Abstract
The palm is of great importance for maintaining a functioning hand. The reconstructive demands of thickness, texture, color matching, pliability, and sensation for palmar defects represent a unique challenge for plastic surgeons. This study introduced a novel versatile design for the ulnar palmar artery perforator flap (UPAPF) to cover large palmar soft-tissue defects of the hand. The fifth metacarpophalangeal joint was identified as a landmark where the perforator was nearly 1 to 1.5 cm proximal. A template of the defect was outlined after adequate debridement. Meticulous dissection was executed under loupe magnification to trace the perforator until an adequate length of the pedicle was obtained for rotation. The harvested type B fasciocutaneous flap was rotated nearly 90° to be insetting on the palmar defect. Two patients were presented with a soft-tissue defect of the palm measuring 4.8 × 5.5 cm2 and 3.8 × 5 cm2, respectively. The flap was harvested and positioned at the defects. The flaps survived in the 2 cases with minimal donor site complications. The patients acquired protective sensations within the flap at the end of the follow-up period. The UPAPF provides a stable coverage for palmar soft-tissue defects with satisfactory aesthetic and functional results. It is a convenient addition to the armamentarium for reconstructing palmar soft-tissue defects of the hand.
Keywords: palm, soft-tissue defect, reconstruction, ulnar palmar artery perforator
Introduction
The palm is of great importance for maintaining a functioning hand. While the soft-tissue coverage of the palm protects the underneath vital structures, it has peerless sensory and functional components. The thick, glabrous palmar skin resists the shearing forces of daily life activities and transfers different sensations. 1 Palmar soft-tissue defects can lead to serious functional disability of the hand. It results in exposed vital functional structures and loss of the anatomical architecture of the palm. 2 The reconstructive demands of thickness, texture, color matching, pliability, and sensation for palmar defects represent a unique challenge for hand surgeons. The reconstruction necessitates durable coverage, protecting against contracture development. 3 It should facilitate the gliding of tendons with an adequate range of motion for fingers and joints. The long-term stability, durability, and sensibility of the palm should be maintained to protect it from chronic shearing stress. This should be accomplished while minimizing the donor site morbidity and providing satisfactory aesthetic results.4,5
There are many local and regional flaps for soft-tissue reconstruction of the palm. While the ulnar artery forearm flap has been a successful solution for palm reconstruction, the ulnar artery needed to be sacrificed. The distally based radial forearm flap is the mainstay flap for palm reconstruction. However, it needed a section from the radial artery, resulting in significant donor site morbidity.6-8 Distant flaps are associated with prolonged immobility and stiffness due to late rehabilitation. Furthermore, extensive palmar soft-tissue defect and additional soft-tissue damage to the forearm may impede the local and regional reconstruction options. Free flaps provided excellent soft-tissue coverage and early rehabilitation. Conversely, this reconstruction option needed special equipment, microsurgery training, and prolonged operation time.9,10 These limitations highlighted the need for feasible, safe, and versatile flaps to cover the palmar soft-tissue defects of the hand.
Local perforator flaps are widely used for microsurgical reconstruction of the hand. 11 These flaps provided better accuracy, minimum donor site morbidity, and thinness coverage. They have the benefits of using a matched tissue in reconstruction; furthermore, no major vessels scarify or microvascular sutures are needed.12,13 The rich vascular network of the hand offered constant perforators in the hypothenar area. The ulnar palmar artery perforator flap (UPAPF) was introduced to cover soft-tissue defects of the little finger.14 -16 However, there is no available evidence for the use of UPAPF for the reconstruction of palmar soft-tissue defects. This study introduced a novel versatile design for the UPAPF to cover large soft-tissue defects of the palm.
Materials and Methods
All surgical interventions were carried out in conformity with the Declaration of Helsinki and after a complete explanation of the possible benefits and risks of the surgical procedure. All patients were assigned informed consent before the surgery. The study was performed from January 2020 to March 2022.
Surgical Procedure
The surgical procedures were carried out under general anesthesia. The tourniquet was applied at the proximity of the arm. The patients were supine while the operated limb was slightly laterally abducted. A handheld Doppler probe was used to locate the ascending branch of the septocutaneous perforator of the ulnar palmar digital artery. This septocutaneous perforator travels between the superficial and deep layers of the hypothenar muscles. The flap was harvested based on the ascending branch of the septocutaneous perforator of the ulnar palmar digital artery. The fifth metacarpophalangeal joint was identified as a landmark where the perforator was constant and approximately 1 to 1.5 cm proximal to the metacarpophalangeal joint. This perforator is more volar, constant, and reliable. Hypothenar fascia must be included in the flap to capture the perforator branches and their communications. The line between the fifth metacarpal bone and the abductor digiti minimi muscle was identified as the axis of the flap. A template of the defect was outlined after adequate debridement. The flap was designed to be slightly larger than the defect dimensions. The flap extended proximally closer to the styloid process of the ulna to cover larger palmar defects. Primary closure or the need for grafting of the donor site was detected based on the pinch test.
The incision was performed at the radial dorsal aspect of the flap. It was in a distal to proximal direction down to the extensor paratenon on the dorsal aspect and the fascia of abductor digiti minimi on the palmar side. Meticulous dissection was executed under loupe magnification to trace the perforator until an adequate length of the pedicle was obtained for rotation. The harvested type B fasciocutaneous flap was rotated nearly 90° to be inset into the palmar defect. The tourniquet was deflated to assess the intraoperative viability of the flap (Figure 1).
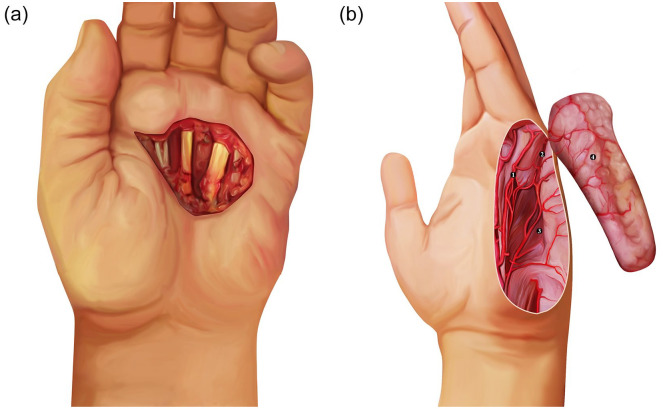
Figure 1.
A diagramatic illustration of the design and the anatomical landmarks of the ulnar palmar artery perforator flap for reconstructing soft-tissue defects of the palm.
Note. (a) A soft-tissue defect at the distal aspect of the palm. (b) The location of the ulnar palmar artery perforator and the flap design: (1) The ulnar palmar artery of the little finger, (2) the septocutaneous perforator of the ulnar palmar artery of the little finger, (3) the abductor digit minimi muscle, and (4) the harvested ulnar palmar artery perforator flap.
Results
Case 1
A female patient, aged 65 years, diabetic and hypertensive, presented with recurrent dermatofibrosarcoma at the distal palm of the left hand of 1-year duration. The lesion measured 2 × 3 cm, infiltrating the third common digital artery. Excision was done with a safety margin based on intraoperative frozen section, resulting in a soft-tissue defect of 4.8 × 5.5 cm2 in the distal part of the palm. The UPAPF was harvested as per the size of the defect to cover the exposed flexor tendons and the neurovascular structures traversing the distal palm. The donor site was closed primarily and the viability of the flap was established intraoperatively. The duration from flap harvesting to insetting was 32 minutes. The patient received postoperative radiotherapy and chemotherapy. Twenty-two months postoperatively, the flap survived completely with an acceptable appearance and texture apart from guttering at the donor site. The patient acquired protective sensations within the flap at the end of the follow-up period. The patient achieved full range of motion at the end of follow-up. There was no evidence of the recurrence of the dermatofibrosarcoma (Figures 2 and 3).
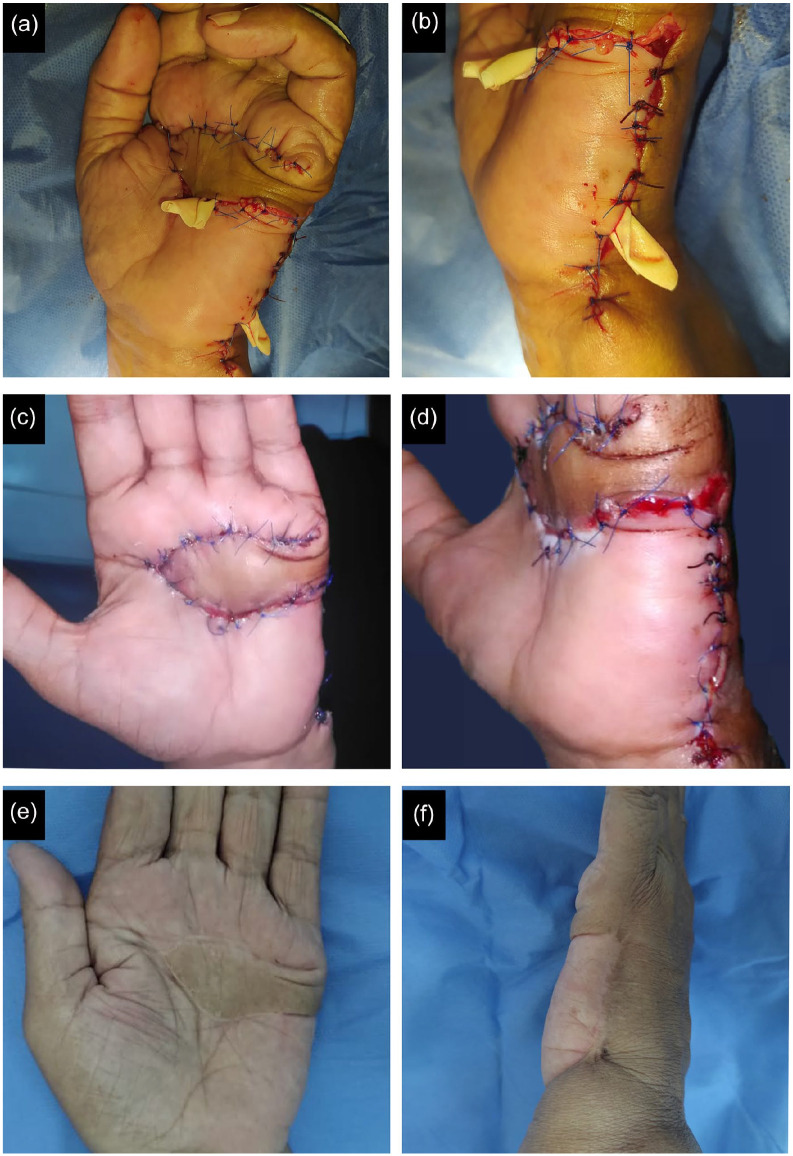
Figure 2.
Female patient, aged 65 years, presented with recurrent dermatofibrosarcoma at the distal palm of the left hand of 1-year duration.
Note. (a) Recurrent dermatofibrosarcoma at the distal palm of the left hand. (b) Excision of the tumor was done with a safety margin. (c) A soft-tissue defect resulted at the distal palm measuring 4.8 × 5.5 cm2. (d) Locating the ulnar palmar artery perforator 1 cm proximal to the fifth metacarpophalangeal joint and flap marking. (e) Harvesting of the ulnar palmar artery perforator flap and rotating it nearly 90o as pedicle-based flap. (f) Insisting on the ulnar palmar artery perforator flap to cover the palmar soft-tissue defect.
Figure 3.
Immediate intra-operative and post-operative results of ulnar palmar artery perforator flap for reconstructing soft tissue defect of the distal palm of the left after recurrent dermatoliposaracoma excision.Note. (a) Intraoperative closure the soft-tissue defect of the palm using the ulnar palmar artery perforator flap. (b) Primary closure of the donor site. (c) Recipient site 10 days after insetting on the flap. (d) Donor site 10 days postoperatively after insetting on the ulnar palmar artery perforator. (e) The recipient site 22 months postoperatively showing complete healing of the ulnar palmar artery perforator flap. (f) The donor site 22 months postoperatively showing complete healing.
Case 2
A male patient, aged 35 years, nondiabetic and nonhypertensive, presented with contracture of the palm after groin flap to reconstruct a traumatic soft-tissue defect. After contracture release, a soft-tissue defect of 3.8 × 5 cm2 resulted in the distal palm. The UPAPF was harvested and positioned at the defect. The donor site was closed with a thick split-thickness skin graft harvested from the anterolateral aspect of the thigh. The time taken from flap harvesting to insetting was 38 minutes. Six months postoperatively, the flap survived completely and the patient retained an acceptable range of motion at the level of the metacarpophalangeal joints. The graft at the donor site healed uneventfully with no donor site complications and satisfactory cosmetic outcomes. There was clinical evidence of retained protective sensations within the flap. The patient achieved a full range of motion at the end of the follow-up (Figure 4).
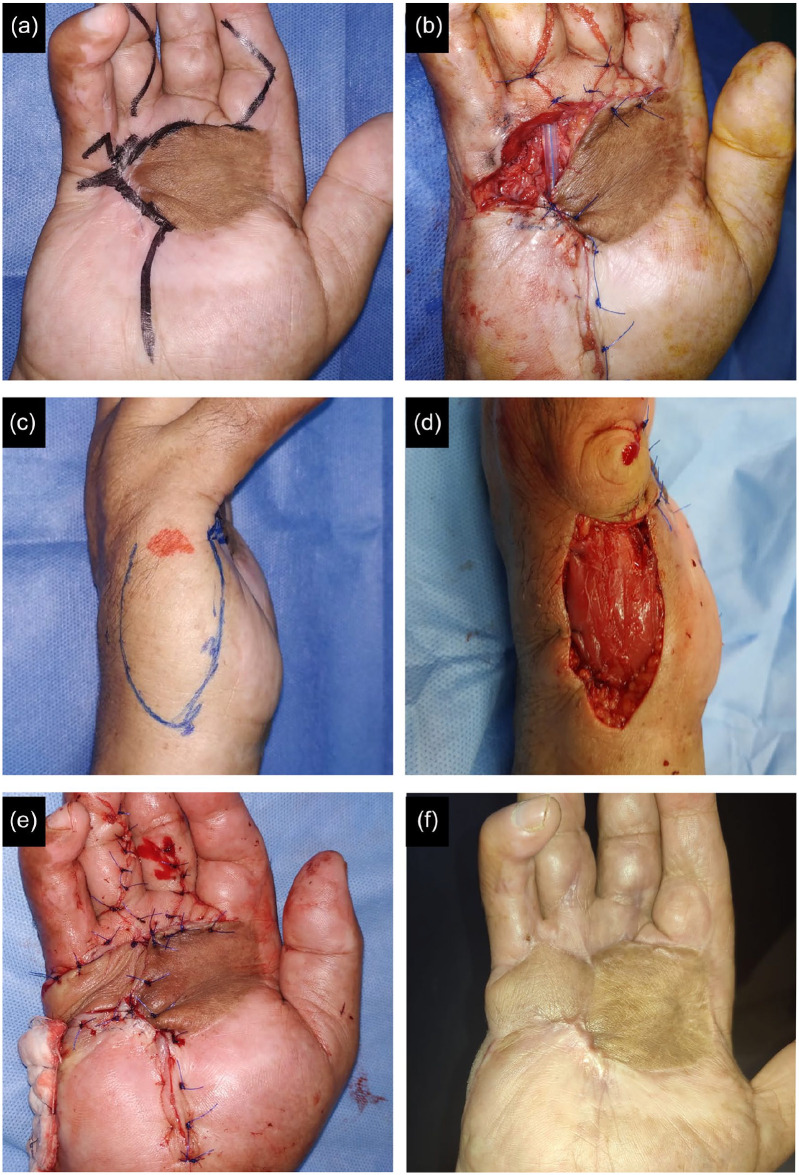
Figure 4.
Male patient, aged 35 years, presented with contracture of the palm after groin flap for reconstruction of a traumatic soft-tissue defect.
Note. (a) Preoperative planning for contracture release. (b) Contracture release resulted in soft-tissue defect measuring 3.8 x 5 cm2. (c) Locating the ulnar palmar artery perforator 1 cm proximal to the fifth metacarpophalangeal joint and flap marking. (d) Harvesting of the ulnar palmar artery perforator flap and rotating it 90o as pedicled flap. (e) Insisting on the ulnar palmar artery perforator flap to cover the palmar soft-tissue defect. (f) The recipient site 6 months postoperatively.
Discussion
Perforator flaps represent a new era for resurfacing soft-tissue defects of the hand. These flaps could individualize the reconstruction procedure with minimal donor site morbidity and acceptable cosmetic outcomes. The skin of the palmar and dorsal aspects of the ulnar side of the hand is ideal for resurfacing soft-tissue defects of the hand. However, the use of perforator-based flaps for coverage of palmar soft-tissue defects is limited.5,17 This study revealed the durability, stability, usability, and versatility of the UPAPF for reconstructing soft-tissue defects of the palm. The flap is easy to harvest and inset, with satisfactory functional and aesthetic results. It can be safely raised without scarifying the main common digital arteries. In accordance with these findings, Hao et al 14 reported the usability of the UPAPF for reconstructing soft-tissue defects of the little finger in 16 cases with acceptable results and no donor site morbidities. In this respect, Estawrow et al 18 reported the reliability of the flap for reconstructing dorsal hand and little finger defects.
The skin of the hypothenar eminence and posteromedial aspect of the hand is supplied mainly by 2 arteries. This includes the septocutaneous perforators arising from the little finger’s ulnar palmar artery and the ulnar artery’s descending dorsal carpal branch. The ulnar palmar digital artery consistently gave off up to 6 perforators lying deep into the hypothenar muscles. The distal half of the ulnar aspect of the hypothenar area is supplied by constant neural and vascular supply from the ulnar palmar digital artery and palmar or dorsal cutaneous branch of the ulnar nerve. 19 The perforators arising from the ulnar palmar digital artery of the little finger have robust connections with the perforators arising from the deep branch of the ulnar artery. 20 The ascending branch of the septocutaneous perforator of the ulnar palmar digital artery is the largest and the primary communicator between the ulnar palmar and dorsal ulnar arteries.16,21 Harvesting the flap based on this branch maintains its viability and does not require sacrificing a major hand artery. The location of the perforator is often proximal to the defect in which the long pedicle is not necessary for flap harvesting. The flap can be propeller-based or island-based to cover adjacent and distal palmar defects. The flap dissection was performed on the subfascial plan without intramuscular dissection of the septocutaneous perforator to the source artery. Herein, the source artery makes no limitation to the surgical procedure, highlighting the flap’s suitability and feasibility for resurfacing palmar soft-tissue defects.
The UPAPF represents a versatile procedure for reconstructing large palmar defects. It can be extended just distal to the styloid process of the ulna with a low risk of flap necrosis. 14 Furthermore, harvesting the flap from the hypothenar eminence results in a larger flap and respects the like with like principle for covering palmar soft-tissue defects. The anastomosis between the ulnar palmar artery and the dorsal carpal branch of the ulnar artery indicates the reliability of flap vascularization for coverage of large palmar defects. There is a constant communicator perforator between the dorsal ulnar branch and palmar system at the metacarpal head. The venous drainage of the flap is maintained through the superficial venous system and the vena comitans associated with ulnar palmar and dorsal perforators. There were minimal donor site complications and neither of the included patients experienced a limited range of motion at the level of the metacarpophalangeal joints. In this respect, Postan et al 22 reported using a proximal hypothenar fasciocutaneous flap based on a cutaneous branch of the deep palmar artery for covering soft-tissue defects over the wrist joint. The flap was associated with no complications and had acceptable wrist movement and sensibility. 22 Tapan et al 23 used the hypothenar island flap based on the proper ulnar palmar digital artery to reconstruct soft-tissue defects of the little finger. Omokawa et al 19 used the reversed flow ulnar hypothenar flap based on the ulnar palmar digital artery of the little finger for reconstructing soft-tissue defects of the fingers. These flaps are relatively smaller than the UPAPF and were used for reconstructing the soft-tissue defects of the little finger rather than the distal palm. Furthermore, the flaps were designed mainly from the hypothenar areas palmar aspect and scarified the little finger’s ulnar palmar digital artery. 24 Yamamoto et al 25 described a free hypothenar flap transfer based on common or ulnar palmar digital arteries for reconstructing soft-tissue defects of the fingers. The donor site was closed by a local transpositional flap to minimize the donor site complications. 25 Our flap is relatively larger and was used for reconstructing soft-tissue defects of the distal palm rather than the fingers.
The hypothenar muscles provided good padding, resulting in stable scars at the donor site. Paradoxically, one of the major drawbacks of the UPAPF is the lack of sensation. This could be resolved by end-to-side neurorrhaphy between the cutaneous branches of the dorsal ulnar nerve and the common digital nerves.26,27 Furthermore, patients may be left with a scar on the ulnar aspect of the hand. This may be associated with a painful scar in an area significantly relevant to hand functions for daily life activities. The palm is divided into 5 aesthetic and functional units. This included the hypothenar, thenar, opposition, central triangular, and metacarpal subunits. The UPAPF is ideal for reconstructing the metacarpal subunit of the palm. The thin flap allows easy gliding of the underlying flexor tendons, accommodating metacarpal and phalangeal joints flexion and extension with an adequate range of motion.
This study represents a new flap design for reconstructing palmar soft-tissue defects. While the study highlighted the usability of the UPAPF, some limitations should be considered. The lack of a comparative arm and limited sample size highlighted the need for further randomized controlled trials to establish more comprehensive evidence for future surgical practice.
Conclusion
The UPAPF is a reliable procedure for reconstructing soft-tissue defects of the palm. It provides stable coverage with satisfactory functional and cosmetic outcomes. It is a convenient addition to the armamentarium for reconstructing palmar soft-tissue defects of the hand.
Footnotes
Author Contributions: Each author took part in the design of the study, contributed to data collections, and participated in writing the manuscript. All authors agree to accept equal responsibility for the accuracy of this article.
Ethical Approval: The study was carried out in conformity with the guidelines reported in the Declaration of Helsinki and after a complete explanation of the possible benefits and risks of the surgical procedure. All patients assigned informed consent before the surgery.
Statement of Human and Animal Rights: The study was carried out in conformity with the guidelines reported in the Declaration of Helsinki and after a complete explanation of the possible benefits and risks of the surgical procedure.
Statement of Informed Consent: Written informed consent was obtained from the patients for their anonymized information to be published in this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Abdelrahman Awadeen  https://orcid.org/0000-0001-9966-9270
https://orcid.org/0000-0001-9966-9270
Ali Mohamed Elameen  https://orcid.org/0000-0001-7701-2171
https://orcid.org/0000-0001-7701-2171
References
- 1. Rehim SA, Chung KC. Local flaps of the hand. Hand Clin. 2014;30(2):137-v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ono S, Sebastin SJ, Yazaki N, et al. Clinical applications of perforator-based propeller flaps in upper limb soft tissue reconstruction. J Hand Surg Am. 2011;36(5):853-863. [DOI] [PubMed] [Google Scholar]
- 3. Biswas D, Wysocki RW, Fernandez JJ, et al. Local and regional flaps for hand coverage. J Hand Surg Am. 2014;39(5):992-1004. [DOI] [PubMed] [Google Scholar]
- 4. Bashir MM, Sohail M, Shami HB. Traumatic wounds of the upper extremity: coverage strategies. Hand Clin. 2018;34(1):61-74. [DOI] [PubMed] [Google Scholar]
- 5. Ahmad M. Management of hand trauma. J of Surg Pakistan. 2008;13(3):128-131. [Google Scholar]
- 6. Chase RA, Hentz VR, Apfelberg D. A dynamic myocutaneous flap for hand reconstruction. J Hand Surg Am. 1980;5(6):594-599. [DOI] [PubMed] [Google Scholar]
- 7. Akdag O, Karamese M, NebilSelimoglu M, et al. Reverse adipofascial radial forearm flap surgery for soft-tissue reconstruction of hand defects. Eplasty. 2016;16:e35. [PMC free article] [PubMed] [Google Scholar]
- 8. Mühlbauer W, Herndl E, Stock W. The forearm flap. Plastic and Reconstr Surg. 1982;70(3):336-344. [DOI] [PubMed] [Google Scholar]
- 9. Horta R, Silva P, Costa-Ferreira A, et al. Microsurgical soft-tissue hand reconstruction: an algorithm for selection of the best procedure. J Hand Microsurg. 2011;3(2):73-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roh SY, Lee KJ, Lee DC, et al. Palmar hand wound coverage with the free flaps. Arch of Reconstr Microsurg. 2014;23(2):45-50. [Google Scholar]
- 11. Mitsunaga N, Mihara M, Koshima I, et al. Digital artery perforator (DAP) flaps: modifications for fingertip and finger stump reconstruction. J Plast Reconstr Aesthet Surg. 2010;63(8):1312-1317. [DOI] [PubMed] [Google Scholar]
- 12. Georgescu AV, Matei I, Ardelean F, et al. Microsurgical nonmicrovascular flaps in forearm and hand reconstruction. Microsurgery. 2007;27(5):384-394. [DOI] [PubMed] [Google Scholar]
- 13. Ono S, Ogawa R, Eura S, et al. Perforator-supercharged perforator-based propeller flaps. Plast Reconstr Surg. 2012;129(5):875e-877e. [DOI] [PubMed] [Google Scholar]
- 14. Hao PD, Zhuang YH, Zheng HP, et al. The ulnar palmar perforator flap: Anatomical study and clinical application. J of Plastic, Reconstr & Aesthetic Surg. 2014;67(5):600-606. [DOI] [PubMed] [Google Scholar]
- 15. Morris SF, Tang M, Almutari K, et al. The anatomic basis of perforator flaps. Clin in Plastic Surg. 2010;37(4):553-570. [DOI] [PubMed] [Google Scholar]
- 16. Appleton SE, Morris SF. Anatomy and physiology of perforator flaps of the upper limb. Hand Clin. 2014;30(2):123-135v. [DOI] [PubMed] [Google Scholar]
- 17. Mel’nikov V, Korshunov V, Romanov S, et al. Reconstruction of soft tissue of hand using island and perforator flaps. Traumatol and Orthopedics of Russia. 2014;20(3):39-43. [Google Scholar]
- 18. Estawrow MA, Gad AM. Reliability of perforator-based UPM flap for coverage of little finger and dorsal hand defect. Plast Reconstr Surg Glob Open. 2022;10(2):e4130. doi: 10.1097/GOX.0000000000004130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Omokawa S, Ryu J, Tang JB, et al. Anatomical basis for a fasciocutaneous flap from the hypothenar eminence of the hand. Br J Plast Surg. 1996;49(8):559-563. [DOI] [PubMed] [Google Scholar]
- 20. 克之 漆. Study of the anatomical bases of a perforator flap from the hypothenar eminence. Kawasaki Med. 2002; 26: 139-147. [Google Scholar]
- 21. Georgescu AV, Matei IR. Propeller perforator flaps in forearm and hand reconstruction. Eur J Orthop Surg Traumatol. 2019;29(2):357-366. [DOI] [PubMed] [Google Scholar]
- 22. Postan D. The proximal fasciocutaneous hypothenar flap based on the cutaneous branch of the deep palmar artery: a case report. Hand. 2021;16(6):NP1-NP4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tapan M, İğde M, Yıldırım AR, et al. Hypothenar island flap: a safe and excellent choice for little finger defects. Indian J Plast Surg. 2015;48(3):288-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Omokawa S, Yajima H, Inada Y, et al. A reverse ulnar hypothenar flap for finger reconstruction. Plast Reconstr Surg. 2000;106(4):828-833. [DOI] [PubMed] [Google Scholar]
- 25. Yamamoto T, Daniel BW, Kageyama T, et al. Expanding indication of free hypothenar flap transfer: sequential pedicled ulnar palm flap transfer to a relatively large hypothenar flap donor site. J Plast Reconstr Aesthet Surg. 2022;75(1):332-339. [DOI] [PubMed] [Google Scholar]
- 26. Voche P, Ouattara D. End-to-side neurorrhaphy for defects of palmar sensory digital nerves. Br J Plast Surg. 2005;58(2):239-244. [DOI] [PubMed] [Google Scholar]
- 27. Lucchina S, Fusetti C, Lazzaro L, et al. End-to-side innervated sensate radial forearm flap in the hand: a 5-year follow-up. Hand Surg Rehabil. 2019;38(3):207-210. [DOI] [PubMed] [Google Scholar]