Summary
Von Hippel-Lindau is a rare genetic disease that is inherited as an autosomal dominant pattern. Characteristics of this disease include multiple vascularised tumours, particularly cerebellar, retinal and/or visceral. The disease can occur at any age with retinal haemangioblastomas as one of the earliest manifestations. The gold-standard investigation for cerebral haemangioblastomas is MRI or cerebral CT and for retinal haemangioblastomas is fluorescein angiography. We present the case of a woman in her late 30s who reported a primary concern of diminished vision in both eyes for the past 6 months. Fundus examination revealed blurred disc margins, optic nerve head haemangioblastomas and peripheral retinal haemangioblastomas in both eyes. Blood investigations showed polycythaemia. A 24-hour urine protein report showed increased levels. MRI showed multiple cystic lesions in the posterior fossa, on the right optic nerve in the optic canal, multiple cortical cysts in both kidneys and a soft tissue space-occupying lesion.
Keywords: von Hippel-Lindau Disease, Hemangioblastoma, Magnetic Resonance Imaging, Ophthalmology, Retina
Background
Von Hippel-Lindau (VHL) is a rare genetic disease that is inherited as an autosomal dominant pattern.1 This disease was characterised independently by Von Hippel in 19112 and Lindau in 1926.3 Its incidence is about 1 in every 36 000 live births.4 For this disease to occur, the VHL gene which is situated on the short arm of chromosome 3, undergoes mutation in both of its alleles.5 Characteristics of this disease include multiple vascularised tumours, particularly cerebellar, retinal and/or visceral. The disease can occur at any age with retinal haemangioblastomas (RHs) as one of the earliest manifestations.6
Case presentation
A woman in her late 30s visited the outpatient department (OPD) at our medical college, presenting with decreased vision in both eyes, with the right eye affected more than the left, over the past 6 months. There was a history of brain surgery (cyst resection) done 7 years ago. There was no history of trauma. In her family history, her brother suffered from similar complaints and died 4 years ago in his late 20s. She has five children, ranging in age from early adolescence to early 20s, none of whom have experienced similar symptoms.
On examination, the patient’s Glasgow Coma Scale (GCS) score was 15/15.
Ophthalmic examination details are provided in table 1.
Table 1. Ophthalmic examination.
| Right eye | Left eye | |
| Vision | Finger count close to face | 6/9 |
| Conjunctiva | Normal | Normal |
| Cornea | Bright and clear | Bright and clear |
| Anterior chamber | Normal depth | Normal depth |
| Iris | Normal pattern | Normal pattern |
| Pupil | Round, regular and reactive | Round, regular and reactive |
| Lens | Clear | Clear |
| Extraocular movements | Full | Full |
| Intraocular pressure | Cannot be assessed | Cannot be assessed as the patient was uncooperative |
| Fundus | PapilloedemaCup disc ratio cannot be assessed, optic nerve head haemangioblastoma, pseudohole near macular region, Erm temporal to disc | PapilloedemaCup disc ratio cannot be assessed, optic nerve head haemangioblastoma, foveal reflex was present, 1 haemangioblastoma inferotemporally to disc |
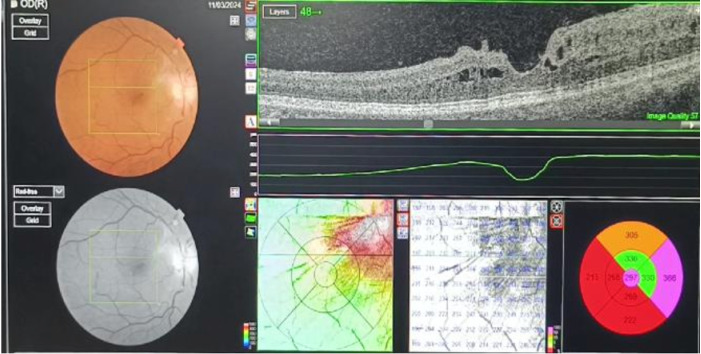
Fundus of the left eye shows blurred disc margins (papilloedema) with optic nerve head (ONH) haemangioblastoma and peripheral RH (inferotemporal to disc) (figures1 2). Fundus of the right eye shows blurred disc margins (papilloedema) with ONH haemangioblastoma and epiretinal membrane with pseudohole (figures3 4).
Figure 1. Fundus of the left eye shows papilloedema and haemangioblastomas on the optic nerve head and inferotemporal to the optic disc.
Figure 2. Posterior pole of left eye with haemangioblastoma inferotemporal to disc.
Figure 3. Fundus of the right eye shows papilloedema with optic nerve head haemangioblastoma and epiretinal membrane with pseudohole temporal to disc.
Figure 4. Optical coherence tomography shows pseudohole at the posterior pole temporal to disc near the macular region.
Investigations
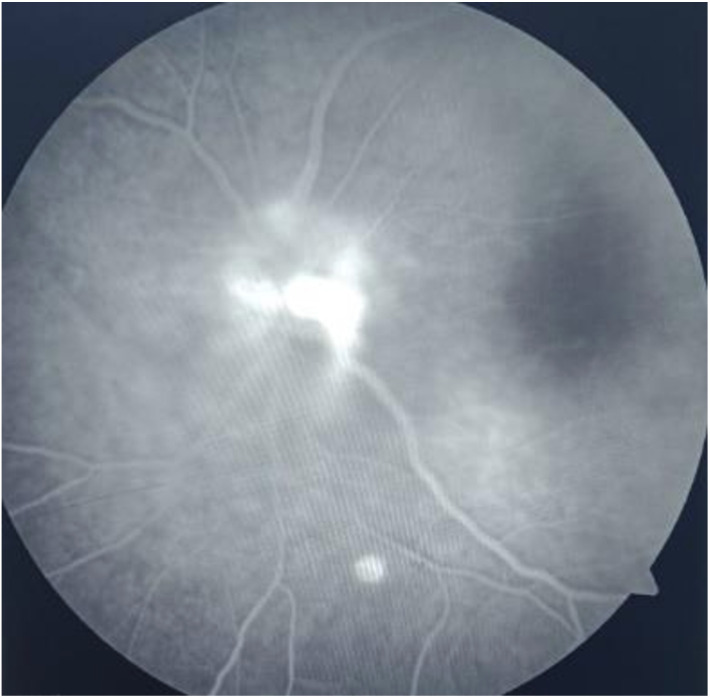
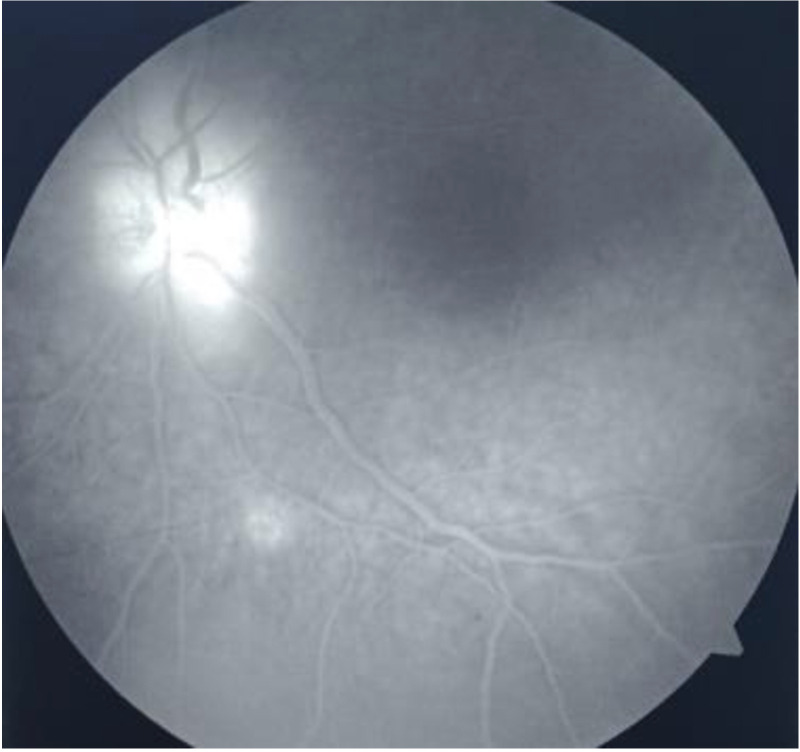
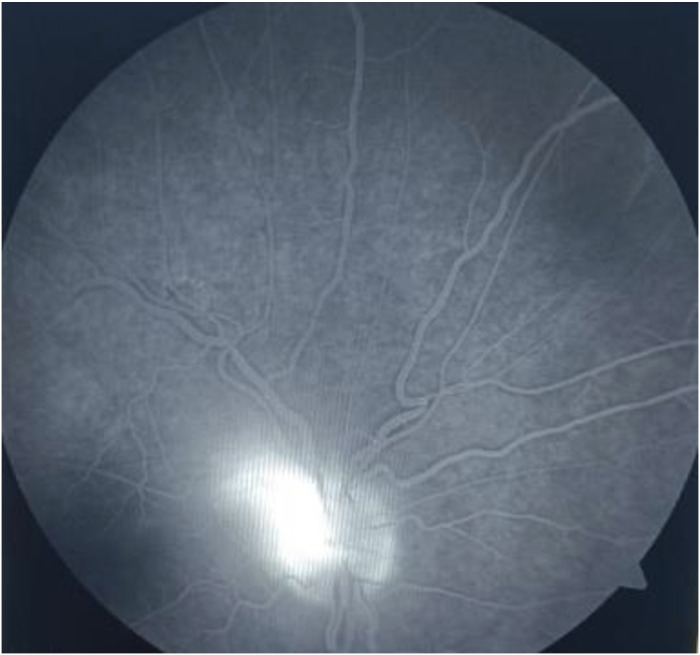
Fundus Fluorescein Angiography (FFA) : (a) Early-phase angiography of a typical RH with feeder vessels shows hyperfluorescence (figures5 6) and (b) hyperfluorescence increases in intensity and size in the late phase (figures7 8).
Figure 5. FFA shows hyperfluorescence of the optic nerve head and retinal haemangioblastoma in the early phase in the left eye.
Figure 6. FFA shows hyperfluorescence of optic nerve head haemangioblastoma in the early phase in the right eye.
Figure 7. FFA shows hyperfluorescence of the optic nerve head and retinal haemangioblastoma in the late phase in the left eye.
Figure 8. FFA shows hyperfluorescence of optic nerve head haemangioblastoma in the late phase in the right eye.
Blood investigations
Blood investigations reveal polycythaemia7 with haemoglobin levels of 174 g/L, Red blood cell count (RCC) of 6.86× 10¹²/L, White blood cell count (WCC) of 11.3 × 10⁹/L, Mean corpuscular haemoglobin (MCH) of 25.4 pgm and Mean corpuscular volume (MCV) of 74.7 fL.
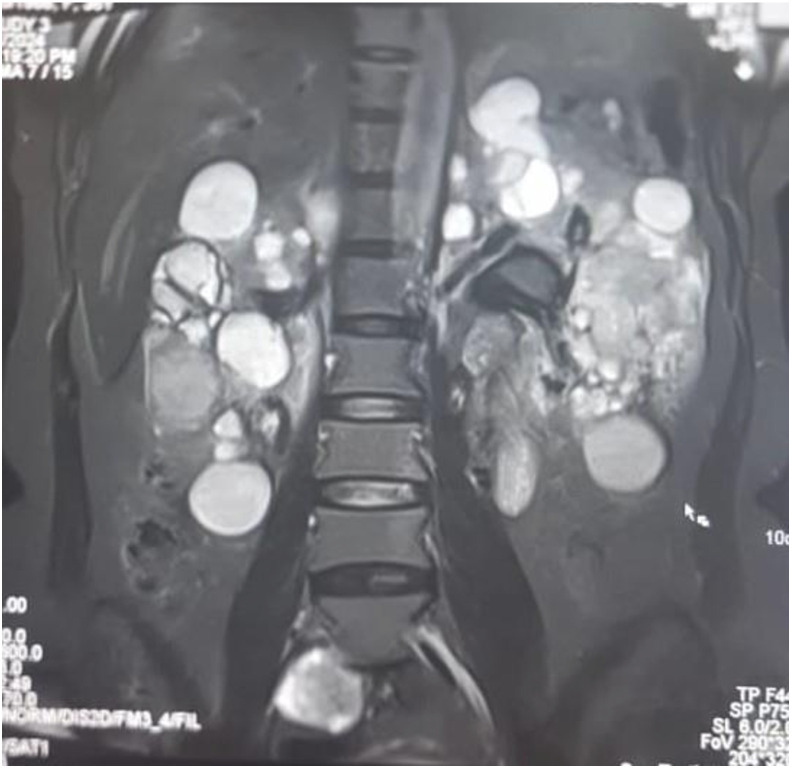
A 24-hour urine protein report showed increased levels of 624.6 mg/24 hours. A renal Doppler ultrasound showed bilateral corticomedullary cysts with no evidence of significant renal artery stenosis. A 24-hour urine/plasma catecholamines and metanephrines were advised but were unavailable at our tertiary healthcare centre.
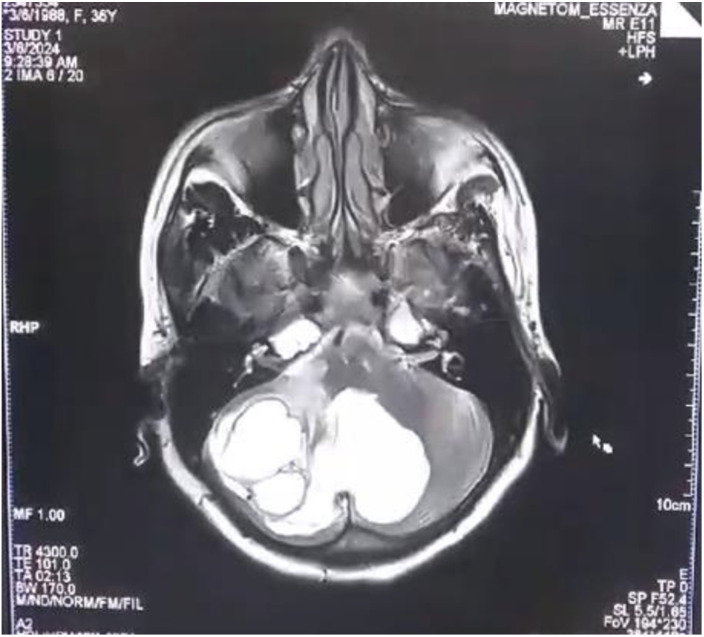
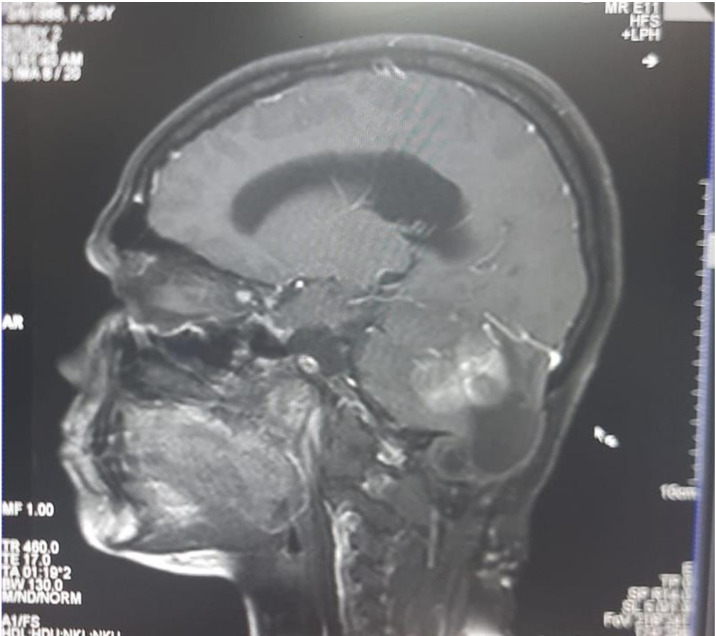
MRI: MRI of the head showed multiple cystic space-occupying lesions in the posterior fossa (figure 9) and a well-circumscribed mass on the right optic nerve in the optic canal (figure 10). Since we suspected it to be a VHL disease, the most probable diagnosis was thought to be an optic nerve haemangioblastoma. MRI also showed bilateral enlarged kidneys with variable sized cortical cysts and a soft tissue space-occupying lesion in the mid part of left kidney (figure 11). A soft tissue lesion in the retroperitoneum, located in the right paramedian aspect of the L5 vertebra, is suggestive of an extra-adrenal pheochromocytoma.
Figure 9. MRI shows multiple cystic lesions in the posterior fossa.
Figure 10. MRI shows right optic nerve haemangioblastoma in the optic canal.
Figure 11. MRI shows bilaterally enlarged kidneys with variable sized cortical cysts and extra-adrenal pheochromocytoma.
Differential diagnosis
The differential diagnosis of retinal capillary haemangiomas includes retinal macroaneurysms, and retinal vasoproliferative tumours, racemose haemangioma, retinal cavernous haemangioma, coats disease and Wyburn-Mason syndrome. The absence of a prominent feeder vessel leading to the lesion is the main distinguishing characteristic between retinal capillary haemangiomas and all these other entities.
As genetic testing was not available at our centre, the diagnosis of VHL was based on the criteria: a positive family history with one or more typical lesions and the investigations performed.
Treatment
Laser photocoagulation was planned for RHs. Her family was counselled regarding the examination of her five children and the recommendation for genetic testing. For brain and spinal lesions, the patient was referred to a neurosurgeon.
Outcome and follow-up
The patient did not seek treatment as advised, then later on followed up after a few months with worsening of vision in both eyes, Perception of Light (PL) +, Projection of Rays (PR) accurate in all quadrants in the right eye and finger count close to face in the left eye.
Discussion
RHs are ocular manifestations of VHL disease. This vascular retinal tumour was first described by Eugen von Hippel between 1867 and 1939.8 The term retinal angiomatosis was adopted as the description of the vascular nature of the disease was more detailed.2 9 10 Early detection and treatment is highly beneficial in symptomatic RH cases as the risk of progression to blindness is high in the11,13. The diagnosis is strongly suspected or even confirmed by the fundus aspect of the tumours. Haemangioblastomas involving the ONH in a VHL disease are rare findings and only a few cases have been reported.14 The gold-standard investigation for cerebral haemangioblastomas, which are most often associated with ocular involvement, is MRI or cerebral CT. For small angiomas, juxtapapillary angiomas and angiomas obscured by epiretinal membranes, fluorescein angiography is the preferred diagnostic tool. Optic nerve haemangioblastoma is an uncommon finding and is mostly associated with VHL disease and only a few cases have been reported.15 Laser photocoagulation is the basic treatment for small peripheral retinal angiomas16 17 while larger lesions can be treated with brachytherapy or cryotherapy.18 19
Learning points.
A multidisciplinary approach is often required in the management of Von Hippel-Lindau disease patients, as in this disease, multiple tumours occur in various organs of the body which leads to various manifestations and its associated complexities.
The role of the ophthalmologist is important in the management of this condition since the ocular involvement may be indicative of the disease.
In rare cases like these, early detection cannot only preserve the patient’s vision but also save their life.
Psychological evaluation and counselling of patients and their families should be done.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Consent obtained directly from patient(s).
Contributor Information
Bhupinderjeet Singh, Email: bjeetrandhawa@gmail.com.
Reena Kumari, Email: rkreenakmr09@gmail.com.
Dinesh Kumar Bhagat, Email: dineshbhgt23@gmail.com.
Deeksha Bhatia, Email: deekshabhatia007@gmail.com.
References
- 1.Shuin T, Yamasaki I, Tamura K, et al. Von Hippel-Lindau disease: molecular pathological basis, clinical criteria, genetic testing, clinical features of tumors and treatment. Jpn J Clin Oncol. 2006;36:337–43. doi: 10.1093/jjco/hyl052. [DOI] [PubMed] [Google Scholar]
- 2.Hippel E. Die anatomische Grundlage der von mir beschriebenen sehr seltenen Erkrankung der Netzhaut. Graefe's Arch Ophthalmol. 1911;79:350–77. doi: 10.1007/BF01966371. [DOI] [Google Scholar]
- 3.Lindau A. Studien über Kleinhirncysten. Bau, Pathogenese und Beziehungen zur Angiomatosis retinae. Acta Pathol Microbiol Scand. 1926;1:1–128. [Google Scholar]
- 4.Lefebvre M, Foulkes WD. Pheochromocytoma and paraganglioma syndromes: genetics and management update. Curr Oncol. 2014;21:e8–17. doi: 10.3747/co.21.1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martins R, Bugalho MJ. Paragangliomas/Pheochromocytomas: clinically oriented genetic testing. Int J Endocrinol. 2014;2014:794187. doi: 10.1155/2014/794187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nabih O, Hamdani H, El Maaloum L, et al. Retinal angioma of Von hippel-lindau disease: A case report. Ann Med Surg (Lond) 2022;74:103292. doi: 10.1016/j.amsu.2022.103292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Q, Tong D, Liu G, et al. HIF2A germline-mutation-induced polycythemia in a patient with VHL-associated renal-cell carcinoma. Cancer Biol Ther. 2017;18:944–7. doi: 10.1080/15384047.2017.1394553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hippel E. Über eine sehr seltene Erkrankung der Netzhaut. Graefes Arhiv für Ophthalmologie. 1904;59:83–106. doi: 10.1007/BF01994821. [DOI] [Google Scholar]
- 9.Neumann HP, Wiestler OD. Clustering of features of von Hippel-Lindau syndrome: evidence for a complex genetic locus. Lancet. 1991;337:1052–4. doi: 10.1016/0140-6736(91)91705-y. [DOI] [PubMed] [Google Scholar]
- 10.Webster AR, Maher ER, Bird AC, et al. A clinical and molecular genetic analysis of solitary ocular angioma. Ophthalmology . 1999;106:623–9. doi: 10.1016/S0161-6420(99)90127-6. [DOI] [PubMed] [Google Scholar]
- 11.Webster AR, Maher ER, Moore AT. Clinical characteristics of ocular angiomatosis in von Hippel-Lindau disease and correlation with germline mutation. Arch Ophthalmol. 1999;117:371–8. doi: 10.1001/archopht.117.3.371. [DOI] [PubMed] [Google Scholar]
- 12.Ridley M, Green J, Johnson G. Retinal angiomatosis: the ocular manifestations of von Hippel-Lindau disease. Can J Ophthalmol. 1986;21:276–83. [PubMed] [Google Scholar]
- 13.Salazar FG, Lamiell JM. Early identification of retinal angiomas in a large kindred von Hippel-Lindau disease. Am J Ophthalmol. 1980;89:540–5. doi: 10.1016/0002-9394(80)90063-x. [DOI] [PubMed] [Google Scholar]
- 14.Vásquez Montoya JD, Velez JM, Naranjo Vanegas M, et al. Optic nerve haemangioblastoma in association with von Hippel-Lindau syndrome: case report and literature review. BJR Case Rep. 2024 doi: 10.1093/bjrcr/uaae007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Darbari S, Meena RK, Sawarkar D, et al. Optic Nerve Hemangioblastoma: Review. World Neurosurg. 2019;128:211–5. doi: 10.1016/j.wneu.2019.04.224. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg MF, Koenig S. Argon laser treatment of von Hippel– Lindau retinal angiomas. I. Clinical and angiographic findings. Arch Ophthal. 1974;92:121–5. doi: 10.1001/archopht.1974.01010010127009. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt D, Natt E, Neumann HP. Long-term results of laser treatment for retinal angiomatosis in von Hippel-Lindau disease. Eur J Med Res. 2000;5:47–58. [PubMed] [Google Scholar]
- 18.Welch RB. Von Hippel-Lindau disease: the recognition and treatment of early angiomatosis retinae and the use of cryosurgery as an adjunct to therapy. Trans Am Ophthalmol Soc. 1970;68:367–424. [PMC free article] [PubMed] [Google Scholar]
- 19.Kreusel KM, Bornfeld N, Lommatzsch A, et al. Ruthenium-106 brachytherapy for peripheral retinal capillary hemangioma. Ophthalmology. 1998;105:1386–92. doi: 10.1016/S0161-6420(98)98017-4. [DOI] [PubMed] [Google Scholar]