Abstract
We report a case highlighting key clinical, CSF, and imaging findings of primary diffuse leptomeningeal gliomatosis of the spine.
Keywords: glioma, myelopathy, paresthesias
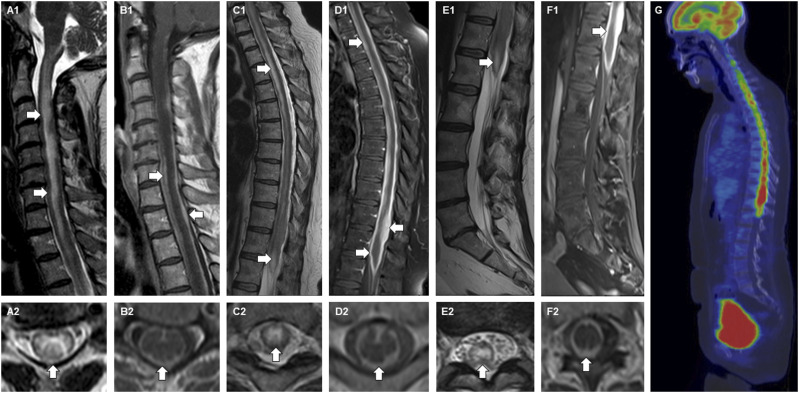
A 52-year-old woman presented to our emergency department, at a tertiary academic medical center, with 12 weeks of progressive lower extremity paresthesias after nondiagnostic medical evaluation locally. MRI of the spine demonstrated longitudinally extensive T2 hyperintensity (arrows) throughout the cervical (panels A1-A2), thoracic (panels C1-C2), and lumbar (panels E1-E2) spinal cord with diffuse leptomeningeal and subpial enhancement (arrows, panels B1-B2, D1-D2, F1-F2). A lumbar puncture showed a lymphocytic pleocytosis of 22 total nucleated cells and elevated protein of 280 mg/dL. Other infectious and inflammatory studies, as well as cytology and flow cytometry, were unremarkable. FDG-PET of the body demonstrated hypermetabolic activity throughout the spine (panel G). Biopsy of the spine was performed and confirmed a diagnosis of primary diffuse leptomeningeal gliomatosis (PDLG). The patient passed away 3 months after presentation. (Figure 1).
Figure 1.
MRI Spine and FDG-PET findings in a patient with primary diffuse leptomeningeal gliomatosis.Sagittal and axial T2 sequences of the cervical (A1-A2), thoracic (C1-C2), and lumbar (E1-E2) spine accompanied by sagittal and axial T1-post gadolinium sequences of the cervical (B1-B2), thoracic (D1-D2), and lumbar (F1-F2) spine. Sagittal FDG-PET (G).
PDLG is a rare cause of leptomeningeal enhancement. The initial differential is often broad, including infectious (e.g., tuberculous meningitis), inflammatory (e.g., sarcoidosis), and neoplastic considerations. Symptoms and signs at presentation are non-specific but can indicate increased intracranial pressure, cranial nerve palsies, seizures, and/or spinal cord pathology as in our case. Diagnostic evaluation generally includes imaging of the neuroaxis and lumbar puncture, with CSF studies classically demonstrating pleocytosis, elevated protein, and at times low glucose. MRI will classically demonstrate diffuse leptomeningeal enhancement. Often tissue biopsy is required to make the diagnosis. PDLG is associated with a poor prognosis and there is no standardized treatment at this time.1,2
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Hannah Padilla https://orcid.org/0009-0007-5527-9554
Reece M. Hass https://orcid.org/0000-0001-8298-3407
Rafid Mustafa https://orcid.org/0000-0003-2827-0507
References
- 1.Tauziede-Espariat A, Maues de Paula A, Pages M, et al. Primary leptomeningeal gliomatosis in children and adults: a morphological and molecular comparative study with literature review. Neurosurgery. 2016;78(3):343-352. [DOI] [PubMed] [Google Scholar]
- 2.Yomo S, Tada T, Hirayama S, et al. A case report and review of the literature. J Neuro Oncol. 2007;81(2):209-216. [DOI] [PubMed] [Google Scholar]