Abstract
Objective: To identify the independent risk factors for postpartum depression in elderly primiparas and to evaluate the effects of mindfulness-based psychological intervention. Methods: A retrospective analysis was conducted on 75 women with postpartum depression who received treatment at the First Hospital of Nanchang from January 2021 to March 2022. Among them, 33 women who received routine psychological health management were included in the control group, while the remaining 42 who received mindfulness-based psychological intervention on the basis of routine psychological health management were included in the study group. In addition, 80 women without postpartum depression who delivered during the same period at our hospital were selected as the non-depression group. The self-cognitive function scores, depression and anxiety scores, sleep quality and progesterone level were compared between the two groups before and after the intervention. Logistic regression analysis was used to identify the influencing factors for postpartum depression in elderly primiparas. Results: Before the intervention, no significant difference was found in General Self-Efficacy Scale (GSES) scores between the two groups (P > 0.05). After the intervention, the GSES scores significantly improved in both groups, with the study group showing a significantly higher improvement compared to the control group (P < 0.05). Before the intervention, no significant difference was observed between the two groups in Edinburgh Postnatal Depression Scale (EPDS) and 7-item Generalized Anxiety Disorder Questionnaire (GAD-7) scores (all P > 0.05). After the intervention, the EPDS and GAD-7 scores significantly decreased in both groups, with the study group showing a significantly greater reduction compared to the control group (all P < 0.05). Before the intervention, no significant difference was found in Pittsburgh Sleep Quality Index (PSQI) scores between the two groups (P > 0.05). After the intervention, the PSQI scores notably decreased in both groups, with the study group showing notably lower scores compared to the control group (P < 0.05). Before the intervention, there was no significant difference in progesterone levels between the two groups (P > 0.05). After the intervention, progesterone levels significantly decreased in both groups, and the intervention group showed significantly lower levels compared to the control group (P < 0.05). Logistic regression analysis identified age (P < 0.0001; OR: 5.471; 95% CI: 2.504-11.956), education level (P = 0.029; OR: 2.370; 95% CI: 1.094-5.137), pregnancy complications (P = 0.006; OR: 3.665; 95% CI: 1.460-9.199), and newborn Apgar score (P = 0.046; OR: 2.895; 95% CI: 1.017-8.242) as independent risk factors for postpartum depression in elderly primiparas. Conclusion: Mindfulness-based psychological intervention demonstrates positive effects on enhancing self-efficacy, emotional well-being, and sleep quality among elderly primiparas experiencing postpartum depression. Additionally, advanced maternal age, higher education level, presence of pregnancy complications, and relatively lower newborn Apgar score are independent risk factors for postpartum depression in elderly primiparas.
Keywords: Elderly primiparas, postpartum depression, mindfulness-based psychological intervention, self-efficacy, anxiety
Introduction
In recent years, there has been a growing trend of delayed childbirth due to societal advancements, changes in reproductive attitudes, and the availability of assisted reproductive technologies [1]. Additionally, factors such as miscarriage and uterine fibroids also affect women’s fertility, contributing to the increased number of primiparas (first-time postpartum women) at advanced maternal age (≥ 35 years) [2]. Advanced maternal age is often considered as one of the high-risk factors in obstetrics, which can lead to psychological stress in pregnant women, with anxiety, fear, and depression being the most common [3]. Psychological issues arising during the postpartum period can significantly impact maternal recovery by disrupting sleep patterns, impeding physical healing, affecting caregiving abilities, and potentially contributing to the development of postpartum depression [4]. Postpartum depression is a prevalent mental health issue that significantly impacts both the mother and the family. Current interventions for postpartum depression include psychological counselling, cognitive-behavioral therapy, medication, and supportive care [3]. However, several challenges remain in effectively treating postpartum depression. First, there may be difficulties in identifying and diagnosing postpartum depression since the mothers often hesitate to report their psychological distress or symptoms. Second, concerns about the effects of medication on breastfeeding may prevent some mothers from pharmacological treatments [4]. Furthermore, psychological counselling and cognitive-behavioral therapy require a significant amount of time and ongoing participation, which can be challenging for new mothers, especially those caring for a newborn [4]. Elderly primiparas are at a higher risk of developing postpartum depression [5], with several independent risk factors influencing this outcome. Understanding these factors is crucial for providing appropriate interventions and support [6]. In recent years, mindfulness-based psychological interventions, grounded in the theory of mindfulness, has been gaining clinical attention. These interventions aim to guide postpartum women to accept and experience various internal and external stimuli without judgment, gradually changing their attitudes and perceptions towards life [7]. While mindfulness interventions have shown benefits in other populations, research specifically focused on postpartum women remains limited. The psychological well-being of postpartum women encounters a diverse challenges during the late stages of childbirth and the parenting process. Therefore, it is crucial to explore and evaluate the effectiveness of mindfulness interventions in this population.
This study aimed to explore the effects of mindfulness-based psychological intervention in alleviating postpartum depression among elderly primiparas and to identify the independent risk factors for postpartum depression in this population. The goal was to provide a more comprehensive understanding and develop effective intervention strategies to enhance the psychological well-being of elderly primiparas. The innovation of this study lies in its focus on addressing postpartum depression in older primiparous women and utilizing mindfulness-based interventions, as well as identification of independent risk factors associated with postpartum depression. Mindfulness interventions emphasize self-awareness, emotion regulation, and mind-body connection, offering a low-dependency and low-risk approach to managing postpartum depression.
Methods and materials
Sample information
A retrospective analysis was conducted on the data from 75 postpartum women who received treatment at the First Hospital of Nanchang from January 2021 to March 2022. Among them, 33 women who received routine psychological health management were included in the control group, while the remaining 42 who received mindfulness-based psychological intervention in addition to routine psychological health management were included in the study group. Additionally, 80 postpartum women without depression who delivered during the same period at the First Hospital of Nanchang were selected as the non-depression group. This study was conducted after obtaining approval from the Ethics Committee of the First Hospital of Nanchang.
Inclusion and exclusion criteria
Inclusion criteria: Postpartum women who met the clinical diagnostic criteria for postpartum depression [8]: age ≥ 35 years, primipara, within 6 weeks post-delivery; postpartum women with Edinburgh Postnatal Depression Scale (EPDS) score ≥ 9 points; postpartum women without other chronic diseases; postpartum women with good understanding and communication abilities, and complete clinical data.
Exclusion criteria: Postpartum women who were taking antidepressant medications; postpartum women with a history of mental illness or family history of mental illness; postpartum women with significant organ dysfunctions (brain, heart, liver, kidneys, etc.).
Intervention methods
Control group: Routine psychological health management was provided to the control group. This included techniques to manage pain and emotional anxiety associated with postpartum physical discomfort. For example, attention diversion techniques were employed when the postpartum women experienced pain, and appropriate analgesic medications were provided as needed. Additionally, the women were educated on the causes of postpartum depression, self-health management strategies, and various intervention measures to enhance their understanding of the condition. They were encouraged to actively participate in psychological counseling sessions and to adhere to medical advice, including taking prescribed medications as necessary.
Study group: In addition to routine psychological health management, the study group received mindfulness-based psychological intervention. A WeChat discussion group was established, and the women were invited to join. Mindfulness guidance texts or videos were shared in the group, encouraging timely learning. The intervention included the following components: (1) Mindfulness-based stress reduction techniques were introduced, and training manuals and videos were distributed. Beneficiaries of mindfulness-based stress reduction were invited to share their experiences to enhance confidence in the intervention among postpartum women. Participants were encouraged to engage in introductory training with relaxing background music, while remote nursing staff guided them in entering a state of mindfulness through proper breathing techniques. Emphasis was placed on calming the minds, gradually focusing on the breath and providing detailed descriptions of their experiences. Mindfulness breathing techniques were summarized, and women were allowed to choose their preferred posture for self-practice. (2) The staff guided the women in practicing mindful walking, breathing, eating, and other behaviors and encouraged them to let go of distractions and focus on their surroundings (such as air, the ground, or food) and their own bodies for 20 minutes. (3) Meditation training was conducted through videos. The participants were instructed to sit quietly in a calm environment for 20 minutes, feeling their emotions and thoughts and experiencing the process of arising and dissipating. (4) The nursing staff taught the new mothers how to effectively identify their negative emotions and guided them in practicing self-reflection. (5) The nursing staff guided the women to recognize and reflect on their negative thoughts.
The women were regularly reminded through the WeChat group to practice daily and adhere to the exercises for 8 weeks.
Data collection
Clinical data and various indicator data of the postpartum women were collected through the Laboratory Information System, including age, pre-pregnancy body mass index (BMI), educational level, fetal gender, pregnancy complications, mode of delivery, newborn Apgar scores, lifestyle status, and various scores.
Outcome measures
(1) Baseline data comparison between the two groups was conducted, including age, pre-pregnancy BMI, educational level, fetal gender, pregnancy complications, and mode of delivery. (2) The General Self-Efficacy Scale (GSES) was adopted to analyze the changes in self-perceived cognitive functioning scores before and after the intervention in postpartum women. The scale has a maximum score of 40, with higher scores indicating better cognitive functioning [9]. (3) The Edinburgh Postnatal Depression Scale (EPDS) was adopted to analyze the depression levels in postpartum women. The scale consists of 10 items, scored on a 4-point scale (0, 1, 2, 3), with a total score ranging from 0 to 30. Higher scores indicate more severe depression [10]. (4) The 7-item Generalized Anxiety Disorder Questionnaire (GAD-7) was adopted to analyze the anxiety levels before and after the intervention in postpartum women [11]. The GAD-7 consists of 7 items, including symptoms such as nervousness, restlessness, and irritability. Each item has 4 response options, scored from 0 to 3, resulting in a total score ranging from 0 to 21. Higher scores indicate poorer emotional states, and scores above 5 suggest the presence of mild anxiety. (5) The Pittsburgh Sleep Quality Index (PSQI) was used to assess the sleep quality before and after the intervention in postpartum women [12]. The total score ranges from 0 to 21, with higher scores indicating a higher degree of sleep disturbances. (6) Before and 8 weeks after the intervention, venous blood samples (5 mL) were collected from the postpartum women and centrifuged to obtain plasma, which was then stored at -80°C for future use. Then, progesterone in the serum was determined using enzyme-linked immunosorbent assay (ELISA; Abcam; kit number: ab108670). (7) Logistic multiple regression analysis was used to identify risk factors for postpartum depression in older primiparous women.
Statistical analysis
Statistical analysis was performed using SPSS 20.0 (IBM Corp, Armonk, NY, USA), and graphs were created using GraphPad Prism 7 (GraphPad Software, San Diego, USA). Counting data were presented as [n (%)] and compared between groups via the chi-square test. Measurement data were normally distributed and expressed as mean ± standard deviation (x±sd), and the comparison between the two groups was conducted using the t-test. Logistic multiple regression analysis was conducted to identify independent risk factors influencing the occurrence of postpartum depression in elderly primiparas. P < 0.05 was considered statistically significant.
Results
Baseline data comparison
A comparison of baseline data between the control and study groups revealed no significant differences regarding age, gender, pre-pregnancy BMI, educational level, and other clinical baseline data (all P > 0.05, Table 1).
Table 1.
Comparison of baseline data between the two groups
| Factors | Study group (n = 42) | Control group (n = 33) | χ2/t | P |
|---|---|---|---|---|
| Age | 0.2511 | 0.6163 | ||
| 35-44 years | 31 | 26 | ||
| ≥ 45 years | 11 | 7 | ||
| Pre-pregnancy BMI | 0.0914 | 0.7624 | ||
| ≥ 23 kg/m2 | 24 | 20 | ||
| < 23 kg/m2 | 18 | 13 | ||
| Education level | 0.2064 | 0.9765 | ||
| Below junior high school | 2 | 1 | ||
| Senior high school | 9 | 8 | ||
| Junior college | 18 | 14 | ||
| Bachelor or above | 13 | 10 | ||
| Fetal gender | 0.2012 | 0.6537 | ||
| Male | 20 | 14 | ||
| Female | 22 | 19 | ||
| Pregnancy complication | 0.1207 | 0.7283 | ||
| Yes (≥ 1) | 13 | 9 | ||
| No | 29 | 24 | ||
| Mode of delivery | 0.1122 | 0.7376 | ||
| Vaginal delivery | 20 | 17 | ||
| Cesarean delivery | 22 | 16 | ||
| Newborn Apgar score | 0.0541 | 0.8161 | ||
| ≤ 7 points | 8 | 7 | ||
| > 7 points | 34 | 26 | ||
| Housewife or not | 0.7694 | 0.3804 | ||
| Yes | 9 | 10 | ||
| No | 33 | 23 |
Note: BMI: body mass index.
Comparison of self-efficacy between the two groups before and after the intervention
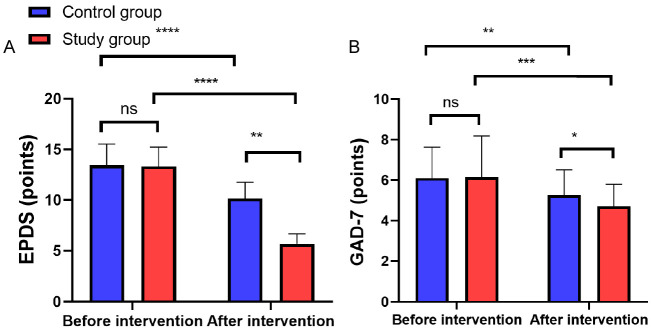
Before the intervention, no significant difference was found in GSES scores between the two groups (P > 0.05). After the intervention, the GSES scores significantly improved in both groups, with the study group showing a significantly higher improvement compared to the control group (P < 0.05, Figure 1).
Figure 1.
Comparison of GSES scores between the two groups before and after intervention. Notes: ns indicates P > 0.05; *** indicates P < 0.001; **** indicates P < 0.0001. GSES: General Self-Efficacy Scale.
Comparison of depression and anxiety levels between the two groups before and after the intervention
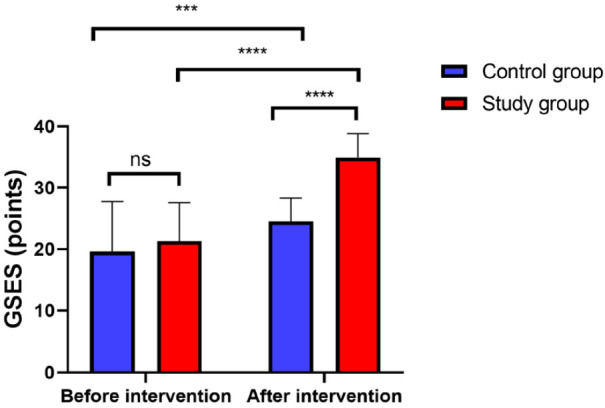
Before the intervention, no significant differences were observed in EPDS and GAD-7 scores between the two groups (both P > 0.05). After the intervention, both EPDS and GAD-7 scores significantly decreased in both groups, with the study group showing a significantly greater reduction compared to the control group (P < 0.05, Figure 2).
Figure 2.
Comparison of GAD-7 scores between the two groups before and after intervention. A: Comparison of EPDS score; B: Comparison of GAD-7 score. Notes: ns indicates P > 0.05; * indicates P < 0.05; ** indicates P < 0.01; *** indicates P < 0.001; **** indicates P < 0.0001. EPDS: Edinburgh Postnatal Depression Scale; GAD-7: the 7-item Generalized Anxiety Disorder Questionnaire.
Comparison of sleep quality between the two groups before and after the intervention
Before the intervention, no significant difference was observed in PSQI scores between the two groups (P > 0.05). After the intervention, the PSQI scores significantly decreased in both groups, with the study group showing a significantly greater reduction compared to the control group (P < 0.05, Figure 3).
Figure 3.
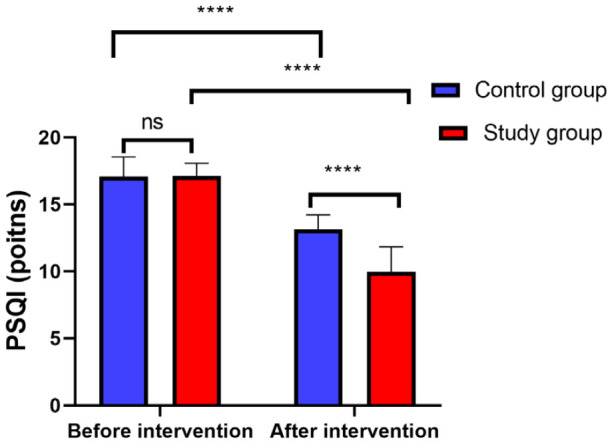
Comparison of PSQI scores between the two groups before and after intervention. Notes: ns indicates P > 0.05; **** indicates P < 0.0001. PSQI: Pittsburgh Sleep Quality Index.
Comparison of progesterone levels between the two groups before and after intervention
There was no significant difference in progesterone levels between the two groups before the intervention (P > 0.05). However, after the intervention, the progesterone levels significantly de-creased in both groups, with the study group exhibiting significantly lower levels compared to the control group (P < 0.05), as shown in Figure 4.
Figure 4.
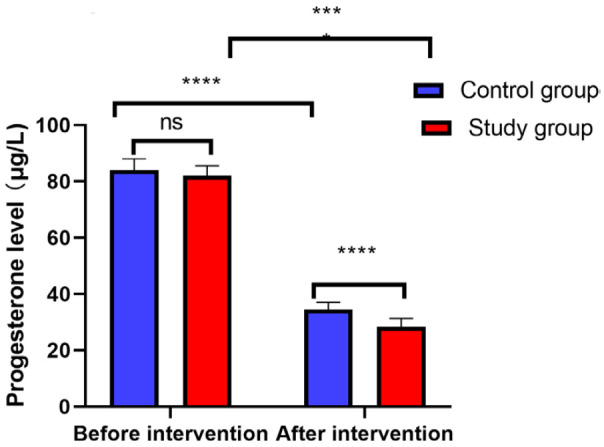
Comparison of progesterone levels between the two groups before and after intervention. Notes: ns indicates P > 0.05; **** indicates P < 0.0001.
Univariate analysis for the influencing factors of postpartum depression in elderly primiparas
A total of 75 postpartum women with depression were included in the depression group, while 80 non-depressed postpartum women were included in the non-depression group. The relevant characteristics of the two groups were compared using univariate analysis. The results identified age, educational level, pregnancy complications, mode of delivery, newborn Apgar score, and being a housewife as significant influencing factors for postpartum depression in elderly primiparas (all P < 0.05, Table 2).
Table 2.
Univariate analysis of influencing factors for postpartum depression in elderly primiparas
| Factors | Depression group (n = 75) | Non-depressiongroup (n = 80) | χ2/t | P | |
|---|---|---|---|---|---|
| Age | 19.101 | < 0.0001 | |||
| ≥ 40 years | 38 | 14 | |||
| < 40 years | 37 | 66 | |||
| Pre-pregnancy BMI | 2.3611 | 0.1244 | |||
| ≥ 23 kg/m2 | 44 | 42 | |||
| < 23 kg/m2 | 31 | 48 | |||
| Education level | 4.9351 | 0.0263 | |||
| Below Junior college | 20 | 35 | |||
| Junior college and above | 55 | 45 | |||
| Fetal sex | 0.0731 | 0.7869 | |||
| Male | 34 | 38 | |||
| Female | 41 | 42 | |||
| Pregnancy complication | 6.6951 | 0.0097 | |||
| Yes (≥ 1) | 22 | 10 | |||
| No | 53 | 70 | |||
| Mode of delivery | 0.1553 | 0.6935 | |||
| Vaginal delivery | 37 | 42 | |||
| Cesarean delivery | 38 | 38 | |||
| Newborn Apgar score | 4.0231 | 0.0449 | |||
| ≤ 7 points | 15 | 7 | |||
| > 7 points | 60 | 73 | |||
| Housewife or not | 4.1921 | 0.0406 | |||
| Yes | 19 | 10 | |||
| No | 56 | 70 | |||
Note: BMI: body mass index.
Multivariate analysis for the influencing factors of postpartum depression in elderly primiparas
Variables that showed significant differences in the univariate analysis were assigned with values (Table 3) and included in a logistic regression model. The logistic regression analysis identified age, educational level, pregnancy complications, and newborn Apgar score as independent influencing factors for postpartum depression in elderly primiparas (Table 4).
Table 3.
Assignment table
| Factors | Assignment | |
|---|---|---|
|
| ||
| 0 | 1 | |
| Age | < 40 years | ≥ 40 years |
| Education level | Below Junior college | Junior college and above |
| Pregnancy complication | No | Yes |
| Mode of delivery | Vaginal delivery | Cesarean delivery |
| Newborn Apgar score | > 7 points | ≤ 7 points |
| Housewife or not | No | Yes |
| Depression or not | No | Yes |
Table 4.
Multivariate logistic regression analysis of influencing factors for postpartum depression in elderly primiparas
| Factors | B | S.E. | Wals | df | Sig. | Exp (B) | 95% C.I. For EXP (B) | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Lower limit | Upper limit | |||||||
| Age | 1.700 | 0.399 | 18.156 | 1 | < 0.0001 | 5.471 | 2.504 | 11.956 |
| Education level | 0.863 | 0.395 | 4.784 | 1 | 0.029 | 2.370 | 1.094 | 5.137 |
| Pregnancy complication | 1.700 | 0.399 | 18.156 | 1 | < 0.0001 | 5.471 | 2.504 | 11.956 |
| Mode of delivery | 0.863 | 0.395 | 4.784 | 1 | 0.029 | 2.370 | 1.094 | 5.137 |
| Newborn Apgar score | 1.299 | 00.470 | 7.652 | 1 | 0.006 | 3.665 | 1.460 | 9.199 |
| Housewife or not | -0.002 | 0.375 | 0.000 | 1 | 0.996 | 0.998 | 0.478 | 2.083 |
Discussion
Depression is a prevalent complication in clinical obstetrics and gynecology and is among the most prevalent mental disorders during the postpartum period. Notably, elderly primiparous women are at a higher risk of developing postpartum depression compared to younger primiparous women [13,14]. This study investigated the effects of mindfulness-based psychological interventions on postpartum depression in elderly primiparas and identified the independent risk factors for postpartum depression in this population.
The GSES is a widely used tool for assessing individuals’ levels of self-efficacy, with significant implications in psychological research and clinical practice. It is crucial for evaluating individuals’ self-efficacy levels, predicting behavioral performance, guiding interventions and training, among other aspects [15]. The study found notably higher GSES scores in postpartum women who received mindfulness-based psychological interventions than those who received routine health management, suggesting a more positive impact of mindfulness-based psychological interventions on enhancing maternal self-efficacy. This could be because mindfulness-based psychological interventions focus on the present moment and a conscious mental state. By cultivating mindfulness, these interventions enhance the awareness of maternal emotions and experiences, help postpartum women learn to accept and regulate emotions, and strengthen their confidence and coping skills when facing difficulties and challenges, thereby enhancing their self-efficacy [16]. EPDS and GAD-7 are commonly used tools for assessing postpartum depression and symptoms of generalized anxiety, respectively. Lower EPDS and GAD-7 scores indicate milder depressive and anxiety symptoms [17,18]. The study found that women who received mindfulness-based psychological interventions had significantly lower EPDS and GAD-7 scores compared to the control group, indicating less severe postpartum depression and generalized anxiety symptoms after the intervention. Mindfulness-based psychological interventions have demonstrated effectiveness in alleviating symptoms of maternal depression and anxiety. This positive outcome can be attributed to the cultivation of awareness and acceptance of the present moment, which enables them to effectively cope with negative emotions and stress. By developing mindfulness skills, women enhance their emotional regulation abilities, allowing for better management of postpartum emotional fluctuations and anxiety [19]. In addition, mindfulness-based psychological interventions provide emotional support and cognitive restructuring, helping postpartum women cope more positively with difficulties and negative thoughts. This study also found notably lower PSQI scores in the study group compared to the control group, indicating that mindfulness-based psychological interventions were more effective in improving sleep quality. Mindfulness-based psychological interventions, as a non-pharmacological approach, can be incorporated into postpartum mental health management to help improve sleep and promote overall physical and mental well-being [20]. In this study, we observed a significant decrease in progesterone levels in both groups after the intervention, with the study group exhibiting a significantly lower progesterone levels than the control group. These findings suggest that mindfulness-based psychological intervention is more effective in reducing progesterone levels and alleviating depressive symptoms. However, it is important to note that progesterone levels alone may not be the sole determinant of depressive symptoms, and the relationship between progesterone and postpartum depression is complex [21]. Postpartum depression is influenced by various factors, including hormonal changes, psychosocial factors, and individual differences. The positive effects observed in the study group may be attributed to the comprehensive approach of mindfulness-based psychological intervention, which addresses multiple aspects of the participants’ well-being and provides effective support for managing depressive symptoms. However, further research is needed to fully understand the mechanisms underlying the relationship between progesterone levels, mindfulness-based interventions, and the alleviation of postpartum depression symptoms.
The study also analyzed the influencing factors of postpartum depression in elderly primiparous women. The results revealed that advanced maternal age, higher educational level, presence of pregnancy complications, and lower newborn Apgar score were independent risk factors for postpartum depression in elderly primiparous women. Xiong et al. [22] have found that advanced maternal age increases the risk of postpartum depression. As women age, their physical fitness and energy levels decline, leading to a lack of confidence in their physical recovery and ability to care for a newborn. Additionally, factors such as a lack of childbirth experience or hearing about the difficulties of first-time childbirth from others, contribute to the anxieties experienced by elderly primiparous women. Furthermore, the results of current study revealed that a higher level of education was associated with a greater likelihood of experiencing depression among postpartum women. This may be related to the differences in cognitive levels regarding pregnancy and childbirth among postpartum women with different educational backgrounds. Lower levels of education are associated with less consideration and attention given to issues related to pregnancy and childbirth, relying more on information provided by healthcare professionals. On the other hand, higher levels of education enable access to various sources of information related to pregnancy and childbirth, leading to a more comprehensive consideration of physiological, psychological, and social aspects. Moreover, having only partial knowledge of medical information or relying on anecdotal experiences from others may increase psychological burden and susceptibility to depression. The incidence of various complications during the perinatal period is significantly higher in elderly primiparous women compared to women of average maternal age [23]. This may be attributed to the health condition of elderly primiparous women themselves. Declining levels of estrogen and progesterone, along with the deterioration of skeletal muscle function and decreased immune response, result in reduced physical stress tolerance during the perinatal period, making them more susceptible to illness. This, in turn, increases the psychological burden of elderly primiparous women and raises the risk of developing postpartum depression. Liu et al. [24] have also found a correlation between gestational diabetes and postpartum depression, which support the results of this study. However, this study is limited by the sample size and cannot extensively address the impact of various complications on the occurrence of postpartum depression in elderly primiparous women. Furthermore, the Apgar score of the baby is related to the occurrence of postpartum depression in the mother, a relationship that may be even more significant in elderly primiparous women. It is possible that primiparous women have higher expectations for their infants, and if the newborn’s health is poor, it can lead to a significant psychological gap in the primiparous mothers. They may struggle to accept the situation and worry about their child’s future growth and development. Since all participants in this study were elderly primiparous women, their age-related concerns about their newborns’ health might be greater than those of younger mothers, causing considerable physical and psychological stress and increasing the likelihood of developing depression.
However, this study still has certain limitations. As a retrospective study, the conclusions are based on existing data and statistical analysis, which may limit the ability to establish causality. Therefore, further research is needed to validate these results and explore the underlying mechanisms in greater depth. Additionally, the small sample size of this study may affect the reliability and generalizability of the research findings.
Conclusion
Mindfulness-based psychological intervention is beneficial for improving self-efficacy, emotional state, and sleep quality among elderly primiparas with postpartum depression. Additionally, advanced maternal age, relatively high education level, presence of pregnancy complications, and relatively lower newborn Apgar scores are identified as independent risk factors for postpartum depression in elderly primiparas.
Disclosure of conflict of interest
None.
References
- 1.Ajayi AI, Ahinkorah BO, Seidu AA, Adeniyi OV. Prevalence and correlates of induced abortion: results of a facility-based cross-sectional survey of parturient women living with HIV in South Africa. Reprod Health. 2022;19:220. doi: 10.1186/s12978-022-01520-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cabella W, Velázquez C. Abortion legalization in uruguay: effects on adolescent fertility. Stud Fam Plann. 2022;53:491–514. doi: 10.1111/sifp.12204. [DOI] [PubMed] [Google Scholar]
- 3.Liu S, Lin Q, Feng Y, Zhong D, Jiang C, Zhang L. The protective role of social support on prenatal depression among pregnant women of advanced maternal age: a Three-Trimester follow-up study in China. J Obstet Gynaecol. 2022;42:3456–3463. doi: 10.1080/01443615.2022.2135986. [DOI] [PubMed] [Google Scholar]
- 4.Stewart DE, Vigod SN. Postpartum depression: pathophysiology, treatment, and emerging therapeutics. Annu Rev Med. 2019;70:183–196. doi: 10.1146/annurev-med-041217-011106. [DOI] [PubMed] [Google Scholar]
- 5.Correa-de-Araujo R, Yoon SSS. Clinical outcomes in high-risk pregnancies due to advanced maternal age. J Womens Health (Larchmt) 2021;30:160–167. doi: 10.1089/jwh.2020.8860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masembe S, Migisha R, Turyasingura G, Aheisibwe H, Nzabandora E, Lule JC. Adverse maternal outcomes and associated factors among mothers of advanced age delivering at a tertiary hospital, southwestern Uganda: a cross-sectional study. BMC Pregnancy Childbirth. 2024;24:348. doi: 10.1186/s12884-024-06557-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schlosser M, Demnitz-King H, Barnhofer T, Collette F, Gonneaud J, Chételat G, Jessen F, Kliegel M, Klimecki OM, Lutz A, Marchant NL Medit-Ageing Research Group. Effects of a mindfulness-based intervention and a health self-management programme on psychological well-being in older adults with subjective cognitive decline: secondary analyses from the SCD-Well randomised clinical trial. PLoS One. 2023;18:e0295175. doi: 10.1371/journal.pone.0295175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore Simas TA, Whelan A, Byatt N. Postpartum depression-new screening recommendations and treatments. JAMA. 2023;330:2295–2296. doi: 10.1001/jama.2023.21311. [DOI] [PubMed] [Google Scholar]
- 9.Skliarova T, Pedersen H, Hafstad H, Vaag JR, Lara-Cabrera ML, Havnen A. The construct validity of an abridged version of the general self-efficacy scale for adults with attention-deficit/hyperactivity disorder. Front Psychiatry. 2023;14:1212961. doi: 10.3389/fpsyt.2023.1212961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park SH, Kim JI. Predictive validity of the Edinburgh postnatal depression scale and other tools for screening depression in pregnant and postpartum women: a systematic review and meta-analysis. Arch Gynecol Obstet. 2023;307:1331–1345. doi: 10.1007/s00404-022-06525-0. [DOI] [PubMed] [Google Scholar]
- 11.Toussaint A, Hüsing P, Gumz A, Wingenfeld K, Härter M, Schramm E, Löwe B. Sensitivity to change and minimal clinically important difference of the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7) J Affect Disord. 2020;265:395–401. doi: 10.1016/j.jad.2020.01.032. [DOI] [PubMed] [Google Scholar]
- 12.Zitser J, Allen IE, Falgàs N, Le MM, Neylan TC, Kramer JH, Walsh CM. Pittsburgh Sleep Quality Index (PSQI) responses are modulated by total sleep time and wake after sleep onset in healthy older adults. PLoS One. 2022;17:e0270095. doi: 10.1371/journal.pone.0270095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chawla A, Bansal NL, Liu C, Olagunju AT. Postpartum depression in correctional populations. J Correct Health Care. 2024;30:65–70. doi: 10.1089/jchc.23.08.0071. [DOI] [PubMed] [Google Scholar]
- 14.Gebrekristos LT, Groves AK, McNaughton Reyes L, Moodley D, Beksinska M, Maman S. Intimate partner violence victimization during pregnancy increases risk of postpartum depression among urban adolescent mothers in South Africa. Reprod Health. 2023;20:68. doi: 10.1186/s12978-023-01605-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brennan BA. Psychometric evaluation of the clinical and simulation general self-efficacy scale. Nurs Educ Perspect. 2023;44:105–106. doi: 10.1097/01.NEP.0000000000000979. [DOI] [PubMed] [Google Scholar]
- 16.Chayadi E, Baes N, Kiropoulos L. The effects of mindfulness-based interventions on symptoms of depression, anxiety, and cancer-related fatigue in oncology patients: a systematic review and meta-analysis. PLoS One. 2022;17:e0269519. doi: 10.1371/journal.pone.0269519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stasik-O’Brien SM, McCabe-Beane JE, Segre LS. Using the EPDS to identify anxiety in mothers of infants on the neonatal intensive care unit. Clin Nurs Res. 2019;28:473–487. doi: 10.1177/1054773817740532. [DOI] [PubMed] [Google Scholar]
- 18.Ahmadi A, Ponder WN, Carbajal J, Schuman DL, Whitworth J, Yockey RA, Galusha JM. Validation of the PCL-5, PHQ-9, and GAD-7 in a sample of veterans. J Occup Environ Med. 2023;65:643–654. doi: 10.1097/JOM.0000000000002898. [DOI] [PubMed] [Google Scholar]
- 19.Mao F, Sun Y, Li Y, Cui N, Cao F. Internet-delivered mindfulness-based interventions for mental health outcomes among perinatal women: a systematic review. Asian J Psychiatr. 2023;80:103321. doi: 10.1016/j.ajp.2022.103321. [DOI] [PubMed] [Google Scholar]
- 20.Peters AL, Saunders WJ, Jackson ML. Mindfulness-based strategies for improving sleep in people with psychiatric disorders. Curr Psychiatry Rep. 2022;24:645–660. doi: 10.1007/s11920-022-01370-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stefaniak M, Dmoch-Gajzlerska E, Jankowska K, Rogowski A, Kajdy A, Maksym RB. Progesterone and its metabolites play a beneficial role in affect regulation in the female brain. Pharmaceuticals (Basel) 2023;16:520. doi: 10.3390/ph16040520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiong R, Deng A. Incidence and risk factors associated with postpartum depression among women of advanced maternal age from Guangzhou, China. Perspect Psychiatr Care. 2020;56:316–320. doi: 10.1111/ppc.12430. [DOI] [PubMed] [Google Scholar]
- 23.Koutra K, Vassilaki M, Georgiou V, Koutis A, Bitsios P, Kogevinas M, Chatzi L. Pregnancy, perinatal and postpartum complications as determinants of postpartum depression: the Rhea mother-child cohort in Crete, Greece. Epidemiol Psychiatr Sci. 2018;27:244–255. doi: 10.1017/S2045796016001062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu X, Wang S, Wang G. Prevalence and risk factors of postpartum depression in women: a systematic review and meta-analysis. J Clin Nurs. 2022;31:2665–2677. doi: 10.1111/jocn.16121. [DOI] [PubMed] [Google Scholar]