Abstract
Hip disorders in infants and children may result from congenital, infectious, developmental, inflammatory, neoplastic, and traumatic etiologies. Postoperative pain management associated with hip pathologies can be challenging especially due to complex innervation of the hip and surrounding structures. Given the adverse effect profile of systemic opioids, regional anesthesia offers an excellent alternative with more beneficial adverse effect profile. Various peripheral regional anesthetic techniques have been reported with variable results regarding analgesia and differing adverse effect profiles. The pericapsular nerve group (PENG) block is a novel motor-sparing regional anesthetic technique where the local anesthetic agent is deposited in the musculofascial plane between the psoas tendon and the pubic ramus. The main target is the genicular branches of the femoral, obturator, and accessory obturator nerve, which innervate the hip capsule. The anatomy involved with PENG block is reviewed and previous reports of PENG block in pediatric-aged patients, including single shot or continuous catheter techniques, are reviewed.
Keywords: regional anesthesia, orthopedic surgery, pediatric anesthesiology, pericapsular nerve group block, lateral femoral cutaneous nerve block
Introduction
Orthopedic procedures involving the hip, femur, and upper thigh in pediatric patients are associated with moderate-to-severe postoperative pain.1,2 While there are various options for controlling pain, regional anesthetic blockade is frequently chosen to supplement general anesthesia intraoperatively and provide postoperative analgesia following major orthopedic surgery involving the hip and femur.3–5 Various regional anesthetic techniques have been shown to decrease intraoperative volatile anesthetic requirements, decrease opioid consumption postoperatively, and reduce the time to discharge.6,7 Limiting the need for perioperative systemic opioid administration improves the postoperative course and decreases opioid-related adverse effects including nausea, vomiting, confusion, constipation, respiratory depression, and sedation. The initial experience with regional anesthesia in infants and children included primarily neuraxial techniques such as lumbar and caudal epidural anesthesia. However, with advances in regional anesthesia including the use of point-of-care ultrasound, neuraxial blocks are being replaced with peripheral nerve blockade to achieve a selective unilateral blockade for procedures involving the hip and thigh.8–12
Initial Reports of PENG Blockade in Adults
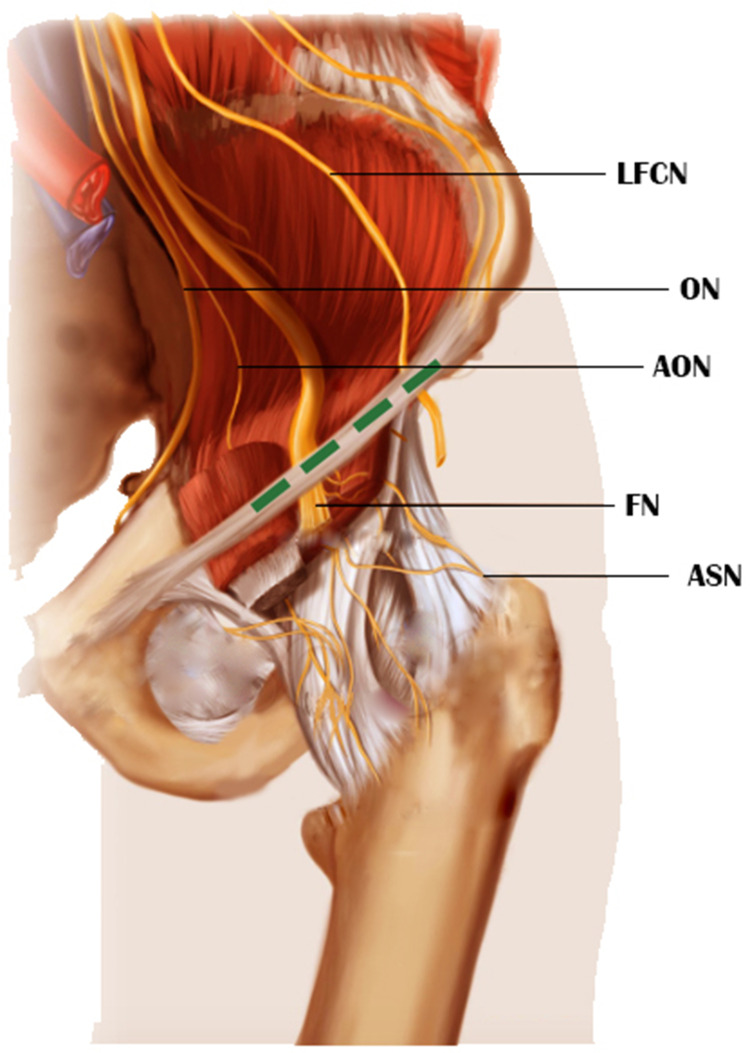
In 2018, the pericapsular nerve group (PENG) block was first described by Girón-Arango L et al.13 These investigators studied the innervation of the capsule of the hip joint, noting that the anterior aspect of the capsule is much more richly innervated than the posterior aspect. Therefore, the nerves providing sensation to the hip capsule itself should be the crucial target for analgesia of the hip. As the hip capsule is innervated anteriorly by branches of the femoral nerve (FN), obturator nerve (ON), and accessory obturator nerve (AON), Girón-Arango et al identified the target point for injection for successful PENG block, as the myofascial plane between the ilio-pubic ramus posteriorly and the psoas tendon anteriorly (Figures 1 and 2). Due to the proximity of this target point to the subpectineal plane, the articular branches (genicular nerves) of the ON can also be successfully blocked by the novel technique.
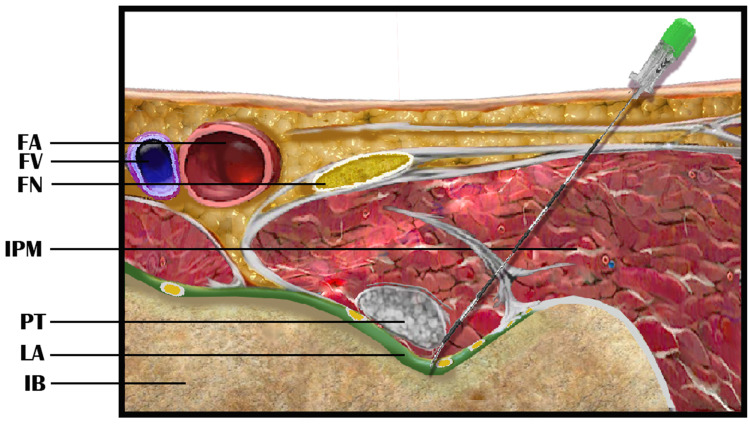
Figure 1.
Diagram showing the technique for pericapsular nerve group (PENG) block. The needle is inserted from a lateral to medial direction using an in-plane approach under ultrasound guidance. The tip of the needle should target the myofascial plane between the iliac bone (IB) anteriorly and the psoas tendon (PT) posteriorly. Anterior displacement of the PT during local anesthetic (LA) agent injection can be used to confirm the correction location of the injection. FA: femoral artery; FV: femoral vein; FN: femoral nerve; IPM: Iliopsoas muscle.
Figure 2.
Diagram showing the innervation of the Hip and hip capsule including the femoral nerve (FN) and the lateral femoral cutaneous nerve (LFCN). The dashed green line showing ultrasound probe position for PENG block. ON: obturator nerve; AON: accessory obturator nerve; ASN: Articular sensory nerve.
Girón-Arango et al applied this novel motor sparing regional anesthetic technique in 5 elderly patients (62–80 years old), ASA II–VI, undergoing surgical procedures for various pathology of the hip and femur (two intertrochanteric fractures, two subcapital fractures, and one metastatic tumor to the femoral head and acetabulum).13 The PENG block was performed while the patients were supine, using a curvilinear low-frequency ultrasound probe. Four patients received 20 mL of 0.25% bupivacaine with 1:400,000 epinephrine and one patient had received 20 mL of 0.5% ropivacaine with both epinephrine 1:200,000 and 4 mg of dexamethasone. All patients were evaluated 30 minutes after placement of the PENG block by assessing pain response to hip flexion and 15° straight leg raising of the fractured side. The PENG block was successful in all 5 patients as they were comfortable, reporting significant dynamic pain relief (median reduction of pain was 7 points). No (quadriceps) muscle weakness was noted.13
The initial case series was followed by randomized controlled trials in adults, which had been conducted to compare this novel regional technique (PENG block) with traditional types of regional anesthesia (fascia iliaca compartment block [FICB], either single shot or continuous catheter infusions).14,15 In a prospective trial in 90 adults with a femoral shaft fracture, following placement of spinal anesthesia, the patients were randomized to receive either a PENG block (n=45) with 20 mL of 0.25% bupivacaine or a FICB (n=45) with 30 mL of 0.25% bupivacaine.16 The authors used a Visual Analog Scale (VAS) scores to assess pain at rest and with passive leg raise to 15° before and 30 minutes after the block. No difference was noted in pain at rest and with passive left raise to 15° before the block, while 30 minutes after performing the PENG block, the VAS scores at rest and passive leg raise were significantly less than FICB.
Current understanding of the PENG block’s mechanism of action is largely based on studies conducted on cadavers. To further investigate the analgesic mechanisms following a PENG block, Balocco et al conducted an imaging study involving 10 patients scheduled for hip surgery. These patients received an ultrasound-guided PENG block involving 18 mL of 0.5% ropivacaine mixed with 2 mL of a contrast agent. Following the block, a high-resolution CT scan was performed to create a three-dimensional reconstruction of the injectate’s distribution. Notably, the injectate was primarily contained within the epimysium of the iliacus and psoas muscles, with limited spread to the hip capsule. Contrast dye was identified in the iliacus and/or the psoas muscle in all patients, but no spread to the subpectineal plane or obturator foramen was observed.17
Initial Reports of PENG Blockade in Pediatric-Aged Patients
Subsequently, preliminary data suggested the potential utility of the PENG block in pediatric-aged patients. In 2019, Orozco et al reported the report of the use of a PENG block in a pediatric-age patient, an 8-year-old child scheduled for removal of osteo-synthesis material from left hip.18 The patient had a femoral fracture secondary to a large metaphyseal cyst for which corrective surgery with bone grafting and hip osteosynthesis was performed 10 months earlier. After the induction of general anesthesia, PENG, FN, and LFCN blocks were performed using linear high-frequency probe. No intraoperative opioids were administered. The pain score was 2/10 without additional analgesia during first 72 postoperative hours.
To date, there are no prospective randomized trials of PENG blockade in pediatric-aged patients. Table 1 summarizes previous case reports and case series of PENG blockade in pediatric-aged patients.18–27 Our review of literature identified a total of 10 publications (6 case reports and 4 case series) with a total of 16 patients. The patients ranged from 2 to 16 years old and in weight from 14.3 to 45.7 kg. The indications for this novel regional block varied, including hip fracture, developmental dysplasia of the hip, and congenital dysplasia of the hip. The majority of patients (n=14) received general anesthesia with a PENG block while two patients received spinal anesthesia and a PENG block. Fifteen patients received a unilateral technique while one patient received bilateral blockade. A LFCN block was performed in addition to the PENG block in 2 of the 16 patients, while an erector spinae plane (ESP) block was performed at the L4 vertebral level in addition to the PENG block in one patient. A single-shot technique was reported in 15 patients, while a continuous infusion via an indwelling catheter was used in one patient.
Table 1.
Case Reports of PENG Block (Single Shot or Catheter) in Pediatric Patients
| Authors | Age/sex | Single shot/Catheter | Anesthesia type/Comments |
|---|---|---|---|
| Orozco S et al18 | Eight-year-old. | Unilateral, single shot. | General anesthesia. Open hip surgery for removal of osteo-synthesis material. 10 mL of 0.5% bupivacaine containing epinephrine was injected in the musculofascial plane between the psoas tendon and pubic ramus (PENG block). In addition, femoral and LFC nerve blocks were performed. Pain score was 2/10 without additional analgesia during first 72 postoperative hours. |
| Aksu C et al19 | Eight-year-old boy, 15 kg. | Unilateral, single shot. | General anesthesia. Elective CDH surgery. 10 mL of 0.25% bupivacaine was deposited at the target point for PENG block. The surgery lasted 3 hours. Patient received one dose of oral ibuprofen during the first 24 postoperative hours. |
| Wyatt K et al20 | Nine-year-old girl, 45.7 kg. | Unilateral, catheter. | General anesthesia. Repair of traumatic femoral neck fracture. Unilateral injection of 14 mL of bupivacaine 0.25%. At the end of the procedure, a PENG catheter was placed and threaded to a depth of 7 cm (2 cm beyond the needle tip). Postoperative infusion of 0.1% ropivacaine at 6 mL/hr. FLACC score was 0/10. Infusion was discontinued on POD 1. No complications reported. |
| Ince I et al21 | Four-year-old girl, 17 kg. | Unilateral, single shot. | General anesthesia. Pemberton and proximal femur varus derotational osteotomy for CDH. A total of 20 mL (8 mL for PENG and 12 mL for ESP block) of 0.25% bupivacaine. ESP block was performed at the L4 level. The surgical procedure lasted 95 minutes. FLACC score was 0–1. There was no need for additional analgesic agents postoperatively. No complications. |
| Acharya U et al22 | Case series of 9 adults and one 16-year-old adolescent male. | Unilateral, single shot. | Spinal anesthesia. Subtrochanteric hip fracture. PENG block was performed to help in sitting positioning of patients before SAB. A total of 20 mL of 0.125% bupivacaine with 4 mg dexamethasone administered using ultrasound guided out-of-plane technique. PENG block was performed as an alternative regional anesthetic technique to prevent positional pain with hip fracture. NRS was 6 before the block and decreased to 1 following PENG block. Patients tolerated sitting position for SAB |
| Anido Guzmán JA et al23 | Five-year-old girl, 16 kg. | Bilateral, single shot. | General anesthesia. Varus derotational osteotomy and adductor tenotomy. Bilateral injection of 10 mL of 0.25% bupivacaine without epinephrine at the target point and 3 mL of the same local anesthetic concentration near the LFC nerve. The FLACC score was 0–1 until discharge 48 hours postoperatively. |
| Xu M et al24 | Seven-year-old girl, 16 kg. | Unilateral, single shot. | General anesthesia. Open left hip surgery for DDH. The preoperative CT scan showed spina bifida and myelomeningocele. PENG block with 2.5 mL/kg of 0.2% ropivacaine at the target point. The surgical procedure lasted 100 minutes. Pain score was 2/10 during the first 24 postoperative hours with a sufentanil infusion at 0.05 μg/kg/h. |
| Yörükoğlu HU et al,25 | Five patients, 10–20 months of age. | Single shot. | General anesthesia. DDH surgery. PENG block with 0.5 mL/kg of 0.25% bupivacaine. FLACC scores were between 0 and 2 during the first 24 hours. Two patients received paracetamol. No other analgesic agents were used during the first 24 postoperative hours. No complications. |
| Domagalska M et al26 | Four-year-old, 14.3 kg, male and two-year-old, 18 kg female. | Unilateral, single shot | General anesthesia for the first patient and SAB for the second patient. Transiliac osteotomy with femoral subtrochanteric osteotomy. After the induction of general anesthesia in patient 1, PENG block was performed with 7.5 mL of 0.2% ropivacaine. The procedure lasted 105 minutes. The highest FLACC score was 3/10. After SAB in the second patient, PENG block was performed with 5 mL of 0.2% ropivacaine. The procedure lasted 75 minutes. The highest FLACC score was 2/10. Neither patient required supplemental opioids. Both participated in physical therapy on POD 1. No complications. |
| Irrou R et al27 | Four-year-old, 15 kg girl and 2-year-old, 12 kg male. | Unilateral, single shot | General anesthesia. Open hip surgery for DDH for the first patient and Dega trans-iliac osteotomy with femoral subtrochanteric osteotomy for the second. PENG blocks were performed with 1.25 mL/kg of 0.2% ropivacaine. FLACC scores were 2–3 of 10. Both patients participated in physical therapy on POD 1. No complications. |
Abbreviations: PENG, pericapsular nerve group; CDH, congenital dysplasia of the hip; DDH, developmental dysplasia of the hip; FLACC, face, legs, activity, cry, and consolability score; POD, postoperative day; LFC, lateral femoral cutaneous; ESP, erector spinae plane; NRS, Numeric rating scale; SAB, subarachnoid block; FICB, fascia iliaca compartment block.
Various regimens including different volumes and type of local anesthetic agents were used for the PENG blocks. None of the anecdotal experience has examined the effect of different local anesthetic agents, concentrations, volumes, or additives in either adults or pediatrics. A cadaveric study of Çiftçi et al showed that 30 mL compared to 20 mL of dye resulted in a more extensive spread from the insertion site around the FN, LFCN, and ON.28 The authors concluded that PENG block is a safe and effective method for providing analgesia after hip surgery, but they did caution regarding the potential for motor blockade especially with high volumes of the local anesthetic agent.28
In clinical practice, in both adults and children, various volumes and concentrations of local anesthetic agents have been used. Girón-Arango et al performed the PENG block in 4 of 5 patients with 20 mL of 0.25% bupivacaine with epinephrine 1:400,000. In general, a higher volume of the local anesthetic solution (20–30 mL of 0.25–0.5% bupivacaine or levobupivacaine with or without epinephrine) has been used in the majority of published case reports and case series describing PENG blocks in adults. In terms of adjunctive agents, epinephrine, dexamethasone, and dexmedetomidine have been reported in the adult literature.13,29–31 In a prospective, randomized, double-blinded trial in 28 adult hip surgery patients, the addition of dexamethasone (8 mg) to the local anesthetic solution of PENG (20 mL of 0.5% ropivacaine) resulted in decreased pain scores and rest and with movement.30 Additionally, patients in the dexamethasone group had a longer time to the first request for postoperative rescue analgesia (445.0 ± 17.4 versus 388.9 ± 19.0 minutes, p<0.05) and lower postoperative dose requirements for rescue analgesia. Kangarli N et al reported that the addition of dexmedetomidine (100 µg) to the PENG block solution (15 mL of 0.5% bupivacaine and 5 mL of 2% lidocaine) also reduced postoperative rescue opioid doses and bolus patient-controlled analgesia (PCA) doses.31 To date, the only adjuncts reported in pediatric-aged patients include the addition of epinephrine to the local anesthetic solution and a single-case report regarding the use of dexamethasone (4 mg).22
In the pediatric age group, there has been no clear dosing regimen determined for the volume or concentration of the local anesthetic agent. Volumes of the local anesthetic reported for single-shot PENG block ranged from 5 to 20 mL depending on the size of the patient. The local anesthetic used included 0.25% bupivacaine, 0.5% bupivacaine, and 0.2% ropivacaine, while one report used 0.1% ropivacaine for catheter infusion.18–27 Outcomes of the PENG blocks have generally been favorable with the majority of authors using the FLACC pain scale to assess analgesia. The studies have reported adequate analgesia without significant adverse effects, such as quadriceps weakness, rupture of bursa, local anesthetic systemic toxicity, hematoma, or infection.
Regarding continuous nerve block (PENG block catheter), just one pediatric case report has been reported in literature.20 PENG block catheter has the same indications as for single shot; however, it lasts longer (several days) especially for complex surgical procedures during which the expected postoperative pain is much higher or in patients who may need extended relief to improve recovery and mobilization. Continuous catheters reduce the need for systemic opioids, helping minimize opioid-related side effects, such as nausea, constipation, and respiratory depression. It is noteworthy that although the literature is still limited, there are few reports of complications resulting from the performance of PENG block catheter in adults, such as intravascular catheter migration/cannulation, infection, potential catheter displacement due to self-removal in uncooperative patients, and local anesthetic systemic toxicity (LAST).32
Anatomy and Performance of the PENG Block
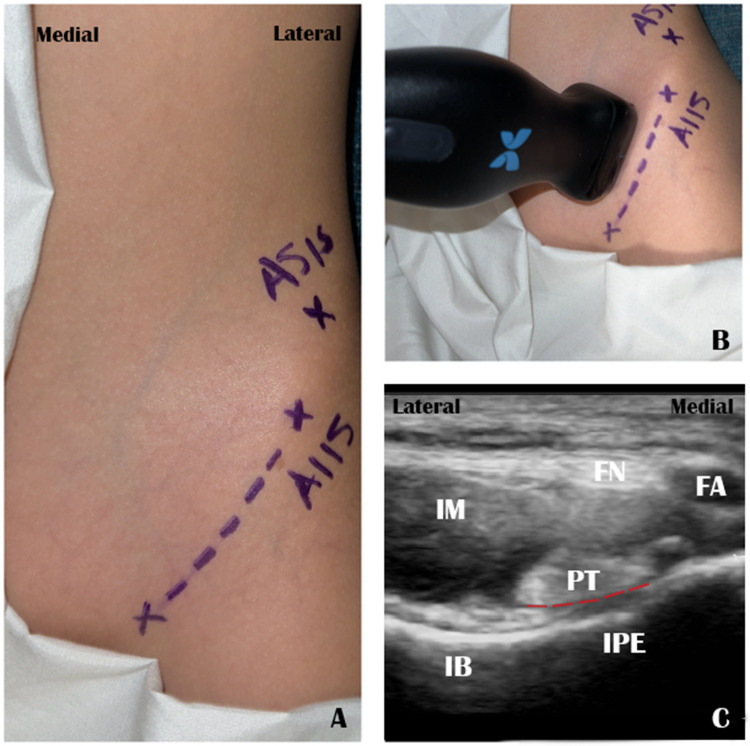
To perform the PENG block, 6 anatomical structures needed to be identified including four bony or ligamentous structures and two major muscles (Figures 1 and 2). The bony and ligamentous structures include the anterior superior iliac spine (ASIS), anterior inferior iliac spine (AIIS), inguinal ligament (IL), and symphysis pubis. The two major muscles are the psoas major and the iliacus. The principal function of both muscles is hip flexion. The genicular branches of the femoral and accessory obturator nerves can be found between the AIIS and the iliopubic eminence (IPE). To obtain the ideal ultrasound image, the patient is positioned in the supine position. The high frequency linear probe (instead of the curved low-frequency probe used by Girón et al) may be preferable in pediatric-aged patients given the characteristic lower depth of the anatomical structures. The probe is initially aligned with the pubic ramus to visualize the AIIS, femoral artery, FN, psoas tendon, and IPE (a ridge on the hip bone marking the junction of the ilium and the pubis), while the patient is in supine position. As the needle is directed from the lateral to the medial direction (in-plane approach), the tip should target the myofascial plane between the ilium anteriorly and the psoas tendon posteriorly (Figure 3). One of the confirming signs of effective PENG block is observing anterior displacement of the psoas tendon when the local anesthetic agent is injected.33,34
Figure 3.
Picture showing optimum position of the linear ultrasound probe on a child for the PENG block (A: anatomical landmarks, (B) optimum probe position, (C) ultrasound image of PENG block). The dashed red line on the ultrasound image is the target point for the deposition of the local anesthetic agent to block the genicular branches of FN, ON, and AON. ASIS: anterior superior iliac spine; AIIS: anterior inferior iliac spine; IPE: Iliopectineal eminence; IM: iliacus muscle; IB: iliac bone; FN; femoral nerve; FA: femoral artery; PT: psoas tendon.
As many surgical procedures on the hip include an incision on the lateral aspect of the thigh, the PENG block may be combined with an LFCN block to provide sensory blockade to the incisional site on the lateral aspect of the hip. The LFCN is a sensory nerve that originates from the lumbar plexus (posterior division of L2 and L3), with significant anatomic variability, especially at the level of the IL and ASIS. The LFCN exits the pelvis, travelling over the sartorius or between the fascial layers of the sartorius and the tensor fasciae latae muscles. The LFCN terminates by dividing into two main branches including the anterolateral branch to innervate the anterolateral thigh (including the knee joint) and a posterior branch to the greater trochanteric region. Distally, both branches run subcutaneously.35
Three anatomical structures needed to be identified to perform LFCN block including the ASIS and two muscles (sartorius and tensor fascia latae). The LFCN is generally located 1–2 centimeters medial and inferior to ASIS, within almost 1 cm from the skin surface. While the patient is still in supine position, a higher frequency superficial ultrasound probe should be applied axially caudad to ASIS. Both the sartorius and tensor fascia latae are easily identified superficial to rectus femoris. Superficial to these two muscles, the fat canal bounded by two fascial layers can be demonstrated. The LFCN can be visualized inside this fat canal as small honeycomb structures (oval hypoechoic small structure with a hyperechoic rim).35
Potential Adverse Events of PENG Block
Apart from the general complications of peripheral nerve blockade (eg, infection, bleeding, paresthesia, neuropathy, allergic reaction from medication, catheter dislodgment, local anesthetic leakage, local anesthetic systemic toxicity), the PENG block has specific adverse effects. Although the PENG block is intended to be a motor-sparing technique, inadvertent muscle (quadriceps) weakness had been reported in adult patients following application (≥25%).34 There are three primary contributing factors that may increase the incidence of quadriceps weakness after PENG block including a high injecting pressure (pressure overload), high injecting volume (volume overload), and inadvertent injection of the iliopectineal bursa (bursal rupture). All these factors result in spread of the injectate anteromedially to surround the FN, causing unwanted muscle weakness.36
Yu et al hypothesized that a more superficial injection point of the local anesthetic agent or needle placement medial to the psoas tendon (rather than posterior) may result in superficial spread of a significant proportion of the local anesthetic agent causing inadvertent FN block or FICB. Moreover, postoperative performance of the block may allow spread of the local anesthetic to unanticipated locations due to normal tissue planes being disrupted by the surgical procedure. Therefore, PENG block is one of the analgesic techniques of choice for the hip procedures when post-procedural quadriceps weakness is not an immediate concern. However, in situations where early mobilization is crucial (eg, enhanced recovery after surgery clinical pathway after total hip arthroplasty), the potential for motor blockade of the FN with PENG block should be considered.37
Although the technique is performed using ultrasound-guidance, there is the potential for inadvertent needle injury to surrounding or deep structures including the FN, LFCN, or even the ureter. However, no such injuries have been reported following PENG block. Prior to needle insertion, the FN should be identified during the scanning phase of PENG block. As the pelvic part of the ureter lies on the pelvic wall near the ON, it has the potential to be injured by a more medial needle advancement or a medial to lateral needling technique.
Limitation of Regional Anesthesia in Pediatric Age Group
Whereas, the application of regional anesthesia in infants, children, and adolescents has significantly improved the scope of pediatric pain management, there are still several limitations and considerations with these techniques. Contrary to the adult age group, where most regional anesthetic techniques are performed awake or with mild sedation, regional anesthetic techniques in children and infants are generally performed after the induction of general anesthesia. Given size and volume constraints in infants and children, strict adherence to recommended dosing guidelines for local anesthetic agents is required for both single shot and continuous techniques. Local anesthetic system toxicity (neurotoxicity and cardiotoxicity) is more likely to occur in infants and young children than in adults because of decreased clearance and low protein binding. Judicious local anesthetic dosing should be applied to avoid excessive motor blockade (quadriceps weakness) which could prevent patient ambulation and active participation in physical therapy.38
Conclusion
Although increasingly used in the adult population, clinical experience with the PENG in the pediatric-aged patient remains anecdotal and primarily retrospective with the majority of clinical information contained in single-case reports or small case series. The reported literature regarding the use of PENG block in pediatric patients includes 16 patients from 10 different publications (6 case reports and 4 case series). Future trials are needed to clearly identify the optimal surgical procedures for which a PENG block may be indicated, effective dosing volumes and concentrations, and the utility of adjunctive agents in addition to the local anesthetic agent.
These trials should compare the PENG block with other peripheral nerve blockade (FN block or FICB) and central neuraxial techniques (epidural anesthesia or lumbar plexus block). In general, the PENG block has demonstrated motor-sparing effects with a limited incidence of FN blockade, making it a potential alternative to more complex procedures like the lumbar plexus block. However, prospective, randomized trials are needed to assess its true clinical value and efficacy in the pediatric age group.
Acknowledgments
The authors acknowledge Nema Shaltoot for her effort in drawing all figures for this study.
Reflective Questions
How does the analgesic efficacy of PENG block compare to other regional anesthetic techniques in pediatric-aged patients following hip and femur surgery?
Are there specific indications other than hip surgery for PENG block in infants and children?
What is the optimal volume and concentration of the local anesthetic agent for PENG block in pediatric patients?
Is there any advantage to using adjuncts in addition to the local anesthetic agent such as dexamethasone?
How can we minimize the risk of quadriceps muscle weakness after PENG block?
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Eastburn E, Hernandez M, Boretsky K. Technical success of the ultrasound-guided supra-inguinal fascia iliaca compartment block in older children and adolescents for hip arthroscopy. Pediatr Anesth. 2017;27:1120–1124. [DOI] [PubMed] [Google Scholar]
- 2.Desmet M, Vermeylen K, Van Herreweghe I, et al. A longitudinal supra-inguinal fascia iliaca compartment block reduces morphine consumption after total hip arthroplasty. Reg Anesth Pain Med. 2017;42(3):327–333. doi: 10.1097/AAP.0000000000000543 [DOI] [PubMed] [Google Scholar]
- 3.Ross AK, Eck JB, Tobias JD. Pediatric regional anesthesia: beyond the caudal. Anesth Analg. 2000;91(1):16–26. doi: 10.1213/00000539-200007000-00004 [DOI] [PubMed] [Google Scholar]
- 4.Shamim R, Prasad G, Bais PS, et al. Ultrasound-guided suprainguinal fascia iliaca compartment block in patients undergoing Hip and femur surgeries: a retrospective analysis. Anesth Essays Res. 2020;14(3):525–530. doi: 10.4103/aer.AER_9_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray JM, Derbyshire S, Shields MO. Lower limb blocks. Anaesthesia. 2010;65(s1):57–66. doi: 10.1111/j.1365-2044.2010.06240.x [DOI] [PubMed] [Google Scholar]
- 6.Wong J, Marshall S, Chung F, Sinclair D, Song D, Tong D. Spinal anesthesia improves the early recovery profile of patients undergoing ambulatory knee arthroscopy. Can J Anaesth. 2001;48(4):369–374. doi: 10.1007/BF03014965 [DOI] [PubMed] [Google Scholar]
- 7.Rappaport B, Mellon RD, Simone A, Woodcock J. Defining safe use of anesthesia in children. N Engl J Med. 2011;364(15):1387–1390. doi: 10.1056/NEJMp1102155 [DOI] [PubMed] [Google Scholar]
- 8.Schloss B, Bhalla T, Klingele K, Phillips D, Prestwich B, Tobias JD. A retrospective review of femoral nerve block for postoperative analgesia after knee surgery in the pediatric population. J Pediatr Orthop. 2014;34(4):459–461. doi: 10.1097/BPO.0000000000000113 [DOI] [PubMed] [Google Scholar]
- 9.Dadure C, Raux O, Gaudard P, et al. Continuous psoas compartment blocks after major orthopedic surgery in children: a prospective computed tomographic scan and clinical studies. Anesth Analg. 2004;98:623–628. doi: 10.1213/01.ANE.0000100662.87610.16 [DOI] [PubMed] [Google Scholar]
- 10.Manion SC, Tobias JD. Lumbar plexus blockade in children. Amer J Pain Manage. 2005;15:120–126. [Google Scholar]
- 11.Villalobos MA, Veneziano G, Miller R, et al. Evaluation of postoperative analgesia in pediatric patients after hip surgery: lumbar plexus block versus caudal epidural analgesia. Loco Reg Anesth. 2019;12:997–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dalens B, Tanguy A, Vanneuville G. Lumbar plexus block in children: a comparison of two procedures in 50 patients. Anesth Analg. 1988;67(8):750–758. doi: 10.1213/00000539-198808000-00006 [DOI] [PubMed] [Google Scholar]
- 13.Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular nerve group (PENG) block for Hip fracture. Reg Anesth Pain Med. 2018;43(8):859–863. doi: 10.1097/AAP.0000000000000847 [DOI] [PubMed] [Google Scholar]
- 14.Natrajan P, Bhat RR, Remadevi R, Joseph IR, Vijayalakshmi S, Paulose TD. Comparative study to evaluate the effect of ultrasound-guided pericapsular nerve group block versus fascia iliaca compartment block on the postoperative analgesic effect in patients undergoing surgeries for hip fracture under spinal anesthesia. Anesth Essays Res. 2021;15(3):285–289. doi: 10.4103/aer.aer_122_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duan L, Zhang L, Shi CG, et al. Comparison of continuous pericapsular nerve group (PENG) block versus continuous fascia iliaca compartment block on pain management and quadriceps muscle strength after total hip arthroplasty: a prospective, randomized controlled study. BMC Anesthesiol. 2023;23(1):233. doi: 10.1186/s12871-023-02190-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalashetty MB, Channappagoudar R, Alwandikar V, Naik DL, Hulakund SY, Guddad A. Comparison of pericapsular nerve group block with fascia iliaca compartment block in adult patients undergoing Hip surgeries: a double-blinded randomized control study. Anesth Essays Res. 2022;16(3):397–401. doi: 10.4103/aer.aer_123_22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balocco AL, Gautier N, Van Boxstael S, et al. Pericapsular nerve group block: a 3D CT scan imaging study to determine the spread of injectate. Reg Anesth Pain Med. 2024;rapm–2024–105459. [DOI] [PubMed] [Google Scholar]
- 18.Orozco S, Muñoz D, Jaramillo S, Herrera AM. Pediatric use of pericapsular nerve group (PENG) block for hip surgical procedures. J Clin Anesth. 2019;57:143–144. doi: 10.1016/j.jclinane.2019.04.010 [DOI] [PubMed] [Google Scholar]
- 19.Aksu C, Cesur S, Kuş A. Pericapsular nerve group (PENG) block for postoperative analgesia after open reduction of pediatric congenital dysplasia of the Hip. J Clin Anesth. 2020;61:109675. doi: 10.1016/j.jclinane.2019.109675 [DOI] [PubMed] [Google Scholar]
- 20.Wyatt K, Zidane M, Liu CJ. Utilization of a continuous pericapsular nerve group (PENG) block with an opioid-sparing repair of a femoral neck fracture in a pediatric patient. Case Rep Orthop. 2020;2020:2516578. doi: 10.1155/2020/2516578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ince I, Kilicaslan A, Kutlu E, Aydin A. Combined pericapsular nerve block (PENG) and lumbar erector spinae plane (ESP) block for congenital hip dislocation surgery. J Clin Anesth. 2020;61:109671. doi: 10.1016/j.jclinane.2019.109671 [DOI] [PubMed] [Google Scholar]
- 22.Acharya U, Lamsal R. Pericapsular nerve group block: an excellent option for analgesia for positional pain in hip fractures. Case Rep Anesthesiol. 2020;2020:1830136. doi: 10.1155/2020/1830136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anido Guzmán JA, Robles Barragán FJ, Funcia de la Torre I, Alfonso Sanz F, Becerra Cayetano IA, de la Hoz Serrano C. Bilateral pericapsular nerves group (PENG) block for analgesia in pediatric Hip surgery. Rev Esp Anestesiol Reanim. 2022;69(8):502–505. doi: 10.1016/j.redar.2021.05.018 [DOI] [PubMed] [Google Scholar]
- 24.Xu M, He YL, Du B. Pericapsular nerve group block for a child with spina malformation for hip surgery. J. Pediatr Surg Care Rep. 2022;86:102464. [Google Scholar]
- 25.Yörükoğlu HU, Cesur S, Aksu C, Kuş A. Opioid sparing effect of PENG block in open reduction of pediatric developmental dysplasia of the hip: a case series. Reg Anesth Pain Med. 2022;47(Suppl 1):A288–A289. [DOI] [PubMed] [Google Scholar]
- 26.Domagalska M, Wieczorowska-Tobis K, Reysner T, Geisler-Wojciechowska A, Grochowicka M, Kowalski G. Pericapsular nerve group (PENG) block in children under five years of age for analgesia in surgery for Hip dysplasia. Case Report J Pers Med. 2023;13:454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Irrou R, Nassik H. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia in pediatric hip and knee surgery: case reports (2 Cases). Ann Surg Perioper Care. 2023;8(2):1061. doi: 10.26420/AnnSurgPerioperCare.2023.1061 [DOI] [Google Scholar]
- 28.Çiftçi B, Ahıskalıoğlu A, Altıntaş HM, Tekin B, Şakul BU, Alıcı HA. A possible mechanism of motor blockade of high volume pericapsular nerve group (PENG) block: a cadaveric study. J Clin Anesth. 2021;74:110407. doi: 10.1016/j.jclinane.2021.110407 [DOI] [PubMed] [Google Scholar]
- 29.Senthil KS, Kumar P, Ramakrishnan L. Comparison of pericapsular nerve group block versus fascia iliaca compartment block as postoperative pain management in hip fracture surgeries. Anesth Essays Res. 2021;15(4):352–356. doi: 10.4103/aer.aer_119_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Balasubramaniam A, Kumar Naggaih S, Tarigonda S, Madhusudhana R. Ultrasound-guided pericapsular nerve group block for hip surgery: a randomized controlled trial study comparing ropivacaine and ropivacaine with dexamethasone. Cureus. 2023;15(1):e34261. doi: 10.7759/cureus.34261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kangarli N, Turkoz A. PENG block with dexmedetomidine in combination with local anesthetics for robotic Hip replacement surgery analgesia: case series. Reg Anesth Pain Med. 2023;3:A279. [Google Scholar]
- 32.Del Buono R, Padua E, Pascarella G, Soare CG, Barbara E. Continuous PENG block for hip fracture: a case series. Reg Anesth Pain Med. 2020;45(10):835–838. doi: 10.1136/rapm-2020-101446 [DOI] [PubMed] [Google Scholar]
- 33.Kaur G, Saikia P, Dey S, et al. Pericapsular nerve group (PENG) block—a scoping review. Ain-Shams J Anesthesiol. 2022;14(1):29. doi: 10.1186/s42077-022-00227-0 [DOI] [Google Scholar]
- 34.Del Buono R, Padua E, Pascarella G, et al. Pericapsular nerve group block: an overview. Minerva Anestesiol. 2021;87(4):458–466. doi: 10.23736/S0375-9393.20.14798-9 [DOI] [PubMed] [Google Scholar]
- 35.Becciolini M, Pivec C, Riegler G. Ultrasound of the lateral femoral cutaneous nerve: a review of the literature and pictorial essay. J Ultrasound Med. 2022;41(5):1273–1284. doi: 10.1002/jum.15809 [DOI] [PubMed] [Google Scholar]
- 36.Yeoh S-R, Chou Y, Chan S-M, Hou J-D, Lin J-A. Pericapsular nerve group block and iliopsoas plane block: a scoping review of quadriceps weakness after two proclaimed motor-sparing hip blocks. Healthcare. 2022;10(8):1565. doi: 10.3390/healthcare10081565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu HC, Moser JJ, Chu AY, Montgomery SH, Brown N, Endersby RVW. Inadvertent quadriceps weakness following the pericapsular nerve group (PENG) block. Reg Anesth Pain Med. 2019;44(5):611–613. doi: 10.1136/rapm-2018-100354 [DOI] [PubMed] [Google Scholar]
- 38.Shah RD, Suresh S. Applications of regional anaesthesia in paediatrics. Br J Anaesth. 2013;111(Suppl 1):i114–i124. doi: 10.1093/bja/aet379 [DOI] [PubMed] [Google Scholar]