Abstract
Objectives
To 1) estimate the utilization and costs of physician and diagnostic imaging (DI) services for shoulder, knee, and low-back pain (LBP) conditions; and 2) examine determinants of the utilization and costs of these services.
Methods
All patients visiting a physician for shoulder, knee, or LBP conditions (identified by the ICD-9 codes) in Alberta, Canada, in fiscal year (FY) 2022/2023 were included. Interested outcomes included numbers and costs of physician visits and DI exams stratified by condition, physician specialty, DI modality, and patients’ sex and age. Multivariate regressions were used to examine determinants of the outcomes.
Results
In FY 2022/2023, 10.4%, 7.0%, and 6.7% of the population saw physicians for shoulder, knee, and LBP conditions, respectively. This costs Alberta $307.04 million ($67.93 per capita), of which shoulder accounted for 41%, knee 28%, and LBP 31%. In the same FY, 17,734 computed tomography (CT), 43,939 magnetic resonance imaging (MRI), 686 ultrasound (US), and 170,936 X-ray exams related to shoulder/knee/LBP conditions were ordered for these patients, costing another $29.07 million, of which CT accounted for 14%, MRI 48%, US 0%, and X-ray 37%. Female, older age, comorbidity scores, and capital zone used physician services more frequently. Patients with a higher comorbidity index scores or more physician visits were more likely being referred for CT or MRI.
Conclusion
Musculoskeletal conditions are common and result in patients seeking healthcare services. Visits to family physicians, specialists, and the ordering of DI contribute to extensive utilization of health services, contributing to considerable health system costs.
Keywords: Cost, diagnostic imaging, musculoskeletal, physician service
Introduction
Musculoskeletal (MSK) conditions are an important driver of disability-adjusted life years. 1 It is estimated that MSK conditions affect 11 million Canadians aged 12 years and older annually. 2 In Canada and other jurisdictions, an estimated 22%–26% of the general population seek health care for MSK conditions annually,3–6 amounting to 242.8 visits per 1000 population. 5 Frequent knee pain affects between 7% and 25% of adults, and an estimated 3% and 2% of adults have consulted primary care each year for spine and shoulder conditions, respectively.6–13 It is estimated that 14% to 45% of visits to primary care physicians are related to MSK conditions 14 ; the annual visit rate to primary care per 1000 population for shoulder, knee, and spine conditions is 32, 47, and 20, respectively.3,4
MSK conditions have become the leading cause of pain, years lived with disability, and one of the most common reasons for accessing public health resources.5,15 All medically necessary healthcare services provided by hospitals and doctors must be publicly provided, as outlined in the Canada Health Act. However, the magnitude of public health resources utilized to diagnose and treat MSK conditions is largely unknown.
Diagnostic imaging (DI), including X-ray and more expensive technology such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), make up a portion of these public system costs as they are commonly recommended for diagnosis and guidance for follow-up and treatment of MSK conditions. The growth in DI over the past several decades has inarguably yielded benefits to patients, both in terms of longer and improved quality of life. However, some of the growth in demand can be attributed to the overutilization or inappropriate use of DI services.16,17
While visit rates by MSK patients to various healthcare providers have been well studied, a population-based comprehensive picture of health service utilization and associated cost of DI and specialist investigation has yet to be established.
This study aims to develop reproducible costing methods to determine the healthcare utilization and associated costs to a public healthcare system for patients with MSK conditions, in Alberta (population ∼4.5 million), Canada. The specific objectives are to estimate the magnitude and determinants of 1) the utilization and cost of physician services for shoulder, knee, and LBP conditions (the most frequent three) and 2) the utilization and cost of DI services among these patients. Findings from this study will serve as a baseline for the evaluation of future interventions aiming at reducing variation and cost of MSK care, with lessons that can be shared nationally and internationally.
Methods
We applied a retrospective population-level cross-sectional study design to Alberta patients with shoulder, knee, and LBP conditions to examine the magnitude and determinants of utilization and cost of physician and DI services from a public health system perspective.
The Alberta Health Care Insurance Plan (AHCIP) Claims database was used to identify patients and determine the magnitude and determinants of utilization and cost of physician services. 18 Shoulder, knee, and LBP patients were identified based upon a shoulder, knee, or LBP condition code being listed in the most responsible diagnosis field of a claim in fiscal year (FY) 2022/2023 (using the International Classification of Disease [ICD] 9 codes in Supplement Table S1). Unique lifetime identifiers of identified patients were then linked to the Alberta Health Services (AHS) DI database to obtain patients’ records of DI services in the same FY 2022/23. The AHCIP Claims database consists of processed claims from all Alberta physicians for eligible Albertans. These data are collected to pay medical doctors and to track shadow-billing (e.g., on salary doctors) claims. The data elements extracted and used in the present analysis included patient information (e.g., identifier, demographic information, and location), provider information (GP or specialist), date of service, diagnosis, and amount paid or assessed for each claim.
Outcomes of interest included i) total number of patients with associated number and cost of physician visits, stratified by condition, physician specialty (general practitioner [GP] or specialist), sex (male or female), age group (<18; 18–64; or >64 years old), and geographic area (zones); ii) total number and cost of DI exams, stratified by condition and type of DI (CT, MRI, ultrasound, and general radiation or X-ray). We only included shoulder/knee/LBP–related DI as identified by the Common Procedure/Examination List or CPEL codes (Supplemental Table S2). 19 Order (instead of service) dates were used to avoid bias from wait times because some DI ordered in the studied year were not performed in the same year. Data from private DI services were unavailable and therefore not included in this study.
Costs for physician services were defined as paid amounts for fee-for-service claims that physicians submitted to AHCIP. Costs for on-salary physician services (∼10%) were not directly available; therefore, the Alberta Health system shadow bill assessed amounts were used as a proxy. 20 Costs or paid amounts for DI services were not available in the AHS DI database. Therefore, the cost per exam by modality of DI was obtained from the AHS DI Department. This included costs for staffing and benefits, consumable products including radioisotopes, service contracts, professional fees, and provincial program support staff; and excluded costs for capital equipment and construction. All costs were converted to 2023 CAD using the Canadian Consumer Price Index via the Bank of Canada inflation calculator. 21
Statistical analysis
Descriptive statistics were computed for all healthcare utilization and cost outcomes. The utilization and costs were stratified by sex and age of patients and by MSK condition as well as physician specialty (GP or specialist).
We performed multivariate regression analyses to examine determinants of the outcomes of interest. Negative binomial regressions were used for the numbered outcomes (e.g., number of physician visits). A gamma regression model with log link was used to examine the determinants of costs. Independent variables in these regressions included patient demographic characteristics (e.g., age and sex), provider characteristics (e.g., specialty and location in terms of zone within Alberta), and clinical characteristics (e.g., comorbidity measured in terms of the Charlson comorbidity index). 22 For CT and MRI models, numbers of visits to GP or specialist were also included.
Statistical significance was defined as p-values <0.05. All details about methods, data, and Stata syntax will be available upon reasonable request. Stata/SE 16.0 (https://www.stata.com/) was used for data analyses. Ethical approval was received from the Conjoint Health Research Ethics Board (CHREB) at the University of Calgary (File # REB22-0249).
Results
Physician visits and cost
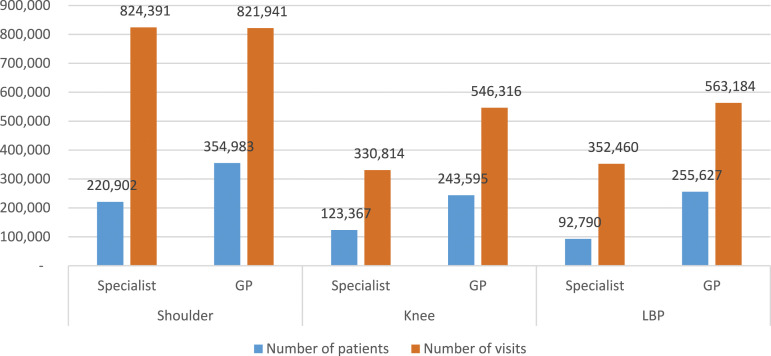
Figure 1 and Table 1 present the total number and cost of physician visits for shoulder, knee, and LBP conditions, by specialty. In total, there were 470,755 patients with shoulder conditions who made 1,646,332 visits to physicians (3.5 visits per patient, of which specialist visits accounted for 50% and GP for 50%), costing $131.92 million in FY 2022/23. There were 315,464 patients with knee conditions, with 877,130 total physician visits (2.8 visits per patient, of which specialist visits accounted for 38% and GP for 62%) at a cost of $81.29 million. There were 304,235 LBP patients, with 915,644 total physician visits (3.0 visits per patient, of which specialist visits accounted for 38% and GP for 62%) at a cost of $93.83 million. Dividing the total cost by the number of patients (or visits), the cost per patient (or per visit) was estimated at $280.23 ($80.13) for shoulder conditions, $257.67 ($92.67) for knee conditions, and $308,42 ($102.48) for LBP conditions (Table 1 and Supplemental Tables S3-S5). The 95% confidence intervals of these unit costs are shown in Supplemental Table S6.
Figure 1.
Number of patients and visits by condition and physician type.
Table 1.
Cost results by condition and physician type.
| Condition | Physician specialty | Number of patients | Number of visits | Cost per patient ($) | Cost per visit ($) | Total cost (M$) |
|---|---|---|---|---|---|---|
| Shoulder | Specialist | 220,902 | 824,391 | $372.06 | $99.70 | $82.19 |
| GP | 354,983 | 821,941 | $140.10 | $60.51 | $49.73 | |
| Total a | 470,755 | 1,646,332 | $280.23 | $80.13 | $131.92 | |
| Knee | Specialist | 123,367 | 330,814 | $388.37 | $144.83 | $47.91 |
| GP | 243,595 | 546,316 | $137.01 | $61.09 | $33.37 | |
| Total a | 315,464 | 877,130 | $257.67 | $92.67 | $81.29 | |
| LBP | Specialist | 92,790 | 352,460 | $633.16 | $166.69 | $58.75 |
| GP | 255,627 | 563,184 | $137.24 | $62.29 | $35.08 | |
| Total a | 304,235 | 915,644 | $308.42 | $102.48 | $93.83 |
aA patient could visit both GP and specialist.
Given the population of Alberta as of Oct 1, 2022, was 4,519,930, 23 the treated prevalence was estimated at 10.4% for shoulder conditions, 7.0% for knee conditions, and 6.7% for LBP conditions. The average physician cost per capita for all Albertans per year was estimated to be $29.19, $17.98, and $20.76 for shoulder, knee, and LBP conditions, respectively (not shown in Tables). Compared to the physician cost of $1185 per capita per year in Alberta for any disease, 24 these MSK conditions accounted for 5.7%.
In terms of patient characteristics, across the three MSK conditions, females accounted for 55%–56% of patients; 55%–58% of physician visits; and 55%–56% of the total cost (Supplemental Tables S3-S5). The cost per patient for females was slightly higher (1.01–1.04 times) than that of males. There were differences noted across age groups: patients <18 years old accounted for 4% of total patients and 3%–4% of total cost; patients 18–64 years old accounted for 53%–67% of total patients and 50%–58% of total cost; and patients >64 years old accounted for 30%–43% of total patients and 39%–46% of total cost. The highest cost per patient was found in the oldest group across all conditions. Urban patients accounted for 70% of total GP costs and 72% of total specialist costs (Supplemental Tables S7).
Diagnostic imaging utilization and cost
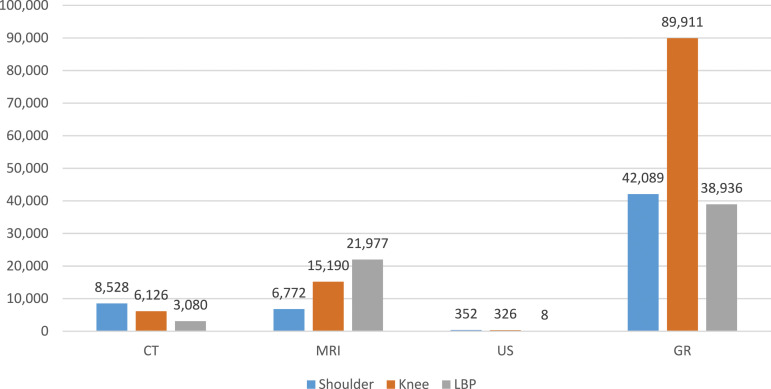
There were 470,755 patients who visited a physician for a shoulder condition in FY 2022/23, with a total of 57,741 public DI exams ordered for shoulder-related reasons in the same FY (Supplemental Tables S8). This represents 0.12 exams per patient. Of the total number of exams, CT accounted for 8528 (15%), MRI for 6772 (12%), US for 352 (1%), and X-ray for 42,089 (73%) (Figure 2).
Figure 2.
Number of related DI exams by condition.
There were 315,464 patients who saw a physician for a knee condition in FY 2022/23, with a total of 111,553 public DI exams ordered for knee-related reasons in the same FY (Supplemental Tables S9). This resulted in 0.35 exams per patient. Of the total number of exams, CT accounted for 6126 (5%), MRI for 15,190 (14%), US for 326 (0%), and X-ray for 89,911 (81%) (Figure 2).
There were 304,235 patients who saw a physician for an LBP condition in FY 2022/23, with a total of 64,001 public DI exams ordered for LBP-related reasons in the same FY (Supplemental Tables S10). That represents 0.21 exams per patient. Of the total number of exams, CT accounted for 3080 (5%), MRI for 21,977 (34%), US for 8 (0%), and X-ray for 38.936 (61%) (Figure 2).
The cost for shoulder/knee/LBP-related DI services was estimated at $29.07 million (Table 2), of which CT, MRI, US, and X-ray accounted for 14.3%, 48.5%, 0.4%, and 36.8%, respectively. Of these costs, patients with shoulder conditions accounted for 23.6%, patients with knee conditions 41.3%, and patients with LBP conditions 35.1%.
Table 2.
Cost of DI exams ($M).
| Conditions | CT | MRI | US | GR | All DI exams |
|---|---|---|---|---|---|
| Shoulder | $ 2.00 | $ 2.17 | $ 0.06 | $ 2.63 | $ 6.87 |
| Knee | $ 1.44 | $ 4.87 | $ 0.06 | $ 5.63 | $ 11.99 |
| LBP | $ 0.72 | $ 7.05 | $ 0.00 | $ 2.44 | $ 10.21 |
| Total | $ 4.17 | $ 14.09 | $ 0.12 | $ 10.70 | $ 29.07 |
For all studied MSK conditions, the number of CT and MRI scans per patient was similar between males and females (calculated from Supplemental Tables S8-S10). In terms of age, the number of exams per patient varied by condition and type of exam. Of all LBP patients, the oldest received the most MRIs (Supplemental Table S10), while of all knee patients the youngest received the most MRIs (Supplemental Table S9).
Multivariate analyses (Supplemental Table S11) showed that males used less physician services than females (IRR = 0.963, p < .001), as did younger patients. Compared to the 18–64 years old age group, patients <18 years used less physician services (IRR = 0.748, p < .001), while patients >64 years used more (IRR = 1.324, p < .001). Differences were also noticed between Alberta’s five geographic health zones (Calgary and Edmonton—the two biggest cities of Alberta were considered as urban—see Supplemental Table S7). Compared to the Calgary zone, a higher physician visit rate was found in the North zone (IRR = 1.01, p < .01), and lower physician visit rates were found in Edmonton, South, and Central zones (IRR = 0.89 to 0.98, p < .001). Regarding the Charlson comorbidity index, people with a higher score used more physician services (IRR = 1.53, p < .001). People in the North zone used less physician services (IRR = 0.97, p < .001), but their costs were higher (coefficient = 1.06, p < .001).
Regarding determinants of CT and MRI ordering (Supplemental Table S12), males were more likely to be referred for CT and MRI exams than females (IRR = 1.09 and IRR = 1.15, respectively, both p < .001). Compared to the 18–64 years-old age group, patients >64 years old were more likely to be referred for CT (IRR = 1.05, p < .05) but less likely for MRI (IRR = 0.51, p < .001), while patients <18 years old were less likely to be referred for CT (IRR = 0.81, p < .001) but more likely for MRI (IRR = 1.52, p < .001). Compared to the Calgary zone, Edmonton and Central zones patients were less likely to be referred for CT exams (IRR = 0.91 and IRR = 0.92, with p < .001 and p < .05, respectively), while North zone was more likely (IRR = 0.1.25, p < .001). For MRI exams, relative to the Calgary zone, patients in the Edmonton, North, and South zones were more likely to have this assessment (IRR = 1.36, p < .001, IRR = 1.61, p < .001, and IRR = 1.09, p < .001, respectively), while patients in the Central zone were similarly likely (IRR = 1.01, p > .05). Patients with higher comorbidity index scores were more likely to be referred for CT (IRR = 1.71, p < .01) but similarly for MRI exams (IRR = 0.996, p > .05). There was a positive correlation between the number of visits to GP or specialist and the likelihood of being referred for CT (IRR = 1.05, p < .001) and MRI exams (IRR = 1.02, p < .001).
Discussion
Our comprehensive population-based study highlights the prevalence and pattern of healthcare utilization for patients with shoulder, knee, and LBP conditions in Alberta, Canada. The results indicate that Albertans frequently visited physicians for these MSK conditions. In the FY 2022/23, 10.4%, 7.0%, and 6.7% of the population saw physicians for shoulder, knee, and LBP conditions, respectively. This costs Alberta $307.04 million ($67.93 per capita), of which shoulder accounted for 43%, knee for 26%, and LBP for 31%. In the same FY, 17,734 CT, 43,939 MRI, 686 US, and 170,936 X-ray exams related to shoulder/knee/LBP conditions were ordered for these patients. Based on the cost per exam of $234.9 for CT, $320.6 for MRI, $172.0 for US, and $62.6 for X-ray (M. MacMillan, personal communication, March 15, 2020), the total cost for these DI services was estimated at $29.07 million, of which CT, MRI, US, and X-ray accounted for 14%, 48%, 0%, and 37%, respectively. In total, $336.11 million were expended on physician visits and DI for shoulder, knee, and LBP conditions in Alberta in the FY 2022/23, equivalent to 6.1% of all physician costs and 1.4% of the total provincial healthcare budget. 25 This demonstrates a significant burden attributable to MSK diseases annually. These findings are comparable to a similar study completed by Power et al. (2022) in Ontario, Canada. 26
Our results also indicate that patient factors such as female, older age, and comorbidities are drivers for physician visits; and the more physician visits, the greater the likelihood of CT and MRI exams being ordered. This is consistent with previous studies. For example, Kazanjian et al., 27 reported that females are twice as likely as males to visit their regular family physician. Steven Globerman 28 reported that per-capita spending on healthcare is substantially higher for individuals aged 65+ than for younger individuals. Fisher et al. 29 reported that health service use and associated costs consistently increased as the number of comorbidities increased.
Additionally, the North zone had the highest proportion of physician visits compared to the other four zones, yet only has ∼8% of the province’s total population. However, this population largely lives in rural and remote areas. This finding could be attributed to poorer health and challenges with scarce healthcare resources often experienced by rural/remote residents. This forces rural residents to seek care from generalists and emergency departments, who have to provide a wide range of services across multiple health conditions and sustain a heavy workload in isolation with high levels of clinical responsibility.30,31 This results in care variations often with multiple recurrent visits, unnecessary advanced DI (i.e., MRI), and a significant proportion of patients referred to urban specialists. 32
Our findings suggest that there is heavy reliance on the public health system to diagnose and treat patients with MSK conditions. The demand for MSK assessment and associated costs are expected to increase as the population ages. 33 Research supports early assessment and intervention to improve functional outcomes and minimize long-term disability and morbidity. 34 This relies on prompt diagnosis and initiation of appropriate treatment plans. 35 Our findings continue to support evidence that a large proportion of Albertans rely on pursuing structural diagnosis through DI and specialist consultation. Specialist consultation is typically unnecessary unless non-operative treatments fail to yield positive functional outcomes. Approximately 75% and 95% of patients with shoulder and LBP,36–38 respectively, can effectively be managed non-operatively and with active exercise therapy delivered by allied healthcare providers in the private sector. Excessive reliance on imaging can delay diagnosis and treatment, contribute to long wait times and wasted resources, and potentially lead to inappropriate interventions. Unnecessary specialist referrals also delay diagnosis and subsequent treatment of patients in which surgery is indicated, while delaying early appropriate treatment for non-surgical candidates. From a societal perspective, our findings can support policymakers and healthcare professionals better coordinate and enhance patient-oriented care and health service delivery.
Limitations
Strengths of our study included its population-based design and wide breadth of conditions and services included. However, we acknowledge that there are several limitations. As with all administrative data, ICD-9 codes used in claims are designed to represent diagnostic and not functional status. Therefore, it prevented us from distinguishing service utilization among individuals with different levels of functioning and complexity of needs. 39 There is an inability to quantify whether all DI referrals were actually carried out. This impacts the accuracy of the total DI costs reported here. It was not feasible to use administrative databases to identify the appropriateness of DI exams and why the number of US related to shoulder and knee conditions was lower than expected, and further study is required. Another limitation was that this study used a public health system perspective, which does not include healthcare services not insured according to the Canada Health Act such as the cost of physiotherapy services (covered by private insurance), private DI (<10% of all CT and MRI exams), 40 out-of-pocket expenditures for aids (i.e., therapy equipment) and over-the-counter medications, or indirect costs for lost productivity. Again, our results only present a fraction of the total utilization and cost across the entire spectrum of care for MSK conditions. Also, the prevalence reported here does not include patients who are not treated by physicians but by physiotherapists or any other providers who are not covered by the AHCIP. Future studies that include patient and private sector perspectives would provide a more comprehensive evaluation and provide a more wholesome view of the total utilization and cost of MSK conditions.
Conclusion
Our findings show that MSK conditions are a significant burden to the healthcare system. Visits to family physicians, specialists, and the ordering of DI contribute to extensive utilization and public health system costs. Using costs to understand the magnitude of health service utilization for MSK assessment and treatment for shoulder, knee, and LBP conditions is a critical first step to changing health policies aiming to reduce the burden of MSK conditions on individuals and society. The methodology used in this paper is reproducible in other health systems or organizations and can be used to understand, prioritize, and address the drivers of MSK assessment and treatment costs.
Supplemental Material
Supplemental Material for Costs of physician and diagnostic imaging services for shoulder, knee, and low back pain conditions: A population-based study in Alberta, Canada by Nguyen Xuan Thanh, Breda Eubank, Arianna Waye, Jason Werle, Richard Walker, David A Hart, David M Sheps, Geoff Schneider, Tim Takahashi, Tracy Wasylak, and Mel Slomp in British Journal of Pain.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Nguyen Xuan Thanh https://orcid.org/0000-0003-3984-7877
References
- 1.GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020; 396(10258): 1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canadian Institute of Health Research . Institute of musculoskeletal health and arthritis. IMHA 2014–2018 strategic plan: enhancing musculoskeletal, skin and oral health. Ottawa, ON: Canadian Institute of Health Research. 2019. https://cihr-irsc.gc.ca/e/48830.html (Accessed 20 July 2020). [Google Scholar]
- 3.Jordan KP, Kadam UT, Hayward R, et al. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Muscoskel Disord 2010; 11(1): 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacKay C, Canizares M, Davis AM, et al. Health care utilization for musculoskeletal disorders. Arthritis Care Res 2010; 62(2): 161–169. [DOI] [PubMed] [Google Scholar]
- 5.Power JD, Perruccio AV, Desmeules M, et al. Ambulatory physician care for musculoskeletal disorders in Canada. J Rheumatol 2006; 33(1): 133–139. [PubMed] [Google Scholar]
- 6.Slim ZN, Chaaya M, Habib RR, et al. High burden of musculoskeletal conditions: a problem that has only recently come to recognition. Chron Illness 2011; 7: 311–320. [DOI] [PubMed] [Google Scholar]
- 7.Jinks C, Jordan K, Croft P. Measuring the population impact of knee pain and disability with the western Ontario and McMaster universities osteoarthritis index (WOMAC). Pain 2002; 100: 55–64. [DOI] [PubMed] [Google Scholar]
- 8.Grotle M, Hagen KB, Natvig B, et al. Prevalence and burden of osteoarthritis: results from a population survey in Norway. J Rheumatol 2008; 35: 677–684. [PubMed] [Google Scholar]
- 9.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001; 60: 91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felson DT, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum 1998; 41: 1343–1355. [DOI] [PubMed] [Google Scholar]
- 11.Nguyen US, Zhang Y, Zhu Y, et al. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med 2011; 155(11): 725–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lo T. A study of healthcare utilization in patients with chronic low back pain using Alberta’s administrative health data: a SUDA project. Edmonton: Institute of Health Economics, 2020. https://www.ihe.ca/publications/a-study-of-healthcare-utilization-in-patients-with-chronic-low-back-pain-using-alberta-s-administrative-health-data (Accessed 6 August 2020). [Google Scholar]
- 13.Linsell L, Dawson J, Zondervan K, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology 2006; 45(2): 215–221. [DOI] [PubMed] [Google Scholar]
- 14.Flook NW. Primary care physicians and musculoskeletal disorders–the challenges increase. J Rheumatol 2006; 33(1): 4–5. [PubMed] [Google Scholar]
- 15.Orenstein S, Kania-Richmond A, Cunningham C. The bone and joint health strategic clinical network in partnership with the primary health care integration network. Edmonton, AB: Musculoskeletal Care in Alberta’s Primary Care Networks, 2021. https://www.albertahealthservices.ca/assets/about/scn/ahs-scn-bjh-msk-care-in-pcns.pdf. [Google Scholar]
- 16.Vanderby S, Pena-Sanchez JN, Kalra N, et al. Finding the truth in medical imaging: painting the picture of appropriateness for magnetic resonance imaging in Canada. Can Assoc Radiol J 2015; 66: 323–331. [DOI] [PubMed] [Google Scholar]
- 17.Emery DJ, Shojania KG, Forster AJ, et al. Overuse of magnetic resonance imaging. JAMA Intern Med 2013; 173(9): 823–825. [DOI] [PubMed] [Google Scholar]
- 18.Alberta Health. Analytics and performance reporting branch. In Overview of administrative health datasets. Edmonton, AB: Alberta Health . 2017, https://open.alberta.ca/dataset/overview-of-administrative-health-datasets. Accessed July 20, 2020.
- 19.Alberta Health Services . Diagnostic imaging common procedure/examination list. April 1st, 2023. Alberta, Canada: Alberta Health Services, 2019. [Google Scholar]
- 20.Thanh NX, Dmytruk K, O’Connell P, et al. Return on investment of the diabetes foot care clinical pathway implementation in Alberta, Canada. Diabetes Res Clin Pract 2020; 165: 108241. DOI: 10.1016/j.diabres.2020.108241. [DOI] [PubMed] [Google Scholar]
- 21.Bank of Canada . Inflation calculator. Ottawa, ON: Bank of Canada. https://www.bankofcanada.ca/rates/related/inflation-calculator/, (Accessed 1 Oct 2021). [Google Scholar]
- 22.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011; 173(6): 676–682. [DOI] [PubMed] [Google Scholar]
- 23.Statistics Canada . Summary statistics, estimated (1996 to 2021), projected (2022 to 2046), medium scenario, Alberta. 2022-2046-01-Alberta-population-projections-summary.xlsx (live.com). Ottawa, ON: Statistics Canada. Accessed January 25, 2024. [Google Scholar]
- 24.Canadian Institute for Health Information . National health expenditure trends. In: CBC. How Alberta went from being one of the lowest-spending provinces on health care to one of the highest. Toronto, ON: Canadian Institute for Health Information, 2019. Available from. https://www.cbc.ca/news/canada/calgary/alberta-health-spending-history-1.5289747. 2018. Accessed July 20, 2020. [Google Scholar]
- 25.Government of Alberta . Health annual report 2023/24. Edmonton, AB, Government of Alberta. https://www.alberta.ca/government-and-ministry-annual-reports#23-24 (accessed 3 September 2024). [Google Scholar]
- 26.Power JD, Perruccio AV, Paterson JM, et al. Healthcare utilization and costs for musculoskeletal disorders in Ontario, Canada. J Rheumatol 2022; 49(7): 740–747. [DOI] [PubMed] [Google Scholar]
- 27.Kazanjian A, Morettin D, Cho R. Health care utilization by Canadian women. BMC Women Health 2004; 4(Suppl 1): S33. DOI: 10.1186/1472-6874-4-S1-S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Globerman S. Aging and expenditure in health care. Calgary, AB: Fraser Research Bulletin, 2021. https://www.fraserinstitute.org/sites/default/files/aging-and-expenditures-on-health-care.pdf (Accessed 11 July 2022). [Google Scholar]
- 29.Fisher K, Griffith L, Gruneir A, et al. Comorbidity and its relationship with health service use and cost in community-living older adults with diabetes: a population-based study in Ontario, Canada. Diabetes Res Clin Pract 2016; 122: 113–123. [DOI] [PubMed] [Google Scholar]
- 30.Haggerty JL, Roberge D, Lévesque JF, et al. An exploration of rural–urban differences in healthcare-seeking trajectories: implications for measures of accessibility. Health Place 2024; 28: 92–98. DOI: 10.1016/j.healthplace.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 31.Murphy P, Burge F, Wong ST. Measurement and rural primary health care: a scoping review. Rural Rem Health 2019; 19: 4911. DOI: 10.22605/RRH4911. [DOI] [PubMed] [Google Scholar]
- 32.Laurent S. Rural Canada: access to health care. Toronto, ON: Canadian Institute for Health Information. https://publications.gc.ca/Collection-R/LoPBdP/BP/prb0245-e.htm#32end (2002). [Google Scholar]
- 33.Briggs AM, Cross MJ, Hoy DG, et al. Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 world health organization world report on ageing and health. Gerontol 2016; 56 Suppl 2(2): S243–S255. DOI: 10.1093/geront/gnw002. [DOI] [PubMed] [Google Scholar]
- 34.Bath B, Grona SL, Janzen B. A spinal triage programme delivered by physiotherapists in collaboration with orthopaedic surgeons. Physiother Can 2012; 64: 356–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boakye O, Birney A, Suter E, et al. Scope of practice review: providers for triage and assessment of spine-related disorders. J Multidiscip Healthc 2016; 9: 227–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boorman RS, More KD, Hollinshead RM, et al. The rotator cuff quality-of-life index predicts the outcome of nonoperative treatment of patients with a chronic rotator cuff tear. J Bone Joint Surg Am 2014; 96: 1883–1888. DOI: 10.2106/JBJS.M.01457. [DOI] [PubMed] [Google Scholar]
- 37.Boorman RS, More KD, Hollinshead RM, et al. What happens to patients when we do not repair their cuff tears? five-year rotator cuff quality-of-life index outcomes following nonoperative treatment of patients with full-thickness rotator cuff tears. J Shoulder Elbow Surg 2018; 27: 444–448. DOI: 10.1016/j.jse.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 38.Van Middelkoop M, Rubinstein SM, Verhagen AP, et al. Exercise therapy for chronic nonspecific low-back pain. Best Pract Res Clin Rheumatol 2010; 24(2): 193–204. [DOI] [PubMed] [Google Scholar]
- 39.Arim RG, Miller AR, Guèvremont A, et al. Children with neurodevelopmental disorders and disabilities: a population-based study of healthcare service utilization using administrative data. Dev Med Child Neurol 2017; 59(12): 1284–1290. [DOI] [PubMed] [Google Scholar]
- 40.Canadian Agency for Drugs and Technologies in Health . Privately operated medical imaging facilities across Canada: CADTH health technology review. Ottawa, ON: Canadian Agency for Drugs and Technologies in Health, 2023. https://www.ncbi.nlm.nih.gov/books/NBK594387/. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Costs of physician and diagnostic imaging services for shoulder, knee, and low back pain conditions: A population-based study in Alberta, Canada by Nguyen Xuan Thanh, Breda Eubank, Arianna Waye, Jason Werle, Richard Walker, David A Hart, David M Sheps, Geoff Schneider, Tim Takahashi, Tracy Wasylak, and Mel Slomp in British Journal of Pain.