Abstract
Purpose
Exercise is a vital adjunct therapy for patients with hypertension comorbidities. However, medical personnel and patients face significant obstacles in implementing exercise prescription recommendations. AI has been developed as a beneficial tool in the healthcare field. The performance of intelligent tools such as ChatGPT 4.0 and Intelligent Health Promotion Systems (IHPS) in issuing exercise prescriptions for patients with hypertension comorbidities remains to be verified.
Patients and Methods
After collecting patient information through IHPS hardware and questionnaire systems, the data were input into the software terminals of ChatGPT 4.0 and IHPS according to the five stages of the Transtheoretical Model, resulting in exercise prescriptions. Subsequently, experts from various fields scored the accuracy, comprehensiveness, and applicability of each prescription, along with providing professional recommendations based on their expertise. By comparing the performance of both systems, their capability to serve this specific group was evaluated.
Results
In most cases, ChatGPT scored significantly higher than IHPS in terms of accuracy, comprehensiveness, and applicability. However, when patients exhibited certain functional movement disorders, GPT’s exercise prescriptions involved higher health risks, whereas the more conservative approach of IHPS was advantageous.
Conclusion
The path of generating exercise prescriptions using artificial intelligence, whether via ChatGPT or IHPS, cannot achieve a completely satisfactory state.But can serve as a supplementary tool for professionals issuing exercise prescriptions to patients with hypertension comorbidities, especially in alleviating the financial burden of consulting costs. Future research could further explore the performance of AI in issuing exercise prescriptions, harmonize it with physiological indicators and phased feedback, and develop an interactive user experience.
Keywords: artificial intelligence, exercise prescription, hypertension, intelligent health promotion systems, transtheoretical model
Introduction
Over the past two to three decades, the prevalence of hypertension has steadily increased, primarily due to extended life expectancy and changes in lifestyle.1 Concurrently, hypertension often coexists with multiple chronic diseases such as diabetes, chronic kidney disease, and coronary heart disease, potentially increasing the cardiovascular risk for affected individuals or specific populations.2 Therefore, the coexisting risk factors and clinical sequelae require a multidisciplinary approach to assessment and management, which can consume considerable medical resources. With the advent of the digital information era, scientists are exploring the use of emerging technologies such as the internet and robotics to rationalize the allocation of medical resources.
As the development of chat tools progresses, the chatbot ChatGPT has emerged as a cutting-edge intelligent chatbot that resonates significantly across science, industry, and society, showing rapid growth in various fields.3 Given its outstanding performance in the prevention and management of chronic diseases,4 scholars are exploring its potential as a supplementary tool for prescribing, a capability that has already been substantiated.5 The ability to perform such tasks extends beyond artificial intelligence alone; health promotion systems also prove to be valuable tools.
The Intelligent Health Promotion System (IHPS) integrates wearable devices, data analytics, and artificial intelligence to utilize personal health indicators and health questionnaire data. This integration enables the exchange of information between IoT endpoints and health service systems, thereby generating personalized comprehensive assessment reports.6 Many scholars have applied exercise prescriptions generated by this system to middle-aged and elderly residents, thereby improving health outcomes for participants.7,8
For chronic disease patients, regular physical exercise not only improves quality of life but also significantly aids in long-term disease management.9 Despite acknowledging the benefits of physical activity, the adherence of chronic disease patients to exercise regimens remains suboptimal, potentially due to exercise prescriptions not fully considering the patient’s chronic disease history, willingness to exercise, and contraindications.8 The introduction of health behavior change theories has been effective in improving chronic disease management.10 The Transtheoretical Model (TTM), in particular, stages patient readiness to exercise and facilitates the creation of more personalized exercise prescriptions. This helps practitioners develop patient-centered plans to implement and sustain lifestyle changes.11 Additionally, TTM can be integrated with chatbots to effectively enhance adherence to health behaviors,12 altering their health trajectories. However, research comparing the efficacy of health promotion service systems and intelligent chatbots in issuing personalized exercise prescriptions based on TTM is still inconclusive.
This paper begins with the Transtheoretical Model (TTM) to explore the introduction of health behavior change theories. It compares the exercise prescriptions issued by health promotion service systems and ChatGPT for patients with hypertension comorbidities, assessing their capabilities in this area. The study aims to determine whether these systems can serve as consultation tools for general patients or as supplementary aids for professional healthcare providers.
Materials and Methods
Research Objectives and Design
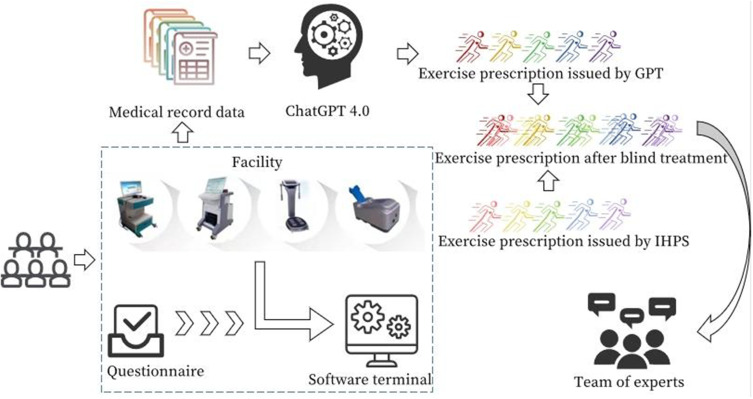
To minimize human error and ensure the authenticity and objectivity of medical records, this study recruited real patients to obtain medical data. A mixed-methods approach, differing from traditional qualitative and quantitative research, was chosen to avoid experts’ cognitive biases. As illustrated in Figure 1, data were input into ChatGPT 4.0 and the health promotion service system to generate exercise prescriptions. Initially, two experts specializing in exercise prescriptions reviewed these prescriptions, followed by a collective evaluation from another 22 experts. The first author was responsible for collecting and organizing data from both experts and patients.
Figure 1.
Research procedure.
Participants
Using purposive sampling, from December 2023 to February 2024, physical examinations and questionnaire surveys were conducted on patients who met the inclusion and exclusion criteria. The criteria were as follows: (1) community residents who provided informed consent; (2) individuals with a clear clinical diagnosis of hypertension accompanied by at least one other condition; (3) individuals possessing adequate language skills and cognitive functions.
Research Tools
The Health Promotion Service System consists of hardware devices and a software terminal. The hardware includes:
Body Composition Analyzer (Model: BX-BCA-100): Measures multiple body composition indicators such as hydration, protein content, bone mineral content, and fat.
Ultrasound Bone Density Scanner (Model: BX-BDI-500A): Acquires characteristics indicative of bone strength.
Cardiovascular Function Tester (Model: BX-CFTI-100): Captures characteristics indicative of the physiological and pathological state of the cardiovascular system.
Arteriosclerosis Detector (Model: BX-AS-100B): Measures the stiffness and blockage level of arteries.
Spirometer (Model: TSN100-FH): Measures lung capacity and expansion capability.
Handgrip Strength Tester (Model: TSN100-WL): Reflects forearm and hand muscle strength, assessing physical development and condition.
Flexibility Tester (Model: TSN100-TQ): Evaluates body flexibility.
Reaction Time Tester (Model: TSN100-FY): Assesses the coordination and rapid response capability of the nervous and muscular systems.
Balance Tester (Model: TSN100-ZL): Evaluates balance ability.
The software component, Intelligent Health Promotion Service System Software (Version: IIM-BSS-100), uses these tools along with provided questionnaires to collect primary indicators. The questionnaires cover a wide range of topics including medical history, symptoms, lifestyle, dietary habits, physical activity, and behavior patterns. By assessing body composition, bone density, cardiovascular function, and lifestyle, the system ultimately provides an intelligent, personalized lifestyle intervention plan for chronic disease patients.
Exercise Prescription
ChatGPT
Create a new conversation window and use the same question format to ask ChatGPT for exercise prescriptions for 10 different patients in the same dialogue. Each prescription is generated through a single interaction to closely replicate the scenario where a person without professional background consults with a chatbot. To ensure consistency within the sample group, all prescriptions from GPT are completed in the same conversation window.
The fixed question format is:
Please create a comprehensive exercise prescription based on the file, including five parts: expected health benefits, exercise principles, weekly plan, movement guidance, and precautions. Expand the expected health benefits according to the type of chronic disease; for the exercise principles section, list a table according to the FITT principles, including frequency (how often), intensity (how difficult, adjusted by heart rate, perceived exertion scale, and the principle of maximum repetition), time (how long), and type (what kind, please choose suitable exercise types based on fitness levels and ensure variability by listing 2-3 different exercise options; also, differentiate as much as possible from other exercise prescriptions in this conversation). The weekly plan should also be tabulated, seamlessly integrating rest days with exercise days and including necessary annotations. In the movement guidance section, clearly and specifically write the following: rhythm control for aerobic exercises and posture control during the process, clearly explain the specific actions for anaerobic exercises, and help patients understand and perform the actions accurately. For each type of exercise, provide frequency and intensity recommendations tailored to the patient’s condition. In the precautions section, make targeted recommendations based on the content of the patient information.
Intelligent Health Promotion System
After completing health assessments and online questionnaire surveys, an electronic health record is generated. Based on the comprehensive assessment results, the system further utilizes an inference engine to access a knowledge base for personalized exercise intervention planning. The main reasoning processes of a scientific fitness guidance plan include:
Setting Exercise Goals and Benefits: Based on the user’s complaints and current major health issues, the primary exercise goals are determined, and related exercise benefits are displayed.
Developing a Structured Exercise Prescription: According to the user’s current exercise habits and major health issues, aerobic and resistance exercise plans are formulated sequentially.
Creating Specific Movement Guidance: Based on the user’s current major health issues, suitable warm-up stretching exercises, relaxation stretches, and specialized health exercises are selected from the project library.
Providing Exercise Correction Suggestions and Risk Control Measures: Exercise precautions are identified based on the user’s current exercise habits and major health issues, to address during the exercise.
Several Important Points to Note
Ensuring Comparability Between Groups: To ensure comparability between groups and prevent evaluators from distinguishing between AI-generated and system-output real human action details through images, the image portion of the movement guidance in the service system has been removed.
Evidence of Iterative Interaction: Evidence suggests that iterative interactions significantly enhance the accuracy and precision of GPT-generated exercise prescriptions. However, this depends on the questioner’s level of expertise. Based on the “weakest link” principle, we use answers generated from a single interaction to simulate scenarios where individuals without professional backgrounds consult GPT. For this study, we provide them with an example based on the research’s sentence structure.
Previous Research Findings: Previous studies have found that GPT tends to produce some repetitiveness in multiple exercise prescriptions generated in the same window. Considering that this study aims to explore the scenario where patients or professionals consult GPT for a single exercise prescription for a single patient — a situation that can realistically avoid cross-contamination between different patients’ exercise prescriptions — we have added “as distinct as possible from other exercise prescriptions in this conversation” to the exercise principles section.
Expert Inquiry
To ensure a comprehensive evaluation, the evaluators hail from over ten different professional fields, including Sports Science, Human Anatomy, Rehabilitation, Clinical Medicine, General Medicine, Psychology, Nursing, Geriatric Medicine, Computer Science, and Electronic Information Engineering. Each expert has been deeply involved in their respective field for more than ten years. However, all experts hold at least a doctor’s degree and have senior professional titles. The initial intent of selecting a multidisciplinary, cross-disciplinary panel of experts to evaluate the GPT and the health promotion service system was to reduce barriers in the sharing and transformation of resources, establish a more effective resource integration and control mechanism, and to uncover interdisciplinary issues that transcend single professional domains and offer innovative value, thereby providing more possibilities for solving complex problems.
Each expert is required to use a 6-point Likert scale to evaluate accuracy, a 3-point Likert scale to evaluate comprehensiveness, and a 4-point Likert scale to evaluate applicability.
Data Analysis
The authority coefficient (Cr) is derived from experts’ self-assessments, significantly impacting the reliability of evaluations. The authority coefficient (Cr) is calculated as the average of the judgment basis (Ca) and familiarity (Cs), and a Cr value of 0.7 or higher is considered to indicate reliable research results. Judgment basis includes practical experience, theoretical knowledge, references to domestic and international literature, and intuitive impressions. Experts’ familiarity is ranked from very familiar to unfamiliar and scored from 1.0, 0.8 to 0.2. Descriptive statistics and consistency measures are utilized to analyze survey results using SPSS 27.0, and expert ratings are visually analyzed using GraPhad Prism 10.1.2. The researcher standardizes the expert recommendations to form a narrative evaluation.
Results
The average authority coefficient of the experts was 0.87, exceeding the threshold of 0.7, which is considered to indicate reliable expert opinions. The consistency coefficients are shown in Table 1.
Table 1.
Expert Consistency Evaluation
| Accuracy | Applicability | Comprehensiveness | ||||
|---|---|---|---|---|---|---|
| GPT | IHPS | GPT | IHPS | GPT | IHPS | |
| Wa | 0.623 | 0.717 | 0.446 | 0.759 | 0.712 | 0.503 |
| P | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
Note: aKendall coordination coefficient.
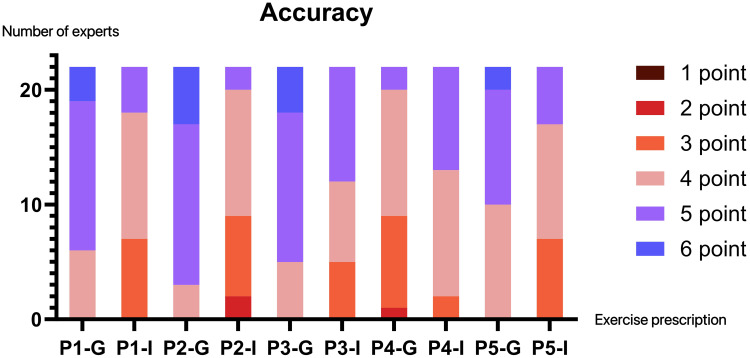
In the 1 to 6 Likert scale for accuracy, GPT’s average accuracy score was 4.64, while IHPS scored 4.38. Both had Kendall’s consistency indices greater than 0.6, indicating a high degree of agreement among the experts.The resulting exercise prescriptions are detailed in the Supplementary Materials; the patient information is available in Table 2.
Table 2.
Patient Information Data
| Number | ① | ② | ③ | ④ | ⑤ |
|---|---|---|---|---|---|
| Age/years | 75 | 69 | 79 | 70 | 70 |
| Gender | Female | Male | Female | Female | Male |
| Weight/kg | 60.4 | 97.2 | 64.2 | 74.6 | 85.1 |
| Height/cm | 160 | 175 | 167 | 160 | 165 |
| BMI | 23.6 | 31.7 | 23.0 | 29.1 | 31.3 |
| Body fat percentage | 27.2% | 26.6% | 22.1% | 42.2% | 26.2% |
| BMR/Kcal | 1215 | 1995 | 1357 | 1281 | 1735 |
| Balance | Weak | Weak | Weak | Medium | Well |
| Upper body strength | Weak | Weak | Weak | Weak | Medium |
| Flexibility | Medium | Weak | Excellent | Medium | Excellent |
| Vital capacity | Weak | Well | Weak | Weak | Well |
| Sensitivity | Weak | Weak | Weak | Well | Weak |
| Coordination | Weak | Weak | Weak | Weak | Medium |
| Arteriosclerosis | Early phase | Signs of atherosclerosis | Early phase | Early phase | Signs of atherosclerosis |
| BMD | Normal | Osteopenia | Normal | Osteopenia | Osteopenia |
| Chronic history | Hypertension Diabetes |
Hypertension Chronic nephritis |
Hypertension COPD |
Hypertension Parkinsonism |
Hypertension Gouty arthritis |
| Drug usage | Insulin; Aspirin; Irbesartan | Irbesartan; Felodipine; Febuxostat; Atorvastatin calcium | Irbesartan and hydrochlorothiazide | Nifedipine; Levodopa |
Zhenju; Benzbromarone |
| Motor contraindications | Lower back pain, can not hold the same position for a long time | Prolapse of lumbar intervertebral disc, can not hold the same position for a long time | |||
| Exercise willingness | No motor intention | Intention to exercise within 6 months | Intention to exercise within 1 month | Regular exercise but less than 1 month | Exercise regularly for more than half a year |
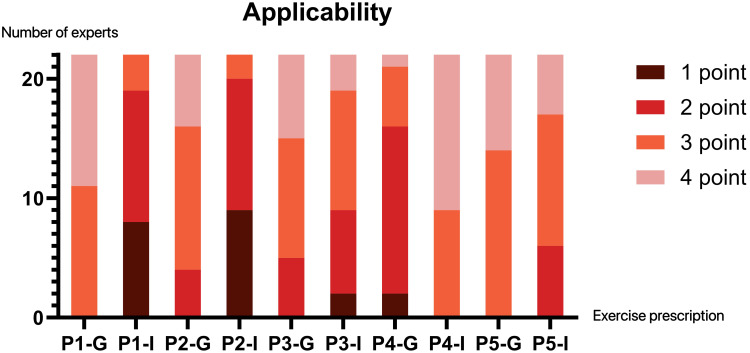
For applicability, scored on a 1 to 4 Likert scale, GPT’s average applicability score was 3.05 compared to 2.53 for IHPS. GPT’s applicability had a Kendall’s consistency coefficient of 0.446, indicating moderate agreement among experts, while IHPS showed higher expert consistency.
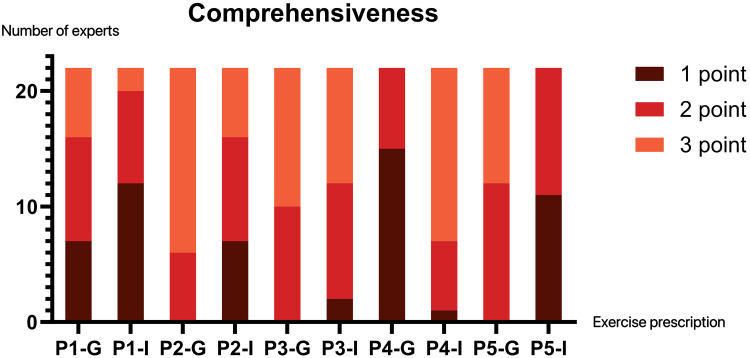
In the 1 to 3 Likert scale for comprehensiveness, GPT scored an average of 2.25, and IHPS scored 1.96. GPT’s Kendall’s consistency coefficient was 0.712, indicating a high degree of agreement among experts; IHPS’s consistency index was 0.503, signifying moderate agreement.
Across the three dimensions of accuracy, comprehensiveness, and applicability (Figures 2–4), the trends in expert opinions were generally uniform, with GPT outperforming IHPS in the scores for the first three patients. GPT’s prescription for the fourth patient was significantly lower than IHPS across all dimensions, but for the fifth patient, GPT still had a slight edge.
Figure 2.
Visual analysis of expert accuracy scores for ChatGPT and IHPS.
Figure 3.
Visual analysis of expert applicability scores for ChatGPT and IHPS.
Figure 4.
Visual analysis of expert comprehensiveness scores for ChatGPT and IHPS.
Patient Number 1
The patient’s lower back pain limits their ability to maintain a prolonged posture, but moderate physical activity can effectively alleviate this pain.13 However, both GPT and IHPS exhibit shortcomings in clearly identifying risks, potentially causing patients to question or fear the exercise prescription.14
For diabetic patients, exercise is crucial for glycemic control. IHPS not only highlights the importance of different types of exercise in managing blood sugar and preventing complications but also suggests combining exercise with medication and diet to maximize health benefits. Detailed explanations of health benefits can enhance patients’ exercise adherence and contribute to sustainable healthy living.15 For hypertensive patients, exercise plays a vital role in cardiovascular health, and IHPS provides more comprehensive information about health benefits, helping alleviate patient concerns and promoting understanding.16
Insufficient lung capacity poses challenges to the cardiovascular system. Numerous studies have shown that regular high-intensity exercise can reduce cardiovascular morbidity and mortality,17–19 and even long-term regular high-intensity exercise can induce ventricular remodeling and significantly improve lung function.20 Compared to IHPS, GPT mentions the role of aerobic exercise in improving cardiopulmonary function and effectively preventing and alleviating cardiovascular disease in older adults.21 According to the stages of the Transtheoretical Model, the patient is in a phase of lacking exercise motivation and habits, making cardiopulmonary function improvement the primary goal at this stage, laying the foundation for progression to higher exercise intensities later on.22
Guidelines suggest that moderate-intensity aerobic exercise can offer the maximum health benefits for diabetic patients with comorbid hypertension while controlling risks. IHPS recommends walking as an aerobic activity, but the intensity may be too low for patients to achieve the expected results.23 However, the system’s recommendations on target intensity and subjective perception are more vivid, and the proposed wellness exercises are simpler and easier to follow, though they may not yield the expected improvements in balance, agility, and flexibility. IHPS offers a repetitive, cyclic exercise plan, whereas GPT’s progressive, self-regulated plan based on personal preferences and needs ensures variability and adherence throughout the exercise process. GPT’s explanation of exercise intensity based on heart rate is more objective and convenient, increasing readability,24 but the overall description leans toward professionalism, which might pose challenges for patients without an exercise background.
For patients with lower back muscle injuries, GPT’s recommendation of brisk walking should include a specific caution to avoid downhill running or jumping, as it can increase shear stress on the lumbar-sacral area and exacerbate pain.25 Walking in water reduces the pressure on the spinal extensor muscles, which is comparable to the maximum pressure applied on land, helping improve muscle strength and endurance.26 Research shows that core strength training can help chronic back pain patients strengthen deep trunk muscles, achieving pain relief and functional improvement.27
The American College of Sports Medicine (ACSM) recommends that diabetic patients without contraindications exercise at least three days per week, with no more than two consecutive days of inactivity,23 and for hypertensive patients, daily aerobic exercise is suggested. GPT’s plan alternates rest days with exercise days to effectively reduce exercise fatigue.28
More comprehensive and scientific precautions help chronic disease patients mitigate disease risks. Diabetic patients should be alert to the risk of hypoglycemia; both GPT and IHPS emphasize the importance of blood sugar monitoring and dietary adjustments before and after exercise to prevent severe physiological reactions, such as arrhythmias or even death.29 However, GPT does not mention contraindicated actions like the Valsalva maneuver for hypertensive patients. The coexistence of diabetes and hypertension may lead to overactive sympathetic nervous activity and parasympathetic dysfunction.30 Numerous studies have identified hypertension as a risk factor for diabetic foot;31–33 therefore, GPT and IHPS should also be mindful of early signs of poor skin condition in diabetic foot patients to ensure timely prevention and control.
Drug interactions are also common, and personalized medication guidance is crucial for controlling disease risks in patients. However, the advice provided by GPT and IHPS in this regard is too general, which may fail to raise sufficient patient awareness and vigilance.34
Patient Number 2
In men, the effect of exercise on improving bone density in middle-aged and elderly individuals is particularly significant.35 The patient’s BMI meets the criteria for obesity, and fat accumulation can affect normal bone metabolism,36 becoming a risk factor for bone health. As both prescriptions state, regular exercise can improve bone density. Additionally, IHPS highlights the prognostic value of physical activity for chronic diseases. Studies show that low-intensity physical activity can stimulate the sympathetic nervous system and influence renal hemodynamics.37 However, this report does not mention the specific impact of regular exercise on physical fitness, whereas GPT emphasizes the positive role of physical fitness in mitigating cardiovascular risk factors,38 thereby reducing the incidence of cardiovascular events—a simple and feasible approach.
The Japanese Society of Renal Rehabilitation39 advises that patients with chronic glomerulonephritis should not overly restrict their physical activity. Similarly, the 2020 guidelines of the American College of Sports Medicine (ACSM)40 recommend moderate- to low-intensity exercise training for patients with chronic kidney disease to promote disease management. For elderly individuals with low bone mass and cardiovascular risk, falls can lead to irreversible physical damage, and exercise interventions aimed at improving balance, gait, and muscle strength can effectively prevent falls. IHPS’s recommendation of diabolo exercises aligns with this goal.41
Regarding the weekly plan, ACSM40 suggests combining aerobic and resistance training, while IHPS recommends that the patient freely arrange some aerobic and stretching exercises. It is undeniable that a low-frequency exercise regimen may lead to better adherence and execution,42 but it still falls short of the ideal baseline. GPT’s prescription includes strength training, which has a positive impact on bone health.43 However, it is crucial to select the appropriate weight based on the 1-RM principle44 and avoid high-impact exercises that could cause unnecessary muscle and bone damage.45
Cultural differences in the acceptance of exercise programs are notably heterogeneous,46 and localized exercises (eg, Tai Chi, Qigong) are more easily accepted by Chinese individuals.47 However, yoga, as a low-cost and non-invasive therapy, can also benefit patients with chronic kidney disease.48 GPT’s guidance on Thai yoga poses is insufficient, and it should provide at least 1–2 specific movements as a reference. According to the Transtheoretical Model stages, the patient is in a phase of long-term inactivity, combined with reduced bone mass, requiring strict fall prevention to avoid fragility fractures.49 Both prescriptions include warnings in the precautions section that could help the patient in this regard.
However, both prescriptions lack personalized guidance on medication management. For example, amlodipine, as a calcium channel blocker, commonly causes ankle edema;50 the patient should rest in bed during the acute phase and elevate the affected limb to improve circulation.51 Furthermore, existing evidence indicates52,53 that the benefits of exercise during treatment with febuxostat and atorvastatin outweigh the risks.
Patient Number 3
In medical decision-making, individuals weigh expected benefits against the associated costs to guide their actions, making it crucial to enhance patients’ perceptions of benefits.54 Comparing the expected health benefits provided by GPT and IHPS, IHPS aligns more with achievable health benefit definitions, especially for patients without a professional background, as GPT focuses more on improvements in physical fitness without clearly demonstrating the impact on disease. IHPS emphasizes improving cardiovascular health through early exercise interventions to reduce the incidence of cardiovascular diseases.55 Age and being female are identified as independent factors for osteoporosis,56 making GPT’s recommendation to maintain normal bone mass particularly urgent for this patient.
The basic principle of exercise training is progressive overload,57 where, with repeated exercise, the organs and systems gradually adapt, improving muscle oxygen delivery and consumption at peak and submaximal workloads.58 However, COPD patients may reach a “ventilatory ceiling” during exercise, which does not improve with training.59 Nonetheless, there is ample evidence that the oxidative capacity of myofibrils and capillary density improves during exercise, enhancing skeletal muscle adaptability.60,61 Thus, incorporating a graded exercise test in the exercise prescription is necessary. The ACSM recommends using a 6-minute walk test to determine the maximum heart rate for COPD patients, ensuring exercise intensity remains within tolerable limits.40 Experimental evidence supports heart rate targets as a feasible marker for endurance training intensity prescriptions in COPD patients.62 IHPS’s subjective intensity perception makes it easier for patients to understand,40 and on the modified Borg scale, a subjective rating of 4–6 is considered feasible, effective, and safe.63 Even so, both systems should specify the method for measuring exercise intensity in the precautions.
It is worth noting that GPT recommends walking and stationary cycling, which are simple and easy-to-maintain activities, and are also suggested by the International Respiratory Society.59 Yoga can also improve exercise capacity and lung function, particularly breathing techniques,64 but beginners should have an assistant nearby to prevent falls. IHPS’s diabolo exercises have significant positive effects on the mental health of older adults,65 but they lack emphasis on breathing exercises, which are critical for COPD patients, as exercise intolerance is often linked to respiratory issues.66 Respiratory muscle training is an essential component of exercise prescriptions for patients with impaired lung capacity, helping to overcome disease-related pathologies associated with the pulmonary system,67 and it also positively impacts blood pressure.68 However, neither exercise prescription mentions this aspect.
The patient has had an intention to exercise over the past month, but their physical function is limited. IHPS aligns better with the Transtheoretical Model, recommending a gradual introduction of strength training, which is beneficial to avoid patient dropout and helps gradually improve functional indicators. A progressive increase in prescription difficulty can effectively help the patient adapt over time.69
Hydrochlorothiazide may pose risks for COPD patients with respiratory difficulties, and strenuous exercise that increases cardiopulmonary load should be avoided.70 Moreover, given that air pollution is a major non-communicable factor contributing to increased COPD-related mortality,71 IHPS’s recommendation that the patient exercise outdoors during periods of good air quality is commendable.
Patient Number 4
The pathological mechanism of Parkinson’s disease leads to weight loss and reduced physical activity, and the use of levodopa accelerates bone loss, increasing the risk of fractures in Parkinson’s patients compared to their peers.72 Adequate exercise helps improve motor symptoms such as bradykinesia, gait, and turning performance.73 GPT suggests that specific balance training can enhance the patient’s coordination and balance, reducing the risk of falls at its root and increasing life expectancy.74 IHPS emphasizes the positive impact of exercise on weight management, and precise weight control can significantly slow the functional decline in Parkinson’s patients.75 Hypertension exacerbates the risk of Parkinson’s disease and affects the cardiovascular system, making early intervention by IHPS particularly important.76,77
The SPARX2 and Park-in-Shape studies confirm that Parkinson’s patients should engage in aerobic exercise three times a week to achieve potential health benefits.78,79 However, both IHPS and GPT fall short in prescribing the appropriate aerobic intensity. GPT considers balance disorders, highlighting that aquatic exercise is more effective in improving mobility and quality of life for Parkinson’s patients than land-based exercise and/or standard care.80 Additionally, guidelines suggest that an intensity based on 70%-85% of maximum heart rate is most suitable for Parkinson’s patients,81 which is consistent with GPT’s recommendations. IHPS places significant emphasis on the value of resistance training, supported by scientific research,82 and the potential benefits of Tai Chi are particularly notable.83 For lumbar disc herniation, IHPS includes specific exercises to help relieve chronic lower back pain.84 The patient has already established initial exercise habits, but only through the reasonable arrangement of long-term regular exercise can lasting effects be achieved.78 GPT’s exercise plan is appropriately structured to effectively promote adherence.
Considering that disease progression and medication-induced movement disorders in Parkinson’s patients significantly increase the risk of falls,85 GPT emphasizes exercise safety. However, in terms of lumbar disc herniation and cardiovascular health, IHPS provides more detailed guidance, which is also an important component of disease management for Parkinson’s patients.
Patient Number 5
For gout patients, the pain caused by tophi significantly affects quality of life, and along with reduced bone mass, it is listed as an independent risk factor for fragility fractures.86 Exercise can accelerate the metabolism of uric acid, reduce inflammation, and help alleviate pain.87 GPT clearly outlines the expected benefits of exercise for gout and mentions the positive correlation between a higher body mass index and the risk of gout.88 IHPS emphasizes the positive impact of obesity management on cardiovascular health and highlights the importance of exercise in hypertension management.
Research has shown that exercising at 64–76% of maximum heart rate, as well as GPT’s recommended 50–65% of maximum heart rate, can effectively improve hyperuricemia.89 Although GPT recommends stationary cycling to relieve pain and improve joint function in arthritis patients, its clinical effectiveness in reducing stiffness and improving quality of life is limited.90 IHPS recommends walking as the preferred aerobic exercise for gout patients,88 while the Five-Animal Frolics exercise, which combines rehabilitation and exercise, is an effective method for restoring control over lumbar stabilizing muscles, improving mobility, and relieving pain.91 Both systems emphasize the importance of warm-up and cool-down exercises before and after workouts, which is crucial for patients with joint stiffness to prevent exercise-related injuries.92 The American College of Sports Medicine (ACSM) notes that resistance training can improve function, reduce pain, and increase muscle strength in arthritis patients. However, for patients with limited joint mobility, resistance training should start at the lowest intensity and gradually increase. For patients with multi-joint stiffness, specific joint mobility exercises are essential and can effectively alleviate stiffness and localized pain.93
During the acute and inflammatory phases of gout, strict immobilization is necessary, as vigorous exercise can increase serum antioxidant levels and cause a short-term surge in uric acid levels.94 This is not mentioned in either exercise prescription. Additionally, high body fat can significantly increase the stress on bones during intense exercise, making the joint protection measures mentioned by IHPS particularly important, as weight-bearing movements should be avoided. Even without explicit mention, it is important to include dietary recommendations for specific conditions, such as a low-purine, low-sodium diet for gout patients, which IHPS fails to address. Furthermore, in terms of medication management, avoiding the overlap of peak drug concentrations and periods of high heart rate during strenuous exercise is crucial to reduce the risk of adverse reactions. However, this is also missing from the exercise prescription provided by IHPS.
Discussion
The relatively low expert consensus on GPT’s applicability rating may stem from GPT’s lack of consideration for the exercise preferences of Chinese older adults, incorporating activities such as Pilates and yoga into its exercise prescriptions. The acceptance and cultural tolerance of different exercise modalities vary significantly across countries, meaning that cultural preferences should be a factor in designing exercise prescriptions,95 even if these activities perform well on the global stage. Similarly, some divergence in expert opinion was observed in the comprehensiveness rating for IHPS, possibly due to the system offering prescriptions with overly low intensity for patients with higher health risks, which may not achieve the expected health benefits. While these may not entirely be shortcomings, they offer constructive insights for improving more human-centered service plans in the future.
In summary, when considering accuracy, comprehensiveness, and applicability, GPT generally performs better for patients with fewer movement limitations, particularly in meeting the basic requirements of an exercise prescription. In line with the key points of the Transtheoretical Model, combining light aerobic exercise with an emphasis on strength, flexibility, and balance training is beneficial for older adults. Strength training is related to enhancing and maintaining daily living activities and may include activities such as weightlifting and progressive resistance with resistance bands. Flexibility and balance can be improved through activities such as Tai Chi, stretching exercises, and yoga.69
Furthermore, exercise prescriptions generated by GPT in the same chat session often display inevitable repetition. Even when explicitly instructed to avoid this, repeated elements can still appear across prescriptions for different patients. This could be due to GPT forming a standardized paradigm to meet user needs during iterative interactions. However, such cross-contamination between prescriptions could interfere with the diversity of other patients’ exercise prescriptions.
The exercise prescriptions generated by IHPS are based on mature algorithms, prioritizing patient safety. For hypertensive patients, IHPS explicitly advises which movements to avoid in the precautions section and divides the exercise routine into stages based on the patient’s current exercise habits, offering more detailed and specific recommendations for each stage. However, this approach also has a dual nature: an overemphasis on safety concerns may intentionally lower the intensity of the exercise prescription, which could prevent patients from achieving the expected health benefits. Additionally, IHPS provides scientifically sound advice based on the patient’s existing exercise habits, implying that the system assumes the patient is suited for these activities. In reality, selecting appropriate exercise activities is a critical aspect of the FITT principle, and offering more suitable exercise options can be beneficial for disease management. The limitations of the algorithm are also evident, as the current system does not encompass enough chronic diseases, leading to a severe lack of disease-specific knowledge in many exercise prescriptions.
In terms of expected benefits, there is significant heterogeneity between the two systems. GPT focuses on improving physical fitness, while IHPS emphasizes the degree to which exercise benefits the patient’s disease. Both systems fall short in the area of medication management, as the level of personalization needs improvement. The interaction between medications is crucial in chronic disease management, especially for patients with comorbidities who often take two or more medications. Increased heart rate and metabolism during exercise can enhance the effects of antihypertensive drugs, increasing the likelihood of medication-related complications. Therefore, providing corresponding risk guidance for patients during exercise is essential to alleviate the burden of disease management on both patients and caregivers.
Moreover, both exercise prescriptions lack adaptability. Regular changes to the exercise activities, intensity, and frequency through real-time assessment can prevent exercise plateaus, increase motivation, and promote long-term adherence.96 Including a section that advises patients to revisit their healthcare provider for periodic adjustments to the exercise prescription when they experience low perceived exertion or exercise fatigue due to physiological adaptation is critical.
AI is still far from being able to fully replace human expertise. However, based on current advancements, both GPT and IHPS are capable of meeting the needs of low-risk populations as preliminary consultation tools. For hypertensive patients with comorbidities, these tools could serve as collaborative aids for healthcare professionals, potentially reducing healthcare resource use and improving work efficiency. Studies have already demonstrated AI’s usability for the elderly; interactive robots have been shown to effectively reduce negative emotions and behaviors, increase social engagement, and enhance caregiving experiences for dementia patients.97 Some people, however, may argue that AI lacks the ability to consider complex situations from the patient’s perspective, raising ethical and privacy concerns—areas where AI has potential for future development.98
It is undeniable that GPT, when trained by professionals in specific fields and improved through iterative interactions, can produce more accurate and superior results. However, to maintain objectivity, this study employed a third-person observational approach to minimize the influence of external factors that could alter the model’s responses, ensuring a clearer distinction between the model’s inherent knowledge and potential external influences.
This study has three limitations: First, it is based on single-session generated exercise prescriptions, but GPT’s random sampling nature can result in significant variability. Future research could investigate the stability of GPT’s exercise prescriptions by generating prescriptions for the same user’s profile across multiple chat sessions. Second, exercise prescriptions require dynamic adjustments based on the patient’s progress. This study focused on initial exercise prescriptions generated based on the patient’s health condition and habits, so it could not assess the systems’ ability to provide phase-based adjustments. Future studies could issue prescriptions at various stages of a patient’s disease progression to further compare the two systems. Lastly, the evaluation of accuracy, comprehensiveness, and applicability was based on expert ratings, which may not fully represent the actual performance of GPT and IHPS, especially in models specifically trained for medical applications.
Conclusion
AI is far from replacing human expertise, but both GPT and IHPS can meet the needs of individuals at low health risk for initial consultations. For patients with comorbid hypertension, these tools could serve as collaborative aids for professionals, potentially saving healthcare resources and enhancing efficiency. Studies have demonstrated AI’s usability among the elderly, including interactive robots that can reduce negative emotions and behaviors in dementia patients, enhancing social engagement and caregiving experiences.96 Despite some concerns that AI cannot fully comprehend complex scenarios from a human perspective, including ethical and privacy issues, these represent potential areas for AI’s future development.97
However, it is undeniable that GPT, trained by professionals in specific fields and refined through iterative interactions, can produce more accurate results. To maintain objectivity, this study employs a third-person observational method to minimize external influences on model responses, helping to clearly distinguish between the model’s intrinsic knowledge and potential external impacts.
This study has limitations: firstly, it is based on exercise prescriptions generated in a single instance, and GPT’s random selection might lead to variability in prescriptions. Future research could explore the stability of GPT’s prescriptions using data from the same user across multiple dialogues. Secondly, the use of expert scoring for accuracy, comprehensiveness, and applicability may not fully represent the specific performance of GPT and IHPS, especially those models trained in specific medical fields.
Acknowledgments
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Institutional Review Board Statement
This study was designed in full compliance with the relevant ChatGPT4.0 terms of use and was only used to generate exercise prescription results and did not involve human experiments, thus complying with the license for the use of artificial intelligence tools.And the study was conducted by the Declaration of Helsinki, and approved by the Ethics Committee of Bengbu Medical University (No. 2023-253).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Wang JG, Zhang W, Li Y, Liu L. Hypertension in China: epidemiology and treatment initiatives. Nat Rev Cardiol. 2023;20(8):531–545. doi: 10.1038/s41569-022-00829-z [DOI] [PubMed] [Google Scholar]
- 2.Shrestha PL, Shrestha PA, Vivo RP. Epidemiology of comorbidities in patients with hypertension. Current Opinion in Cardiology. 2016;31(4):376–380. doi: 10.1097/HCO.0000000000000298 [DOI] [PubMed] [Google Scholar]
- 3.Kocoń J, Cichecki I, Kaszyca O, et al. ChatGPT: jack of all trades, master of none. Info Fusion. 2023;99:101861. doi: 10.1016/j.inffus.2023.101861 [DOI] [Google Scholar]
- 4.Biswas SS. Role of chat gpt in public health. Ann Biomed Eng. 2023;51(5):868–869. doi: 10.1007/s10439-023-03172-7 [DOI] [PubMed] [Google Scholar]
- 5.Washif J, Pagaduan J, James C, Dergaa I, Beaven C. Artificial intelligence in sport: exploring the potential of using ChatGPT in resistance training prescription. Biol Sport. 2024;41(2):209–220. doi: 10.5114/biolsport.2024.132987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun T, Xu X, Zhu N, Zhang J, Ma Z, Xie H. A Service-Learning Project Based on a Community-Oriented Intelligent Health Promotion System for Postgraduate Nursing Students: mixed Methods Study. JMIR Medical Education. 2023;9(1):e52279. doi: 10.2196/52279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muellmann S, Forberger S, Möllers T, Bröring E, Zeeb H, Pischke CR. Effectiveness of eHealth interventions for the promotion of physical activity in older adults: a systematic review. Preventive Med. 2018;108:93–110. doi: 10.1016/j.ypmed.2017.12.026 [DOI] [PubMed] [Google Scholar]
- 8.Sun T, Xu Y, Xie H, Ma Z, Wang Y. Intelligent personalized exercise prescription based on an ehealth promotion system to improve health outcomes of middle-aged and older adult community dwellers: pretest–posttest study. J Med Inter Res. 2021;23(5):e28221. doi: 10.2196/28221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pedersen BK, Saltin B. Exercise as medicine–evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25:1–72. doi: 10.1111/sms.12581 [DOI] [PubMed] [Google Scholar]
- 10.Hashemzadeh M, Rahimi A, Zare-Farashbandi F, Alavi-Naeini AM, Daei A. Transtheoretical model of health behavioral change: a systematic review. Iranian J Nurs Midwifery Res. 2019;24(2):83–90. doi: 10.4103/ijnmr.IJNMR_94_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gillespie ND, Lenz TL. Implementation of a tool to modify behavior in a chronic disease management program. Adv Prevent Med. 2011;2011:1–5. doi: 10.4061/2011/215842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aggarwal A, Tam CC, Wu D, Li X, Qiao S. Artificial intelligence–based chatbots for promoting health behavioral changes: systematic review. J medi Inter rese. 2023;25:e40789. doi: 10.2196/40789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alzahrani H, Mackey M, Stamatakis E, Zadro JR, Shirley D. The association between physical activity and low back pain: a systematic review and meta-analysis of observational studies. Sci Rep. 2019;9(1):8244. doi: 10.1038/s41598-019-44664-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bordeleau M, Vincenot M, Lefevre S, et al. Treatments for kinesiophobia in people with chronic pain: a scoping review. Front Behav Neuroscie. 2022;16:933483. doi: 10.3389/fnbeh.2022.933483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robroek SJ, Bredt FJ, Burdorf A. The (cost-) effectiveness of an individually tailored long-term worksite health promotion programme on physical activity and nutrition: design of a pragmatic cluster randomised controlled trial. BMC Public Health. 2007;7:1–11. doi: 10.1186/1471-2458-7-259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lucas SJ, Cotter JD, Brassard P, Bailey DM. High-intensity interval exercise and cerebrovascular health: curiosity, cause, and consequence. J Cereb Blood Flow Metab. 2015;35(6):902–911. doi: 10.1038/jcbfm.2015.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thompson PD, Franklin BA, Balady GJ, Blair SN, Corrado D, Costa F; American College of Sports Medicine. Exercise and acute cardiovascular events: placing the risks into perspective: a scientific statement from the American Heart Association Council on Nutrition. Phys Act Metab Coun Clin Card Circul. 2007;115(17):2358–2368. [DOI] [PubMed] [Google Scholar]
- 18.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081. [DOI] [PubMed] [Google Scholar]
- 19.Eijsvogels TM, Molossi S, Lee DC, Emery MS, Thompson PD. Exercise at the extremes: the amount of exercise to reduce cardiovascular events. J Amer Card. 2016;67(3):316–329. doi: 10.1016/j.jacc.2015.11.034 [DOI] [PubMed] [Google Scholar]
- 20.Domenech-Ximenos B, Garza MSDL, Prat-González S, et al. Exercise-induced cardio-pulmonary remodelling in endurance athletes: not only the heart adapts. Eur J Preven Cardio. 2020;27(6):651–659. doi: 10.1177/2047487319868545 [DOI] [PubMed] [Google Scholar]
- 21.Mei N, Chang Y. Effect of aerobic exercise on physical function indices in the elderly. Revista Brasileira de Medicina do Esporte. 2022;29:e2022_0236. doi: 10.1590/1517-8692202329012022_0236 [DOI] [Google Scholar]
- 22.Ozemek C, Laddu DR, Lavie CJ, et al. An update on the role of cardiorespiratory fitness, structured exercise and lifestyle physical activity in preventing cardiovascular disease and health risk. Prog Cardiovasc Diseases. 2018;61(5–6):484–490. doi: 10.1016/j.pcad.2018.11.005 [DOI] [PubMed] [Google Scholar]
- 23.Christmas C, Andersen RA. Exercise and older patients: guidelines for the clinician. J Am Geriatr Soc. 2000;48(3):318–324. doi: 10.1111/j.1532-5415.2000.tb02654.x [DOI] [PubMed] [Google Scholar]
- 24.Scherr J, Wolfarth B, Christle JW, Pressler A, Wagenpfeil S, Halle M. Associations between Borg’s rating of perceived exertion and physiological measures of exercise intensity. Eur J Appl Physiol. 2013;113:147–155. doi: 10.1007/s00421-012-2421-x [DOI] [PubMed] [Google Scholar]
- 25.Levine D, Colston MA, Whittle MW, Pharo EC, Marcellin-Little DJ. Sagittal lumbar spine position during standing, walking, and running at various gradients. J Athletic Train. 2007;42(1):29. [PMC free article] [PubMed] [Google Scholar]
- 26.Chevutschi A, Lensel G, Vaast D, Thevenon A. An electromyographic study of human gait both in water and on dry ground. J Physiothropology. 2007;26(4):467–473. doi: 10.2114/jpa2.26.467 [DOI] [PubMed] [Google Scholar]
- 27.Kumar T, Kumar S, Nezamuddin M, Sharma VP. Efficacy of core muscle strengthening exercise in chronic low back pain patients. J Back Musculoskrehabil. 2015;28(4):699–707. doi: 10.3233/BMR-140572 [DOI] [PubMed] [Google Scholar]
- 28.Anemaet WK, Hammerich AS. A framework for exercise prescription. Top Geriatric Rehabil. 2014;30(2):79–101. doi: 10.1097/TGR.0000000000000011 [DOI] [Google Scholar]
- 29.Nakhleh A, Shehadeh N. Hypoglycemia in diabetes: an update on pathophysiology, treatment, and prevention. World J Diab. 2036;12(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patil L, Jadhav A, Borade NG (2013). A Comparative study of heart rate variability during Valsalva maneuver in healthy, hypertensive and hypertensive diabetic.
- 31.Al-Rubeaan K, Al Derwish M, Ouizi S, et al. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015;10(5):e0124446. doi: 10.1371/journal.pone.0124446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ouyang W, Jia Y, Jin L. Risk factors of diabetic foot ulcer in patients with type 2 diabetes: a retrospective cohort study. Am J Transl Res. 2021;13(8):9554. [PMC free article] [PubMed] [Google Scholar]
- 33.Rossboth S, Lechleitner M, Oberaigner W. Risk factors for diabetic foot complications in type 2 diabetes—a systematic review. Endocrinol Diab Metabol. 2021;4(1):e00175. doi: 10.1002/edm2.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goetz LH, Schork NJ. Personalized medicine: motivation, challenges, and progress. Fertil Sterility. 2018;109(6):952–963. doi: 10.1016/j.fertnstert.2018.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mages M, Shojaa M, Kohl M, et al. Exercise effects on bone mineral density in men. Nutrients. 2021;13(12):4244. doi: 10.3390/nu13124244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cao JJ. Effects of obesity on bone metabolism. J Orthopaedic Surg Res. 2011;6:1–7. doi: 10.1186/1749-799X-6-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Svarstad E, Myking O, Ofstad J, Iversen BM. Effect of light exercise on renal hemodynamics in patients with hypertension and chronic renal disease. Scand J Urol. 2002;36(6):464–472. doi: 10.1080/003655902762467648 [DOI] [PubMed] [Google Scholar]
- 38.Taylor-Piliae RE, Haskell WL, Stotts NA, Froelicher ES. Improvement in balance, strength, and flexibility after 12 weeks of Tai chi exercise in ethnic Chinese adults with cardiovascular disease risk factors. Alternative Therapies in Health and Medicine. 2006;12(2):50–59. [PubMed] [Google Scholar]
- 39.Yamagata K, Hoshino J, Sugiyama H, et al. Clinical practice guideline for renal rehabilitation: systematic reviews and recommendations of exercise therapies in patients with kidney diseases. Ren Replace Ther. 2019;5(1):1–19. doi: 10.1186/s41100-019-0209-8 [DOI] [Google Scholar]
- 40.Liguori G; American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. Lippincott Williams & Wilkins; 2020. [Google Scholar]
- 41.Sun M, Min L, Xu N, Huang L, Li X. The effect of exercise intervention on reducing the fall risk in older adults: a meta-analysis of randomized controlled trials. Int J Environ Res Public Health. 2021;18(23):12562. doi: 10.3390/ijerph182312562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duncan GE, Anton SD, Sydeman SJ, et al. Prescribing exercise at varied levels of intensity and frequency: a randomized trial. Archives of Internal Medicine. 2005;165(20):2362–2369. doi: 10.1001/archinte.165.20.2362 [DOI] [PubMed] [Google Scholar]
- 43.Benedetti MG, Furlini G, Zati A, Letizia Mauro G. The effectiveness of physical exercise on bone density in osteoporotic patients. Biomed Res Int 2018. doi: 10.1155/2018/4840531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Daly RM, Dunstan DW, Owen N, Jolley D, Shaw JE, Zimmet PZ. Does high-intensity resistance training maintain bone mass during moderate weight loss in older overweight adults with type 2 diabetes? Osteoporosis Int. 16:1703–1712. doi: 10.1007/s00198-005-1906-4 [DOI] [PubMed] [Google Scholar]
- 45.Vereijken A, Aerts I, Jetten J, et al. Association between functional performance and return to performance in high-impact sports after lower extremity injury: a systematic review. J Sports Sci Med. 2020;19(3):564. [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang C, Zhang J, Su J, Liu S, Zhang L. Review of Research on Yoga Intervention and Health Promotion Based on Citespace-A Comparative Analysis between China and the United States. J Asian Society Healt Exe. 2019;1(2):43–70. [Google Scholar]
- 47.Brown D, Leledaki A. Eastern movement forms as body-self transforming cultural practices in the West: towards a sociological perspective. Cultural Socio. 2010;4(1):123–154. doi: 10.1177/1749975509356866 [DOI] [Google Scholar]
- 48.Gautam S, Kiran UV. Clinical Effects of Yoga and Meditational Practices on the Holistic Health of Chronic Kidney Disease Patients: a Systematic Review. Cureus. 2024;16(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Uusi-Rasi K. Bone mass and strength and fall-related fractures in older age. J Osteoporosis. 2019;2019. doi: 10.1155/2019/5134690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Muhammad M, Nuhu JM, Hassan TM. Therapeutic exercise for hypertension: an update for exercise prescribers. Niger J Cardiol. 17(1):11–20. doi: 10.4103/njc.njc_24_19 [DOI] [Google Scholar]
- 51.Sims D. Effects of positioning on ankle edema. J Orthop Sports Phys Ther. 1986;8(1):30–33. doi: 10.2519/jospt.1986.8.1.30 [DOI] [PubMed] [Google Scholar]
- 52.Hays AG, Iantorno M, Schär M, et al. The influence of febuxostat on coronary artery endothelial dysfunction in patients with coronary artery disease: a Phase 4 randomized, placebo-controlled, double-blind, crossover trial. Am Heart J. 2018;197:85–93. doi: 10.1016/j.ahj.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 53.Schweitzer AM, Gingrich MA, Hawke TJ, Rebalka IA. The impact of statins on physical activity and exercise capacity: an overview of the evidence, mechanisms, and recommendations. Eur J App Physio. 2020;120:1205–1225. doi: 10.1007/s00421-020-04360-2 [DOI] [PubMed] [Google Scholar]
- 54.Singer E, Couper MP, Fagerlin A, et al. The role of perceived benefits and costs in patients’ medical decisions. Health Expect. 2014;17(1):4–14. doi: 10.1111/j.1369-7625.2011.00739.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vasan RS, Pan S, Larson MG, Mitchell GF, Xanthakis V. Arteriosclerosis, atherosclerosis, and cardiovascular health: joint relations to the incidence of cardiovascular disease. Hypertension. 2021;78(5):1232–1240. doi: 10.1161/HYPERTENSIONAHA.121.18075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen XX, Tian CW, Bai LY, et al. Relationships among body weight, lipids and bone mass in elderly individuals with fractures: a case-control study. World J Orthoped. 2023;14(9):720. doi: 10.5312/wjo.v14.i9.720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Watkins AL. Practical applications of progressive resistance exercises. J Amer Med Asso. 1952;148(6):443–446. doi: 10.1001/jama.1952.02930060025008 [DOI] [PubMed] [Google Scholar]
- 58.Morris NR, Walsh J, Adams L, Alision J. Exercise training in COPD: what is it about intensity? Respirology. 2016;21(7):1185–1192. doi: 10.1111/resp.12864 [DOI] [PubMed] [Google Scholar]
- 59.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. doi: 10.1164/rccm.201309-1634ST [DOI] [PubMed] [Google Scholar]
- 60.Maltais F, Simard AA, Simard C, Jobin J, Desgagnés P, LeBlanc P. Oxidative capacity of the skeletal muscle and lactic acid kinetics during exercise in normal subjects and in patients with COPD. Am J Respir Crit Care Med. 1996;153(1):288–293. doi: 10.1164/ajrccm.153.1.8542131 [DOI] [PubMed] [Google Scholar]
- 61.Whittom FRANÇOIS, Jobin JEAN, Simard PM, et al. Histochemical and morphological characteristics of the vastus lateralis muscle in patients with chronic obstructive pulmonary disease. Med Sci Sports Exercise. 1998;30(10):1467–1474. doi: 10.1097/00005768-199810000-00001 [DOI] [PubMed] [Google Scholar]
- 62.Fabre C, Chehere B, Bart F, Mucci P, Wallaert B, Grosbois J-M. Relationships between heart rate target determined in different exercise testing in COPD patients to prescribed with individualized exercise training. Int J Chronic Obstr Pulm Dis. 2017;Volume 12:1483–1489. doi: 10.2147/COPD.S129889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gloeckl R, Schneeberger T, Jarosch I, Kenn K. Pulmonary rehabilitation and exercise training in chronic obstructive pulmonary disease. Dtsch Arztebl Int. 2018;115(8):117. doi: 10.3238/arztebl.2018.0117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cramer H, Haller H, Klose P, Ward L, Chung VC, Lauche R. The risks and benefits of yoga for patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Clin rehabilitat. 2019;33(12):1847–1862. doi: 10.1177/0269215519860551 [DOI] [PubMed] [Google Scholar]
- 65.Wong MYC, Ou KL, Chung PK, Chui KYK, Zhang CQ. The relationship between physical activity, physical health, and mental health among older Chinese adults: a scoping review. Front Public Health. 2023;10:914548. doi: 10.3389/fpubh.2022.914548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.O’Donnell DE, Guenette JA, Maltais F, Webb KA. Decline of resting inspiratory capacity in COPD: the impact on breathing pattern, dyspnea, and ventilatory capacity during exercise. Chest. 2012;141(3):753–762. doi: 10.1378/chest.11-0787 [DOI] [PubMed] [Google Scholar]
- 67.Shei R. Time to move beyond a “one-size fits all” approach to inspiratory muscle training. Front Physiol. 2022;12:766346. doi: 10.3389/fphys.2021.766346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang Z, Wang B, Wu H, Chai X, Wang W, Peng CK. Effects of slow and regular breathing exercise on cardiopulmonary coupling and blood pressure. Med Biol Eng Comput. 2017;55:327–341. doi: 10.1007/s11517-016-1517-6 [DOI] [PubMed] [Google Scholar]
- 69.Burbank PM, Reibe D, Padula CA, Nigg C. Exercise and older adults: changing behavior with the transtheoretical model. Orthop Nurs. 2002;21(4):51–63. doi: 10.1097/00006416-200207000-00009 [DOI] [PubMed] [Google Scholar]
- 70.Kaabi W, Aouinti I, Charfi O, et al. A persistent dyspnea induced by hydrochlorothiazide. Therapies. 2019;74(4):498–499. doi: 10.1016/j.therap.2019.03.009 [DOI] [PubMed] [Google Scholar]
- 71.Duan RR, Hao K, Yang T. Air pollution and chronic obstructive pulmonary disease. Chronic Diseases and Translational Medicine. 2020;6(04):260–269. doi: 10.1016/j.cdtm.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Malochet-Guinamand S, Durif F, Thomas T. Parkinson’s disease: a risk factor for osteoporosis. Joint Bone Spine. 2015;82(6):406–410. doi: 10.1016/j.jbspin.2015.03.009 [DOI] [PubMed] [Google Scholar]
- 73.Xu X, Fu Z, Le W. Exercise and Parkinson’s disease. Inter Rev Neurobi. 2019;147:45–74. [DOI] [PubMed] [Google Scholar]
- 74.Fasano A, Canning CG, Hausdorff JM, Lord S, Rochester L. Falls in Parkinson’s disease: a complex and evolving picture. Mov Disord. 2017;32(11):1524–1536. doi: 10.1002/mds.27195 [DOI] [PubMed] [Google Scholar]
- 75.Kim R, Jun JS. Impact of overweight and obesity on functional and clinical outcomes of early Parkinson’s disease. J Am Med Directors Assoc. 2020;21(5):697–700. doi: 10.1016/j.jamda.2019.11.019 [DOI] [PubMed] [Google Scholar]
- 76.Müller J, Myers J. Association between physical fitness, cardiovascular risk factors, and Parkinson’s disease. European J Prevent Card. 2018;25(13):1409–1415. doi: 10.1177/2047487318771168 [DOI] [PubMed] [Google Scholar]
- 77.Chen J, Zhang C, Wu Y, Zhang D. Association between hypertension and the risk of Parkinson’s disease: a meta-analysis of analytical studies. Neuroepidemiology. 2019;52(3–4):181–192. doi: 10.1159/000496977 [DOI] [PubMed] [Google Scholar]
- 78.Schenkman M, Moore CG, Kohrt WM, et al. Effect of high-intensity treadmill exercise on motor symptoms in patients with de novo Parkinson disease: a Phase 2 randomized clinical trial. JAMA neurol. 2018;75(2):219–226. doi: 10.1001/jamaneurol.2017.3517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.van der Kolk NM, de Vries NM, Kessels RP, et al. Effectiveness of home-based and remotely supervised aerobic exercise in Parkinson’s disease: a double-blind, randomised controlled trial. Lancet Neurol. 2019;18(11):998–1008. doi: 10.1016/S1474-4422(19)30285-6 [DOI] [PubMed] [Google Scholar]
- 80.Gomes Neto M, Pontes SS, Almeida LDO, da Silva CM, da Conceição Sena C, Saquetto MB. Effects of water-based exercise on functioning and quality of life in people with Parkinson’s disease: a systematic review and meta-analysis. Clin rehabilitat. 2020;34(12):1425–1435. doi: 10.1177/0269215520943660 [DOI] [PubMed] [Google Scholar]
- 81.Alberts JL, Rosenfeldt AB, Bloem BR, Brundin P. The universal prescription for Parkinson’s disease: exercise. J Parkinsons Dis. 2020;10(s1):S21–S27. doi: 10.3233/JPD-202100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lima LO, Scianni A, Rodrigues-de-Paula F. Progressive resistance exercise improves strength and physical performance in people with mild to moderate Parkinson’s disease: a systematic review. J Physiotherapy. 2013;59(1):7–13. doi: 10.1016/S1836-9553(13)70141-3 [DOI] [PubMed] [Google Scholar]
- 83.Song R, Grabowska W, Park M, et al. The impact of Tai Chi and Qigong mind-body exercises on motor and non-motor function and quality of life in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Related Disord. 2017;41:3–13. doi: 10.1016/j.parkreldis.2017.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jeong D, Choi -H-H, Kang J-I, et al. Effect of lumbar stabilization exercise on disc herniation index, sacral angle, and functional improvement in patients with lumbar disc herniation. J Phys Ther Sci. 2017;29(12):2121–2125. doi: 10.1589/jpts.29.2121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Huot P, Johnston TH, Koprich JB, Fox SH, Brotchie JM, Sibley DR. The pharmacology of L-DOPA-induced dyskinesia in Parkinson’s disease. Pharmacol Rev. 2013;65(1):171–222. doi: 10.1124/pr.111.005678 [DOI] [PubMed] [Google Scholar]
- 86.Wang Y, Zhou R, Zhong W, Hu C, Lu S, Chai Y. Association of gout with osteoporotic fractures. International Orthopaedics. 2018;42:2041–2047. doi: 10.1007/s00264-018-4033-5 [DOI] [PubMed] [Google Scholar]
- 87.Jablonski K, Young NA, Henry C, et al. Physical activity prevents acute inflammation in a gout model by downregulation of TLR2 on circulating neutrophils as well as inhibition of serum CXCL1 and is associated with decreased pain and inflammation in gout patients. PLoS One. 2020;15(10):e0237520. doi: 10.1371/journal.pone.0237520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jia E, Zhu H, Geng H, et al. The effects of aerobic exercise on body composition in overweight and obese patients with gout: a randomized, open-labeled, controlled trial. Trials. 2022;23(1):745. doi: 10.1186/s13063-022-06695-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hou Y, Ma R, Gao S, et al. The effect of low and moderate exercise on hyperuricemia: protocol for a randomized controlled study. Front Endocrinol. 2021;12:716802. doi: 10.3389/fendo.2021.716802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Luan L, Bousie J, Pranata A, Adams R, Han J. Stationary cycling exercise for knee osteoarthritis: a systematic review and meta-analysis. Clin rehabilitat. 2021;35(4):522–533. doi: 10.1177/0269215520971795 [DOI] [PubMed] [Google Scholar]
- 91.Zhang SK, Yang Y, Gu ML, Mao SJ, Zhou WS. Effects of low back pain exercises on pain symptoms and activities of daily living: a systematic review and meta-analysis. Percep Motor Skills. 2022;129(1):63–89. doi: 10.1177/00315125211059407 [DOI] [PubMed] [Google Scholar]
- 92.Millar AL. Action Plan for Arthritis. Human Kinetics; 2003. [Google Scholar]
- 93.Nurhasanah A, Trismiyana E, Pribadi T. Latihan rentang gerak sendi (ROM) untuk menurunkan nyeri sendi pada pasien dengan asam urat tinggi. J Quali Health Rese Case Stu Rep. 2023;3(1):8–14. [Google Scholar]
- 94.Saladini F, Mos L, Fania C, Garavelli G, Casiglia E, Palatini P. Regular physical activity prevents development of hypertension in young people with hyperuricemia. J Hypert. 2017;35(5):994–1001. doi: 10.1097/HJH.0000000000001271 [DOI] [PubMed] [Google Scholar]
- 95.Liu J, Kowal I, Yang Y, et al. Culturally tailored group Qigong exercise in older Chinese immigrants: a feasibility study. Geriatric Nurs. 2023;51:245–252. doi: 10.1016/j.gerinurse.2023.03.021 [DOI] [PubMed] [Google Scholar]
- 96.Foster C. A new approach to monitoring exercise training. J Strength Cond Res. 2001;15(1):109–115. [PubMed] [Google Scholar]
- 97.Hung L, Liu C, Woldum E, et al. The benefits of and barriers to using a social robot PARO in care settings: a scoping review. BMC Geriatr. 2019;19:1–10. doi: 10.1186/s12877-019-1244-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Turner NR, Berridge C. How I want technology used in my care: learning from documented choices of people living with dementia using a dyadic decision making tool. Inform Health Soc Care. 2023;48(4):387–401. doi: 10.1080/17538157.2023.2252066 [DOI] [PMC free article] [PubMed] [Google Scholar]