Abstract
Objective: To evaluate the effectiveness of graded nursing based on the risk early warning concept in long-term bedridden patients. Methods: The medical records of 124 long-term bedridden patients admitted to the Department of Orthopaedics at the Yongzhou Hospital of Traditional Chinese Medicine from April 2022 to March 2024 were collected retrospectively. Patients were separated into two groups: the control group which received routine nursing, and the study group which received graded nursing based on the “risk early warning” concept. Key metrics recorded included turnover frequency and time to first out-of-bed activity, Braden score, incidence of pressure injury (PI), activities of daily living (ADL), motor function, quality of life, negative emotions, complications, and patient satisfaction. Results: Low Barden score was a risk factor for PI in long-term bedridden patients (P<0.05, OR=0.040, 95% CI: 0.006-0.254). The turnover interval time and the time to first out-of-bed activity in the study group were shorter than those of the control group (all P<0.05). Compared to the control group, the Braden score, modified Barthel index score, Fugl-Meyer assessment score and quality of life scores of the study group were substantially higher (all P<0.05). The incidence of PI in the study group (4.62%) was lower than that of the control group (22.03%), and the area of PI in the study group was smaller than that of the control group (all P<0.05). Compared to the control group, the scores of self-rating anxiety scale and self-rating depression scale in the study group were substantially lower (all P<0.05). The study group had lower total incidence of complications (3.08% vs. 20.34%) and higher total satisfaction (95.38% vs. 79.66%) than the control group (all P<0.05). Conclusion: Graded nursing based on the risk early warning concept is highly effective in managing long-term bedridden patients. It reduces the occurrence of PI and complications, shortens the turnover interval time and the time to first out-of-bed activity, improves activities of daily living and motor function as well as quality of life, relieves negative emotions, and improves patient satisfaction.
Keywords: Bedridden, graded nursing, risk early warning concept, pressure injury, quality of life, negative emotions
Introduction
With the increasing prevalence of cerebrovascular diseases, respiratory diseases, and osteoporotic fractures, the number of patients requiring long-term bedridden treatment is also increasing [1]. These patients often experience significant limitation in performing daily living activities and are unable to adjust their body position independently. This results in persistent pressure on local tissues, poor blood circulation, inadequate tissue nutrition, and increased risk of complications such as pressure injury (PI), infections and muscular atrophy [2]. PI has emerged as a pervasive health challenge among long-term bedridden patients, which is related to factors such as persistent ischemia and hypoxia of tissues, insufficient nutrition, lack of exercise, excretion disorder, and circulation disorder. They mainly manifest as degeneration, ulceration and necrosis of skin tissues, frequently observed over bony eminences [3,4]. Long-term bedridden patients have a longer immobilization time, and most of them are middle-aged people with underlying diseases and compromised immune function, further elevating the risk of PI development [5]. The occurrence of PI not only impairs the patient’s physical function but also poses a risk of possibly fatal infection. It also brings great psychological pain to the patient, exacerbates familial and societal burdens, and delays the patient’s recovery progress [6]. The clinical nursing of long-term bedridden patients is complex and involves managing numerous risk factors. Therefore, how to reduce the risk of complications in long-term bedridden patients has become a significant challenge in nursing work.
Graded nursing represents a patient-centered system that classifies patients based on their health status and self-care capabilities. By formulating corresponding treatment strategies for patients in different grades, it facilitates the execution of precise and targeted intervention protocols and maximizes nursing effectiveness [7]. The concept of risk early warning enhances risk management and early warning awareness and improves preventive measures by assessing the risk of patients, identifying the types of risk factors, and issuing early warning signals [8]. Graded nursing based on the risk early warning concept enables a systematic categorization of patient risk factors, thus helping medical personnel to manage patients according to their risk levels. This study aimed to evaluate the effectiveness of graded nursing based on risk early warning concept in long-term bedridden patients by retrospectively analyzing their medical records.
Materials and methods
Research subjects
The medical records of 124 long-term bedridden patients admitted to the Department of Orthopaedics at the Yongzhou Hospital of Traditional Chinese Medicine from April 2022 to March 2024 were collected retrospectively. According to the nursing modality the patients received, 59 cases who were admitted from April 2022 to March 2023 and received routine nursing were taken as the control group. 65 cases admitted from April 2023 to March 2024 who received graded nursing based on risk early warning concept were taken as the study group. This study was approved by the Ethics Committee of the Yongzhou Hospital of Traditional Chinese Medicine.
Inclusion criteria: Patients bedridden for ≥1 month; Patient unable to turn over independently and requiring assistance from others for care; Patients with clear consciousness who can cooperate with various treatments and nursing operations.
Exclusion criteria: Patients with skin injury and dermatosis before admission; Patients with organic diseases of vital organs; Patients with malignant tumors; Patients with hematological diseases and autoimmune diseases; Patient with severe consciousness disturbance.
Nursing methods
The control group received routine nursing until being discharge from the hospital. The specific contents included routine education, regular turnover, and meticulous maintenance of skin, clothing, and bedding in a clean and dry state. PIs were reported promptly, and targeted treatments were administered as needed, along with preventive measures for other complications.
The study group received graded nursing based on risk early warning concept until discharge. The specific contents: (1) Establishment of a graded nursing team: A specialized team was formed based on the concept of risk early warning. It is composed of experienced nurses who had undergone professional training and assessment. They developed specialized nursing protocols for long-term bedridden patients. (2) Risk Assessment and Identification: Potential risks during the nursing process were identified by combining documentary evidence, clinical knowledge and experience and the patient’s specific situation. Identified risks included advanced age, being long-term bedridden, extended hospitalization time, low Barden score, abnormal body temperature and blood pressure, hospital-acquired infection, inadequate patient care, and insufficient health education. The probability, measurability and severity of all risk factors were scored on a scale of 1 to 3 points, with the risk score calculated as the product of these three factors. Risk score ≥18 points indicated a high-risk early warning level, 9 points ≤ risk score <18 points indicated a medium-risk early warning level, and risk score <9 points indicated a low-risk early warning level. Higher risk levels necessitated earlier intervention measures. (3) Implementation of Graded Nursing Based on Risk Levels: Patients at each risk level received corresponding nursing cares [9,10]. Specific nursing measures are shown in Table 1. (4) Education and Communication: Education was provided to patients and their families through various channels such as informational materials, lectures, and broadcasts. The mechanism, clinical manifestations, common sites, and negative effects of PIs in long-term bedridden patients were explained. Family members were guided on measures to prevent PIs. Efforts were also made to address patients’ negative emotions, reduce anxiety and depression, and enhance communication. (5) Continuous Evaluation and Improvement: Nurses conducted weekly reviews to discuss ongoing issues in the nursing process. Newly identified risk factors were incorporated into the risk early warning grading nursing plan, which was continuously refined and improved.
Table 1.
Specific nursing measures for long-term bedridden patients with different risk warning levels
| Graded nursing | Nursing measures |
|---|---|
| Low-risk early warning level nursing | Set up green early warning signs and put them on patients’ bedside cards and medical records |
| Instruct the patient’s family members to carry out proper physical function exercises for the patient, such as turning over and relaxing muscles regularly | |
| Make bedside turn-over cards, and record the patient’s turn-over time | |
| Put protective tools such as foam dressings and cushions under the patient’s bone protuberance and body gap | |
| Guide patients and their families to use bedpans correctly, and remove skin residues in time after urination and defecation | |
| Adjust the diet according to the patient’s specific condition, providing trace elements and nutrients to patients with severe malnutrition. For those who cannot eat orally, nasal feeding should be given | |
| Medium-risk early-warning level nursing | Set up yellow early warning signs and put them on patients’ bedside cards and medical records |
| Observe the patient’s breathing closely and conduct regular respiratory function training such as lip-contraction breathing and abdominal breathing exercises | |
| Use liquid dressing to form a lipid protective film on the skin surface | |
| High-risk early-warning level nursing | Set up red early warning signs and put them on patients’ bedside cards and medical records |
| An air cushion bed should be used for patients, with the air cushion properly inflated and placed on the bed surface. The surface should be covered with sheets, and the tightness and air flow of each connecting hose should be checked regularly |
Data collection
Baseline data collection
Baseline data were collected retrospectively from electronic medical records and outpatient examination records, including sex, age, body mass index, primary disease types, nutritional status, duration of bedridden status, and Barden score at admission. The number of patients with PIs was counted, and patients were screened for major risk factors associated with the development of PIs. Clinical data and questionnaire records at admission and discharge were collected retrospectively.
Activity time
The turnover interval time and the time to first out-of-bed activity were recorded.
Risk assessment of PI
At the time of admission and discharge, the risk of developing PI was evaluated by the Braden rating scale [11]. The Braden scale includes perception, humidity, mobility, activity, nutrient intake, friction and shear force. The score for the first five items was 1-4 points, and the score for friction and shear force was 1-3 points, resulting in a total score range of 6 to 23. Lower scores indicate a higher risk of PI.
Occurrence of PI
The occurrence and size of PI during hospitalization were documented. The National Pressure Ulcer Advisory Panel (NPUAP) was used to classify the degree of PI [12]. Phase I: Non-blanchable erythema of intact skin; Phase II: Partial-thickness skin loss or blisters; Phase III: Full-thickness skin loss, presenting as large blisters or deep craters; Phase IV: Deep tissue necrosis that may extend to surrounding muscles, bones, and joints.
Ability of daily living (ADL) and motor function
At the time of admission and discharge, the modified Barthel index (MBI) was used to evaluate the ADL of patients [13]. The MBI includes 10 items, each scored between 1 and 5, with a total score of 100. Lower scores indicate a poorer ability to perform daily activities. The Fugl-Meyer assessment (FMA) was used to evaluate the motor function at the time of admission and discharge [14]. The FMA evaluates upper limb function (0-66 points) and lower limb function (0-34 points), with a total score of 100 points. Lower scores reflect poorer motor function.
Quality of life
The quality of life (QoL) assessment scale, WHO-QOL-BREF, was used to evaluate the QoL of patients at both admission and discharge [15]. The scale includes four domains: physical, psychological, social function, and environment, with a total of 24 items. Each item is scored from 1-5, resulting in a total score of 100 points. Lower scores indicate a poorer quality of life.
Negative emotion
Negative emotions were assessed by Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) [16,17]. Both SAS and SDS consist of 20 items, each scored from 1-4 points. The total raw score is multiplied by 1.25 to obtain a standardized score, with a maximum score of 100 points. Lower scores indicate fewer negative emotions experienced by the patient.
Incidence of complications
The complications during hospitalization were recorded, including pulmonary infection, urinary tract infection, venous thrombosis of lower extremity, and disuse muscular atrophy.
Patient satisfaction
At discharge, patient satisfaction was evaluated using a satisfaction questionnaire developed by the hospital. The questionnaire covered aspects such as daily guidance, nursing procedures, health education, and overall quality of care. The total score was 100 points, with >85 points indicating very satisfied, 60-85 indicating generally satisfied, and <60 indicating dissatisfied. Total satisfaction rate = (cases of very satisfied + generally satisfied)/total number of cases × 100%.
Observation index
Primary outcomes
The primary focus was on comparing the incidence of PI, QOL score, SAS, and SDS scores between the control and study groups.
Secondary outcomes
Logistic regression was employed to identify risk factors influencing PI in long-term bedridden patients. Baseline data from the two groups were compared. Activity time, Braden score, MBI score, FMA score, incidence of complications and total satisfaction were compared between control and study groups.
Statistical methods
GraphPad Prism 8.0.2 software was adopted for data processing. The Shapiro-Wilk test was used for normality test, and normally distributed measured data were described as mean ± SD. Their comparison between groups was conducted by the independent-samples t test, and the intra-group comparison was by paired samples t test. Counted data were compared by the χ2 test or Fisher’s exact test. The risk factors were analyzed by binary Logistic regression. Statistical significance was set at P<0.05.
Results
Comparison of baseline data between the two groups
Analysis of the baseline data from subjects showed that sex, age, body mass index, main disease types, nutritional status and bedridden time showed no significant differences between the two groups (all P>0.05), as detailed in Table 2.
Table 2.
Comparison of baseline data between the control group and study group (x̅±s)/[n (%)]
| Group | Control group (n=59) | Study group (n=65) | χ2/t value | P value |
|---|---|---|---|---|
| Sex | 0.054 | 0.816 | ||
| Male | 33 (55.93%) | 35 (53.85%) | ||
| Female | 26 (44.07%) | 30 (46.15%) | ||
| Age (years) | 62.29±7.35 | 61.98±7.60 | 0.226 | 0.822 |
| Body mass index (kg/m2) | 24.16±3.25 | 23.57±3.22 | 1.017 | 0.311 |
| Main disease types | 0.750 | 0.862 | ||
| Cerebrovascular disease | 19 (32.20%) | 21 (32.31%) | ||
| Respiratory diseases | 18 (30.51%) | 16 (24.62%) | ||
| Cardiovascular disease | 12 (20.34%) | 14 (21.54%) | ||
| Other | 10 (16.95%) | 14 (21.54%) | ||
| Nutritional status | 2.217 | 0.137 | ||
| Without malnutrition | 50 (84.75%) | 48 (73.85%) | ||
| With malnutrition | 9 (15.25%) | 17 (26.15%) | ||
| Bedridden time (months) | 0.368 | 0.544 | ||
| 1-3 | 35 (59.32%) | 42 (64.62%) | ||
| >3 | 24 (40.68%) | 23 (35.38%) |
Note: χ2: data from chi-square test; t: data from t-test.
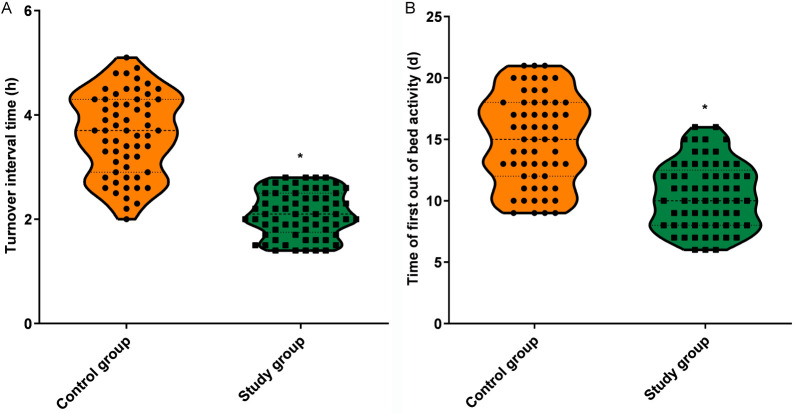
Comparison of activity time between the two groups
The turnover interval time and the time to first out-of-bed activity in the study group were all shorter than those of the control group (all P<0.05), as detailed in Figure 1.
Figure 1.
Comparison of activity time between control group and study group. A. Turnover interval time; B. Time to first out-of-bed activity. Note: Compared to control group, *P<0.05.
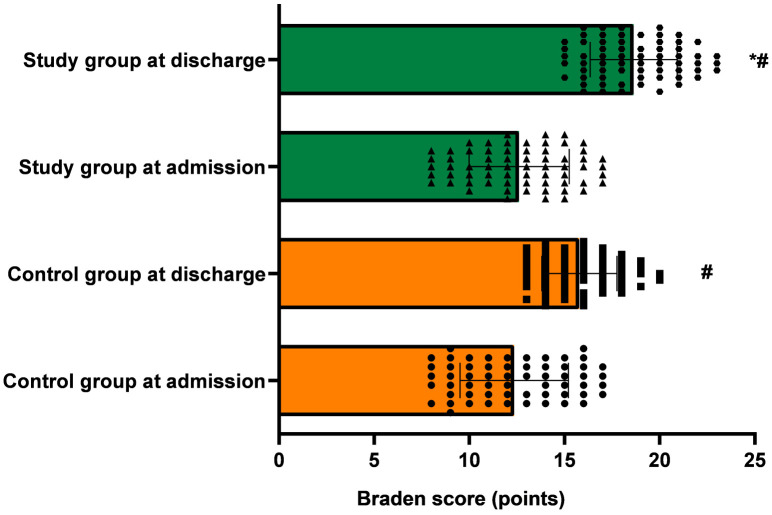
Comparison of Braden score between the two groups at admission and discharge
The Braden score showed no significant differences between the two groups at admission (P>0.05). At discharge, the Braden score of both groups was higher than that of admission; Notably, compared to the control group, the Braden score of the study group was substantially higher (all P<0.05), as detailed in Figure 2.
Figure 2.
Braden score at admission and discharge in control group and study group. Note: Compared to admission, #P<0.05; Compared to control group at discharge, *P<0.05. PI: Pressure injury.
Comparison of incidence of PIs between the two groups
Whether the subjects developed PI during hospitalization was counted. There were no phase III or IV PIs in both groups. The incidence of PI in the study group (4.62%) was significantly lower than that of the control group (22.03%), and the PI size in the study group was notably smaller than that of the control group (all P<0.05), as detailed in Table 3.
Table 3.
Comparison of incidence of PI between control group and study group (x̅±s)/[n (%)]
| Group | Control group (n=59) | Study group (n=65) | χ2/t value | P value |
|---|---|---|---|---|
| Phase I | 8 (13.56%) | 3 (4.62%) | ||
| Phase II | 5 (8.47%) | 0 (0.00%) | ||
| Phase III | 0 (0.00%) | 0 (0.00%) | ||
| Phase IV | 0 (0.00%) | 0 (0.00%) | ||
| Incidence of PI | 13 (22.03%) | 3 (4.62%) | 8.350 | 0.004 |
| PI area (cm2) | 7.59±1.26 | 5.13±0.35 | 3.261 | 0.006 |
Note: χ2: data from chi-square test; t: data from t-test; PI: Pressure injury.
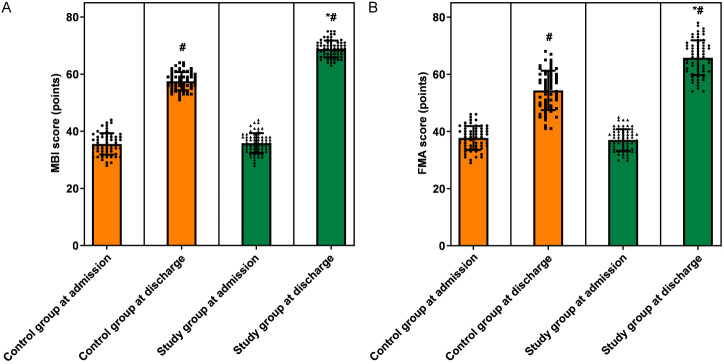
Comparison of ADL and motor function between the two groups at admission and discharge
At admission, the MBI and FMA scores showed no significant differences between the two groups (all P>0.05). At discharge, the scores of MBI and FMA significantly increased in both groups, and the scores of MBI and FMA in the study group were notably higher than those of the control group (all P<0.05), as detailed in Figure 3.
Figure 3.
Ability of daily living and motor function at admission and discharge in control group and study group. A. MBI score; B. FMA score. Note: Compared to admission, #P<0.05; Compared with control group at discharge, *P<0.05. MBI: modified Barthel index; FMA: Fugl-Meyer assessment.
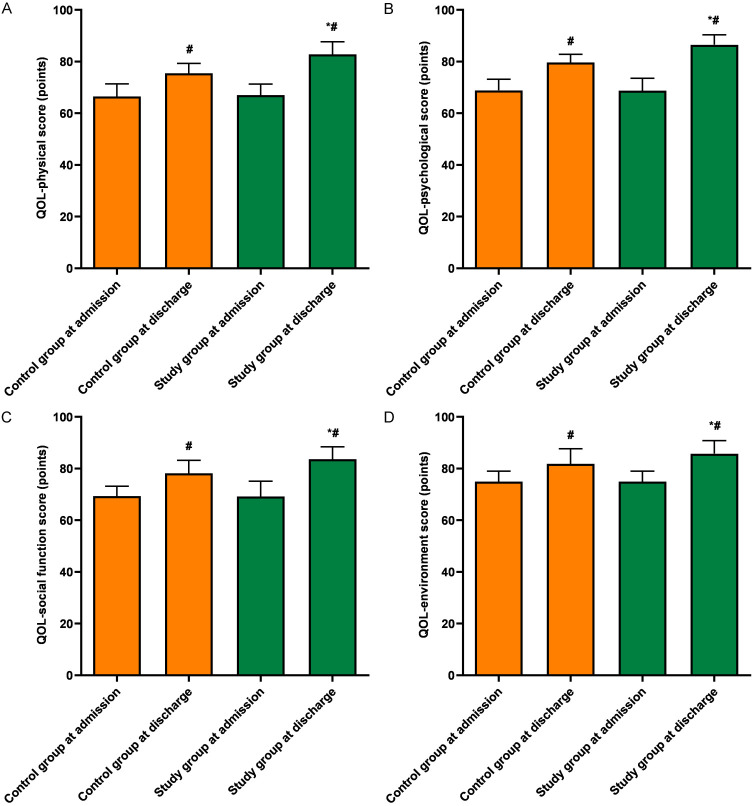
Comparison of QoL between the two group at admission and discharge
At admission, the QoL scores showed no significant difference between the two groups (all P>0.05). However, the QoL scores increased in both groups at discharge; Notably, the QoL score of the study group was higher than that of the control group (all P<0.05), as detailed in Figure 4.
Figure 4.
Quality of life scores at admission and discharge in control group and study group. A. QoL-physical score; B. QoL-psychological score; C. QoL-social function score; D. QoL-environment score. Note: Compared with admission, #P<0.05; Compared to control group at discharge, *P<0.05. QoL: Quality of life.
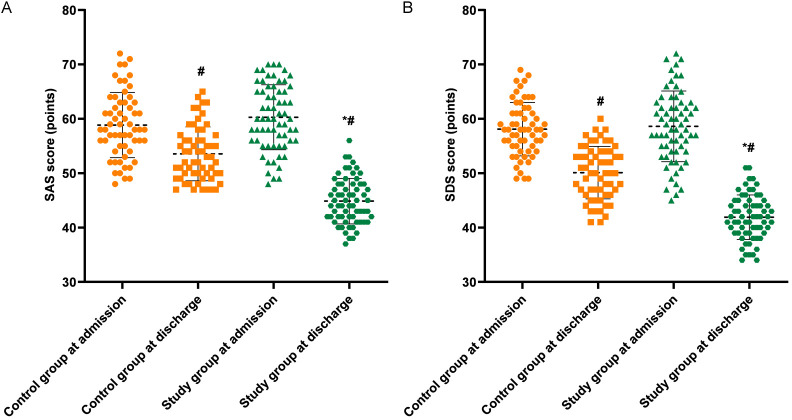
Comparison of SAS and SDS between the two group at admission and discharge
At admission, the SAS and SDS scores showed no significant differences between the two groups (all P>0.05). However, at discharge, the scores of SAS and SDS decreased significantly in both groups, and the scores in the study group were substantially lower than those of the control group (all P<0.05), as shown in Figure 5.
Figure 5.
Negative emotions at admission and discharge in control group and study group. A. SAS score; B. SDS score. Note: Compared to admission, #P<0.05; Compared with control group at discharge, *P<0.05. SAS: Self-rating anxiety scale; SDS: Self-rating depression scale.
Comparison of incidence of complications between the two groups
The incidence of complications during hospitalization was recorded for both groups. The study group showed a lower total incidence of complications (3.08%) compared to the control group (20.34%) (P<0.05). Detailed results are provided in Table 4.
Table 4.
Comparison of incidence of complications between control group and study group [n (%)]
| Group | Control group (n=59) | Study group (n=65) | χ2 value | P value |
|---|---|---|---|---|
| Pulmonary infection | 3 (5.08%) | 0 (0.00%) | ||
| Urinary tract infection | 4 (6.78%) | 1 (1.54%) | ||
| Venous thrombosis of lower extremity | 3 (5.08%) | 1 (1.54%) | ||
| Disuse muscular atrophy | 2 (3.39%) | 0 (0.00%) | ||
| Total incidence rate | 12 (20.34%) | 2 (3.08%) | - | 0.003 |
Note: χ2: data from Fisher’s exact test.
Comparison of patient satisfaction between the two groups
Patient satisfaction with nursing care was assessed. The study group reported a higher total satisfaction rate (95.38%) compared to the control group (79.66%) (P<0.05). Detailed results are available in Table 5.
Table 5.
Comparison of patient satisfaction between control group and study group [n (%)]
| Group | Control group (n=59) | Study group (n=65) | χ2 value | P value |
|---|---|---|---|---|
| Very satisfied | 27 (45.76%) | 43 (66.15%) | ||
| Generally satisfied | 20 (33.90%) | 19 (29.23%) | ||
| Dissatisfied | 12 (20.34%) | 3 (4.62%) | ||
| Total satisfaction | 47 (79.66%) | 62 (95.38%) | 7.191 | 0.007 |
Note: χ2: data from chi-square test.
Univariate analysis of risk factors for PI in long-term bedridden patients
According to the presence of PI, the patients were further grouped into a PI group (n=16) and a non-PI group (108) for the analysis of PO-associated risk factors. The age of patient with PI was higher than those without PI. The body mass index of PI group was lower than that of non-PI group. The malnutrition rate and the rate of bedridden time >3 months in PI group were higher than those in non-PI group. The Barden score at admission of the PI group was lower than that of non-PI group (all P<0.05, Table 6).
Table 6.
Univariate analysis of risk factors for PI in long-term bedridden patients (x̅±s)/[n (%)]
| Factor | Non-PI group (n=108) | PI group (n=16) | χ2/t value | P value |
|---|---|---|---|---|
| Sex | 0.174 | 0.677 | ||
| Male | 60 (55.56%) | 8 (50.00%) | ||
| Female | 48 (44.44%) | 8 (50.00%) | ||
| Age (years) | 61.33±7.35 | 67.50±5.91 | 3.202 | 0.002 |
| Body mass index (kg/m2) | 24.25±3.08 | 21.14±3.01 | 3.782 | <0.001 |
| Main disease types | 1.912 | 0.591 | ||
| Cerebrovascular disease | 36 (33.33%) | 4 (25.00%) | ||
| Respiratory diseases | 28 (25.93%) | 6 (37.50%) | ||
| Cardiovascular disease | 24 (22.22%) | 2 (12.50%) | ||
| Other | 20 (18.52%) | 4 (25.00%) | ||
| Nutritional status | 9.344 | 0.002 | ||
| Without malnutrition | 90 (83.33%) | 8 (50.00%) | ||
| With malnutrition | 18 (16.67%) | 8 (50.00%) | ||
| Bedridden time (months) | 10.741 | 0.001 | ||
| 1-3 | 73 (67.59%) | 4 (25.00%) | ||
| >3 | 35 (32.41%) | 12 (75.00%) | ||
| Barden score at admission (points) | 13.08±2.40 | 8.50±0.52 | 7.588 | <0.001 |
Note: χ2: data from chi-square test; t: data from t-test; PI: Pressure injury.
Multivariate analysis of risk factors for PI in long-term bedridden patients
Low Barden score was identified as an independent risk factor for PI in long-term bedridden patients (P<0.05, OR=0.040, 95% CI: 0.006-0.254), as shown in Table 7.
Table 7.
Multivariate analysis of risk factors for PI in long-term bedridden patients
| Factor | Coefficient of regression | Standard error | Wald value | P value | OR value | 95% CI |
|---|---|---|---|---|---|---|
| Age | 0.110 | 0.098 | 1.249 | 0.264 | 1.116 | 0.920-1.354 |
| Body mass index | 0.234 | 0.299 | 0.614 | 0.433 | 1.264 | 0.703-2.273 |
| Nutritional status | -1.585 | 1.666 | 0.905 | 0.341 | 0.205 | 0.008-5.365 |
| Bedridden time | 0.005 | 1.478 | 0.000 | 0.997 | 1.005 | 0.055-18.223 |
| Barden score at admission | -3.226 | 0.947 | 11.615 | 0.001 | 0.040 | 0.006-0.254 |
Discussion
Prolonged exposure to pressure, shear force, and friction renders long-term bedridden patients highly susceptible to PI. This condition can also lead to infections, increasing treatment costs, exacerbating negative emotions of patients, reducing patient satisfaction with care, and adversely affecting their psychological state and quality of life [18].
In routine care, nursing staff often develop care plans based on immediate needs of patients. However, these nursing plans often lack the ability to identify risk factors, foresight and effective risk management, leading to deficiencies in the nursing process and suboptimal patient recovery outcomes [19]. Furthermore, He et al. reported that graded nursing for patients with heart disease could improve care efficiency, accelerate cardiopulmonary recovery, and enhance both quality of life and overall health status [20]. Traditional graded nursing provides care according to the patients’ condition, but does not account for individual risk factors, lacks precision in its assessment process and overlooks the psychological wellbeing of patients as well as the prevention of complications. Unlike previous nursing approaches, this study integrates the concept of risk early warning into graded nursing, allowing for classification based on comprehensive risk factors. This enables nurses to prioritize management according to the patient’s risk level and proactively implement preventive measures. In this study, long-term bedridden patients treated with graded nursing based on risk early warning concept showed positive outcomes. This nursing method could shorten the turnover interval time and the time to the first out-of-bed activity, improve Braden score, lower the risk of PI, and reduce PI size. This study implemented an early warning management system considering patient, hospital and nursing work factors, dividing patients into three risk categories: low, medium and high. This approach focuses on multiple warning factors such as age, duration of bedridden status, hospitalization time, Barden score, vital signs, hospital environment and nursing content. Different nursing methods were applied based on the patient’s risk level. The use of different color-coded warning signs helped nurses to quickly assess the risk level of patients, enhancing their responsibility for long-term bedridden patients and providing a more intuitive application of care strategies [21]. By instructing patients and their families on regular turn-over, muscle relaxation, limb function exercise and other measures, the vertical pressure on the skin can be reduced. This can enhance the patient’s blood circulation, and improve blood flow speed, thereby improving blood circulation, enhancing blood flow speed, and lowering the risk of local tissue necrosis [22]. The implementation of foam dressing decompression, skin cleaning, nutrition supplementation and other methods is conducive to mitigating the irritation of skin secretions and excretions on local tissues, effectively preventing the formation of PI [23,24]. Respiratory function training, the use of liquid dressings and air cushion bed are tailored for long-term bedridden patients, reducing the risk of complications and preventing the expansion of skin damage [25,26]. In addition, graded nursing based on risk early warning concept offers long-term bedridden patients both health education and psychological counseling, promoting awareness of the dangers of PI, improving disease cognition, encouraging early mobilization, and equipping patients’ families with the necessary knowledge and skills to prevent and manage complications [27,28]. Finally, this nursing scheme requires nurses to regularly review their work, find the shortcomings in implementation, and continuously refine the nursing scheme, so as to enhance the proficiency of nursing staff, strengthen intervention on risk factors, and continuously improve the quality of care, which accelerates rehabilitation of long-term bedridden patients [29].
The application of graded nursing based on risk early warning concept in long-term bedridden patients can improve nurses’ ability to identify risks, and prioritizes intervention for high-risk individuals. It promotes the rational allocation of nursing resources, and improves nursing efficiency and quality [30]. This study demonstrated that graded nursing based on risk early warning concept can improve the MBI, FMA, and QOL scores of patients and reduce the occurrence of complications, indicating that the scheme can improve rehabilitation effect, and reduce the occurrence of infection and muscular atrophy through functional exercise, diet regulation, complication prevention, health education and psychological counseling, so as to improve the patients’ ADL and motor function, and optimize their quality of life. Additionally, the study found that compared to the control group, the scores of SAS and SDS in the study group were substantially lower. Under the management of the risk early warning grading nursing scheme, nurses employed educational methods such as informational materials, lectures, and broadcasts to educate patients and their families. This approach helped patients better understand their condition, increased their confidence in the rehabilitation process, and alleviated feelings of unease [31]. Concurrently, nursing staff are encouraged to attend to patients’ emotional well-being, enhance communication, and address patients’ psychological concerns such as anxiety and depression [32]. Graded nursing based on risk early warning concept draws nurses’ attention to risk factors, strengthens weak links in nursing, increases communication with patients, and then fosters patient satisfaction.
Braden score is an effective tool for identifying patients at high risk of PI and is widely considered a reliable method to promote PI prevention [33]. Deng et al. conducted risk assessment on elderly bedridden patients and assessed their PI risk using Braden score, finding that predictive nursing intervention effectively reduced the incidence of PI [34]. It is important to note that Braden score considers factors such as pressure, nutrition, and activity, and may not fully capture all aspects of PI risk in long-term bedridden patients. Unlike previous studies, this study used not only Braden score to assess the patient risk, but also implemented a comprehensive grading system that considered individual patient factors, hospital environment factors, nursing operation factors and other risk warning factors for long-term bedridden patients. Moreover, in this study, multivariate analysis showed that a lower Barden score was a significant risk factor for PI. Hence, early identification of risk factors for long-term bedridden patients and corresponding nursing intervention are crucial to improve the rehabilitation outcomes.
This study has some limitations, such as less retrospective collection of medical records and short observation period, which may have introduced data bias. Future research should aim to refine the nursing content according to the actual clinical circumstances, and carry out a large sample multi-center prospective study to validate these findings.
Conclusion
The application of graded nursing based on risk early warning concept in long-term bedridden patients is highly effective. It reduces the incidence of PI and complications, shortens the turnover interval time and the time to first out-of-bed activity, enhances the ability of daily living and motor function, improves patients’ quality of life, relieves negative emotions of patients, and improves patient satisfaction. This approach provides new ideas for promoting the recovery of long-term bedridden patients.
Disclosure of conflict of interest
None.
References
- 1.Cardoso R, Parola V, Neves H, Bernardes RA, Duque FM, Mendes CA, Pimentel M, Caetano P, Petronilho F, Albuquerque C, Sousa LB, Malça C, Durães R, Xavier W, Parreira P, Apóstolo J, Cruz A. Physical rehabilitation programs for bedridden patients with prolonged immobility: a scoping review. Int J Environ Res Public Health. 2022;19:6420. doi: 10.3390/ijerph19116420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mamom J, Daovisan H. Listening to caregivers’ voices: the informal family caregiver burden of caring for chronically ill bedridden elderly patients. Int J Environ Res Public Health. 2022;19:567. doi: 10.3390/ijerph19010567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nancy GA, Kalpana R, Nandhini S. A study on pressure ulcer: influencing factors and diagnostic techniques. Int J Low Extrem Wounds. 2022;21:254–263. doi: 10.1177/15347346221081603. [DOI] [PubMed] [Google Scholar]
- 4.Edsberg LE, Cox J, Koloms K, VanGilder-Freese CA. Implementation of pressure injury prevention strategies in acute care: results from the 2018-2019 international pressure injury prevalence survey. J Wound Ostomy Continence Nurs. 2022;49:211–219. doi: 10.1097/WON.0000000000000878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozcan O, Karaali HK. Physiotherapists’ knowledge on pressure ulcer prevention. Int Wound J. 2023;20:1893–1902. doi: 10.1111/iwj.14049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu Y, Luo M, Liu Q, Liu H. Preventive effect of cluster nursing on pressure ulcers in orthopedic patients and predictive value of serum IL-6 and TNF-α for the occurrence of pressure ulcers. Am J Transl Res. 2023;15:1140–1149. [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang Q, Yu Y. Effects of graded emergency nursing on resuscitation outcomes, prognosis, and nursing satisfaction in patients with acute myocardial infarction. Am J Transl Res. 2021;13:10586–10592. [PMC free article] [PubMed] [Google Scholar]
- 8.Langkjaer CS, Bundgaard K, Bunkenborg G, Nielsen PB, Iversen KK, Bestle MH, Bove DG. How nurses use national early warning score and individual early warning score to support their patient risk assessment practice: a fieldwork study. J Adv Nurs. 2023;79:789–797. doi: 10.1111/jan.15547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Labeau SO, Afonso E, Benbenishty J, Blackwood B, Boulanger C, Brett SJ, Calvino-Gunther S, Chaboyer W, Coyer F, Deschepper M, François G, Honore PM, Jankovic R, Khanna AK, Llaurado-Serra M, Lin F, Rose L, Rubulotta F, Saager L, Williams G, Blot SI DecubICUs Study Team; European Society of Intensive Care Medicine (ESICM) Trials Group Collaborators. Prevalence, associated factors and outcomes of pressure injuries in adult intensive care unit patients: the DecubICUs study. Intensive Care Med. 2021;47:160–169. doi: 10.1007/s00134-020-06234-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horn SD, Bender SA, Bergstrom N, Cook AS, Ferguson ML, Rimmasch HL, Sharkey SS, Smout RJ, Taler GA, Voss AC. Description of the national pressure ulcer long-term care study. J Am Geriatr Soc. 2002;50:1816–1825. doi: 10.1046/j.1532-5415.2002.50510.x. [DOI] [PubMed] [Google Scholar]
- 11.Bergstrom N, Braden BJ, Laguzza A, Holman V. The braden scale for predicting pressure sore risk. Nurs Res. 1987;36:205–210. [PubMed] [Google Scholar]
- 12.Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised national pressure ulcer advisory panel pressure injury staging system: revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43:585–597. doi: 10.1097/WON.0000000000000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taghizadeh G, Martinez-Martin P, Meimandi M, Habibi SAH, Jamali S, Dehmiyani A, Rostami S, Mahmuodi A, Mehdizadeh M, Fereshtehnejad SM. Barthel index and modified rankin scale: psychometric properties during medication phases in idiopathic Parkinson disease. Ann Phys Rehabil Med. 2020;63:500–504. doi: 10.1016/j.rehab.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Rech KD, Salazar AP, Marchese RR, Schifino G, Cimolin V, Pagnussat AS. Fugl-meyer assessment scores are related with kinematic measures in people with chronic hemiparesis after stroke. J Stroke Cerebrovasc Dis. 2020;29:104463. doi: 10.1016/j.jstrokecerebrovasdis.2019.104463. [DOI] [PubMed] [Google Scholar]
- 15.Kumar P, Sen RK, Aggarwal S, Jindal K, Rajnish RK. Assessment and reliability of the World Health Organisation quality of life (WHO QOL-BREF) questionnaire in total hip replacement patients. J Clin Orthop Trauma. 2020;11(Suppl 5):S756–S759. doi: 10.1016/j.jcot.2020.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 17.Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 18.Liu ZF, Meng J, Jing N, Liu XY. Effects of predictive nursing interventions on pressure ulcer in older bedridden patients: a meta-analysis. Int Wound J. 2024;21:e14676. doi: 10.1111/iwj.14676. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.Gu YH, Wang X, Sun SS. Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients. World J Clin Cases. 2022;10:43–50. doi: 10.12998/wjcc.v10.i1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He K, Deng Y. Effect of graded cardiac rehabilitation care on clinical efficacy and quality of life in patients with CHD after OPCAB. Am J Transl Res. 2023;15:1820–1830. [PMC free article] [PubMed] [Google Scholar]
- 21.Cuttler SJ, Barr-Walker J, Cuttler L. Reducing medical-surgical inpatient falls and injuries with videos, icons and alarms. BMJ Open Qual. 2017;6:e000119. doi: 10.1136/bmjoq-2017-000119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tervo-Heikkinen T, Heikkilä A, Koivunen M, Kortteisto T, Peltokoski J, Salmela S, Sankelo M, Ylitörmänen T, Junttila K. Nursing interventions in preventing pressure injuries in acute inpatient care: a cross-sectional national study. BMC Nurs. 2023;22:198. doi: 10.1186/s12912-023-01369-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Visconti AJ, Sola OI, Raghavan PV. Pressure injuries: prevention, evaluation, and management. Am Fam Physician. 2023;108:166–174. [PubMed] [Google Scholar]
- 24.Walker RM, Chaboyer W, Cooke M, Whitty JA, Thalib L, Lockwood I, Latimer S, Campbell J, Probert R, Gillespie BM. Effectiveness of Prophylactic foam dressings in the prevention of sacral pressure injuries in at-risk hospitalised patients: the EEPOC trial. Trials. 2023;24:70. doi: 10.1186/s13063-022-06999-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li D, Fei X, Xu L, Wang Y, Tian J, Li Y. Pressure-sensitive antibacterial hydrogel dressing for wound monitoring in bed ridden patients. J Colloid Interface Sci. 2022;627:942–955. doi: 10.1016/j.jcis.2022.07.030. [DOI] [PubMed] [Google Scholar]
- 26.Kim SY, Kim HJ, An JW, Lee Y, Shin YS. Effects of alternating pressure air mattresses on pressure injury prevention: a systematic review of randomized controlled trials. Worldviews Evid Based Nurs. 2022;19:94–99. doi: 10.1111/wvn.12570. [DOI] [PubMed] [Google Scholar]
- 27.Tian J, Ren G, Fan G, Zhang M. Effect of mind map health education mode on prevention of pressure ulcers. Altern Ther Health Med. 2023;29:631–637. [PubMed] [Google Scholar]
- 28.Burston A, Miles SJ, Fulbrook P. Patient and carer experience of living with a pressure injury: a meta-synthesis of qualitative studies. J Clin Nurs. 2023;32:3233–3247. doi: 10.1111/jocn.16431. [DOI] [PubMed] [Google Scholar]
- 29.Han C, Yang F, Liu L. Effectiveness of continuous care interventions in elderly patients with high-risk pressure ulcers and impact on patients’ activities of daily living. Altern Ther Health Med. 2024;30:118–123. [PubMed] [Google Scholar]
- 30.Jiang H, Qin L, Wang L, Jin Y, Gong L, Yang Y. The protective effect of MEWS-based graded nursing on the life safety of car accident patients. Altern Ther Health Med. 2024:AT9694. [PubMed] [Google Scholar]
- 31.Thomas DC, Chui PL, Yahya A, Yap JW. Systematic review of patient education for pressure injury: evidence to guide practice. Worldviews Evid Based Nurs. 2022;19:267–274. doi: 10.1111/wvn.12582. [DOI] [PubMed] [Google Scholar]
- 32.Qian L, Yan S, Ting ST, Han ZM, Qi T. Complications and psychological impact of pressure ulcers on patients and caregivers. Int Wound J. 2024;21:e14836. doi: 10.1111/iwj.14836. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 33.Chung ML, Widdel M, Kirchhoff J, Sellin J, Jelali M, Geiser F, Mücke M, Conrad R. Risk factors for pressure ulcers in adult patients: a meta-analysis on sociodemographic factors and the Braden scale. J Clin Nurs. 2023;32:1979–1992. doi: 10.1111/jocn.16260. [DOI] [PubMed] [Google Scholar]
- 34.Deng GL, Lei YL, Tan H, Geng BC, Liu Z. Effects of predictive nursing interventions on pressure ulcer in elderly bedridden patients. Int Wound J. 2024;21:e14690. doi: 10.1111/iwj.14690. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]