Abstract
To retrospectively evaluate the trends in utilization and results of computed tomography pulmonary angiography (CTPA study) for detection of acute pulmonary embolism (PE) in the hospital inpatients during different phases of COVID-19 public health emergency. We conducted an Institutional Review Board (IRB)-approved retrospective review of CTPA studies for our hospital inpatients in the years from 2019 to 2023, ranging from the prepandemic year (2019) to the year coinciding with the end of public health declarations (2023). Collected characteristics included patient age, patient sex, and result of the study. The utilization of CTPA studies for inpatients was higher in 2020 to 2023, compared to 2019 (3.8% in 2023 compared to 2.4% in 2019, P < .001). The increase in utilization was also statistically significant in each group, when stratified by age and sex (OR = 1.46 for female, OR = 1.71 for male, OR = 1.93 for elderly, and OR = 1.29 for non-elderly inpatients in 2023, compared to 2019). The positivity rate of acute PE in the inpatients was overall higher in 2021, 2022, and 2023, compared to 2019 (for example, 18.5% in 2023 compared to 14.3% in 2019, P = .01). When stratified by age and sex, only the non-elderly patients continued to have a significantly higher rate of acute PE in 2023, compared to 2019 (OR = 1.39). While studies spanning longer time frames and involving multiple institutions are needed to understand and generalize this conclusion, we conclude that the utilization and positivity rates of CTPA studies in inpatients remains high at the end of the COVID-19 pandemic public health emergency.
Keywords: COVID-19, CT pulmonary angiography, end of public health declarations, inpatients, pulmonary embolism
1. Introduction
Incidents of thromboembolism, including pulmonary embolism (PE), emerged as some of the initial and most serious complications linked to coronavirus infectious disease 2019 (COVID-19).[1] Considering that Computed Tomography Pulmonary Angiography (CTPA) is the preferred diagnostic tool for detection of PE,[2] it is understandable that its utilization saw a significant increase throughout the pandemic.[3]
Following remarkable strides in converting COVID-19 into a manageable condition, the World Health Organization concluded the public health emergency related to COVID-19 on May 5, 2023.[4] Similarly, the United States Department of Health and Human Services announced the conclusion of the COVID-19 public health emergency on May 11, 2023, stating that the country was in a better position than at any prior point during the pandemic.[5] However, the end of the public health emergency does not necessarily mean that all aspects of the healthcare system impacted by the pandemic have returned to their prepandemic state.
Moreover, some studies have urged caution in adopting the conclusion of these public health emergencies, citing concerns such as the relatively low additional vaccine effectiveness and the increased transmissibility of new viral variants.[6,7] A particular area of uncertainty involves the field of radiology in concerning the utilization and positivity patterns for CTPA studies. Studies that have examined the status of CTPA studies, particularly in terms of utilization and positivity rates after the end of the public health emergency are lacking. Understanding the utilization and outcomes of CTPA studies is essential not only for radiology but also for the ordering departments, as they navigate the postpandemic era.
The objective of this study is to perform a 5-year comprehensive assessment of the utilization and positivity rates of CTPA studies in inpatients spanning different phases of the COVID-19 pandemic.
2. Methods
Patients requiring a stay in the hospital for 1 or more days were designated as inpatients, including patients admitted directly to the hospital, patients admitted through the emergency department, and patients admitted through surgical services. A retrospective review, approved by our Institutional Review Board (IRB), was conducted on adult inpatients (age ≥ 18 years) who presented to the department of Radiology for CTPA studies. This review spanned 5 distinct years, 2019 to 2023. The year 2020 coincided with the World Health Organization (WHO) declaration of COVID-19 as a pandemic,[4] while the year 2023 coincided with the conclusion of COVID-19 public health emergency declarations by the World Health Organization and the United States Department of Health and Human Services.[4,5] The year 2019, therefore, serves as a prepandemic year for our purposes. Patient’s age, sex, and result of the CTPA study were recorded.
To compute CTPA study utilization which is defined as the ratio of CTPA studies ordered to all adult inpatient admissions in a given period, total number of adult inpatient admissions in each of the 5 years was recorded. CTPA studies for patients with complex cardiac history (such as repaired complex congenital heart disease and aortic root replacement), studies definitively identifying chronic pulmonary emboli with no acute component, and nondiagnostic studies (such as due to inadequate contrast bolus administration) were excluded. After these exclusions, presented in Appendix 1, Supplemental Digital Content, http://links.lww.com/MD/N846, 1326 studies in 2019, 1380 studies in 2020, 1874 studies in 2021, 1734 studies in 2022, and 1742 studies in 2023 were included in the analysis.
The results of the included CTPA studies were categorized into positive or negative (for acute PE) based on the findings in the study reports. The characteristics that were documented for analysis encompassed patient age, patient sex, and result of the study. For stratified analysis, adult patients were divided into 2 groups by age (non-elderly: age ≥ 18 years and <65 years; elderly: age ≥ 65 years). A patient was determined to have pulmonary infection if such information was documented in the chart and suspected to have pulmonary infection if such suspicion was present in the radiology report impression. This cohort included those with COVID-19 infection.
Continuous variables were reported as mean with range while categorical variables were reported as frequencies. A P-value of >.05 was considered to be statistically significant. Statistical significance was determined using Student t test, Pearson χ2 test, and odds ratios as applicable. 95% confidence intervals were obtained with odds ratios. Scipy (version 1.10.1, Enthought, Inc., Austin, Texas, USA) was used for analysis.
3. Results
The review identified 1326 CTPA studies in 2019 (mean age 61 years; 50.3% female), 1380 studies in 2020 (mean age 62 years; 45.9% female), 1874 studies in 2021 (mean age 61 years; 44.3% female), 1734 studies in 2022 (mean age 62 years; 46.6% female), and 1742 CTPA studies in 2023 (mean age 63 years; 46.1% female).
3.1. Overall study utilization
A total of 55,286 adult inpatient admissions occurred in 2019, 47,112 occurred in 2020, 49,660 occurred in 2021, 46,991 occurred in 2022, and 45,840 occurred in 2023. Utilization of CTPA study was 2.4% in 2019, 2.9% in 2020, 3.8% in 2021, 3.7% in 2022, and 3.8% in 2023. Compared to 2019, CTPA study utilization was significantly higher in all the subsequent years (Table 1).
Table 1.
CTPA study utilization: overall.
| Year | CTPA (n) | Admissions (n) | CTPA % (%) | P-value | Odds ratio | 95% CI |
|---|---|---|---|---|---|---|
| 2020 | 1380 | 47,112 | 2.9 | <.001* | 1.22 | [1.13, 1.32] |
| 2021 | 1874 | 49,660 | 3.8 | <.001* | 1.57 | [1.46, 1.69] |
| 2022 | 1734 | 46,991 | 3.7 | <.001* | 1.54 | [1.43, 1.66] |
| 2023 | 1742 | 45,840 | 3.8 | <.001* | 1.58 | [1.43, 1.70] |
Compared to CTPA utilization in 2019 which was 2.4%, higher overall utilization was noted in all the subsequent years.
CI = confidence interval, CTPA = computed tomography pulmonary angiography.
Statistical significance.
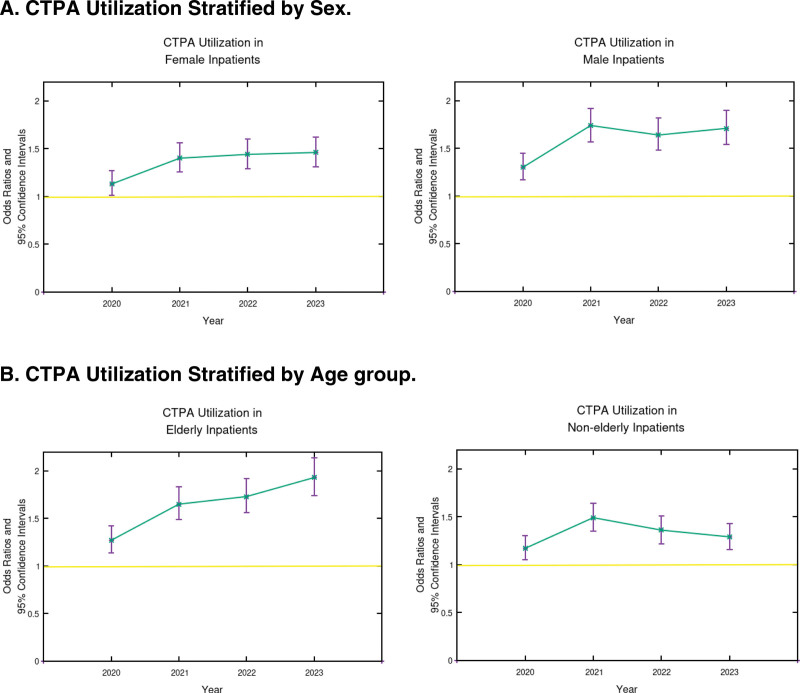
3.2. Study utilization by sex
Sex was non-binary or not reported for 3 patients in 2019, 7 patients in 2020, 9 patients in 2021, 4 patients in 2022, and 7 patients in 2023. Significant increase in CTPA study utilization was noted in both female and male patients during 2020 to 2023, compared to 2019. The odds of a female inpatient admitted in 2023 in receiving a CTPA study were 1.46 times those in 2019, while the odds of a male inpatient admitted in 2023 in receiving a CTPA study were 1.71 times those in 2019 (Fig. 1A). Moreover, the utilization in male patients was significantly higher in the years 2020 to 2023, when compared with female patients (Table 2).
Figure 1.
Stratified CTPA Utilization. (A) CTPA Utilization Stratified by Sex: Compared to 2019, significant increase in CTPA utilization was noted within both female and male patients in all the subsequent years. (B) CTPA utilization stratified by age group: compared to 2019, significant increase in CTPA utilization was noted within both elderly and non-elderly inpatients in all the subsequent years. Yellow line represents an odds ratio of 1. CTPA = computed tomography pulmonary angiography.
Table 2.
CTPA study utilization: differences by sex.
| Year | Male CTPA % (%) | Female CTPA % (%) | P-value | Odds ratio | 95% CI |
|---|---|---|---|---|---|
| 2019 | 2.4 | 2.4 | .73 | 0.98 | [0.88, 1.09] |
| 2020 | 3.1 | 2.7 | .03* | 1.13 | [1.01, 1.26] |
| 2021 | 4.1 | 3.4 | <.001* | 1.21 | [1.11, 1.33] |
| 2022 | 3.9 | 3.5 | .02* | 1.12 | [1.02, 1.24] |
| 2023 | 4 | 3.5 | .005* | 1.15 | [1.04, 1.26] |
Compared to CTPA utilization in the female patients, male patients had an increased utilization from 2020 to 2023.
CI = confidence interval, CTPA = computed tomography pulmonary angiography.
Statistical significance.
3.3. Study utilization by age
Significant increase in CTPA study utilization was noted in both elderly and non-elderly inpatients during 2020 to 2023, compared to 2019. The odds of an elderly inpatient admitted in 2023 in receiving a CTPA study were 1.93 times those in 2019, while the odds of a non-elderly inpatient admitted in 2023 in receiving a CTPA study were 1.29 times those in 2019 (Fig. 1B). While utilization in the non-elderly patients was greater until 2021, more studies were utilized in the elderly in the year 2023 (Table 3).
Table 3.
CTPA study utilization: differences by age group.
| Year | Elderly CTPA % (%) | Non-elderly CTPA % (%) | P-value | Odds ratio | 95% CI |
|---|---|---|---|---|---|
| 2019 | 2.1 | 2.8 | <.001* | 1.34 | [1.2, 1.5] |
| 2020 | 2.6 | 3.3 | <.001* | 1.23 | [1.11, 1.37] |
| 2021 | 3.4 | 4.2 | <.001* | 1.21 | [1.1, 1.33] |
| 2022 | 3.6 | 3.8 | .3 | 1.05 | [0.96, 1.16] |
| 2023 | 4 | 3.6 | .03* | 0.9 | [0.81, 0.99] |
Compared to CTPA utilization in the elderly patients, non-elderly patients had an increased utilization until 2021. In 2023, CTPA was utilized more in the elderly patients.
CI = confidence interval, CTPA = computed tomography pulmonary angiography.
Statistical significance.
3.4. Overall study results
14.3% CTPA studies were positive for acute PE in 2019. The positivity rate increased to 16.9% in 2020, 19.6% in 2021, 19.3% in 2022, and remained high at 18.5% in 2023, although slightly trending down. Compared to 2019, increases in 2021, 2022, and 2023 were statistically significant (Table 4).
Table 4.
CTPA study: overall positivity rate.
| Year | Positive (n) | Total CTPA (n) | Positive % (%) | P-value | Odds ratio | 95% CI |
|---|---|---|---|---|---|---|
| 2020 | 233 | 1380 | 16.9 | .13 | 1.18 | [0.95, 1.46] |
| 2021 | 367 | 1874 | 19.6 | .001* | 1.37 | [1.13, 1.66] |
| 2022 | 334 | 1734 | 19.3 | .003* | 1.34 | [1.11, 1.64] |
| 2023 | 323 | 1742 | 18.5 | .01* | 1.29 | [1.06, 1.58] |
Compared to 2019, significantly more CTPA studies were positive for acute PE in 2021, 2022, and 2023.
CI = confidence interval, CTPA = computed tomography pulmonary angiography, PE = pulmonary embolism.
Statistical significance.
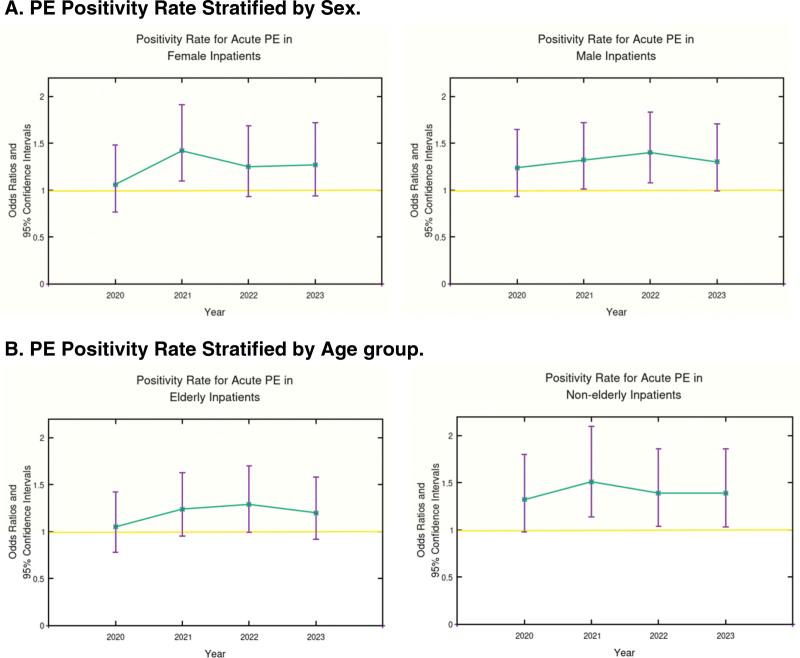
3.5. Positivity rate by sex
Female inpatients had a significantly higher positivity rate for acute PE in 2021, compared to 2019. Male inpatients had a significantly higher positivity rate for acute PE in 2021 and 2022, compared to 2019. Positivity rates for either sex in 2023 were not significantly different from 2019 (Fig. 2A). When PE positivity rates were compared between male and female patients, there was a significant increase in male PE positivity rates in 2020 and 2022. No such significant difference was noted in 2023 (Table 5).
Figure 2.
Stratified PE positivity rates. (A) Stratified PE positivity rate by sex: female inpatients had a significant increase in positivity rate for acute PE in 2021, while male inpatients noticed significant increase in 2021 and 2022, when compared to 2019. In 2023, no significant increase in positivity rate for acute PE noted in either male or female patients, compared to 2019. (B) Stratified PE positivity rate by age group. Elderly inpatients had no significant increase in positivity rate for acute PE in any subsequent year, compared to 2019. Non-elderly inpatients had a significant increase in acute PE positivity rate in 2021 to 2023, compared to 2019. Yellow line represents an odds ratio of 1. CTPA = computed tomography pulmonary angiography, PE = pulmonary embolism.
Table 5.
CTPA study positivity rate: differences by sex.
| Year | Male CTPA % (%) | Female CTPA % (%) | P-value | Odds ratio | 95% CI |
|---|---|---|---|---|---|
| 2019 | 15.5 | 13 | .29 | 1.19 | [0.87, 1.64] |
| 2020 | 19.2 | 13.9 | .03* | 1.38 | [1.03, 1.87] |
| 2021 | 20.5 | 18.6 | .43 | 1.1 | [0.87, 1.4] |
| 2022 | 21.8 | 16.3 | .02* | 1.33 | [1.04, 1.71] |
| 2023 | 20.3 | 16.6 | .11 | 1.22 | [0.96, 1.57] |
Male patients had significantly higher PE positivity rates in 2020 and 2022. No significant difference in PE positivity rates between male and female patients in 2023.
CI = confidence interval, CTPA = computed tomography pulmonary angiography, PE = pulmonary embolism.
Statistical significance.
3.6. Positivity rate by age
No significant difference was noted in positivity rate for acute PE in elderly inpatients in 2020 to 2023, compared to 2019. In the non-elderly inpatients, positivity rates were significantly higher in 2021, 2022, and 2023, compared to 2019 (Fig. 2B). However, the relative positivity rates between the 2 age groups were not significantly different during any year (Table 6). The positive rates in these age groups with presence or suspicion of pulmonary infection was also not statistically significant in the year 2020 (15.3% in the elderly vs 17.5% in the non-elderly patients; P = .19).
Table 6.
CTPA study positivity rate: differences by age group.
| Year | Elderly CTPA % (%) | Non-elderly CTPA % (%) | P-value | Odds ratio | 95% CI |
|---|---|---|---|---|---|
| 2019 | 16 | 12.8 | .16 | 0.8 | [0.58, 1.1] |
| 2020 | 16.9 | 16.9 | 1 | 1 | [0.75, 1.34] |
| 2021 | 19.9 | 19.3 | .82 | 0.97 | [0.77, 1.22] |
| 2022 | 20.8 | 17.7 | .2 | 0.85 | [0.67, 1.1] |
| 2023 | 19.3 | 17.7 | .5 | 0.92 | [0.72, 1.17] |
No significant difference was noted between PE positivity rates of elderly and non-elderly patients in any year.
CI = confidence interval, CTPA = computed tomography pulmonary angiography, PE = pulmonary embolism.
* Statistical significance.
4. Discussion
PE is recognized as a severe complication associated with COVID-19 infection, leading to higher rates of morbidity and mortality.[8,9] Given that CTPA is the preferred method for diagnosing PE in patients, its utilization experienced a notable increase throughout the COVID-19 pandemic. In their research involving 74,063 European adults prior to the pandemic and 45,397 patients during the pandemic, Kucukceran and Ayranci documented a significant increase in utilization of CTPA up to 8.2%.[3] Similarly, Schulz et al reported increased CTPA usage of up to 61.8% during the pandemic based on an analysis of 1090 cases in the United States.[1]
We also observed a significant increase in CTPA utilization in all the 4 years (2020 to 2023), compared to the prepandemic year 2019. In our study, not only was the overall CTPA study utilization higher, but utilization was also higher in each of the examined individual groups (female, male, elderly, and non-elderly), ascertaining that increase in CTPA study utilization was not sex- or age- specific but more likely directed by the clinical need. We believe this increase in utilization across the different stages of the pandemic appears to be driven by several factors. Initially, clinical decision-making tools like the Wells score and the Pulmonary Embolism Rule-out Criteria (PERC), which are used to evaluate the risk of PE before proceeding to diagnostic imaging, had not been adapted for COVID-19 patients, casting doubt on their effectiveness in this new context.[10,11] Moreover, there is a possibility that the application and positive findings of D-dimer tests, which help in the diagnosis of clotting disorders, might have escalated, although a detailed examination of D-dimer usage and clinical decision-making tools is beyond this study’s scope. Elevated D-dimer levels, which can arise from infections and not just thromboembolic events, exhibit low specificity for acute PE in COVID-19 patients, often leading to its use as an indicator of the severity of COVID-19 rather than solely for detecting thromboembolic diseases.[12–14] This complexity most likely placed additional pressure on healthcare providers to use CTPA studies for COVID-19 patients amid the pandemic’s evolution.
While the utilization of CTPA studies during the various phases of the pandemic were reported to be unequivocally high, there is substantial disagreement in literature on the positivity rate for acute PE. In a small retrospective single-center study of 62 patients, Kaminetzky et al found increased incidence of PE during the pandemic.[15] In a study involving 1090 cases, Schulz et al reported no significant increase in incidence of PE.[1] In our study, we note an overall increased rate of PE in 2020 to 2023, compared to 2019. Analysis of 3358 patients by Freund et al[16] and analysis of 1090 cases by Schulz et al[1] noticed no significant association of COVID-19 infection with an increased risk of PE. Interestingly, Low et al found that patients with pulmonary infection (including COVID-19) are more likely to have a negative CTPA study, which they postulated was likely due to the publication of several studies that demonstrated association between COVID-19 infection and thrombosis.[17] While we did not specifically stratify our patients by pulmonary infection in the entire timeline, we did not find a significant difference between CTPA positivity rates in the year 2020 in the elderly and the non-elderly patients with known or suspected pulmonary infection.
Research has consistently shown a higher occurrence of PE in men than in women and our findings confirm this observation.[18,19] The salient mechanism proposed to explain this behavior was the difference in adaptive immune systems in the sexes, with females producing more antiviral cytokine type 1 interferon than male patients.[18] The correlation between age and PE has been found to be only slight at the most,[20,21] and our results also confirm this finding.
It is interesting to note that in a study conducted by a group from our institution (of which several members are also part of the current study), there was no significant difference in utilization or positivity rates in CTPA examinations in the emergency department patients.[22] This is fundamentally different from the findings in the current study which saw increased utilization and positivity rates of CTPA examinations at the end of the pandemic in the inpatients. While an elaborate comparison of possible contributory factors is beyond the scope of the current study, we agree with Lutsey et al in that outpatient cases generally represent patients with fewer comorbidities and healthier patients are usually managed on an outpatient basis rather than as inpatients.[23]
5. Limitations
This study has some limitations. It is a retrospective review of data from a single institution. Institutional policies affecting patient care during the COVID-19 pandemic were not fully analyzed. Patient factors such as active infections including COVID-19, comorbidities, etc, were not fully examined. Utilization of PE risk scoring tools and D-dimer testing prior to CTPA being ordered were not examined. Extradepartmental factors such as availability and safety of patient transportation and availability of support during the pandemic were not evaluated. Future studies are needed to establish postpandemic normalization after 2023.
During the preparation of this work, the authors used ChatGPT v4 in order to improve the readability. After using this tool/service, the authors reviewed and edited the content as needed and takes full responsibility for the content of the publication.
6. Interpretation
We found that the utilization and positivity rates of CTPA studies in inpatients remains high at the end of the COVID-19 pandemic public health emergency. Future studies are needed to examine these rates and the long-term consequences.
Author contributions
Conceptualization: Vamshi K. Mugu.
Data curation: Vamshi K. Mugu.
Formal analysis: Vamshi K. Mugu.
Investigation: Vamshi K. Mugu.
Methodology: Vamshi K. Mugu.
Project administration: Ashish Khandelwal.
Resources: Ashish Khandelwal.
Software: Vamshi K. Mugu.
Supervision: Riddhi S. Parikh, Brendan M. Carr, Ashish Khandelwal.
Validation: Vamshi K. Mugu, Riddhi S. Parikh, Brendan M. Carr, Ashish Khandelwal.
Visualization: Vamshi K. Mugu.
Writing – original draft: Vamshi K. Mugu, Ashish Khandelwal.
Writing – review & editing: Vamshi K. Mugu, Riddhi S. Parikh, Brendan M. Carr, Ashish Khandelwal.
Supplementary Material
Abbreviations:
- COVID-19
- coronavirus disease 2019
- CTPA
- computed tomography pulmonary angiography
- IRB
- institutional review board
- PE
- pulmonary embolism
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Supplemental Digital Content is available for this article.
How to cite this article: Mugu VK, Parikh RS, Carr BM, Khandelwal A. CT pulmonary angiography in the inpatients: A 5-year retrospective view at the end of COVID-19 public health emergency. Medicine 2024;103:45(e40351).
Contributor Information
Riddhi S. Parikh, Email: Parikh.Riddhi@mayo.edu.
Brendan M. Carr, Email: Carr.Brendan@mayo.edu.
Ashish Khandelwal, Email: Khandelwal.Ashish@mayo.edu.
References
- [1].Schulz K, Mao L, Kanne J. Computed tomography pulmonary angiography utilization in the emergency department during the COVID-19 pandemic. J Thorac Imaging. 2022;37:225–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Soffer S, Klang E, Shimon O, et al. Deep learning for pulmonary embolism detection on computed tomography pulmonary angiogram: a systematic review and meta-analysis. Sci Rep. 2021;11:15814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Küçükceran K, Ayranci MK. The effect of a pandemic on computed tomography pulmonary angiography results and utilize in the emergency department. Clin Exp Health Sci. 2022;12:280–4. [Google Scholar]
- [4].Burki T. WHO ends the COVID-19 public health emergency. Lancet Respir Med. 2023;11:588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Xavier Becerra. Statement on End of the COVID-19 Public Health Emergency. https://www.hhs.gov/about/news/2023/05/11/hhs-secretary-xavier-becerra-statement-on-end-of-the-covid-19-public-health-emergency.html. Accessed November 14, 2023. [Google Scholar]
- [6].Martín-Sánchez FJ, Martínez-Sellés M, Molero García JM, et al. Insights for COVID-19 in 2023. Rev Esp Quimioter. 2023;36:114–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].The Lancet. The COVID-19 pandemic in 2023: far from over. Lancet. 2023;401:79. [DOI] [PubMed] [Google Scholar]
- [8].Suh YJ, Hong H, Ohana M, et al. Pulmonary embolism and deep vein thrombosis in COVID-19: a systematic review and meta-analysis. Radiology. 2021;298:E70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].The Lancet Haematology. COVID-19 coagulopathy: an evolving story. Lancet Haematol. 2020;7:e425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Franco-Moreno AI, Bustamante-Fermosel A, Ruiz-Giardin JM, Muñoz-Rivas N, Torres-Macho J, Brown-Lavalle D. Utility of probability scores for the diagnosis of pulmonary embolism in patients with SARS-CoV-2 infection: a systematic review. Rev Clin Esp (Barc). 2023;223:40–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kirsch B, Aziz M, Kumar S, et al. Wells score to predict pulmonary embolism in patients with coronavirus disease 2019. Am J Med. 2021;134:688–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lippi G, Bonfanti L, Saccenti C, Cervellin G. Causes of elevated D-dimer in patients admitted to a large urban emergency department. Eur J Intern Med. 2014;25:45–8. [DOI] [PubMed] [Google Scholar]
- [13].Ozen M, Yilmaz A, Cakmak V, et al. D-dimer as a potential biomarker for disease severity in COVID-19. Am J Emerg Med. 2021;40:55–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zhan H, Chen H, Liu C, et al. Diagnostic value of D-dimer in COVID-19: a meta-analysis and meta-regression. Clin Appl Thromb Hemost. 2021;27:10760296211010976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kaminetzky M, Moore W, Fansiwala K, et al. Pulmonary embolism at CT pulmonary angiography in patients with COVID-19. Radiol Cardiothorac Imaging. 2020;2:e200308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Freund Y, Drogrey M, Miró O, et al. ; the IMPROVING EMERGENCY CARE FHU Collaborators. Association between pulmonary embolism and COVID-19 in emergency department patients undergoing computed tomography pulmonary angiogram: the PEPCOV international retrospective study. Acad Emerg Med. 2020;27:811–20. [DOI] [PubMed] [Google Scholar]
- [17].Low CL, Kow RY, Abd Aziz A, et al. Diagnostic yield of CT pulmonary angiogram in the diagnosis of pulmonary embolism and its predictive factors. Cureus. 2023;15:e40484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Peckham H, de Gruijter NM, Raine C, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11:6317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wilcox T, Smilowitz NR, Seda B, Xia Y, Hochman J, Berger JS. Sex differences in thrombosis and mortality in patients hospitalized for COVID-19. Am J Cardiol. 2022;170:112–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Xie J, Tong Z, Guan X, Du B, Qiu H. Clinical characteristics of patients who died of coronavirus disease 2019 in China. JAMA Netw Open. 2020;3:e205619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gómez CA, Sun CK, Tsai IT, et al. Mortality and risk factors associated with pulmonary embolism in coronavirus disease 2019 patients: a systematic review and meta-analysis. Sci Rep. 2021;11:16025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Mugu VK, Carr BM, Olson MC, Khandelwal A. CT pulmonary angiography in the emergency department: utilization and positivity rates during various phases of the COVID-19 pandemic. Emerg Radiol. 2024;31:293–301. [DOI] [PubMed] [Google Scholar]
- [23].Lutsey PL, Walker RF, MacLehose RF, et al. Inpatient versus outpatient acute venous thromboembolism management: trends and postacute healthcare utilization from 2011 to 2018. J Am Heart Assoc. 2021;10:e020428. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.