Abstract
Objectives: To investigate the effect of nursing risk management in cardiovascular interventional catheterization rooms, reduce perioperative complications and enhance treatment outcomes. Methods: This retrospective study included 60 patients who underwent cardiovascular interventional surgery at the Fourth Affiliated Hospital of Soochow University from January 2023 to January 2024. Patients were divided into two groups based on the nursing approach received. The observation group (n=32) received nursing risk management intervention, while the control group (n=28) received routine nursing care. Outcomes compared included psychological status, nursing satisfaction, postoperative complications, and general clinical information. Results: Both groups showed significant reductions in Self-Rating Anxiety Scale and Self-Rating Depression Scale scores, with the observation group achieving lower scores post-intervention (both P<0.05). Nursing satisfaction was higher in the observation group (93.75%) compared to the control group (78.57%) (P<0.05). The rate of postoperative complications was lower in the observation group (6.2% vs. 17.9%) (P=0.047). Multiple regression analysis identified urinary retention (P=0.007) and nursing risk management (P<0.001) as independent factors influencing patients’ psychological status. Conclusion: Nursing risk management in cardiovascular interventional catheterization rooms can reduce anxiety and depression, decrease postoperative complications, and improve nursing satisfaction.
Keywords: Nursing risk management, perioperative nursing, cardiovascular interventional catheter room
Introduction
Cardiovascular interventional catheterization rooms play a crucial role in diagnosing and treating various cardiovascular conditions [1]. These specialized facilities are equipped with advanced imaging technology and interventional tools that enable healthcare providers to perform minimally invasive procedures for diagnosing and treating heart and blood vessel diseases [2]. These procedures often involve small incisions or catheters inserted through blood vessels, reducing the need for open surgery and promoting faster recovery times [3]. The advanced imaging technology in catheterization rooms provides real-time visualization of the heart and blood vessels, allowing for precise diagnosis and treatment of cardiovascular conditions [4]. By offering minimally invasive procedures and precise treatments, catheterization rooms can improve patient outcomes, reduce complications, and enhance the overall quality of care for individuals with cardiovascular diseases [5]. Due to the invasive nature of cardiovascular interventions, there is a higher risk of emergent situations and serious complications during the perioperative period. Cardiovascular intervention catheterization is conducted by a specialized department that manages patients with high nursing risks, limited self-care abilities, and complex nursing needs. Therefore, patients undergoing cardiovascular interventions are more likely to experience nursing risks and emergencies. Strengthening nursing interventions is essential in these settings [6,7].
Nursing risk management is a critical aspect of clinical practice, aiming to identify, assess, and mitigate potential risks to patient safety and the quality of care. In clinical settings, nursing risk management involves various strategies to prevent adverse events, errors, and harm to patients. This includes implementing protocols and guidelines, conducting risk assessments, monitoring patient outcomes, and fostering a culture of safety within healthcare organizations [8]. Current research in nursing risk management focuses on developing evidence-based practices and tools to enhance patient safety and reduce risks in clinical settings. Studies are exploring the effectiveness of different risk management strategies, such as error reporting systems, simulation training, and interdisciplinary collaboration, in improving patient outcomes and reducing adverse events [9,10]. Researchers are also investigating the impact of organizational factors, such as staffing levels, workload, and communication, on nursing risk management practices and patient safety [11,12].
Therefore, the aim of this study was to investigate the effect of nursing risk management in cardiovascular interventional catheterization rooms, with a focus on reducing perioperative complications and ensuring effective treatment.
Materials and methods
Study design
This retrospective study included 60 patients who underwent cardiovascular intervention surgery at the Fourth Affiliated Hospital of Soochow University from January 2023 to January 2024. The patients were divided into two groups based on the nursing care they received. The observation group (n=32) received nursing risk management intervention, while the control group (n=28) received routine nursing care. The study was approved by the local institutional review board of the Fourth Affiliated Hospital of Soochow University.
Inclusion and exclusion criteria
Inclusion criteria: (1) Laboratory and imaging examinations consistent with clinical indications for cardiovascular intervention surgery [13]. (2) No recent history of cardiovascular surgery. (3) Normal cognition and high compliance.
Exclusion criteria: (1) Severe liver function impairment. (2) Severe renal insufficiency. (3) Presence of systemic infection. (4) Thrombocytopenia or coagulation dysfunction. (5) Carotid artery stenosis. (6) Pregnant or lactating women.
Methods
The control group received routine nursing care, which included: (1) Monitoring basic vital signs after admission. (2) Providing health education to patients and their families. (3) Offering psychological counseling to prevent fear, anxiety, and other negative emotions. (4) Giving basic lifestyle guidance. (5) Administering medication, managing complications, and caring for medical equipment.
The observation group received nursing risk management intervention, which included: (1) Health education: Many patients have limited understanding of cardiovascular intervention therapy, often leading to misconceptions and rejection of treatment. Nursing staff provided personalized, one-on-one explanations to clarify the benefits and value of the therapy, described the surgical process to patients and their families, and encouraged active participation in the treatment. (2) Psychological counseling: Patients often experience anxiety and fear during intervention therapy. Nursing staff maintained open communication with patients in the cardiovascular intervention catheterization room, helped alleviate psychological stress, bolstered their confidence in the treatment, and ensured close cooperation throughout the procedure. (3) Intraoperative nursing: Nursing staff maintained a comfortable surgical environment with appropriate temperature (22°C to 25°C) and relative humidity (45% to 60%). They closely monitored the patient’s condition during surgery, ensured the patient was kept warm, and pre-warmed all intravenous infusion fluids to reduce the risk of hypothermia-related events. Staff also remained vigilant for any changes in the patient’s condition and addressed issues promptly.
Observation indicators
The primary outcomes included psychological state and postoperative complications. The Self-Rating Anxiety Scale (SAS) [14] and Self-Rating Depression Scale (SDS) [15] were used to assess the psychological state of the patients. Both scales range from 0 to 100, with higher scores indicating more severe anxiety and depressive symptoms. The Cronbach’s alpha for SAS and SDS were 0.89 and 0.87, respectively. Postoperative complications included urinary retention, ventricular fibrillation, and hematoma formation.
The secondary outcomes included general clinical information, sleep quality, quality of life, and nursing satisfaction. Nursing satisfaction was assessed using a self-developed scale based on the Newcastle Nursing Satisfaction Scale (NSNS) [16]. This questionnaire evaluated 10 aspects of patient satisfaction, with a maximum score of 50. Scores were categorized as follows: 50 points indicated very satisfied, 45-49 points indicated satisfied, 35-44 points indicated fair, and less than 35 points indicated unsatisfied. Nursing care satisfaction (%) was calculated as (number of very satisfied cases + number of satisfied cases)/total number of cases × 100%. Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI), developed by Buysse [17]. The PSQI includes 23 items, 18 of which are scored on a scale of 0 to 3. The total score ranges from 0 to 21, with higher scores indicating poorer sleep quality. Quality of life was assessed using the SF-36 questionnaire [18], developed by the American Medical Outcomes Research Group in 1992. The SF-36 includes eight dimensions: physical function, psychological function, physical pain, emotional function, social function, and mental health. Scores for each dimension were calculated and converted into a standardized score ranging from 0 to 100, with higher scores indicating a better quality of life.
Statistical analysis
SPSS 22.0 software was used for statistical analysis. The sample size was calculated using power analysis, with the final sample size determined to be approximately 60 after accounting for attrition [19]. The number of patients in the two groups was determined through careful screening and statistical analysis of the medical database, based on specific inclusion and exclusion criteria, resulting in 32 cases in the observation group and 28 cases in the control group. Measurement data were expressed as mean ± standard deviation (x±sd), and independent samples t-tests were used for between-group comparisons, while paired t-tests were used for within-group comparisons. Categorical data were expressed as percentages (%), and the χ2 test was used for comparisons. A difference was considered statistically significant at P<0.05.
Results
Comparison of clinical characteristics between the two groups
There were no statistically significant differences between the two groups in terms of age, gender, BMI, smoking history, marital status, cardiovascular diseases, and past medical history (all P>0.05), indicating that the groups were comparable (Table 1).
Table 1.
Comparison of clinical characteristics between the two groups
| Observation group (n=32) | Control group (n=28) | t/χ2 | P | |
|---|---|---|---|---|
| Age (years) | 41.05±7.91 | 40.35±7.19 | 0.397 | 0.692 |
| Sex | 1.361 | 0.176 | ||
| Male (n%) | 18 (56.3%) | 17 (60.7%) | ||
| Female (n%) | 14 (43.7%) | 11 (39.3%) | ||
| Body mass index | 20.7±2.28 | 20.4±2.76 | 1.808 | 0.073 |
| Smoking | 22 (68.8%) | 20 (71.4%) | 1.209 | 0.229 |
| Marital status | 0.333 | 0.739 | ||
| Married | 10 (31.3%) | 9 (32.1%) | ||
| Single | 11 (34.4%) | 8 (28.6%) | ||
| Divorced or separated | 8 (25%) | 7 (25%) | ||
| Widowed | 1 (3.1%) | 2 (7.1%) | ||
| Unknown/missing | 2 (6.2%) | 2 (7.1%) | ||
| Diabetes | 17 (53.1%) | 15 (53.6%) | 1.005 | 0.317 |
| Hypertension | 8 (25%) | 7 (25.0%) | 0.392 | 0.696 |
| Chronic obstructive pulmonary disease | 5 (15.6%) | 4 (14/3%) | 0.965 | 0.326 |
| Cardiovascular diseases | 0.867 | 0.443 | ||
| Coronary heart disease | 22 (68.8%) | 20 (71.4%) | ||
| Congenital heart disease | 5 (15.6%) | 4 (14/3%) | ||
| Arrhythmia | 2 (6.25%) | 2 (7.1%) | ||
| Aortic valve stenosis | 2 (6.2%) | 2 (7.1%) |
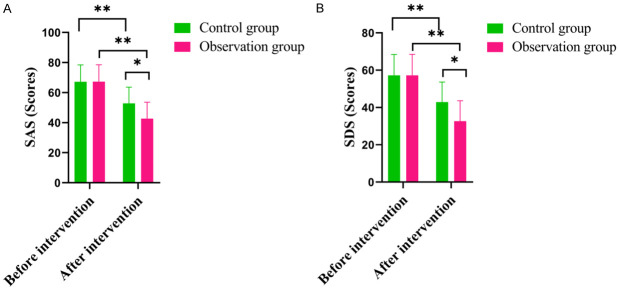
Comparison of psychological status between the two groups
Before the intervention, the SAS and SDS scores were similar between the two groups. After the intervention, both groups showed a significant decrease in SAS/SDS scores, with the observation group having significantly lower scores (both P<0.05) (Figure 1).
Figure 1.
Comparison of psychological status between the two groups. A: Self-Anxiety Scale (SAS); B: Self-Depression Scale (SDS). *P<0.05, **P<0.01, compared to the control group.
Comparison of nursing satisfaction between the two groups
In the observation group, 10 patients were basically satisfied with their nursing care, compared to 5 patients in the control group. The satisfaction rate in the observation group was 93.75%, significantly higher than in the control group (78.57%) (P<0.05) (Table 2).
Table 2.
Comparison of nursing satisfaction between the two groups [cases (%)]
| Basically Satisfaction | Satisfaction | Very Satisfaction | Satisfaction Rate | |
|---|---|---|---|---|
| Observation group (n=32) | 10 (31.25%) | 17 (53.1%) | 3 (9.4%) | 30 (93.75%) |
| Control group (n=28) | 5 (17.86%) | 15 (53.6%) | 2 (7.2%) | 22 (78.57%) |
| t | 6.42 | 2.93 | 3.39 | 5.17 |
| P | 0.041 | 0.74 | 0.33 | 0.02 |
Comparison of postoperative complication between the two groups
The incidence of urinary retention, ventricular fibrillation, and hematoma formation was higher in the control group compared to the observation group. The total incidence of postoperative complications in the observation group was significantly lower than in the control group (6.2% vs. 17.9%), with a statistically significant difference (P=0.047) (Table 3).
Table 3.
Comparison of postoperative complication between the two groups [cases (%)]
| Urinary retention | Ventricular fibrillation | Bleeding hematoma | Total occurrence rate | |
|---|---|---|---|---|
| Observation group (n=32) | 0 (0.0%) | 1 (3.1%) | 1 (3.1%) | 2 (6.2%) |
| Control group (n=28) | 1 (3.6%) | 2 (7.1%) | 2 (7.1%) | 5 (17.9%) |
| T | - | - | - | 7.987 |
| P | - | - | - | 0.047 |
Comparison of sleep quality between the two groups
After the intervention, the PSQI scores in both groups were lower than before the intervention, with the observation group showing significantly greater improvement in PSQI scores compared to the control group (8.05±1.91 vs. 10.35±1.19, P<0.001) (Table 4).
Table 4.
Comparison of sleep quality between the two groups
| Observation group (n=32) | Control group (n=28) | t | P | |
|---|---|---|---|---|
| Before intervention | 18.05±3.91 | 18.35±3.19 | 0.188 | 0.876 |
| After intervention | 8.05±1.91 | 10.35±1.19 | 8.076 | <0.001 |
| t | 5.911 | 2.917 | - | - |
| p | 0.011 | 0.038 | - | - |
Comparison of quality of life between the two groups
Compared to the control group, the observation group had higher scores in physical function, psychological function, social function, and material function after the intervention, with significant differences between the two groups (P<0.05) (all Figure 2).
Figure 2.
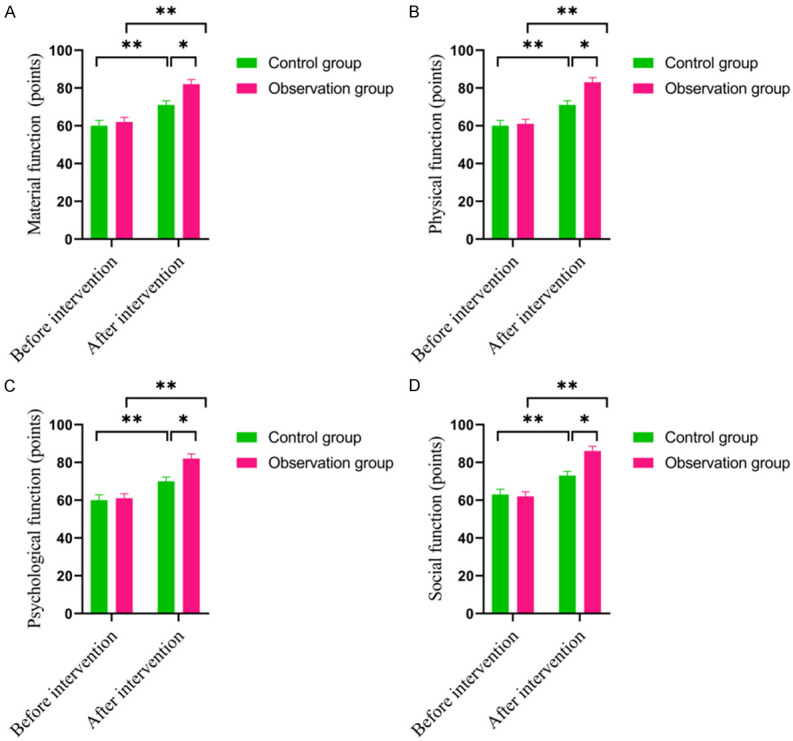
Comparison of quality of life between the two groups. A: Material function; B: Physical function; C: Psychological function; D: Social function. *P<0.05, **P<0.01, compared to the control group.
Relationship between patients’ psychological state and independent variables
Regression analysis showed that being divorced or separated, widowed, undergoing nursing risk management, and experiencing urinary retention were significantly correlated with patients’ psychological state. Factors such as age, BMI, smoking, marital status, ventricular fibrillation, hematoma formation, diabetes, hypertension, and chronic obstructive pulmonary disease did not show significant correlations with patients’ psychological state (Table 5).
Table 5.
Relationship between patients’ psychological state and independent variables
| Indexes | Rho | P |
|---|---|---|
| Age | -0.038 | 0.543 |
| Body mass index (kg/m2) | 0.035 | 0.610 |
| Smoking | 0.010 | 0.868 |
| Married (Marital status) | -0.071 | 0.454 |
| Single (Marital status) | -0.070 | 0.461 |
| Divorced or separated (Marital status) | 0.138 | 0.025 |
| Widowed (Marital status) | 0.139 | 0.027 |
| Nursing risk management | 0.262 | <0.001 |
| Urinary retention | 0.178 | 0.006 |
| Ventricular fibrillation | 0.174 | 0.064 |
| Bleeding hematoma | -0.043 | 0.743 |
| Diabetes | 0.276 | 0.073 |
| Hypertension | 0.276 | 0.073 |
| Chronic obstructive pulmonary disease | 0.174 | 0.064 |
Note: The person correlation analysis method is used for normal distribution data and Spearman correlation analysis method is used for non-normal distribution data.
Multiple regression analysis
Multiple regression analysis identified urinary retention (P=0.007) and nursing risk management (P<0.001) as independent factors, with both showing statistically significant differences (P<0.05) (Table 6).
Table 6.
Multiple regression analysis
| Dependent variables | Independent variables | B | SE | β | P Value | OR (95% CI) |
|---|---|---|---|---|---|---|
| Patients’ psychology state | Urinary retention | 0.85 | 0.32 | 7.15 | 0.007 | 2.35 (1.26-4.38) |
| Nursing risk management | 1.39 | 0.39 | 12.76 | <0.001 | 4.02 (1.87-8.62) |
Note: B: nonstandard regression coefficient; SE: standard error; b: standardized regression coefficient; β: multiple correlation coefficient adjusted for the degrees of freedom.
Discussion
Our study found that nursing risk management intervention significantly improved psychological status, increased nursing satisfaction, and reduced the incidence of postoperative complications. The catheterization room requires substantial medical resources, and patients’ demands for medical services are rising. Improving the quality of nursing care in the catheterization room has become a critical task. The catheterization room is primarily responsible for the treatment and care of cardiovascular diseases, with many patients being elderly and presenting with rapidly progressing, urgent, and severe conditions [20]. Clinical studies have demonstrated that effective nursing risk management is essential during the clinical treatment process to reduce complications and improve patient outcomes [21]. Nursing risk management in the catheterization room is crucial. In clinical practice, comprehensive nursing risk control, along with personalized care, should be implemented to minimize adverse reactions and complications [22]. Nursing risk management intervention involves targeted nursing plans developed by a clinical nursing pathway team based on the specific conditions of patients, which aids in their recovery. As a new approach, nursing risk management is increasingly valued in clinical practice, as it supports the implementation of various responsibility systems [23]. Implementing nursing risk management in the catheterization room can enhance the nursing management system, improve nurses’ work efficiency, reduce departmental nursing risks, and increase work satisfaction.
In our research, we observed that the implementation of nursing risk management led to a significant decrease in patients’ SAS and SDS scores, aligning with the findings of Jim’s study [24]. Effective risk management strategies often include enhanced communication between healthcare providers and patients. Clear communication helps reduce patient anxiety by providing a better understanding of procedures and potential outcomes, thereby minimizing uncertainty and fear [25]. Implementing risk management strategies can also empower patients by involving them in decision-making processes and providing the necessary information and resources to actively participate in their care [26]. Empowered patients are more likely to feel in control of their situation, which can decrease feelings of helplessness and anxiety [27]. Additionally, risk management involves ongoing monitoring and assessment of patients’ emotional well-being throughout their care journey. By regularly checking in with patients and addressing any concerns or changes in their mental health, healthcare providers can intervene early and prevent the escalation of anxiety and depression symptoms [28].
Furthermore, our study found that nursing satisfaction significantly improved following the implementation of nursing risk management. Risk management protocols can streamline processes and enhance efficiency in the cardiovascular intervention catheterization room. By identifying and mitigating potential risks, nurses can focus more on delivering quality care, leading to higher job satisfaction [29]. Additionally, a robust risk management program fosters better communication and teamwork among healthcare providers. When all team members are aligned on potential risks and strategies to address them, collaboration and trust are strengthened, resulting in a more positive work environment [30]. Prioritizing risk management in the catheterization room equips nurses to provide higher-quality care, thereby increasing job satisfaction and overall nursing satisfaction in the workplace.
In summary, the implementation of nursing risk management in cardiovascular intervention catheterization rooms can effectively reduce patient anxiety and depression, decrease postoperative complications, and enhance nursing satisfaction, demonstrating its high application value.
Disclosure of conflict of interest
None.
References
- 1.Rogers T, Campbell-Washburn AE, Ramasawmy R, Yildirim DK, Bruce CG, Grant LP, Stine AM, Kolandaivelu A, Herzka DA, Ratnayaka K, Lederman RJ. Interventional cardiovascular magnetic resonance: state-of-the-art. J Cardiovasc Magn Reson. 2023;25:48. doi: 10.1186/s12968-023-00956-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vergara-Escudero E, Gherciuc A, Buyck D, Eid A, Arango S, Richardson S, Perry TE. Initial experience of using first-person wearable video recording technology during central venous catheter placement in the cardiac operating room. J Cardiothorac Vasc Anesth. 2024;38:1409–1416. doi: 10.1053/j.jvca.2024.02.038. [DOI] [PubMed] [Google Scholar]
- 3.Steffel J, Wright DJ, Schäfer H, Rashid-Fadel T, Lewalter T. Insertion of miniaturized cardiac monitors outside the catheter operating room: experience and practical advice. Europace. 2017;19:1624–1629. doi: 10.1093/europace/euw304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li L, Lin P, Gao X. Health-related quality of life in children and adolescents living in the north-east of China before and after cardiac catheter interventional treatment. Cardiol Young. 2017;27:1118–1122. doi: 10.1017/S104795111600247X. [DOI] [PubMed] [Google Scholar]
- 5.Lin H, Luo S, Chen Y, Guo H. The clinical practice of “mind and body simultaneous nursing” mode in interventional catheter room. J Interv Radiol. 2012;21:608–610. [Google Scholar]
- 6.White K, Macfarlane H, Hoffmann B, Sirvas-Brown H, Hines K, Rolley JX, Graham S. Consensus statement of standards for interventional cardiovascular nursing practice. Heart Lung Circ. 2018;27:535–551. doi: 10.1016/j.hlc.2017.10.022. [DOI] [PubMed] [Google Scholar]
- 7.Lisanti AJ, Fitzgerald J, Helman S, Dean S, Sorbello A, Griffis H. Nursing practice with transthoracic intracardiac catheters in children: international benchmarking study. Am J Crit Care. 2019;28:174–181. doi: 10.4037/ajcc2019350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li D, Liu Y, Pan M, Zhao L. Application and effect evaluation of nursing risk management in nursing of cardiovascular medicine. Contrast Media Mol Imaging. 2022;2022:9253868. doi: 10.1155/2022/9253868. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9.Fabrizzio GC, Erdmann AL, Santos JLGD. Theoretical model for management of nursing research groups. Rev Gaucha Enferm. 2023;44:e20220254. doi: 10.1590/1983-1447.2023.20220254.en. [DOI] [PubMed] [Google Scholar]
- 10.Xiaoyu L, Jinxue L, Fengqiong J, Yan Z, Qiaohua Y. Development and application of nursing risk management evaluation system. Stud Health Technol Inform. 2021;284:414–420. doi: 10.3233/SHTI210761. [DOI] [PubMed] [Google Scholar]
- 11.Teigné D, Mabileau G, Lucas M, Moret L, Terrien N. Safety culture in French nursing homes: a randomised controlled study to evaluate the effectiveness of a risk management intervention associated with care. PLoS One. 2022;17:e0277121. doi: 10.1371/journal.pone.0277121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wei W, Gan M, Liu Y, Yang M, Liu J. Mediating effects of nurses ‘personal and organizational values between organizational commitment and turnover: cross-sectional study. PLoS One. 2021;16:e0258387. doi: 10.1371/journal.pone.0258387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuno T, Kiyohara Y, Maehara A, Ueyama HA, Kampaktsis PN, Takagi H, Mehran R, Stone GW, Bhatt DL, Mintz GS, Bangalore S. Comparison of intravascular imaging, functional, or angiographically guided coronary intervention. J Am Coll Cardiol. 2023;82:2167–2176. doi: 10.1016/j.jacc.2023.09.823. [DOI] [PubMed] [Google Scholar]
- 14.Dunstan DA, Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatry. 2020;20:90. doi: 10.1186/s12888-019-2427-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tung VS, Thong NV, Mai NP, Linh LT, Son DC, Ha TT, Hoa NT, Long NT, Tuan NV. Diagnostic value in screening severe depression of the hamilton depression rating scale, hamilton anxiety rating scale, beck depression inventory scale, and Zung’s self-rating anxiety scale among patients with recurrent depression disorder. Acta Inform Med. 2023;31:249–253. doi: 10.5455/aim.2023.31.249-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodríguez-Herrera C, López-Jiménez JJ, Del Toro-Valero A, Torres-Carrillo NM, Torres-Carrillo N, Godínez-Peña CA, Méndez-Magaña AC, Herrera-Godina MG, Fletes-Rayas AL. The Newcastle satisfaction with nursing scales in a Mexican Oncology Hospital. Afr Health Sci. 2021;21:60–66. doi: 10.4314/ahs.v21i1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Y, Muthurangu V, Wurdemann HA. Toward autonomous pulmonary artery catheterization: a learning-based robotic navigation system. Annu Int Conf IEEE Eng Med Biol Soc. 2023;2023:1–5. doi: 10.1109/EMBC40787.2023.10340140. [DOI] [PubMed] [Google Scholar]
- 18.Wu YY, Yang YJ. Safe management strategy for nursing of emergency interventional surgery in the catheterization room. Chinese Journal of Integrative Nursing. 2021;7:87. [Google Scholar]
- 19.Yang CF, Xiong H, Li M, Liu YY. The impact of patient education on the nursing care of perioperative patients in the interventional catheterization room. J Clin Nurs Res. 2024;8:19–24. [Google Scholar]
- 20.Xu J. The effect of quality control circle nursing mode on reducing infection and improving nursing quality during PICC catheterization in cardiothoracic surgery. Int J Nurs. 2019;38:2229–2232. [Google Scholar]
- 21.The Lancet. Physician burnout: the need to rehumanise health systems. Lancet. 2019;394:1591. doi: 10.1016/S0140-6736(19)32669-8. [DOI] [PubMed] [Google Scholar]
- 22.Zhang J, Feng ZX. Application of strengthening the management of nosocomial infection at improving the quality of nursing management in operating room. China Medical Herald. 2013;10:145–147. [Google Scholar]
- 23.Street M, Phillips NM, Haesler E, Kent B. Refining nursing assessment and management with a new postanaesthetic care discharge tool to minimize surgical patient risk. J Adv Nurs. 2018;74:2566–2576. doi: 10.1111/jan.13779. [DOI] [PubMed] [Google Scholar]
- 24.Jim A. Strategic healthcare change: balancing change and stability. J Healthc Manag. 2023;68:9–14. doi: 10.1097/JHM-D-22-00228. [DOI] [PubMed] [Google Scholar]
- 25.Hickey E, Man B, Helm KVT, Lockhart S, Duffecy J, Morris MA. Preferred communication strategies for people with communication disabilities in health care encounters: a qualitative study. J Gen Intern Med. 2024;39:790–797. doi: 10.1007/s11606-023-08526-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swift JK, Mullins RH, Penix EA, Roth KL, Trusty WT. The importance of listening to patient preferences when making mental health care decisions. World Psychiatry. 2021;20:316–317. doi: 10.1002/wps.20912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Wit M, Cooper C, Reginster JY WHO-ESCEO Working Group. Practical guidance for patient-centred health research. Lancet. 2019;393:1095–1096. doi: 10.1016/S0140-6736(19)30034-0. [DOI] [PubMed] [Google Scholar]
- 28.Scott J, Stewart J. Interventional nurses raising the bar in the cath lab. Heart Lung Circ. 2018;27:777–778. doi: 10.1016/j.hlc.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Kane K, Kennedy F, Absolom KL, Harley C, Velikova G. Quality of life support in advanced cancer-web and technological interventions: systematic review and narrative synthesis. BMJ Support Palliat Care. 2023;13:e221–e234. doi: 10.1136/bmjspcare-2020-002820. [DOI] [PubMed] [Google Scholar]
- 30.Al-Jayyousi GF, Abdul Rahim H, Alsayed Hassan D, Awada SM. Following interprofessional education: health education students’ experience in a primary interprofessional care setting. J Multidiscip Healthc. 2021;14:3253–3265. doi: 10.2147/JMDH.S318110. [DOI] [PMC free article] [PubMed] [Google Scholar]