Abstract
Objective: Intertrochanteric femur fractures are prevalent among the elderly, leading to substantial morbidity. Proximal femoral nail anti-rotation (PFNA) is commonly used for internal fixation, but excessive lateral migration of the PFNA blade poses a significant complication. Understanding the risk factors for this complication is crucial for optimizing patient care. Methods: A retrospective case-control study was conducted on elderly patients with intertrochanteric femur fractures who underwent PFNA internal fixation. Patients were categorized based on the occurrence of excessive lateral migration of the blade. The differences in general information, surgical indices, imaging measures, fracture stability indicators, VAS score, Harris score, and other factors were analyzed. Single factor correlation analysis and multivariate logistic regression were utilized to identify risk factors associated with excessive blade lateral migration. Results: Risk factors significantly associated with excessive blade lateral migration included the Singh index for osteoporosis, quality of calcar reduction, surgical indices (hospital stays, revision surgery for blade prominence), imaging measures (blade position, lateralization, and migration), fracture stability indicators (tip-apex distance, AO/OTA classification), and postoperative functional outcomes (VAS and Harris scores). Multivariate logistic regression identified these factors as independent predictors of excessive lateral migration, underlining the multifactorial nature of this complication. Conclusion: This study identified several significant risk factors for excessive lateral migration of the PFNA blade, including bone quality, calcar reduction, surgical indices, imaging measures, and fracture stability indicators.
Keywords: Blade excessive lateral migration, proximal femoral nail anti-rotation, intertrochanteric femur fracture, elderly patients, risk factors
Introduction
Intertrochanteric femur fractures are a prevalent and serious clinical issue, particularly affecting the elderly [1,2]. These fractures occur between the greater and lesser trochanters of the proximal femur and are often associated with low-energy trauma, such as falls from standing, due to the osteoporotic nature of bones in this population [2]. The underlying cause involves a combination of osteoporosis-induced bone weakening and the mechanical forces exerted on the hip during a fall, culminating in a disruption of bone integrity [3].
Clinically, intertrochanteric fractures manifest as pain, an inability to bear weight, and noticeable deformity in the affected hip, with the limb typically shortened and externally rotated [4]. Diagnosis is primarily based on clinical assessment followed by radiographic confirmation using X-rays [5]. These fractures are classified through systems like the Evans and the AO/OTA classification, which help guide the development of treatment strategy [6]. Increasing with age, the incidence of these fractures highlights a growing concern with the aging global population, particularly in women aged 65 and older [7]. These fractures are associated with substantial mortality risks - around 20-30% within the first year post-fracture - often due to complications including thrombosis, pneumonia, and reduced mobility [8].
Surgical intervention is the cornerstone of treatment for intertrochanteric fractures, as it aims to stabilize the fracture, facilitate early mobilization, and minimize risks linked to extended immobility [8]. The Proximal Femoral Nail Anti-Rotation (PFNA) has gained wide acceptance for its minimally invasive nature and biomechanical advantages, allowing for early weight-bearing [9]. This procedure entails closed fracture reduction under fluoroscopy and the subsequent insertion of an intramedullary nail with a helical blade into the femur, reducing surgical time and blood loss, and enhancing outcomes in terms of fracture union and functional recovery [10,11]. Nonetheless, complications like blade migration and fixation failure have been noted, prompting efforts to identify and mitigate risk factors through ongoing research and improvements in surgical techniques and implant designs [12]. Thus, this study focused on understanding patient-related factors, enhancing preoperative assessment that contribute to tailored surgical plans to improve patient outcome and reduce complications.
Materials and methods
Study design
This is a retrospective case-control study conducted between April 2021 and February 2023. This study was approved by the Institutional Review Board and Ethics Committee of Shengli Oilfield Central Hospital. Informed consent was waived by the Institutional Review Board and Ethics Committee for this retrospective study due to the exclusive use of de-identified patient data, which poses no potential harm or impact on patient care.
Inclusion criteria [13,14]: patients aged 60 or above; those with radiologically confirmed acute, closed, unilateral intertrochanteric fractures due to trauma and treated with internal fixation surgery; those who had normal mental and cognitive function; those with complete clinical data; those who completed a 4-month follow-up.
Exclusion criteria: patients with multiple fractures, fractures associated with severe visceral injuries, a history of trauma or surgery in the affected limb, a history of hip joint dysfunction such as osteoarthritis or avascular necrosis of the femoral head, pathologic fracture, cognitive impairment, or coagulation disorders.
This study included 200 patients who were admitted to Shengli Oilfield Central Hospital with intertrochanteric femur fractures and underwent PFNA internal fixation. The patients were categorized into two groups based on the occurrence of excessive lateral migration of the helical blade.
Surgical procedure
All the patients underwent PFNA internal fixation [15]. First, the surgical site was disinfected, and the patient was positioned on an orthopedic traction bed. Fracture manipulation was then guided using a C-arm X-ray fluoroscopy machine, with continuous monitoring to ensure the patient remained relaxed. Closed reduction and traction achieved 20°-30° of femoral varus. After confirming satisfactory reduction, a 5 cm vertical incision was made along the lateral aspect of the greater trochanter. The skin and fascia lata were incised to expose the apex of the greater trochanter [15].
A guide pin was inserted at the junction of the anterior 1/3 and posterior 2/3 of the greater trochanter, extending into the intramedullary cavity, and its position was verified by fluoroscopy. The intramedullary cavity was then reamed, and the appropriate nail was inserted. A protective sleeve for the helical blade was placed, with its tip inserted into the lateral cortex of the femur. Drilling proceeded until the drill tip was 0.5 cm below the joint surface. The helical blade was inserted into the femoral head and rotated clockwise, followed by the insertion of distal locking screws. The intramedullary nail cap was secured, and reduction and fixation were confirmed by C-arm X-ray fluoroscopy. The wound was closed in layers, and nail length and diameter were recorded [16].
Lateralization measures
To determine the average amount of lateralization of a helical blade during the treatment, we measured the distance along the fixed angle of the blade lateral to the cortex (standardized for magnification) at the final follow-up [13]. The amount of lateral migration of the blade was measured by comparing the immediate postoperative radiographs with the most recent radiograph. It was calculated as the change in relative length of the unengaged part of the blade [17]. Excessive lateral migration is defined as a displacement distance of the helical blade exceeding 1 cm [16].
General information
Patient general information was obtained through systematic retrieval of medical records, including age, gender, BMI, duration of disease, smoking history, drinking history, hypertension, diabetes, hyperlipidemia, education level, social support, cause of injury, history of fracture, ASA grade, Singh index-osteoporosis, intraoperative blood loss, operation time, revision surgery, revision surgery for blade prominence, and hospital stays.
Imaging examination
The immediate postoperative radiographs were used to assess reduction accuracy and hardware position. The quality of calcar reduction was graded as good or poor to detect the amount of residual displacement between the neck and shaft [18]. A good reduction had normal or slightly valgus neck-shaft alignment on the anteroposterior (AP) radiograph, less than 20 degrees of angulation on the lateral radiograph, and translation of less than 4 mm on either view [12]. Otherwise, the reduction was graded as poor. The position of lesser trochanter was evaluated and defined as displaced or nondisplaced. The blade position within the femoral head was evaluated using the tip-apex distance (TAD) method.
All radiographs were reviewed by a chief orthopedic resident or a board-certified orthopedic trauma surgeon. The fracture pattern was classified according to the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association (AO/OTA) classification using the preoperative radiographs [10,14]. Fractures were further classified as stable or unstable [19].
Visual analog scale (VAS)
The patients’ pain levels were assessed preoperatively and at 1 week and 1 month postoperatively. The VAS was evaluated using a 10 cm long scale, with 10 graduations, ranging from “0” representing no pain to “10” indicating the most severe and intolerable pain. The Cronbach’s alpha was 0.94 [20].
Harris score
The Harris hip score was used to assess the results of hip surgery and provide a numerical rating of hip function (score range, 0-100 points, with 0-69 indicating poor function, 70-79 indicating fair function, 80-89 indicating good function, and 90-100 indicating excellent function). Cronbach’s alpha was 0.792 for the total score [21].
Statistical analysis
Using G*Power 3.1.9.7 [10,14], the “Means: Difference between two independent means (two groups)” option based on t-tests was selected for post hoc analysis. The settings included the selection of a two-tailed mode, an effect size of d=0.5, and an α error probability of 0.05. Subsequently, the sample sizes of the two groups were entered, and the power (1-β error probability) was calculated, resulting in a power of 0.852.
To compare the characteristics of patients between the two groups, an independent t test was performed for continuous variables, and the χ2 test was performed for categorical variables. Data were represented as means with standard deviations (SD) for continuous variables and as numbers and percentages for categorical variables. The characteristics of patients were taken as possible confounding factors for assessing post-operative clinical outcome. P<0.05 was considered as significant. The correlation analysis was examined using Spearman correlation analysis for categorical variables. All analyses were performed using SPSS 29.0 software (SPSS Inc., Chicago, IL, USA). Logistic regression was performed with all significant variables from the bivariate analysis to determine which variables were independently predictive of excessive lateral migration of the PFNA blade.
Results
General information
The mean age of patients in the non-occurrence group (68.58 ± 5.16 years) and the occurrence group (69.17 ± 5.36 years) showed no significant difference (t=0.673, P=0.503). Gender distribution, with 71 (46.71%) males and 81 (53.29%) females in the non-occurrence group and 25 (52.08%) males and 23 (47.92%) females in the occurrence group, also revealed no significant difference (χ2=0.234, P=0.628). Similarly, BMI, duration of disease, smoking history, drinking history, hypertension, diabetes, hyperlipidemia, education level, social support, cause of injury, history of fracture, and ASA grade did not demonstrate statistically significant differences between the two groups. Notably, the Singh index for osteoporosis did reveal a statistically significant difference, with a higher occurrence of blade excessive lateral migration in patients with a Singh index of III (31.25%) compared to those with a Singh index of I-II (4.17%) and IV-VI (64.58%) (χ2=11.816, P=0.003) (Table 1).
Table 1.
General information of patients in the occurrence and non-occurrence groups
| Item | Non-occurrence group (n=152) | Occurrence group (n=48) | t/χ2 | P |
|---|---|---|---|---|
| Age (years) | 68.58 ± 5.16 | 69.17 ± 5.36 | 0.673 | 0.503 |
| Gender (M/F) | 71 (46.71%)/81 (53.29%) | 25 (52.08%)/23 (47.92%) | 0.234 | 0.628 |
| BMI (kg/m2) | 22.79 ± 3.24 | 22.26 ± 3.45 | 0.940 | 0.350 |
| Duration of disease (months) | 1.23 ± 0.56 | 1.15 ± 0.48 | 0.885 | 0.379 |
| Smoking history [n (%)] | 21 (13.82%) | 8 (16.67%) | 0.064 | 0.800 |
| Drinking history [n (%)] | 32 (21.05%) | 11 (22.92%) | 0.005 | 0.942 |
| Hypertension [n (%)] | 39 (25.66%) | 13 (27.08%) | 0.000 | 0.994 |
| Diabetes [n (%)] | 28 (18.42%) | 8 (16.67%) | 0.004 | 0.952 |
| Hyperlipidemia [n (%)] | 18 (11.84%) | 7 (14.58%) | 0.063 | 0.802 |
| Education level [n (%)] | 0.177 | 0.915 | ||
| Primary school | 58 (38.16%) | 19 (39.58%) | ||
| Junior school | 62 (40.79%) | 18 (37.50%) | ||
| Senior high school or above | 32 (21.05%) | 11 (22.92%) | ||
| Social support [n (%)] | 0.204 | 0.652 | ||
| Living alone | 55 (36.18%) | 15 (31.25%) | ||
| Living with spouse | 97 (63.82%) | 33 (68.75%) | ||
| Cause of injury [n (%)] | 0.101 | 0.750 | ||
| Fall | 149 (98.03%) | 46 (95.83%) | ||
| Other | 3 (1.97%) | 2 (4.17%) | ||
| History of fracture [n (%)] | 5 (3.29%) | 3 (6.25%) | 0.240 | 0.624 |
| ASA grade [n (%)] | 2.544 | 0.280 | ||
| I-II | 24 (15.79%) | 12 (25.00%) | ||
| III | 112 (73.68%) | 33 (68.75%) | ||
| IV | 16 (10.53%) | 3 (6.25%) | ||
| Singh index-osteoporosis [n (%)] | None | 0.003 | ||
| I-II | 2 (1.32%) | 2 (4.17%) | ||
| III | 19 (12.5%) | 15 (31.25%) | ||
| IV-VI | 131 (86.18%) | 31 (64.58%) |
BMI: Body Mass Index; ASA: American Society of Anesthesiologists.
Surgical indices
As shown in Table 2, the comparisons between the non-occurrence group and the occurrence group revealed no significant differences in blood loss (78.12 ± 10.13 mL vs. 81.26 ± 10.47 mL, t=1.826, P=0.072) or operation time (103.43 ± 20.35 min vs. 107.68 ± 20.19 min, t=1.270, P=0.208). However, the occurrence group demonstrated a higher incidence of revision surgery for blade prominence (8.33% vs. 0.00%, χ2=9.023, P=0.003) and a longer hospital stay (12.45 ± 6.67 days vs. 9.43 ± 3.56 days, t=2.998, P=0.004) compared to the non-occurrence group.
Table 2.
Surgical indices in the occurrence and non-occurrence groups
| Item | Non-occurrence group (n=152) | Occurrence group (n=48) | t/χ2 | P |
|---|---|---|---|---|
| Blood loss | 78.12 ± 10.13 | 81.26 ± 10.47 | 1.826 | 0.072 |
| Operation time (min) | 103.43 ± 20.35 | 107.68 ± 20.19 | 1.270 | 0.208 |
| Revision surgery for blade prominence [n (%)] | 0 (0.00%) | 4 (8.33%) | 9.023 | 0.003 |
| Hospital stays (days) | 9.43 ± 3.56 | 12.45 ± 6.67 | 2.998 | 0.004 |
Imaging measures
No significant difference was identified in lesser trochanter displacement between the non-occurrence and occurrence groups (7.89% vs. 10.42%, χ2=0.062, P=0.803) (Table 3). However, significant differences were observed between blade position in the lateral view (χ2=12.092, P=0.002), the quality of calcar reduction (χ2=9.487, P=0.002), immediate postoperative lateralization (t=8.514, P<0.001), final lateralization (t=16.175, P<0.001), and final migration (t=9.695, P<0.001). Specifically, the occurrence group showed a higher prevalence of the inferior blade position in the AP view, a poorer calcar reduction, and significantly greater immediate postoperative lateralization, final lateralization, and final migration compared to the non-occurrence group.
Table 3.
Imaging measures in the occurrence and non-occurrence groups
| Item | Non-occurrence group (n=152) | Occurrence group (n=48) | t/χ2 | P |
|---|---|---|---|---|
| Lesser trochanter displace [n (%)] | 12 (7.89%) | 5 (10.42%) | 0.062 | 0.803 |
| Blade position head in AP [n (%)] | 5.189 | 0.075 | ||
| Superior | 14 (9.21%) | 1 (2.08%) | ||
| Centre | 117 (76.97%) | 44 (91.67%) | ||
| Inferior | 21 (13.82%) | 3 (6.25%) | ||
| Blade position head in lateral [n (%)] | 12.092 | 0.002 | ||
| Anterior | 6 (3.95%) | 2 (4.17%) | ||
| Centre | 128 (84.21%) | 30 (62.50%) | ||
| Posterior | 18 (11.84%) | 16 (33.33%) | ||
| Quality of calcar reduction [n (%)] | 9.487 | 0.002 | ||
| Good | 135 (88.82%) | 33 (68.75%) | ||
| Poor | 17 (11.18%) | 15 (31.25%) | ||
| Immediate postoperative lateralization (mm) | 1.83 ± 0.51 | 5.02 ± 2.58 | 8.514 | <0.001 |
| Final lateralization (mm) | 3.34 ± 1.23 | 14.58 ± 4.76 | 16.175 | <0.001 |
| Final migration (mm) | 2.65 ± 1.02 | 8.48 ± 4.13 | 9.695 | <0.001 |
AP: anterior-posterior.
Fracture stability indicators
The comparison between the non-occurrence group and the occurrence group revealed significant differences in the TAD (24.38 ± 8.43 mm vs. 20.34 ± 8.15 mm, t=2.924, P=0.005) (Table 4). In contrast, no significant differences were found in nail length (401.28 ± 42.18 mm vs. 397.15 ± 48.26 mm, t=0.571, P=0.569) or nail diameter (11.27 ± 0.79 mm vs. 11.35 ± 0.85 mm, t=0.584, P=0.561). However, the results of AO/OTA classification demonstrated a higher proportion of A2 fractures (62.50%) in the occurrence group compared to the non-occurrence group (42.11%) (χ2=7.228, P=0.027). Additionally, the occurrence group showed a higher percentage of unstable fractures (43.75%) compared to the non-occurrence group (21.05%) (χ2=8.519, P=0.004). These findings highlight the critical role of fracture stability indicators, particularly TAD, AO/OTA classification, and fracture type, for understanding the risk of excessive lateral migration of the PFNA blade in this specific patient population.
Table 4.
Fracture stability indicators in the occurrence and non-occurrence groups
| Item | Non-occurrence group (n=152) | Occurrence group (n=48) | t/χ2 | P |
|---|---|---|---|---|
| TAD (mm) | 20.34 ± 8.15 | 24.38 ± 8.43 | 2.924 | 0.005 |
| Nail length (mm) | 397.15 ± 48.26 | 401.28 ± 42.18 | 0.571 | 0.569 |
| Nail diameter (mm) | 11.35 ± 0.85 | 11.27 ± 0.79 | 0.584 | 0.561 |
| AO/OTA classification [n (%)] | 7.228 | 0.027 | ||
| A1 | 50 (32.89%) | 13 (27.08%) | ||
| A2 | 64 (42.11%) | 30 (62.50%) | ||
| A3 | 38 (25.00%) | 5 (10.42%) | ||
| Fracture type [n (%)] | 8.519 | 0.004 | ||
| Stable | 120 (78.95%) | 27 (56.25%) | ||
| Unstable | 32 (21.05%) | 21 (43.75%) |
TAD: tip-apex distance; AO/OTA: Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association.
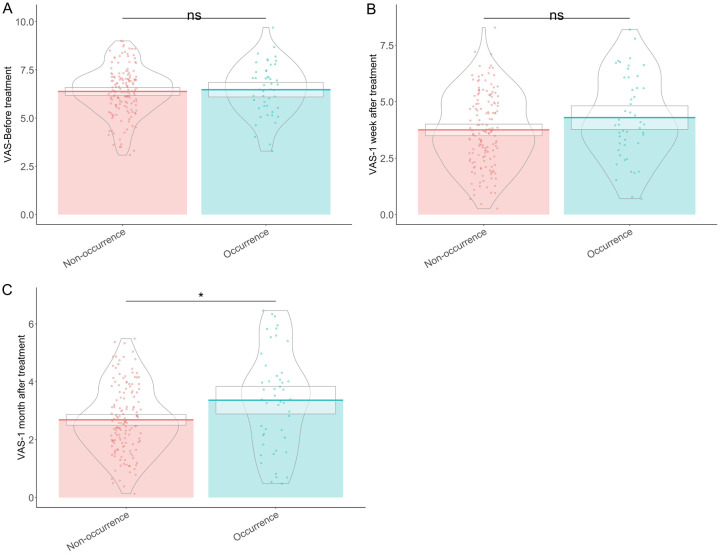
VAS scores
The analysis revealed no significant differences in VAS scores before treatment (6.38 ± 1.25 vs. 6.47 ± 1.33, t=0.415, P=0.679) and at 1 week after treatment (3.75 ± 1.62 vs. 4.29 ± 1.84, t=1.839, P=0.070) (Figure 1). However, at 1 month after treatment, a significant difference was found, with higher VAS scores in the occurrence group compared to the non-occurrence group (3.36 ± 1.68 vs. 2.68 ± 1.16, t=2.609, P=0.011). This emergence of a difference in VAS scores at the 1-month follow-up, indicates a possible association between pain level and the occurrence of excessive lateral migration of the PFNA blade in this patient cohort.
Figure 1.
VAS scores of patients in the occurrence and non-occurrence groups before (A), 1 week after (B), and 1 month after (C) treatment. ns: no significant difference; *: P<0.05.
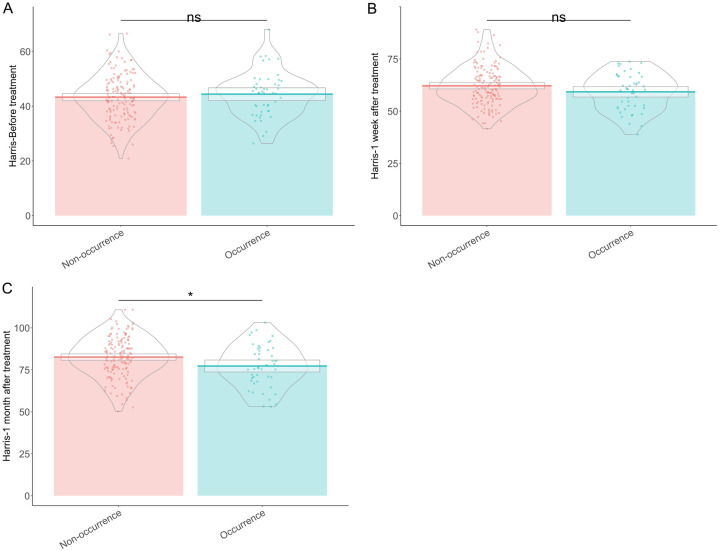
Hip joint scores (Harris)
In examining hip joint scores (Harris) among the patients, the comparison between the non-occurrence group and the occurrence group revealed no significant difference in hip joint scores before treatment (43.29 ± 8.36 vs. 44.38 ± 8.19, t=0.796, P=0.428) and at 1 week after treatment (62.12 ± 9.26 vs. 59.23 ± 8.79, t=1.960, P=0.053) (Figure 2). However, a significant difference emerged at 1 month after treatment, with a higher hip joint score in the non-occurrence group compared to that of the occurrence group (82.56 ± 12.12 vs. 77.24 ± 12.58, t=2.576, P=0.012). The emergence of a significant difference in hip joint scores at the 1-month follow-up suggests a pcorrelation between hip joint function and the occurrence of excessive lateral migration of the PFNA blade in this patient population.
Figure 2.
Hip joint scores (Harris) of patients in the occurrence and non-occurrence groups before (A), 1 week after (B) and 1 month after (C) treatment. ns: no significant difference; *: P<0.05.
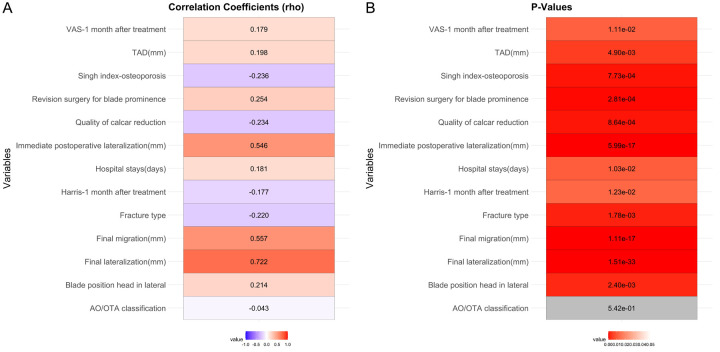
Single-factor correlation analysis
As shown in Figure 3, Singh index (rho=-0.236, P<0.001), quality of calcar reduction (rho=-0.234, P<0.001), fracture type (rho=-0.220, P=0.002), Harris at 1 month after treatment (rho=-0.177, P=0.012), revision surgery for blade prominence (rho=0.254, P<0.001), hospital stays (rho=0.181, P=0.010), blade position head in lateral (rho=0.214, P=0.002), immediate postoperative lateralization (rho=0.546, P<0.001), final lateralization (rho=0.722, P<0.001), final migration (rho=0.557, P<0.001), TAD (rho=0.198, P=0.005), and VAS at 1 month after treatment (rho=0.179, P=0.011) exhibited significant associations with excessive lateral migration of the PFNA blade, underlining their possible relevance as risk factors in this specific patient population. The highest positive correlations factors were final lateralization, final migration, and immediate postoperative lateralization, while the highest negative correlations factors were Singh index, quality of calcar reduction, and fracture type.
Figure 3.
Single-factor correlation analysis of risk factors for excessive blade lateral migration. Blue suggests negative correlation, red suggests positive correlation, and grey suggests no significant correlation.
Multivariate logistic regression analysis
As shown in Table 5, multivariate logistic regression analysis identified that lower Singh index (OR: 0.357, 95% CI: 0.182-0.686, P=0.002) and better quality of calcar reduction (OR: 0.277, 95% CI: 0.125-0.615, P=0.001) were associated with reduced risk. In contrast, longer hospital stays (OR: 1.150, 95% CI: 1.070-1.243, P<0.001), lateral blade position in the head (OR: 2.906, 95% CI: 1.407-6.081, P=0.004), immediate postoperative lateralization (OR: 4.509, 95% CI: 2.892-8.028, P<0.001), final lateralization (OR: 5.596, 95% CI: 2.739-22.111, P<0.001), final migration (OR: 2.520, 95% CI: 1.932-3.583, P<0.001), higher TAD (OR: 1.061, 95% CI: 1.020-1.106, P=0.004), fracture type (OR: 0.343, 95% CI: 0.171-0.686, P=0.002), VAS score 1 month post-treatment (OR: 1.470, 95% CI: 1.149-1.901, P=0.003), and Harris score 1 month post-treatment (OR: 0.966, 95% CI: 0.939-0.992, P=0.011) were associated with increased risk. Independent influencing factors included Singh index, hospital stays, blade position, calcar reduction quality, postoperative lateralization, final lateralization, final migration, TAD, fracture type, VAS, and Harris scores.
Table 5.
Multivariate logistic regression analysis of risk factors associated with excessive blade lateral migration
| Item | Coefficient | Std Error | Wald | P Value | OR | CI Lower | CI Upper |
|---|---|---|---|---|---|---|---|
| Singh index-osteoporosis | -1.030 | 0.335 | 3.075 | 0.002 | 0.357 | 0.182 | 0.686 |
| Hospital stays (days) | 0.140 | 0.038 | 3.689 | <0.001 | 1.150 | 1.070 | 1.243 |
| Blade position head in lateral | 1.067 | 0.372 | 2.868 | 0.004 | 2.906 | 1.407 | 6.081 |
| Quality of calcar reduction | -1.284 | 0.404 | 3.177 | 0.001 | 0.277 | 0.125 | 0.615 |
| Immediate postoperative lateralization (mm) | 1.506 | 0.258 | 5.831 | <0.001 | 4.509 | 2.892 | 8.028 |
| Final lateralization (mm) | 1.722 | 0.508 | 3.389 | <0.001 | 5.596 | 2.739 | 22.111 |
| Final migration (mm) | 0.924 | 0.156 | 5.926 | <0.001 | 2.520 | 1.932 | 3.583 |
| TAD (mm) | 0.059 | 0.021 | 2.861 | 0.004 | 1.061 | 1.020 | 1.106 |
| Fracture type | -1.070 | 0.352 | 3.037 | 0.002 | 0.343 | 0.171 | 0.686 |
| VAS-1 month after treatment | 0.385 | 0.128 | 3.015 | 0.003 | 1.470 | 1.149 | 1.901 |
| Harris-1 month after treatment | -0.035 | 0.014 | 2.551 | 0.011 | 0.966 | 0.939 | 0.992 |
Discussion
This study aimed to identify and analyze the risk factors associated with excessive lateral migration of the helical blade after PFNA surgery among elderly patients with intertrochanteric femur fracture. Excessive migration of the helical blade is a known complication that can lead to clinical failure, requiring revision surgery and prolonged hospital stays [22]. Our findings provide crucial insight into the multifactorial nature of this complication and suggest that both patient-related and surgical factors contribute significantly to the risk of blade migration.
Excessive lateral migration of the helical blade has been identified primarily with poorer osteoporosis grade as measured by the Singh index. Patients with low Singh indices demonstrated a higher propensity for blade migration. This observation underscores the importance of bone quality in the stability of the helical blade. Osteoporotic bones are less capable of providing adequate purchase for the blade, leading to decreased stability and increased risk of migration [23]. Poorer bone quality means that the compressive forces exerted by the helical blade are less effectively counteracted by the surrounding bone, leading to progressive lateral migration [24]. Hence, managing osteoporosis either preoperatively or through the selection of more suitable fixation devices might mitigate this risk.
Additionally, the quality of calcar reduction emerged as a vital factor. Good calcar reduction provides better mechanical support and stability, reducing the forces acting to displace the blade laterally [25]. Conversely, poor reduction alignment means that there is residual displacement at the fracture site, which alters the biomechanics of the hip joint and increases the likelihood of the blade cutting out [26]. This poor biomechanical environment can lead to abnormal stress distributions that favor lateral migration [27]. Thus, meticulous attention to achieving an optimal reduction intraoperatively cannot be overemphasized.
The hospital stay duration was another significant risk factor, with longer stays correlating with a higher incidence of blade migration. This finding suggests that extended hospital stays could be an indicator of complications or suboptimal initial stabilization [24]. These patients may have experienced more significant soft-tissue damage, compromised overall health, or other complications that necessitated prolonged hospitalization and, therefore, might have been predisposed to mechanical complications such as blade migration [25]. Prolonged immobilization could also adversely affect muscle strength and joint stability, indirectly contributing to the migration [28].
Blade position within the femoral head, particularly a lateral blade position, was associated with an increased risk of migration. Proper blade placement is critical for mechanical stability [22]. A centered or slightly inferior position might reduce the shear stresses that act on the blade during weight-bearing activities [16]. An inappropriate lateral position, however, increases these shear forces, thereby favoring lateral migration [18]. Therefore, ensuring the intraoperative accuracy of blade placement using both AP and lateral fluoroscopic views is crucial.
Immediate postoperative lateralization, final lateralization, and final migration were strongly associated with excessive blade migration. These measurements indicate that suboptimal immediate postoperative blade positioning is a clear marker for future complications. The mechanisms here likely involve initial improper positioning that leads to progressively worsening displacement as the patient begins to bear weight and mobilize postoperatively [29]. Early identification and potentially revising the fixation if early displacements are detected could help prevent further complications.
The TAD was also identified as a significant factor. As an established metric for predicting cut-out risks in hip fracture surgeries, TAD represents the combined distance from the tip of the blade to the apex of the femoral head in both AP and lateral planes [30]. A larger TAD indicates improper screw placement, which does not provide adequate mechanical purchase and increases the likelihood of cut-out and lateral migration [23]. Therefore, surgeons should aim for a TAD of less than 25 mm to minimize these risks.
The presence of unstable fractures and specific types of fractures as classified by AO/OTA was also correlated with higher risks of migration. Unstable fracture patterns inherently lead to less biomechanical stability after fixation [11]. In these cases, the fixation construct, including the blade, has to compensate for a higher degree of instability, thus facing greater forces that predispose it to displacement [11,12]. This provides a clear mandate for more rigid fixation techniques or alternative surgical approaches for managing unstable fracture patterns.
Regarding pain and functional outcome measured by the VAS scores and Harris hip scores, respectively, correlations with these factors highlight that clinical symptoms can be both indicators and outcomes of the migration process. Higher VAS scores at one month post-treatment in the occurrence group suggest that excessive blade migration leads to increased pain, possibly due to micromotion at the fracture site and resultant mechanical irritation [31]. Similarly, poorer Harris scores indicate that functional recovery was adversely affected by blade migration, rendering these patients less capable of achieving optimal hip joint function postoperatively [31].
It is critical to acknowledge that the multivariate logistic regression analysis identified independent risk factors, including the Singh index, hospital stay duration, blade position, calcar reduction quality, immediate postoperative lateralization, final lateralization, final migration, TAD, fracture type, VAS, and Harris scores. These factors collectively underscore the multifactorial etiology behind excessive blade migration. Intervention strategies must be multifaceted, addressing patient-specific factors such as osteoporosis management and perioperative care, as well as surgical technique-specific factors such as optimal blade position and reduction quality [32].
While our study provides valuable insight into the risk factors associated with excessive lateral migration of the helical blade in PFNA, several limitations must be acknowledged. First, the retrospective design inherently carries arisk of selection bias, and the reliance on de-identified data may limit the granularity of the clinical details available. Additionally, this study was conducted at a single institution, which may affect the generalizability of the findings to broader populations. The sample size, while sufficient for statistical analysis, may still be limited in capturing all possible variables influencing blade migration. The lack of long-term follow-up data precludes the assessment of longer-term outcome and complications, and there may be unmeasured confounders influencing the results.
Conclusion
Excessive lateral migration of the helical blade in the PFNA procedure is a significant complication influenced by a combination of patient-related and surgical factors. The study elucidates the critical nature of osteoporosis management, intraoperative reduction quality, and proper blade placement to minimize the risk of this complication. Future research should focus on developing enhanced fixation techniques and preoperative optimization strategies that improve bone quality, aiming to provide better a outcome for patients undergoing PFNA for intertrochanteric femur fracture. Enhanced intraoperative imaging and navigation tools could also play a pivotal role in to ensure optimal surgical outcome.
Disclosure of conflict of interest
None.
References
- 1.Li K, Yang H, Jiang Z, Peng W, Zhou X. Effect of proximal femoral nail antirotation on clinical outcome, inflammatory factors and myocardial injury markers in patients with femoral trochanteric fracture. Am J Transl Res. 2022;14:4795–4803. [PMC free article] [PubMed] [Google Scholar]
- 2.Sandifer PA, Hulick RM, Graves ML, Spitler CA, Russell GV, Hydrick JM, Jones LC, Bergin PF. Extent and morbidity of lateralization of a trochanteric fixation nail blade. Orthopedics. 2017;40:e886–e891. doi: 10.3928/01477447-20170810-05. [DOI] [PubMed] [Google Scholar]
- 3.Wang H, Yang W, Ding K, Zhu Y, Zhang Y, Ren C, Zhao K, Zhang Q, Chen W, Zhang Y. Biomechanical study on the stability and strain conduction of intertrochanteric fracture fixed with proximal femoral nail antirotation versus triangular supporting intramedullary nail. Int Orthop. 2022;46:341–350. doi: 10.1007/s00264-021-05250-8. [DOI] [PubMed] [Google Scholar]
- 4.Guobin C, Cui Y, Maoquan Z, Qishu X. A comparison between proximal femoral nail antirotation (PFNA) and inter Tan nail for the surgical treatment of unstable intertrochanteric fracture: a case series. Asian J Surg. 2021;44:1095–1096. doi: 10.1016/j.asjsur.2021.05.025. [DOI] [PubMed] [Google Scholar]
- 5.Jing J, Jiang H, Liu C, Zhang L. Common peroneal nerve injury after proximal femoral nail antirotation (PFNA): a case report. Asian J Surg. 2023;46:2399–2401. doi: 10.1016/j.asjsur.2022.12.027. [DOI] [PubMed] [Google Scholar]
- 6.Chang HM, Lu WY, Kuan FC, Su WR, Chen PY, Su PF, Hsu KL. Wound drainage after proximal femoral nail antirotation (PFNA) fixation may negatively affect the patients with intertrochanteric fractures: a prospective randomized controlled trial. Injury. 2021;52:575–581. doi: 10.1016/j.injury.2020.10.033. [DOI] [PubMed] [Google Scholar]
- 7.Wang J, Ma JX, Lu B, Bai HH, Wang Y, Ma XL. Comparative finite element analysis of three implants fixing stable and unstable subtrochanteric femoral fractures: Proximal Femoral Nail Antirotation (PFNA), Proximal Femoral Locking Plate (PFLP), and Reverse Less Invasive Stabilization System (LISS) Orthop Traumatol Surg Res. 2020;106:95–101. doi: 10.1016/j.otsr.2019.04.027. [DOI] [PubMed] [Google Scholar]
- 8.Zheng L, Wong DW, Chen X, Chen Y, Li P. Risk of proximal femoral nail antirotation (PFNA) implant failure upon different lateral femoral wall thickness in intertrochanteric fracture: a finite element analysis. Comput Methods Biomech Biomed Engin. 2022;25:512–520. doi: 10.1080/10255842.2021.1964488. [DOI] [PubMed] [Google Scholar]
- 9.She Z, Yang F, Zhang S, Yang L, Wang X. A novel intramedullary nail design of intertrochanteric fracture fixation improved by proximal femoral nail antirotation. Comput Methods Biomech Biomed Engin. 2023:1–11. doi: 10.1080/10255842.2023.2286917. [DOI] [PubMed] [Google Scholar]
- 10.Nie SB, Zhao YP, Li JT, Zhao Z, Zhang Z, Zhang LC, Tang PF. Medial support nail and proximal femoral nail antirotation in the treatment of reverse obliquity inter-trochanteric fractures (Arbeitsgemeinschaft fur Osteosynthesfrogen/Orthopedic Trauma Association 31-A3.1): a finite-element analysis. Chin Med J (Engl) 2020;133:2682–2687. doi: 10.1097/CM9.0000000000001031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liang Y, Liu S, Li L, Zhong F. Proximal femoral nail antirotation versus external fixation for unstable intertrochanteric fractures in elderly patients: a randomized controlled trial. Medicine (Baltimore) 2022;101:e29384. doi: 10.1097/MD.0000000000029384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee YK, Kim JT, Park CH, Song JU, Kim TY, Koo KH. Analysis of risk factor for nail breakage in patients with mechanical failures after proximal femoral nail antirotation in intertrochanteric fractures. Medicine (Baltimore) 2022;101:e29436. doi: 10.1097/MD.0000000000029436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Y, Chen W, Zhang L, Xiong C, Zhang X, Yu K, Ju J, Chen X, Zhang D, Zhang Y. Finite element analysis of Proximal Femur Bionic Nail (PFBN) compared with proximal femoral nail antirotation and intertan in treatment of intertrochanteric fractures. Orthop Surg. 2022;14:2245–2255. doi: 10.1111/os.13247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cai Y, Zhu W, Wang N, Yu Z, Chen Y, Xu S, Feng J. Therapeutic effects of the proximal femoral nail for the treatment of unstable intertrochanteric fractures. Evid Based Complement Alternat Med. 2022;2022:1001354. doi: 10.1155/2022/1001354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo J, Dong W, Jin L, Yin Y, Zhang R, Hou Z, Zhang Y. Treatment of basicervical femoral neck fractures with proximal femoral nail antirotation. J Int Med Res. 2019;47:4333–4343. doi: 10.1177/0300060519862957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jin Z, Xu S, Yang Y, Wei Y, Tian Y, Wang Z, Bai L. Cemented hemiarthroplasty versus proximal femoral nail antirotation in the management of intertrochanteric femoral fractures in the elderly: a case control study. BMC Musculoskelet Disord. 2021;22:846. doi: 10.1186/s12891-021-04586-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zheng L, Chen X, Zheng Y, He X, Wu J, Lin Z. Cement augmentation of the proximal femoral nail antirotation for the treatment of two intertrochanteric fractures - a comparative finite element study. BMC Musculoskelet Disord. 2021;22:1010. doi: 10.1186/s12891-021-04878-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi W, Zhang Y, Xu Y, Zeng X, Fu H, Yu W. Conversion of failed proximal femoral nail antirotation to uncemented or cemented femoral component fixation: a multicentre retrospective study with a median 10-year follow-up. BMC Musculoskelet Disord. 2022;23:375. doi: 10.1186/s12891-022-05323-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lenz M, Schwinn J, Hofmann-Fliri L, Schwyn R, Knobe M, Klos K, Kielstein H, Hofmann GO, Gueorguiev B. Influence of reduced tip-apex distance on helical blade fixation-a biomechanical study. J Orthop Res. 2019;37:649–654. doi: 10.1002/jor.24202. [DOI] [PubMed] [Google Scholar]
- 20.Tangkanjanavelukul P, Thaitalay P, Srisuwan S, Petchwisai P, Thasanaraphan P, Saramas Y, Nimarkorn K, Warojananulak W, Kanchanomai C, Rattanachan ST. Feasibility biomechanical study of injectable Biphasic Calcium Phosphate bone cement augmentation of the proximal femoral nail antirotation (PFNA) for the treatment of two intertrochanteric fractures using cadaveric femur. Biomed Phys Eng Express. 2024;10 doi: 10.1088/2057-1976/ad4e3c. [DOI] [PubMed] [Google Scholar]
- 21.Yen SH, Lu CC, Ho CJ, Huang HT, Tu HP, Chang JK, Chen CH, Lin SY. Impact of wedge effect on outcomes of intertrochanteric fractures treated with intramedullary proximal femoral nail. J Clin Med. 2021;10:5112. doi: 10.3390/jcm10215112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu KT, Lin SJ, Chou YC, Cheng HH, Wen PC, Lin CH, Yeh WL. Ipsilateral femoral neck and shaft fractures fixation with proximal femoral nail antirotation II (PFNA II): technical note and cases series. J Orthop Surg Res. 2020;15:20. doi: 10.1186/s13018-019-1524-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nie S, Li M, Ji H, Li Z, Li W, Zhang H, Licheng Z, Tang P. Biomechanical comparison of medial sustainable nail and proximal femoral nail antirotation in the treatment of an unstable intertrochanteric fracture. Bone Joint Res. 2020;9:840–847. doi: 10.1302/2046-3758.912.BJR-2020-0284.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liao CS, He FZ, Li XY, Han PF. Proximal femoral nail antirotation versus InterTan nail for the treatment of intertrochanteric fractures: a systematic review and meta-analysis. PLoS One. 2024;19:e0304654. doi: 10.1371/journal.pone.0304654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baek SH, Baek S, Won H, Yoon JW, Jung CH, Kim SY. Does proximal femoral nail antirotation achieve better outcome than previous-generation proximal femoral nail? World J Orthop. 2020;11:483–491. doi: 10.5312/wjo.v11.i11.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Öner K, Durusoy S, Özer A. A new proximal femoral nail antirotation design: is it effective in preventing varus collapse and cut-out? Jt Dis Relat Surg. 2020;31:426–431. doi: 10.5606/ehc.2020.75113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rana R, Behera H, Behera S 2nd, G A, Singh M. Outcomes of ipsilateral femoral neck and shaft fractures treated with proximal femoral nail antirotation 2. Cureus. 2021;13:e18511. doi: 10.7759/cureus.18511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh S. Proximal femoral nail versus proximal femoral nail antirotation: functional and radiological outcome in intertrochanteric fractures of femur. Cureus. 2021;13:e19093. doi: 10.7759/cureus.19093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rai B, Singh J, Singh V, Singh G, Pal B, Kumar D, Poddar M. Evaluation of the outcomes of proximal femoral nail antirotation II in the treatment of trochanteric fracture in elderly patients. Cureus. 2022;14:e24896. doi: 10.7759/cureus.24896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li X, Xu J. Comparison of proximal femoral nail antirotation and total hip arthroplasty in the treatment of femoral intertrochanteric fracture. Pak J Med Sci. 2022;38:1016–1020. doi: 10.12669/pjms.38.4.5830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baral P, Chaudhary P, Shah AB, Banjade D, Jha SC. Outcome of proximal femoral nail antirotation II fixation of peritrochanteric fracture of femur. J Nepal Health Res Counc. 2020;18:301–306. doi: 10.33314/jnhrc.v18i2.2956. [DOI] [PubMed] [Google Scholar]
- 32.Durgut F, Şahin E, Çiftçi S, Kerem BA. Proximal femoral nail antirotation versus cemented calcar-replacement hemiarthroplasty for unstable intertrochanteric fracture in elderly: an overall survival study. Turk J Med Sci. 2022;52:463–466. doi: 10.3906/sag-2105-28. [DOI] [PMC free article] [PubMed] [Google Scholar]