Abstract
Background:
We aimed to review the effect of community-based health insurance on health-related outcomes in Ethiopia.
Methods:
A systematic review was undertaken utilizing a major relevant published literature review from September 2017 to June 15, 2023. PubMed, Scopus, Web of Science, Science Direct, Google Scholar, Semantic Scholar, EMBASE, ProQuest, Hinari, and the Cochrane Library were used to search for relevant literature. Moreover, the Prisma flow model was used to select eligible findings.
Results:
Overall, 72% of the articles employed cross-sectional comparative study designs and procedures, and 36% of them employed samples ranging in size from 501 to 1000 participants. Furthermore, 76% were studied using descriptive statistics and logistic regression, whereas fewer utilized a random model, a probity model, or a correlation model. Similarly, 32% of the research used two-stage stratified sampling methods, and around 40% of the data revealed that the scheme increased healthcare utilization services. About 72 % of the reviewed study results showed that the scheme reduced catastrophic health expenditure and increases utilization of healthcare services. And the 20% reviewed studies stated that the CBHI boosts household satisfaction level. Moreover 12% of the reviewed studies stated that, CBHI increased QoL (quality of life).
Conclusion:
Most of the studies provide evidence of the positive effect of CBHI in Ethiopia. Mainly, its membership improved the utilization of health services and decreased the incidence of catastrophic health expenditures. Thus, all actors should cooperate to strengthen it to solve the effective attribute of the deprived value of health care and continuity of care delivery system related to the country’s new policy.
Keywords: Community-based health insurance scheme, Health-related outcomes, Systematic review, Ethiopia
Introduction
Health insurance positively affects the quality of life, which measures health interventions’ impact on health-related conditions through medical supply availability and empowering women and children in financial healthcare (1). Ethiopia ranks low compared to other low-income countries in terms of health-related indicators (2). She bears a high burden of preventable communicable diseases. According to the country’s Ministry of Health (2015) report, the top three leading causes of mortality were malaria, pneumonia, and respiratory tract diseases (1, 3, 4). Despite this high burden, utilization of modern healthcare services is limited (3). One of the reasons for the low utilization of healthcare services is the direct user fee charge (5). CBHI is a new method of protecting low-income people’s money against medical disasters. It is becoming increasingly popular as a technique for improving access to primary care for the poor, particularly informal sector.
Health care is too expensive for individuals living in developing nations (6) and millions of its people continue to suffer and die as a result of health-related problems (6–8). To reduce the direct costs of healthcare, a health insurance program should be implemented (9).
CBHI has emerged as an alternative to out-of-pocket healthcare expenditures in low- and middle-income countries (10). Six African countries (Rwanda, Tanzania, Mali, Ghana, Senegal, and Ethiopia) are presently pursuing UHC through CBHI (11, 12). CBHIs promote equity in the healthcare sector by reaching out to those who do not have access to financial protection against healthcare costs. However, implementation-related difficulties lead many schemes to under-perform (13).
CBHI schemes are being implemented in African countries as a crucial risk-mitigation program, aiming to help them transition to universal health care, making them a significant step towards achieving national health insurance coverage (14, 15). The CBHI scheme in sub-Saharan Africa has shown promise in improving healthcare access; however, enrollment and renewal rates remain low (15, 16). CBHI households have higher yearly outpatient visits and are 70% more likely to seek treatment compared to non-CBHI households, while they have lower total yearly out-of-pocket payments at the point of use (17, 18).
Ethiopia’s CBHI enrollment coverage varies by region, with factors influencing family enrollment decisions, but no pooled research exists to inform decision-making on this issue (19, 20). Thus, we aimed to assess the effect of the CBHI scheme on health-related outcomes in Ethiopia.
Methods
We searched studies reporting the effect of community-based health insurance schemes on health-related outcomes in Ethiopia that were published between October 2017 and June 2023. This period is chosen because the present CBHI plan, health-related results, and up-to-date information are necessary to explain and satisfy the review article’s objective. To collect the data/findings the researchers use databases such as PubMed, Scopus, Web of Science, Science Direct, Google Scholar, Semantic Scholar, EMBASE, ProQuest, Hinari, and the Cochrane Library, with supplementary hand searching of references. The online databases contain archives of most English biomedical journals. Scientific papers published online by the Centre for Disease Control and the WHO with the keywords “community-based”, “community-based health insurance scheme”, “Health insurance”, “health-related outcomes”, “utilization of healthcare services”, “catastrophic health expenditure” and “Ethiopia” were also included in this analysis.
We used the Effective Public Health Practice Project Quality Assessment Tool (EPHPP) to grade the quality of the quantitative studies in this review (EPHPP, 2023). Each of the components was given one of three strength ratings: strong, moderate, or weak, which were then put together to establish the total product quality. The papers rated weak are excluded from the review. The quality was assessed by three reviewers and disputes were resolved through dialogue.
Data collection and selection stages
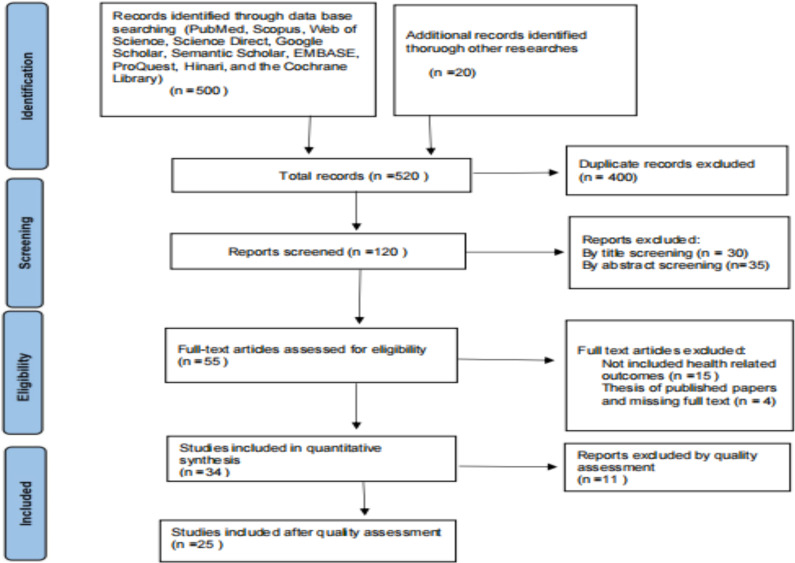
The study team found over 500 publications and reviewed each article’s title, summary, and whole body for relevance and appropriateness. A total of 25 papers were determined to be eligible (Fig. 1).
Fig. 1:
PRISMA Flow Diagram (21)
Inclusion and Exclusion Criteria
We opted to include papers in the review based on criteria such as relevant key instruments to collect raw data, such as media and other information, on the effect of the CBHI scheme on health-related outcomes in Ethiopia. All quantitative and qualitative full papers published from October 2017 to June 2023 and written in English are included. Studies that did not meet these criteria, such as all abstracts, case reports, conference reports, articles without full text, studies with incomplete data and published thesis papers were excluded from the study.
Results
Overview of CBHI in Ethiopia
The Ethiopian government has been striving to develop CBHI for the informal sector to achieve UHC (18). Thirteen rural districts in the country’s four major regions were the first to implement the plan, and the scale-up began in 2015 (22, 23). In just one year, the country’s CBHI adoption rate increased to 41% (24, 25). Ethiopia rates low in terms of access to modern healthcare and a range of other health metrics, and the majority of the nation’s high illness burden is caused by avoidable ailments and diseases (26, 27). Despite the effort, current healthcare services remain underutilized. To be effective, more than 80% of families in rural Ethiopian woredas’ must be covered by CBHI (26, 27).
Key findings from the Reviewed literature
Table 1 shows that out of 25 reviewed studies, 8 (32%) reviewed papers answered the question by assessing the impact of CBHI on health services utilization (6, 20, 28–33). The majority of 18 (72%) of the reviewed studies were conducted using cross-sectional comparative study design and methods to address the research questions (1, 7, 20, 28–42). Five (20%) of the reviewed studies used community-based cross-sectional study design and methods (36, 38, 41, 43, 44). The remaining 3 (12%) are qualitative study design (45–47) and quantitative research design and methods (39, 43, 48). However, only one (4%) of the reviewed studies used a data-layered, structured-based survey study (37).
Table 1:
Characteristics of the individual included studies, Ethiopia (n = 25), 2023.
| Author name Published year | Aim of the study | Study design | Sample size | Study setting | The model used for analysis | Purpose of Model |
|---|---|---|---|---|---|---|
| Bayked etal., 2023(6) | To evaluate the impact of Ethiopia’s CBHI | Systematic review | 23 studies | Ethiopia | Random Model | To measure the effect of estimates |
| Alemayehu et al., 2023a(33) | To assess Health services utilization and financial risk protection | Comparative cross-sectional | 4301 Households | Ethiopia | Logistic regression Model | To measure financial risk protection and Health Services Utilization |
| Asfaw et al., 2022a(41) | investigates the household welfare impact of CBHI | Cross-sectional | 531 households | Chilga District, Amhara Regional State, Central Gondar Zone, Ethiopia | Probit and propensity score matching (PSM) | To measure the impact of CBHI on welfare |
| Mulat et al., 2022(45) | To identify early achievements in scaling up CBHI | Qualitative design | 18 Key informants | Ethiopia | NA | NA |
| Kassa, 2023(30) | to evaluate the impact of CBHI on CHE | Comparative cross-sectional study | 472 households | Kutaber district, Ethiopia. | A probit regression mode | To identify co-variants that affected CBHI scheme participation. |
| Addise et al., 2021 (42) | To assess the magnitude of satisfaction and associated factors | Community based cross-sectional study | 627 households | Nilemo District, Hadiya Zone, Southern Ethiopia | Bivariate and multivariate logistic regression | to determine associations |
| Moyehodie et al., 2022a(28) | To identify factors associated with CBHI, Health Care Service Utilization | community-based cross-sectional study | 619 households | Gonder town, Amhara, Ethiopia | binary logistic regression analyses | To determine association |
| Demissie and Gutema, 2020 (20) | To analyze the effects of a CBHI on healthcare | comparative cross-sectional | 405 household heads | Yirgalem town, southern Ethiopia. | Multivariate logistic regression | To identify the effect of HRQoL |
| Gebru and Lentiro, 2018(1) | to measure the impact of CBHI on HRQoL | comparative community-based cross-sectional | 1964 Households | SNNPR | linear regression analysis | To describe the functional predictors of health-related QoL. |
| Christian, 2017(47) | To establish the impact of the public health project on CBHI performance | Qualitative | 45 staff working for CBHI | Ethiopia | NA | Na |
| Moyehodie et al., 2022b(51) | To identify the individual and community-level factors associated with CBHI enrollment | EDHS | 8663 Households nested and 305 community | nationally representative, Ethiopia | NA | NA |
| Gashaw, 2020(7) | To assess the level of household satisfaction in CBHI | Cross-sectional (Quantitative) | 336 CBHI beneficiaries | Addis Ababa, Ethiopia | NA | NA |
| Abdilwohab et al., 2021(40) | To establish the impact of the public health project on CBHI performance | A community-based cross-sectional | 386 HHs | Addis Ababa | Na | NA |
| Shigute et al., 2020(35) | To measure the impact of CBHI on Health-related quality of life | Comparative community-based cross-sectional | 1964 HHs | Southern Ethiopia | NA | NA |
| Atinafu etal., 2018 (32) | To compare differences in health care utilization between CBHI member and non-member households | Comparative community-based cross-sectional | 652 (326 insured and 326 uninsured) | North-west, Ethiopia | NA | NA |
| Workneh and Woreta, 2017(34) | To assess the compliance of the community to the CBHI scheme | A community-based cross-sectional | 511 respondents | The hudere district, Northwest, Ethiopia | Bivariate and Multivariate logistic regression models | To find associated factors with the outcome variables |
| Mekonen etal., 2018 (29) | investigated the effect of CBHI on catastrophic health expenditure | A community-based cross-sectional | 454 (224 insured and 230 uninsured) | Northeast Ethiopia | A Multi stage sampling technique and propensity score matching | To determine the effect of CBHI on catastrophic health expenditure. |
| Jembere, 2018(31) | To examine access, use and quality of services after the introduction of the scheme in Ethiopia | Cross-sectional | 344 head of HHs | Thehudere district, Northwest, Ethiopia | Statistical test T-test and ANOVA model Pearson correlation | To examine group differences and see the relationship |
| Mitiku Kebede and Geberetsadik, 2019(37) | to assess the level of household satisfaction with the CBHI scheme and associated factors | Cross-sectional study | 528 households | Sheko district; southwest Ethiopia. | logistic regression analyses | To determine the independent predictors of household’s satisfaction with CBHI |
| Fufa etal., 2021(39) | to assess the satisfaction level of the Community for health insurance | A facility-based cross-sectional | 399 patients | Arsi Nagele Woreda Health Centres | logistic regression | To identify determinant factors the satisfaction of CBHI client on the public health service |
| Geferso and Sharo, 2022(48) | to determine community-based health insurance utilization and its associated factors among rural households | A quantitative community-based cross-sectional | 600 households | Akaki District, Oromia special zone surrounding Finfinnee, Oromia, Ethiopia | A binary logistic regression model | to identify the factors associated with CBHI utilization |
| Bantie and Zewdie, 2020(43) | to determine knowledge and attitude levels towards CBHI | community-based cross-sectional | 335 informal workers. | Bahir Dar City | Logistic regression analysis | To identify potential associations between the study variables. |
| Kaso et al., 2022 (44) | assessed the CBHI membership renewal rate | community-based cross-sectional | 537 respondents | Yirga Chafe district, Gedeo zone, Southern Ethiopia | logistic regression model | determine factors associated with the CBHI scheme |
| Girmay and Reta, 2022(38) | To assess CBHI services usage and related factors | Community-based cross-sectional | 652 participants | Gulele Subcity | Logistic regression model | To find associated factors |
| Mussa et al., 2021(53) | To examine CBHI enrollment | Cross-sectional | 5398 PSMP beneficiary households | Ethiopia | Logistics regression model | To identify factors associated with households’ CBHI enrollment decisions |
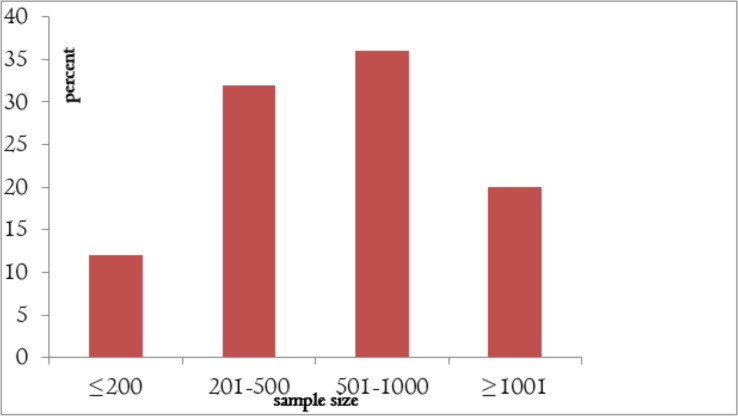
Fig. 2 indicated that the majority 9 (36%) of reviewed studies conducted their research using a sample size between 501 and 1000 participants (28, 32, 34, 37, 38, 41, 42, 44, 48). Followed by 8 (32%) were sample sizes between 201 and 500 participants (7, 20, 29, 30, 39, 40, 43, 46).
Fig. 2:
the percentage of the sample size used to address research questions among 25 examined papers in Ethiopia (2017–2023)
Regarding study setting as shown in Table 1, the majority (32%) of the reviewed studies were conducted at the national level of the country. Followed by 4 (16%) conducted in SNNPR and 3 (12%) were in Addis Ababa, Ethiopia. Two (8%) of the reviewed studies were also conducted in Thehudered District, North East, Ethiopia. and two (8%) were conducted in Chilga District, Amhara Regional State, Ethiopia. The remaining were conducted in Kutaber district, Yirgalem town, Southern, Sheku district, South West, Ethiopia, Arsi-Negle woreda health centre, Akaki District, Oromia Special Zone, Oromia, Ethiopia and Yirga Chafe district, Gedeo zone, Southern Ethiopia.
Table 2 shows that the majority of 8 studies (32%) of reviewed studies used two-stage stratified sampling techniques (1, 7, 28, 33, 34, 40, 47, 49, 50). Followed by 5 (20%) who used multistage sampling techniques (6, 20, 30, 31, 48, 51) and Five (20%) were using simple random sampling (33, 36, 37, 41, 44, 51, 52), four (16%) were purposive sampling techniques (20, 39, 42, 45) and 2 (8%) were systematic sampling techniques technique (38, 43), and 1(4) is mixed method (46).
Table 2:
The sampling technique, data collection, analysis, and key relevant results Ethiopia (n = 25), 2023.
| Author name Published year | Sampling technique | Data collection Instruments | Method of Analysis | Key relevant results |
|---|---|---|---|---|
| Bayked etal., 2023(6) | A multistage sampling technique. | Joana Briggs Institute checklists to assess the risk of bias | Descriptive statistics by using Microsoft Excel and Rev Man-5 | The UHC provided by the scheme was 45.6% |
| Alemayehu etal, 2023a(33) | A multistage sampling technique. | Propensity score matching (PSM) accounts for possible selection bias | Descriptive statistics and Logistic regression (Bivariate and Multivariable) | CBHI membership resulted in a 28–43% reduction in annual OOP payment as compared to non-member households |
| Asfaw etal, 2022(41) | A multistage sampling technique. | The primary data was also collected from observation and key informant interviews Secondary data: published and unpublished documents | Descriptive statistical Econometric analysis approach | The insured households associated with visits increased by 2.6 times, reduced per-capita health expenditure |
| Mulat etal, 2022(45) | Purposive sampling technique | Semi-structured interview guide | directed content analysis (also called deductive content analysis) | CBHI received strong political support and early pilots helped to inform the process of scaling up the scheme. |
| Kassa, 2023(30) | multistage sampling techniques | Household survey questionnaire | propensity score matching analysis: Descriptive and logistic regression | The magnitude of CHE was 39.1% with total household expenditure and 1.8% with non-food expenditure measures among insured households. |
| Addise etal., 2021(42) | stratified sampling and systematic sampling | pre-tested structured questionnaire. | Descriptive statistics, bivariate, and multivariate logistic regression | The magnitude of household heads’ satisfaction was 54.1%. |
| Moyehodie etal, 2022a (28) | Simple random sampling | Survey | Chi-square and bi- variate logistic analysis | Out of the total households, 511(82.6%) were using the CBHI scheme for health care service utilization |
| Demissie and Negara, 2020(20) | Randomly selected sample | Household survey, focus group discussions | Descriptive, multivariate and bi-variate logistic regression | The CBHI member households were about three times more likely to utilize outpatient care than their non-member counterparts |
| Gebru and Latino, 2018(1) | two-stage stratified sampling | World Health Organization QoL-BREF too | Descriptive statistics and logistic regression | QoL among CBHI-insured household heads increased by 12.41% than un-insured family heads |
| Christian, 2017(47) | Two-stage stratified sampling | Questionnaire and interview guide | Descriptive statistics and logistic regression | 89% of respondents confirmed that the project helps a lot the CBHI staff to improve their level of CBHI management. |
| Moyehodie etal., 2022b(51) | Randomly selected sample | Ethiopian Mini Demographics and Health Survey 2019 | Multilevel logistic regressions | The prevalence of CBHI enrollment in Ethiopia was 20% |
| Gashaw, 2020(7) | two-stage stratified sampling | Structured questionnaire | Descriptive statistics, bivariate and multivariate logistic regression | There was no significant association between socio-demographic characteristics and level of satisfaction of patients |
| Abdilwohab, 2021(40) | Two-stage stratified sampling | Pe-tested structured questionnaires | Descriptive statistics and bivariate and multivariable linear regression | CBHI process and management-related factors were also significantly associated with satisfaction. |
| Shigute etal., 2020(35) | Randomly selected sample | World Health Organization QoL-BRIEF Tool | Descriptive summary, simple and multiple linear regression | QoL among CBHI-insured household heads increased by 12.4% than those noninsured family heads |
| Atinafu etal, 2018(32) | Two-stage stratified sampling | Structure questionnaire | Descriptive summary, simple and multiple regression, X2 test | There was a significant difference in the rate of healthcare utilization between insured (50.5%) and uninsured (29.3%) households |
| Workeneh, 2017(34) | Two-stage stratified sampling | Self-Administered, structured, pre-tested questionnaire | Descriptive Bivariate and multivariate logistic regression | Appropriately 77.9% of the study population complied with CBHI requirements |
| Mokenen etal., 2018 (29) | multistage random sampling | survey | Multivariate logistic regression and propensity score matching | The total level of catastrophic health expenditure was found to be 20%. Among the households with catastrophic health expenditure, 4.41% were insured, whereas the remaining 15.64% were non-insured. |
| Jembere, 2018(31) | Mixed method | Household survey, FGDs, key informant and in-depth interviews | Descriptive and qualitative | CBHI improve access and overall quality of health service |
| Mitiku Kebede, 2019(37) | Simple random sampling method | Pre-tested and structured questionnaire. | Descriptive statistics, bivariate and multivariable logistic regression analyses | About 45% of households in the Sheko zone in Ethiopia were not satisfied with the CBHI scheme. |
| Fufa etal., 2021(39) | Purposively Systematic random sampling | Pre-test structured questioners And semi-structured questioners | Descriptive statistics, bivariate and multivariable logistic regression analyses | Overall customer satisfaction with health services received from the selected health institutions was 63.4 %. |
| Geferso and sharo, 2022(48) | Multistage sampling design | A standardized and structured questionnaire | Descriptive, Bivariate and multivariate logistic regressions | The magnitude of CBHI utilization was 398 (66.3%) |
| Banitie etal, 2020(43) | Systematically | Structured face-to-face interviews using a newly developed and validated questionnaire. | Descriptive statistics, bivariate and multivariable logistic regression analyses | 51% of them had good knowledge of CBHI, while 56% of participants had a favorable attitude towards CBHI. |
| Kaso, 2022 (44) | Simple random sampling technique | Structured questionnaire | Descriptive statistics and Multivariate logistic regression | The respondents’ CBHI membership renewal rate was 82.68%. |
| Girmay and Reta, 2022(38) | Systematically | Face-to-face interview | Descriptive methods fitted binary logistic regression | 60% of respondents utilize the CBHI services |
| Mussa etal., 2021(53) | Simple random sampling | Integrated safety nets programs baseline survey implemented | Binary logistic regression and multiple regression | Current CBHI enrollment is higher among PW households (70.1%) than PDS clients (50.3%) |
Most (76%) of the reviewed studies were analyzed by using descriptive statistics and logistic regression (1, 7, 20, 28–30, 33, 34, 38–40, 42–44, 47, 48, 51, 53, 54). Followed by 3(12%) who used descriptive statistics and an econometric analysis approach (32, 41, 52) and 3(12%) qualitative and descriptive statistics (6, 45, 46).
Majority 10(40%) of the reviewed study results showed that the scheme increases utilization of healthcare services (6, 20, 28, 31–33, 38, 41, 45, 48). Followed by, 7(32%) of the reviewed studies result showed the CBHI scheme reduced catastrophic health expenditure (1, 6, 20, 29, 32, 34, 47, 54). Followed by 5 (20%) reviewed studies stated that the CBHI boosts household satisfaction level (7, 37, 39, 40, 42). Three (12%) of the reviewed studies also showed that utilizing the CBHI services is strongly required to assure quality health care or increase QoL(quality of life) (1, 46, 55). and the last 12 % of the reviewed researches talked about the benefits of CBHI on community management and other resource utilization practices.
Regarding to the gap, the CBHI system provided 45.6% of UHC while reducing yearly OOP expenditures by 28–43% (33, 56)). In a given matching algorithm, insured households associated with visits increased by 2.6 times, per-capita health expenditure decreased by 17–14% points, per-capita consumption of non-food items increased by 12–14% points, and per-capita consumption of food items decreased by 12–13% points (41) . CBHI had significant government support, and early pilots aided in understanding the scaling-up process (45). Outpatient department (OPD) visits per capita were 2.09 among CBHI member families, 1.53 among non-member CBHI woreda households, and 1.75 among non-CBHI woreda households (30).
When compared to uninsured family heads, QoL increased by 12.4% among CBHI-insured household heads (7). Healthcare use rates vary considerably between insured (50.5%) and uninsured (29.3%). 77.9% of the study population satisfied CBHI requirements (1, 57).
Discussion
Ethiopia has seen significant improvements in health outcomes and economic growth over the past decade, yet its total health spending remains among the lowest in Africa (45). Ethiopia launched a CBHI strategy intending to cover 80% of districts and 80% of the population by 2020 (58).
The research indicates that few studies have examined the impact of CBHI on health service utilization, despite the importance of tailored designs and evidence-based implementation. The study found that only 4% of studies analyzed the effects of the CBHI scheme on healthcare utilization, comparing differences in healthcare utilization between CBHI member households and non-member factors.
This review concluded that 84% of articles published from 2018–2023 and 16% in 2017 were evaluated. The majority of studies under review used appropriate methodologies and study designs, such as cross-sectional comparative studies, data-layered surveys, mixed cross-sectional studies with low and medium risk, community-based cross-sectional studies, qualitative study designs, and quantitative study designs. However, only 4% of the studies examined employed structured and layered data for their surveys, which revealed measurement bias. Omair (2015) argued that descriptive studies are equivalent in that they are all based on a single sample and do not include a comparison group as part of the research design. This review of research found 36% used samples of 201 to 500 people and nearly all (88%) of the studies reviewed used samples of less than 1000 people for their study evaluations, but the sample size had to be large enough for the study to have appropriate statistical power to detect significant changes. Even if it is allowed, there may be practical and financial reasons for it.
We found that close to two-fifths of reviewed studies were conducted at the national level of the country (Ethiopia), and the remaining 86% were conducted in SNNPR, Addis Ababa, Thehudered District, North East, Chilga District, Amhara Regional State, Kutaber district, Yirgalem town, Sheku district, South West, Arsi-Negle woreda health centre, Akaki District, Oromia Special Zone, Oromia, Yirga Chafe district, Gedeo zone, Southern Ethiopia. This review study found that 40% of the evaluated research employed a logistic regression model to analyze its data, while some used no model at all. Additionally, the majority of the studies examined contained probity and propensity models. Mebratie et al classified the 48 schemes into three categories: 25 community-involved health insurance schemes operated by the government, 7 insurance programs initiated by healthcare professionals, and 16 community-based prepaid health clubs. Ethiopia’s CBHI approach fits within category (25). The 2019 Ethiopian Mini-Demographic and Health Survey used face-to-face interviews, key informant advice, and structured questions. Only a small proportion of researchers used the WHO QoL BRIEF instrument, the Jana Briggs Institute checklist, propensity score matching (PSM), and the integrated safety net programs baseline survey.
About 72% of the study results showed that the scheme reduced catastrophic health expenditure and increases utilization of healthcare services. The 20% reviewed studies stated that the CBHI boosts household satisfaction level. The last 12% of the reviewed researches talked about the benefits of CBHI on community management, resource utilization practices and enrollment factors. Numerically, the CBHI system provided 45.6% of UHC while reducing yearly OOP expenditures by 28–43%, healthcare use rates vary considerably between insured (50.5%) and uninsured (29.3%), and QoL increased by 12.4%.
Conclusion
Most studies prove that Ethiopia’s CBHI program significantly reduced beneficiaries’ exposure to catastrophic health expenditure, improved their health status, and played a significant role in improving health-related QoL.
The government and associated organizations should increase public awareness of CBHI programs, improve their accessibility and coverage, and reduce the cost of premium services for the less fortunate. Depending on the level of risk sharing and the government’s initiatives to boost domestic income, CBHI’s financial stability will vary. To reach bigger and more stable population coverage, it is crucial to improve the quality of the healthcare system and pharmaceutical accessibility. New partners would boost the amount of funding available for CBHI expansion. A reliable information system, along with operational staff training, would improve CBHI performance and provide information to support decisions.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Footnotes
Conflict of Interest
The authors declare that there is no conflict of interests.
References
- 1.Gebru T, Lentiro K. (2018). The impact of community-based health insurance on health-related quality of life and associated factors in Ethiopia: a comparative cross-sectional study. Health Qual Life Outcomes, 16: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CSA, ICF (2016). Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. [Google Scholar]
- 3.Geta ET, Wakjira A, Hailu WB. (2023). Disparities in modern health service utilization across socio-demographic and economic inequalities among households in Gida Ayana district, Oromia Regional state, Ethiopia: a community-based cross-sectional study. BMC Health Serv Res, 23(1): 597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mebratie AD, Sparrow R, Yilma Z, et al. (2015). Enrollment in Ethiopia’s community-based health insurance scheme. World Dev, 74: 58–76. [DOI] [PubMed] [Google Scholar]
- 5.Feleke S, Mitiku W, Zelelew H, Ashagari T. (2015). Ethiopia’s community-based health insurance: a step on the road to universal health coverage. USAID Health Finance and Governance, Abt Associates.
- 6.Bayked EM, Toleha HN, Kebede SZ, et al. (2023). The impact of community-based health insurance on universal health coverage in Ethiopia: a systematic review and meta-analysis. Glob Health Action, 16 (1): 2189764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gashaw D. (2020). Level of household satisfaction in community based health insurance beneficiaries on medical laboratory services and its associated factors in selected health centers. Food Sci Qual Manag, 98: 29–35. [Google Scholar]
- 8.Nevondwe L, Odeku KO. (2014). Financing the national health insurance scheme of South Africa: opportunities and challenges. J Soc Sci, 39 (1): 9–18. [Google Scholar]
- 9.Wang W, Temsah G, Mallick L. (2017). The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health Policy Plan, 32 (3): 366–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fadlallah R, El-Jardali F, Hemadi N, et al. (2018). Barriers and facilitators to implementation, up-take and sustainability of community-based health insurance schemes in low- and middle-income countries: a systematic review. Int J Equity Health, 17 (1): 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ly MS, Bassoum O, Faye A. (2022). Universal health insurance in Africa: a narrative review of the literature on institutional models. BMJ Glob Health, 7 (4): e008219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang H, Switlick K, Ortiz C, et al. (2012). Health insurance handbook: how to make it work. Vol. 219-World Bank Publications. [Google Scholar]
- 13.Habiyonizeye Y. Implementing community-based health insurance schemes: lessons from the case of Rwanda feeding [Master’s thesis]. Akershus University, Norway; 2013. [Google Scholar]
- 14.Azmeraw S. Determinants of Community Based Health Insurance Program Implementation in Ebinat District, Amhara Regional State, Ethiopia [PhD thesis]. Bahir Dar University, Ethiopia; 2022. [Google Scholar]
- 15.Hailie MT, Hassen SL, Temesgen MM. (2021). Client satisfaction on community based health insurance scheme and associated factors at Boru Meda Hospital, Northeast, Ethiopia: institutional based cross-sectional study. BMC Health Serv Res, 21 (1): 1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO (2019). Primary health care on the road to universal health coverage: 2019 global monitoring report: executive summary.
- 17.Likka MH, Handalo DM, Weldsilase YA, Sinkie SO. (2018). The effect of community-based health insurance schemes on utilization of healthcare services in low- and middle-income countries: a systematic review protocol of quantitative evidence. JBI Database System Rev Implement Rep, 16 (3): 653–661. [DOI] [PubMed] [Google Scholar]
- 18.Kigume R, Maluka S. (2021). The failure of community-based health insurance schemes in Tanzania: opening the black box of the implementation process. BMC Health Serv Res, 21 (1): 646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kakama AA, Namyalo PK, Basaza RK. (2020). Feasibility and desirability of scaling up Community-based Health Insurance (CBHI) in rural communities in Uganda: lessons from Kisiizi Hospital CBHI scheme. BMC Health Serv Res, 20 (1): 662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Demissie B, Gutema NK. (2020). Effect of Community-Based Health Insurance on Utilization of Outpatient Health Care Services in Southern Ethiopia: A Comparative Cross-Sectional Study. Risk Manag Healthc Policy, 13: 141–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Page MJ, McKenzie JE, Bossuyt PM, et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg, 88: 105906. [DOI] [PubMed] [Google Scholar]
- 22.Mebratie A, Sparrow R, Debebe ZY, et al. (2014). Dropping out of Ethiopia’s Community Based Health Insurance scheme. ISS Working Paper Series/General Series, 591: 1–40. [Google Scholar]
- 23.Lavers T. (2019). Social protection in an aspiring ‘developmental state’: The political drivers of Ethiopia’s PSNP. African Affairs, 118(473):646–671. [Google Scholar]
- 24.USAID Health Financing Improvement Program (2022). Annual Performance Report Year 4 (October 1, 2021–September 30, 2022). Abt Associates, Rockville MD. [Google Scholar]
- 25.WHO (2020). Community based health insurance. Geneva (CH): World Health Organization; updated 2020. [Google Scholar]
- 26.FMoH E. (2017). Ethiopian health accounts household health service utilization and expenditure survey 2015/2016. Federal Democratic Republic of Ethiopia Ministry of Health, Addis Ababa. [Google Scholar]
- 27.Woldemichael A, Takian A, Sari AA, Olyaeemanesh A. (2019). Availability and inequality in accessibility of health center-based primary healthcare in Ethiopia. PLoS One, 14 (3): e0213896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moyehodie YA, Mulugeta SS, Amare YS. (2022). The effects of individual and community-level factors on community-based health insurance enrollment of households in Ethiopia. PLoS One, 17 (10): e0275896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mekonen AM, Gebregziabher MG, Teferra AS. (2018). The effect of community based health insurance on catastrophic health expenditure in Northeast Ethiopia: A cross sectional study. PLoS One, 13 (10): e0205972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kassa AM. (2023). In Ethiopia’s Kutaber district, does community-based health insurance protect households from catastrophic health-care costs? A community-based comparative cross-sectional study. PLoS One, 18 (2): e0281476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jembere MY. (2018). Community based health insurance scheme as a new healthcare financing approach in rural Ethiopia: role on access, use and quality of healthcare services, the case of Tehuledere district, Northeast Ethiopia. Fam Med Med Sci Res, 7:2. [Google Scholar]
- 32.Atnafu DD, Tilahun H, Alemu YM. (2018). Community-based health insurance and healthcare service utilization, North-West, Ethiopia: a comparative, cross-sectional study. BMJ Open, 8 (8): e019613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alemayehu YK, Dessie E, Medhin G, et al. (2023). The impact of community-based health insurance on health service utilization and financial risk protection in Ethiopia. BMC Health Serv Res, 23 (1): 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Workneh SG, Biks GA, Woreta SA. (2017). Community-based health insurance and communities’ scheme requirement compliance in Thehuldere district, northeast Ethiopia: cross-sectional community-based study. Clinicoecon Outcomes Res, 9: 353–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shigute Z, Mebratie AD, Sparrow R, et al. (2020). The effect of Ethiopia’s community-based health insurance scheme on revenues and quality of care. Int J Environ Res Public Health, 17 (22): 8558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mussa EC, Otchere F, Vinci V, et al. (2021). Linking poverty-targeted social protection and Community Based Health Insurance in Ethiopia: Enrolment, linkages, and gaps. Soc Sci Med, 286: 114312. [DOI] [PubMed] [Google Scholar]
- 37.Mitiku KK, Geberetsadik SM. (2019). Household satisfaction with community-based health insurance scheme and associated factors in piloted Sheko district; Southwest Ethiopia. PLoS One, 14 (5): e0216411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Girmay AM, Reta MT. (2022). Community-based health insurance service utilization and associated factors in Addis Ababa, Ethiopia. Public Health Challenges, 1 (3): e18. [Google Scholar]
- 39.Fufa G, Ermeko T, Mohammed AY, Lette A. (2021). Assessing factors associated with poor community based health insurance client satisfaction level with public health care services in Negele Arsi Woreda Health Centers, West Arsi Zone Ethiopia. Arch Med, (13)5: 21. [Google Scholar]
- 40.Abdilwohab MG, Abebo ZH, Godana W, et al. (2021). Factors affecting enrollment status of households for community based health insurance in a resource-limited peripheral area in Southern Ethiopia. Mixed method. PLoS One, 16 (1): e0245952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Asfaw DM, Shifaw SM, Belete AA, Aychiluhm SB. (2022). The impact of community-based health insurance on household’s welfare in Chilga district, Amhara, Ethiopia. Front Public Health, 10: 868274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Addise T, Alemayehu T, Assefa N, Erkalo D. (2021). The magnitude of satisfaction and associated factors among household heads who visited health facilities with community-based health insurance scheme in Anilemo District, Hadiya Zone, southern Ethiopia. Risk Manag Healthc Policy, 14: 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bantie GM, Woya AA, Zewdie BM. (2020). Community-based health insurance and associated factors in North-Western Ethiopia. The case of Bahir Dar city. Int J Gen Med, 13: 1207–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaso AW, Yohanis Y, Debela BG, Hareru HE. (2022). Community-based health insurance membership renewal rate and associated factors among households in Gedeo zone, southern Ethiopia. J Environ Public Health, 2022:8479834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mula AK, Mao W, Bharali I, et al. (2022). Scaling up community-based health insurance in Ethiopia: a qualitative study of the benefits and challenges. BMC Health Serv Res, 22 (1): 473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jembere MY. (2018). The role of community based health insurance scheme on financial protection and healthcare seeking behavior of households in Tehuledere District, Northeast Ethiopia. International Journal of Health Economics and Policy, 3 (2): 13–19. [Google Scholar]
- 47.Christian K. Public health project and community based health insurance performance in Rwanda A case study of public health project in Karongi district [PhD thesis]: Mount Kenya University, Kenya; 2017. [Google Scholar]
- 48.Geferso AT, Sharo SB. (2022). Community-based health insurance utilization and its associated factors among rural households in Akaki District, Oromia, Ethiopia. Adv Public Health, 1–12.
- 49.Mirach TH, Demissie GD, Biks GA. (2019). Determinants of community-based health insurance implementation in west Gojjam zone, Northwest Ethiopia: a community based cross sectional study design. BMC Health Serv Res, 19: 544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Atinafu W. Practices and challenge on community based health insurance: the case of Basketo special woreda [PhD thesis]: Haremaya University, Ethiopia; 2022. [Google Scholar]
- 51.Moyehodie YA, Fenta SM, Mulugeta SS, et al. (2022). Factors Associated with Community Based Health Insurance Healthcare Service Utilization of Households in South Gondar Zone, Amhara, Ethiopia. A Community-Based Cross-Sectional Study. Health Serv Insights, 15: 11786329221096065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shigute Z, Strupat C, Burchi F, et al. (2020). Linking social protection schemes: the joint effects of a public works and a health insurance programme in Ethiopia. J Dev Stud, 56 (2): 431–448. [Google Scholar]
- 53.Mussa EC, Agegnehu D, Nshakira-Rukundo E. (2022). Impact of conditional cash transfers on enrolment in community-based health insurance among female-headed households in south Gondar zone, Amhara region, Ethiopia. SSM Popul Health, 17: 101030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Badacho AS, Tushune K, Ejigu Y, Berheto TM. (2016). Household satisfaction with a community-based health insurance scheme in Ethiopia. BMC Res Notes, 9: 424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shigute Z, Mebratie AD, Sparrow R, et al. (2017). Uptake of health insurance and the productive safety net program in rural Ethiopia. Soc Sci Med, 176: 133–141. [DOI] [PubMed] [Google Scholar]
- 56.Bayked EM, Toleha HN, Kebede SZ, et al. (2023). The impact of community-based health insurance on universal health coverage in Ethiopia: a systematic review and meta-analysis. Glob Health Action, 16 (1): 2189764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tilahun H, Atnafu DD, Asrade G, et al. (2018). Factors for healthcare utilization and effect of mutual health insurance on healthcare utilization in rural communities of South Achefer Woreda, North West Ethiopia. Health Econ Rev, 8: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ethiopia F (2015). Health Sector Transformation Plan (HSTP): 2015/16-– 2019/20, Addis Ababa. Available from: https://ephi.gov.et/wp-content/uploads/2023/01/2.-Ethiopia-Health-Sector-Transformation-Plan-I-2015-2020-Endline-Review.pdf