Abstract
Objective: To evaluate the clinical efficacy of open versus arthroscopic rotator cuff repair in treating moderate rotator cuff tears. Methods: A retrospective study was conducted on 68 patients diagnosed with moderate rotator cuff tears and who were treated surgically at Hangzhou Fuyang Hospital of Traditional Chinese Medicine Orthopedics and Traumatology from September 2021 to April 2023. Patients were categorized based on the surgical methods they received: the minimally invasive group (MIG, n=37, undergoing arthroscopic rotator cuff repair) and the open surgery group (OSG, n=31, undergoing open rotator cuff repair). Operative indicators, perioperative and follow-up pain intensity, shoulder joint scores, range of motion, and complication incidence were compared between the two groups. Additionally, the factors affecting prognosis were also analyzed. Results: The MIG had shorter operative time, shorter hospital stay, smaller incision length, and less intraoperative blood loss than the OSG (all P<0.05). At 6 weeks and 3 months postoperatively, the MIG reported significantly lower Visual Analogue Scale (VAS) scores and higher Constant-Murley scores compared to the OSG (all P<0.05). At the 6-month follow-up, the MIG exhibited higher University of California-Los Angeles scores and Constant scores, as well as greater forward flexion, abduction, and lateral rotation angles than OSG (all P<0.05). The incidence of complications was lower in the MIG compared to the OSG (P<0.05). The binomial logistic regression analysis identified surgical approach as an independent risk factor for postoperative complications (P<0.05). Conclusion: Arthroscopic rotator cuff repair for patients with rotator cuff tears involves minimal trauma and allows for rapid postoperative recovery. Additionally, the procedure helps restore shoulder joint function and improve the range of motion, offering promising clinical applications.
Keywords: Rotator cuff tear, arthroscopy, rotator cuff repair, open surgery, shoulder joint function, range of motion
Introduction
The shoulder joint is a major articulation point in the human body with a complex structure. The rotator cuff is a group of tendons that envelop the humeral head, resembling a cuff of tendons [1,2]. It plays a pivotal role in the movement and stabilization of the shoulder joint, with its four muscles working together to assist the shoulder joint in functional activities [3]. Clinical practice shows that the shoulder joint’s unique anatomical structure, with its unstable bony structure, thin surrounding joint capsule, and few joint ligaments, leads to a close mechanical interplay between the rotator cuff muscles and surrounding tissues; consequently, any issue with any of the rotator cuff muscles can impair shoulder function [4,5]. Additionally, tendon degeneration and subacromial impingement pose risks for rotator cuff tears, leading to pain and mobility impairments [6]. Data indicate that patients with shoulder pain caused by rotator cuff tears account for approximately 17%-41% of total shoulder pain cases, and the incidence of rotator cuff tears is about 20% among individuals aged 20-60 years and up to 54% in those over 60; most patients with rotator cuff tears seek medical attention due to the significant impact on their daily lives [7,8].
Current treatment measures for moderate rotator cuff tears primarily involve surgical and conservative approaches. For individuals with mild or asymptomatic conditions, conservative treatments such as non-steroidal anti-inflammatory drugs, physical shock wave therapy, acupuncture, massage, local blockade, and appropriate stretching are recommended [9,10]. However, for those with more pronounced symptoms or higher expectations for shoulder joint function recovery, surgical intervention is advised. Common surgical treatments for rotator cuff tears include open surgery and arthroscopic surgery, both aimed at anatomical reduction and managing combined injuries [11,12]. Open surgery offers excellent intraoperative visibility, minimal operational complexity, and thorough repair of rotator cuff injuries, but it also presents drawbacks such as significant trauma and extended postoperative recovery periods [13]. The advancement of imaging techniques has led to the increased utilization of arthroscopic surgery [14]. This study investigated the merits and demerits of open surgery versus arthroscopic surgery for patients with rotator cuff tears through a comparative group design. The innovation lies in the comparative analysis of quantitative data, revealing that arthroscopic rotator cuff repair has the advantages of minimal trauma and rapid postoperative recovery, and that the surgery has a positive significance on the improvement of the joint function of patients through short-term follow-up, thereby providing more clinical data to enhance the prognosis of patients with rotator cuff tears.
Study design and patients
Patient selection
This retrospective study received approval from the Ethics Committee of Hangzhou Fuyang Hospital of Traditional Chinese Medicine Orthopedics and Traumatology. All participants provided written informed consent before joining the study. Clinical data were collected from patients diagnosed with rotator cuff tears and who underwent surgical treatment at Hangzhou Fuyang Hospital of Traditional Chinese Medicine Orthopedics and Traumatology from September 2021 to April 2023. A total of 187 patients were screened based on the following inclusion and exclusion criteria:
Inclusion criteria: (1) Patients diagnosed with rotator cuff tears via MRI and physical examination; (2) History of illness less than 6 months; (3) No surgical history on the affected shoulder; (4) Complete information in the hospital’s medical record system (general clinical data, preoperative and postoperative joint function scores, range of motion during the preoperative period and postoperative follow-up); (5) Patients with a minimum of 6 months of follow-up results.
Exclusion criteria: (1) Incomplete clinical data; (2) Presence of shoulder osteoarthritis; (3) History of shoulder fractures or other shoulder surgeries; (4) Intraoperative change of surgical approach.
After screening 187 patients based on the inclusion and exclusion criteria, 68 patients were included in the study. These 68 patients were categorized into the minimally invasive group (MIG, n=37, undergoing arthroscopic rotator cuff repair) and the open surgery group (OSG, n=31, undergoing open rotator cuff repair). Baseline clinical data were collected from the medical record system and compared between the two groups, showing no statistically significant differences (P>0.05) (Table 1).
Table 1.
Comparison of general clinical data between the two groups (x̅ ± s)/[n (%)]
| Clinical data | MIG (n=37) | OSG (n=31) | t/χ2 | P | |
|---|---|---|---|---|---|
| Gender | Male | 17 | 13 | 0.110 | 0.740 |
| Female | 20 | 18 | |||
| Average age (years) | 58.22±9.42 | 57.81±11.91 | 0.151 | 0.881 | |
| Side of rotator cuff tears | Left side | 16 | 12 | 0.143 | 0.705 |
| Right side | 21 | 19 | |||
| Rotator cuff tear classification | Small | 11 | 10 | 0.628 | 0.730 |
| Medium | 20 | 18 | |||
| Large | 6 | 3 | |||
| Massive | 0 | 0 | |||
| Underlying disease | Hypertension | 5 | 6 | 0.424 | 0.515 |
| Diabetes | 2 | 1 | 0.190 | 0.663 | |
MIG: minimally invasive group; OSG: open surgery group.
Data extraction
Based on the hospital medical record system, the following data of the enrolled patients were primarily collected.
Primary observation indicators
(1) The operation related indicators, including operative time, hospital stay, incision length, and intraoperative blood loss, were collected and compared between the two groups.
(2) The joint range of motion, including forward flexion, abduction, and lateral rotation angles, was compared between the two groups preoperatively (upon admission) and at a 6-month follow-up postoperatively (until October 2023).
Secondary observation indicators
(1) Pain intensity was compared between the two groups preoperatively, at 6 weeks, 3 months, and 6 months postoperatively using the Visual Analogue Scale (VAS) [15]. The VAS is a 0-10 cm line, with 0 indicating no pain and 10 indicating severe pain. Participants selected a point on the line that best represented their pain intensity.
(2) The Constant-Murley (CM scale) shoulder joint scores were compared between the two groups preoperatively, at 6 weeks, 3 months, and 6 months postoperatively [16]. The CM scale includes pain (15 points), activities of daily living (10 points), arm elevation (10 points), abduction muscle strength (25 points), forward flexion (10 points), abduction (10 points), external rotation (10 points), and internal rotation (10 points), totaling 100 points. Higher scores indicate better shoulder joint function.
(3) The University of California-Los Angeles (UCLA) scores were compared between the two groups preoperatively, at 6 weeks, 3 months, and 6 months postoperatively [17]. The UCLA score includes pain (10 points), function (10 points), active forward flexion (5 points), forward flexion strength (5 points), and patient satisfaction (5 points), totaling 35 points. Higher scores indicate greater patient satisfaction.
Outcome measures
This study aimed to compare and analyze the differences in perioperative indicators and postoperative joint function between patients with rotator cuff tears undergoing open surgery and those undergoing arthroscopic surgery. The expected goal of this research is to demonstrate that arthroscopic surgery alleviates the degree of intraoperative injury, promotes the recovery of postoperative joint function, and reduces the incidence of complications.
Statistical methods
Data collection for this study was conducted using Excel 2021, and data processing was performed with SPSS 26.0. All measurement data followed a normal distribution and were presented as mean ± standard deviation. Differences between groups were analyzed using an independent samples t-test, while comparisons at different time points were conducted using repeated measures ANOVA with post hoc multiple comparisons. Counting data were presented as rates, and group differences were assessed using the chi-square test. Univariate analysis was considered statistically significant at P<0.1 (to prevent type II errors), and risk factors were analyzed using the binomial logistic regression. Statistical significance was set at P<0.05.
Results
Comparison of operative indicators between the two groups
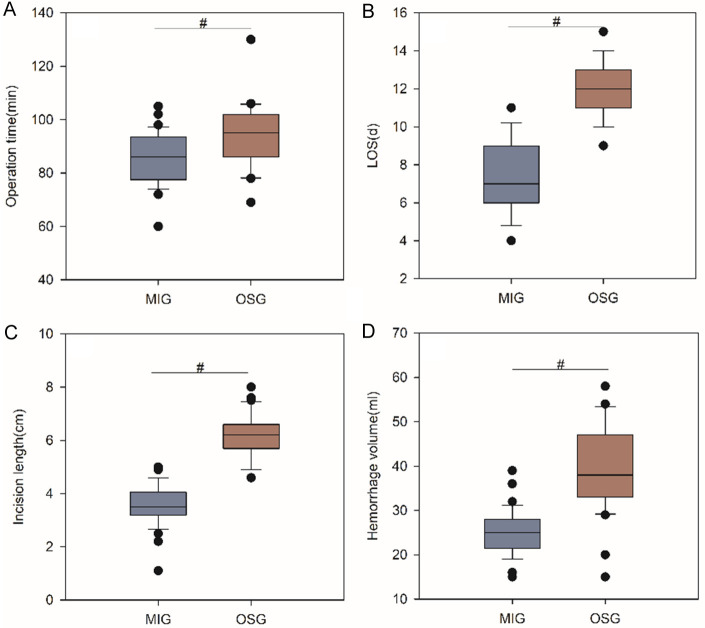
Operative indicators, including operative time (Figure 1A), hospital stay (Figure 1B), incision length (Figure 1C), and intraoperative blood loss (Figure 1D), were collected for both the MIG and the OSG. These indicators were significantly lower in the MIG than in the OSG (all P<0.05) (Figure 1).
Figure 1.
Comparison of operative indicators between the two groups. A: Operative time; B: Hospital stay; C: Incision length; D: Intraoperative blood loss. # represents a statistically significant difference between the groups. MIG: minimally invasive group; OSG: open surgery group.
Comparison of preoperative and postoperative pain intensity between the two groups
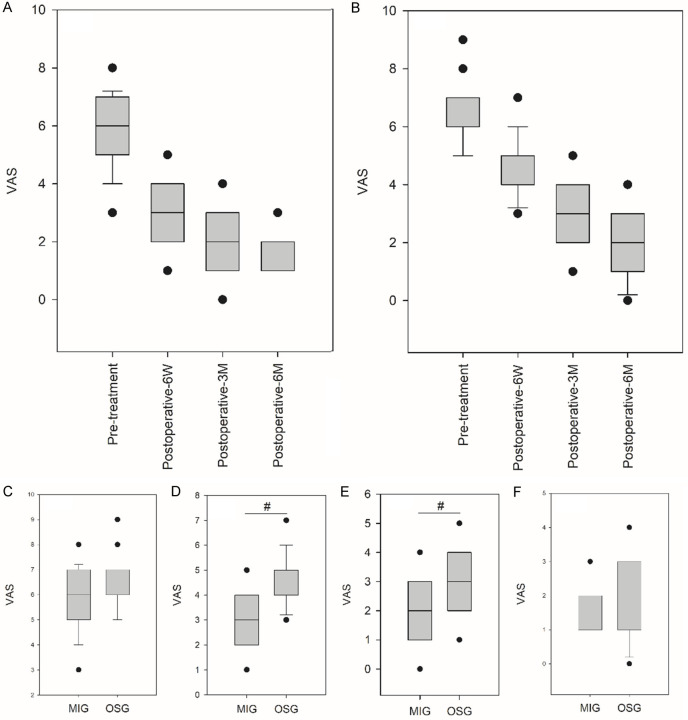
Overall, both the MIG and the OSG showed a decreasing trend in postoperative VAS scores (Figure 2A, 2B). There was no significant difference in preoperative VAS scores between the two groups (P>0.05) (Figure 2C). Follow-up data collected at 6 weeks, 3 months, and 6 months postoperatively were compared between the two groups, revealing that at 6 weeks postoperatively (Figure 2D) and at 3 months postoperatively (Figure 2E), VAS scores in the MIG were significantly lower than those in the OSG (both P<0.05). However, at 6 months postoperatively (Figure 2F), there was no significant difference in VAS scores between the two groups (P>0.05) (Figure 2).
Figure 2.
Comparison of preoperative and postoperative pain intensity between the two groups. (A, B) VAS score in MIG (A) and OSG (B) at pre-treatment, 6 weeks, 3 months and 6 months post-treatment. (C) Comparison of VAS score between the MIG and OSG before treatment. (D) Comparison of VAS score between the MIG and OSG at post-operative 6 weeks. (E) Comparison of VAS score between the MIG and OSG at post-operative 3 months. (F) Comparison of VAS score between the MIG and OSG at post-operative 6 months. # represents a significant difference between groups at the same time point. VAS: Visual Analogue Scale; MIG: minimally invasive group; OSG: open surgery group.
Comparison of preoperative and postoperative CM scores, UCLA scores, and constant scores between the two groups
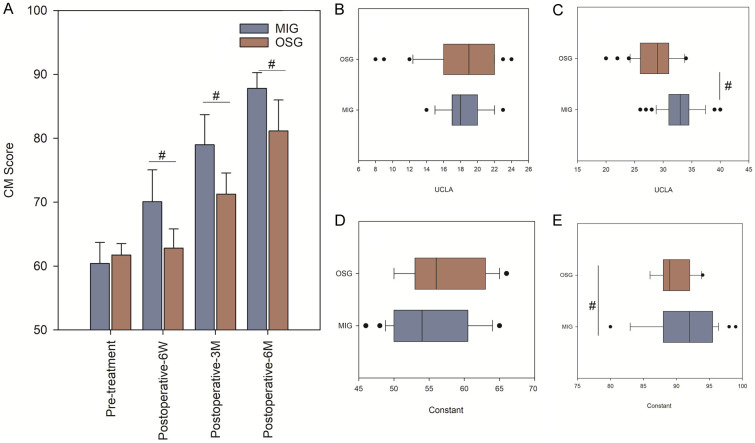
There was no significant difference in preoperative CM scores (Figure 3A), UCLA scores (Figure 3B), and Constant scores (Figure 3D) between the two groups (all P>0.05). However, at 6 weeks, 3 months, and 6 months postoperatively, patients in the MIG reported significantly higher CM scores than those in the OSG (P<0.05) (Figure 3A); at 6 months postoperatively, patients in the MIG demonstrated significantly higher UCLA scores (Figure 3C) and Constant scores (Figure 3E) compared to those in the OSG (both P<0.05) (Figure 3).
Figure 3.
Comparison of preoperative and postoperative CM scores, UCLA scores, and Constant scores between the two groups. (A) Comparison of CM scores at pre-treatment, 6 weeks, 3 months and 6 months post-treatment. (B, D) Comparison of UCLA scores (B) and Constant scores (D) between MIG and OSG before treatment. (C, E) Comparison of UCLA scores (C) and Constant scores (E) between MIG and OSG at the 6 months postoperatively. # represents a statistically significant difference between the groups at the same time point. CM: Constant-Murley; UCLA: University of California-Los Angeles; MIG: minimally invasive group; OSG: open surgery group.
Comparison of preoperative and postoperative shoulder joint function between the two groups
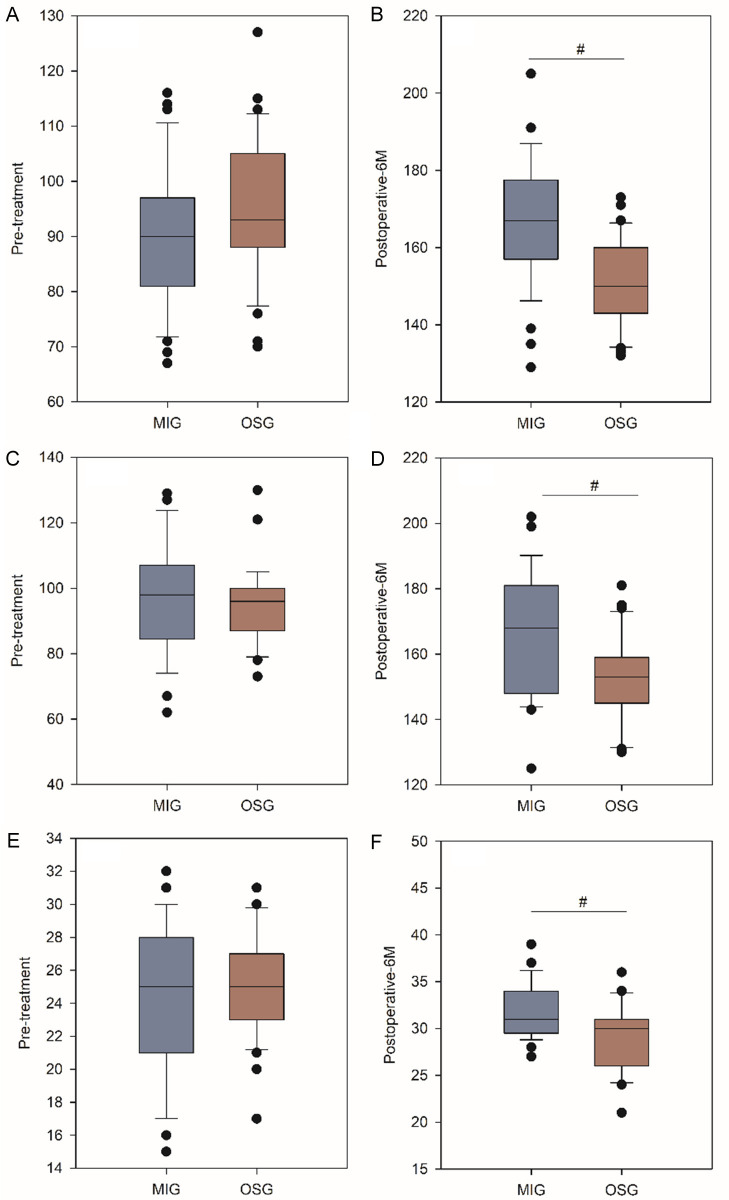
There were no significant differences in preoperative joint forward flexion (Figure 4A), abduction (Figure 4C), and lateral rotation angles (Figure 4E) between the two groups (all P>0.05). However, at the 6-month follow-up, patients in the MIG had significantly greater forward flexion (Figure 4B), abduction (Figure 4D), and lateral rotation angles (Figure 4F) compared to those in the OSG (all P<0.05).
Figure 4.
Comparison of joint forward flexion, abduction, and lateral rotation angles preoperatively and at 6 months postoperatively between the two groups. (A, C, E) Comparison of joint forward flexion (A), abduction (C), and lateral rotation (E) angles between MIG and OSG before treatment. (B, D, F) Comparison of joint forward flexion (B), abduction (D), and lateral rotation (F) angles between MIG and OSG at the 6-month postoperatively. # represents a statistically significant difference between the groups at the same time point. MIG: minimally invasive group; OSG: open surgery group.
Comparison of complications between the two groups
At 6 months postoperatively, the MIG had 2 cases of adhesion healing, 1 case of shoulder swelling, and 1 case of wound infection, with a total complication incidence of 10.81% (4/37), significantly lower than the 25.81% (8/31) observed in the OSG (P<0.05) (Table 2).
Table 2.
Comparison of incidence of complications between the two groups
| Group | Number of cases | Adhesion healing | Shoulder swelling | Wound infection | Total incidence |
|---|---|---|---|---|---|
| MIG | 37 | 2 | 1 | 1 | 4 (10.81) |
| OSG | 31 | 2 | 5 | 1 | 8 (25.81) |
| χ2 | - | - | - | - | 3.569 |
| P | - | - | - | - | 0.003 |
MIG: minimally invasive group; OSG: open surgery group.
Analysis of prognostic factors in patients with moderate rotator cuff tears
To analyze the prognostic factors in patients with moderate rotator cuff tears, postoperative complications were used as the dependent variable (complications =0, no complications =1), and gender, age, tear location, underlying diseases, operative time, hospital stay, incision length, blood loss, preoperative VAS score, and surgical approach were used as independent variables. Univariate analysis indicated that age, classification, and surgical approach were the single factors affecting postoperative complications (P<0.1, Table 3). Further incorporating the aforementioned factors into a binomial logistic regression analysis revealed that the surgical approach was an independent risk factor for postoperative complications (P<0.05, Table 4).
Table 3.
Univariate analysis of prognostic factors in patients with moderate rotator cuff tears
| Variable | B | Standard error | Wald | P | Exp (B) |
|---|---|---|---|---|---|
| Gender | -0.515 | 0.770 | 0.447 | 0.504 | 0.598 |
| Age | -0.099 | 0.042 | 5.691 | 0.017 | 0.906 |
| Tear location | 0.046 | 0.822 | 0.003 | 0.955 | 1.047 |
| Classification | 1.253 | 0.690 | 3.293 | 0.070 | 3.501 |
| Diabetes | -18.441 | 21988.559 | 0.000 | 0.999 | 0.000 |
| Hypertension | 0.611 | 1.025 | 0.355 | 0.551 | 1.841 |
| Operative time | 0.002 | 0.036 | 0.004 | 0.948 | 1.002 |
| Hospital stay | -0.209 | 0.211 | 0.973 | 0.324 | 0.812 |
| Incision length | -0.111 | 0.445 | 0.062 | 0.803 | 0.895 |
| Blood loss | 0.012 | 0.045 | 0.074 | 0.786 | 1.012 |
| Preoperative VAS score | -0.192 | 0.460 | 0.174 | 0.676 | 0.825 |
| Surgical approach | 2.365 | 0.569 | 4.031 | 0.011 | 3.715 |
VAS: Visual Analogue Scale.
Table 4.
Binomial logistic regression analysis of prognostic factors in patients with moderate rotator cuff tears
| Risk factor | B | S.E. | Wald | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| Surgical approach | 1.885 | 0.856 | 4.871 | 0.026 | 6.401 | 1.212-30.265 |
Discussion
In recent years, changes in residents’ lifestyles and increasing work pressures have led to a rise in shoulder joint pain and functional impairments, particularly rotator cuff injuries [18]. Rotator cuff injuries often result from a combination of factors, including muscle tendon tissue degeneration, excessive load accumulation, and minor traumas. These injuries affect daily life and can lead to muscle atrophy, significantly reducing quality of life. Therefore, it is advisable to actively initiate intervention therapy for patients with rotator cuff injuries [19,20].
There remains clinical controversy over the choice of treatment for rotator cuff tears. Some scholars [21] argue that traditional open surgery offers a wider field of view, enabling more comprehensive repairs and potentially benefiting long-term shoulder joint recovery. However, other scholars [22] contend that traditional open surgery causes significant trauma, increasing the risk of postoperative complications such as joint swelling, stiffness, pain, and adhesions, which can negatively impact patient prognosis. This study revealed that compared to traditional open surgery, arthroscopic rotator cuff repair has advantages including reduced intraoperative bleeding, shorter hospital stays, and smaller incision lengths. These findings suggest that arthroscopic procedures result in less trauma and facilitate faster perioperative recovery. Unlike other studies [23], the results of this study indicate that arthroscopic rotator cuff repair requires shorter operative time than open surgery. Factors influencing operative time include the surgeon’s skill level, the type of arthroscope used, and the extent of the patient’s injury. The shorter operative time observed in this study for arthroscopic procedures may be attributed to the surgeon’s extensive experience and thorough arthroscopic exploration.
Further follow-up results indicated that postoperative pain intensity in MIG patients was lower than those in the OSG. The reason for the aforementioned phenomenon can be attributed to the following points. (1) Traditional open surgery has the advantage of a clear intraoperative view, but with larger trauma, leading to a higher incidence of postoperative adhesions in local tissues and joints [24]. These adhesions can induce joint mobility disorders, resulting in pain. (2) The shoulder joint, a large and highly flexible joint in the human body, may experience functional impairments in the early postoperative period. Active postoperative rehabilitation is crucial for accelerating joint recovery. However, open surgery entails significant trauma, making early rehabilitation challenging for patients, who may also subjectively resist such activities. This inadvertently prolongs joint immobilization, ultimately making it difficult to eliminate local inflammation and resulting in persistent pain [25,26].
Joint function is a crucial indicator for assessing surgical out-comes. The comparative results in this study indicated that at the 6-month postoperative follow-up, CM and UCLA scores were significantly higher in the MIG than in the OSG, suggesting superior postoperative shoulder joint function in the MIG. This aligns with other studies [27]. A prospective study involving 48 patients with rotator cuff tears showed that arthroscopic rotator cuff repair improved Constant scores at 1 year and 2 years postoperatively, and this improvement could be attributed to the fact that arthroscopic surgery avoids extensive tendon dissection, preventing secondary injury and enhancing postoperative recovery [28]. Recent advancements in imaging technology have enabled arthroscopic rotator cuff repair to sufficiently decompress the subacromial space, preserve the deltoid insertion, and perform tension-free repair, facilitating postoperative joint function recovery [29]. Additionally, the high flexibility of arthroscopy allows for thorough exploration and timely repair of the glenohumeral joint, synergizing with rotator cuff repair to lay a solid foundation for postoperative joint function recovery [30]. Finally, the range of motion in the two groups at the 6-month follow-up corroborated this viewpoint, indicating that arthroscopic rotator cuff repair significantly enhances postoperative joint range of motion, which is crucial for improving patients’ quality of life.
Arthroscopic rotator cuff repair for patients with rotator cuff tears involves minimal trauma and promotes rapid postoperative recovery. This procedure also helps restore shoulder joint function and improve the range of motion, showing promising clinical application prospects. Inevitably, this study still has limitations, including its retrospective nature, short follow-up duration, and single-center study design, which may lead to biased results. Future large-scale, multi-center prospective studies would enhance the applicability of the findings.
Disclosure of conflict of interest
None.
References
- 1.Narvani AA, Imam MA, Godenèche A, Calvo E, Corbett S, Wallace AL, Itoi E. Degenerative rotator cuff tear, repair or not repair? A review of current evidence. Ann R Coll Surg Engl. 2020;102:248–255. doi: 10.1308/rcsann.2019.0173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agha O, Diaz A, Davies M, Kim HT, Liu X, Feeley BT. Rotator cuff tear degeneration and the role of fibro-adipogenic progenitors. Ann N Y Acad Sci. 2021;1490:13–28. doi: 10.1111/nyas.14437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCrum E. MR imaging of the rotator cuff. Magn Reson Imaging Clin N Am. 2020;28:165–179. doi: 10.1016/j.mric.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 4.Plancher KD, Shanmugam J, Briggs K, Petterson SC. Diagnosis and management of partial thickness rotator cuff tears: a comprehensive review. J Am Acad Orthop Surg. 2021;29:1031–1043. doi: 10.5435/JAAOS-D-20-01092. [DOI] [PubMed] [Google Scholar]
- 5.Lafrance S, Charron M, Roy JS, Dyer JO, Frémont P, Dionne CE, Macdermid JC, Tousignant M, Rochette A, Doiron-Cadrin P, Lowry V, Bureau N, Lamontagne M, Sandman E, Coutu MF, Lavigne P, Desmeules F. Diagnosing, managing, and supporting return to work of adults with rotator cuff disorders: a clinical practice guideline. J Orthop Sports Phys Ther. 2022;52:647–664. doi: 10.2519/jospt.2022.11306. [DOI] [PubMed] [Google Scholar]
- 6.Ganokroj P, Peebles AM, Vopat ML, Provencher MT. Superior capsular reconstruction for irreparable rotator cuff tear. Clin Sports Med. 2023;42:109–124. doi: 10.1016/j.csm.2022.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Longo UG, Risi Ambrogioni L, Candela V, Berton A, Carnevale A, Schena E, Denaro V. Conservative versus surgical management for patients with rotator cuff tears: a systematic review and META-analysis. BMC Musculoskelet Disord. 2021;22:50. doi: 10.1186/s12891-020-03872-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nyffeler RW, Schenk N, Bissig P. Can a simple fall cause a rotator cuff tear? Literature review and biomechanical considerations. Int Orthop. 2021;45:1573–1582. doi: 10.1007/s00264-021-05012-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Longo UG, Carnevale A, Piergentili I, Berton A, Candela V, Schena E, Denaro V. Retear rates after rotator cuff surgery: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2021;22:749. doi: 10.1186/s12891-021-04634-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuan FC, Shih CA, Su WR, Garcia AV, Kuroiwa T, Iida N, Hsu KL. Definition of irreparable rotator cuff tear: a scoping review of prospective surgical therapeutic trials to evaluate current practice. BMC Musculoskelet Disord. 2023;24:952. doi: 10.1186/s12891-023-07067-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shepet KH, Liechti DJ, Kuhn JE. Nonoperative treatment of chronic, massive irreparable rotator cuff tears: a systematic review with synthesis of a standardized rehabilitation protocol. J Shoulder Elbow Surg. 2021;30:1431–1444. doi: 10.1016/j.jse.2020.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Huang DG, Wu YL, Chen PF, Xia CL, Lin ZJ, Song JQ. Surgical or nonsurgical treatment for nontraumatic rotator cuff tears: study protocol clinical trial. Medicine (Baltimore) 2020;99:e20027. doi: 10.1097/MD.0000000000020027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davies MR, Chi H, Kaur G, Liu M, Ma CB, Kim HT, Liu X, Feeley BT. Rotator cuff tear size regulates fibroadipogenic progenitor number and gene expression profile in the supraspinatus independent of patient age. Am J Sports Med. 2022;50:208–215. doi: 10.1177/03635465211054512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ruderman L, Leinroth A, Rueckert H, Tabarestani T, Baker R, Levin J, Cook CE, Klifto CS, Hilton MJ, Anakwenze O. Histologic differences in human rotator cuff muscle based on tear characteristics. J Bone Joint Surg Am. 2022;104:1148–1156. doi: 10.2106/JBJS.21.01304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hwang WY, Kim K, Cho HY, Yang EJ, Suh DH, No JH, Lee JR, Hwang JW, Do SH, Kim YB. The voiding VAS score is a simple and useful method for predicting POUR after laparoscopy for benign gynaecologic diseases: a pilot study. J Obstet Gynaecol. 2022;42:2469–2473. doi: 10.1080/01443615.2022.2071149. [DOI] [PubMed] [Google Scholar]
- 16.Hollman F, de Raadt WM, Wolterbeek N, van Rhijn LW, Auw Yang KG. Interchangeability of diverse analog scales used within the constant-murley score. Arthrosc Sports Med Rehabil. 2021;3:e521–e526. doi: 10.1016/j.asmr.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu S, Chen JY, Hao Y, Chang CCP, Lie DTT. Threshold scores for treatment success after arthroscopic bankart repair using Oxford Shoulder Instability Score, Constant-Murley Score, and UCLA shoulder score. J Orthop. 2020;22:242–245. doi: 10.1016/j.jor.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mancini MR, Horinek JL, Phillips CJ, Denard PJ. Arthroscopic rotator cuff repair: a review of surgical techniques and outcomes. Clin Sports Med. 2023;42:81–94. doi: 10.1016/j.csm.2022.08.004. [DOI] [PubMed] [Google Scholar]
- 19.Morgan CN, Bonner KF, Griffin JW. Augmentation of arthroscopic rotator cuff repair: biologics and grafts. Clin Sports Med. 2023;42:95–107. doi: 10.1016/j.csm.2022.08.010. [DOI] [PubMed] [Google Scholar]
- 20.Migliorini F, Maffulli N, Eschweiler J, Schenker H, Tingart M, Betsch M. Arthroscopic versus mini-open rotator cuff repair: a meta-analysis. Surgeon. 2023;21:e1–e12. doi: 10.1016/j.surge.2021.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Zhao J, Luo M, Pan J, Liang G, Feng W, Zeng L, Yang W, Liu J. Risk factors affecting rotator cuff retear after arthroscopic repair: a meta-analysis and systematic review. J Shoulder Elbow Surg. 2021;30:2660–2670. doi: 10.1016/j.jse.2021.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Berthold DP, Garvin P, Mancini MR, Uyeki CL, LeVasseur MR, Mazzocca AD, Voss A. Arthroscopic rotator cuff repair with biologically enhanced patch augmentation. Oper Orthop Traumatol. 2022;34:4–12. doi: 10.1007/s00064-021-00754-3. [DOI] [PubMed] [Google Scholar]
- 23.Davey MS, Hurley ET, Carroll PJ, Galbraith JG, Shannon F, Kaar K, Mullett H. Arthroscopic rotator cuff repair results in improved clinical outcomes and low revision rates at 10-year follow-up: a systematic review. Arthroscopy. 2023;39:452–458. doi: 10.1016/j.arthro.2022.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Harada Y, Yokoya S, Sumimoto Y, Adachi N. Clinical outcomes and tendon lengthening after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2023;32:1214–1221. doi: 10.1016/j.jse.2022.11.013. [DOI] [PubMed] [Google Scholar]
- 25.Stenson J, Sanders B, Lazarus M, Austin L. Arthroscopic transosseous rotator cuff repair. J Am Acad Orthop Surg. 2023;31:e366–e375. doi: 10.5435/JAAOS-D-22-00057. [DOI] [PubMed] [Google Scholar]
- 26.He L, Li Y, Liao X, Wang Y, Pu L, Gao F, Wang G. Effects of evidence-based nursing combined with enhanced recovery after surgery on shoulder joint function and neurological function after arthroscopic rotator cuff injury repair. Medicine (Baltimore) 2021;100:e27951. doi: 10.1097/MD.0000000000027951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Theosmy EG, Bradian AK, Cheesman QT, Radack TM, Lazarus MD, Austin LS. Opioid-free arthroscopic rotator cuff repair. Orthopedics. 2021;44:e301–e305. doi: 10.3928/01477447-20201216-03. [DOI] [PubMed] [Google Scholar]
- 28.Lapner P, Bouliane M, Pollock JW, Coupal S, Sabri E, Hodgdon T, Old J, McIlquham K, MacDonald P, Stranges G, Berdusco R, Marsh J, Dubberley J, McRae S. Intraoperative channeling in arthroscopic rotator cuff repair: a multicenter randomized controlled trial. Am J Sports Med. 2023;51:323–330. doi: 10.1177/03635465221138562. [DOI] [PubMed] [Google Scholar]
- 29.Han C, Liu M, Lian X, Sun T, Yan S, Bai X, Gan D, Leng B, Qiu Y, Ren Y. Tranexamic acid use in arthroscopic rotator cuff repair is an effective and safe adjunct to improve visualization: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2023;32:2389–2399. doi: 10.1016/j.jse.2023.06.013. [DOI] [PubMed] [Google Scholar]
- 30.Sandow MJ, Schutz CR. Arthroscopic rotator cuff repair using a transosseous knotless anchor (ATOK) J Shoulder Elbow Surg. 2020;29:527–533. doi: 10.1016/j.jse.2019.07.017. [DOI] [PubMed] [Google Scholar]