Abstract
Objective: To evaluate operative outcomes and postoperative complications of laparoscopic treatment for pediatric inguinal hernia using meta-analysis. Methods: We conducted a comprehensive search of databases including the Chinese Journal Full-text Database, Wanfang, PubMed, Web of Science, ScienceDirect, VIP Chinese Science, and Technology Journal Database, ProQuest, JSTOR, Wiley, and IEEE Xplore. Relevant randomized controlled trials (RCTs) on laparoscopic surgery for pediatric inguinal hernia were collected, and data were analyzed using Review Manager 5.3. Results: A total of 18 RCTs involving 5,750 children (3,357 in the laparoscopic group and 2,393 in the open surgery group) were included. Compared to the open surgery group, the laparoscopic group had significantly shorter operative times for bilateral hernias [(mean difference (MD) = -11.43, P = 0.04)], and lower incidences of metachronous contralateral inguinal hernia (MCIH) (MD = 0.17, P = 0.02) and testicular ascent (MD = 0.19, P = 0.03). However, there were no significant differences in operative time for unilateral hernia (MD = 0.47, P = 0.87), complication rate (MD = 0.87, P = 0.60), postoperative recurrence (MD = 1.46, P = 0.18), incision infection rate (MD = 2.54, P = 0.34), or testicular atrophy rate (MD = 0.36, P = 0.19). Conclusion: Laparoscopic surgery for pediatric inguinal hernia is effective, especially for bilateral cases, reducing operative time and lowering the risk of MCIH and testicular ascent.
Keywords: Laparoscopic, hernia, inguinal, open operation, child, meta
Introduction
The inguinal region is the triangular area at the junction of the lower abdominal wall and the thigh. An inguinal hernia occurs when internal organs protrude through a defect in the inguinal area, commonly referred to as a “hernia” [1]. This condition is frequently seen in pediatric surgery, with an incidence ranging from 0.8% to 4.4% [2]. The primary pathologic cause is a congenital failure of the vaginalis process to close, with increased intra-abdominal pressure acting as a triggering factor [3,4].
Currently, most researchers agree that as children grow, the abdominal wall muscles, aponeurosis, and other tissues continue to strengthen. Therefore, simple high ligation of the hernia sac remains the standard treatment for pediatric inguinal hernia [5]. However, open surgery, which involves dissecting the inguinal canal and freeing the spermatic cord and hernia sac, carries risks such as spermatic vessel injury, testicular atrophy, and iatrogenic cryptorchidism. Besides, this method has several disadvantages, including high trauma, scarring, and a prolonged recovery time [6].
In recent years, advancements in technology, and in minimally invasive surgery have led to the widespread adoption of laparoscopic techniques in pediatric inguinal hernia repair. Laparoscopic surgery offers advantages such as minimal invasiveness, faster recovery, lower recurrence rate, and improved cosmetic outcome [7,8]. However, the clinical efficacy, surgical outcome, recurrence rate, and complications associated with laparoscopic surgery in children remain debated. Currently, there is insufficient high-quality, large-scale clinical data to validate conclusively its benefits through evidence-based medicine.
Meta-analysis, a statistical method for quantitatively synthesizing independent research results, can provide comprehensive evidence for these surgical comparisons [9]. Therefore, we conducted a meta-analysis to compare surgical outcomes, recurrence rates, and postoperative complications between laparoscopic and traditional open surgery for pediatric inguinal hernia, aiming to provide stronger evidence-based guidance for clinical decision-making.
Materials and methods
PROSPERO statement
This study has been registered with PROSPERO (CRD42024578885).
Retrieval tool
We systematically searched multiple databases, including the Chinese Journal Full-text Database, VIP Chinese Science and Technology Journal Database, ProQuest, Wanfang, PubMed, JSTOR, Web of Science, ScienceDirect, Wiley, and IEEE Xplore, to collect randomized controlled trials (RCTs) comparing laparoscopic and traditional open surgery for pediatric inguinal hernia. The search covered studies from database inception to February 31, 2024. English search terms included “children”, “inguinal hernia”, “groin hernia”, “direct inguinal”, “laparoscope”, “laparoscopic surgery”, “open surgery”, and “traditional surgery”, connected with “OR” or “AND” as appropriate. We also manually searched the reference lists of included studies.
English subject terms included “laparoscopic”, “open operation”, “infantile inguinal hernia”, and “child”. Free terms included “efficacy”, “operative time bilateral”, “MCIH”, “testis ascending”, “operative time unilateral”, “complication”, “postoperative recurrence”, “incision infection”, “testis atrophy”, “RCT”, and “randomized controlled trial”. We adjusted the search strategy based on the specific database and used a combination of subject and free terms. The detailed search strategy is as follows: (((((((((((((((laparoscopic[Title/Abstract]) AND (open operation[Title/Abstract])) AND (infantile inguinal hernia[Title/Abstract])) AND (child[Title/Abstract])) AND (efficacy[Title/Abstract])) OR (operative time bilateral[Title/Abstract])) OR (MCIH[Title/Abstract])) OR (metachronous contralateral inguinal hernia[Title/Abstract])) OR (testis ascending[Title/Abstract])) OR (operative time unilateral[Title/Abstract])) OR (complication[Title/Abstract])) OR (postoperative recurrence[Title/Abstract])) OR (incision infection[Title/Abstract])) OR (testis atrophy[Title/Abstract])) OR (RCT[Title/Abstract])) OR (randomized controlled trial[Title/Abstract]).
Inclusion criteria
Studies were included if they met the following criteria: (1) RCT design; (2) Subjects were children; (3) Clear diagnosis of inguinal hernia [10]; (4) Comparison of laparoscopic surgery with open surgery; (5) Clear outcome indicators; (6) Complete data and published in English.
Exclusion criteria
Studies were excluded if they met any of the following: (1) Subjects had hydrocele, testicular insufficiency, testicular mass, history of abdominal or groin surgery, recurrent hernia; (2) Reviews, case reports, clinical guidelines, or conference abstracts; (3) Poor study design, lack of clear results, or unclear data reporting; (4) Incomplete data or logical errors; (5) Duplicate publications.
RCT bias risk assessment
The risk of bias in included RCTs was assessed using the Cochrane tool [11]. This tool evaluates several types of bias: selection, performance, detection, attrition, and reporting bias. Two independent researchers conducted the assessment, and any disagreements were resolved through discussion or consultation with a third party.
Literature screening and data extraction
We systematically searched databases to identify literature related to the clinical efficacy of laparoscopic treatment for pediatric inguinal hernia. We reviewed abstracts and keywords, selecting studies based on predefined inclusion and exclusion criteria. The extracted data included the first author, publication year, number of cases (laparoscopy/open group), age, sex, follow-up duration, outcome measures, and measured data. This process was conducted independently by two researchers using standardized protocols. After extraction, discrepancies were resolved through discussion or by consulting a third researcher.
Outcome measures included operative time, recurrence rate, complication rate, incision infection rate, MCIH incidence, testicular atrophy rate, and testicular ascent rate. Recurrence was defined as the reappearance of a bulge at or near the site of the previous repair, confirmed by ultrasound as containing a loop of intestine [12]. Operative time was measured from anesthesia induction to wound closure, including unilateral and bilateral cases [13]. MCIH refers to the development of a contralateral hernia after previous inguinal hernia surgery [14].
Statistical analysis
Meta-analysis was conducted using Review Manager 5.3. The Cochrane Q test and I2 statistic were used to assess heterogeneity among studies. The Z-test was applied to further analyze inter-study variability. If heterogeneity was absent (P > 0.1, I2 < 50%), a fixed-effects model (FEM) was employed. In cases of significant heterogeneity, a random-effects model (REM) was adopted. The I2 statistic quantifies variability between studies, with I2 = 0 indicating that all variability is due to sampling error. I2 values between 0.25 and 0.5 indicate moderate heterogeneity, while values above 0.5 suggest high heterogeneity.
Mean difference (MD) and relative risk (RR) were used as effect measures for continuous and categorical data, respectively, with 95% confidence intervals (CI) provided. A funnel plot was generated to evaluate publication bias, and sensitivity analysis was performed by comparing FEM and REM results. The Begg rank correlation test and Egger’s linear regression method were used in STATA 15.0 to detect publication bias. Evidence quality was graded using GRADEpro 3.6.
Results
Literature screening process
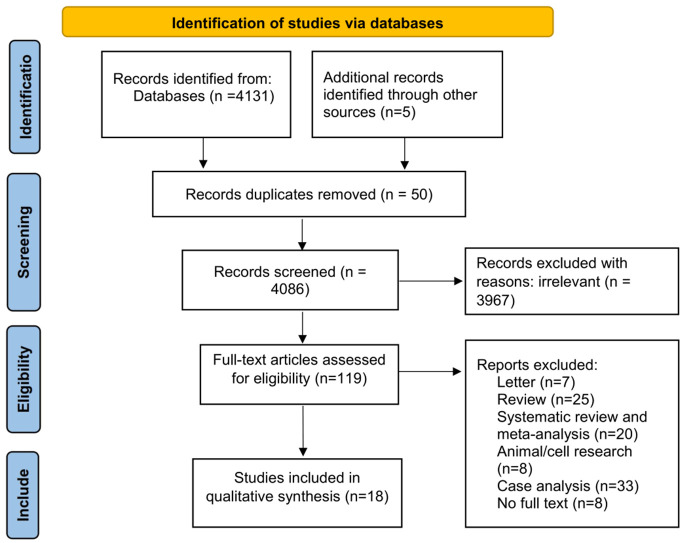
We initially identified 4,136 studies, and after a rigorous screening process, 18 studies were included in the meta-analysis [15-32]. These studies comprised 3,357 laparoscopic and 2,393 open surgical procedures (Figure 1).
Figure 1.
Literature screening and elimination flow chart.
Data from the 18 studies
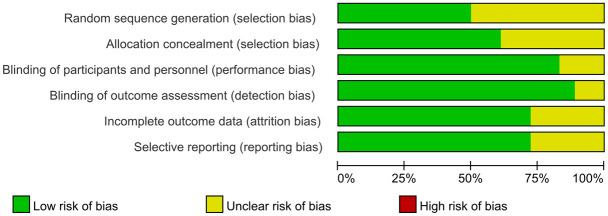
Complete information was obtained from all 18 studies (Table 1). Overall, the studies were of high quality with minimal impact on the strength of evidence in the meta-analysis. Low bias risk in random sequence generation (selection bias), allocation concealment (selection bias), participant and personnel blinding (performance bias), outcome assessment blinding (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias) have been demonstrated. Other studies showed some uncertainty in the degree of bias risk (Figure 2).
Table 1.
Information from 18 studies included
| First author and year | Surgery | Cases | Age (months) | Gender (Male/female) | Follow-up time | Outcome indicator |
|---|---|---|---|---|---|---|
| Celebi S 2014 [15] | Laparoscopy | 30 | 8.24±2.60 | - | 3 months after surgery | ① ③ |
| Open | 32 | 7.83±1.58 | - | |||
| Koivusalo AI 2009 [16] | Laparoscopy | 47 | 6.00 | (36/11) | 2 years after surgery | ① ② ③ |
| Open | 42 | 6.10 | (30/12) | |||
| Saranga Bharathi R 2008 [17] | Laparoscopy | 35 | 5.58±3.52 | (30/5) | 3.5 months (mean) | ① ② ③ |
| Open | 34 | 3.14±0.92 | (32/2) | |||
| Chan KL 2005 [18] | Laparoscopy | 41 | 4.67±3.81 | (34/7) | 12.21±2.83 | ① ② ③ |
| Open | 42 | 3.83±2.85 | (33/9) | 11.79±2.54 | ||
| Shalaby R 2012 [19] | Laparoscopy | 125 | 58 1-12 months, 45 12-24 months, 22 > 24 months | (38/87) | 24 months (mean) | ② ③ ④ ⑥ ⑦ |
| Open | 125 | 50 1-12 months, 55 12-24 months, 20 > 24 months | (92/33) | |||
| Timberlake MD 2015 [20] | Laparoscopy | 38 | 21.5 months (median) | (34/4) | 51 days (median) | ② |
| Open | 38 | 23 months (median) | (36/2) | 47 days (median) | ||
| Nah SA 2011 [21] | Laparoscopy | 28 | 5.39±4.11 | (23/5) | 3 months (median) | ② ③ ⑥ ⑦ |
| Open | 35 | 3.1 months (median) | (31/4) | 4 weeks - 3 years | ||
| Mishra PK 2014 [22] | Laparoscopy | 27 | NR | (24/3) | 4 weeks - 3 years | ② ③ ④ ⑤ ⑥ |
| Open | 45 | NR | (40/5) | 4 weeks - 2 years | ||
| Lin CD 2011 [23] | Laparoscopy | 24 | 7.17±4.21 | (20/4) | 22.9±10.5 months | ① ② |
| Open | 31 | 5.39±4.11 | (25/6) | 20.2±10.5 months | ||
| Koivusalo A 2007 [24] | Laparoscopy | 18 | 5.1 months (median) | (17/1) | 26 months (median) | ② |
| Open | 15 | 9.1 months (median) | (14/1) | |||
| Jun Z 2016 [25] | Laparoscopy | 84 | 1.8 years (median) | (48/36) | 3-9 month | ② |
| Open | 42 | 2 years (median) | (20/22) | |||
| Hassan ME 2007 [26] | Laparoscopy | 15 | 39 months (median) | (15/0) | 3 months | ② |
| Open | 18 | 44 months (median) | (18/0) | |||
| Endo M 2009 [27] | Laparoscopy | 1257 | 3.7±3.2 | (694/563) | 1-11 years | ① ② |
| Open | 308 | 3.8±2.9 | (226/82) | |||
| Amano H 2017 [28] | Laparoscopy | 1033 | 49.0±36.2 | (488/545) | 29.1±24.3 months | ② ④ ⑤ ⑦ |
| Open | 995 | 48.8±36.0 | (632/363) | 49.3±50.5 months | ||
| Ahmed A 2022 [29] | Laparoscopy | 148 | 4.58±2.97 | (133/15) | 6 months after surgery | ① ② |
| Open | 148 | 4.96±3.13 | (133/15) | |||
| Kara YA 2021 [30] | Laparoscopy | 227 | 4.56±3.74 | (144/83) | 30.4 months | ① ② ③ |
| Open | 178 | 4.19±3.34 | (123/55) | 24.4 months (mean) | ||
| Ergün E 2021 [31] | Laparoscopy | 85 | (73/12) | 12 months after the surgery | ① ② | |
| Open | 55 | (44/11) | ||||
| Suttiwongsing A 2022 [32] | Laparoscopy | 95 | 3 years (median) | (62/) | 23.7±0.7 months | ① ② |
| Open | 210 | 3 years (median) | (146/) | 33.1±5.7 months |
Note: Outcome indicator: ① Operation time (min); ② Recurrence rate; ③ Complication rate; ④ Incision infection rate; ⑤ MCIH occurrence rate; ⑥ Testis atrophy rate; ⑦ Testicular ascent rate; NR: not reported.
Figure 2.
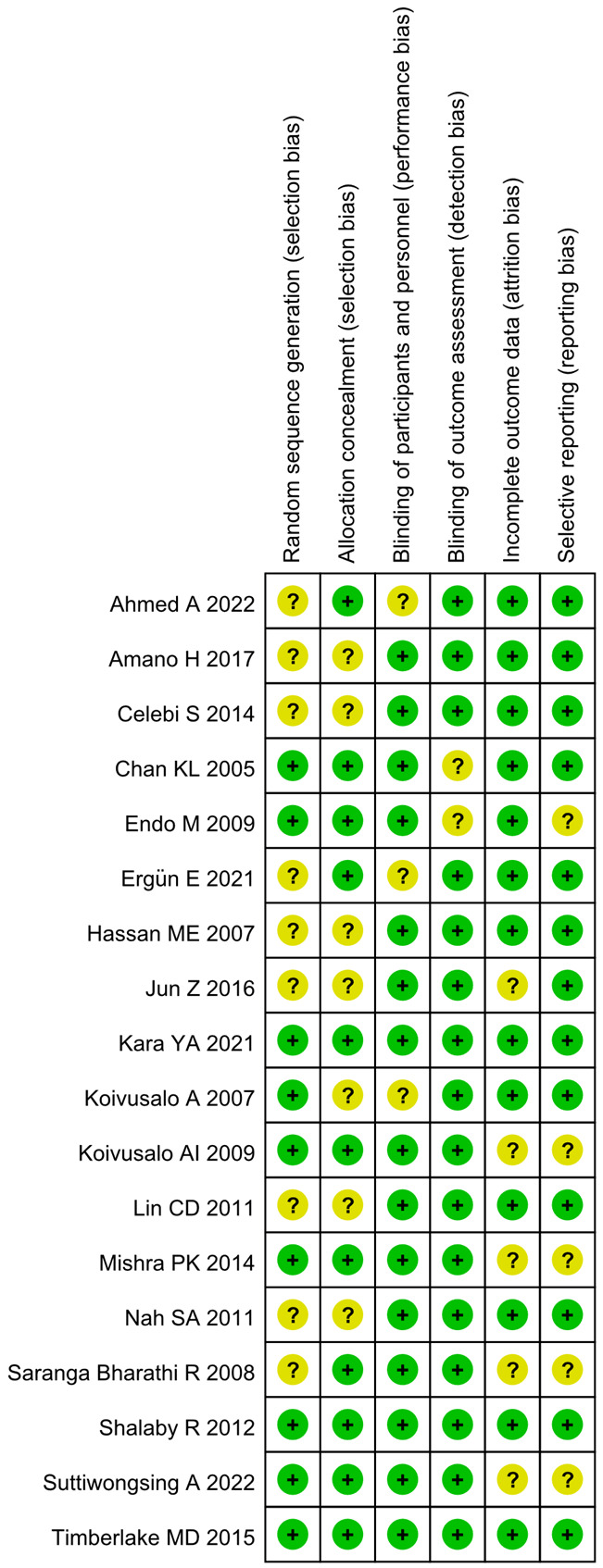
Risk of bias across studies. Note: Kara YA 2021, Shalaby R 2012, and Timberlake MD 2015 demonstrated a higher risk of bias in random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias). Other studies displayed some degree of uncertainty regarding these risks of bias.
More than 50% of studies had low risk of bias for allocation concealment, participant and personnel blinding, outcome assessment blinding, incomplete outcome data, and selective reporting. Additionally, over 75% of studies demonstrated low risk of performance and detection bias (Figure 3).
Figure 3.
Risk of bias in 18 studies. Note: Among the included studies, more than 50% had a low risk of bias for allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias). Furthermore, more than 75% of studies showed a low risk of bias in participants and personnel (performance bias) and blinding of outcome assessment (detection bias).
Meta-analysis
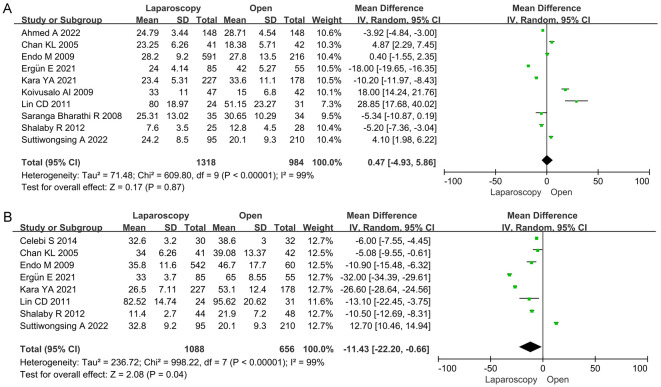
Operation time
Ten papers reported the operative time for unilateral hernias. Meta-analysis showed no significant difference in operative time between the groups (MD = 0.47, 95% CI: -4.93-5.86, P = 0.87) (Figure 4A). For bilateral hernias, eight studies were included, and meta-analysis indicated that the laparoscopic group had a shorter operative time (MD = -11.43, 95% CI: -22.20-0.66, P = 0.04) (Figure 4B).
Figure 4.
Forest map of operation time comparison. Note: (A) Operative Time (min) Unilateral; (B) Operative Time (min) Bilateral.
Complication rate
Eight papers reported complication rates, and meta-analysis revealed no significant difference between the laparoscopic and open surgery groups (MD = 0.87, 95% CI: 0.51-1.46, P = 0.60) (Figure 5).
Figure 5.
Forest map comparing complication rates.
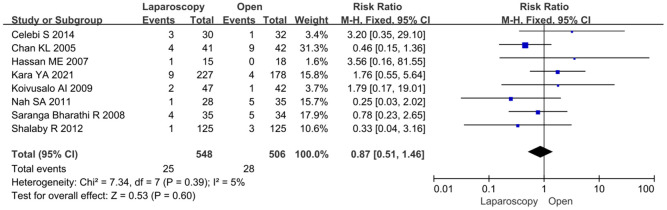
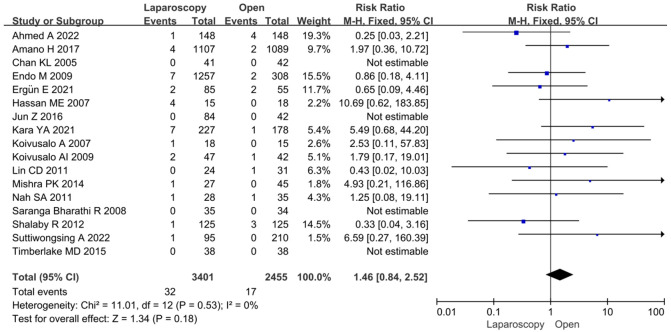
Postoperative recurrence rate
Seventeen studies provided data on recurrence rates, and meta-analysis showed no significant difference between the groups (MD = 1.46, 95% CI: 0.84-2.52, P = 0.18) (Figure 6).
Figure 6.
Forest map comparing postoperative recurrence rates.
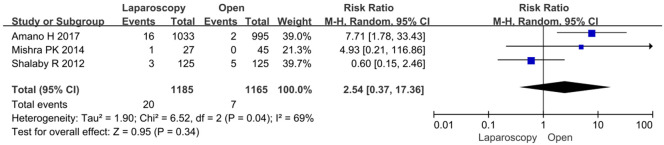
Incision infection rate
Three studies reported incision infection rates. Meta-analysis showed no significant difference between the groups (MD = 2.54, 95% CI: 0.37-17.36, P = 0.34) (Figure 7).
Figure 7.
Forest map of incision infection rate comparison.
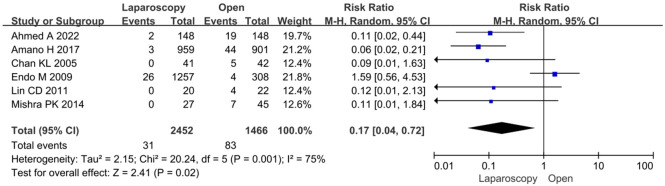
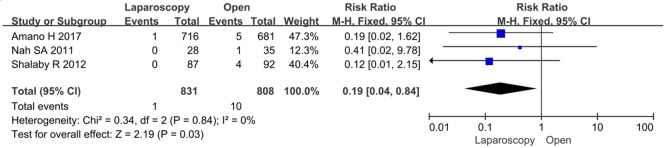
MCIH occurrence rate
Six studies reported the occurrence of MCIH. The incidence was significantly lower in the laparoscopic group (MD = 0.17, 95% CI: 0.04-0.72, P = 0.02) (Figure 8).
Figure 8.
Forest map of metachronous contralateral inguinal hernia, occurrence rate.
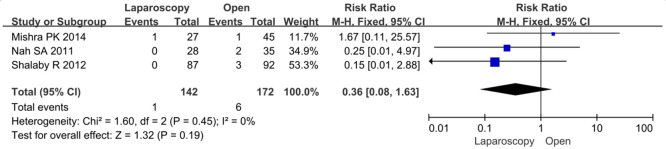
Testicular atrophy rate
Three studies reported the rate of testicular atrophy, and meta-analysis showed no significant difference between the groups (MD = 0.36, 95% CI: 0.08-1.63, P = 0.19) (Figure 9).
Figure 9.
Forest map comparing testicular atrophy rates.
Testicular ascent rate
Three studies reported the rate of testicular ascent. Meta-analysis indicated that the testicular ascent rate was significantly lower in the laparoscopic group (MD = 0.19, 95% CI: 0.04-0.84, P = 0.03) (Figure 10).
Figure 10.
Forest map for comparison of testicular ascent rate.
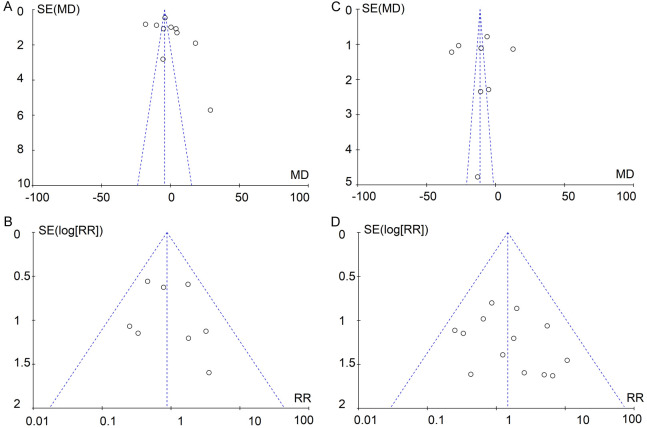
Publication bias risk assessment and sensitivity analysis
A funnel plot (Figure 11) was used to assess publication bias. For operative time (unilateral and bilateral), there was evidence of publication bias, as some studies intersected with or were outside the funnel plot’s confidence limits. However, no publication bias was found for complication rate or recurrence rate, as the funnel plots showed good symmetry. Due to limited data, publication bias could not be evaluated for incision infection rate, MCIH incidence, testicular atrophy rate, or testicular ascent rate. Sensitivity analysis, conducted by comparing FEM and REM results, showed no significant change in the combined effect sizes for all outcomes except testicular ascent, indicating that the meta-analysis results were robust and reliable.
Figure 11.
Publication bias assessment. Note: (A) Operative Time Unilateral; (B) Operative Time Bilateral; (C) Complication rate; (D) Postoperative recurrence rate. MD: mean difference; RR: relative risk; SE: standard error.
Among the 10 studies on unilateral operative time, the Begg rank correlation test (P = 0.353) and Egger linear regression method (P = 0.603) indicated no significant publication bias. For bilateral operative time (8 studies), Begg (P = 0.692) and Egger (P = 0.125) also showed no significant publication bias. Similarly, for complication rate (8 studies), the Begg (P = 0.412) and Egger (P = 0.569) tests suggested no significant publication bias. Regarding recurrence rate (17 studies), Begg (P = 0.620) and Egger (P = 0.553) indicated no significant publication bias. The same was true for incision infection rate (Begg: P = 0.559, Egger: P = 0.163), MCIH incidence (Begg: P = 0.713, Egger: P = 0.125), testicular atrophy rate (Begg: P = 0.367, Egger: P = 0.072), and testicular ascent rate (Begg: P = 0.621, Egger: P = 0.103).
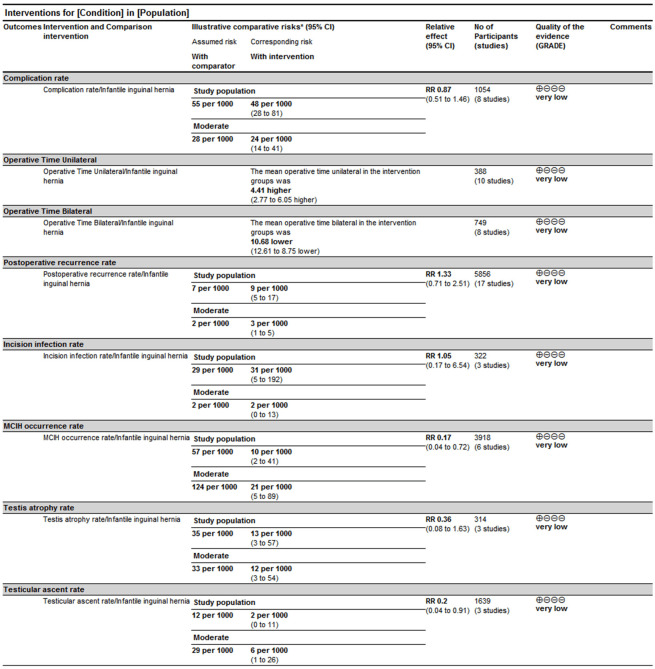
GRADE assessment
Using GRADEpro 3.6 software, the quality of evidence for operation time, complication rate, postoperative recurrence rate, incision infection rate, MCIH occurrence rate, testicular atrophy rate, and testicular ascent rate was assessed as very low (Figure 12).
Figure 12.
GRADE assessment. Note: MCIH: metachronous contralateral inguinal hernia.
Discussion
Inguinal hernia is a common congenital condition in children, with surgery being the definitive treatment. Traditional high ligation of the hernia sac has several limitations, such as visible scarring, inability to simultaneously detect contralateral occult hernias, significant trauma, and a relatively high recurrence rate [33]. Christophersen et al. [34] reported that the recurrence rate after open inguinal hernia repair can be as high as 5%. Therefore, it is crucial to explore other effective surgical methods for pediatric inguinal hernia treatment. Laparoscopic surgery has gained popularity due to its advantages, including minimal trauma, faster recovery, reduced blood loss, and the ability to explore contralateral hernias and visualize local anatomy [35].
Ensuring patient safety during surgery is paramount. Our systematic analysis revealed several benefits of laparoscopic surgery in treating pediatric inguinal hernia, including shorter bilateral operative time, lower rate of MCIH, and reduced testicular ascent. The shorter operative time for bilateral hernias in laparoscopic surgery, compared to open surgery, may be due to the smaller incisions, the use of electrocoagulation, and the lack of need to separate the hernia sac. Additionally, the clearer visual field in laparoscopic procedures helps avoid injury to key structures such as blood vessels and nerves, reducing the need for additional intraoperative maneuvers and shortening the operative time [36]. However, the operative time for unilateral hernias showed no significant advantage performed by laparoscopy, likely because unilateral hernia repairs are less complex and can be performed quickly, regardless of the surgical approach [37]. Pulikkal et al. [38] also demonstrated that the average operative time for unilateral hernia repair was 8 minutes, while bilateral hernia repair took 11 minutes, with similar findings in laparoscopic surgery.
The discrepancy in operative times between different studies could be attributed to individual patient factors and the surgeon’s proficiency with laparoscopic techniques. For instance, in laparoscopic surgery, there is no need to separate the spermatic cord or open the cremaster muscle. However, Zhang et al. [39] found that laparoscopic surgery extended the operative time, which contradicts our findings, possibly due to the surgeons’ varying levels of expertise. Therefore, continuous improvement in laparoscopic technical standards and training programs is essential.
Our quantitative analysis also showed a lower incidence of MCIH following laparoscopic surgery (0.3%) compared to open surgery (3.7%) [40]. MCIH often occurs after unilateral hernia repair, and most experts believe it originates from a contralateral patent processus vaginalis (CPPV), though the exact mechanism is still unclear [41]. Laparoscopic percutaneous high ligation (LPEC) allows for the timely detection and treatment of CPPV on the contralateral side, reducing the risk of postoperative MCIH [42].
Testicular displacement after hernia repair in children may result from factors such as excessive manipulation of the hernia sac, which can lead to damage of the testis, spermatic cord, and surrounding tissues. These injuries may impair blood supply to the testis, slow the development of testicular interstitial cells, and reduce testosterone production. In some cases, surgical trauma can directly damage receptors on target cells, further affecting hormone levels. Obayashi et al. [43] identified birth weight below 932 g and spermatic duct hematoma as risk factors for testicular displacement. The lower risk of testicular ascent following laparoscopic hernia repair may be due to the less invasive nature of the procedure.
Our study confirmed that laparoscopic surgery is an effective and safe treatment for infantile inguinal hernia. As such, we recommend laparoscopic surgery as the first choice, provided economic conditions allow. However, in cases with specific conditions - such as infants younger than six months, patients with inguinal wall defects, or those with incarcerated hernias - traditional open surgery may be more appropriate.
The GRADE system was used to assess the quality of evidence across different outcome measures. Our analysis found that the quality of evidence was “Very Low” for operative time, complication rate, recurrence rate, incision infection rate, MCIH rate, testicular atrophy rate, and testicular ascent rate. This suggests that future studies may alter the conclusions in these areas.
Despite establishing strict inclusion and exclusion criteria and conducting a risk-of-bias assessment, our study has several limitations. Some included studies exhibited high heterogeneity, likely due to differences in patient age, physical characteristics, and surgical complexity. Furthermore, certain outcomes, such as incision infection rate, testicular atrophy rate, and testicular ascent rate, were based on only three studies, limiting the robustness of the findings. Another limitation is that our study did not account for the specific type of laparoscopic technique used, which may influence outcome. Additionally, the relatively small number of included studies made it difficult to conduct subgroup analyses based on age or disease severity.
As a result, while our meta-analysis provides valuable insights, more further research is needed to strengthen the evidence base. Due to these limitations, the conclusions presented here should be interpreted cautiously and considered a reference for clinical decision-making.
In conclusion, based on current evidence, laparoscopic surgery for infantile inguinal hernia is effective, especially for bilateral cases, where it shortens operative time and reduces the risk of MCIH and testicular displacement. However, this evidence does not definitively establish that laparoscopic surgery is safer than open surgery.
Disclosure of conflict of interest
None.
References
- 1.Huang Y, Huang C, Luo J, Cheng T. Laparoscopic inguinal hernia repair and synchronous peritoneal dialysis catheter placement: a single-center experience. J Laparoendosc Adv Surg Tech A. 2023;33:1184–1188. doi: 10.1089/lap.2023.0297. [DOI] [PubMed] [Google Scholar]
- 2.Wimper Y, Stortelder E, Botden SMBI, de Blaauw I. Inguinal hernia in children: easily incarcerated. Ned Tijdschr Geneeskd. 2021;165:D5330. [PubMed] [Google Scholar]
- 3.Raitio A, Kalliokoski N, Syvänen J, Harju S, Tauriainen A, Hyvärinen A, Gissler M, Helenius I, Sankilampi U. High incidence of inguinal hernias among patients with congenital abdominal wall defects: a population-based case-control study. Eur J Pediatr. 2021;180:2693–2698. doi: 10.1007/s00431-021-04172-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinoshita S, Ohyama T, Kawaguchi C, Ikeda N, Sho M. Significance of umbilical trocar size and intra-abdominal pressure on postoperative pain after transabdominal preperitoneal repair for inguinal hernia. Asian J Endosc Surg. 2021;14:63–69. doi: 10.1111/ases.12813. [DOI] [PubMed] [Google Scholar]
- 5.Hassler KR, Saxena P, Baltazar-Ford KS. Open inguinal hernia repair. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed] [Google Scholar]
- 6.Shah MY, Raut P, Wilkinson TRV, Agrawal V. Surgical outcomes of laparoscopic total extraperitoneal (TEP) inguinal hernia repair compared with Lichtenstein tension-free open mesh inguinal hernia repair: a prospective randomized study. Medicine (Baltimore) 2022;101:e29746. doi: 10.1097/MD.0000000000029746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amundson JR, Attaar M, Forester B, Francis S, Kuchta K, Denham W, Linn J, Ujiki MB, Haggerty SP. Laparoscopic and robotic inguinal hernia repair are safe and effective after prior pelvic or low abdominal surgery. Am J Surg. 2023;225:252–257. doi: 10.1016/j.amjsurg.2022.08.011. [DOI] [PubMed] [Google Scholar]
- 8.Hidalgo NJ, Guillaumes S, Bachero I, Butori E, Espert JJ, Ginestà C, Vidal Ó, Momblán D. Bilateral inguinal hernia repair by laparoscopic totally extraperitoneal (TEP) vs. laparoscopic transabdominal preperitoneal (TAPP) BMC Surg. 2023;23:270. doi: 10.1186/s12893-023-02177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solaini L, Cavaliere D, Avanzolini A, Rocco G, Ercolani G. Robotic versus laparoscopic inguinal hernia repair: an updated systematic review and meta-analysis. J Robot Surg. 2022;16:775–781. doi: 10.1007/s11701-021-01312-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shakil A, Aparicio K, Barta E, Munez K. Inguinal hernias: diagnosis and management. Am Fam Physician. 2020;102:487–492. [PubMed] [Google Scholar]
- 11.Marcolin P, Mazzola Poli de Figueiredo S, Oliveira Trindade B, Bueno Motter S, Brandão GR, Mao RD, Moffett JM. Prophylactic mesh augmentation in emergency laparotomy closure: a meta-analysis of randomized controlled trials with trial sequential analysis. Hernia. 2024;28:677–690. doi: 10.1007/s10029-023-02943-4. [DOI] [PubMed] [Google Scholar]
- 12.Vitiello A, Abu Abeid A, Peltrini R, Ferraro L, Formisano G, Bianchi PP, Del Giudice R, Taglietti L, Celentano V, Berardi G, Bracale U, Musella M. Minimally invasive repair of recurrent inguinal hernia: multi-institutional retrospective comparison of robotic versus laparoscopic surgery. J Laparoendosc Adv Surg Tech A. 2023;33:69–73. doi: 10.1089/lap.2022.0209. [DOI] [PubMed] [Google Scholar]
- 13.Wolak PK, Strzelecka A, Piotrowska A, Dąbrowska K, Wolak PP, Piotrowska I, Nowak-Starz G. The operative time for unilateral inguinal hernia repair in children performed with percutaneous internal ring suturing (PIRS) or open approach method. J Clin Med. 2021;10:1293. doi: 10.3390/jcm10061293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu L, Chen X, Xu W, Liu J, Huang X, Xiong J, Lv Z. The relationship between contralateral patent processus vaginalis and metachronous contralateral inguinal hernia in children with unilateral inguinal hernia: a prospective observational study. Hernia. 2022;26:1161–1168. doi: 10.1007/s10029-022-02638-2. [DOI] [PubMed] [Google Scholar]
- 15.Celebi S, Uysal AI, Inal FY, Yildiz A. A single-blinded, randomized comparison of laparoscopic versus open bilateral hernia repair in boys. J Laparoendosc Adv Surg Tech A. 2014;24:117–21. doi: 10.1089/lap.2013.0397. [DOI] [PubMed] [Google Scholar]
- 16.Koivusalo AI, Korpela R, Wirtavuori K, Piiparinen S, Rintala RJ, Pakarinen MP. A single-blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics. 2009;123:332–7. doi: 10.1542/peds.2007-3752. [DOI] [PubMed] [Google Scholar]
- 17.Saranga Bharathi R, Arora M, Baskaran V. Pediatric inguinal hernia: laparoscopic versus open surgery. JSLS. 2008;12:277–81. [PMC free article] [PubMed] [Google Scholar]
- 18.Chan KL, Hui WC, Tam PK. Prospective randomized single-center, single-blind comparison of laparoscopic vs open repair of pediatric inguinal hernia. Surg Endosc. 2005;19:927–32. doi: 10.1007/s00464-004-8224-3. [DOI] [PubMed] [Google Scholar]
- 19.Shalaby R, Ibrahem R, Shahin M, Yehya A, Abdalrazek M, Alsayaad I, Shouker MA. Laparoscopic hernia repair versus open herniotomy in children: a controlled randomized study. Minim Invasive Surg. 2012;2012:484135. doi: 10.1155/2012/484135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Timberlake MD, Sukhu TA, Herbst KW, Rasmussen S, Corbett ST. Laparoscopic percutaneous inguinal hernia repair in children: review of technique and comparison with open surgery. J Pediatr Urol. 2015;11:262, e1–6. doi: 10.1016/j.jpurol.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 21.Nah SA, Giacomello L, Eaton S, de Coppi P, Curry JI, Drake DP, Kiely EM, Pierro A. Surgical repair of incarcerated inguinal hernia in children: laparoscopic or open? Eur J Pediatr Surg. 2011;21:8–11. doi: 10.1055/s-0030-1262793. [DOI] [PubMed] [Google Scholar]
- 22.Mishra PK, Burnand K, Minocha A, Mathur AB, Kulkarni MS, Tsang T. Incarcerated inguinal hernia management in children: ‘a comparison of the open and laparoscopic approach’. Pediatr Surg Int. 2014;30:621–4. doi: 10.1007/s00383-014-3507-9. [DOI] [PubMed] [Google Scholar]
- 23.Lin CD, Tsai YC, Chang SJ, Yang SS. Surgical outcomes of mini laparoscopic herniorrhaphy in infants. J Urol. 2011;185:1071–6. doi: 10.1016/j.juro.2010.10.044. [DOI] [PubMed] [Google Scholar]
- 24.Koivusalo A, Pakarinen MP, Rintala RJ. Laparoscopic herniorrhaphy after manual reduction of incarcerated inguinal hernia. Surg Endosc. 2007;21:2147–9. doi: 10.1007/s00464-007-9318-5. [DOI] [PubMed] [Google Scholar]
- 25.Jun Z, Juntao G, Shuli L, Li L. A comparative study on trans-umbilical single-port laparoscopic approach versus conventional repair for incarcerated inguinal hernia in children. J Minim Access Surg. 2016;12:139–42. doi: 10.4103/0972-9941.169953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hassan ME, Mustafawi AR. Laparoscopic flip-flap technique versus conventional inguinal hernia repair in children. JSLS. 2007;11:90–3. [PMC free article] [PubMed] [Google Scholar]
- 27.Endo M, Watanabe T, Nakano M, Yoshida F, Ukiyama E. Laparoscopic completely extraperitoneal repair of inguinal hernia in children: a single-institute experience with 1,257 repairs compared with cut-down herniorrhaphy. Surg Endosc. 2009;23:1706–12. doi: 10.1007/s00464-008-0300-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amano H, Tanaka Y, Kawashima H, Deie K, Fujiogi M, Suzuki K, Morita K, Iwanaka T, Uchida H. Comparison of single-incision laparoscopic percutaneous extraperitoneal closure (SILPEC) and open repair for pediatric inguinal hernia: a single-center retrospective cohort study of 2028 cases. Surg Endosc. 2017;31:4988–4995. doi: 10.1007/s00464-017-5472-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ahmed A, Hashim I, Mehmood F, Haider N, Chattha AA, Ayub A. Outcome of laparoscopic percutaneous extra peritoneal closure versus open repair for paediatric inguinal hernia. J Ayub Med Coll Abbottabad. 2022;34:403–406. doi: 10.55519/JAMC-03-10505. [DOI] [PubMed] [Google Scholar]
- 30.Kara YA, Yağız B, Balcı Ö, Karaman A, Özgüner İF, Karaman İ. Comparison of open repair and laparoscopic percutaneous internal ring suturing method in repairing inguinal hernia in children. Cureus. 2021;13:e14262. doi: 10.7759/cureus.14262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ergün E, Yağız B, Kara YA, Abay AN, Balcı Ö, Eryılmaz S, Özgüner İF, Karaman A, Karaman İ. Comparison of laparoscopic percutaneous internal ring suturing method and open inguinal hernia repair in children under 3 months of age. Turk J Surg. 2021;37:215–221. doi: 10.47717/turkjsurg.2021.5157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Suttiwongsing A, Khorana J, Ruangwongroj P, Niruttiwat K. Laparoscopic extraperitoneal technique versus open inguinal herniotomy in children: historical controlled intervention study. World J Pediatr Surg. 2022;5:e000436. doi: 10.1136/wjps-2022-000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao J, Zhai XQ, Li HC, Chong T. High ligation of the hernia sac in open nonmesh inguinal herniorrhaphy is an important cause of iatrogenic vas deferens injury. Asian J Androl. 2023;25:708–712. doi: 10.4103/aja202312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Christophersen C, Fonnes S, Andresen K, Rosenberg J. Lower recurrence rate after groin and primary ventral hernia repair performed by high-volume surgeons: a systematic review. Hernia. 2022;26:29–37. doi: 10.1007/s10029-020-02359-4. [DOI] [PubMed] [Google Scholar]
- 35.Cao Y, Ding Z, Qiang H. Analysis on influencing factors of recurrence after indirect inguinal hernia laparoscopic surgery. J Healthc Eng. 2022;2022:2978745. doi: 10.1155/2022/2978745. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 36.Chinn J, Tellez R, Huy B, Farzaneh C, Christian A, Ramsay J, Kim H, Smith B, Hinojosa MW. Comparison of BMI on operative time and complications of robotic inguinal hernia repair at a VA medical center. Surg Endosc. 2022;36:9398–9402. doi: 10.1007/s00464-022-09259-x. [DOI] [PubMed] [Google Scholar]
- 37.Ota M, Nitta T, Kataoka J, Fujii K, Ishibashi T. A study of the effectiveness of the bilateral and contralateral occult inguinal hernia repair by total extraperitoneal repair with intraperitoneal examination. Asian J Endosc Surg. 2022;15:97–102. doi: 10.1111/ases.12976. [DOI] [PubMed] [Google Scholar]
- 38.Pulikkal Reghunandanan R, Ali Usman A, Basheer S, Kuttichi L, Els Jojo J, Abdul Rasheed MF. Laparoscopic versus open inguinal hernia repair: a comparative study. Cureus. 2023;15:e48619. doi: 10.7759/cureus.48619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang L, Zhang R, Zhang J, Hu H, Chen Z, Fu Y, Li S. To use a simple hernia needle for single-port laparoscopic percutaneous inguinal hernia repair in children: a 5-year experience study. Front Pediatr. 2024;11:1298643. doi: 10.3389/fped.2023.1298643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu S, Xing X, He R, Zhao H, Zhong L, Sun J. Comparison of laparoscope-assisted single-needle laparoscopic percutaneous extraperitoneal closure versus open repair for pediatric inguinal hernia. BMC Surg. 2022;22:334. doi: 10.1186/s12893-022-01787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tanaka K, Miyaki Y, Abe K, Ueda-Abe E, Shibuya S, Takahashi T, Suzuki K. The outcome of closure of inguinal hernia with laparoscopic percutaneous extraperitoneal closure in young adults. World J Surg. 2024;48:371–376. doi: 10.1002/wjs.12022. [DOI] [PubMed] [Google Scholar]
- 42.Risteski T, Memeti S. Benefits of contralateral patent processus vaginalis closure during laparoscopic surgery for inguinal hernia in female children. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2022;43:69–75. doi: 10.2478/prilozi-2022-0020. [DOI] [PubMed] [Google Scholar]
- 43.Obayashi J, Wakisaka M, Tanaka K, Furuta S, Ohyama K, Kitagawa H. Risk factors influencing ascending testis after laparoscopic percutaneous extraperitoneal closure for pediatric inguinal hernia and hydrocele. Pediatr Surg Int. 2021;37:293–297. doi: 10.1007/s00383-020-04789-8. [DOI] [PubMed] [Google Scholar]