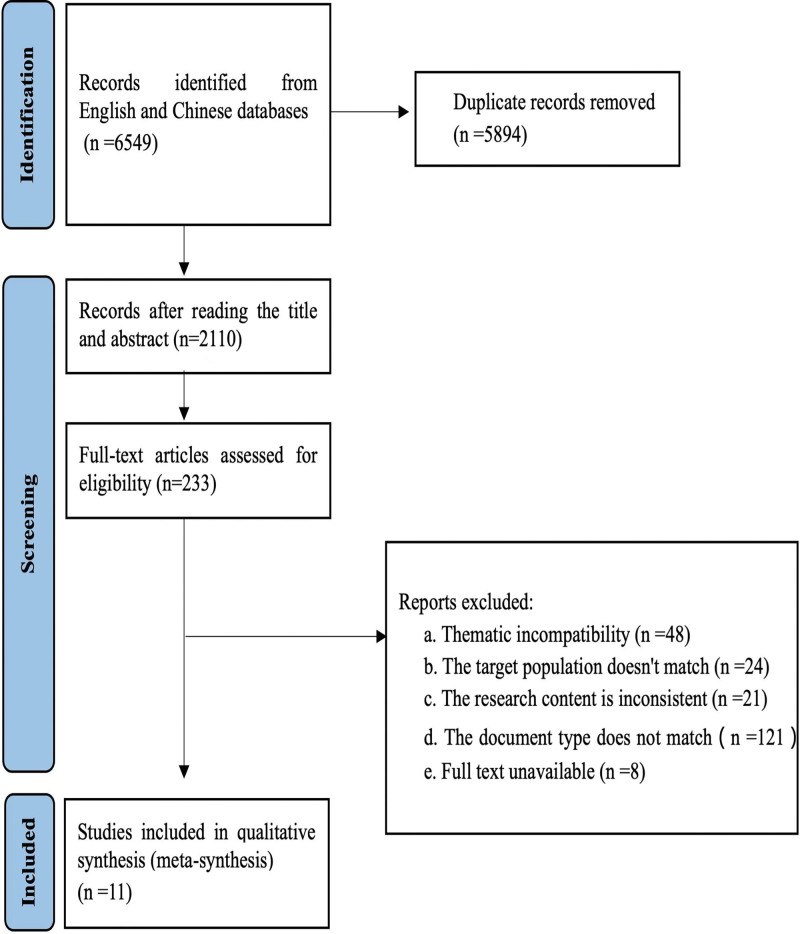
In total, 6549 findings were yielded through the search. After removing 5894 duplicate articles, the remaining 233 articles continued to be reviewed by the title and abstract. Following reading the full text, 11 qualitative articles were included in this article. Further process of the data extraction can be found in Figure 1.
Figure 1.
Flow diagram of the literature search.
3.2. Characteristics included in the study
In our research, 11 studies were conducted in 5 countries (Rwanda, Sweden, Netherlands, UK, USA), 80% were developed countries. A total of 194 stroke patients participated in the study, their ages ranged from 24 to 89 years old. The included studies mainly used the following methods: interviews (n = 9), focus groups (n = 1), and mixed method (n = 1) (Table 2).
Table 2.
Characteristics of the studies.
| Country | First author | Participants | Methods | Aim | Themes |
|---|---|---|---|---|---|
| Rwanda | Gerard Urimubenshi[27] | Stroke patients; age range: 24–79; n = 10 | Phenomenological study; Face-to-face in-depth interviews |
Patient’s physical activity experience | 1. Disease experience; 2. Limitations of walking, self-care activities, and home life activities; 3. Participation restrictions; 4. Psychological experience. |
| Sweden | Karin Tornbom[28] | Stroke patients; age range: 38–64; n = 8 |
Descriptive qualitative research; Semi-structured interviews; In-depth interviews |
Patients’ views and experiences on physical activity or walking motivation and disorder | 1. Negative psychological factors; 2. Fatigue; 3. Fear of falling; 4. Injury experience; 5. Environmental factors |
| Sweden | Karin Tornbom[29] | Stroke patients; age range:38–64; n = 8 |
Descriptive qualitative research; Semi-structured interviews; In-depth interviews |
Participate in the treadmill walking experience using virtual reality | 1. Pleasant and unforgettable experience; 2. Fatigue from too much exercise; 3. Suggestions for improving virtual reality experience. |
| USA | Barbara Resnick[30] | Stroke patients; mean age: 64 ± 12; n = 29 | Descriptive qualitative research; Focus group interviews or telephone interviews |
Motivation of patients to participate in aerobic exercise | 1. Personal goals; 2. Physical and mental benefits; 3. Benefits of supervised exercise; 4. Verbal encouragement; 5. Social support; 6. Improvement of activities of daily living tools; 7. Self-determination. |
| UK | Niall Maclean[31] | Stroke patients; age range: 38–86; n = 22 | Descriptive qualitative research; Semi-structured interviews |
Positive and negative factors of patient motivation for recovery | 1. Rehabilitation confidence; 2. Interpersonal relationship; 3. Role transformation; 4. The role of professionals and family members; 5. Patients’ views on the nature, purpose and function of rehabilitation. |
| Netherlands | Jacqueline Outermans[32] | Stroke patients; age range: 46–89; n = 36 | Phenomenological research; Mixed methods (semi-structured interviews, structured interviews, focus group interviews) |
Promoting factors and obstacle factors of patients’ outdoor walking | 1. Intention to walk outdoors; 2. Ability to walk outdoors; 3. Opportunity to walk outdoors. |
| USA | Ryan R[33] | Stroke patients; age range: 43–79; n = 15 | Phenomenological research; semi-structured interviews |
Patient’s conceptual understanding of Physical Activity | 1. Moderate to vigorous physical activity; 2. Physical activity in daily life or occupation; 3. Avoid sedentary. |
| UK | Jennifer Hall[34] | Stroke patients; mean age:75; n = 31 | Descriptive qualitative research; Observation method, semi-structured interviews |
Patients’ perceptions and experiences with sedentary behavior | 1. Levels and patterns of sedentary behavior after stroke; 2. Physical function and social environment; 3. Ability to stand and move after stroke; 4. Emotion and motivation; 5. Role of nursing staff; 6. Intervention to reduce sedentary behavior. |
| Sweden | Kirsti S. Roaldsen[35] | Stroke patients; age range: 36–61; n = 10 | Descriptive qualitative research; Semi-structured, face-to-face interviews | Patients’ cognition of sedentary behavior and physical activity | 1. Physical activity is a form of treatment; 2. Insecurity; 3. Restrictions on physical activity; 4. Risk of sedentary behaviour. |
| USA | Ryan Bailey[36] | Stroke patients; age range: 18–80; n = 15 | Phenomenological research; Semi-structured, in-depth interviews |
Socio-psychological factors of patients’ physical activity | 1. Expected results; 2. Self-efficacy; 3. Self-management; 4. Social support. |
| Sweden | Ann-Sofie B. Jansson[37] | Stroke patients; age range: 18–80; n = 10 | Phenomenological research; Semi-structured interviews |
Experience and influencing factors of physical activity of patients | 1. Social support; 2. Obstacles and opportunities; 3. Individual motivation. |
3.3. Quality evaluation results
All selected articles were of medium quality by the Joanna Briggs Institute for Qualitative Research, only 3 studies have consistent philosophical perspectives and methodology, the vast majority of studies overlook the relationship between researchers and research subjects. The CERqual was employed for the assessment of theme quality, 2 themes were high quality and 1 was medium quality, mainly due to limitations in “relevance” and “adequacy” in the third theme “strategies to improve compliance with physical activity in stroke patients.” Specific details are shown in Tables 3 and 4.
Table 3.
Literature quality evaluation.
| First author | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Grade* |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gerard Urimubenshi[27] | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | B |
| Karin Tornbom[28] | U | Y | Y | Y | Y | Y | N | Y | Y | Y | B |
| Karin Tornbom[29] | U | Y | Y | Y | Y | Y | N | Y | Y | Y | B |
| Barbara Resnick[30] | U | Y | Y | Y | Y | N | N | Y | Y | Y | B |
| Niall Maclean[31] | U | Y | Y | Y | Y | Y | N | Y | U | Y | B |
| Jacqueline Outermans[32] | U | Y | Y | Y | Y | Y | N | Y | Y | Y | B |
| Ryan R[33] | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | B |
| Jennifer Hall[34] | U | Y | Y | Y | Y | Y | N | Y | Y | Y | B |
| Kirsti S. Roaldsen[35] | U | Y | Y | Y | Y | Y | N | Y | Y | Y | B |
| Ryan Bailey[36] | U | Y | Y | Y | Y | N | N | Y | Y | Y | B |
| Ann-Sofie B. Jansson[37] | Y | Y | Y | Y | Y | Y | N | Y | N | Y | B |
Q1. Is there congruity between the stated philosophical perspective and the research methodology? Q2. Is the methodology consistent with the questions posed? Q3. Is there congruity between the research methodology and the methods used to collect data? Q4. Is there congruity between the research methodology and the representation and analysis of data? Q5. Is there congruity between the research methodology and the interpretation of results? Q6. Is there a statement locating the researcher culturally or theoretically? Q7. Is the influence of the researcher on the research, and vice-versa, addressed? Q8. Are participants, and their voices, adequately represented? Q9. Is the research ethical according to current criteria or, for recent studies, and is there evidence of ethical approval by an appropriate body? Q10. Are the conclusions drawn in the research report flow from the analysis or interpretation, of the data?
Note: Y = Yes; N = NO; U = Unclear.
Table 4.
GRADE-CERqual approach for assessing confidence.
| Theme | Label | The number of Study | A | B | C | D | Overall rating |
|---|---|---|---|---|---|---|---|
| D1 | Physical activity of stroke patients is affected by obstructive factors | 11 | Minor concerns (11 studies moderate rigor) | Minor concerns (5 countries represented in the studies) |
No or minor concerns (Theme consistent across 11 studies) |
Moderate concerns (Themes are richly described across 3/11) |
High |
| D2 | Physical activity of stroke patients is affected by promoting factors | 5 | Minor concerns (5 studies moderate rigor) | Minor concerns (4 countries represented in the studies) |
Moderate concerns (Theme consistent across 5 studies) |
Minor concerns (Themes are richly described across 3/5) |
High |
| D3 | Strategies to improve compliance with physical activity in stroke patients | 5 | Minor concerns (5 studies moderate rigor) | Moderate concerns (2 countries represented in the studies) |
No or minor concerns (Theme consistent across 5 studies) |
Moderate concerns (Themes are richly described across 1/5) |
Moderate |
Note: A, “Methodological limitations,” the methodological limitations were assessed using the JBI. B, “Relevance,” relevance was appraised through a comparison of each finding to the context of the research question. C, “Coherence,” coherence was evaluated by reviewing the fit between the primary data and the review findings. D, ‘Adequacy of data’, adequacy was determined by assessing the depth of data supporting a synthesis theme. Overall rating: high, moderate, low, very low.
3.4. Meta-synthesis
Using the Thomas and Harden-based thematic approach, we have identified 3 key themes, including 12 subthemes.
3.5. Theme 1: physical activity of stroke patients is affected by obstructive factors
3.5.1. Subtheme 1: the barriers are decreased physical function and uncomfortable symptoms
Limb hemiplegia, decreased coordination, and muscle weakness in stroke patients are vital factors affecting PA.[38] Moreover, patients of different ages have different adaptability to PA, some elderly patients stated that walking too much or too fast had a negative impact on the heart. Apart from this, the studies portrayed that symptoms such as fatigue, joint and back pain also brought troubles to patients.
“I love gardening, I still do, I can’t do it, I try but after sort of half-an-hour, three-quarters I’m totaled.[37]”
“It was too much. I felt my heart beat too quickly, that can’t be good for me at my age? I did not like it very much.[32]”
3.5.2. Subtheme 2: physical environmental constraints discourage stroke patients from physical activity
Several included studies claimed that physical environmental constraints were mainly related to inclement weather, uneven ground, crowded environment, and convenient facilities, which were similar to the results of the study by Ezeugwu VE.[39] Some patients highlighted that the narrow space caused by the successive placement of medical devices reduced space available for movement.[40] In addition, on account of depending on wheelchairs or other scooters, the opportunity of walking is decreasing.
“I cannot use my wheelchair out of the house because there are many stones outside there.[27]”
“It were windy and I felt as though I could get blown over here.[34]”
“I barely dare to walk outside in this kind of weather because if I fall then I can’t catch myself.[28]”
“Let’s be honest, I have a mobility scooter that I love. Why would I walk with my rollator? You can only use that for exercise around the house perhaps, but nothing much else.[32]”
3.5.3. Subtheme 3: caregiver-related factors are considered as obstacles
Insufficient human resources and limited time for healthcare personnel prevent patients from completing PA programs on a regular basis. Another frequently mentioned humanistic environmental constraints were the overprotection of family and friends due to fear of falling or bodily injury, which resulted in limited opportunities to engage in PA.
“There weren’t enough staff around and I was immobile anyway with my leg.[34]”
“My wife also, because she saw me fall twice and had to help me. So you do not want to wait for it to happen a third time.[32]”
“[Family] would jump after me and get ahead of me so that I wouldn’t hurt myself. When I first came up here [to a senior apartment complex], the first month was just everybody wanting to be here all of the time. And I said, you don’t have to babysit me.[36]”
3.5.4. Subtheme 4: the obstructive factor is negative psychological experience
As shown in the included studies, a variety of negative psychological experiences which affect PA were common among stroke patients, which were similar to the results on the study by Sánchez-Sánchez ML.[38] Some patients are ashamed of the gaze of others or distressed by the lack of guidance after discharge. Fear of falling is the most important source of anxiety for patients, resulting in inadequate activity in patients who live alone in particular. Older patients have low expectations for future recovery, so they are not inclined to change sedentary behavior (SB).
“I prefer to go alone. I feel like I am in the way. I am fine walking by myself.[32]”
“Walking is just more complicated. Perhaps you think all it takes is a little push from someone or other and I am down.[32]”
“I don’t want the others in the stable to be there because I know everyone watches each other.[35]”
3.5.5. Subtheme 5: the obstructive factor is insufficient information
Most of the patients were afraid to participate in the training because they did not understand their rehabilitation plan. After discharge, the professional did not provide relevant information, resulting in the anxiety of patients. Besides, the inconsistent rehabilitation information provided by professionals caused patients to have contradictory psychology.
“The ultimate aim is to get me walking... I don’t understand the steps. How they [the physiotherapists] plan it.[31]”
“The help was good downstairs [in the physiotherapy gym] but when I come up here, I go to bed again so what can I do?... So I don’t know what is good or bad... I just don’t know... you can’t bother people just because you want to learn how to walk.[31]”
3.5.6. Subtheme 6: the obstructive factor is the insufficient understanding of physical activity
As indicated in included studies, some patients only associated the PA with exercise equipment, and have not yet realized the harm of insufficient PA. Furthermore, more patients were skeptical about the benefits of PA, and they perceived that an active and healthy lifestyle cannot weaken the risk of stroke. Consistent with the results on the studies by Hallgren M,[41] some patients also believed that sedentary behaviors related to mental activities such as reading were different from passive sedentary behaviors such as watching TV, which was beneficial to health. Thus, PA-related knowledge education is of vital to change their misconception.
“When a lot of people think of physical activity, they think of... exercise equipment.[33]”
“I wouldn’t anticipate the [health] benefits of reducing sedentary behavior at all.[34]”
“I think maybe half of the sedentary things is good providing you’re keeping your brain going and you’re not sitting there just thinking of nothing.[29]”
3.6. Theme 2: physical activity of stroke patients is affected by promoting factors
3.6.1. Subtheme 7: the facilitator is adequate social support
Social support is mainly provided by healthcare professionals, families, and the community. Their encouragement can boost patient confidence in exercising. However, compared with them, the advice of medical staff can promote patients to carry out PA more, and their supervision during exercise provides patients with a sense of security. Except for verbal encouragement, it is also a good way to indirectly help patients break sedentary behavior.
“Family and friends...[are] inspiring. On Facebook, my son posted my picture for participating in a walkathon. So many of my friends in California and [back home] said, ‘You can do it,’ or they told me, ‘I have a similar problem, and you can do it.’ It reinforces my desire.[36]”
“I would rather exercise at a physiotherapy clinic than at a regular gym. I feel safe and there is a physiotherapist who is there and helps all the time.[35]”
“People do listen to the medical people... I think that incentivises people...the voice of authority.[34]”
3.6.2. Subtheme 8: the facilitators are positive physical and psychological experience
Some patients reported that after PA, their muscle strength became stronger and their pain was effectively relieved. In addition to the improvement of physical function, positive emotions such as happiness and satisfaction can be brought, and have a lasting impact on health. PA also gives patients the courage to try new things, boosts their self-confidence, and reduces their dependence on others.
“I like being able to basically move up and move around and do whatever I want. It gives you independence. A sense of satisfaction.[36]..”
“Physical activity gives me harmony. It makes you happy, you know, the endorphins are bubbling, and it makes you very positive.[35]”
“With exercise I can make the pain go away, or at least reduce it. That’s why I avoid a lot of painkillers.[35]”
3.6.3. Subtheme 9: strong behavioral belief improves initiative
In our included studies, behavioral belief was defined as a determination to perform PA. Studies also demonstrated that a strong behavioral belief was a motivating factor for PA. However, patients’ belief in daily PA was affected by psychological perception, mastery of experience, lack of information, and existing negative emotions leading to the loss of behavioral belief.
“I think I should walk at least a little every day, I just have that feeling I should stay limber... because I know exercise is good for me.[32]”
“I’ll be semi-depressed or in a bad mood for a while, but then I’m like, You can overcome this[36]!”
“[At first] it was slow and you would wobble and couldn’t walk. I just kept it up. I just kept trying... I think that confidence comes from being able to do it. When you start and you realize, ‘I’m not going to fall down,’ then you have the confidence to keep going.[36]”
3.7. Theme 3: strategies to improve compliance with physical activity in stroke patients
3.7.1. Subtheme 10: use virtual reality (VR) technology to improve the enthusiasm of physical activity
Walking in the traditional sense was considered a boring form, while virtual reality placed patients outdoors to help find the feeling of PA before a stroke. The visual and auditory feedback brought by VR made patients more willing to walk. Thus, patients suggested using wind sounds and more natural sounds to add authenticity, and hoped to increase the variety of videos to improve exercise motivation.
“The bird sounds gave another sense of really being present... and even the footsteps, even if they weren’t exactly synched. Otherwise, I would have wanted to put in more senses! You could have a fan that blows, little breezes on your face as you walk...and smell if you go past a lilac hedge, that would have been lovely.[29]”
3.7.2. Subtheme 11: establish a group intervention program and fully consider patients’ preferences
Group intervention is very important for patients to maintain regular exercise. Meanwhile, the intervention also needs to consider the abilities and preferences of patients. Most patients were unwilling to engage in meaningless activities. Thereby, choosing the most acceptable and favorite things for patients, such as making a cup of tea, and doing crafts can promote patients to persist in PA for a long time.[42]
“Everybody’s different... there’s no 2 stroke people the same.[29]”
3.7.3. Subtheme 12: optimize intervention methods and form physical activity routines
According to the results, establishing a PA routine was important for patients. Achieving the goal of PA in daily activities has been proven to be a feasible plan by some studies.[33,43] More and more patients tried hard to integrate sports into their daily activities (housework, shopping, gardening). And in life, the appropriate use of reminders can promote PA, English C[44] demonstrated that PA and daily energy expenditure could be increased by activity monitor. Besides, partial patients perceived regular PA as a job to motivate them to adhere to it day after day.
“An alarm of some sort that makes you think, ‘oh I’ve been sitting too long.[34]”
“When a [television] commercial comes on, I do a load of wash or take care of putting it in the dryer, or do kitchen essentials that need to be done, putting food away, or getting some water to drink. I’m not sedentary.[36]”
“I don’t say ‘I’m going to exercise now’, I say ‘I’m going to work’ - this is my job.[35]”
4. Discussion
A previous study[21] conducted a systematic review of PA in elderly stroke patients in the community, yet it was limited to the inclusion of cross-sectional and cohort studies exploring the intensity and duration of PA in stroke patients. This meta-synthesis identifies barriers and facilitators of PA in stroke patients from the perspective of inner experience, emphasizing the importance of developing relevant strategies, and indicating the establishment of diversified interventions at multiple levels, including patients, family caregivers, and health professionals.
Although PA have been extensively studied, the distinction between them remains blurred in the minds of patients and even health professionals. The study of Geelen SJG et al[45] pointed out that professionals define PA in different ways, which is inconsistent with patients’ definitions. Therefore, it is important to unify the concept. In addition, PA is usually not prioritized, and the term should be as common in health education as “quit smoking and alcohol,” increasing patients’ perception of it. Taken together, it is necessary to strengthen the systematic training of PA-related knowledge for medical staff, and actively use Internet technology, health lectures, publicity manuals and other methods to strengthen the popularization of PA.
Social support is also an important factor affecting the PA of patients.[46] However, the workload of medical personnel and excessive protection from family caregivers often lead them to neglect patients’ PA and prolonged sitting, which is consisted with the study of Alsop T.[47] In fact, this is also closely related to insufficient knowledge acquisition. Zisberg A et al[48] reported that the participation of multiple social roles can help improve patients’ PA levels. In the future, hospitals and Primary Care should actively implement relevant policies and improve infrastructure to encourage patients to increase their PA. In addition, nonprofessionals such as family members and friends should learn to respect and understand the ability boundaries of patients, we need to give full attention but not overprotect.
Both the physical and caregiver-related environment have an indispensable impact on the PA of stroke patients.[49] People tend to prioritize risk reduction over PA, which helps cultivate a culture of bed rest to promote consistency with the models of biomedical care.[47] PA is considered to increase the risk of falls. In fact, increasing PA can improve limb function and reduce the risk of falls. In addition, there are differences in the economic level of different regions, as well as differences in infrastructure. Healthcare professionals can provide patients in different regions with corresponding community resources, like the distance of fitness centers or community centers, to promote PA. In view of the lack of PA in stroke patients, a few developed countries have promulgated relevant guidelines to provide social support, which suggests that localized guidelines and norms should be developed in the future.
The patients in this study indicated that it was challenging to maintain PA in the long term, and habit formation was the best way to face the challenge. The World Health Organization 2020 guidelines recommended that stroke patients performed aerobic exercise 3 times a week,[50] but most patients have not reached this goal due to physiological, psychological, and social environment factors. Structured exercise programs often make it impossible for patients to adhere, while enjoyable forms of PA can improve patients’ compliance, and integrating PA into daily life is an achievable, low-cost, safe and effective method for stroke patients. Evaluating the emotional response of patients to exercise is a feasible tool for customizing exercise plans. Measuring patients’ pleasant or unpleasant experiences helps them regulate themselves, when patients have the autonomy to choose their exercise intensity, they are more likely to have a positive exercise experience and adhere to the plan.
Stroke patients are often accompanied by anxiety, depression, shame, and other negative emotions.[51] This is linked to poor access to information, lack of social support, and fear of falling. Hamre C’s[52] study clarified that higher levels of anxiety and depression symptoms are related to less PA, which may be because negative emotions reduce patients’ social activities and further increase SB. A systematic review[53] shows that exercise is an effective measure to improve depression levels. By understanding the interaction mechanism between PA, SB, and negative emotions in stroke patients, medical staff can carry out corresponding psychological nursing according to the psychological experience of patients, such as mindfulness yoga and meditation training. In addition, with the development of internet technology, adjusting the VR system to suit personal abilities and preferences can be effective.[29]
5. Conclusion
Through the meta-integration of 11 qualitative studies, this study deeply expounded the experience and attitude of PA of stroke patients. The hindering factors, promoting factors, and countermeasures of PA were discussed. Medical staff should focus on the PA of stroke patients, attach importance to knowledge education and environment optimization, provide personalized nursing for patients, promote the formation of PA habits, and improve compliance. This study still has limitations: First, 11 studies focused on developed countries, including the United States (n = 3), the United Kingdom (n = 2), Sweden (n = 4), and the Netherlands (n = 1). Only 1 study focused on developing country. Therefore, this result may not apply to other countries. Secondly, there are language constraints and publication bias in article retrieval. Thirdly, Potential bias in patient self-reports and variability in qualitative research quality need to be addressed. In the future, the process of qualitative research can be optimized to further explore the PA experience of stroke patients, and then offer a basis for formulating a standardized PA program applied to such patients and improving PA compliance.
Acknowledgments
We thank all participants and authors who provided the original data.
Author contributions
Data curation: Yun Tang, Xinchen Yang, Yue Shu.
Investigation: Xinchen Yang, Yifan Fan, Yue Shu.
Methodology: Yun Tang, Yue Shu.
Project administration: Xingru Li.
Supervision: Yun Tang.
Writing – original draft: Xingru Li.
Writing – review & editing: Yun Tang, Yue Shu.
Supplementary Material
Abbreviations:
- PA
- physical activity
- SB
- sedentary behavior
- VR
- virtual reality
The protocol was registered with PROSPERO (CRD42023409107).
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Supplemental Digital Content is available for this article.
How to cite this article: Li X, Yang X, Fan Y, Tang Y, Shu Y. Experience of physical activity in patients with stroke: A qualitative meta-synthesis. Medicine 2024;103:45(e40500).
Contributor Information
Xingru Li, Email: lixingru97@126.com.
Xinchen Yang, Email: 1768303926@qq.com.
Yifan Fan, Email: 18326401169@163.com.
Yue Shu, Email: shuyue202212@163.com.
References
- [1].Hankey GJ. Secondary stroke prevention. Lancet Neurol. 2014;13:178–94. [DOI] [PubMed] [Google Scholar]
- [2].Ashizawa R, Yamashita K, Take K, et al. Nonleisure-time physical activity guidance following minor ischemic stroke: a randomized clinical trial. Adapt Phys Activ Q. 2021;38:329–47. [DOI] [PubMed] [Google Scholar]
- [3].Strath SJ, Kaminsky LA, Ainsworth BE, et al. Guide to the assessment of physical activity: Clinical and research applications: a scientific statement from the American Heart Association. Circulation. 2013;128:2259–79. [DOI] [PubMed] [Google Scholar]
- [4].Aguiar LT, Nadeau S, Martins JC, Teixeira-Salmela LF, Britto RR, Faria Christina Danielli Coelho de Morais. Efficacy of interventions aimed at improving physical activity in individuals with stroke: a systematic review. Disabil Rehabil. 2020;42:902–17. [DOI] [PubMed] [Google Scholar]
- [5].Gordon NF, Gulanick M, Costa F, et al. Physical activity and exercise recommendations for stroke survivors: an American Heart Association scientific statement from the council on clinical cardiology, subcommittee on exercise, cardiac rehabilitation, and prevention; the council on cardiovascular nursing; the council on nutrition, physical activity, and metabolism; and the stroke council. Circulation. 2004;109:2031–41. [DOI] [PubMed] [Google Scholar]
- [6].Billinger SA, Arena R, Bernhardt J, et al. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2532–53. [DOI] [PubMed] [Google Scholar]
- [7].Winstein CJ, Stein J, Arena R, et al. Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2016;47:e98–e169. [DOI] [PubMed] [Google Scholar]
- [8].Overview | Stroke rehabilitation in adults | Guidance | NICE. NICE; 12 Jun 2013 [cited 11 Jun 2023]. Available: https://www.nice.org.uk/guidance/cg162. Accessed December 10, 2023. [Google Scholar]
- [9].Fuentes B, Gállego J, Gil-Nuñez A, et al. Guidelines for the preventive treatment of ischaemic stroke and TIA (I). Update on risk factors and life style. Neurol Barc Spain. 2012;27:560–74. [DOI] [PubMed] [Google Scholar]
- [10].osn-post-stroke-community-based-exercise-guidelines-2016-final.pdf. Available at: https://www.strokenetworkseo.ca/sites/default/files/files/osn-post-stroke-community-based-exercise-guidelines-2016-final.pdf. Accessed December 10, 2023. [Google Scholar]
- [11].Living Clinical Guidelines for Stroke… | InformMe - Stroke Foundation. [cited 11 Jun 2023]. Available at: https://informme.org.au/guidelines/living-clinical-guidelines-for-stroke-management. Accessed December 10, 2023. [Google Scholar]
- [12].Kramer SF, Hung SH, Brodtmann A. The impact of physical activity before and after stroke on stroke risk and recovery: a narrative review. Curr Neurol Neurosci Rep. 2019;19:28. [DOI] [PubMed] [Google Scholar]
- [13].Okuyama J, Seto S, Fukuda Y, et al. Mental health and physical activity among children and adolescents during the COVID-19 Pandemic. Tohoku J Exp Med. 2021;253:203–15. [DOI] [PubMed] [Google Scholar]
- [14].Bovim MR, Indredavik B, Hokstad A, Cumming T, Bernhardt J, Askim T. Relationship between pre-stroke physical activity and symptoms of post-stroke anxiety and depression: AN observational study. J Rehabil Med. 2019;51:755–60. [DOI] [PubMed] [Google Scholar]
- [15].Apriliyasari RW, Budi IS, Tan MP, Tsai P-S. Physical activity and depression in Indonesian adults with stroke: a nationwide survey. J Nurs Scholarship. 2023;55:356–64. [DOI] [PubMed] [Google Scholar]
- [16].Rand D, Eng JJ, Tang P-F, Jeng J-S, Hung C. How active are people with stroke?:Use of accelerometers to assess physical activity. Stroke. 2009;40:163–8. [DOI] [PubMed] [Google Scholar]
- [17].West T, Bernhardt J. Physical activity patterns of acute stroke patients managed in a rehabilitation focused stroke unit. Biomed Res Int. 2013;2013:438679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Vanroy C, Vissers D, Vanlandewijck Y, et al. Physical activity in chronic home-living and sub-acute hospitalized stroke patients using objective and self-reported measures. Top Stroke Rehabil. 2016;23:98–105. [DOI] [PubMed] [Google Scholar]
- [19].Tudor-Locke C, Craig CL, Aoyagi Y, et al. How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act. 2011;8:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hendrickx W, Riveros C, Askim T, et al. Identifying factors associated with sedentary time after stroke. Secondary analysis of pooled data from nine primary studies. Top Stroke Rehabil. 2019;26:327–34. [DOI] [PubMed] [Google Scholar]
- [21].English C, Manns PJ, Tucak C, Bernhardt J. Physical activity and sedentary behaviors in people with stroke living in the community: a systematic review. Phys Ther. 2014;94:185–96. [DOI] [PubMed] [Google Scholar]
- [22].Thompson ED, Pohlig RT, McCartney KM, et al. Increasing activity after stroke: a randomized controlled trial of high-intensity walking and step activity intervention. Stroke. 2024;55:5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Treloar C, Champness S, Simpson PL, Higginbotham N. Critical appraisal checklist for qualitative research studies. Indian J Pediatr. 2000;67:347–51. [DOI] [PubMed] [Google Scholar]
- [25].Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. 2015;13:179–87. [DOI] [PubMed] [Google Scholar]
- [26].Colvin CJ, Garside R, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 4: how to assess coherence. Implementation Sci. 2018;13:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Urimubenshi G. Activity limitations and participation restrictions experienced by people with stroke in Musanze district in Rwanda. Afr Health Sci. 2015;15:917–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Törnbom K, Sunnerhagen KS, Danielsson A. Perceptions of physical activity and walking in an early stage after stroke or acquired brain injury. PLoS One. 2017;12:e0173463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Törnbom K, Danielsson A. Experiences of treadmill walking with non-immersive virtual reality after stroke or acquired brain injury - A qualitative study. PLoS One. 2018;13:e0209214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Resnick B, Michael K, Shaughnessy M, Kopunek S, Nahm ES, Macko RF. Motivators for treadmill exercise after stroke. Top Stroke Rehabil. 2008;15:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Maclean N, Pound P, Wolfe C, Rudd A. Qualitative analysis of stroke patients’ motivation for rehabilitation. BMJ. 2000;321:1051–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Outermans J, Pool J, van de Port I, Bakers J, Wittink H. What’s keeping people after stroke from walking outdoors to become physically active? A qualitative study, using an integrated biomedical and behavioral theory of functioning and disability. BMC Neurol. 2016;16:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Bailey RR, Stevenson JL. How adults with stroke conceptualize physical activity: an exploratory qualitative study. Am J Occupational Therap. 2021;75:7502345010p1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Hall J, Morton S, Fitzsimons CF, et al. Factors influencing sedentary behaviours after stroke: findings from qualitative observations and interviews with stroke survivors and their caregivers. BMC Public Health. 2020;20:967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Roaldsen KS, Walter C, Gäverth J, Dohrn I-M. Between commitment and avoidance - working age stroke survivors’ perceptions of physical activity and sedentary behaviour: a qualitative study. BMC Neurol. 2022;22:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Bailey R. Examining daily physical activity in community-dwelling adults with stroke using social cognitive theory: an exploratory, qualitative study. Disabil Rehabil. 2020;42:2631–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Jansson A-SB, Carlsson G. Physical activity on prescription at the time of stroke or transient ischemic attack diagnosis - from a patient perspective. Disabil Rehabil. 2021;43:1121–8. [DOI] [PubMed] [Google Scholar]
- [38].Sánchez-Sánchez ML, Arnal-Gómez A, Cortes-Amador S, et al. Association of barriers, fear of falling and fatigue with objectively measured physical activity and sedentary behavior in chronic stroke. J Clin Med. 2021;10:1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Ezeugwu VE, Garga N, Manns PJ. Reducing sedentary behaviour after stroke: perspectives of ambulatory individuals with stroke. Disabil Rehabil. 2017;39:2551–8. [DOI] [PubMed] [Google Scholar]
- [40].Morton S, Hall J, Fitzsimons C, et al. A qualitative study of sedentary behaviours in stroke survivors: non-participant observations and interviews with stroke service staff in stroke units and community services. Disabil Rehabil. 2022;44:5964–73. [DOI] [PubMed] [Google Scholar]
- [41].Hallgren M, Nguyen T-T-D, Owen N, et al. Cross-sectional and prospective relationships of passive and mentally active sedentary behaviours and physical activity with depression. Br J Psychiatry J Ment Sci. 2020;217:413–9. [DOI] [PubMed] [Google Scholar]
- [42].Voss ML, Pope JP, Larouche R, Copeland JL. Stand When You Can: development and pilot testing of an intervention to reduce sedentary time in assisted living. BMC Geriatr. 2020;20:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Saunders DH, Sanderson M, Hayes S, et al. Physical fitness training for stroke patients. Cochrane Database Syst Rev. 2020;3:CD003316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].English C, Healy GN, Coates A, Lewis L, Olds T, Bernhardt J. Sitting and activity time in people with stroke. Phys Ther. 2016;96:193–201. [DOI] [PubMed] [Google Scholar]
- [45].Sjg G, Bm G, Rhh E, et al. Barriers to and solutions for improving physical activity in adults during hospital stay: a mixed-methods study among healthcare professionals. Disabil Rehabil. 2022;44:4004–13. [DOI] [PubMed] [Google Scholar]
- [46].Bailey RR. Self-efficacy, self-regulation, social support, and outcomes expectations for daily physical activity in adults with chronic stroke: a descriptive, exploratory study. Occup Ther Health Care. 2019;33:129–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].T A, J W, I R, N M, S B, S G. Perspectives of health professionals on physical activity and sedentary behaviour in hospitalised adults: a systematic review and thematic synthesis. Clin Rehabil. 2023;37:1386–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Zisberg A, Agmon M, Gur-Yaish N, Rand D, Hayat Y, Gil E. No one size fits all-the development of a theory-driven intervention to increase in-hospital mobility: the “WALK-FOR” study. BMC Geriatr. 2018;18:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Tosi FC, Lin SM, Gomes GC, et al. A multidimensional program including standing exercises, health education, and telephone support to reduce sedentary behavior in frail older adults: Randomized clinical trial. Exp Gerontol. 2021;153:111472. [DOI] [PubMed] [Google Scholar]
- [50].Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Fini NA, Holland AE, Keating J, Simek J, Bernhardt J. How Physically Active Are People Following Stroke? Systematic Review and Quantitative Synthesis. Phys Ther. 2017;97:707–17. [DOI] [PubMed] [Google Scholar]
- [52].Hamre C, Fure B, Helbostad JL, et al. Factors associated with level of physical activity after minor stroke. J Stroke Cerebrovasc Dis. 2021;30:105628. [DOI] [PubMed] [Google Scholar]
- [53].Mammen G, Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am J Prev Med. 2013;45:649–57. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.