ABSTRACT
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) syndrome is a rare central nervous system inflammatory disorder with an unknown pathophysiology. We present the case of a 51‐year‐old female exhibiting clinical and radiological features consistent with CLIPPERS syndrome. She manifested diplopia, vertigo, gait ataxia, and lower limb asthenia, accompanied by impaired tandem gait, right sixth nerve palsy, and coarse horizontal nystagmus during the physical examination. Magnetic resonance imaging (MRI) revealed punctate and curvilinear lesions centered in the pons. Treatment with glucocorticoids resulted in significant clinical improvement, and the patient was discharged with a maintenance dose of prednisolone. Throughout a four‐year follow‐up period, the patient remained symptom‐free without any relapses using the low‐dose corticosteroid. The CLIPPERS syndrome diagnosis remains challenging, but recent evidence supports an autoimmune pathogenesis. Although corticosteroid treatment has shown significant clinical improvement, there are no established guidelines or clinical trials on the optimal therapeutic regimen. Despite its rarity, clinicians should consider CLIPPERS syndrome in patients with compatible clinical and radiological features to prevent irreversible neurological damage.
Keywords: CLIPPERS, CNS autoimmune disease, corticosteroid therapy, magnetic resonance imaging
1. Introduction
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) syndrome is a rare central nervous system inflammatory disorder primarily affecting the brainstem, notably the pons. First described by Pittock et al. in 2010 [1], the pathophysiology of CLIPPERS remains unknown, although studies have revealed significant clinical, radiological, and pathological insights.
Clinical onset symptoms often include gait ataxia, diplopia, and dysarthria, with gait ataxia being the most prevalent initial symptom observed in three out of five patients. Subsequently, it manifested in all five patients during follow‐up [2]. Magnetic resonance imaging (MRI) depicts a distinctive pattern of punctate and curvilinear lesions centered in the pons and cerebellum. These lesions typically measure between 1 and 3 mm, with a trend of decreasing size as the distance from the pons increases [1]. Although specific pathologic findings are lacking, biopsies of the pons and cerebellum have demonstrated perivascular infiltration of CD3‐reactive T lymphocytes and CD20‐positive B lymphocytes in the white matter [1]. Despite the uncertainty in findings and an unknown pathogenesis, CLIPPERS patients exhibit a dramatic response to immunosuppressive treatment. This study aims to present the long‐term follow‐up outcomes of a CLIPPERS patient and provide a review of the current literature. To the best of our knowledge, this is one of the longest follow‐up periods (50 months) reported in the literature regarding CLIPPERS response to glucocorticoid treatment.
2. Case Presentation
2.1. Case History
A 51‐year‐old female was admitted to our hospital on March 2, 2020, presenting symptoms over the preceding 3 weeks, including diplopia and deviation of the right eye, vertigo, gait ataxia, and lower limb weakness. Physical examination revealed impaired tandem gait, right sixth nerve palsy, noticeable coarse horizontal nystagmus, and a positive Babinski's sign. The peripheral nervous system was intact. Also, additional symptoms like fever, B symptoms, extracerebral organ manifestations, and meningism were absent in the patient. The patient did not report any history of autoimmune or neurological disease in the first‐degree relatives.
2.2. Methods
Serum antibodies against aquaporin‐4 water channel (neuromyelitis optica immunoglobulin G; NMO‐IgG) and myelin oligodendrocyte glycoprotein immunoglobulin G (MOG‐IgG) were assessed, yielding negative results. CSF analysis was negative for oligoclonal bands (OCBs), and no pleocytosis was observed in CSF. T2‐weighted and Gd‐contrast brain MRI revealed multiple hyperintense punctate and curvilinear lesions centered in the pons (Figures 1 and 2).
FIGURE 1.
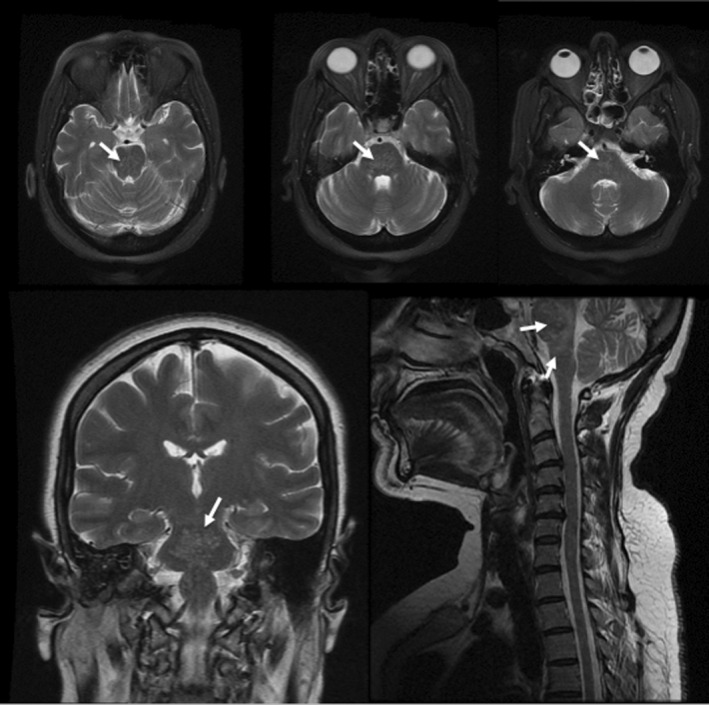
Initial MRI was performed, and multiple hyperintense punctate and curvilinear lesions (white arrows) were revealed in T2 weighted brain MRI in axial, coronal, and sagittal sequences suggestive of chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS).
FIGURE 2.
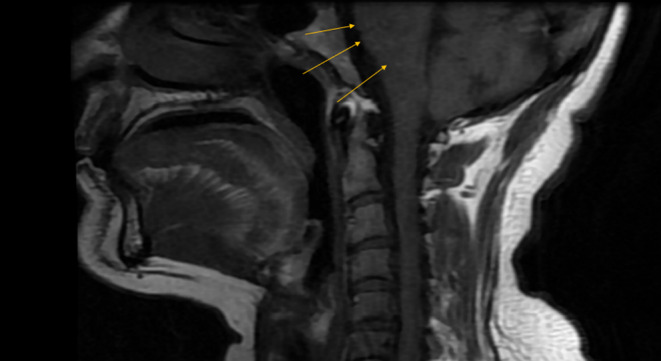
Brain T1 Gd‐enhanced MRI showing hyperintensities in the pons (indicating CLIPPERS).
Treatment commenced with intravenous Methylprednisolone at a daily dose of 1 g for 5 days, followed by oral prednisolone (75 mg daily). With substantial symptom improvement, the patient was discharged, maintaining a daily dose of 5 mg of prednisolone.
2.3. Conclusion and Results
Over 4 years of follow‐up (March 2020 to May 2024), continuous clinical symptoms and serial MRI assessment revealed no instances of relapse or recurrence of CLIPPERS and significant improvement of abnormal gadolinium enhancement in MRI. Consequently, the patient's treatment regimen with a prednisolone dose of 5 mg was maintained. Regarding side effects, the patient experienced mild corticosteroid‐related side effects (such as weight gain and hyperglycemia) during the initial high‐dose treatment phase, but these were well managed, and no significant adverse effects were observed with the low‐dose maintenance therapy.
3. Discussion
Thirteen years after the initial report of CLIPPERS, its underlying pathogenesis remains elusive. However, recent evidence is shedding light on the potential autoimmune nature of this condition, aligning with established mechanisms. With this hypothesis in mind, the pathogenesis of CLIPPERS can be categorized into three plausible mechanisms [3]. The theory of organ‐specific autoimmunity posits the concentration of autoimmune agents in perivascular areas elicits an inflammatory response. This concept is supported by findings from Pittock et al. [1]. Another hypothesis implicates the dysfunction of regulatory T cells triggered by viral infections, particularly the Epstein–Barr virus [4, 5]. Mele et al. [6] contributed to the third hypothesis, underscoring the pivotal role of TH17 immune cells in perivascular lymphocyte infiltration in CLIPPERS syndrome. Additionally, some evidence supports the notion of CLIPPERS having premalignant characteristics [7, 8].
Despite advancements in understanding CLIPPERS syndrome, its diagnosis remains a formidable challenge. Considering the pathophysiology of CLIPPERS, Tobin et al. [9] proposed a set of diagnostic criteria for the syndrome; as follows. the diagnostic criteria encompassed a triad of clinical, MRI, and neuropathological features: clinical features include (i) subacute pontocerebellar dysfunction, (ii) corticosteroid therapy responsiveness of symptoms, (iii) absence of peripheral nervous system disease and, (iv) lack of better diagnosis for clinical presentation explanation. MRI features in Tobin's criteria include, (i) homogenous, gadolinium‐enhancing nodular lesions in pons and cerebellum, measuring less than 3 mm in diameter, (ii) significant improvement in abnormal gadolinium enhancement with corticosteroid treatment, (iii) homogenous abnormal T2 signal does not remarkably exceed the area of post‐gadolinium enhancement in size, and (iv) spinal cord lesions with similar T2 signal and gadolinium enhancement pattern. Neuropathological features encompass following: (i) perivascular predominance and parenchymal infiltration of dense lymphocytic inflammation in either white or gray matter, (ii) T cells predominating infiltration with a higher CD4 than CD8 and varying macrophage components, (iii) The absence of myelin loss or focal secondary myelin loss, and (iv) The absence of an alternative explanation for pathological presentation.
Taieb et al. conducted a study involving 42 patients, with an average follow‐up of 50 months, based on Tobin et al.'s 2017 criteria [10]. The diagnostic criteria encompassed a triad of clinical, MRI, and neuropathological features. Patients were classified into three groups: non‐CLIPPERS (11 patients), definite CLIPPERS (11 patients), and probable CLIPPERS (20 patients). Following the 50‐month follow‐up, the initial diagnosis changed for 2 patients (one from definite CLIPPERS to probable CLIPPERS, and vice versa), yielding a sensitivity and specificity of 69% and 93%, respectively, for the proposed criteria. All clinical and MRI criteria were met in our case, but the neuropathological investigation was not available, making it a probable CLIPPERS case. As we mentioned, the negative results of NMO‐IgG and MOG‐IgG besides the absence of OCBs in CSF during the follow‐ups will be more diagnostic of CLIPPERS over demyelinating diagnoses such as seropositive neuromyelitis optica spectrum disorder (NMOSD), myelin oligodendrocyte glycoprotein antibody disease (MOGAD), and multiple sclerosis (MS). Also, our case did not meet any red flags such as (i) inadequate response to glucocorticoids, (ii) absence of common symptoms or existing additional symptoms like fever, B symptoms, extracerebral organ manifestations, and meningism, (iii) MRI findings revealing spared brainstem, or existence of pontine lesions with necrosis that are suggestive of primary CNS lymphoma, and space‐occupying lesions suggestive of tumors, and (iv) the existence of abnormal cells or pleocytosis [11]. However, in this case, the remarkable response to corticosteroid therapy in 4 years of follow‐up making is highly suggestive of CLIPPERS.
The nomenclature of CLIPPERS suggests a treatment approach grounded in corticosteroids. Pittock et al. utilized intravenous glucocorticosteroids (1 g daily for 5 days of methylprednisolone) in seven patients and oral glucocorticosteroids (80 mg daily prednisone) in one patient [1]. Remarkably, clinical symptoms exhibited marked improvement within 2 to 4 days of intravenous methylprednisolone administration, although the patient receiving oral prednisolone did not show similar progress [1]. Taieb et al., on the other hand, advocated for the prescription of high‐dose intravenous methylprednisolone (ranging from 500 mg to 1 g for up to 10 days), followed by oral prednisone (1 mg/kg/day) with gradual tapering. Notably, no instances of relapse were reported when the corticosteroid maintenance dose exceeded 20 mg/day [12], which aligns with our findings; however, our case did not exhibit any signs of relapses during the low‐dose (5 mg daily) corticosteroid therapy. As of now, no established guidelines or clinical trials exist for the therapeutic regimen of CLIPPERS; treatment is primarily informed by case reports and accumulated experiences.
Although CLIPPERS is a relatively rare disorder, its significant response to treatment underscores the importance of an accurate diagnosis to prevent irreversible damage.
Author Contributions
Masoud Etemadifar: conceptualization, investigation, methodology, resources, supervision, writing – review and editing. Seyyed‐Ali Alaei: investigation, methodology, writing – original draft. Zahra‐Sadat Mirian: investigation, writing – review and editing. Mahdi Norouzi: writing – original draft, writing – review and editing.
Ethics Statement
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgments
The authors express their gratitude to the patient for allowing the publication of her anonymized case.
Funding: The authors received no specific funding for this work.
Data Availability Statement
The authors have nothing to report.
References
- 1. Pittock S. J., Debruyne J., Krecke K. N., et al., “Chronic Lymphocytic Inflammation With Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS),” Brain: A Journal of Neurology 133, no. 9 (2010): 2626–2634. [DOI] [PubMed] [Google Scholar]
- 2. Simon N. G., Parratt J. D., Barnett M. H., et al., “Expanding the Clinical, Radiological and Neuropathological Phenotype of Chronic Lymphocytic Inflammation With Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS),” Journal of Neurology, Neurosurgery, and Psychiatry 83, no. 1 (2012): 15–22. [DOI] [PubMed] [Google Scholar]
- 3. Cao L., Liu M., Guo L., Li M., Xu M., and Wang R., “The Pathogenesis Hypothesis and Research Progress of CLIPPERS: A Literature Review,” Medicine 102, no. 11 (2023): e33211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Xu D., Fu J., Jin L., et al., “Circulating and Liver Resident CD4+CD25+ Regulatory T Cells Actively Influence the Antiviral Immune Response and Disease Progression in Patients With Hepatitis B,” Journal of Immunology 177, no. 1 (2006): 739–747. [DOI] [PubMed] [Google Scholar]
- 5. Weng C. F., Chan D. C., Chen Y. F., Liu F. C., and Liou H. H., “Chronic Hepatitis B Infection Presenting With Chronic Lymphocytic Inflammation With Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS): A Case Report,” Journal of Medical Case Reports 19, no. 9 (2015): 266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mélé N., Guiraud V., Labauge P., Oppenheim C., Mas J. L., and Taieb G., “Effective Antituberculous Therapy in a Patient With CLIPPERS: New Insights Into CLIPPERS Pathogenesis,” Neurol Neuroimmunol Neuroinflammation 1, no. 1 (2014): e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Doubrovinskaia S., Sahm F., Thier M. C., et al., “Primary CNS Lymphoma After CLIPPERS: A Case Series,” Journal of Neurology, Neurosurgery, and Psychiatry 92, no. 12 (2021): 1348–1349. [DOI] [PubMed] [Google Scholar]
- 8. Lin A. W., Das S., Fraser J. A., et al., “Emergence of Primary CNS Lymphoma in a Patient With Findings of CLIPPERS,” Canadian Journal of Neurological Sciences 41, no. 4 (2014): 528–529. [DOI] [PubMed] [Google Scholar]
- 9. Tobin W. O., Guo Y., Krecke K. N., et al., “Diagnostic Criteria for Chronic Lymphocytic Inflammation With Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS),” Brain: A Journal of Neurology 140, no. 9 (2017): 2415–2425. [DOI] [PubMed] [Google Scholar]
- 10. Taieb G., Mulero P., Psimaras D., et al., “CLIPPERS and Its Mimics: Evaluation of New Criteria for the Diagnosis of CLIPPERS,” Journal of Neurology, Neurosurgery, and Psychiatry 90, no. 9 (2019): 1027–1038. [DOI] [PubMed] [Google Scholar]
- 11. Galazky I., Büntjen L., Voges J., Sandalcioglu I. E., Mawrin C., and Haghikia A., “Brain Biopsy in Patients With CLIPPERS Syndrome: Why and When? A Case Report and Literature Review,” Therapeutic Advances in Neurological Disorders 1, no. 15 (2022): 17562864211062821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Taieb G., Allou T., and Labauge P., “Therapeutic Approaches in CLIPPERS,” Current Treatment Options in Neurology 19, no. 5 (2017): 17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors have nothing to report.


