Abstract
Background
In clinical practice, psoriasis is a prevalent chronic inflammatory cutaneous disease featured with the development of red plaque with silvery scales, which considerably affects cutaneous health and quality of life of those afflicted.
Objective
This research aimed to examine the association between the body roundness index (BRI) and psoriasis, using data sourced from the National Health and Nutrition Examination Survey (NHANES).
Methods
Our study used a cross-sectional design, including 8,479 adults, of whom 234 were diagnosed with psoriasis. Multivariable logistic regression was used to analyze the relationship between BRI and psoriasis, with stepwise adjustments for covariables.
Results
Results from multivariable logistic regression analyses indicated a significant positive relationship between BRI and the risk of developing psoriasis; specifically, after comprehensive adjustment for covariables, per 1 unit increase in BRI was linked to an 11% rise in psoriasis risk (OR = 1.11, 95% CI = 1.05–1.17). Furthermore, psoriasis patients exhibited higher average BRI compared to non-psoriasis patients and a greater prevalence of comorbidities such as hypertension and smoking.
Conclusion
These findings suggest that higher BRI is positively correlated with the risk of psoriasis in the adult population in the US. BRI could potentially act as a practical anthropometric index for more accurately predicting the risk of developing psoriasis.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12944-024-02365-w.
Keywords: BRI, Psoriasis, Cross-sectional study, NHANES
Introduction
Psoriasis, a chronic inflammatory cutaneous condition, is characterized by the development of red plaques with silvery scales, significantly affecting patients’ quality of life and mental health [1]. Beyond its dermatological manifestations, psoriasis is linked to a variety of comorbid conditions, encompassing cardiovascular diseases and metabolic disorders, which contribute to substantial economic burdens on both patients and healthcare systems [2]. Current treatment options encompass topical therapies, phototherapy, and systemic medications [3]; however, these modalities often exhibit limitations in efficacy and adverse effects, necessitating a deeper understanding of the disease’s underlying factors and mechanisms for effective intervention and management.
Existing literature has established associations between anthropometric indexes and psoriasis. Several studies indicate that the risk of suffering psoriasis increases with an increase in body mass index (BMI) [4–6]. For instance, a longitudinal prospective study has substantiated that elevations in BMI, as well as waist and hip circumferences are significantly correlated with an increased risk of psoriasis [7]. Furthermore, a clinical trial with an open-label and single-arm design revealed that obese individuals with psoriasis who achieved a 12% reduction in body weight experienced a 50-75% decrease in psoriasis area and severity index (PASI) scores, alongside notable improvements in quality of life metrics [8].
Introduced by Thomas in 2013, the BRI represents a newly proposed anthropometric index [9]. Compared to BMI, BRI additionally takes waist circumference into account, thereby providing a more holistic evaluation of visceral fat distribution within the body. BRI has emerged as a promising metric for evaluating body shape, current research has shown that the BRI is associated with the risk of various diseases, including metabolic syndrome, cardiovascular diseases, and colorectal cancer [10–14]. Nonetheless, the connection between BRI and psoriasis remains ambiguous, and to date, no studies have explored this relationship within the general population of the United States. This study endeavors to shed light on the potential association between BRI and psoriasis by analyzing NHANES data, thereby underscoring the importance of anthropometric indexes in understanding psoriasis pathogenesis and risk assessment.
In summary, our work seeks to fill the existing knowledge gap regarding the association between BRI and psoriasis by utilizing a nationally representative dataset. By investigating the interplay between demographic factors, anthropometric index, and clinical outcomes, this research aims to provide valuable insights into the multifaceted nature of psoriasis and its management.
Methods
Study population
The participant data was sourced from NHANES database, an annual assessment implemented by the Centers for Disease Control and Prevention (CDC), focused on assessing the health and nutritional conditions of individuals in the US, across both adult and pediatric populations. This survey is distinguished by its integration of interviews and physical assessments. NHANES composes a vital initiative of the National Center for Health Statistics (NCHS), which is tasked with sharing essential health statistics nationwide.
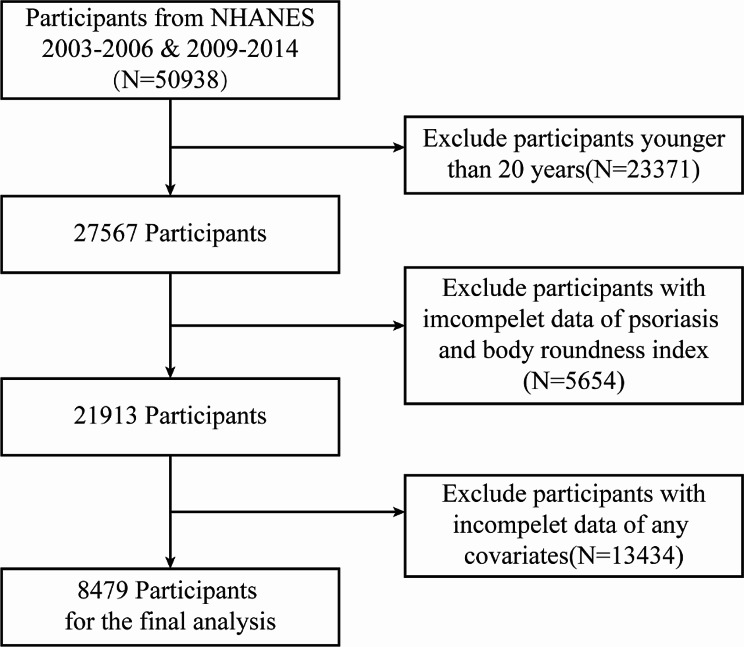
For this study, data used from the psoriasis questionnaire surveys included in the NHANES database for five cycles from 2003 to 2006 and 2009–2014, research subjects are adults aged 20 and older. Inclusion and exclusion of the study population according to the flowchart in Fig. 1. Among the 50,938 eligible respondents for analysis, 23,371 were excluded due to being under 20 years of age, 3,503 were excluded due to missing psoriasis questionnaire information, 2,151 were excluded due to incomplete BRI data, and 13,434 were excluded due to missing covariable information. The final sample size was 8,479 adults.
Fig. 1.
Flowchart for inclusion of study participants
Assessment of psoriasis
Psoriasis diagnoses were performed by qualified dermatologist through careful morphological evaluation of skin lesions characterized by well-defined red plaque with silvery scales. Data acquisition was facilitated via an interviewer-assisted questionnaire. Specifically, participants were asked, “Have you ever been informed by a healthcare provider that you have psoriasis?” In this analysis, individuals who responded affirmatively were classified as with psoriasis, while those who declined to answer or expressed uncertainty were classified as without psoriasis.
Definition of BRI
BRI is a novel anthropometric index that assesses body type by measuring height (in centimeters) and waist circumference (WC) (in centimeters). Information regarding height and WC was extracted from the participants’ examination documentation. BRI is computed utilizing the following formula:
 |
In the subsequent analysis, we will treat BRI as a continuous variable and perform multiple regression analysis using quintiles within the BRI range according to the method of Zhang et al. [14].
Assessment of covariables
Drawing from pertinent previous research, the covariable in this research involves age, gender, race/ethnicity, education level, poverty income ratio (PIR), the level of triglyceride (TG) and low-density lipoprotein (LDL), smoking status, alcohol drinking status, personal medical history of hypertension, diabetes, cardiovascular disease (CVD) and survey cycle. These factors were gathered through household interviews or laboratory examination. The assessment of covariables is briefly described here; for a detailed definition, please refer to the supplementary materials.
Statistical analysis
According to the analytical protocols provided by NHANES, our investigation utilized a complex sampling design along with appropriate sampling weights. For consecutive variables demonstrating a normal distribution, descriptive statistics were expressed as mean ± standard deviation (SD), while those not conforming to a normal distribution were represented as median with interquartile range (IQR). Categorical data was presented in terms of frequency (percentage). Group comparisons for consecutive variables that adhere to a normal distribution were conducted using an independent samples t-test. The assessment of categorical variables was performed using the chi-square test; however, in instances where the assumptions necessary for the chi-square test were not upheld, Fisher’s exact test was employed as an alternative method.
Multivariable logistic regression analysis was undertaken to evaluate the relationship between BRI and psoriasis. Model 1 represents the crude, unadjusted model. Model 2 adjusts for basic demographic factors, including age, gender, and race/ethnicity. Model 3 further incorporates adjustments for educational level, marital status, PRI, smoking status, alcohol drinking status, history of hypertension, diabetes, CVD status, TG, and LDL levels based on the adjustments made in Model 2. We divided the BRI into quintiles based on the method of Zhang et al. and used the partial Mann-Kendall test to examine the trend [14].
Additionally, restricted cubic spline (RCS) regressions were performed to assess the dose-response relationship between BRI and psoriasis after accounting for all covariables noted in Model 3. In the RCS analysis, we set up three knots at the 10th, 50th, and 90th percentiles of the BRI to determine whether there is a nonlinear association between BRI and psoriasis.
All statistical procedures were performed utilizing R software (version 4.4.1, R Project for Statistical Computing, Vienna, Austria) alongside EmpowerStats (version 4.1, Boston, Massachusetts). A two-sided P-value of less than 0.05 was established as the threshold for statistical significance across all tests.
Results
Basic characteristics
In this study, 8,479 adults aged 20 and older were included according to flowchart of Fig. 1, meanwhile the excluded participants data were listed in the Supplementary materials Table S1. The participants were categorized into two distinct groups: those diagnosed with psoriasis (n = 234) and those without psoriasis (n = 8,245). Notably, Table 1 illustrates the significant differences observed between the two-population concerning various demographic and health-related factors in terms of age, BRI, smoking status, hypertension, and CVD characteristics. The average age of individuals in the psoriasis group was recorded at 49.7 ± 16.0 years, which is significantly older than the average age of 45.9 ± 17.0 years for the without psoriasis group (P < 0.001). The BRI of the psoriasis group was 6.0 ± 2.6, significantly higher than that of the without psoriasis group at 5.3 ± 2.3(P < 0.001). The psoriasis group exhibited significantly higher proportions of smokers, as well as a higher prevalence of hypertension and CVD, compared to the group without psoriasis (P < 0.05).
Table 1.
Characteristics of participants in the NHANES 2003–2006 and 2009–2014 cycles
| Characteristic | Participants a | |||
|---|---|---|---|---|
| Total (N = 8479) |
Without Psoriasis (N = 8245) |
With Psoriasis (N = 234) |
P value | |
| Age, mean ± SD | 46.0 ± 16.9 | 45.9 ± 17.0 | 49.7 ± 16.0 | < 0.001 |
| Gender, N (%) | 0.813 | |||
| Male | 4112(48.5) | 4000(49.1) | 112(48.2) | |
| Female | 4367(51.5) | 4245(50.9) | 122(51.8) | |
| Year cycle | 0.459 | |||
| 2003–2004 | 1091(12.9) | 1060(15.5) | 31(18.4) | |
| 2005–2006 | 1277(15.1) | 1241(16.9) | 36(20.4) | |
| 2009–2010 | 2159(25.5) | 2099(21.2) | 60(19.5) | |
| 2011–2012 | 1882(22.2) | 1824(22.8) | 58(24.1) | |
| 2013–2014 | 2070(24.4) | 2021(23.6) | 49(17.6) | |
| Race and ethnicity b, N (%) | < 0.001 | |||
| Mexican American | 1988(23.4) | 1951(13.2) | 37(7.2) | |
| Non-Hispanic Black | 4011(47.3) | 3863(70.1) | 148(82.4) | |
| Non-Hispanic White | 1703(20.1) | 1671(10.4) | 32(6.5) | |
| Other | 777(9.2) | 760(6.3) | 17(3.9) | |
| Educational level, N (%) | 0.251 | |||
| High school or less | 1945(22.9) | 1898(15.9) | 47(14.4) | |
| Some college | 1880(22.2) | 1830(22.2) | 50(17.9) | |
| College graduate or higher | 4654(54.9) | 4517(62.0) | 137(67.8) | |
| Marital status, N (%) | 0.781 | |||
| Married | 4455(52.5) | 4329(57.0) | 126(56.7) | |
| Never married | 1645(19.4) | 1613(18.3) | 32(16.6) | |
| Living with partner | 756(8.9) | 736(8.2) | 20(7.4) | |
| Others c | 1623(19.1) | 1567(16.4) | 56(19.3) | |
| Family PIR, N (%) | 0.431 | |||
| < 1.3 | 2637(31.1) | 2562(21.1) | 75(20.1) | |
| 1.3 to < 3.5 | 3091(36.5) | 3025(35.6) | 66(31.8) | |
| ≥ 3.5 | 2751(32.4) | 2658(43.3) | 93(48.1) | |
| Smoking status, N (%) | 0.025 | |||
| No | 4703(55.5) | 4592(55.0) | 111(46.3) | |
| Yes | 3776(44.5) | 3653(45.0) | 123(53.7) | |
| Alcohol drinking, N (%) | 0.447 | |||
| No | 2259(26.6) | 2205(21.7) | 54(18.8) | |
| Yes | 6220(73.4) | 6040(78.3) | 180(81.2) | |
| Hypertension, N (%) | < 0.001 | |||
| No | 5333(62.9) | 5218(66.1) | 115(49.3) | |
| Yes | 3146(37.1) | 3027(33.9) | 119(50.7) | |
| Diabetes, N (%) | 0.956 | |||
| No | 7440(87.7) | 7239(90.7) | 201(90.8) | |
| Yes | 1039(12.3) | 1006(9.3) | 33(9.2) | |
| CVD, N (%) | 0.027 | |||
| No | 8216(96.9) | 7998(97.3) | 218(94.7) | |
| Yes | 263(3.1) | 247(2.7) | 16(5.3) | |
| TG (mmol/L), mean ± SD | 121.5 ± 67.6 | 121.2 ± 67.5 | 129.7 ± 69.5 | 0.057 |
| LDL (mmol/L), mean ± SD | 114.3 ± 35.3 | 114.3 ± 35.5 | 115.5 ± 35.6 | 0.611 |
| BRI, mean ± SD | 5.3 ± 2.3 | 5.3 ± 2.3 | 6.0 ± 2.6 | < 0.001 |
Abbreviations SD: standard deviation; PIR: poverty impact ratio; CVD: cardiovascular disease; TG: triglyceride; LDL: low-density lipoprotein; BRI: body roundness index
a Data are presented as unweighted number (weighted percentage) unless otherwise specified
b Race and ethnicity were self-reported
c Included widowed, divorced, or separated
Association between BRI and psoriasis
To investigate the association between BRI and psoriasis, a multiple regression analysis was undertaken, and after gradually adjusting for the influence of covariables, we used the first quintile interval of BRI as a reference control (Table 2). The analysis revealed a robust positive association between the risk of psoriasis and BRI, implying that an increase in BRI is related to a heightened risk of psoriasis (P < 0.001). The unadjusted model 1 indicated a positive association between BRI and psoriasis risk, which persisted through adjusted models 2 and 3. In the fully adjusted model 3, data indicated that for per 1 unit increase in BRI, the risk of suffering psoriasis escalated by 11% (OR = 1.11, 95%CI = 1.05–1.17). After fully adjusting for covariables, the second quintile Q2 (BRI:3.42 to < 4.45, OR = 1.45, 95%CI = 0.77–2.76) was not found to be statistically significant difference from the reference group Q1. However, significant differences emerged starting from the third quintile Q3 (BRI:4.45 to < 5.45, OR = 1.74, 95%CI = 1.02–2.98), with even more pronounced differences in Q4 (BRI:5.45 to < 6.96, OR = 1.87, 95%CI = 1.13–3.11) and Q5 (BRI:>6.96, OR = 2.04, 95%CI = 1.26–3.29). As the BRI increases, the risk of suffering psoriasis in the population significantly increases. In all three multiple regression models, the results of the trend test indicate that with the increase of BRI, the risk of psoriasis in the population shows a statistically significant trend of increasing (P for trend < 0.05).
Table 2.
Associations of body roundness index with psoriasis among adults aged ≥ 20 years (N = 8479)
| Prevalence (95% CI) | Model 1a | Model 2b | Model 3c | ||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | ||
| Per 1 unit increase | 3.09(2.55,3.64) | 1.11(1.06,1.18) | < 0.001 | 1.11(1.05,1.17) | < 0.001 | 1.11(1.05,1.17) | < 0.001 |
| Quintiles | |||||||
| Q1(< 3.42) | 1.88(1.13,2.62) | 1(Ref.) | 1(Ref.) | 1(Ref.) | |||
| Q2(3.42 to < 4.45) | 2.72(1.67,3.77) | 1.46(0.78,2.74) | 0.240 | 1.40(0.74,2.71) | 0.294 | 1.45(0.77,2.76) | 0.256 |
| Q3(4.45 to < 5.45) | 3.36(2.10,4.61) | 1.82(1.04,3.17) | 0.039 | 1.75(1.01,3.04) | 0.051 | 1.74(1.02,2.98) | 0.047 |
| Q4(5.45 to < 6.96) | 3.59(2.42,4.77) | 1.95(1.18,3.23) | 0.012 | 1.89(1.13,3.14) | 0.018 | 1.87(1.13,3.11) | 0.019 |
| Q5(> 6.96) | 4.13(3.00,5.27) | 2.25(1.40,3.63) | 0.001 | 2.16(1.31,3.57) | 0.004 | 2.04(1.26,3.29) | 0.005 |
| P for trend | < 0.001 | < 0.001 | 0.002 | ||||
Abbreviations OR: odds ratio; CI: confidence interval; Q: quintiles
a Model 1: Unadjusted
b Model 2: Adjusted for age, gender, and race/ethnicity
c Model 3: Full adjusted for the variables in Model 2 plus educational level, marital status, PIR, education level, Smoking status, alcohol drinking, hypertension, diabetes, CVD status, TG and LDL level
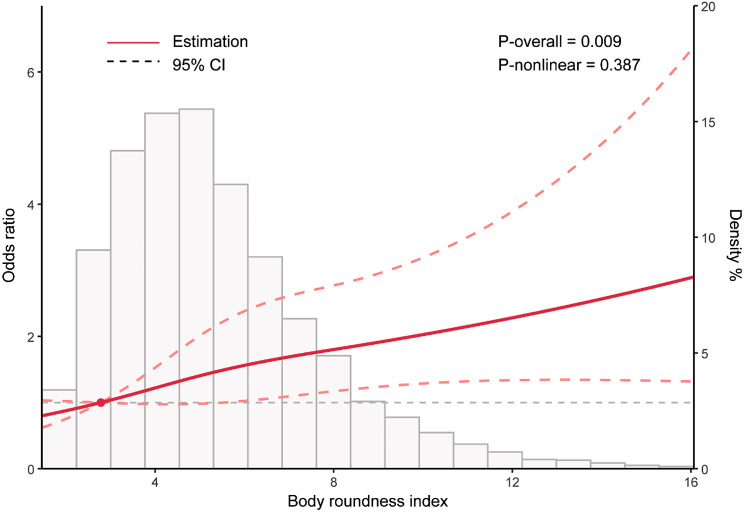
RCS analyses
To examine potential nonlinear association between BRI and psoriasis, we conducted an RCS analysis using model 3 with comprehensive adjustment for covariables (Fig. 2). The findings revealed that there is no significant nonlinear association between BRI and psoriasis (P-nonlinear = 0.387); however, a positive dose-response relationship was identified (P-overall = 0.009).
Fig. 2.
The dose-response relationship between BRI and psoriasis after full adjustment. The solid curved line represents the estimates for the association of psoriasis with BRI, and dashed line range is the 95% CI
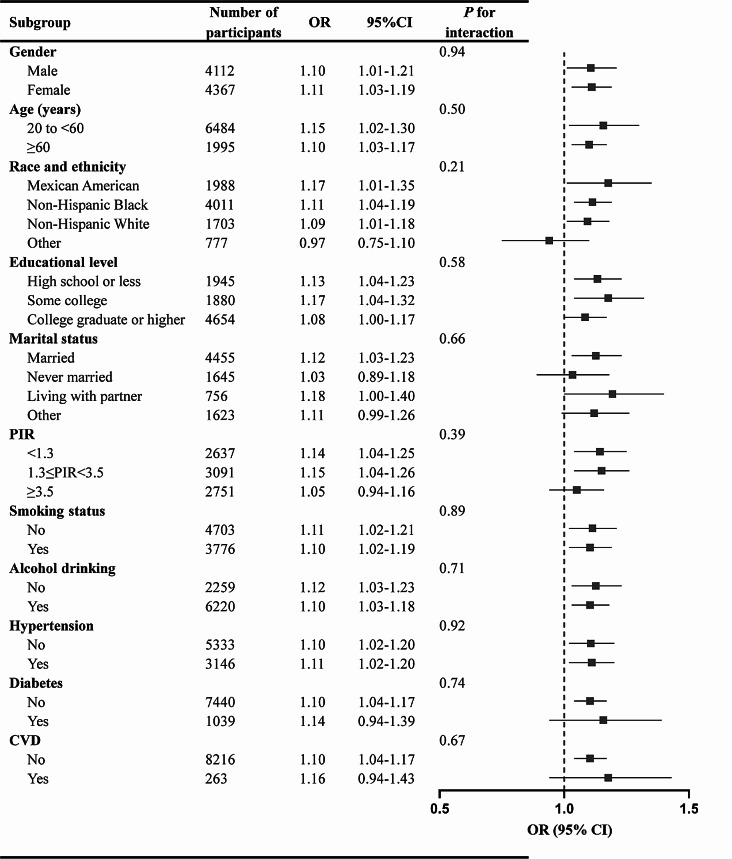
Subgroup analyses
Subsequently, subgroup analyses were performed to ascertain whether the relationship between BRI and psoriasis varied across different subgroups. The findings from the subgroup analysis indicated that there were no statistical differences among various subgroups(P > 0.05), thereby reinforcing the stability of the positive association between BRI and psoriasis across all examined populations (Fig. 3).
Fig. 3.
Subgroup analysis of the effect of body roundness index on psoriasis (N = 8479)
Discussion
Through a cross-sectional study of NHANES data, the findings demonstrated a significant positive association between the BRI and psoriasis. After comprehensive adjustment for covariables, individuals presenting with a higher BRI are at an increased risk for developing psoriasis. BRI is an emerging anthropometric index designed to more accurately reflect an individual’s body shape and fat distribution. The calculation method of BRI emphasizes the importance of waist circumference, which, compared to traditional BMI, better represents abdominal fat distribution, thereby reflecting the accumulation of visceral fat and associated metabolic risks. Obesity is a complex metabolic disease, typically defined as an excessive buildup of body fat that adversely affects overall health, leading to various conditions such as cardiovascular diseases, diabetes, certain cancers, mental health, and psoriasis [15, 16]. The relationship between obesity and psoriasis has been confirmed by numerous studies [17–19], with the risk of psoriasis significantly higher in obese patients compared to those of normal weight. A large-scale retrospective cohort study indicated that the risk of psoriasis escalates in obese individuals, particularly among individuals with a BMI ≥ 30, where the incidence of psoriasis markedly rose [6]. Another study shows that obesity not only increases the incidence of psoriasis but may also lead to worsening of the condition and poor treatment response [20]. Abdominal obesity (i.e., excess visceral fat) is more strongly associated with psoriasis, which may be related to the inflammatory cytokines released by visceral fat, such as leptin and tumor necrosis factor-alpha (TNF-α). These cytokines can promote inflammatory responses and exacerbate the symptoms of psoriasis [21], in contrast, the increase in subcutaneous fat has a relatively small impact on psoriasis [22]. Several studies have demonstrated the relationship between BMI and psoriasis [23–25]. Our research indicates that BRI is positively correlated with an increased risk of psoriasis among American adults, and that BRI may be a better predictor of psoriasis than BMI due to its better response to visceral fat accumulation. Indeed, the waist-to-hip ratio (WHR) is also an important indicator commonly used in clinical practice to assess body shape and fat distribution [26]. Research shows that the BRI has a significant association with the WHR in predicting the risk of cardiovascular diseases and diabetes. An increase in the WHR is positively correlated with the occurrence of cardiovascular diseases, insulin resistance, and diabetes [27–29]. Recent studies have also indicated that BRI can also predict the risk of these diseases. Therefore, both the waist-to-hip ratio and the BRI have their advantages in risk assessment for diseases; the former is more traditional and widely used, while the latter is an emerging assessment method that may provide a more comprehensive risk evaluation. Additional prospective studies are necessary to validate these findings.
The relationship mechanism between BRI and psoriasis may require further exploration, but there are still some possible explanations. Adipose tissue is not only a site for energy storage, but recent studies suggest that it is also an active endocrine organ capable of secreting various inflammatory cytokines, for instance TNF-α and interleukin-6 (IL-6). These cytokines are generally elevated in obese patients, leading to the occurrence of systemic chronic low-grade inflammation. Research shows that obesity-related inflammatory factors can activate the immune system, promoting the onset and worsening of psoriasis [30]. In addition, the increase of inflammatory factors in the skin microenvironment of obese patients may exacerbate the abnormal proliferation of keratinocytes, thereby promoting the pathological changes of psoriasis [31]. In the state of obesity, the functions of macrophages and lymphocytes in adipose tissue are altered, leading to immune system dysregulation [32]. Research shows that obesity can lead to the activation of the NLRP3 inflammasome, further increasing the risk of metabolic diseases and autoimmune diseases such as psoriasis [33]. Recent research results indicate that obesity can induce dysregulation of skin-resident PPARγ (+) Treg cells and promote the exacerbation of IL-17 A-mediated psoriatic inflammation [17]. Obesity is one of the main causes of metabolic syndrome, which is closely related to the occurrence of psoriasis. Studies have shown that obese patients often accompany metabolic abnormalities such as hypertension, hyperglycemia, and hyperlipidemia, all of which can exacerbate the symptoms of psoriasis [34]. In addition, the systemic inflammatory response caused by metabolic syndrome may exacerbate the pathological process of psoriasis by promoting an inflammatory state in the skin [35].
Our research has the following advantages. First, to our knowledge, we established the relationship between BRI and psoriasis for the first time in published studies. Moreover, we determined the linear association between BRI and the risk of psoriasis through multiple regression analysis and RCS curve analysis. These results can help us better understand the association between BRI and psoriasis. Studies using the NHANES database have representative samples with multi-ethnic advantages, and the large sample size also makes our results more stable and generalizable. Therefore, BRI, as a straightforward and user-friendly evaluation tool within clinical practice, can quickly reflect the trend of abdominal obesity in patients and assist clinicians in taking intervention measures such as enhancing dietary habits and promoting physical activity to mitigate the risk of developing psoriasis.
However, our research also has considerable limitations. Firstly, the lack of clinical validation of our findings poses a challenge to the generalizability of the results, as the data was derived from a cross-sectional design. This methodology inherently constrains our capacity to determine causal relationships between BRI and psoriasis. Furthermore, potential biases related to the NHANES dataset, such as sampling variations and the absence of biological markers, may limit the accuracy of our conclusions. Additionally, the reliance on self-reported measures for certain variables may introduce reporting biases that could influence the observed associations. These factors collectively underscore the necessity for future research to incorporate longitudinal studies and experimental designs that can provide a more robust understanding of the association between BRI and psoriasis.
Conclusions
Our study demonstrated that a higher BRI is positively correlated with the risk of psoriasis in the adult population in the US. BRI may regarding as a convenient anthropometric index for more accurately predicting the risk of developing psoriasis. Future studies should delve into the underlying mechanisms and potential benefits of BRI concerning psoriasis through longitudinal and foundational research.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
All authors thank the staff involved in the establishment and maintenance of the NHANES database.
Abbreviations
- BRI
Body roundness index
- NHANES
National health and nutrition examination survey
- OR
Odd ratio
- US
United States
- BMI
Body mass index
- PASI
Psoriasis area and severity index
- CDC
Centers for disease control and prevention
- NCHS
National center for health statistics
- IRB
Institutional review board
- WC
Waist circumference
- PIR
Poverty income ratio
- LDL
Low-density lipoprotein
- TG
Triglyceride
- SD
Standard deviation
- CVD
Cardiovascular disease
- RCS
Restricted cubic spline
- WHR
Waist-to-Hip Ratio
Author contributions
Conceptualization: JB Zhang and GL Bai; Methodology and Statistical analysis: JB Zhang; Data visualization: Q Liu and Y Zhan; Original draft preparation: GL Bai and YT Peng; Draft review and editing: JB Zhang and XY Shao; Funding acquisition: AJ Chen. All authors have read and approved the final version of the manuscript.
Funding
This research was funded by the Natural Science Foundation Project of Chongqing (grant number: 2024NSCQ-LZX0086).
Data availability
The dataset utilized in this research can be accessed at the following website: https://www.cdc.gov/nchs/nhanes/.
Declarations
Ethical approval
The research methodology for NHANES has received approval from the NCHS Institutional Review Board (IRB), with all participants providing informed consent prior to their involvement in the study. As all NHANES data is publicly accessible, no additional IRB approval is required for human research.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Aijun Chen, Email: chenaijun@hospital.cqmu.edu.cn.
Jingbo Zhang, Email: 49554556samael@gmail.com.
References
- 1.Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker. J Psoriasis Lancet. 2021;397(10281):1301–15. [DOI] [PubMed] [Google Scholar]
- 2.Takeshita J, Grewal S, Langan SM, Mehta NN, Ogdie A, Van Voorhees AS, et al. Psoriasis and comorbid diseases: implications for management. J Am Acad Dermatol. 2017;76(3):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armstrong AW, Read C, Pathophysiology. Clinical presentation, and treatment of psoriasis: a review. JAMA. 2020;323(19):1945–60. [DOI] [PubMed] [Google Scholar]
- 4.Gisondi P, Fostini AC, Fossa I, Girolomoni G, Targher G. Psoriasis and the metabolic syndrome. Clin Dermatol. 2018;36(1):21–8. [DOI] [PubMed] [Google Scholar]
- 5.Hsu S, Green LJ, Lebwohl MG, Wu JJ, Blauvelt A, Jacobson AA. Comparable efficacy and safety of brodalumab in obese and nonobese patients with psoriasis: analysis of two randomized controlled trials. Br J Dermatol. 2020;182(4):880–8. [DOI] [PubMed] [Google Scholar]
- 6.Norden A, Rekhtman S, Strunk A, Garg A. Risk of psoriasis according to body mass index: a retrospective cohort analysis. J Am Acad Dermatol. 2022;86(5):1020–6. [DOI] [PubMed] [Google Scholar]
- 7.Setty AR, Curhan G, Choi HK. Obesity, waist circumference, weight change, and the risk of psoriasis in women: nurses’ Health Study II. Arch Intern Med. 2007;167(15):1670–5. [DOI] [PubMed] [Google Scholar]
- 8.Castaldo G, Rastrelli L, Galdo G, Molettieri P, Rotondi Aufiero F, Cereda E. Aggressive weight-loss program with a ketogenic induction phase for the treatment of chronic plaque psoriasis: a proof-of-concept, single-arm, open-label clinical trial. Nutrition. 2020;74:110757. [DOI] [PubMed] [Google Scholar]
- 9.Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obes (Silver Spring). 2013;21(11):2264–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rico-Martin S, Calderon-Garcia JF, Sanchez-Rey P, Franco-Antonio C, Martinez Alvarez M, Sanchez Munoz-Torrero JF. Effectiveness of body roundness index in predicting metabolic syndrome: a systematic review and meta-analysis. Obes Rev. 2020;21(7):e13023. [DOI] [PubMed] [Google Scholar]
- 11.Cai X, Song S, Hu J, Zhu Q, Yang W, Hong J, et al. Body roundness index improves the predictive value of cardiovascular disease risk in hypertensive patients with obstructive sleep apnea: a cohort study. Clin Exp Hypertens. 2023;45(1):2259132. [DOI] [PubMed] [Google Scholar]
- 12.Gao W, Jin L, Li D, Zhang Y, Zhao W, Zhao Y, et al. The association between the body roundness index and the risk of colorectal cancer: a cross-sectional study. Lipids Health Dis. 2023;22(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang X, Ding L, Hu H, He H, Xiong Z, Zhu X. Associations of body-roundness index and Sarcopenia with Cardiovascular Disease among Middle-aged and older adults: findings from CHARLS. J Nutr Health Aging. 2023;27(11):953–9. [DOI] [PubMed] [Google Scholar]
- 14.Zhang X, Ma N, Lin Q, Chen K, Zheng F, Wu J, et al. Body roundness index and all-cause Mortality among US adults. JAMA Netw Open. 2024;7(6):e2415051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Piche ME, Tchernof A, Despres JP. Obesity phenotypes, diabetes, and Cardiovascular diseases. Circ Res. 2020;126(11):1477–500. [DOI] [PubMed] [Google Scholar]
- 16.Takeshita J, Grewal S, Langan SM, Mehta NN, Ogdie A, Van Voorhees AS, et al. Psoriasis and comorbid diseases: Epidemiology. J Am Acad Dermatol. 2017;76(3):377–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sivasami P, Elkins C, Diaz-Saldana PP, Goss K, Peng A, Hamersky Mt, et al. Obesity-induced dysregulation of skin-resident PPARgamma(+) Treg cells promotes IL-17A-mediated psoriatic inflammation. Immunity. 2023;56(8):1844–61. e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kunz M, Simon JC, Saalbach A, Psoriasis. Obesity and fatty acids. Front Immunol. 2019;10:1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jensen P, Skov L. Psoriasis Obes Dermatology. 2016;232(6):633–9. [DOI] [PubMed] [Google Scholar]
- 20.Vata D, Tarcau BM, Popescu IA, Halip IA, Patrascu AI, Gheuca Solovastru DF et al. Update on obesity in Psoriasis patients. Life (Basel). 2023;13(10). [DOI] [PMC free article] [PubMed]
- 21.Bavoso NC, Pinto JM, Soares MMS, Diniz MDS, Teixeira Junior AL. Psoriasis in obesity: comparison of serum levels of leptin and adiponectin in obese subjects - cases and controls. Bras Dermatol. 2019;94(2):192–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Constantin C, Surcel M, Munteanu A, Neagu M. Insights into nutritional strategies in Psoriasis. Nutrients. 2023;15(16). [DOI] [PMC free article] [PubMed]
- 23.Budu-Aggrey A, Brumpton B, Tyrrell J, Watkins S, Modalsli EH, Celis-Morales C, et al. Evidence of a causal relationship between body mass index and psoriasis: a mendelian randomization study. PLoS Med. 2019;16(1):e1002739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu MY, Yu CL, Yang SJ, Chi CC. Change in body weight and body mass index in psoriasis patients receiving biologics: a systematic review and network meta-analysis. J Am Acad Dermatol. 2020;82(1):101–9. [DOI] [PubMed] [Google Scholar]
- 25.Puig L. Obesity and psoriasis: body weight and body mass index influence the response to biological treatment. J Eur Acad Dermatol Venereol. 2011;25(9):1007–11. [DOI] [PubMed] [Google Scholar]
- 26.White H, Chroust A, Jubran R, Heck A, Bhatt RS. Waist-to-hip ratio sensitivity in early infancy. Infant Child Dev. 2020;29(3). [DOI] [PMC free article] [PubMed]
- 27.Kulaga Z, Swiader-Lesniak A, Kotowska A, Litwin M. Population-based references for waist and hip circumferences, waist-to-hip and waist-to-height ratios for children and adolescents, and evaluation of their predictive ability. Eur J Pediatr. 2023;182(7):3217–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khanna D, Peltzer C, Kahar P, Parmar MS. Body Mass Index (BMI): a Screening Tool Analysis. Cureus. 2022;14(2):e22119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jang SY, Kim J, Kim S, Lee ES, Choi EJ. [Impact of Anthropometric Indices of Obesity on the risk of Incident Hypertension in adults with prehypertension: a secondary analysis of a Cohort Study]. J Korean Acad Nurs. 2024;54(1):18–31. [DOI] [PubMed] [Google Scholar]
- 30.Ikeda K, Morizane S, Akagi T, Hiramatsu-Asano S, Tachibana K, Yahagi A et al. Obesity and Dyslipidemia synergistically exacerbate psoriatic skin inflammation. Int J Mol Sci. 2022;23(8). [DOI] [PMC free article] [PubMed]
- 31.Teklu M, Parel PM, Mehta NN. Psoriasis and Cardiometabolic diseases: the impact of inflammation on Vascular Health. Psoriasis (Auckl). 2021;11:99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Altun I, Yan X, Ussar S. Immune Cell Regulation of White Adipose Progenitor Cell Fate. Front Endocrinol (Lausanne). 2022;13:859044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu KK, Cheung SW, Cheng KK. NLRP3 inflammasome activation in adipose tissues and its implications on metabolic diseases. Int J Mol Sci. 2020;21(11). [DOI] [PMC free article] [PubMed]
- 34.Cho SI, Kim YE, Jo SJ. Association of Metabolic Comorbidities with Pediatric Psoriasis: a systematic review and Meta-analysis. Ann Dermatol. 2021;33(3):203–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rathod A, Neema S, Radhakrishnan S, Vendhan S, Tripathy DM, Vasudevan B. Palmoplantar Plaque Psoriasis is Associated with diabetes, hypertension, obesity, and metabolic Syndrome-A case-control study. Indian Dermatol Online J. 2022;13(5):606–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset utilized in this research can be accessed at the following website: https://www.cdc.gov/nchs/nhanes/.