Abstract
Objective: To systematically evaluate the clinical efficacy of traditional Chinese acupuncture and moxibustion in treating post-stroke aphasia through meta-analysis. Methods: Major Chinese and international databases were searched from their inception to December 2023. The search terms included “randomized controlled clinical studies on acupuncture treatment for stroke-related aphasia”. After screening by specialists, the selected studies were analyzed using RevMan 5.3 software. Results: A total of 1,900 documents were retrieved, of which 10 studies involving 848 cases met the inclusion criteria and were included in the meta-analysis. The results indicated that traditional Chinese acupuncture could enhance the effectiveness of language rehabilitation training both as a standalone treatment and in combination with other assessment measures. Acupuncture improved the clinical effectiveness of language rehabilitation training for patients with post-stroke aphasia (RR = 3.75, 95% CI [2.54, 2.55], P < 0.00001). When combined with language rehabilitation therapy, acupuncture significantly improved patients’ comprehension (MD = 0.95, 95% CI [0.89, 1.02], P < 0.00001), repetition (MD = 0.82, 95% CI [0.76, 0.88], P < 0.00001), reading (MD = 1.95, 95% CI [1.89, 2.01], P < 0.00001), and spontaneous speech abilities (MD = 10.90, 95% CI [9.56, 12.23], P < 0.00001), compared to the control group. Conclusion: Acupuncture improves the clinical efficacy of language rehabilitation training for stroke-related aphasia. It also enhanced patients’ comprehension, repetition, and spontaneous speech abilities more effectively than monotherapy. However, the overall quality of the included studies was low, emphasizing the need for high-quality randomized controlled trials to further validate these findings.
Keywords: Acupuncture, aphasia, stroke, meta-analysis, systematic review
Introduction
Stroke, often referred to as a “brain attack”, is a serious neurological disorder caused primarily by ischemic stroke (due to vascular blockage) or hemorrhagic stroke (from blood vessel rupture) [1,2]. Both types result in a sudden interruption of blood supply to specific brain regions, leading to brain cell damage or even death [3,4]. Despite advancements in diagnostic and therapeutic techniques that have lowered stroke-related mortality, many patients still experience varying degrees of tissue damage. Among the complications, aphasia is common and significantly impacts patients’ quality of life by impairing their ability to communicate [5,6]. Thus, effectively improving aphasic symptoms is essential for enhancing patient outcomes.
Traditionally, speech therapy has been the most widely used and effective treatment for aphasia. It involves the restoration of language abilities through patient cooperation with professional speech therapists, undergoing structured training and exercises. However, achieving optimal treatment outcomes through this method alone remains challenging [7,8]. The rehabilitation of post-stroke aphasia typically relies on non-pharmacologic approaches, including speech rehabilitation, neuromodulation technology, and behavioral guidance techniques. In recent years, acupuncture therapy has gained popularity for rehabilitating patients with post-stroke sequelae and has been recommended by international guidelines as a viable treatment option for post-stroke rehabilitation [9].
Several systematic reviews and meta-analyses have been conducted on the efficacy of acupuncture and moxibustion in treating post-stroke aphasia, but their conclusions have been inconsistent, complicating evidence-based decision-making [10]. Given this background, the present study aims to systematically evaluate the efficacy of acupuncture combined with language rehabilitation therapy for post-stroke aphasia, providing robust evidence to inform clinical practice.
Materials and methods
Literature search
A comprehensive search was conducted across major domestic and international databases, including CNKI, WanFang, PubMed, and VIP. The search strategy focused on three main aspects: clinical conditions (stroke, cerebral infarction, aphasia, cerebral hemorrhage), rehabilitation methods (acupuncture, moxibustion, electroacupuncture), and study design (randomized controlled trials). The search period covered from the inception of each database to 2023. This study’s protocol was registered with the International Prospective Register of Systematic Reviews (registration number: CRD42024572088).
Inclusion criteria
(1) Study Type: All clinical randomized controlled trials evaluating the effectiveness of acupuncture combined with language rehabilitation therapy for post-stroke aphasia were included. (2) Study Subjects: Patients diagnosed with post-stroke aphasia were eligible, irrespective of their source, age, gender, or race [11]. (3) Intervention Measures: The experimental group received acupuncture (including traditional acupuncture, electroacupuncture, and moxibustion) combined with language rehabilitation therapy, while the control group received only language rehabilitation therapy. (4) Outcome Events: The primary outcome was the overall efficacy rate. Secondary outcomes included comprehension ability, repetition ability, communication ability, and spontaneous speech ability.
Exclusion criteria
(1) Aphasia caused by conditions other than stroke. (2) Studies that did not meet the established research criteria. (3) Publications that were conference reports, appeared in illegal journals, or were meta-analyses. (4) Articles published multiple times in different journals. (5) Studies that only involved literature review results. (6) Treatments for aphasia that did not include language rehabilitation therapy and/or combined acupuncture therapy.
Literature quality assessment and data extraction
The quality of the included studies was assessed using the risk of bias tool for randomized controlled trials provided by the Cochrane Collaboration in Review Manager 5.3 [12]. Key domains assessed included study methods, blinding, allocation concealment, completeness of results, and potential bias. The risk level of bias was categorized based on these assessments. Literature screening and data extraction were independently conducted by Jixin Li and Yingping Jiang, with disagreements resolved through discussion or consultation with a third party. Initially, titles and abstracts were screened to identify possibly eligible articles, which were then subjected to full-text review for final inclusion. Quality assessment focused on methodological rigor and evidence quality, performed independently by Jixin Li and Yingping Jiang. Disputes were resolved using the aforementioned approach.
Data analysis
The clinical efficacy of acupuncture for post-stroke aphasia was evaluated using Review Manager 5.3. Treatment effectiveness was analyzed as a dichotomous variable, with the odds ratio (OR) as the effect measure. Comprehension ability, repetition ability, reading ability, and spontaneous speech ability were treated as continuous variables, with the mean difference used as the statistical measure. The 95% confidence intervals were calculated. Meta-analysis employed fixed-effect or random-effect models based on study heterogeneity. The I2 statistic was used to assess heterogeneity: I2 ≤ 25% indicated low heterogeneity, I2 ≥ 50% indicated moderate heterogeneity, and I2 ≥ 75% indicated high heterogeneity. Subgroup analysis was conducted to explore sources of heterogeneity. A P-value < 0.05 was considered significant.
Results
Literature search results
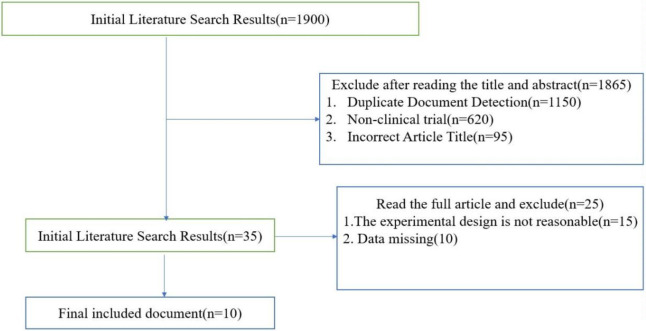
The initial search yielded 1,900 documents. After screening titles and abstracts, 1,865 documents were excluded for not meeting the inclusion criteria. The remaining 35 documents underwent full-text review, and 25 were deemed ineligible. Consequently, 10 articles were included, all of which were published studies conducted in China [13-22]. The literature search and selection process are illustrated in Figure 1.
Figure 1.
Research flow chart.
General characteristics of included literature
The study included 10 articles with a total of 848 patients: 436 in the experimental group and 412 in the control group. The basic characteristics of the included studies are presented in Table 1.
Table 1.
General characteristics of included literature
| Included study | Case | Intervention measurement | Primary outcome indicator | ||
|---|---|---|---|---|---|
|
|
|
||||
| Experimental group | Control group | Experimental group | Control group | ||
| ZQ Wang et al 2022 [13] | 60 | 60 | Acupuncture + speech rehabilitation training | Speech rehabilitation training | Overall efficacy rate + Chinese aphasia test method |
| KK Zhang et al 2019 [14] | 45 | 32 | Acupuncture + mild moxibustion | Needling | Overall efficacy rate + Chinese aphasia test method |
| L Liu et al 2019 [15] | 42 | 43 | Acupuncture + speech rehabilitation training | Speech rehabilitation training | Overall efficacy rate + Chinese aphasia test method |
| QS Huang et al 2022 [16] | 58 | 57 | Acupuncture + speech rehabilitation training | Speech rehabilitation training | Overall efficacy rate + Chinese aphasia test method |
| PX Weng et al 2019 [17] | 45 | 45 | Acupuncture + speech rehabilitation training | Speech rehabilitation training | Overall efficacy rate + Chinese Aphasia Test + SAQOL-39g |
| XF Jiang et al 2020 [18] | 40 | 37 | Acupuncture and moxibustion | Speech rehabilitation training | Overall efficacy rate + Chinese aphasia test method |
| HM Xu et al 2017 [19] | 43 | 43 | Acupuncture and moxibustion | Conventional method | Overall efficacye rate + Chinese aphasia test method |
| ZL Ding et al 2017 [20] | 32 | 31 | Acupuncture + Traditional Chinese medicine + conventional Western medicine | Conventional western medicine | Overall efficacy rate + Chinese aphasia test + syndrome score |
| XJ Yin et al 2019 [21] | 24 | 17 | Acupuncture + speech rehabilitation training | Speech rehabilitation training | Overall efficacy rate + Chinese aphasia test method |
| LY Tang et al 2016 [22] | 47 | 47 | Acupuncture and moxibustion | Western medicine | Overall efficacy rate + Chinese aphasia test method |
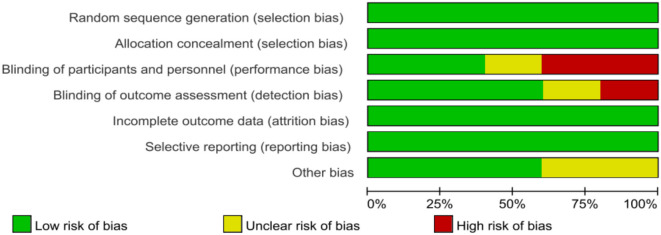
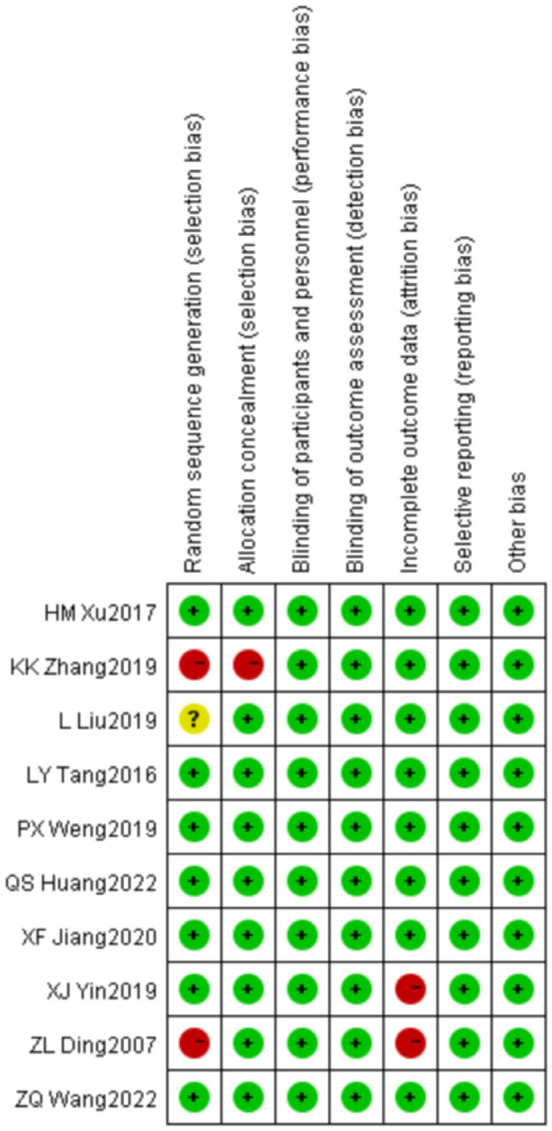
Overall quality assessment of included literature
The overall quality of the included studies was deemed fair.
Randomization: Nine articles were assessed as low risk for randomization; seven explicitly used the random number table method, and two used the block randomization method [26]. One article did not specify the randomization method and was thus assessed as having an unclear risk.
Blinding and Allocation Concealment: None of the 10 articles described blinding or allocation concealment methods, leading to an assessment of unclear risk.
Completeness of Data: All 10 articles presented complete data with no dropouts, indicating low risk.
Outcome Reporting: Nine articles provided complete outcome data and were assessed as low risk. One article only reported treatment efficacy rates without relevant sub-outcome indicators, resulting in an unclear risk assessment.
Potential Bias: None of the 10 articles mentioned potential biases that could affect the results, leading to an unclear risk assessment. The quality assessment results are illustrated in Figures 2 and 3.
Figure 2.
Bias risk analysis for included trials.
Figure 3.
Summary of risk of bias in included trials.
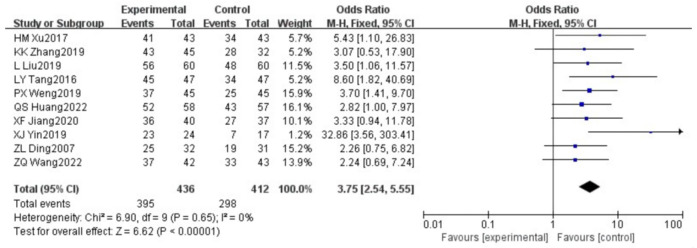
Meta-analysis results
Overall efficacy of acupuncture treatment
The meta-analysis of the efficacy of acupuncture treatment for post-stroke aphasia showed that all selected studies used aphasia treatment efficacy rate as the primary outcome indicator [10-20]. The forest plot is presented in Figure 4. The heterogeneity test indicated homogeneity among the studies (χ2 = 6.90, df = 9, P = 0.65, I2 = 0%), so a fixed-effects model was used. The combined effect size was OR = 3.75, 95% CI [2.54, 5.55], Z = 6.62 (P < 0.00001), indicating a significant difference (Figure 4).
Figure 4.
Comparison of clinical efficacy of acupuncture combined with speech rehabilitation for post-stroke aphasia.
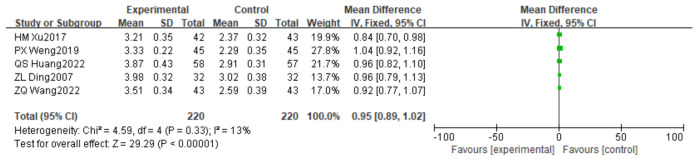
Comprehension ability based on Chinese Aphasia Examination scoring criteria
This analysis included 5 articles with 440 patients. The statistical results based on the Chinese Aphasia Examination scoring criteria are shown in Figure 5. The heterogeneity test results were χ2 = 4.59, df = 4, P = 0.33, I2 = 13%, indicating low heterogeneity. A random-effects model was adopted, yielding a combined effect size of MD = 0.95, 95% CI [0.89, 1.02], Z = 29.29 (P < 0.00001), indicating a significant difference.
Figure 5.
Comparison of comprehension scores in post-stroke aphasia treated with acupuncture and speech rehabilitation.
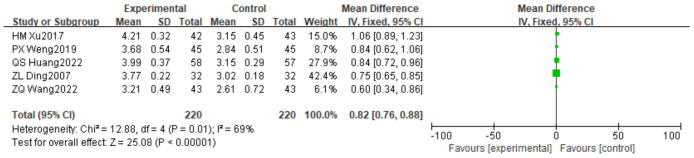
Repetition ability based on Chinese Aphasia Examination scoring criteria
This analysis included 5 articles with 440 patients. The results based on the Chinese Aphasia Examination scoring criteria are shown in Figure 6. The heterogeneity test results were χ2 = 12.88, df = 4, P = 0.01, I2 = 69%, indicating moderate heterogeneity. A fixed-effects model was used, and the combined effect size was MD = 0.82, 95% CI [0.76, 0.88], Z = 25.08 (P < 0.00001).
Figure 6.
Comparison of rehearsal ability scores in post-stroke aphasia treated with acupuncture and speech rehabilitation.
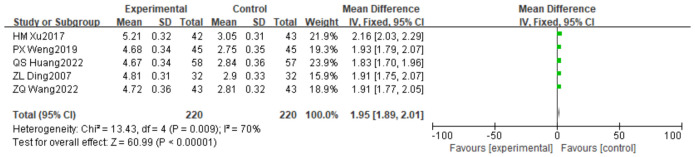
Reading ability based on Chinese Aphasia Examination scoring criteria
This analysis included 5 articles with 440 patients. The statistical results are shown in Figure 7. The heterogeneity test results were χ2 = 13.43, df = 4, P < 0.00001, I2 = 70%, indicating high heterogeneity. A fixed-effects model was used, and the combined effect size was MD = 1.95, 95% CI [1.89, 2.01], Z = 33.15 (P < 0.00001).
Figure 7.
Comparison of reading ability score in post-stroke aphasia treated with acupuncture and speech rehabilitation.
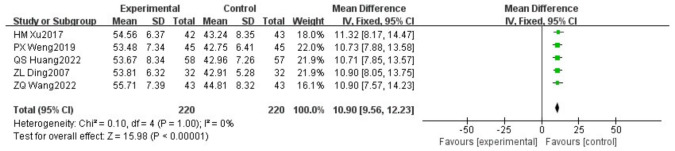
Spontaneous speech ability based on Chinese Aphasia Examination scoring criteria
This analysis included 5 articles with 440 patients. The results are shown in Figure 8. The heterogeneity test results were χ2 = 0.10, df = 4, P = 1, I2 = 0%, indicating no heterogeneity. A fixed-effects model was used, and the combined effect size was MD = 10.90, 95% CI [9.56, 12.23], Z = 15.98 (P < 0.00001).
Figure 8.
Comparison of spontaneous language ability scores in post-stroke aphasia treated with acupuncture and speech rehabilitation.
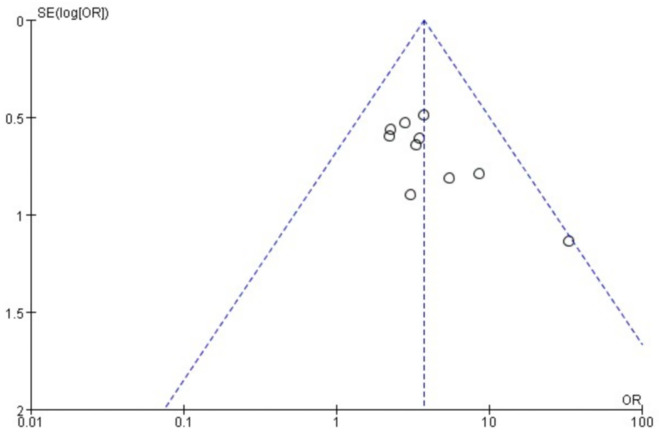
Publication bias analysis
Among the 10 included articles, efficacy was used as the evaluation indicator. A funnel plot was created to assess potential publication bias related to acupuncture combined with language function training for post-stroke aphasia. The results indicated that the smaller studies were symmetrically distributed around the overall effect, suggesting minimal publication bias (Figure 9). However, slight asymmetry was observed, possibly due to the tendency for studies with significant results to be more readily published. This publication bias may have influenced the study’s findings. Sensitivity analysis showed that heterogeneity was not driven by specific articles.
Figure 9.
Funnel plot of included studies on the efficacy of acupuncture combined with speech rehabilitation for post-stroke aphasia.
Discussion
Stroke has emerged as a significant public health issue due to its high incidence and disability rates, posing a severe threat to the population’s health. It is primarily caused by cerebrovascular obstruction, leading to brain dysfunction [23]. Common symptoms include unilateral weakness, speech difficulties, and slurred speech, which substantially impact patients’ quality of life and impose significant economic and psychological burdens on society and families. Studies have demonstrated that active speech rehabilitation can effectively treat aphasia by reshaping brain language function, increasing neuronal activity in affected brain regions, and promoting neurotransmitter release. Continuous stimulation of speech neurons aids in normalizing speech function, gradually improving patients’ conditions.
In traditional Chinese medicine (TCM), post-stroke aphasia is categorized as “difficulty in pronunciation”. Its pathogenesis is associated with factors such as wind, fire, phlegm, qi deficiency, blood stasis, and liver-kidney yin deficiency. These factors result in symptoms mainly affecting the brain, heart, kidneys, liver, and spleen. Aphasia is primarily attributed to the obstruction of blood vessels in the tongue by wind, phlegm, and stasis, leading to tongue stiffness and speech difficulties. Therefore, treatment focuses on resolving phlegm, dispelling stasis, enhancing blood circulation, and restoring speech function.
This meta-analysis, which included 10 studies with 468 patients, found that acupuncture combined with language rehabilitation therapy was more effective for post-stroke aphasia than language rehabilitation alone. It improved patients’ comprehension, repetition, reading, and spontaneous speech abilities, suggesting that integrating acupuncture with TCM may provide additional therapeutic benefit for aphasia patients [24,25].
In TCM, the head is considered the gathering place of yang energy. The Du meridian, along with the three yang meridians of the hand and foot, ascends to the head, closely connecting with the body’s organs. The tongue, regarded as the organ of speech, serves as a conduit for energy exchange through the meridians. In post-stroke aphasia, impaired speech or language comprehension reflects organ imbalance and qi and blood deficiency. Needling specific points on the head can activate related meridians and organs, promote energy flow, improve blood circulation, and enhance cognitive function, speech, and wisdom [26].
Domestic research has explored various acupuncture techniques, including body acupuncture, scalp acupuncture, tongue acupuncture, and Shao’s acupuncture, showing promising results in treating aphasia. Acupuncture enhances physical fitness, arouses consciousness, clears phlegm, opens the orifices, and improves local circulation. It also stimulates key acupoints related to speech, such as “Lian Quan” and “Jin Jin Yu Ye”, facilitating the restoration of speech functions like comprehension, repetition, reading, and self-expression. Needling the Fengchi acupoint directly stimulates intermediate neurons related to sensory fibers, enhancing neuronal activity and aiding in language function recovery. Modern research suggests that needling brain and language areas can improve blood supply to lesion areas, increase synaptic connections, and enhance brain function, aiding aphasia recovery [27,28]. Needling the tongue nerve can accelerate nerve conduction, supporting speech pathway establishment. Animal studies have shown that electroacupuncture at Baihui and Dazhui acupoints in rats with cerebral ischemia-reperfusion injury can promote the proliferation and activation of endogenous neural stem cells, facilitating neural repair and reducing secondary nerve damage [29,30]. These findings indicate that acupuncture holds promise for enhancing recovery in patients with post-stroke aphasia.
However, this study has some limitations. First, the quality of the included studies is generally average, as all are single-center randomized trials conducted in China, potentially introducing selection bias. Second, variations in acupoint selection and needling intensity across studies may increase heterogeneity of the results. Third, differing treatment durations among the studies could affect the outcomes of acupuncture combined with speech function training. Lastly, the exclusive inclusion of Chinese-language studies may pose a bias risk. Therefore, further research with larger, more diverse sample sizes is needed to refine and validate these findings.
In conclusion, acupuncture combined with speech rehabilitation training shows high clinical efficacy for post-stroke aphasia, but further clinical research with larger, varied sample sizes is essential to confirm these results.
Disclosure of conflict of interest
None.
References
- 1.Kimura H. Stroke. Brain Nerve. 2020;72:311–321. doi: 10.11477/mf.1416201530. [DOI] [PubMed] [Google Scholar]
- 2.Saini V, Guada L, Yavagal DR. Global epidemiology of stroke and access to acute ischemic stroke interventions. Neurology. 2021;97(Suppl 2):S6–S16. doi: 10.1212/WNL.0000000000012781. [DOI] [PubMed] [Google Scholar]
- 3.Kuriakose D, Xiao Z. Pathophysiology and treatment of stroke: present status and future perspectives. Int J Mol Sci. 2020;21:7609. doi: 10.3390/ijms21207609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee EC, Ha TW, Lee DH, Hong DY, Park SW, Lee JY, Lee MR, Oh JS. Utility of exosomes in ischemic and hemorrhagic stroke diagnosis and treatment. Int J Mol Sci. 2022;23:8367. doi: 10.3390/ijms23158367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gurková E, Štureková L, Mandysová P, Šaňák D. Factors affecting the quality of life after ischemic stroke in young adults: a scoping review. Health Qual Life Outcomes. 2023;21:4. doi: 10.1186/s12955-023-02090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alsubiheen AM, Choi W, Yu W, Lee H. The effect of task-oriented activities training on upper-limb function, daily activities, and quality of life in chronic stroke patients: a randomized controlled trial. Int J Environ Res Public Health. 2022;19:14125. doi: 10.3390/ijerph192114125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vitti E, Hillis AE. Treatment of post-stroke aphasia: a narrative review for stroke neurologists. Int J Stroke. 2021;16:1002–1008. doi: 10.1177/17474930211017807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Q, Li W, Yin Y, Zhao Z, Yang Y, Zhao Y, Tan Y, Yu J. The effect of music therapy on language recovery in patients with aphasia after stroke: a systematic review and meta-analysis. Neurol Sci. 2022;43:863–872. doi: 10.1007/s10072-021-05743-9. [DOI] [PubMed] [Google Scholar]
- 9.Su XT, Wang L, Ma SM, Cao Y, Yang NN, Lin LL, Fisher M, Yang JW, Liu CZ. Mechanisms of acupuncture in the regulation of oxidative stress in treating ischemic stroke. Oxid Med Cell Longev. 2020;2020:7875396. doi: 10.1155/2020/7875396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wen J, Chen X, Yang Y, Liu J, Li E, Liu J, Zhou Z, Wu W, He K. Acupuncture medical therapy and its underlying mechanisms: a systematic review. Am J Chin Med. 2021;49:1–23. doi: 10.1142/S0192415X21500014. [DOI] [PubMed] [Google Scholar]
- 11.Choi EY, Nieves GA, Jones DE. Acute stroke diagnosis. Am Fam Physician. 2022;105:616–624. [PubMed] [Google Scholar]
- 12.Cumpston MS, McKenzie JE, Welch VA, Brennan SE. Strengthening systematic reviews in public health: guidance in the Cochrane Handbook for Systematic Reviews of Interventions, 2nd edition. J Public Health (Oxf) 2022;44:e588–e592. doi: 10.1093/pubmed/fdac036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang ZQ, Zhu Y, Jiang YF. Clinical effect of Jieyufang combined with acupuncture on aphasia after ischemic stroke. Chin Mod Med. 2022;29:91–94. 98. [Google Scholar]
- 14.Zhang KK, Zhao YH. Clinical observation on 45 cases of motor aphasia after ischemic stroke treated with acupuncture and moxibustion. Chin J Ethnomed Ethnopharm. 2019;28:94–96. [Google Scholar]
- 15.Liu L. To observe the clinical effect of acupuncture and moxibustion on apoplectic aphasia. Women’s Health Res. 2019;74:141. [Google Scholar]
- 16.Huang QS. Effect of acupuncture combined with speech rehabilitation on motor aphasia after ischemic stroke. Clin Res. 2022;30:136–139. [Google Scholar]
- 17.Weng PX, Zheng JL, Chen JB. The impact of acupuncture combined with speech rehabilitation training on functional recovery and quality of life in post-stroke aphasia patients. Chin Clin Res Tradit Chin Med. 2019;11:87–89. [Google Scholar]
- 18.Jiang XF. Clinical observation on treatment of motor aphasia after ischemic stroke with acupuncture and moxibustion. Chin Health Care Nutr. 2020;30:113. [Google Scholar]
- 19.Xu HM, Xie YT, Cui Y. Clinical study on apoplectic aphasia treated with acupuncture and moxibustion. Asia-Pacific Tradit Med. 2017;13:131–132. [Google Scholar]
- 20.Ding ZL, Gao L, Gu SZ. Clinical study on aphasia of acute ischemic stroke treated with acupuncture combined with medicine. Chin J Inf Tradit Chin Med. 2007;14:12–14. [Google Scholar]
- 21.Yin XJ. Effect of acupuncture combined with language training on aphasia after stroke. Chin Health Care Nutr. 2019;29:366. [Google Scholar]
- 22.Tang LY. To study the clinical effect and mechanism of acupuncture and moxibustion on apoplectic aphasia. Chin Pract Med. 2016;11:272–273. [Google Scholar]
- 23.Wang L, Xiong X, Zhang L, Shen J. Neurovascular unit: a critical role in ischemic stroke. CNS Neurosci Ther. 2021;27:7–16. doi: 10.1111/cns.13561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhuo B, Deng S, Li B, Zhu W, Zhang M, Qin C, Meng Z. Possible effects of acupuncture in poststroke aphasia. Behav Neurol. 2023;2023:9445381. doi: 10.1155/2023/9445381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang S, Li L, Jiang R, Ding H, Xu F, Ge L, Kuang P, Wang Z. Tongue acupuncture for the treatment of poststroke aphasia: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2022;2022:4731074. doi: 10.1155/2022/4731074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sang B, Deng S, Zhai J, Hao T, Zhuo B, Qin C, Zhang M, Zhao X, Meng Z. Does acupuncture therapy improve language function of patients with aphasia following ischemic stroke? A systematic review and meta-analysis. NeuroRehabilitation. 2022;51:231–245. doi: 10.3233/NRE-220007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Wang Z, Jiang X, Lv Z, Wang L, Lu L. Effectiveness of acupuncture for poststroke aphasia: a systematic review and meta-analysis of randomized controlled trials. Complement Med Res. 2021;28:545–556. doi: 10.1159/000512672. [DOI] [PubMed] [Google Scholar]
- 28.Zhou D, Liang R, Zhu L, Tang Q. A meta-analysis of functional recovery of aphasia after stroke by acupuncture combined with language rehabilitation training. Medicine (Baltimore) 2023;102:e36160. doi: 10.1097/MD.0000000000036160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ning B, Wang Z, Wu Q, Deng Q, Yang Q, Gao J, Fu W, Deng Y, Wu B, Huang X, Mei J, Fu W. Acupuncture inhibits autophagy and repairs synapses by activating the mTOR pathway in Parkinson’s disease depression model rats. Brain Res. 2023;1808:148320. doi: 10.1016/j.brainres.2023.148320. [DOI] [PubMed] [Google Scholar]
- 30.Liu H, Zhang B, Li XW, Du J, Feng PP, Cheng C, Zhu ZH, Lou KL, Ruan C, Zhou C, Sun XW. Acupuncture inhibits mammalian target of rapamycin, promotes autophagy and attenuates neurological deficits in a rat model of hemorrhagic stroke. Acupunct Med. 2022;40:59–67. doi: 10.1177/09645284211028873. [DOI] [PubMed] [Google Scholar]