Abstract
Background
Hypothyroidism (HT) is the most prevalent endocrine disorder, affecting approximately one in 10 out of 35 adults, with a higher prevalence in females and the elderly.
Purpose
This systematic review (SR) aimed to discuss the effects of yoga on markers and comorbid conditions of HT.
Methods
The SR was registered with the PROSPERO (PROSPERO 2022 CRD42022312990). Google Scholar, PubMed, Cochrane, and EMBASE were searched for the relevant English language interventional studies published from 31 December 1947 to 31 December 2023 by using the keywords ‘meditation OR breath regulation OR yoga OR yoga nidra AND hypothyroidism OR hypothyreosis OR underactive thyroid OR low thyroid’. Of the 4078 screened studies, eight eligible studies (three RCTs, two pilot studies, two pre-post trials, and one case study) with 421 HT patients (392 females and 29 males) and three to six-month yoga interventions were included. Two independent review authors extracted study characteristics and synthesised them descriptively. RCTs and NRSIs were assessed for risk-of-bias (RoB) using Cochrane tools RoB2 and ROBINS-1.
Results
The findings suggest that yoga effectively improves the thyroid profile, lipid profile, heart rate variability, pulmonary functions, anxiety, depression, and quality of life among HT patients.
Conclusion
Yoga may be an inexpensive add-on preventive and therapeutic option for HT. The clinical and methodological heterogeneity among the studies did not allow for meta-analysis (MA). Well-designed MAs are warranted by including rigorous RCTs to draw valid conclusions and defined mechanisms regarding the efficacy of yoga practices/interventions on HT.
Keywords: Yoga, breath regulation, meditation, mind-body medicine, thyroid disorders
Introduction
Hypothyroidism (HT) is the most prevalent endocrine disorder, affecting approximately one in 10 out of 35 adults, showing its higher prevalence in females and the elderly.1, 2 In the USA, HT prevalence grew from 9.5% in 2012 to 11.7% in 2019. 3 In India, 11% of people have HT, compared to 2% in the UK and 4·6% in the USA. 4 Women are affected approximately six times more often than men with an underactive thyroid, 1 which may be due to autoimmune disorders, nutritional deficiencies, or hormonal imbalances. HT is the under-secretion of thyroid hormones (THs) from thyroid glands/impaired resistance of peripheral tissues to the effects of THs, resulting in a hypometabolic clinical state. 5 The signs and symptoms of HT include fatigue, weakness, dry skin, feeling cold, rapid heartbeat, thinning hair, trouble focusing, lousy memory, constipation, obesity, weak appetite, menorrhagia, dyspnoea, hearing impairment, myxoedema, bradycardia, diffuse alopecia, and peripheral oedema. 6 If left untreated, it may lead to hypertension, dyslipidaemia, infertility, cognitive impairment, neuromuscular dysfunction,4, 6, 7 and comorbidities, such as coronary artery disease, obesity, osteoporosis, depression, and sleep apnoea 8 . The treatment of HT focuses mainly on substituting the deficient hormone, and over 78% of HT patients receive thyroxine (T4) monotherapy—levothyroxine (LT4) to reach a euthyroid state.3, 9, 10 Persistent intake of synthetic levothyroxine (levothyroxine, synthroid, and others) might make patients drug-dependent and induce adverse effects.3, 5 Patients need to switch to alternative therapies to control the overall impact of HT on their lives. 11
Yoga is an ancient oriental practice that aims to purify the body, breath, bioenergy, cognition, and emotion to promote holistic wellness as an indispensable foundation for spiritual elevation.12, 13 Yoga includes an array of practices─cleansing technique (shatkarma), pose (asana), conscious breath regulation (pranayama), neuromuscular lock (bandha), seal (mudra), sensory withdrawal (pratyahara), concentration/mindfulness (dharana), and meditation (dhyana).14, 15 Yoga improves psychosomatic health by optimising psycho-neuroendocrine interactions, musculoskeletal health, immune system, cardiopulmonary functions, metabolic processes, bioenergy, and worldly outlook. Yoga is also a psychosomatic intervention for thyroid disorders that can be practised by all age groups and genders with minor side effects. 16 Yoga is a cost-effective and easy option for several physical and mental ailments.17, 18 The American College of Sports Medicine (ACSM) and the American Heart Association (AHA) reported that moderate to low-intensity yoga exercises can mitigate underactive thyroid symptoms. 19 A study consistently showed that a 50-minute yoga session for 10 days significantly decreased body weight, body mass index (BMI), waist circumference, lipid profile, and thyroid-stimulating hormone (TSH) levels 20 of underactive thyroid patients. The untested hypothesis asserts that yoga poses such as sarvangasana, bhujangasana, halasana, surya namaskar, marjariasana, and vipritkarani mitigate thyroid disorders, including HT by inducing mechanical effect and vascular supply on the thyroid. 20 However, no systematic reviews (SRs) and meta-analyses (MAs) synthesise the reported results regarding the effectiveness of yoga interventions in improving primary/secondary markers and comorbid conditions of HT. Therefore, this SR aimed to discuss the impacts of yoga interventions on primary/secondary markers of HT by synthesising the reported effects in the eight interventional studies.
Methods
Registration
This SR followed Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines and was registered with the International Prospective Register of Systematic Reviews (PROSPERO) with registration number PROSPERO 2022 CRD42022312990.
Eligibility Criteria
In this SR, all the full-text interventional studies evaluating the effect of yoga on HT and published in the English language were included. The selection of studies was based on the Population Intervention Comparison Outcome (PICO) statement, as depicted in Table 1.
Table 1. PICO Statement.
| P | Population/Patient | Patients of age group 18–55 years diagnosed with HT and TSH level >3.6 mlU/l |
| I | Intervention | Yoga practices: asanas, breathing techniques, locks, concentrations, mantra and meditations |
| C | Comparison | Passive/active controls, including standard care, diet, naturopathy, exercise, and behaviour moderation inputs) |
| O | Outcome | Primary outcomes: Thyroid profile (T3, T4, TSH and thyroxin medication—LT4): Secondary outcomes:
|
Note: BMI: Body Mass Index, BW: Body Weight, FEV1/FVCG: Forced Expiratory Volume/Forced Vital Capacity, FEV1: Forced Expiratory Volume in one second, FVCG: Forced Vital Capacity, HCG: Hip Circumference, HDL: High-Density Lipoprotein, HF: High-Frequency, hrs: Hours, HR: Heart Rate, HRV: Heart Rate Variability, ICG: Inspiratory Capacity, LDL: Low-Density Lipoprotein, LF: Low-Frequency, M: Male, MVV: Maximal Voluntary Ventilation, PEFR: Peak Expiratory Flow Rate, QoL: Quality of Life, RMSSD: Root Mean Squares of the Difference of Adjacent Intervals, T3: Triidothyronine, T4: Thyroxine, TCG: Total Cholesterol, TP: Total Power, TG: Triglyceride, TSH: Thyroid Stimulating Hormone, VLDL: Very Low-Density Lipoprotein, W/HR: Waist Hip Ratio, WCG: Waist Circumference.
Search Strategy
PubMed, Cochrane, EMBASE, and Google Scholar were searched to identify the relevant studies published from 31 December 1947 to 31 December 2023. Meditation OR breath regulation OR yoga OR yoga Nidra AND hypothyroidism OR hypothyreosis OR low thyroid were used as search keywords. Only articles in the English language were included in the studies. The search was limited and filtered by selecting only interventional studies that mainly assessed the effect of yoga therapy on HT. The detailed search strategy is depicted in Table 2.
Table 2. Detailed Search Strategy.
| Databases | Search Details | No of Articles |
| PubMed | (meditation OR breath regulation OR yoga OR yoga nidra [Title/Abstract] AND (hypothyroidism[Title/Abstract] OR underactive thyroid[Title/Abstract] OR low thyroid[Title/Abstract] OR hypothyreosis [Title/Abstract])) | 8 |
| EMBASE | meditation OR breath regulation OR yoga OR yoga nidra:ti,ab,kw AND (hypothyroidism:ti,ab,kw OR ’underactive thyroid’:ti,ab,kw OR ’low thyroid’:ti,ab,kw OR hypothyreosis:ti,ab,kw) | 16 |
| Cochrane Library | (meditation OR breath regulation OR yoga OR yoga nidra):ti,ab,kw AND (HTOR underactive thyroid OR low thyroid OR hypothyreosis):ti,ab,kw | 37 |
| Google Scholar | meditation OR breath regulation OR yoga OR yoga nidra AND (hypothyroidism OR underactive thyroid OR low thyroid OR hypothyreosis) | 4030 |
Study Selection and Data Extraction
The studies were searched from the above-stated databases, and the search engine was exported to the citation manager, Mendley version 1.19.8. The duplicates were filtered and removed. The retrieved articles were screened individually for titles and abstracts by two independent review authors to verify their eligibility for inclusion. The study characteristics, including author, publication year, country, study design, sample characteristics, intervention, comparator, measures, outcome variables, results, and findings, were extracted from each study and condensed into tabular form.
Risk of Bias in Individual Studies
The quality of studies included in the review was assessed using the Revised Cochrane risk-of-bias tools for randomised controlled trials (RoB2) and non-randomised studies of interventions (ROBINS-I).
Study Selection
A total of 4091 records with 13 duplicates identified from one search engine (Google Scholar = 4030) and three databases (Cochrane = 37, PubMed = 08, EMBASE = 16) were exported to a citation manager, Mendley version 1.19.8. The remaining 4078 records were then screened for irrelevant studies. The screening yielded 10 studies, which were further assessed for eligibility. Of the 10, two descriptive studies were excluded. Finally, eight studies were eligible for this review, as shown in Figure 1.
Figure 1. PRISMA Flow Diagram for Study Selection.

Study Characteristics
Eight studies (three RCTs, two pilot studies, two pre-post clinical trials, and one case study) were eligible to be included in this review. The studies had 421 participants (392 females and 29 males) diagnosed with HT. Yoga therapy for three to six months was the intervention. Table 3 provides a detailed description of the study characteristics.
Table 3. Characteristics of Included Studies.
| Author, Year | Design | Sample Characteristics | Intervention | Comparator | Measures | Outcomes | Results | Findings | |||
| Inclusion | Exclusion | OVs | Pre | Post | |||||||
| Akhtar, 2019 9 | RCT | n = 60 EG = 30 CG = 30 Age Range: ≥18 yrs |
Those patients who refused to participate in the study | Asana: Bhujanga, Kandhara, Vajra, Matsyasana, Halasana Pranayama: Anulom Viom, Kapalbhati, Bharahmari, Ujjyai, Bhastrika Bandh: Jalandharbandh Relaxation Technique: Shavasana Duration: 6 months Session Hrs.: 60 min Frequency/Week: 6 days |
‘-’ | WHO QoL BREF | QoL | Physical | EG:12.03 ± 1.02 CG: 11.56 ± 1.05 |
EG:14.17 ± 0.89***### CG: 11.70 ± 1.14 |
Yoga practices improved the physical and psychological aspects of QoL in the yoga group compared to the controls. |
| Psychological | EG:11.97 ± 0.87 CG: 11.93 ± 1.11 |
EG:14.17 ± 0.89***### CG: 12.04 ± 1.06 |
|||||||||
| Social | EG:9.14 ± 0.79 CG: 9.00 ± 0.96 |
EG:9.10 ± 0.67 CG: 8.96 ± 0.94 |
|||||||||
| Environmental | EG:13.10 ± 0.90 CG: 11.93 ± 0.87 |
EG:13.31 ± 1 0.88 CG: 12.00 ± 0.88 |
|||||||||
| Bhavanani, 2008 21 | A case study | n = 1F Age = 36 yrs |
‘-’ | Asana: Pawanmukta,Vakra, Sarvanga, Suryanamaskar, Vipritkarani, Tricon Pranayam: Suryabhedi, Ujjyai, Pranav, and Bhrahmari Bandh: Jalandharbandh Duration: 6 months Session Hrs.: 60 min Frequency/week: 6 days |
‘-’ | Biochemistry analyser | TSH T4 | TSH | 9.39 | 2.66 | After one year of therapy, yoga practices reduced TSH and normalised FT4. |
| FT4 | 12.57 | 9.39 | |||||||||
| Chintala et al., 2019 22 | RCT | n = 50 FEG = 25 CG = 25 Age = 18-30 yrs |
Pregnant, breastfeeding, addicted to alcohol and drugs, pre-practitioner of pranayam | Asana: Loosning Series Pranayam: Chandrabhedi, Bhrahmari, Nadishudhi, Pranav Relaxation Technique: Shavasan Duration: 1 month Session Hrs.: 60 min Frequency/week: 3 days |
‘-’ | Biochemistry Analyser | HRV T3 T4 TSH |
RR | EG: 937.31 ± 165.97 CG: 808.7 + 127.09 |
EG:880.87 ± 132.8# CG: 799.1 + 118.12 |
Yoga practices significantly reduced LFnu and improved HFnu in the Pranayama group compared to the control. |
| RMSSD | EG: 64.06 ± 22.98 CG: 74.48 ± 12.45 |
EG:68.18 ± 18.08**# CG:75.45 ± 12.08* |
|||||||||
| LF | EG: 74.4 ± 13.08 CG: 62.0 ± 13.98 |
EG:31.90 ± 12.96***### CG:44.80 ± 15.05** |
|||||||||
| HF | EG: 25.65 ± 12.87 CG: 38.0 ± 10.54 |
EG:68.11 ± 21.97***### |CG:539.88 ± 111.9** |
|||||||||
| TP | EG: 104.28 ± 276.09 CG: 891.99 ± 134.96 |
EG:130.76 ± 11.98***## CG: 539.88 ± 111.9** |
|||||||||
| LF/HF | EG:2.90 + 0.53 CG:1.63 + 0.89 |
EG: 0.47 ± 0.11***### CG: 0.81 ± 0.29* |
|||||||||
| Nilakanthan et al., 2016 8 | Pilot Study | n = 22 F Mean Age = 36.7 ± 3.2 yrs |
Subjects with known cardiac disease, hypertension, history of recent surgery, and slip disc | Asana: Suryanamskar, Sukshm Vyam, Asana- Bhujanga, Kandhara, Vajra, Matsyasana, Halasana Pranayama: Anulom Viom, Kapalbhati, Bharahmari. Ujjayi, Bhastrika Bandh: Jalandharbandh Relaxation Technique: Shavasana Duration: 6 Months Session Hrs.: 60 min Frequency/Week: 4 Days |
‘-’ | Biochemistry Analyser | TL TR LDL HDL TSH Thyroxine |
TL | 206.5 ± 27.08 | 190.18 ± 24.70 | Yoga practices significantly reduced TL, LDL and TGs and increased HDL with a non-significant reduction in TSH and a significant reduction in LT4 intake. |
| TR | 142.13 ± 46.72 | 131.86 ± 32.15 | |||||||||
| HDL | 51.72 ± 15.28 | 54.36 ± 13.35 | |||||||||
| LDL | 128.81 ± 17.86 | 116.90 ± 19.46 | |||||||||
| TSH | 3.99 ± 1.53 | 3.43 ± 0.99 | |||||||||
| Thyroxine | 55.571 ± 27.09 | 55.571 ± 27.09 | |||||||||
| Rani et al., 2021 23 | Pilot Study | n = 38 F Mean Age = 34.2 ± 4.7 yrs |
History of psychiatric disorders, addictions, antipsychotic medications, thyroid cancer, abdominal surgery in the past one year; morbid obesity; pregnancy; regular yoga practice habit and change thyroxin dosage in the preceding three months |
Asana: Loosening Practices, Surynamaskar Pranayam: Right Nostril Breathing, Ujjayi Breath with Antar Kumbhaka and Chandra Bhedi Meditation: Sun Meditation, Gayatri Mantra ChantingDuration: 3 months Frequency/week: 5 days Session Hrs.:: 60 min |
‘-’ | DASS-21 Biochemistry Analyser |
TSH Thyroxine Lipid Profile BMI Anxiety Fatigue Stress |
TSH | 5.24 ± 2.2 | 3.29 ± 1.03** | Yoga practices significantly improved depression, TSH, BMI, anxiety, fatigue, lipid profile, and stress. |
| Thyroxine | 45.77 ± 25.61 | 35.00 ± 19.16** | |||||||||
| TG | 117.34 ± 34.06 | 91.63 ± 19.95** | |||||||||
| TC | 218.42 ± 29.88 | 199.85 ± 14.53** | |||||||||
| VLDL | 23.52 ± 7.17 | 18.31 ± 4.00** | |||||||||
| LDL | 148.91 ± 28.75 | 128.27 ± 14.10** | |||||||||
| HDL | 46.35 ± 8.75 | 53.25 ± 5.39** | |||||||||
| BMI | 26.44 ± 2.67 | 24.8 ± 2.23* | |||||||||
| Depression | 13.37 ± 1.8 | 5.61 ± 1.3** | |||||||||
| Anxiety | 12.89 ± 2.5 | 5.37 ± 2.2** | |||||||||
| Fatigue | 46.37 ± 6.2 | 16.26 ± 4.4** | |||||||||
| Stress | 16.26 ± 3.0 | 7.29 ± 2.9** | |||||||||
| Shetty et al., 2020 24 | RCT | n = 60 (29 M + 31 F) EG = 30 CG = 30 Mean Age = 42.4 ± 7.4 yrs |
Patients suffering from any severe organ dysfunction | Naturopathy Hydrotherapy Mud Therapy Fasting Therapy Diet Modification Asana: Suryanamaskar, Halasana, Matsyasana, Vipritkarni Pranayama: Bhastrika, Kapalbhati, Nadishodhan and Relaxation Techniques Duration: 10 days Frequency/week: 6 days Session Hrs.:: 50 min |
‘-’ | Anthropometric Measures Biochemistry Analyser |
Thyroid Profile Lipid Profile Anthropometric Variables BW BMI WC HC |
T3 | EG: 103.4 ± 26.4 CG:117.8 ± 20.5 |
EG:107.9 ± 21.3 CG:116 ± 14.5 |
Naturopathy and yoga practices significantly decreased BW, BMI, WC, TGs, LDL, and TSH and increased HDL in the EG compared to the CC, with no significant change in T3 and T4. |
| T4 | EG:6.4 ± 1 CG:6.7 ± 1.1 |
EG:6.5 ± 0.9 CG:7.1 ± 0.9 |
|||||||||
| TSH | EG:9.8 ± 2.8 CG:10.5 ± 2.2 |
EG:9.0 ± 2.5*# CG:10.2 ± 2 |
|||||||||
| TG | EG:205.3 ± 30.3 CG:199 ± 58.9 |
EG:185.3 ± 30.3*# CG:195.3 ± 55 |
|||||||||
| TC | EG:237.1 ± 29.2 CG:216.4 ± 32.6 |
EG: 206 .1 ± 29.2**## CG:225.6 ± 33.2 |
|||||||||
| VLDL | EG:21.3 ± 3.3 CG:30.9 ± 11.7 |
EG:22.27 ± 5.4 CG:28.2 ± 11 |
|||||||||
| LDL | EG:182.1 ± 28.9 CG:145.7 ± 35.7 |
EG:145.07 ± 30*# CG:158.9 ± 35.7 |
|||||||||
| HDL | EG:33.9 ± 5.1 CG:39.7 ± 7.2 |
EG:38.9 ± 5.3*# CG:38.5 ± 11.9 |
|||||||||
| BW | EG:87.5 ± 11.1 CG:85.3 ± 8.5 |
EG:81.7 ± 10.9**## CG:85.1 ± 8.2 |
|||||||||
| BMI | EG:32.9 ± 2.6 CG:31.6 ± 1.5 |
EG:30.7 ± 2.4**## CG:31.5 ± 1.4 |
|||||||||
| WC | EG:95.0 ± 10 CG:92.6 ± 8.2 |
EG:91.4 ± 9.1*# CG:91.1 ± 9 |
|||||||||
| HC | EG:106.1 ± 8.2 CG:104.8 ± 6.6 |
EG:103.7 ± 8.3 CG:103.6 ± 7.5 |
|||||||||
| W/HR | EG:0.89 ± 0 CG:0.9 ± 0.1 |
EG:0.88 ± 0 CG:0.9 ± 0.1 |
|||||||||
| Singh et al., 2011 25 | Pre-Post | n = 20 F Mean Age = 38.2 ± 3.7 yrs |
Pregnant females, diabetics, severe CVD | Asana: Loosening Execises, Asan- Bhujanga, Kandhara,Vajra, Matsyasana, Pranayama: Anulom Viom, Kapalbhati, Bharahmari, Ujjyai, Bhastrika. Jalandharbandh, Shavasana. Duration: 1 month Frequency/week: 6 days Session Hrs.: 60 min |
‘-’ | WHOQOL-BREF | QoL | Physical | 11.5 ± 1.80 | 14.0 ± 1.52** | Yoga practices significantly improved the QoL—physical health, psychological health, social relationships, and environmental adaptation. |
| Psychological | 11.25 ± 2.98 | 13.6 ± 2.42** | |||||||||
| Social | 12.2 ± 2.23 | 13.9 ± 2.05** | |||||||||
| Environment | 11.55 ± 2.58 | 13.2 ± 2.42** | |||||||||
| OPH | 3.25 ± 0.69 | 3.25 ± 0.69 | |||||||||
| QoL | 3.1 ± 0.3 | 4.4 ± 0.58** | |||||||||
| Swami et al., 2009 26 | Pre- Post | n = 20 F Mean Age = 39.70 ± 8.27 yrs |
Subjects with chronic diseases or with organ system dysfunction | Pranayam: Kapalbhati, Bhastrika, Ujjyai, Anulom Vilom, Bhrahmari, Om Chanting Duration: 6 Months Frequency/Week: 7 Session Hrs.: 45 min |
‘-’ | Spirometry | TSH FVC FEV1 FEV1/FVC PEFR MVV IC |
TSH | 13.67 ± 10.22 | 9.10 ± 8.57 | Yoga practices significantly improved TSH, FVC, FEV1, FEV1/FVC, PEFR, MVV, and IC. |
| FVC | 2.26 ± 0.38 | 2.39 ± 0.43 | |||||||||
| FEV1 | 1.89 ± 0.26 | 2.05 ± 0.26** | |||||||||
| FEV1/FVC | 79.97 ± 4.43 | 81.32 ± 5.59 | |||||||||
| PEFR | 3.02 ± 1.07 | 3.73 ± 1.23** | |||||||||
| MVV | 72.72 ± 3.20 | 77.09 ± 14.43** | |||||||||
| IC | 1.80 ± 0.34 | 1.89 ± 0.35*** | |||||||||
Notes: BMI: Body Mass Index, BW: Body Weight, CG: Control Group, DASS-21: Depression Anxiety And Stress Scale, EG: Experimental Group, F: Female, FEV1/FVCG: Forced Expiratory Volume/Forced Vital Capacity, FEV1: Forced Expiratory Volume in one second, FVCG: Forced Vital Capacity, HCG: Hip Circumference, HDL: High-Density Lipoprotein, HF: High-Frequency, HFnu: Normalised high-frequency power, hrs: Hours, HR: Heart Rate, HRV: Heart Rate Variability, ICG: Inspiratory Capacity, LDL: Low-Density Lipoprotein, LF: Low-Frequency, LFnu: Normalised low-frequency power, M: Male, MVV: Maximal Voluntary Ventilation, n: Sample Size, NA: Not Applicable, OPH: Overall Perception of Health, OVs: Outcome Variables, PEFR: Peak Expiratory Flow Rate, QoL: Quality of Life, RMSSD: Root Mean Squares of the Difference of Adjacent Intervals, SD: Standard Deviation, T3: Triidothyronine, T4: Thyroxine, TCG: Total Cholesterol. TP: Total Power, TG: Triglyceride, TSH: Thyroid Stimulating Hormone, VLDL: Very Low-Density Lipoprotein, W/HR: Waist Hip Ratio, WCG: Waist Circumference, yrs: Years, * and # indicate intra-group and inter-group comparison respectively, *p < .05, **p < .01, ***p < .001, #p < .05, ##p < .01, ###p < .001.
Results
RoB in Studies
All three RCTs were assessed with moderate overall RoB. All NRSIs were assessed with unclear overall RoB. Summary of RoBs regarding included RCTs and NRSIs are shown in Figures 2 and 3.
Figure 2. Summary of RoB for RCTs.
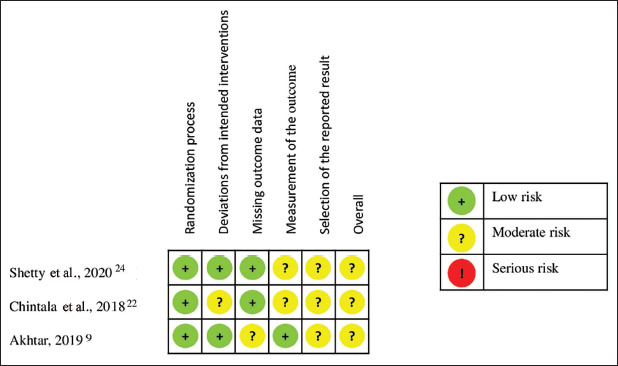
Figure 3. Summary of RoB for NRSIs.

Thyroid Profile and LT4
Four studies8, 23, 24, 26 indicated that yoga interventions significantly improve HT by decreasing TSH levels and doses of LT4 and increasing T3 and T4 levels. Two NRSIs with six-month yoga interventions showed significant effects on reducing doses of LT4.8, 23
Lipid Profile
Three studies8, 23, 24 reported a significant positive effect of yoga intervention incorporating yoga asanas with varied durations from 10 days 24 to 6 months8, 23 in improving lipid profiles, TC, LDL, VLDL, TG and HDL compared to standard care.
Anthropometric Outcomes
Two studies23, 24 indicated the significant effect of yoga interventions on decreasing BMI, BW, WC, HC, and W/HR of underactive thyroid patients after intra and inter-group comparisons.
Pulmonary Functions
One study 26 indicated the significant effect of a six-month yoga intervention on pulmonary functions by increasing FEV1, PEFR, MVV, and IC of underactive thyroid patients.
Heart Rate Variability
One study 22 showed the significant effect of yoga intervention on HRV by increasing RMSSD, HF, and total power and decreasing LF and LF/HF.
Quality of Life Outcomes
Two studies9, 25 indicated a significant effect of the yoga intervention to improve QoL (with an increase in physical, psychological, and environmental aspects but a slight decrease in social aspects). However, Singh et al.’s study 25 showed a significant effect of yoga intervention in improving overall QoL with no difference in overall perception of health.
Mental Health Outcomes
One case study 23 showed the significant positive effect of 6-month yoga intervention on the mental health (rated in terms of depression, anxiety, fatigue, and stress) of HT patients.
Discussion
This SR aimed to investigate the effects of yoga interventions on primary, secondary, and comorbid outcomes of HT. The synthesis of results reported in eight studies8, 9, 21–26 substantiated the beneficial effect of yoga practices in improving TSH, T3, T4, LT4, lipid profile, anthropometric outcomes (BW, BMI, HC), pulmonary functions, HRV, QoL, and mental health outcomes (depression, anxiety, fatigue, and stress) of hypoactive thyroid patients without reporting their adverse effects.
The three RCTs in the SR suggest favourable effects of yoga interventions on thyroid profile and LT4. Six-month yoga nidra practice significantly decreased TSH levels. 23 The actual mechanism underlying these results remains unknown. Studies have shown that breathing exercises, relaxation techniques, and meditation can reduce stress and balance the hypothalamic-pituitary-adrenal axis (HPA axis). 27 Yoga regulates the HPA system, lowers cortisol,28, 29 epinephrine, and norepinephrine, boost immunity (by increasing T cells, NK cells, and CD4 cells)30, 31, increases HRV 32 , empowers pulmonary functions 33 , strengthens glucose tolerance and reduces LDL.31, 34, 35 Regular yoga lowered IL-6, TNF-α 36 , and CRP and increased NK cells, T cells, B cells, and CD4 37 as an indication of inexpensive add-on therapy for HT and comorbid psychological problems. Regularly practicing bhujangasana, sarvangasana, vipritkarani, and halasana may impact the hypothalamic-pituitary-thyroid (HPT) axis and reduce blood TSH. 38 T4 and T3, which comprise just 20% of the circulating T3 in the blood, are the two main hormones secreted by the thyroid gland. Ujjayi breathing increases the intrathoracic pressure due to a slight contraction of the thyroid gland, potentially resulting in the increased secretion of T3 and T4. 39 The remainder of the T3 is created by peripheral tissues, including skeletal muscle, activating enzymes of both types 1 and 2 of iodothyronine deiodinase –DIO1 and DIO2, which split an iodine atom from T4. These yoga poses may affect skeletal muscle and peripheral tissue to activate DIO1 and DIO2, which split an iodine atom from T4. Omkar meditation enhances the circadian rhythm, induces plasma melatonin 33 , and may modulate serum TSH levels.
The two included trials24, 40 showed positive effects of yoga interventions in reducing TG, TC, LDL, and VLDL of hypoactive thyroid patients. Yoga practice stimulates the thyroid gland to secrete THs—T3 and T4. Increased TH lowers plasma levels of phospholipids, TGs, and cholesterol. Conversely, decreased thyroid secretion significantly increases cholesterol, phospholipids, and triglyceride plasma concentrations. THs lower plasma cholesterol levels by several processes, one of which is a marked increase in bile secretion of cholesterol and the resulting loss of cholesterol in feces. THs may cause an increase in LDL receptors in the liver cells, which in turn causes the liver to quickly remove LDL from plasma and secrete cholesterol in these lipoproteins by the liver cells. The consequences are the same as Nilakanthan et al.’s study finding, which reported a significant decrease in lipid profile outcomes after 16 weeks of yoga intervention. 8 An RCT showed a significant reduction in lipid profile after five months of YT.22, 23 Increased postural activity may have contributed to a decrease in TGs, TC, LDL, and an increase in HDL.28, 41 The increase in hepatic lipase and lipoprotein lipase, which can enhance the absorption of TGs by adipose tissue and impact lipoprotein metabolism, may cause a change in lipid profile followed by yoga practice. 20
Yoga interventions significantly improved anthropometric outcomes—BW, BMI, HC, WC, and W/HR-significantly. 24 Another study has shown that bhujangasana (cobra pose), bhastrika (periodic breathing), and kapalabhati (deep breathing) pranayama stimulate metabolic rate and oxygen consumption 42 by reducing body weight. Various studies found that being overweight is associated with overstimulation of the HPA axis, which alters the diurnal cortisol secretion. 43 Abnormal regulation of the HPA axis and perceived stress-dependent cortisol levels are strongly related to perturbations of the endocrine axis. 44 Consistently, an SR and MA including 44 RCTs with a total of 3168 participants reported a significant effect of yoga on improving blood pressure, heart rate, breath rate, waist circumference, waist/hip ratio, total cholesterol, HDL, VLDL, TGs, glycosylated haemoglobin (HbA1c), and insulin resistance in the general population and high cardiovascular risk groups compared to usual care and no intervention. 45
A study showed that yoga intervention significantly impacts pulmonary functions in hypothyroid patients. 26 The three-month practice of Hatha yogic postures, pranayams (nadisodhan, bhastrika, bhramari, sheetali, and shitkari), and omkar meditation divided into two sessions—morning and evening, a day improved cardiorespiratory performance (heart rate, blood pressure, mean arterial pressure, respiratory rate, FVC, FEV1, FEV%, PEFR, and MVV), and psychologic profile (anxiety, depression, and well-being) along with an increase in plasma melatonin level. 33 The improvement in pulmonary functions may be due to better respiratory muscle strength, improved thoracic mobility, and the balance between lung and chest elasticity, which yoga practitioners may have gained from regular yoga practice. 46
A study indicated yoga intervention’s highly significant positive effect on HRV in hypothyroid patients. 22 The increased HRV at rest after practising pranayam indicated a stimulated parasympathetic tone that might reduce the risk of symptoms. 47 Cyclic meditation/mindfulness followed by yoga poses consistently increased HRV by stimulating the parasympathetic tone.28, 32 HRV is decreased mainly because of a significant decrease in vagal activity. 48 Some studies suggest that TSH stimulates sympathetic output from the central nervous system and acts as a neurotransmitter, critical in determining sympathovagal imbalance. 49 Decreased vagal tone and increased sympathetic activity in HT have important clinical implications. Catecholamine receptor desensitisation decreases cardiac output, leading to a compensatory increase in norepinephrine release. 50 Indeed, patients with low vagal tone are more susceptible to cardiovascular diseases such as myocardial infarction, rhythm disorders, and hypertension. 51 Pranayama appears to alter autonomic responses by breath-holding, increasing vagal tone, decreasing sympathetic discharge, and causing relaxation. 52 Various studies have found that slow breathing increases blood pressure oscillations and HRV amplitudes, particularly at a respiration rate of six breaths per minute (0.1 Hz).53, 54
An RCT showed significant improvement in the physical, physiological, social, and environmental domains of QoL 9 , like Cramer et al.’s findings. 16 Rani et al. (2021) reported a significant effect of yoga practices on comorbid psychological conditions of HT—depression, anxiety, fatigue, and stress, aligned with Streeter’s findings that assert a significant effect of yoga to increase thalamic GABA and improve anxiety. 55 The two qualitative studies conducted by Cartwright et al. (2023) and Park et al. (2014) also consistently reported that yoga improved stress, mindfulness, emotional regulation, self-regulation, inclusiveness, social relation and spiritual pursuit.56, 57 Sudarshan kriya yoga (SKY) (including a set of breath regulatory practices ujjayi, bhastrika, pranav, and cyclical breathing) 58 is found supportive of mitigating neuropsychiatric illnesses—depression, anxiety, and stress, by upregulating gene expression—cyclooxygenase-2 gene, antiapoptotic BCL-2 gene, heat shock protein 70, and telomerase reverse transcriptase (hTERT) resulting in robust immune functions 59 ; decreased ACTH and cortisol28, 60; and increased prolactin 61 and oxytocin. 62 SKY also elevates antioxidant markers—superoxide dismutase (SOD) 63 and glutathione peroxidase. 59 Carlson et al. (2004) also reported that a mindfulness-based stress reduction (MBSR) programme comprised of relaxation, meditation, gentle yoga poses, and daily home practice significantly improved overall QoL, stress, and sleep quality and reduced cortisol levels in breast and prostate cancer patients. 64 Yogic breathing practices—ujjayi (breathing against airway resistance) and bhastrika (forceful nasal breathing), initiate adequate interhemispheric synchronisation and generate a dominant global brain rhythm with high-frequency cerebral activity and have been accepted for improving and maintaining physical and emotional health via down-regulation of the HPA axis resulting in enhanced autonomic and emotional control, cognitive functions and the QoL in all age groups.65, 66
The mechanical and vascular effects developed on thyroid by the practice of yoga poses and locks (suryanamaskar, bhujanga, sarvanga, matsya, kandhra, vipritkarani, halasana, tricon, vakra, ardhamatsyendra, jalandharbandh); parasympathetic tone and immunomodulation induced by the practice of ujjayi, bhramari, chandrabhedi, solar meditation, om/Gayatri mantra chanting, and corpse pose; and improved cardiopulmonary function and weight reduction caused by the practice of bhastrika, kpalbhati, suryabhedi, loosening poses, and alternate nostril breathing may prevent and mitigate the HT. The mechanisms of yoga practices’ effects on HT are yet unclear and need to be explored and tested in further studies.
Conclusion
Duly designed yoga interventions, including yoga poses, breath regulations, locks, concentrations, and meditations, may improve thyroid profile, lipid profile, cardiopulmonary functions, anthropometric outcomes, quality of life, and mental health of hypothyroid patients as inexpensive add-on therapy with minimal risk. Definite yoga practices with a detailed mechanism of positive effects on thyroid disorders are still unclear, warranting the need for further explanatory research regarding specific yoga practices versus hypothyroidism.
Limitations and Recommendations
The included eight studies had considerable clinical and methodological heterogeneity. This created a fragile base to conclude the positive effects of yoga interventions on primary/secondary markers and comorbid conditions of hypothyroidism. Moreover, inclusion, discussion, and derived conclusions regarding the impact of yoga on hypothyroidism inferred from more NRSIs warrant the future conduct of more rigorously designed RCTs and their inclusion in SRs and MAs to reach more definite and valid conclusions regarding the effects of yoga interventions on hypothyroidism.
Acknowledgements
The authors thankfully acknowledge the Honorable Acharya Balkrishna, Vice Chancellor, for constant administrative support and motivation and the Department of Yoga Science, University of Patanjali, for academic support.
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
ORCID iDs: Rudra B. Bhandari  https://orcid.org/0000-0002-1864-4619
https://orcid.org/0000-0002-1864-4619
Pintu K. Mahto  https://orcid.org/0000-0002-6195-6386
https://orcid.org/0000-0002-6195-6386
Authors’ Contribution
R.B.B.: Conceptualization, Supervision, Methodology, Writing-original draft, Writing-review and editing, Validation, Visualization, Project Administration. P. K. M.: Data Curation, Formal Analysis, Writing.
Statement of Ethics
Ethical permission was not applicable for this article, as this is a review article drafted from various research articles and not from patients directly.
References
- 1.Brito JP, Ross JS, El Kawkgi OM, et al. Levothyroxine use in the United States, 2008-2018. JAMA Intern Med 2021; 181: 1402–1405. DOI: 10.1001/jamainternmed.2021.2686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang M, Zhang W, Tan J, et al. Role of hypothyroidism in obstructive sleep apnea: a meta-analysis. Curr Med Res Opin 2016; 32: 1059–1064. DOI: 10.1185/03007995.2016.1157461 [DOI] [PubMed] [Google Scholar]
- 3.Wyne KL, Nair L, Schneiderman CP, et al. Hypothyroidism prevalence in the United States: a retrospective study combining national health and nutrition examination survey and claims data, 2009–2019. J Endocr Soc 2023; 7: bvac172. DOI: 10.1210/JENDSO/BVAC172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bagcchi S. Hypothyroidism in India: more to be done. Lancet Diabetes Endocrinol 2014; 2: 778. DOI: 10.1016/S2213-8587(14)70208-6 [DOI] [PubMed] [Google Scholar]
- 5.Chaker L, Razvi S, Bensenor IM, et al. Hypothyroidism. Nat Rev Dis Primers 2022; 8: 1–17. DOI: 10.1038/s41572-022-00357-7 [DOI] [PubMed] [Google Scholar]
- 6.Waldia V. A review study on the effect of sarvangasana on hypothyroidism. World J Pharm Res 2018; 7: 338–344. [Google Scholar]
- 7.Stern M, Finch A, Haskard-Zolnierek KB, et al. Cognitive decline in mid-life: changes in memory and cognition related to hypothyroidism. J Health Psychol 2022; 28: 388–401. DOI: 10.1177/13591053221107745 [DOI] [PubMed] [Google Scholar]
- 8.Nilakanthan S, Metri K, Raghuram N, et al. Effect of 6 months intense Yoga practice on lipid profile, thyroxine medication and serum TSH level in women suffering from hypothyroidism: a pilot study. J Complement Integr Med 2016; 13: 189–193. DOI: 10.1515/jcim-2014-0079 [DOI] [PubMed] [Google Scholar]
- 9.Akhtar J. Role of yoga in improving quality of life of hypothyroidism patients. Int J Adv Med 2019; 6: 341–345. DOI: 10.18203/2349-3933.ijam20191138 [Google Scholar]
- 10.Sue LY, Leung AM.. Levothyroxine for the treatment of subclinical hypothyroidism and cardiovascular disease. Front Endocrinol (Lausanne) 2020; 11: 1–8. DOI: 10.3389/fendo.2020.591588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chawla S, Silva FT, Medeiros SA, et al. The effect of low-fat and low-carbohydrate diets on weight loss and lipid levels: a systematic review and meta-analysis. Nutrients 2020; 12: 1–21. DOI: 10.3390/nu12123774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chopra D and Simon D.. The seven spiritual laws of yoga: a practical guide to healing body, mind, and spirit . John Wiley & Sons, Inc.: New Jersey, NJ, 2004. [Google Scholar]
- 13.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga 2011; 4: 49–54. DOI: 10.4103/0973-6131.85485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rao KR. Foundations of yoga psychology . Springer: Singapore, 2017. DOI: 10.1007/978-981-10-5409-9 [Google Scholar]
- 15.Saraswati SS. Four chapters on freedom: commentary on the yoga sutras of Sage Patanjali . Yoga Publications Trust: Munger, India, 2016. [Google Scholar]
- 16.Cramer H, Lauche R, Anheyer D, et al. Yoga for anxiety: a systematic review and meta-analysis of randomized controlled trials. Depress Anxiety 2018; 35: 830–843. DOI: 10.1002/da.22762 [DOI] [PubMed] [Google Scholar]
- 17.Büssing A, Michalsen A, Khalsa SBS, et al. Effects of yoga on mental and physical health: a short summary of reviews. Evid Based Complement Altern Med 2012; 2012: 165410. DOI: 10.1155/2012/165410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brandão T, Martins I, Torres A, et al. Effect of online Kundalini Yoga mental health of university students during Covid-19 pandemic: a randomized controlled trial. J Health Psychol 2024; 0. DOI: 10.1177/13591053231220710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nair N, Tripathy PK, Gope R, et al. Effectiveness of participatory women’s groups scaled up by the public health system to improve birth outcomes in Jharkhand, eastern India: a pragmatic cluster non-randomised controlled trial. BMJ Glob Health 2021; 6: e005066. DOI: 10.1136/bmjgh-2021-005066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghazvineh D, Daneshvar M, Basirat V, et al. The effect of yoga on the lipid profile: a systematic review and meta-analysis of randomized clinical trials. Front Nutr 2022; 9: 942702. DOI: 10.3389/fnut.2022.942702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhavanani AB. Effect of yoga on subclinical hypothyroidism: a case report. Yoga Mimamsa 2008; 43: 102–107. [Google Scholar]
- 22.Chintala KK, Samudrala V and Krishna BH.. Effect of short term Pranayama on heart rate variability in hypothyroidism. Int J Physiol Nutr Phys Educ 2019; 7: 897–900. DOI: 10.5958/2320-608x.2019.00082.9 [Google Scholar]
- 23.Rani S, Maharana S, Metri KG, et al. Effect of yoga on depression in hypothyroidism: a pilot study. J Tradit Complement Med 2021; 11: 375–380. DOI: 10.1016/J.JTCME.2021.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shetty GB, Shetty B and Shetty P.. Effect of short-term naturopathy and yoga intervention on anthropometric variables, lipid profile and thyroid profile in obese hypothyroid patients: a randomised controlled trial. Int J Basic Clin Pharmacol 2020; 9: 247–253. DOI: 10.18203/2319-2003.ijbcp20200171 [Google Scholar]
- 25.Singh P, Singh B, Dave R, et al. The impact of yoga upon female patients suffering from hypothyroidism. Complement Ther Clin Pract 2011; 17: 132–134. DOI: 10.1016/J.CTCP.2010.11.004 [DOI] [PubMed] [Google Scholar]
- 26.Swami G, Singh S and Singh KP.. Effect of yoga on pulmonary function tests of hypothyroid patients. Indian J Physiol Pharmacol 2009; 54: 51–56. [PubMed] [Google Scholar]
- 27.Malhotra V, Singh S, Sharma S, et al. Effects of yoga asanas and pranayama in non-insulin dependent diabetes mellitus. Indian J Tradit Knowl 2004; 3: 162–167. [Google Scholar]
- 28.Pascoe MC, Thompson DR, Ski CF.. Yoga, mindfulness-based stress reduction and stress-related physiological measures: a meta-analysis. Psychoneuroendocrinology 2017; 86: 152–168. DOI: 10.1016/J.PSYNEUEN.2017.08.008 [DOI] [PubMed] [Google Scholar]
- 29.Sullivan M, Carberry A, Evans ES, et al. The effects of power and stretch yoga on affect and salivary cortisol in women. J Health Psychol 2019; 24: 1658–1667. DOI: 10.1177/1359105317694487 [DOI] [PubMed] [Google Scholar]
- 30.Lim SA, Cheong KJ.. Regular yoga practice improves antioxidant status, immune function, and stress hormone releases in young healthy people: a randomized, double-blind, controlled pilot study. J Altern Complement Med 2015; 21: 530–538. DOI: 10.1089/ACM.2014.0044 [DOI] [PubMed] [Google Scholar]
- 31.Venkatesh HN, Ravish H, Wilma Delphine Silvia CR, et al. Molecular signature of the immune response to yoga therapy in stress-related chronic disease conditions: an insight. Int J Yoga 2020; 13: 9–17. DOI: 10.4103/ijoy.IJOY_82_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarang P and Telles S.. Effects of two yoga based relaxation techniques on Heart Rate Variability (HRV). Int J Stress Manag 2006; 13: 460–475. DOI: 10.1037/1072-5245.13.4.460 [Google Scholar]
- 33.Harinath K, Malhotra AS, Pal K, et al. Effects of hatha yoga and omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med 2004; 10: 261–268. DOI: 10.1089/107555304323062257 [DOI] [PubMed] [Google Scholar]
- 34.Tolahunase M, Sagar R and Dada R.. Impact of yoga and meditation on cellular aging in apparently healthy individuals: a prospective, open-label single-arm exploratory study. Oxid Med Cell Longev 2017; 2017: 7928981. DOI: 10.1155/2017/7928981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kiecolt-Glaser JK, Christian L, Preston H, et al. Stress, inflammation, and yoga practice. Psychosom Med 2010; 72: 113–121. DOI: 10.1097/PSY.0b013e3181cb9377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bower JE, Greendale G, Crosswell AD, et al. Yoga reduces inflammatory signaling in fatigued breast cancer survivors: a randomized controlled trial. Psychoneuroendocrinology 2014; 43: 20–29. DOI: 10.1016/J.PSYNEUEN.2014.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kelly UA, Evans DD, Baker H, et al. Determining psychoneuroimmunologic markers of yoga as an intervention for persons diagnosed with PTSD: a systematic review. Biol Res Nurs 2018; 20: 343–351. DOI: 10.1177/1099800417739152 [DOI] [PubMed] [Google Scholar]
- 38.Singh K, Junnarkar M and Sharma S.. Anxiety, stress, depression, and psychosocial functioning of Indian adolescents. Indian J Psychiatry 2015; 57: 367–374. DOI: 10.4103/0019-5545.171841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mason H, Vandoni M, Debarbieri G, et al. Cardiovascular and respiratory effect of yogic slow breathing in the yoga beginner: what is the best approach. Evid Based Complement Altern Med 2013; 2013: 743504. DOI: 10.1155/2013/743504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anjana K, Archana R and Mukkadan JK.. Effect of om chanting and yoga nidra on blood pressure and lipid profile in hypertension—a randomized controlled trial. J Ayurveda Integr Med 2022; 13: 100657. DOI: 10.1016/j.jaim.2022.100657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Simon Borg-Olivier and Machliss B.. Applied anatomy & physiology of yoga . YogaSynergy Pty Limited: Waverley, NSW, 2011. [Google Scholar]
- 42.Na Nongkhai MP, Huntula S, Kumar R, et al. Effects of an online yoga program on anthropometric parameters among overweight female students during the COVID-19 pandemic. Heliyon 2022; 8: e10661. DOI: 10.1016/j.heliyon.2022.e10661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schinke C, Rullmann M, Luthardt J, et al. HPA axis responsiveness associates with central serotonin transporter availability in human obesity and non-obesity controls. Brain Sci 2022; 12: 1430. DOI: 10.3390/brainsci12111430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Telles S, Nagarathna R and Nagendra HR.. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol 1994; 38: 133–137. [PubMed] [Google Scholar]
- 45.Cramer H, Lauche R, Haller H, et al. Effects of yoga on cardiovascular disease risk factors: a systematic review and meta-analysis. Int J Cardiol 2014; 173: 170–183. DOI: 10.1016/j.ijcard.2014.02.017 [DOI] [PubMed] [Google Scholar]
- 46.Ranjita R, Hankey A, Nagendra HR, et al. Yoga-based pulmonary rehabilitation for the management of dyspnea in coal miners with chronic obstructive pulmonary disease: a randomized controlled trial. J Ayurveda Integr Med 2016; 7: 158–166. DOI: 10.1016/J.JAIM.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kuppusamy M, Kamaldeen D, Pitani R, et al. Effects of yoga breathing practice on heart rate variability in healthy adolescents: a randomized controlled trial. Integr Med Res . 2020; 9: 28–32. DOI: 10.1016/j.imr.2020.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Malliani A. Heart rate variability: from bench to bedside. Eur J Intern Med 2005; 16: 12–20. DOI: 10.1016/j.ejim.2004.06.016 [DOI] [PubMed] [Google Scholar]
- 49.Polikar R, Burger AG, Scherrer U, et al. The thyroid and the heart. Circulation 1993; 87: 1435–1441. DOI: 10.1161/01.CIR.87.5.1435 [DOI] [PubMed] [Google Scholar]
- 50.Christensen NJ. Increased levels of plasma noradrenaline in hypothyroidism. J Clin Endocrinol Metab 1972; 35: 359–363. DOI: 10.1016/j.jacc.2012.03.047 [DOI] [PubMed] [Google Scholar]
- 51.Haensel A, Mills PJ, Nelesen RA, et al. The relationship between heart rate variability and inflammatory markers in cardiovascular diseases. Psychoneuroendocrinology 2008; 33: 1305–1312. DOI: 10.1016/J.PSYNEUEN.2008.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Santra G. Yoga and the need of its integration in modern medicine. J Assoc Physicians India . 2022; 70: 11–12. DOI: 10.5005/japi-11001-0142 [DOI] [PubMed] [Google Scholar]
- 53.Tharion E, Samuel P, Rajalakshmi R, et al. Influence of deep breathing exercise on spontaneous respiratory rate and heart rate variability: a randomised controlled trial in healthy subjects. Indian J Physiol Pharmacol 2012; 56: 80–87. [PubMed] [Google Scholar]
- 54.Beda A, Simpson DM, Carvalho NC, et al. Low-frequency heart rate variability is related to the breath-to-breath variability in the respiratory pattern. Psychophysiology 2014; 51: 197–205. DOI: 10.1111/psyp.12163 [DOI] [PubMed] [Google Scholar]
- 55.Streeter CC, Theodore HW, Owen L, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: a randomized controlled MRS study. J Altern Complement Med 2010; 16: 1145–1152. DOI: 10.1089/acm.2010.0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Park CL, Riley KE, Bedesin E, et al. Why practice yoga? Practitioners’ motivations for adopting and maintaining yoga practice. J Health Psychol 2016; 21: 887–896. DOI: 10.1177/1359105314541314 [DOI] [PubMed] [Google Scholar]
- 57.Cartwright T and Doronda T.. ‘It stretches your body but makes you feel good too’: a qualitative study exploring young people’s perceptions and experiences of yoga. J Health Psychol 2023; 28: 789–803. DOI: 10.1177/13591053221146840/ASSET/IMAGES/LARGE/10.1177_13591053221146840-FIG1.JPEG [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sharma P, Thapliyal A, Singh S, et al. Rhythmic breathing: immunological, biochemical, and physiological effects on health. Adv Mind Body Med 2015; 29: 18–25. [PubMed] [Google Scholar]
- 59.Sharma H, Datta P, Singh A, et al. Gene expression profiling in practitioners of Sudarshan Kriya. J Psychosom Res 2008; 64: 213–218. DOI: 10.1016/j.jpsychores.2007.07.003 [DOI] [PubMed] [Google Scholar]
- 60.Vedamurthachar A, Janakiramaiah N, Hegde JM, et al. Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord 2006; 94: 249–253. DOI: 10.1016/j.jad.2006.04.025 [DOI] [PubMed] [Google Scholar]
- 61.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, et al. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: a randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord 2000; 57: 255–259. DOI: 10.1016/S0165-0327(99)00079-8 [DOI] [PubMed] [Google Scholar]
- 62.Brown RP, Gerbarg PL.. Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression: part I—neurophysiologic model. J Altern Complement Med 2005; 11: 189–201. DOI: 10.1089/acm.2005.11.189 [DOI] [PubMed] [Google Scholar]
- 63.Agte VV, Chiplonkar SA.. Sudarshan Kriya Yoga for improving antioxidant status and reducing anxiety in adults. Altern Complement Ther 2008; 14: 96–100. DOI: 10.1089/act.2008.14204 [Google Scholar]
- 64.Carlson LE, Speca M, Patel KD, et al. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology 2004; 29: 448–474. DOI: 10.1016/S0306-4530(03)00054-4 [DOI] [PubMed] [Google Scholar]
- 65.Kjellgren A, Bood SA, Axelsson K, et al. Wellness through a comprehensive yogic breathing program—a controlled pilot trial. BMC Complement Altern Med 2007; 7: 43. DOI: 10.1186/1472-6882-7-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zope SA, Zope RA, Biri GA, et al. Sudarshan Kriya Yoga: a breath of hope during COVID-19 pandemic. Int J Yoga 2021; 14: 18–25. DOI: 10.4103/ijoy.IJOY_102_20 [DOI] [PMC free article] [PubMed] [Google Scholar]


