Abstract
Objective: To examine the association of proximal femoral nail anti-rotation (PFNA) and dynamic hip screw (DHS) with bone mineral density T-value (BMDT) in middle-aged and elderly patients suffering from hip fractures. Methods: Clinical data were collected from 110 patients with hip fractures who underwent internal fixation surgery between October 2020 and June 2021. Patients treated with DHS were included in the control group, and those treated with PFNA were classified into the observation group. The disparity in BMDT between the two groups was assessed. Patients were further divided into two groups based on the median BMDT at 6 months post-surgery: a high BMDT group (BMDT>-1.1 SD) and a low BMDT group (BMDT≤-1.1 SD). Factors influencing BMDT were analyzed. Results: Repeated measures ANOVA showed that BMDT in the observation group was higher than that in the control group at 7 days, 1 month, 3 months, and 6 months after the surgery (between-group effect: F=258.400, P<0.001). BMDT in both groups increased with time but remained lower than pre-surgery levels (time effect: F=28.760, P<0.001), with an interaction between group and time (F=6.478, P<0.05). Correlation analysis showed a significant correlation between internal fixation techniques and BMDT at 7 days, 1 month, 3 months, 6 months after the surgery (P<0.05). Logistic regression analysis showed that advanced age and a higher VAS score at 72 hours post-surgery were risk factors for low BMDT at 6 months post-surgery, while PFNA was a protective factor (all P<0.05). Conclusion: Compared to DHS, PFNA significantly improves BMDT in middle-aged and elderly patients following hip fracture surgery, promoting better early-stage recovery. PFNA should be prioritized in clinical practice to enhance postoperative outcomes.
Keywords: Middle-aged patients, hip fracture, internal fixation, bone mineral density T-value, correlation, elderly patients
Introduction
Bone mineral density (BMD), commonly expressed as a bone mineral density T-value (BMDT), is a key indicator of bone strength [1]. With increasing age, bone mass decreases, leading to decreased BMD and increased bone fragility, which heightens the risk of fractures, particularly brittle fractures. Hip fracture is the most serious type of brittle fracture, mostly occurring in middle-aged and elderly populations, with high disability and mortality rates [2]. Internal fixation is a surgical method widely used for treating fractures in clinical practice, which involves using external materials to stabilize the fracture ends and maintain anatomical alignment [3]. However, in middle-aged and elderly patients, the natural decline in BMD after fracture increases the risk of recurrent fractures after surgery [4].
Several internal fixation methods are currently available for fractures. According to related research, different internal fixation methods result in various postoperative rehabilitation effect [5]. In recent years, many studies have compared the efficacies of dynamic hip screws (DHS) and proximal femoral nail anti-rotation (PFNA) intramedullary nails for the treatment of hip fractures. Most of these studies have confirmed the effectiveness of PFNA. However, there remains a paucity of research regarding the impact of these treatment modalities on bone density in elderly patients with hip fractures, thereby limiting their applicability in clinical settings [6-8]. Therefore, this study aims to investigate the correlation between changes in BMDT and internal fixation methods in middle-aged and elderly patients with hip fractures, providing valuable insights for clinical decision-making.
Methods
Study design and patients
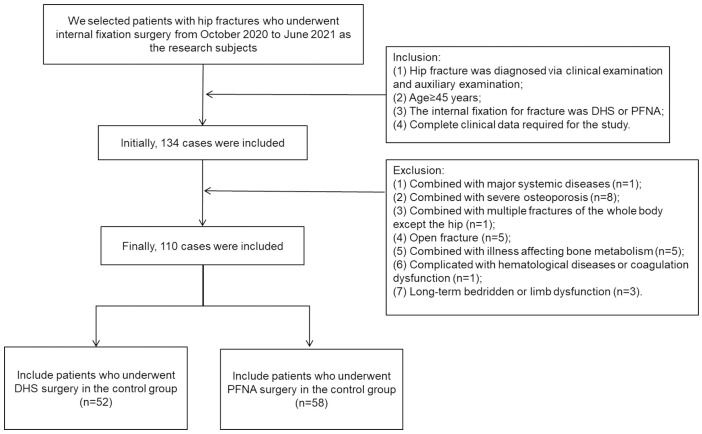
Clinical data from 110 patients with hip fractures who underwent internal fixation at the First Affiliated Hospital of Jinzhou Medical University between October 2020 and June 2021 were retrospectively analyzed. Surgical records and patient data were reviewed, and patients were categorized based on the specific internal fixation methods for fractures. Patients who underwent DHS surgery were included in the control group (n=52), while those who underwent PFNA surgery were assigned into the observation group (n=58). The filtering process is shown in Figure 1. This study was approved by the Ethics Committee of the First Affiliated Hospital of Jinzhou Medical University.
Figure 1.
Flowchart of patient screening. DHS: dynamic hip screw; PFNA: proximal femoral nail anti-rotation.
Inclusion criteria: (1) a diagnosis of hip fracture confirmed by clinical examination and auxiliary examination; (2) age ≥45 years; (3) treatment with either DHS or PFNA for internal fixation; (4) availability of complete clinical data required for the study. Exclusion criteria: (1) presence of major systemic diseases; (2) severe osteoporosis; (3) multiple fractures outside the hip; (4) open fracture; (5) illness affecting bone metabolisms, such as rheumatoid arthritis, thyroid disease, or infection; (6) hematological diseases or coagulation dysfunction; (7) long-term bedridden or limb dysfunction.
Surgical methods
Both groups were administered general or epidural block anesthesia. After successful anesthesia, patients were placed on an orthopedic traction bed. The healthy side of the lower limbs was fixed, while a pad was placed under the affected buttock to elevate it. The affected lower limb was positioned in a traction frame. The neutral position traction, internal rotation, and adduction recovery techniques were performed. Under C-arm fluoroscopy, the fracture was fixed once satisfactory reduction was achieved. If closed reduction was unsatisfactory, an open reduction was performed.
In the control group (DHS), an approximately 12-18 cm long incision was made from the greater trochanter apex of the femur. The greater trochanter and upper part of the femur were fully exposed. After satisfactory fracture reduction under direct vision, a neck-shaft angle guide was used for positioning. A guide pin was drilled into the middle and lower 1/3 of the femoral neck. After confirmation of the position of the guide pin and length of the screw with the assistance of C-arm machine (PLX118C, Puai Medical Equipment Co., Ltd., China), the hole was enlarged. Then, DHS screws of appropriate length were inserted and secured with a sleeve plate. In the observation group (PFNA), a 3-cm incision was made 2 cm above the femoral trochanter. The insertion point was located at the apex of the femoral trochanter or slightly laterally. A guide pin was inserted into the medullary cavity, and once its position was confirmed under C-arm fluoroscopy, reaming was performed. An anti-rotation intramedullary nail was inserted in the main canal. Under visual guidance, a protective sleeve and a special guide pin were inserted. Using C-arm fluoroscopy, an appropriate spiral blade was selected, locked, and the distal locking screw was screwed in. Finally, the internal fracture fixation were completed in both groups, and the incision was irrigated and closed layer by layer. Routine postoperative nursing and rehabilitation training were provided to both groups.
Data collection
Clinical data were collected from the hospital’s electronic information system. General information included age, gender, body mass index (BMI), underlying diseases, fracture type, and the injured side. Perioperative and follow-up data included the visual analogue scale (VAS) score at 72 h post-surgery, postoperative drainage volume, time to non-weight-bearing ambulation, hospital stay duration, fracture healing time, complications, and hip bone BMDT.
Fracture healing criteria [9]: Patients underwent routine postoperative outpatient review once a month. Successful healing was indicated by the absence of significant discomfort or tenderness in the hip during full weight-bearing activity. Radiographs showing obvious trabecular bone growth at the fracture end and a blurred fracture line were also considered indicative of healing.
Hip BMD was measured using a bone densitometer (Lunar Prodigy, General Electric Company, USA). The contralateral hip bone was chosen as the measurement site. The patients were positioned supine during the measurement with the affected site in its natural position and the healthy side internally rotated 15°. The normal reference range for BMDT was -1 SD to 1 SD. A BMDT of -1 SD to -2.5 SD indicated a decrease in bone mass. BMDT≤-2.5 SD was diagnosed as osteoporosis [10].
Outcome measures and statistical analysis
The primary outcome measures included comparing the differences and trends in BMDT before and after surgery within both groups at 7 days, 1 month, 3 months, and 6 months. Additionally, the correlation between postoperative BMDT and the two fracture internal fixation procedures was analyzed. The secondary outcome measures encompassed comparing clinical data between the two groups and identifying the factors influencing postoperative BMDT at 6 months.
SPSS version 26.0 (IBM, USA) was used for data processing. Measurement data with a normal distribution were presented as mean ± standard deviation (x̅ ± sd). Paired sample t-tests and independent sample t-tests were performed for within-group and between-group comparisons, respectively. Enumeration data were expressed as n (%). Chi-squared tests were used for between-group comparisons. A repeated measures ANOVA was employed to compare the BMDT of the two groups at various postoperative time points. Spearman’s correlation coefficient was utilized for correlation analysis, and a binary Logistic regression model was applied to identify the influencing factors. A P value of less than 0.05 was considered statistically significant.
Results
General data
A total of 110 patients were included in this study, with 52 in the control group and 58 in the observation group. No significant differences were observed in the general data between the groups (all P>0.05) (Table 1).
Table 1.
Comparison of general data between the two groups
| General data | Control group (n=52) | Observation group (n=58) | t/χ2 | P |
|---|---|---|---|---|
| Age (years, x̅±sd) | 66.25±5.70 | 67.19±6.32 | 0.815 | 0.417 |
| Sex (n (%)) | 0.116 | 0.733 | ||
| Male | 27 (51.92) | 32 (55.17) | ||
| Female | 25 (48.08) | 26 (44.83) | ||
| BMI (kg/m2, x̅±sd) | 21.49±2.36 | 21.61±2.48 | 0.255 | 0.799 |
| Fracture type (n (%)) | 1.122 | 0.571 | ||
| Intertrochanteric fracture | 25 (48.08) | 29 (50.00) | ||
| Femoral subtrochanteric fracture | 16 (30.77) | 21 (36.21) | ||
| Femoral neck fracture | 11 (21.15) | 8 (13.79) | ||
| Injured side (n (%)) | 0.091 | 0.763 | ||
| Left | 29 (55.77) | 34 (58.62) | ||
| Right | 23 (44.23) | 24 (41.38) | ||
| Combined underlying diseases (n (%)) | 1.214 | 0.545 | ||
| Hypertension | 31 (59.62) | 27 (46.55) | ||
| Diabetes | 18 (34.62) | 23 (39.66) | ||
| CHD | 14 (26.92) | 11 (18.97) |
BMI: body mass index; CHD: coronary heart disease.
Perioperative-related data
No significant differences were observed between the groups in the VAS score at 72 h post-surgery, postoperative drainage volume, time to non-weight-bearing ambulation, hospitalization duration, fracture healing time, and postoperative complication rate (all P>0.05) (Table 2).
Table 2.
Comparison of surgical-related indexes between the two groups
| Index | Control group (n=52) | Observation group (n=58) | t/χ2 | P |
|---|---|---|---|---|
| VAS score at 72 h after the surgery (score, x̅±sd) | 3.69±1.02 | 3.83±0.88 | 0.764 | 0.457 |
| Postoperative drainage volume (mL, x̅±sd) | 71.37±4.62 | 73.47±6.39 | 0.069 | 0.053 |
| Time to non-weight-bearing ambulation (day, x̅±sd) | 15.23±4.49 | 14.79±4.25 | 0.525 | 0.601 |
| Hospitalization time (day, x̅±sd) | 17.67±3.15 | 16.76±2.56 | 1.675 | 0.097 |
| Fracture healing time (week, x̅±sd) | 14.21±2.10 | 14.69±2.05 | 1.206 | 0.230 |
| Postoperative morbidity (n (%)) | 3 (5.76) | 7 (12.07) | 0.665 | 0.415 |
VAS: visual analog scale.
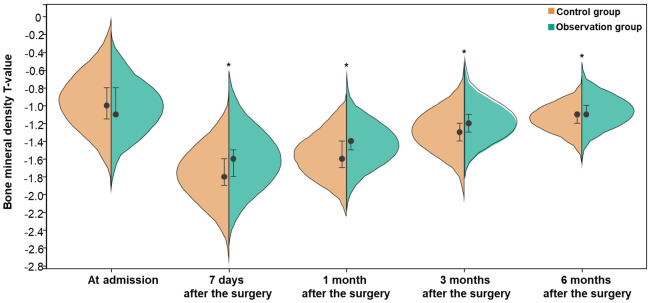
BMDT at different time points
No statistical difference was observed in BMDT between both groups before surgery. BMDT values in the observation group were significantly higher than those in the control group at 7 days, 1 month, 3 months, and 6 months after the surgery (between-group effect: F=258.400, P<0.001). BMDT in both groups increased with time but were lower than those at admission (time effect: F=28.760, P<0.001). Additionally, a significant interaction was observed between group and time (F=6.478, P<0.05) (Figure 2).
Figure 2.
Comparison of bone mineral density T values between the two groups at different time points. Compared with control group, *P<0.05.
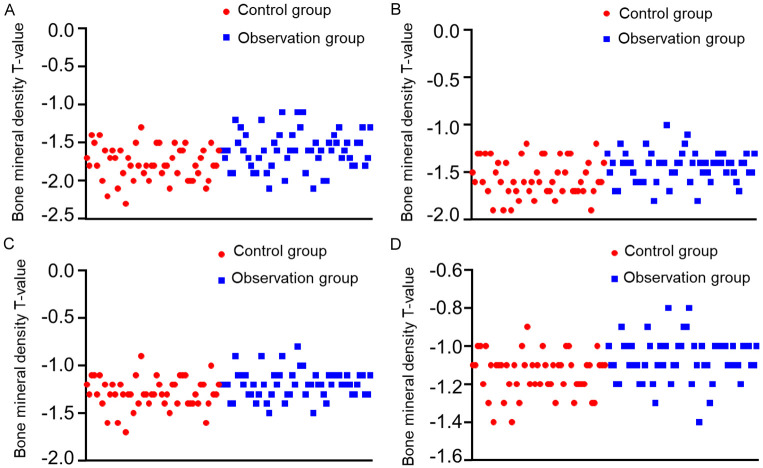
Correlation between internal fixation techniques and BMDT
There was a correlation between the type of internal fixation techniques and BMDT at 7 days, 1 month, 3 months, and 6 months after the surgery (P<0.05) (Table 3). The relationship between BMDT at different postoperative time points and the two types of internal fixations is shown in Figure 3.
Table 3.
Correlation between internal fixation techniques and BMDT
| Internal fixation techniques for fractures | ||
|---|---|---|
|
| ||
| r | P | |
| 7 days after the surgery | 0.504 | 0.001 |
| 1 month after the surgery | 0.492 | 0.002 |
| 3 months after the surgery | 0.383 | 0.003 |
| 6 months after the surgery | 0.533 | <0.001 |
BMDT: bone mineral density T-value.
Figure 3.
The relationship between BMDT and internal fixation techniques for fractures. A: BMDT at day 7 post-surgery; B: BMDT at post-surgery 1 month; C: BMDT at post-surgery 3 months; D: BMDT at post-surgery 6 months. BMDT: bone mineral density T-value.
Differences in clinical data based on different BMDT
Patients were divided into two groups based on the median BMDT at 6 months post-surgery: a high BMDT group (BMDT>-1.1 SD) and a low BMDT group (BMDT≤-1.1 SD). There were significant differences in age, VAS score at 72 hours post-surgery, and internal fixation techniques between the two groups (all P<0.05) (Table 4).
Table 4.
Comparison of clinical data between low and high BMDT groups
| Data | Low BMDT group (n=74) | High BMDT group (n=36) | t/χ2 | P |
|---|---|---|---|---|
| Age (years, x̅±sd) | 68.58±5.65 | 62.97±4.99 | 5.073 | <0.001 |
| Sex (n (%)) | 0.016 | 0.900 | ||
| Male | 40 (54.05) | 19 (52.78) | ||
| Female | 34 (45.95) | 17 (47.22) | ||
| BMI (kg/m2, x̅±sd) | 21.46±2.15 | 21.74±2.91 | 0.510 | 0.612 |
| Fracture type (n (%)) | 2.129 | 0.345 | ||
| Intertrochanteric fracture | 33 (44.59) | 21 (58.33) | ||
| Femoral subtrochanteric fracture | 28 (37.84) | 9 (25.00) | ||
| Femoral neck fracture | 13 (17.57) | 6 (16.67) | ||
| Injured side (n (%)) | 0.064 | 0.800 | ||
| Left | 43 (58.11) | 20 (55.56) | ||
| Right | 31 (41.89) | 16 (44.44) | ||
| Combined underlying diseases (n (%)) | ||||
| Hypertension | 40 (54.05) | 18 (50.00) | 0.160 | 0.689 |
| Diabetes | 30 (40.54) | 11 (30.56) | 1.033 | 0.310 |
| CHD | 18 (24.32) | 7 (19.44) | 0.328 | 0.567 |
| VAS score at 72 hours post-surgery (score, x̅±sd) | 3.89±0.92 | 3.50±0.97 | 2.066 | 0.041 |
| Postoperative drainage volume (mL, x̅±sd) | 72.99±5.51 | 71.42±6.01 | 1.361 | 0.176 |
| Time to non-weight-bearing ambulation (day, x̅±sd) | 15.07±4.38 | 14.86±4.34 | 0.233 | 0.817 |
| Hospitalization time (day, x̅±sd) | 17.50±2.70 | 16.56±3.17 | 1.625 | 0.107 |
| Fracture healing time (week, x̅±sd) | 14.34±2.02 | 14.72±2.20 | 0.909 | 0.365 |
| Postoperative morbidity (n (%)) | 8 (10.81) | 2 (5.56) | 0.298 | 0.368 |
| Internal fixation techniques (n (%)) | 10.650 | 0.001 | ||
| DHS | 43 (58.11) | 9 (25.00) | ||
| PFNA | 31 (41.89) | 27 (75.00) |
BMI: body mass index; CHD: coronary heart disease; VAS: visual analog scale; DHS: dynamic hip screw; PFNA: proximal femoral nail anti-rotation; BMDT: bone mineral density T-value.
Analysis of factors affecting BMDT
In the logistic regression analysis, low BMDT at 6 months post-surgery was the dependent variable, while the independent variables included age, VAS score at 72 hours post-surgery, and the type of internal fixation techniques. The results of Logistic regression showed that advanced age and a higher VAS score at 72 hours post-surgery were risk factors for low BMDT at 6 months post-surgery, while PFNA was a protective factor (all P<0.05) (Table 5).
Table 5.
Analysis of factors affecting low BMDT
| Variable | B | SE | Wald | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| Age | 0.225 | 0.052 | 18.892 | <0.001 | 1.253 | 1.132-1.387 |
| VAS score at 72 hours post-surgery | 0.595 | 0.295 | 4.062 | 0.044 | 1.814 | 1.016-3.235 |
| PFNA | -2.278 | 0.601 | 14.376 | <0.001 | 0.103 | 0.032-0.333 |
VAS: visual analog scale; PFNA: proximal femoral nail anti-rotation; BMDT: bone mineral density T-value.
Discussion
The incidence of hip fragility fractures is progressively increasing each year as the aging population grows, rendering them one of the most severe types of fractures [11]. The reported one-year mortality rate following hip fracture ranges from 22% to 29% [12]. Early surgical intervention may mitigate the occurrence of complications. Middle-aged and elderly patients with hip fractures often experience decreased bone mass, which hinders postoperative fracture healing [13]. For these patients, appropriate internal fixation should be tailored based on individual characteristics. Therefore, it is imperative to analyze BMD changes after internal fixation with different techniques and promptly intervene to enhance post-surgery quality of life.
Currently, the internal fixation methods utilized in clinical settings can be classified as extramedullary or intramedullary fixations. Dynamic hip screw (DHS) represents a prevalent extramedullary fixation technique, primarily employing the DHS device to stabilize the proximal end of the fracture through dynamic screw insertion into the femoral neck. The distal end of the fracture is stabilized with a plate, secured by compressing the neck shaft angle and applying a tension band [14,15]. Sliding compression can enhance dynamic stabilization of the fracture ends, facilitating rapid callus formation and expediting fracture healing [16]. Proximal femoral nail anti-rotation (PFNA) is a novel generation of intramedullary fixation systems that predominantly employs a minimally invasive approach with small incisions for implanting the main nail, subsequently securing it with a spiral blade at its distal end. Postoperatively, the upper femur and femoral neck integrate, and distal locking prevents rotation and shortening, ensuring stable fixation and promoting fracture healing [17,18].
In the current investigation, no statistical difference was observed between DHS and PFNA in terms of VAS score, postoperative drainage volume, time to non-weight-bearing activity, hospitalization time, fracture healing time, and postoperative complication rate. This contrasts with the findings of Zeng et al. [19], which may be attributed to variations in inclusion and exclusion criteria as well as fracture types. Zhu et al. conducted an analysis on 92 cases of intertrochanteric fractures in elderly patients and determined that PFNA and DHS exhibited similar therapeutic effects. However, PFNA demonstrated a shorter operation time, reduced intraoperative blood loss, fewer postoperative complications, and faster patient recovery. A meta-analysis [20] evaluating surgical and postoperative outcomes for middle-aged and elderly patients concluded that PFNA required less operative time and resulted in lower perioperative bleeding compared to DHS, although DHS had the advantage of shorter intraoperative fluoroscopy time. No significant difference was noted in the incidence of postoperative nephropathy. Furthermore, this study results revealed higher BMDT at the hip fracture site in the observation group compared to those in the control group at 7 days, 1 month, 3 months, and 6 months after surgery. These findings suggest that PFNA can effectively improve the BMD at the fracture site. Several factors may account for these observations: (1) While DHS yields favorable clinical outcomes, it does not effectively prevent rotational displacement of fractures. PFNA employs spiral blade-locking technology which aligns more closely with proximal femur anatomy, resulting in effective anti-rotational properties, maintaining stable fracture ends, and facilitating repair and healing of the fractured region [21-23]. (2) The DHS employs traditional drilling and reaming techniques for the implantation of fixation devices, which inevitably leads to the loss of bone tissue within the drill hole. In contrast, the spiral blade of the PFNA directly penetrates the bone, exerting compressive forces that facilitate the formation of a quadrangular intramedullary canal, thereby exhibiting enhanced resistance to cutting [24-26]. (3) The longer fixation arm and thicker main nail of DHS increase bending moment, which can impact blood supply. In contrast, PFNA has a shorter arm, causing less surgical trauma and minimizing damage to the local blood supply [27-29]. (4) PFNA’s hollow design and 5° external deflection angle at the proximal end allow for precise positioning and closed reduction, which reduces trauma to the affected area [30,31]. However, PFNA has certain limitations. For example, the main nail is cylindrical with a large proximal diameter, which may increase the extent of fracture damage [32,33]. The presence of a proximal spiral blade adds surgical complexity, and repeated strikes could result in femoral head and neck fractures as well as inadequate anchoring force [34,35]. Attention should be given to the depth of the main nail implantation, position of the proximal spiral blade, and selection of implanted fixation in the PFNA. Strict adherence to operational norms was maintained to ensure treatment safety.
Correlation analysis revealed a significant association between internal fixation techniques and BMDT at 7 days, 1 month, 3 months, and 6 months post-surgery. Logistic regression analysis indicated that advanced age and a higher VAS score at 72 hours post-surgery were risk factors for low BMDT at 6 months after the surgery, while PFNA was found to be a protective factor. Based on these findings, it is recommended to prioritize internal fixation techniques such as proximal femoral anti-rotation intramedullary nails whenever feasible. Prior to surgery, a comprehensive assessment of the patient’s fracture classification, physical condition, and surgical tolerance should be conducted to ensure the selection of a scientifically sound and rational surgical approach. Close monitoring of the patient’s postoperative pain within 72 hours is essential, with proactive pain management strategies including pain pumps or oral/injectable analgesics. Additionally, an individualized rehabilitation plan tailored to the patient’s age, fracture type, surgical technique employed, and postoperative recovery progress should be formulated. Adjustments in rehabilitation intensity and pace are warranted for elderly patients or those with heightened pain sensitivity.
The study’s limitations, such as the small sample size and retrospective nature, may have affected the generalizability of the findings. Furthermore, the absence of further sub-control analysis for fracture types could have introduced bias into the results. It is essential to recognize that these constraints may have influenced the overall conclusions drawn from this research. Larger sample sizes and multicenter studies are necessary to validate our findings.
Conclusions
Compared to DHS, PFNA significantly enhances BMDT in middle-aged and elderly patients recovering from hip fracture surgery in the early stages. This improvement facilitates postoperative recovery and should be prioritized in clinical practice.
Disclosure of conflict of interest
None.
References
- 1.Ehsanbakhsh A, Azarkar G, Ziaee M, Taghavieh A. Prevalence of bone density reduction and its related factors in hemophilia patients in South Khorasan Province in 2018. Galen Med J. 2020;9:e1711. doi: 10.31661/gmj.v9i0.1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu X, Wang L, Gao M, Wang G, Tang K, Yang J, Song W, Yang J, Lyu L, Cheng X. Comparison of muscle density in middle-aged and older chinese adults between a high-altitude area (Kunming) and a low-altitude area (Beijing) Front Endocrinol (Lausanne) 2021;12:811770. doi: 10.3389/fendo.2021.811770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang LZ, Gao J, Zhang ZC, Wang XW, Zhang JZ, Sun TS. Comparison of clinical effects of total artificial hip replacement and cannulated screw fixation for the treatment of displaced femoral neck fractures in elderly patients. Zhongguo Gu Shang. 2018;31:103–110. doi: 10.3969/j.issn.1003-0034.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Peng YL, Wang ZY, Wang XJ, Ji YT, Wen Y, Mai Y. Lower risk of low bone mineral density in high vitamin E level in older people: a cross-sectional study. Clin Nutr ESPEN. 2024;61:316–321. doi: 10.1016/j.clnesp.2024.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Yu C, Jiang LH, Cai DW, Wu J, Qin J. PFNA and InterTAN intramedullary nailing in elderly patients with femoral intertrochanteric fractures: a Meta analysis. Zhongguo Gu Shang. 2019;32:120–129. doi: 10.3969/j.issn.1003-0034.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Lu JF. Comparison of PFNA and DHS for the treatment of elderly unstable intertrochanteric fractures of femur. Zhongguo Gu Shang. 2019;32:824–829. doi: 10.3969/j.issn.1003-0034.2019.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Wang W, Zhai S, Han XP, Cui Y. Comparative study of proximal femoral nail anti-rotation and dynamic hip screw in the unstable intertrochanteric fractures in the elderly. Zhonghua Yi Xue Za Zhi. 2018;98:357–361. doi: 10.3760/cma.j.issn.0376-2491.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 8.Ouyang X, Ding Y, Yu L, Xin F, Yang X, Sha P, Tong S, Cheng Q, Xu Y. Comparison of the clinical effect of DHS and PFNA on senile osteoporotic fracture and their significance of changes in BALP expression level. J Musculoskelet Neuronal Interact. 2020;20:556–562. [PMC free article] [PubMed] [Google Scholar]
- 9.Garg S, Tank G. Role of biplane double-supported screw fixation (BDSF) in management of fracture neck femur and its comparison with conventional CC screw fixation. Indian J Orthop. 2023;57:2011–2017. doi: 10.1007/s43465-023-01006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang FX, Fan DH, Huang G, He JH. Lumbar spine bone mineral density measurement: comparison of dual-energy X-ray absorptiometry and fat content evaluation by dixon chemical shift MRI. Int J Gen Med. 2022;15:6415–6424. doi: 10.2147/IJGM.S370814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jawad MJ. Evaluation of using PFN (proximal femoral nailing) in treatment of unstable intertrochanteric fractures in elderly patients. J Pak Med Assoc. 2021;71(Suppl 8):S179–S184. [PubMed] [Google Scholar]
- 12.Lunde A, Tell GS, Pedersen AB, Scheike TH, Apalset EM, Ehrenstein V, Sørensen HT. The role of comorbidity in mortality after hip fracture: a nationwide norwegian study of 38,126 women with hip fracture matched to a general-population comparison cohort. Am J Epidemiol. 2019;188:398–407. doi: 10.1093/aje/kwy251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zaib J, Madni A, Saad Azhar M. Predictive value of comprehensive geriatric assessment scores for mortality in patients with hip fracture: a retrospective cohort study. Cureus. 2023;15:e45070. doi: 10.7759/cureus.45070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ma JX, Kuang MJ, Xing F, Zhao YL, Chen HT, Zhang LK, Fan ZR, Han C, Ma XL. Sliding hip screw versus cannulated cancellous screws for fixation of femoral neck fracture in adults: a systematic review. Int J Surg. 2018;52:89–97. doi: 10.1016/j.ijsu.2018.01.050. [DOI] [PubMed] [Google Scholar]
- 15.Voeten S, Deunk J, Vermeulen J, De Lange-De Klerk E, van den Brand H, Zuidema W. The addition of an anti-rotation screw to the dynamic hip screw. Acta Orthop Belg. 2020;86:233–238. [PubMed] [Google Scholar]
- 16.Ceynowa M, Zerdzicki K, Klosowski P, Pankowski R, Rocławski M, Mazurek T. The early failure of the gamma nail and the dynamic hip screw in femurs with a wide medullary canal. A biomechanical study of intertrochanteric fractures. Clin Biomech (Bristol, Avon) 2020;71:201–207. doi: 10.1016/j.clinbiomech.2019.11.006. [DOI] [PubMed] [Google Scholar]
- 17.Wang F, Zou JL, Shang J. Does matching degree matter for proximal femoral intramedullary nail on reoperation rate in intertrochanteric fractures? J Orthop Surg Res. 2022;17:573. doi: 10.1186/s13018-022-03476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mao W, Yang AL, Chang SM, Li Y, Li LL, Ni HF, Dong YH. The impact of banana-shaped fragments on trochanteric hip fractures treated by PFNA. Indian J Orthop. 2023;57:1452–1460. doi: 10.1007/s43465-023-00964-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zeng X, Zhan K, Zhang L, Zeng D, Yu W, Zhang X, Zhao M. Conversion to total hip arthroplasty after failed proximal femoral nail antirotations or dynamic hip screw fixations for stable intertrochanteric femur fractures: a retrospective study with a minimum follow-up of 3 years. BMC Musculoskelet Disord. 2017;18:38. doi: 10.1186/s12891-017-1415-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu H, Liu Y, Sezgin EA, Tarasevičius Š, Christensen R, Raina DB, Tägil M, Lidgren L. Comparative effectiveness research on proximal femoral nail versus dynamic hip screw in patients with trochanteric fractures: a systematic review and meta-analysis of randomized trials. J Orthop Surg Res. 2022;17:292. doi: 10.1186/s13018-022-03189-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Noh JH, Koh SJ, Lee KH. Treatment of proximal femur osteomyelitis occurred after proximal femoral nail antirotation fixation, with antibiotic cement-coated tibia intramedullary nail: a case report. Hip Pelvis. 2018;30:45–52. doi: 10.5371/hp.2018.30.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang L, Wang C, Zhang D, Wang W, Wang F. Effectiveness and safeties of hemocoagulase and tranexamic acid to reduce perioperative blood loss in intertrochanteric fracture PFNA fixation. Acta Orthop Belg. 2023;89:645–650. doi: 10.52628/89.4.11959. [DOI] [PubMed] [Google Scholar]
- 23.Lv J, Li X, Qiu W, Ji J, Cao L, Li L, Zhang Y, Su Z. Effect of knee osteoarthritis on the postoperative outcome of proximal femoral nail anti-rotation in the treatment of intertrochanteric fractures in the elderly: a retrospective analysis. BMC Musculoskelet Disord. 2023;24:868. doi: 10.1186/s12891-023-07012-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gong H, Wang L, Zheng D, Fan Y. The potential application of functionally graded material for proximal femoral nail antirotation device. Med Hypotheses. 2012;79:415–7. doi: 10.1016/j.mehy.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 25.Law GW, Wong YR, Gardner A, Ng YH. Intramedullary nailing confers an increased risk of medial migration compared to dynamic hip screw fixation in unstable intertrochanteric hip fractures. Injury. 2021;52:3440–3445. doi: 10.1016/j.injury.2021.01.011. [DOI] [PubMed] [Google Scholar]
- 26.Tang Y, Wang D, Wang L, Xiong W, Fang Q, Lin W, Wang G. The PFNA in treatment of intertrochanteric fractures with or without lateral wall fracture in elderly patients: a retrospective cohort study. Eur J Med Res. 2023;28:380. doi: 10.1186/s40001-023-01332-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tian Z, Chen J, Zhang Y, Shi L, Li W. A retrospective study of 98 elderly patients with high-risk lateral femoral wall intertrochanteric hip fractures to compare outcomes following surgery with proximal femoral nail antirotation (PFNA) versus dynamic hip screw (DHS) Med Sci Monit. 2022;28:e936923. doi: 10.12659/MSM.936923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sivro M, Lazović F, Omerović Ð, Papović A. The effects of two fixation methods on blood loss in patients with trochanteric fracture: dynamic hip screw vs. proximal femoral nail anti-rotation. Med Glas (Zenica) 2023;20:249–254. doi: 10.17392/1616-23. [DOI] [PubMed] [Google Scholar]
- 29.Guan GP, Wang X, Wang C, Jia XL, Yin J, Liu XH, Yang YL, Liu W. Comparison of PFNA and DHS in the treatment of sarcopenia with Seinsheimer type V subtrochanteric fracture. Eur Rev Med Pharmacol Sci. 2023;27:4442–4449. doi: 10.26355/eurrev_202305_32450. [DOI] [PubMed] [Google Scholar]
- 30.Cui H, Wei W, Shao Y, Du K. Finite element analysis of fixation effect for femoral neck fracture under different fixation configurations. Comput Methods Biomech Biomed Engin. 2022;25:132–139. doi: 10.1080/10255842.2021.1935899. [DOI] [PubMed] [Google Scholar]
- 31.Wang W, Ni B, Shen H, Lu H. Meta-analysis of InterTan, PFNA and PFNA-II internal fixation for the treatment of unstable intertrochanteric fractures in elderly individuals. Acta Orthop Belg. 2023;89:51–58. doi: 10.52628/89.1.9923. [DOI] [PubMed] [Google Scholar]
- 32.van der Sijp MPL, de Groot M, Meylaerts SA, du Pré KJ, Verhage SM, Schipper IB, Niggebrugge AHP. High risks of failure observed for A1 trochanteric femoral fractures treated with a DHS compared to the PFNA in a prospective observational cohort study. Arch Orthop Trauma Surg. 2022;142:1459–1467. doi: 10.1007/s00402-021-03824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheng YX, Sheng X. Optimal surgical methods to treat intertrochanteric fracture: a Bayesian network meta-analysis based on 36 randomized controlled trials. J Orthop Surg Res. 2020;15:402. doi: 10.1186/s13018-020-01943-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen P, Fu D. Failure analysis of proximal femoral nail antirotation in treatment of geriatric intertrochanteric fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33:1270–1274. doi: 10.7507/1002-1892.201905071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen P, Fan Z, Xu N, Wang H. A biomechanical investigation of a novel intramedullary nail used to salvage failed internal fixations in intertrochanteric fractures. J Orthop Surg Res. 2023;18:632. doi: 10.1186/s13018-023-04112-w. [DOI] [PMC free article] [PubMed] [Google Scholar]