Abstract
Objective: The development of objective assessment tools for attention deficit hyperactivity disorder (ADHD) has become a hot research topic. The aim was to explore the value of the P300 wave and integrated visual and auditory continuous performance test (IVA-CPT) in diagnosing ADHD. Methods: We enrolled 30 patients with ADHD and 30 age-matched healthy volunteers in a prospective study to evaluate differences in IVA-CPT and P300 indexes using student t test. These tools’ accuracy in identifying ADHD patients was evaluated using receiver operating characteristic curve analysis. Additionally, the correlation between P300 and IVA-CPT in ADHD patients was evaluated using Pearson correlation analysis. Results: Compared with healthy volunteers, ADHD patients showed longer latency and lower amplitude, and had lower scores of IVA-CPT (P<0.01). There was no significant difference of latency, amplitude, and area below the amplitude of the P300 wave and in the score of IVA-CPT for age and gender within-ADHD groups (P>0.05). Moreover, receiver operating characteristic (ROC) curve showed high accuracy of P300 and IVA-CPT in identifying ADHD patients. Furthermore, both P300 index and IVA-CPT had high accuracy and performance in identification of ADHDin, ADHDhi, and ADHDcom. However, for different subtypes of ADHD, no significant differences were observed of ROC curves between subgroups (P>0.05). In addition, the performance in IVA-CPT was positively correlated with the amplitude, and negatively correlated with the latency of P300. Conclusion: These results support the discriminant validity of P300 and IVA-CPT in distinguishing ADHD patients, providing a theoretical basis for P300 and IVA-CPT testing in the clinical diagnosis of ADHD.
Keywords: Attention deficit hyperactivity disorder (ADHD), event-related potentials (ERPs), P300, integrated visual and auditory continuous performance test (IVA-CPT), diagnosis
Introduction
Attention-deficit/hyperactivity disorder (ADHD), as a common childhood neurodevelopmental disorder, is characterized by developmentally inappropriate essential features that result in impaired attention, hyperactive, and impulsive behaviors [1-3]. According to the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual (DSM-V), the manual distinguishes between three subtypes of the disorder: predominantly hyperactive/impulsive type, predominantly inattentive type, and combined type [4]. ADHS affects 5% of children and usually has an onset before 12 years old [4]. Presently, the diagnosis and classification of ADHD mainly depend on the clinical observation of behavior and on interviews [5,6]. So far there is no clear biological evidence and objective diagnostic criteria for ADHD, which has led to controversy in the medical community. As a result, the search for diagnostic tests are more urgent.
The event-related potential (ERP) is a noninvasive technique that provides information about electro-neurophysiological activity associated with sensory, motor, and cognitive processes [7,8]. ERPs are already one of the most widely used methods in cognitive neuroscience research. They have been applied to estimate the distraction in children using an oddball paradigm [7,9]. One common and well-examined ERPs component in cognitive neuroscience is the P300 (P3) wave, a late positive component emerging approximately 300-400 ms after a stimulus [10,11]. It is generated in the medial cortical or subcortical region, and is sensitive to the delivery of task-relevant information that requires a decision or reaction from the participant. The processing related to attention, memory and emotion also plays a role [12-14]. Therefore, understanding alterations of ERPs in ADHD patients helps identify their attention processes and hints at the underlying pathophysiological mechanisms.
The continuous performance test (CPT), as a neuropsychological tool, can measure processing speed as well as focused, sustained, divided, and alternating attention characteristics in a neuropsychological evaluation [12,15]. The diagnosis of attention problems associated with ADHD can be evaluated using a CPT to quantify the number and severity of symptoms [16,17]. In our study, the IVA-CPT, which is one type of CPT, was applied to assess auditory and visual attention in the same task.
The aim of the study was to assess the diagnostic value of IVA-CPT and P300 for ADHD. As it is increasingly recognized that the P300 wave could provide a relatively objective evaluation index for ADHD, it is important to enhance our understanding of diagnostic value of IVA-CPT in ADHD. To our knowledge, both assessments could help improve the reliability and objectivity of the clinical diagnostics for ADHD. Nonetheless, knowledge gaps remain in the understanding the difference between IVA-CPT and P300 in ADHD diagnosis. Hence, it is of great interest to shed light on the difference between IVA-CPT and P300 in diagnosing ADHD.
Methods
Participants
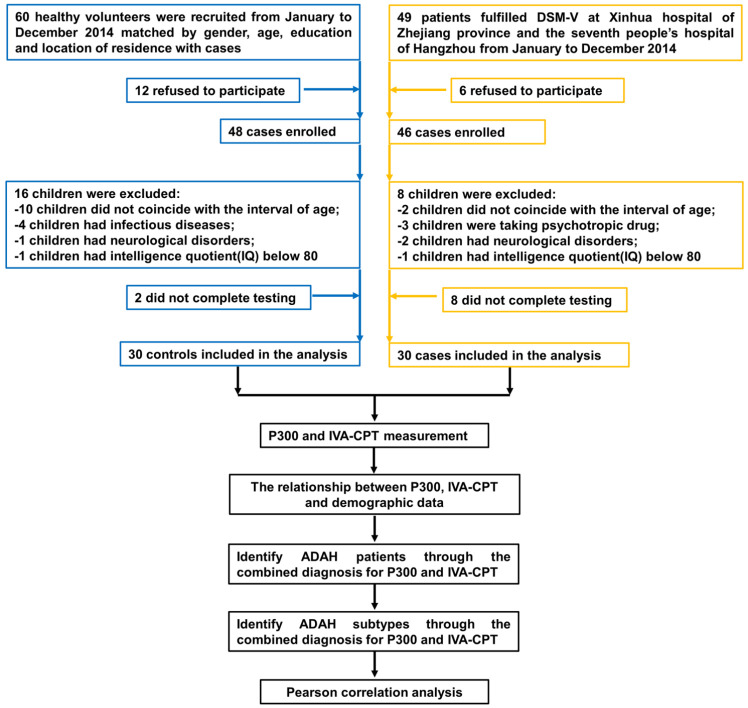
From February to December of 2018, patients with ADHD (age: 8-14 years) were recruited from the 2nd affiliated Hospital of Zhejiang Chinese Medical University. During the same period, healthy volunteers (age: 9-13 years) were recruited from Xinhua Hospital of Zhejiang Province for physical examination. In this study, due to the limited number of ADHD patients, a sample size calculation was not performed prior to the research. To maximize the accuracy and reliability of the study, we included as many patients as possible. The Raven’s Standard Progressive Matrices (RSPM) full intelligence quotient (IQ) scores of all subjects were over 80. According to the diagnostic criteria for ADHD from the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-V) [18], after the parents of the children filled out the diagnostic scale, diagnosis of ADHD in selected children was carried out by two psychiatrists who were at the level of attending physicians. For attention deficit symptoms, patients must meet at least six of the following criteria and have a duration of symptoms for more than six months. The patient’s symptoms are disproportionate to their developmental level and directly negatively impact their learning. Criteria: (a) Often cannot pay attention to details or often make careless mistakes at school or in other activities. (b) Often have difficulties maintaining attention while completing tasks or activities. (c) Often seem to not listen when having direct conversations with others. (d) Often cannot follow instructions and cannot successfully complete tasks, chores, or work. (e) Often have difficulties organizing tasks and activities. (f) Often avoid or reluctantly engage in activities that require brainpower. (g) Often lose important items needed to complete tasks or activities. (h) Often irrelevant stimuli easily cause distraction. (i) Often forget daily activities. For hyperactivity/impulsivity symptoms, patients must meet at least six of the following criteria and have a duration of more than six months. The patient’s symptoms are disproportionate to their developmental level and directly negatively impact their learning. Criteria: (a) Often restless and unable to sit still. (b) Often leave their seat in the classroom or other situations where sitting is required. (c) Often runs and climbs in inappropriate places. (d) Often unable to play quietly or engage in leisure activities. (e) Often very busy, constantly busy like a motor. (f) Often talks too much. (g) Often impatiently answers before others finish their questions. (h) Often unable to wait. (i) Often interrupts or disturbs others. All subjects were right-handed. The flowchart of the study, including the enrollment of cases and controls, are presented in Figure 1. All children with ADHD were drug-naive and remained off medication during the study. Of the children with ADHD, 9 children met the criteria for the inattentive subtype of ADHD, 7 for the hyperactive/impulsive subtype, and 14 for the combined subtype. All the participants had normal or corrected to-normal vision. Each subject had no hearing impairment and learning or reading disabled.
Figure 1.
Flowchart of our study. IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; DSM-V, diagnostic and statistical manual.
The exclusion criteria for both groups included: a) Uncorrected sensory impairment; b) Presence of somatic or mental disorders; c) Taking any psychotropic drug; d) History of traumatic brain injury; e) Prior history or current presentation of neurological or psychiatric disorders; f) Epilepsy other comorbid psychiatric disorders; g) An intelligence quotient (IQ) below 80 (assessed by RSPM). All protocols were conducted in accordance with the Declaration of Helsinki. All subjects and their parents had the right to participate in these studies voluntarily.
Procedures
Both ADHD and healthy volunteers were evaluated for IVA-CPT and P300.
IVA-CPT
The IVA-CPT was completed using special software CCRT and an instrument, designed by Nanjing VISHEE medical technology company in Nanjing, China. The test included 500 stimulus elements, including visual stimuli and auditory stimuli. Each participant was seated in front of the computer monitor about 40-60 cm away from the screen. The center of the monitor was kept at same eye level. A two-button ergonomic mouse was placed in front of the computer screen and the left button was used to record responses. The visual stimuli (1 or 2) were green in color, 4 cm high, and were presented inside a rectangle positioned in the middle of the computer screen. The auditory stimuli (1 or 2) were presented with a scheduled program and each element lasted for 500 ms. Task instructions was given by computer before each item and this study includes three items: a) The warm-up part of the test: each participator who saw or heard a “1” was required to click the mouse, which was presented and recorded as 10 trials respectively for 2-3 min. b) Main part of the test: includes practice (2 min) and test (13 min). Participants were apprised and shown a presentation where they would see or hear a “1” or a “2”. Each participant who saw or heard a “1” (target) was required to click the mouse and when they saw or heard a “2” (error) they were required not to click the mouse. c) Cool-down part of the test: The cool-down was consistent with the warm-up previously described. The entire IVA-CPT test lasted about 20 min to complete instructions, warm-up, main test, and cooldown. Finally, there were several quotients, including full scale attention quotient (FSAQ), auditory attention quotient (AAQ), visual attention quotient (VAQ), full scale response control quotient (FSRCQ), auditory response control quotient (ARCQ) and visual response control quotient (VRCQ).
Event-related potentials (ERPs) test
ERPs signals were measured using WJ-1 Event related potential meter from Guangzhou Runjie Medical Equipment Co., Ltd. (Guangzhou, China) by placing a surface electrode along the left frontal area (F3), right frontal area (F4), left parietal area (P3), right parietal area (P4), central area (Cz) and electrode grounding (Fpz) which were arranged according to the 10-20 international system of EEG. A reference electrode was placed bilaterally on the ears, and the impedance was measured at less than 5 kΩ. Each stimulus contains two degrees, which was composed of three pictures, respectively. The low-difficulty condition (Figure S1) was of one of three pictures Figure S1A-C, which Figure S1A, S1C both had four birds, in different positions, and Figure S1B had five birds. The high-difficulty condition (Figure S2) was of one of three calendars Figure S2A-C, all of which were calendars for July, 2018, but Figure S2A was missing the number 16, Figure S2C was missing number 31, Figure S2B was out modified. We set up the rule that the low-difficulty condition was given to junior grade children (7-10 years) and the high-difficulty condition was appropriate for senior grade children (11-14 years).
Participants were seated in a comfortable chair in front of a computer monitor about 70-80 cm away from the screen. They were arranged in a sound proof and quiet room. After they were wired with electrodes, then the study began. The visual oddball paradigm was applied. They were requested to focus their immediate attention on the stimuli presented at the screen and to point out as quickly as possible the occurrence of a “target” stimulus (Figure S2B) by clicking the mouse with their left index finger while withholding attention on the “non-target” stimuli (Figure S2A, S2C). Each study incorporated 150 stimuli, which were sequentially presented for 1200 ms, with an inter stimulus interval of 1200 ms as well. Participants were allowed a rest period after the practice block. Latency, amplitude and the area below the wave amplitude of P300 were recorded.
Evaluation index
The Major outcome: The Latency, amplitude and the area below the P300 wave amplitude in different areas, and the score of IV-CPT in difference quotients. The secondary outcome: Whether vision and hearing were impaired in patients.
Statistical analysis
The measurement data were expressed by mean ± standard deviation, the independent sample t-test was used for the comparison between the two groups, the Mann-Whitney U test was used for the comparison among more than two groups, and Chi-square test was used for the correlation analysis. Statistical analysis was performed on ERPs measures and IVA-CPT dates separately using the t-test, with group (ADHD vs healthy volunteers). Diagnostic value of P300 and IVA-CPT component was estimated through building receiver operating characteristic curve (ROC) curves, and the area under curve (AUC) was calculated using Delong test. Pearson correlation analysis was used to assess the relationships between auditory attention quotient, auditory control quotient and P300 component. Statistical analysis was performed using the IBM SPSS 22 (IBM, NY, USA) program, and statistically significant differences were indicated as *P<0.05 and **P<0.01, and no significant difference was indicated as “ns”.
Results
Demographic data
The workflow for evaluating the IVA-CPT and P300 diagnostic tools for ADHD was illustrated in Figure 1. A total of 109 participants were enrolled in this study, including 49 patients with ADHD and 60 healthy volunteers. Out of the expected participants, the 49 individuals (19 patients with ADHD and 30 healthy volunteers) were excluded from the studied, mainly according to inconsistent age and the exclusion criteria: Example of exclusions: 1. children who were not within the interval of age; 2. children who had infectious diseases; 3. children who had neurological disorders; and 4. children who had an intelligence quotient (IQ) below 80. Finally, the resulting study samples consisted of 60 participants, which included the 30 ADHD patients (20 male and 10 female) and 30 healthy volunteers (16 male and 14 female). The demographic and clinical characteristics of the participants, such as gender, age, and course of disease were listed in Table 1. The comparative analysis results displayed that there were no statistically significant differences in gender [Male/Female: 20/10 vs 16/14] and age [8-12.25 vs 9-13] between the ADHD patients and the healthy volunteers (Table 1).
Table 1.
Clinical characteristics of study subjects
| Index | ADHD group (n=30) | Healthy volunteers (n=30) | χ2/t value | P value | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| ADHD (n=30) | ADHDin (n=9) | ADHDhi (n=7) | ADHDcom (n=14) | ||||
| Gender (male/female) | 20/10 | 7/2 | 4/3 | 9/5 | 16/14 | χ2=0.259 | 0.578 |
| Age | 9.5 (9-12) | 9 (8.5-12) | 9 (8-14) | 10 (9-12.25) | 10 (9-13) | t=0.657 | 0.329 |
| Course of the disease | 2.9±0.31 | 2.8±0.29 | 2.6±0.18 | 3.1±0.34 | - | - | - |
ADHD, attention deficit hyperactivity disorder; ADHDin, ADHD-inattention; ADHDhi, ADHD-hyperactivity/impulsivity; ADHDcom, ADHD-combination.
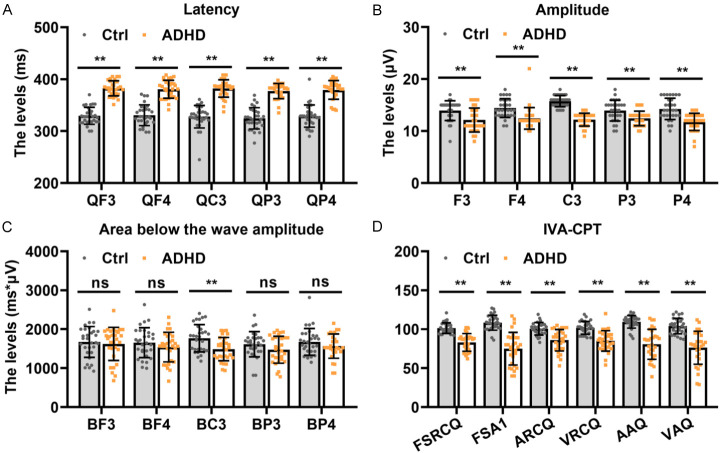
Evaluation of P300 and IVA-CPT
Subsequently, we conducted the ERPs. The latency, amplitude, and area below the wave amplitude of P300, as well as the scores of IVA-CPT in all groups were comparable for ADHD diagnostic evaluation. In terms of latency, our study indicated that ADHD patients had apparently increased levels of QF3, QF4, QC3, QP3 and QP4 compared with the healthy volunteers (all P<0.01, Figure 2A). As shown in Figure 2B, the decrease of the amplitude of test area was observed in ADHD (all P<0.001). There was a significant decrease in the area below the wave amplitude of BC3 between ADHD patients and control, whereas the level of the area below the wave amplitude in BF3, BF4, BP3, and BP4 was similar in both ADHD and control groups (Figure 2C). Figure 2D showed the score of IVA-CPT test analysis in FSAQ, AAQ, VAQ, FSRCQ, ARCQ, and VRCQ. Visual and hearing of ADHD and control groups were not impaired by electrodes (data not shown). Taken together, the results showed significant differences between the two groups for all quotients (all P<0.01).
Figure 2.
Evaluation of P300 and IVA-CPT in the ADHD group compared with the control group. The levels of latency (A), amplitude (B) and the area below the wave amplitude of P300 (C) as well as IVA-CPT (D). **P<0.01 and ns= no significance. IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient.
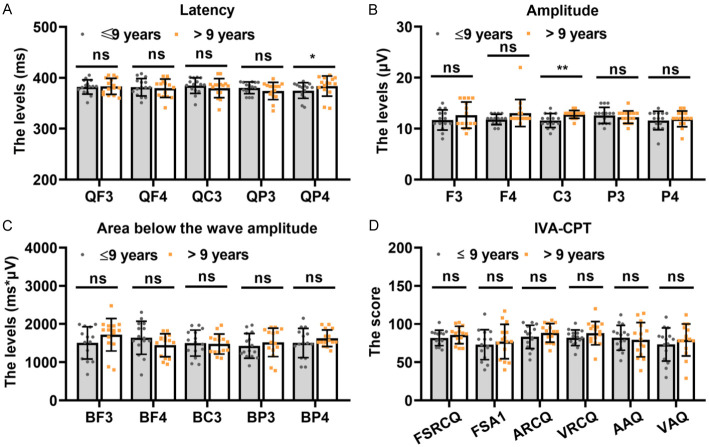
The patients were then divided into two groups based on their age (the age threshold was 9 years old). The level of latency was not significantly different in QF3, QF4, QC3, and QP3 between the two groups, while it was markedly increased in QP4 level in children aged over 9 years old (Figure 3A). Additionally, there was a stronger amplitude in QF4 of children aged over 9 years old when this group was compared to thoes aged less than 9 years old (Figure 3B). However, there were no differences in the area below the wave amplitude and IVA-CPT score for all areas and quotients between the two groups (Figure 3C and 3D).
Figure 3.
Evaluation of P300 and IVA-CPT in individuals aged more than 9 years old or less than 9 years old with ADHD. The levels of latency (A), amplitude (B) and the area below the wave amplitude of P300 (C) as well as IVA-CPT (D). *P<0.05, **P<0.01 and ns= no significance. IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient.
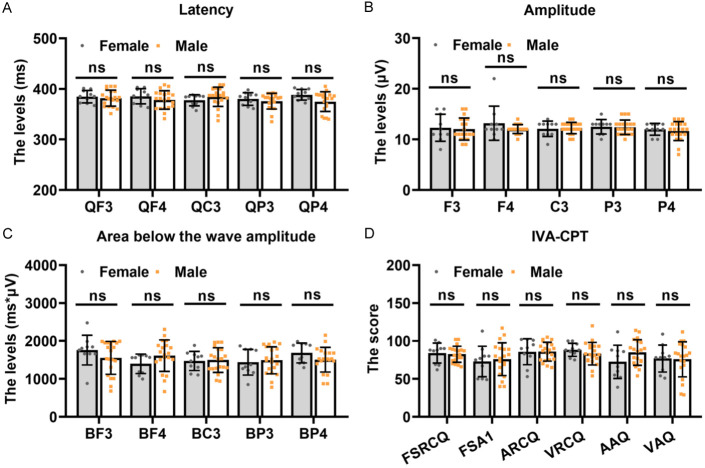
To explore the effect of P300 and IVA-CPT on the gender of ADHD patients, we analyzed the latency, amplitude, and area below the wave amplitude of P300, as well as the score of IVA-CPT in both female and male groups. However, no significant differences were observed between the two groups (Figure 4). Together, these data provide evidence that P300 and IVA-CPT can assist in the diagnosis of ADHD, and that it has nothing to do with age or gender.
Figure 4.
Evaluation of P300 and IVA-CPT in females and males with ADHD. The levels of latency (A), amplitude (B) and the area below the wave amplitude of P300 (C) as well as IVA-CPT (D). ns= no significance. IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient.
The value of P300 and IVA-CPT in ADHD diagnosis
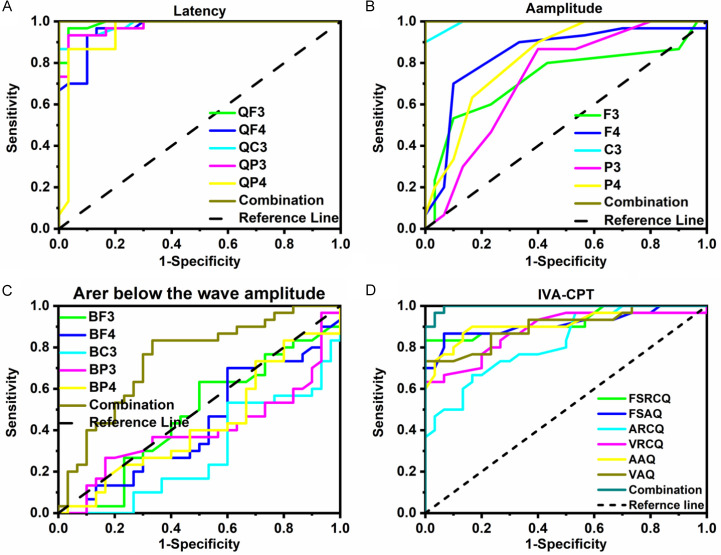
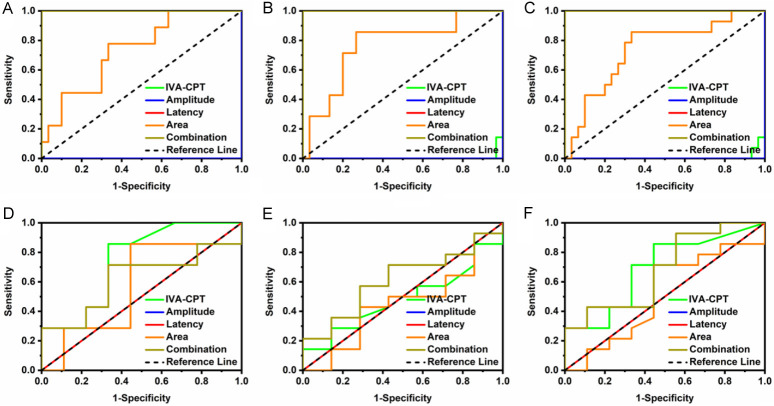
To evaluate the diagnostic capabilities of P300 and IVA-CPT in ADHD patients, ROC curve analysis was plotted to determine the AUC value. We evaluated the predictive power of P300 and IVA-CPT in ADHD patients. As shown in Table 2 and Figure 5, latency of P300, QF3, QF4, QC3, QP3, and QP4 individually can provide high accuracy for identifying ADHD patients, and provided the best performance with AUC value (all AUC>0.948) in distinguishing ADHD patients from the control group (Figure 5A). In particular, the QF3/QF4/QC3/QP3/QP4 combination yielded optimal diagnostic efficiency for ADHD patients, as compared to healthy volunteers (AUC=1). Moreover, we used Delong test to evaluate the performance of IVA-CPT and P300 for distinguishing ADHD patients from healthy volunteers (Table 3). There was no difference in latency among the different areas. Furthermore, for the discrimination between patients with ADHD and healthy volunteers, F3, F4, C3, P3, and P4 in amplitude alone also exhibited high discriminatory capacity (all AUC>0.726) (Figure 5B). The AUC of C3 was significantly increase compared with F3, F4, P3 and P4, shown by Delong test. Especially, combinations had the best performance to distinguishing ADHD (AUC=1), which was significant difference compared with single area. However, this was a lack for BF3, BF4, BC3, BP3, and BP4 alone in distinguishing ADHD patients from healthy volunteers at the area below the wave amplitude level (all AUC<0.5); whereas, the combination provided moderate discriminatory capacity for ADHD patients (AUC=0.746) (Figure 5C). There was no difference of AUC at area below the wave amplitude level between different single areas with Delong test analysis. Yet, BF4 was clearly different compared with the combination. Regarding the IVA-CPT index, we found high accuracy for FSRCQ, FSAQ, ARCQ, VRCQ, AAQ, and VAQ in ADHD diagnosis. Additionally, we attempted to combine each factor with FSRCQ, FSAQ, ARCQ, VRCQ, AAQ, or VAQ to understand their ADHD diagnostic capability. Interestingly, ROC curve analysis showed that combining FSRCQ, FSAQ, ARCQ, VRCQ, AAQ, and VAQ resulted in more effective ADHD detection (AUC=0.996) than that for each factor alone (Table 3; Figure 5D). The above results suggest that the combination diagnosis of P300 index and IVA-CPT index may improve the diagnostic efficiently and accuracy for ADHD patients.
Table 2.
Performance of IVA-CPT and P300 for distinguishing ADHD patients from healthy volunteers
| Index | AUC | Sig. | 95% LCL | 95% UCL | Cut off | Specificity | Sensitivity | Youden index | |
|---|---|---|---|---|---|---|---|---|---|
| IVA-CPT | FSRCQ | 0.923 | <0.001 | 0.852 | 0.994 | 91 | 100 | 83.333 | 0.8333 |
| FSAQ | 0.913 | <0.001 | 0.834 | 0.992 | 95.5 | 93.333 | 86.667 | 0.8 | |
| ARCQ | 0.822 | <0.001 | 0.720 | 0.925 | 93.5 | 83.333 | 66.667 | 0.5 | |
| VRCQ | 0.882 | <0.001 | 0.794 | 0.970 | 88.5 | 100 | 63.333 | 0.633 | |
| AAQ | 0.917 | <0.001 | 0.844 | 0.991 | 103 | 86.667 | 86.667 | 0.733 | |
| VAQ | 0.901 | <0.001 | 0.822 | 0.980 | 85.5 | 100 | 73.333 | 0.733 | |
| Combination | 0.996 | <0.001 | 0.986 | 1.005 | 0.594 | 96.667 | 96.667 | 0.933 | |
| Amplitude | F3 | 0.726 | 0.002 | 0.592 | 0.860 | 11.5 | 90 | 53.333 | 0.433 |
| F4 | 0.841 | <0.001 | 0.733 | 0.950 | 12.5 | 90 | 70 | 0.6 | |
| C3 | 0.993 | <0.001 | 0.981 | 1.005 | 13.5 | 100 | 90 | 0.9 | |
| P3 | 0.728 | 0.002 | 0.597 | 0.859 | 13.5 | 60 | 86.667 | 0.467 | |
| P4 | 0.825 | <0.001 | 0.719 | 0.931 | 13.5 | 60 | 90 | 0.5 | |
| Combination | 1 | <0.001 | 1 | 1 | 0.5 | 100 | 100 | 1 | |
| Latency | QF3 | 0.99 | <0.001 | 0.973 | 1.007 | 356 | 96.667 | 96.667 | 0.933 |
| QF4 | 0.962 | <0.001 | 0.921 | 1.003 | 349.5 | 86.667 | 96.667 | 0.833 | |
| QC3 | 0.984 | <0.001 | 0.961 | 1.007 | 356 | 96.667 | 93.333 | 0.9 | |
| QP3 | 0.978 | <0.001 | 0.948 | 1.007 | 360.5 | 96.667 | 93.333 | 0.9 | |
| QP4 | 0.948 | <0.001 | 0.885 | 1.011 | 359.5 | 96.667 | 86.667 | 0.8333 | |
| Combination | 1 | <0.001 | 1 | 1 | 0.5 | 100 | 100 | 1 | |
| Area below the wave amplitude | BF3 | 0.473 | 0.723 | 0.325 | 0.622 | 1658.5 | 50 | 63.333 | 0.133 |
| BF4 | 0.431 | 0.359 | 0.284 | 0.578 | 1497 | 40 | 70 | 0.1 | |
| BC3 | 0.29 | 0.005 | 0.160 | 0.420 | 1518.5 | 40 | 15.333 | -0.067 | |
| BP3 | 0.398 | 0.174 | 0.250 | 0.546 | 1782.5 | 83.333 | 26.667 | 0.1 | |
| BP4 | 0.429 | 0.348 | 0.283 | 0.57624 | 1360.5 | 20 | 83.333 | 0.033 | |
| Combination | 0.746 | 0.001 | 0.619 | 0.872 | 0.453 | 66.667 | 83.333 | 0.5 | |
IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient; AUC, area under curve; LCL, lower confidence limit; UCL, upper confidence limit.
Figure 5.
The ROC curve of P300 and IVA-CPT in distinguishing ADHD patients from healthy volunteers, including latency (A), amplitude (B) and the area below the wave amplitude of P300 (C) as well as IVA-CPT (D). IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient; ROC, receiver operating characteristic curve.
Table 3.
Performance of Delong test of IVA-CPT and P300 for distinguishing ADHD patients from healthy volunteers
| Index | Difference between areas | Standard Error | 95% Confidence Interval | z statistic | Significance level | |
|---|---|---|---|---|---|---|
| IVA-CPT | FSRCQ-FSAQ | 0.01 | 0.0589 | -0.105 to 0.125 | 0.17 | 0.8652 |
| FSRCQ-ARCQ | 0.101 | 0.0507 | 0.00125 to 0.200 | 1.985 | 0.0472 | |
| FSRCQ-VRCQ | 0.0411 | 0.0291 | -0.0159 to 0.0981 | 1.414 | 0.1575 | |
| FSRCQ-AAQ | 0.00556 | 0.0545 | -0.101 to 0.112 | 0.102 | 0.9187 | |
| FSRCQ-VAQ | 0.0222 | 0.0578 | -0.0911 to 0.136 | 0.384 | 0.7007 | |
| FSAQ-ARCQ | 0.0906 | 0.0633 | -0.0335 to 0.215 | 1.431 | 0.1525 | |
| FSAQ-VRCQ | 0.0311 | 0.0662 | -0.0986 to 0.161 | 0.47 | 0.6383 | |
| FSAQ-AAQ | 0.00444 | 0.0145 | -0.0240 to 0.0329 | 0.306 | 0.7598 | |
| FSAQ-VAQ | 0.0122 | 0.017 | -0.0210 to 0.0455 | 0.72 | 0.4713 | |
| ARCQ-VRCQ | 0.0594 | 0.0699 | -0.0776 to 0.197 | 0.85 | 0.3954 | |
| ARCQ-AAQ | 0.095 | 0.0598 | -0.0223 to 0.212 | 1.588 | 0.1123 | |
| ARCQ-VAQ | 0.0783 | 0.0632 | -0.0455 to 0.202 | 1.24 | 0.2149 | |
| VRCQ-AAQ | 0.0356 | 0.0626 | -0.0871 to 0.158 | 0.568 | 0.5699 | |
| VRCQ-VAQ | 0.0189 | 0.0638 | -0.106 to 0.144 | 0.296 | 0.767 | |
| AAQ-VAQ | 0.0167 | 0.0266 | -0.0356 to 0.0689 | 0.625 | 0.5317 | |
| FSRCQ-Combination | 0.0728 | 0.0355 | 0.00317 to 0.142 | 2.049 | 0.0404 | |
| FSAQ-Combination | 0.0828 | 0.0392 | 0.00594 to 0.160 | 2.111 | 0.0347 | |
| ARCQ-Combination | 0.173 | 0.0514 | 0.0726 to 0.274 | 3.373 | 0.0007 | |
| VRCQ-Combination | 0.114 | 0.0441 | 0.0275 to 0.200 | 2.583 | 0.0098 | |
| AAQ-Combination | 0.0783 | 0.0354 | 0.00892 to 0.148 | 2.212 | 0.027 | |
| VAQ-Combination | 0.095 | 0.039 | 0.0186 to 0.171 | 2.438 | 0.0148 | |
| Amplitude | F3-F4 | 0.115 | 0.0579 | 0.00149 to 0.229 | 1.986 | 0.0471 |
| F3-C3 | 0.267 | 0.0685 | 0.133 to 0.402 | 3.9 | 0.0001 | |
| F3-P3 | 0.00222 | 0.0963 | -0.187 to 0.191 | 0.0231 | 0.9816 | |
| F3-P4 | 0.0989 | 0.0854 | -0.0685 to 0.266 | 1.158 | 0.2468 | |
| F3-Combination | 0.274 | 0.0685 | 0.140 to 0.408 | 3.996 | 0.0001 | |
| F4-C3 | 0.152 | 0.0557 | 0.0430 to 0.261 | 2.732 | 0.0063 | |
| F4-P3 | 0.113 | 0.083 | -0.0500 to 0.276 | 1.358 | 0.1744 | |
| F4-P4 | 0.0161 | 0.0708 | -0.123 to 0.155 | 0.228 | 0.8199 | |
| F4-Combination | 0.159 | 0.055 | 0.0511 to 0.267 | 2.888 | 0.0039 | |
| C3-P3 | 0.265 | 0.0664 | 0.135 to 0.395 | 3.993 | 0.0001 | |
| C3-P4 | 0.168 | 0.0535 | 0.0634 to 0.273 | 3.144 | 0.0017 | |
| C3-Combination | 0.00667 | 0.00487 | -0.00289 to 0.0162 | 1.368 | 0.1714 | |
| P3-P4 | 0.0967 | 0.0791 | -0.0583 to 0.252 | 1.222 | 0.2215 | |
| P3-Combination | 0.272 | 0.0661 | 0.142 to 0.401 | 4.111 | 0.0001 | |
| P4-Combination | 0.175 | 0.0529 | 0.0712 to 0.279 | 3.305 | 0.0009 | |
| Latency | QF3-QF4 | 0.0278 | 0.019 | -0.00954 to 0.0651 | 1.459 | 0.1446 |
| QF3-QC3 | 0.00611 | 0.0148 | -0.0230 to 0.0352 | 0.412 | 0.6805 | |
| QF3-QP3 | 0.0122 | 0.0176 | -0.0223 to 0.0468 | 0.693 | 0.4882 | |
| QF3-QP4 | 0.0422 | 0.0341 | -0.0247 to 0.109 | 1.237 | 0.2162 | |
| QF3-Combination | 0.01 | 0.00831 | -0.00629 to 0.0263 | 1.203 | 0.229 | |
| QF3-Combination | 0.01 | 0.00831 | -0.00629 to 0.0263 | 1.203 | 0.229 | |
| QF4-QC3 | 0.0217 | 0.0241 | -0.0257 to 0.0690 | 0.897 | 0.3696 | |
| QF4-QP3 | 0.0156 | 0.0267 | -0.0367 to 0.0678 | 0.583 | 0.5597 | |
| QF4-QP4 | 0.0144 | 0.041 | -0.0659 to 0.0948 | 0.353 | 0.7245 | |
| QF4-Combination | 0.0378 | 0.0207 | -0.00276 to 0.0783 | 1.827 | 0.0678 | |
| QC3-QP3 | 0.00611 | 0.0125 | -0.0184 to 0.0306 | 0.49 | 0.6244 | |
| QC3-QP4 | 0.0361 | 0.0326 | -0.0278 to 0.100 | 1.108 | 0.268 | |
| QC3-Combination | 0.0161 | 0.0115 | -0.00637 to 0.0386 | 1.405 | 0.1601 | |
| QP3-QP4 | 0.03 | 0.0335 | -0.0357 to 0.0957 | 0.894 | 0.3711 | |
| QP3-Combination | 0.0222 | 0.0147 | -0.00660 to 0.0510 | 1.511 | 0.1308 | |
| QP4-Combination | 0.0522 | 0.0325 | -0.0115 to 0.116 | 1.606 | 0.1083 | |
| Area below the wave amplitude | BF3-BF4 | 0.0422 | 0.0917 | -0.137 to 0.222 | 0.461 | 0.6451 |
| BF3-BC3 | 0.183 | 0.0941 | -0.00105 to 0.368 | 1.949 | 0.0513 | |
| BF3-BP3 | 0.0756 | 0.0778 | -0.0769 to 0.228 | 0.972 | 0.3313 | |
| BF3-BP4 | 0.0439 | 0.0983 | -0.149 to 0.237 | 0.447 | 0.6552 | |
| BF3-Combination | 0.219 | 0.0939 | 0.0348 to 0.403 | 2.331 | 0.0198 | |
| BF4-BC3 | 0.141 | 0.0925 | -0.0403 to 0.322 | 1.525 | 0.1273 | |
| BF4-BP3 | 0.0333 | 0.0922 | -0.147 to 0.214 | 0.362 | 0.7177 | |
| BF4-BP4 | 0.00167 | 0.0936 | -0.182 to 0.185 | 0.0178 | 0.9858 | |
| BF4-Combination | 0.177 | 0.0792 | 0.0215 to 0.332 | 2.231 | 0.0257 | |
| BC3-BP3 | 0.108 | 0.0838 | -0.0564 to 0.272 | 1.287 | 0.1982 | |
| BC3-BP4 | 0.139 | 0.0901 | -0.0372 to 0.316 | 1.547 | 0.1219 | |
| BC3-Combination | 0.0356 | 0.0339 | -0.0308 to 0.102 | 1.05 | 0.2937 | |
| BP3-BP4 | 0.0317 | 0.0958 | -0.156 to 0.219 | 0.331 | 0.7409 | |
| BP3-Combination | 0.143 | 0.0802 | -0.0139 to 0.301 | 1.787 | 0.074 | |
| BP4-Combination | 0.175 | 0.0727 | 0.0324 to 0.318 | 2.406 | 0.0161 |
IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient.
The value of P300 and IVA-CPT in identifying ADHD subtypes
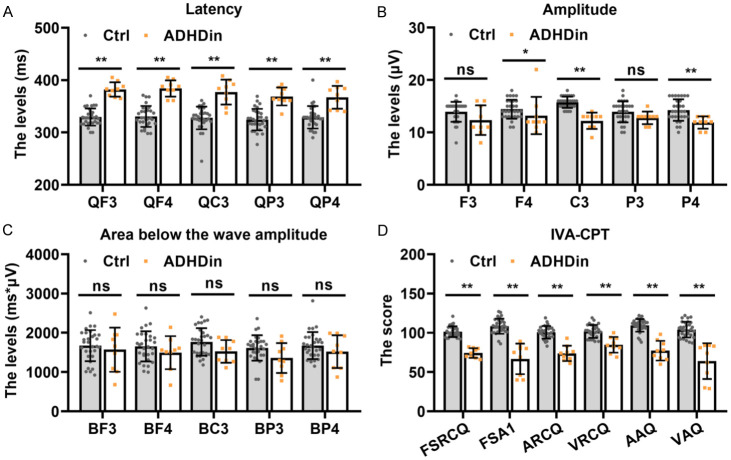
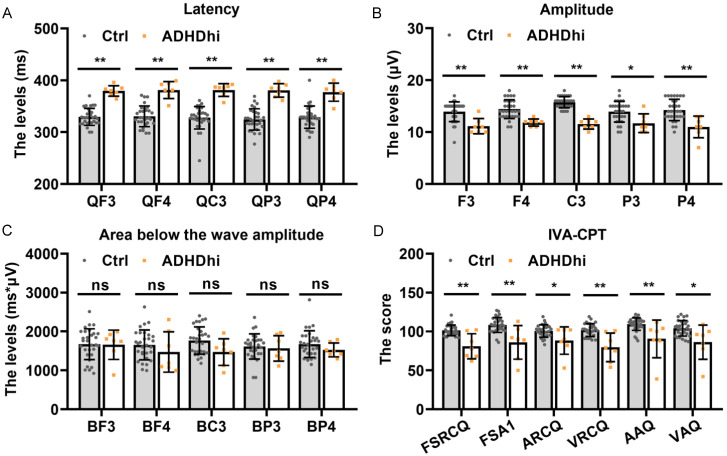
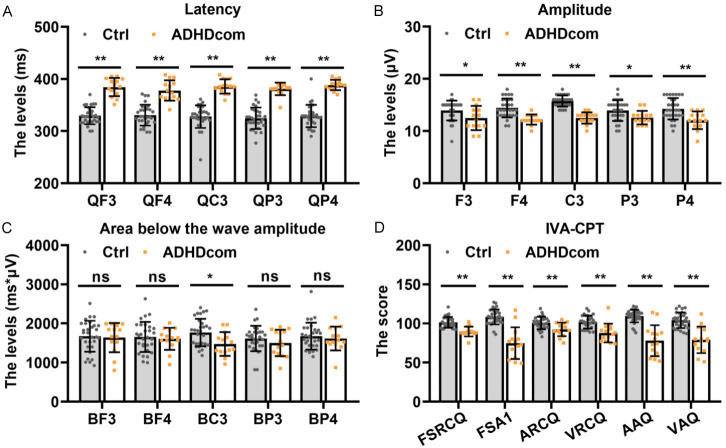
To evaluate the performance of P300 and IVA-CPT in different subtypes of ADHD, P300 and IVA-CPT were applied to patient cases with 3 types of ADHD: ADHD-inattention (ADHDin), ADHD-hyperactivity/impulsivity (ADHDhi), and ADHD-combination (ADHDcom). The latency value in identification of ADHDin showed a remarkable difference in QF3, QF4, QC3, QP3, and QP4 compared to the control group (see Figure 6A). The amplitude did not show a significant difference in QF3 between the control and ADHDin groups, but there was a significant decrease in other areas of the ADHDin group compared to the control group (Figure 6B). As shown in Figure 6C, there were no statistically significant differences in the level of area below the wave amplitude among all groups. In the IVA-CPT analysis, the scores yielded dramatically reduced values for all areas in the ADHDin group (Figure 6D).
Figure 6.
Evaluation of P300 and IVA-CPT in identifying ADHDin patients from healthy volunteers. The levels of latency (A), amplitude (B) and the area below the wave amplitude of P300 (C) as well as IVA-CPT (D). *P<0.05, **P<0.01 and ns= no significance. IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient; ADHDin, ADHD-inattention.
We also analyzed the identification performance of P300 and IVA-CPT in individuals with ADHDhi and ADHDcom. Significant differences in latency and amplitude of P300 analysis and the scores of IVA-CPT in all areas were observed between the control and ADHDhi group, but there was no difference in the area below wave amplitude between the two groups (Figure 7A-D). Similar results were found in the P300 and IVA-CPT analysis for individuals with ADHDcom (Figure 8A-D).
Figure 7.
Evaluation of P300 and IVA-CPT in identifying ADHDhi patients from healthy volunteers. The levels of latency (A), amplitude (B) and the area below the wave amplitude of P300 (C) as well as IVA-CPT (D). *P<0.05, **P<0.01 and ns= no significance. IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient; ADHDhi, ADHD-hyperactivity/impulsivity.
Figure 8.
Evaluation of P300 and IVA-CPT in identifying ADHDcom patients from healthy volunteers. The levels of latency (A), amplitude (B) and the area below the wave amplitude of P300 (C) as well as IVA-CPT (D). *P<0.05, **P<0.01 and ns= no significance. IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient; ADHDcom, ADHD-combination.
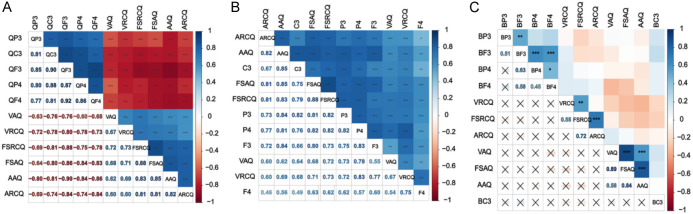
A pairwise comparison of control, ADHDin, ADHDhi and ADHDcom based on the index of P300 and IVA-CPT were measured, and the performance of IVA-CPT and P300 for distinguishing ADHD subtypes from healthy volunteers was analyzed by Delong test. The area below the wave amplitude had high accuracy in identification of control and ADHDin, ADHDhi, and ADHDcom (all AUC>0.737, which was higher than IVA_CPT and amplitude by Delong analysis (Tables 4, 5; Figure 9A-C). Moreover, the AUC value of latency and combination was 1.000 in ADHFin, ADHDhi, and ADHDcom compared to the control group. The results of Delong analysis in Table 5 showed that there was higher accuracy of latency and combination than area below the wave amplitude. However, the value of AUC varied greatly with difference index among ADHD subtypes, ranging from 0.449 to 0.746 (Table 6). IVA-CPT had a moderate performance in distinguishing ADHDin and ADHDhi (AUC=0.746). As shown in Table 7 and Figure 9D-F, the P300 and IVA-CPT did not differ distinctly between the different subtypes of ADHD. Overall, the results supported that P300 and IVA-CPT have the potential to diagnosis ADHD but not the ADHD subtypes.
Table 4.
Performance of IVA-CPT and P300 for distinguishing ADHD subtypes from healthy volunteers
| Index | AUC | Sig. | 95% LCL | 95% UCL | Cut off | Specificity | Sensitivity | Youden index | |
|---|---|---|---|---|---|---|---|---|---|
| ADHDin vs Healthy volunteers | IVA-CPT | 0.000 | 0.000 | 0.000 | 0.000 | 2.000 | 0.000 | 0.000 | 0.000 |
| Amplitude | 0.000 | 0.000 | 0.000 | 0.000 | 2.000 | 0.000 | 0.000 | 0.000 | |
| Latency | 1.000 | 0.000 | 1.000 | 1.000 | 0.500 | 100 | 0.000 | 1.000 | |
| Area below the wave amplitude | 0.737 | 0.033 | 0.563 | 0.911 | 0.471 | 77.778 | 66.667 | 0.444 | |
| Combination | 1.000 | 0.000 | 1.000 | 1.000 | 0.500 | 1.000 | 0.000 | 1.000 | |
| ADHDhi vs Healthy volunteers | IVA-CPT | 0.005 | 0.000 | 0.000 | 0.020 | 2.000 | 0.000 | 0.000 | 0.000 |
| Amplitude | 0.000 | 0.000 | 0.000 | 0.000 | 2.000 | 0.000 | 0.000 | 0.000 | |
| Latency | 1.000 | 0.000 | 1.000 | 1.000 | 0.500 | 1.000 | 0.000 | 1.000 | |
| Area below the wave amplitude | 0.767 | 0.030 | 0.568 | 0.965 | 0.453 | 85.714 | 73.333 | 0.59 | |
| Combination | 1.000 | 0.000 | 1.000 | 1.000 | 0.500 | 1.000 | 0.000 | 1.000 | |
| ADHDcom vs Healthy volunteers | IVA-CPT | 0.007 | 0.000 | 0.000 | 0.023 | 2.000 | 0.000 | 0.000 | 0.000 |
| Amplitude | 0.000 | 0.000 | 0.000 | 0.000 | 2.000 | 0.000 | 0.000 | 0.000 | |
| Latency | 1.000 | 0.000 | 1.000 | 1.000 | 0.500 | 1.000 | 0.000 | 1.000 | |
| Area below the wave amplitude | 0.740 | 0.011 | 0.582 | 0.899 | 0.453 | 85.714 | 66.667 | 0.524 | |
| Combination | 1.000 | 0.000 | 1.000 | 1.000 | 0.500 | 1.000 | 0.000 | 1.000 | |
IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; ADHDin, ADHD-inattention; ADHDhi, ADHD-hyperactivity/impulsivity; ADHDcom, ADHD-combination; AUC, area under curve; LCL, lower confidence limit; UCL, upper confidence limit.
Table 5.
Performance of Delong test of IVA-CPT and P300 for distinguishing ADHD subtypes from healthy volunteers
| Index | Difference between areas | Standard Error | 95% Confidence Interval | z statistic | Significance level | |
|---|---|---|---|---|---|---|
| ADHDin vs Healthy volunteers | IVA_CPT-Amplitude | 0 | 0 | 0.000 to 0.000 | 0 | 1 |
| IVA_CPT-Latency | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| IVA_CPT-Area_below_the_wave_amplitude | 0.263 | 0.0912 | 0.0842 to 0.442 | 2.883 | 0.0039 | |
| IVA_CPT-Combination | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Amplitude-Latency | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Amplitude-Area_below_the_wave_amplitude | 0.263 | 0.0912 | 0.0842 to 0.442 | 2.883 | 0.0039 | |
| Amplitude-Combination | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Latency-Area_below_the_wave_amplitude | 0.263 | 0.0912 | 0.0842 to 0.442 | 2.883 | 0.0039 | |
| Latency-Combination | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Area_below_the_wave_amplitude-Combination | 0.263 | 0.0912 | 0.0842 to 0.442 | 2.883 | 0.0039 | |
| ADHDhi vs Healthy volunteers | IVA_CPT-Amplitude | 0.00476 | 0.00673 | -0.00844 to 0.0180 | 0.707 | 0.4795 |
| IVA_CPT-Latency | 0.00476 | 0.00673 | -0.00844 to 0.0180 | 0.707 | 0.4795 | |
| IVA_CPT-Area_below_the_wave_amplitude | 0.229 | 0.108 | 0.0165 to 0.441 | 2.112 | 0.0347 | |
| IVA_CPT-Combination | 0.00476 | 0.00673 | -0.00844 to 0.0180 | 0.707 | 0.4795 | |
| Amplitude-Latency | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Amplitude-Area_below_the_wave_amplitude | 0.233 | 0.106 | 0.0248 to 0.442 | 2.193 | 0.0283 | |
| Amplitude-Combination | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Latency-Area_below_the_wave_amplitude | 0.233 | 0.106 | 0.0248 to 0.442 | 2.193 | 0.0283 | |
| Latency-Combination | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Area_below_the_wave_amplitude-Combination | 0.233 | 0.106 | 0.0248 to 0.442 | 2.193 | 0.0283 | |
| ADHDcom vs Healthy volunteers | IVA_CPT-Amplitude | 0.00714 | 0.00736 | -0.00728 to 0.0216 | 0.971 | 0.3318 |
| IVA_CPT-Latency | 0.00714 | 0.00736 | -0.00728 to 0.0216 | 0.971 | 0.3318 | |
| IVA_CPT-Area_below_the_wave_amplitude | 0.252 | 0.0842 | 0.0873 to 0.417 | 2.997 | 0.0027 | |
| IVA_CPT-Combination | 0.00714 | 0.00736 | -0.00728 to 0.0216 | 0.971 | 0.3318 | |
| Amplitude-Latency | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Amplitude-Area_below_the_wave_amplitude | 0.26 | 0.0825 | 0.0979 to 0.421 | 3.146 | 0.0017 | |
| Amplitude-Combination | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Latency-Area_below_the_wave_amplitude | 0.26 | 0.0825 | 0.0979 to 0.421 | 3.146 | 0.0017 | |
| Latency-Combination | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Area_below_the_wave_amplitude-Combination | 0.26 | 0.0825 | 0.0979 to 0.421 | 3.146 | 0.0017 |
IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; ADHDin, ADHD-inattention; ADHDhi, ADHD-hyperactivity/impulsivity; ADHDcom, ADHD-combination.
Figure 9.
The ROC curve among healthy volunteers and ADHD subtypes, (A) healthy volunteers vs ADHDin, (B) healthy volunteers vs ADHDhi, (C) healthy volunteers vs ADHDcom, (D) ADHDin vs ADHDhi, (E) ADHDin vs ADHDcom, (F) ADHDhi vs ADHDcom. IVA-CPT, integrated visual and auditory continuous performance test; ADHDin, ADHD-inattention; ADHDhi, ADHD-hyperactivity/impulsivity; ADHDcom, ADHD-combination; ROC, receiver operating characteristic curve.
Table 6.
Performance of IVA-CPT and P300 for distinguishing ADHD subtypes
| Index | AUC | Sig. | 95% LCL | 95% UCL | Cut off | Specificity | Sensitivity | Youden index | |
|---|---|---|---|---|---|---|---|---|---|
| ADHDin vs ADHDhi | IVA-CPT | 0.746 | 0.101 | 0.499 | 0.993 | 0.000 | 85.714 | 66.667 | 0.524 |
| Amplitude | 0.500 | 1.000 | 0.206 | 0.794 | 1.000 | 0.000 | 0.000 | 0.000 | |
| Latency | 0.500 | 1.000 | 0.206 | 0.794 | 2.000 | 0.000 | 0.000 | 0.000 | |
| Area below the wave amplitude | 0.571 | 0.634 | 0.269 | 0.874 | 0.536 | 85.714 | 55.556 | 0.413 | |
| Combination | 0.619 | 0.427 | 0.317 | 0.921 | 0.356 | 71.429 | 66.667 | 0.381 | |
| ADHDhi vs ADHDcom | IVA-CPT | 0.485 | 0.911 | 0.232 | 0.737 | 0.03 | 28.571 | 85.714 | 0.143 |
| Amplitude | 0.500 | 1.000 | 0.232 | 0.768 | 1.000 | 0.000 | 0.000 | 0.000 | |
| Latency | 0.500 | 1.000 | 0.232 | 0.768 | 2.000 | 0.000 | 0.000 | 0.000 | |
| Area below the wave amplitude | 0.449 | 0.709 | 0.180 | 0.718 | 0.687 | 42.857 | 71.43 | 0.143 | |
| Combination | 0.612 | 0.412 | 0.363 | 0.862 | 0.615 | 71.429 | 57.144 | 0.286 | |
| ADHDin vs ADHDcom | IVA-CPT | 0.690 | 0.131 | 0.463 | 0.918 | 0.000 | 85.714 | 55.556 | 0.413 |
| Amplitude | 0.500 | 1.000 | 0.253 | 0.747 | 1.000 | 0.000 | 0.000 | 0.000 | |
| Latency | 0.500 | 1.000 | 0.253 | 0.747 | 2.000 | 0.000 | 0.000 | 0.000 | |
| Area below the wave amplitude | 0.512 | 0.925 | 0.255 | 0.769 | 0.528 | 71.429 | 55.556 | 0.27 | |
| Combination | 0.683 | 0.147 | 0.453 | 0.912 | 0.464 | 92.857 | 44.446 | 0.373 | |
IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; ADHDin, ADHD-inattention; ADHDhi, ADHD-hyperactivity/impulsivity; ADHDcom, ADHD-combination; AUC, area under curve; LCL, lower confidence limit; UCL, upper confidence limit.
Table 7.
Performance of Delong test of IVA-CPT and P300 for distinguishing ADHD subtypes
| Index | Difference between areas | Standard Error | 95% Confidence Interval | z statistic | Significance level | |
|---|---|---|---|---|---|---|
| ADHDin vs ADHDhi | IVA_CPT-Amplitude | 0.246 | 0.13 | -0.00787 to 0.500 | 1.899 | 0.0575 |
| IVA_CPT-Latency | 0.246 | 0.13 | -0.00787 to 0.500 | 1.899 | 0.0575 | |
| IVA_CPT-Area_below_the_wave_amplitude | 0.175 | 0.221 | -0.258 to 0.607 | 0.791 | 0.4287 | |
| IVA_CPT-Combination | 0.127 | 0.0939 | -0.0570 to 0.311 | 1.353 | 0.1762 | |
| Amplitude-Latency | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Amplitude-Area_below_the_wave_amplitude | 0.0714 | 0.162 | -0.246 to 0.389 | 0.441 | 0.659 | |
| Amplitude-Combination | 0.119 | 0.162 | -0.198 to 0.436 | 0.736 | 0.4617 | |
| Latency-Area_below_the_wave_amplitude | 0.0714 | 0.162 | -0.246 to 0.389 | 0.441 | 0.659 | |
| Latency-Combination | 0.119 | 0.162 | -0.198 to 0.436 | 0.736 | 0.4617 | |
| Area_below_the_wave_amplitude-Combination | 0.0476 | 0.19 | -0.324 to 0.419 | 0.251 | 0.8018 | |
| ADHDhi vs ADHDcom | IVA_CPT-Amplitude | 0.0153 | 0.133 | -0.245 to 0.275 | 0.115 | 0.9082 |
| IVA_CPT-Latency | 0.0153 | 0.133 | -0.245 to 0.275 | 0.115 | 0.9082 | |
| IVA_CPT-Area_below_the_wave_amplitude | 0.0357 | 0.117 | -0.194 to 0.266 | 0.304 | 0.7609 | |
| IVA_CPT-Combination | 0.0969 | 0.187 | -0.269 to 0.463 | 0.519 | 0.6039 | |
| Amplitude-Latency | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Amplitude-Area_below_the_wave_amplitude | 0.051 | 0.143 | -0.229 to 0.331 | 0.357 | 0.7213 | |
| Amplitude-Combination | 0.112 | 0.132 | -0.146 to 0.370 | 0.852 | 0.3941 | |
| Latency-Area_below_the_wave_amplitude | 0.051 | 0.143 | -0.229 to 0.331 | 0.357 | 0.7213 | |
| Latency-Combination | 0.112 | 0.132 | -0.146 to 0.370 | 0.852 | 0.3941 | |
| Area_below_the_wave_amplitude-Combination | 0.0612 | 0.147 | -0.226 to 0.349 | 0.417 | 0.6765 | |
| ADHDin vs ADHDcom | IVA_CPT-Amplitude | 0.19 | 0.119 | -0.0419 to 0.423 | 1.606 | 0.1082 |
| IVA_CPT-Latency | 0.19 | 0.119 | -0.0419 to 0.423 | 1.606 | 0.1082 | |
| IVA_CPT-Area_below_the_wave_amplitude | 0.179 | 0.207 | -0.227 to 0.584 | 0.864 | 0.3878 | |
| IVA_CPT-Combination | 0.00794 | 0.0825 | -0.154 to 0.170 | 0.0962 | 0.9234 | |
| Amplitude-Latency | 0 | 0 | 0.000 to 0.000 | 0 | 1 | |
| Amplitude-Area_below_the_wave_amplitude | 0.0119 | 0.136 | -0.254 to 0.278 | 0.0876 | 0.9302 | |
| Amplitude-Combination | 0.183 | 0.12 | -0.0535 to 0.419 | 1.516 | 0.1296 | |
| Latency-Area_below_the_wave_amplitude | 0.0119 | 0.136 | -0.254 to 0.278 | 0.0876 | 0.9302 | |
| Latency-Combination | 0.183 | 0.12 | -0.0535 to 0.419 | 1.516 | 0.1296 | |
| Area_below_the_wave_amplitude-Combination | 0.171 | 0.236 | -0.291 to 0.632 | 0.724 | 0.4688 |
IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; ADHDin, ADHD-inattention; ADHDhi, ADHD-hyperactivity/impulsivity; ADHDcom, ADHD-combination.
Correlation between P300 and IVA-CPT in ADHD patients
To better understand the agreement of ADHD between the IVA-CPT index and P300 component, the results of the confusion matrix were shown in Figure 10. In terms of latency, the IVA-CPT quotients were found to have a negative correlation with QF3, QC3, QF4, QP3 and QP4, as demonstrated in Figure 10A. Interestingly, a negative correlation was also discovered between the P300 component and AAQ, VRCQ, ARCQ, FSAQ and FSRCQ of IVA-CPT. Moreover, a positive correlation was noted in VAQ and F3, C3, F4, P3 and P4 (Figure 10B). Similar patterns were observed in AAQ, VRCQ, ARCQ, FSAQ and FSRCQ, demonstrated in Figure 10B. Through Pearson correlation analysis, however, we did not find any correlation between IVA-CPT and the area below the wave amplitude (P>0.05, Figure 10C). Together, these data provided evidence that P300 shows substantial agreement with IVA-CPT in the diagnosis of ADHD.
Figure 10.
The correlation between P300 and IVA-CPT of ADHD patients. A. The correlation between the latency and IVA-CPT of ADHD patients. B. The correlation between amplitude and IVA-CPT of ADHD patients. C. The correlation between area below the wave amplitude and IVA-CPT of ADHD patients. IVA-CPT, integrated visual and auditory continuous performance test; ADHD, attention deficit hyperactivity disorder; FSAQ, full scale attention quotient; AAQ, auditory attention quotient; VAQ, visual attention quotient; FSRCQ, full scale response control quotient; ARCQ, auditory response control quotient; VRCQ, visual response control quotient.
Discussion
The ERPs is a noninvasive technique in electro-neurophysiology that reflects the cognitive processes associated with attention tasks [19,20]. Previous studies on ERPs have confirmed that patients with ADHD have abnormal sensation or cognitive information processing abilities, based on work by Kaur S, Singh S, Arun P, et al. [21,22]. P300 is the most extensively investigated ERP [23]. It is mainly used in the novel auditory oddball task to derive ERPs. The integrated visual and auditory continuous performance test (IVA-CPT), as a neuropsychological measure, can assess auditory and visual attention in the same task [24,25]. However, pronounced knowledge gaps remain regarding the efficiency difference between IVA-CPT and P300 in diagnosing ADHD. In this study, we performed IVA-CPT and P300 measurements on 30 patients with ADHD and 30 age-matched healthy volunteers.
The latency of P300 reflects the brain’s speed in categorizing, coding and recognizing external stimuli, and reflects the response time for categorizing stimuli [26]. Prolonged latency of P300 indicates a deficiency in attention processing function and a slowing down of brain processing speed [27]. The amplitude of P300 represents the degree of resources activated by the brain during processing. It is also considered to be related to the deficiency in the inhibition control function. Compared to healthy volunteers, we observed longer latency and lower amplitude in ADHD subtypes, reflecting behavior disinhibition, behavior control disorder and central nerve hyperexcitation in ADHD patients. However, some studies have reported indicating that there are no statistically significant differences in the latency of the P300 wave between the ADHD and control group [28]. The contradictory results may be attributed to the different inclusion criteria and study methods used by researchers. Interestingly, the area below the wave amplitude of P300 in BC3 was related to the wave amplitude and the wave duration, indicating the memory time traces of the subjects. There have been no previous reports on the area below the wave amplitude in the past. But there were no statistically significant differences in the above two indexes of P300 among ADHDin, ADHDhi and ADHDcom groups. It can possibly be that when comparing the different subtypes of ADHD, the number of subjects in the various groups are small and uneven, which can affect the comparison results and cause insignificant differences in the area below the wave amplitude. We also considered the influence of age and gender on the diagnostic performance of P300 and IVA-CPT in ADHD. There were no differences in P300 and IVA-CPT performance between different age and sex ADHD patients.
Among the various indexes of the IVA-CPT, the control quotient is primarily used to assess the overall coordination ability and willpower control ability of the study subjects, indicating the incorrect selection of the behavior indexes (mainly for measuring the hyperactivity of the subjects). The attention quotient is used to measure the attention and sensitivity to changes of the study subjects, indicating the selection of behavior indexes (mainly measuring the attention of the study subjects) [29,30]. Hyperactive impulses and attention defects of ADHD patients are mainly assessed through incorrect selection and miss-selection of operations in the test [30]. We measured the scores of AAQ, VRCQ, ARCQ, FSAQ and FSRCQ to evaluate the performance of ADHD. We observed that ADHD patients performed worse on the full and secondary scales for attention and response accuracy compared to healthy volunteers, indicating that ADHD patients suffer from attention function deficiencies and inhibition control issues. These study results are consistent with overseas studies, indicating that the IVA-CPT has high accuracy for diagnosing ADHD [31]. The score of the IVA-CPT was similar to the result of P300 in ADHD patients with different genders and ages. However, the IVA-CPT could not distinguish among the three subtypes of ADHD.
Although the current clinical diagnosis of ADHD relies mainly on the patient’s medical history and early symptoms, we believe that IVA-CPT and ERPs (P300) can provide more objective evidence for diagnosing ADHD. In addition, it is worth noting that although there have been numerous studies on P300 both home and abroad, most of the stimulants are based on audio elements (sounds) [32,33]. Given that the amount of information obtained through vision is significantly greater than that from the auditory sense in the learning process, therefore, we assessed the diagnostic efficiency of IVA-CPT and P300 (auditory sense) in distinguishing ADHD patients from healthy volunteers using ROC curve analysis. Berger et al. [34] revealed fair to excellent diagnostic ability in all CPT indices except impulsivity, which had poor ability to distinguish ADHD children from controls. Interestingly, we found that the component of IVA-CPT exhibited relatively strong discriminatory ability. In particular, the combined component yielded better results than each individual component. The total score yielded excellent diagnostic performance. Therefore, further large-sample studies are required to validate our finding. Additionally, we used Delong test to demonstrate that the latency and amplitude components, but not the area below the wave amplitude which displayed higher AUC values in distinguishing ADHD patients from healthy volunteers. Therefore, the latency and amplitude components hold promising potential as biomarker candidates for ADHD diagnosis. Furthermore, the combination diagnosis of P300 and IVA-CPT could improve the diagnostic efficiently and accurately for ADHD patients compared with single index of P300 and IVA-CPT. The current study further expands the knowledge of IVA-CPT in evaluating ADHD. However, the identifying performance of ADHD subtypes based on the P300 wave and IVA-CPT tests was poor.
The study produced interesting results. We observed strong performance and accuracy of P300 and IVA-CPT in identifying individuals with ADHD and those in the control group, with no correlation to age and gender. However, in different subtypes of ADHD (ADHDin, ADHDhi and ADHDcom), P300 and IVA-CPT were unable to accurately distinguish among them. Therefore, other diagnostic methods are necessary for diagnosing of ADHD subtypes. More importantly, the performance of the P300 and IVA-CPT in diagnosing ADHD subtypes should be further analyzed.
However, there are some limitations in the study. The number of subjects in this study is relatively low, making it difficult to analyze the data for different ADHD subtypes. Therefore, in the future, more studies should be conducted with a larger number of participators that consist of more subtypes of ADHD from multiple hospitals. In terms of ethnicity, the research was conducted in an Asian population. Thus, it is unclear whether IVA-CPT and P300 would have the same predictive value in Caucasian and African groups. A multicenter study is necessary to further validate the effectiveness of IVA-CPT and P300 in diagnosing ADHD.
In conclusion, the significant changes in latency and amplitude of P300, as well as the score of IVA-CPT were identified as useful candidate biomarkers for screening ADHD. Our findings highlight the potential clinical diagnostic value of IVA-CPT and P300 in patients with ADHD.
Acknowledgements
This work was supported by Zhejiang Province Natural Science Foundation (No.: LY13H090012).
All participants or their legal guardians provided written informed consent to participate in this study.
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Magnin E, Maurs C. Attention-deficit/hyperactivity disorder during adulthood. Rev Neurol (Paris) 2017;173:506–515. doi: 10.1016/j.neurol.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Rubia K, Westwood S, Aggensteiner PM, Brandeis D. Neurotherapeutics for attention deficit/hyperactivity disorder (ADHD): a review. Cells. 2021;10:2156. doi: 10.3390/cells10082156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fawns T. Attention deficit and hyperactivity disorder. Prim Care. 2021;48:475–491. doi: 10.1016/j.pop.2021.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Brikell I, Burton C, Mota NR, Martin J. Insights into attention-deficit/hyperactivity disorder from recent genetic studies. Psychol Med. 2021;51:2274–2286. doi: 10.1017/S0033291721000982. [DOI] [PubMed] [Google Scholar]
- 5.Hinshaw SP, Nguyen PT, O’Grady SM, Rosenthal EA. Annual research review: attention-deficit/hyperactivity disorder in girls and women: underrepresentation, longitudinal processes, and key directions. J Child Psychol Psychiatry. 2022;63:484–496. doi: 10.1111/jcpp.13480. [DOI] [PubMed] [Google Scholar]
- 6.Pérez-Gómez J, Amigo-Gamero H, Collado-Mateo D, Barrios-Fernandez S, Muñoz-Bermejo L, Garcia-Gordillo MÁ, Carlos-Vivas J, Adsuar JC. Equine-assisted activities and therapies in children with attention-deficit/hyperactivity disorder: a systematic review. J Psychiatr Ment Health Nurs. 2021;28:1079–1091. doi: 10.1111/jpm.12710. [DOI] [PubMed] [Google Scholar]
- 7.Penengo C, Colli C, Bonivento C, Boscutti A, Balestrieri M, Delvecchio G, Brambilla P. Auditory event-related electroencephalographic potentials in borderline personality disorder. J Affect Disord. 2022;296:454–464. doi: 10.1016/j.jad.2021.09.096. [DOI] [PubMed] [Google Scholar]
- 8.Arjona-Valladares A, Fondevila-Estévez S, Fernández-Linsenbarth I, Díez Á, Ruiz-Sanz FJ, Rodríguez-Lorenzana A, Molina V. Event-related potentials associated to N-back test performance in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2021;111:110347. doi: 10.1016/j.pnpbp.2021.110347. [DOI] [PubMed] [Google Scholar]
- 9.Silkes JP, Anjum J. The role and use of event-related potentials in aphasia: a scoping review. Brain Lang. 2021;219:104966. doi: 10.1016/j.bandl.2021.104966. [DOI] [PubMed] [Google Scholar]
- 10.Ewen JB, Puts NA, Mostofsky SH, Horn PS, Gilbert DL. Associations between task-related modulation of motor-evoked potentials and EEG event-related desynchronization in children with ADHD. Cereb Cortex. 2021;31:5526–5535. doi: 10.1093/cercor/bhab176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fortin J, Grondin S, Blanchet S. Event-related potentials of episodic encoding after traumatic brain injury in older adults. Brain Res. 2021;1766:147504. doi: 10.1016/j.brainres.2021.147504. [DOI] [PubMed] [Google Scholar]
- 12.Häger LA, Åsberg Johnels J, Kropotov JD, Weidle B, Hollup S, Zehentbauer PG, Gillberg C, Billstedt E, Ogrim G. Biomarker support for ADHD diagnosis based on event related potentials and scores from an attention test. Psychiatry Res. 2021;300:113879. doi: 10.1016/j.psychres.2021.113879. [DOI] [PubMed] [Google Scholar]
- 13.Kamita MK, Silva LAF, Magliaro FCL, Fernandes FD, Matas CG. Auditory event related potentials in children with autism spectrum disorder. Int J Pediatr Otorhinolaryngol. 2021;148:110826. doi: 10.1016/j.ijporl.2021.110826. [DOI] [PubMed] [Google Scholar]
- 14.Cui C, Zhang K, Du XM, Sun X, Luo J. Event-related potentials support the mnemonic effect of spontaneous insight solution. Psychol Res. 2021;85:2518–2529. doi: 10.1007/s00426-020-01421-1. [DOI] [PubMed] [Google Scholar]
- 15.Wang FH, Sun LY, Cui XM, Zhao HD, Yang LF, Wang Z, Shi TK. Comparative efficacy of targeted structural patterns of electroencephalography neurofeedback in children with inattentive or combined attention deficit hyperactivity disorder. Brain Behav. 2022;12:e2572. doi: 10.1002/brb3.2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ord AS, Miskey HM, Lad S, Richter B, Nagy K, Shura RD. Examining embedded validity indicators in conners continuous performance test-3 (CPT-3) Clin Neuropsychol. 2021;35:1426–1441. doi: 10.1080/13854046.2020.1751301. [DOI] [PubMed] [Google Scholar]
- 17.Moreno-García I, Delgado-Pardo G, Roldán-Blasco C. Attention and response control in ADHD. Evaluation through integrated visual and auditory continuous performance test. Span J Psychol. 2015;18:E1. doi: 10.1017/sjp.2015.2. [DOI] [PubMed] [Google Scholar]
- 18.Battle DE. Diagnostic and statistical manual of mental disorders (DSM) Codas. 2013;25:191–192. doi: 10.1590/s2317-17822013000200017. [DOI] [PubMed] [Google Scholar]
- 19.O’Reilly JA. Event-related potential arithmetic to analyze offset potentials from conscious mice. J Neurosci Methods. 2019;318:78–83. doi: 10.1016/j.jneumeth.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 20.Leynes PA, Crawford CJ. Event-related potential (ERP) evidence that encoding focus alters recollected features. Brain Cogn. 2018;127:42–50. doi: 10.1016/j.bandc.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Kaur S, Singh S, Arun P, Kaur D, Bajaj M. Event-related potential analysis of ADHD and control adults during a sustained attention task. Clin EEG Neurosci. 2019;50:389–403. doi: 10.1177/1550059419842707. [DOI] [PubMed] [Google Scholar]
- 22.Gamma A, Kara O. Event-related potentials for diagnosing children and adults with ADHD. J Atten Disord. 2020;24:1581–1587. doi: 10.1177/1087054716631821. [DOI] [PubMed] [Google Scholar]
- 23.Gu L, Zhang Z. Exploring potential electrophysiological biomarkers in mild cognitive impairment: a systematic review and meta-analysis of event-related potential studies. J Alzheimers Dis. 2017;58:1283–1292. doi: 10.3233/JAD-161286. [DOI] [PubMed] [Google Scholar]
- 24.MacDonald B, Sadek J. Naturalistic exploratory study of the associations of substance use on ADHD outcomes and function. BMC Psychiatry. 2021;21:251. doi: 10.1186/s12888-021-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moreno-García I, Meneres-Sancho S, Camacho-Vara de Rey C, Servera M. A randomized controlled trial to examine the posttreatment efficacy of neurofeedback, behavior therapy, and pharmacology on ADHD measures. J Atten Disord. 2019;23:374–383. doi: 10.1177/1087054717693371. [DOI] [PubMed] [Google Scholar]
- 26.Uvais NA, Nizamie SH, Das B, Praharaj SK, Ul Haq Katshu MZ. Auditory P300 event-related potential: normative data in the Indian population. Neurol India. 2018;66:176–180. doi: 10.4103/0028-3886.222874. [DOI] [PubMed] [Google Scholar]
- 27.Althen H, Banaschewski T, Brandeis D, Bender S. Stimulus probability affects the visual N700 component of the event-related potential. Clin Neurophysiol. 2020;131:655–664. doi: 10.1016/j.clinph.2019.11.059. [DOI] [PubMed] [Google Scholar]
- 28.Dimoska A, Johnstone SJ, Barry RJ, Clarke AR. Inhibitory motor control in children with attention-deficit/hyperactivity disorder: event-related potentials in the stop-signal paradigm. Biol Psychiatry. 2003;54:1345–1354. doi: 10.1016/s0006-3223(03)00703-0. [DOI] [PubMed] [Google Scholar]
- 29.Fang Y, Han D, Luo H. A virtual reality application for assessment for attention deficit hyperactivity disorder in school-aged children. Neuropsychiatr Dis Treat. 2019;15:1517–1523. doi: 10.2147/NDT.S206742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim J, Lee Y, Han D, Min K, Kim D, Lee C. The utility of quantitative electroencephalography and Integrated visual and auditory continuous performance test as auxiliary tools for the attention deficit hyperactivity disorder diagnosis. Clin Neurophysiol. 2015;126:532–540. doi: 10.1016/j.clinph.2014.06.034. [DOI] [PubMed] [Google Scholar]
- 31.Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490–499. doi: 10.1007/s13311-012-0135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chi MH, Chu CL, Lee IH, Hsieh YT, Chen KC, Chen PS, Yang YK. Altered auditory P300 performance in parents with attention deficit hyperactivity disorder offspring. Clin Psychopharmacol Neurosci. 2019;17:509–516. doi: 10.9758/cpn.2019.17.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chu CL, Lee IH, Chi MH, Chen KC, Chen PS, Yao WJ, Chiu NT, Yang YK. Availability of dopamine transporters and auditory P300 abnormalities in adults with attention-deficit hyperactivity disorder: preliminary results. CNS Spectr. 2018;23:264–270. doi: 10.1017/S1092852917000049. [DOI] [PubMed] [Google Scholar]
- 34.Berger I, Slobodin O, Cassuto H. Usefulness and validity of continuous performance tests in the diagnosis of attention-deficit hyperactivity disorder children. Arch Clin Neuropsychol. 2017;32:81–93. doi: 10.1093/arclin/acw101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.