Abstract
Study Design
Retrospective cohort study.
Objectives
The impact of delayed access to operative treatment on patient reported outcomes (PROs) for lumbar degenerative conditions remains unclear. The goal of this study is to evaluate the association between wait times for elective lumbar spine surgery and post-operative PROs.
Methods
This study is a retrospective analysis of patients surgically treated for a degenerative lumbar conditions. Wait times were calculated from primary care referral to surgery, termed the cumulative wait time (CWT). CWT benchmarks were created at 3, 6 and 12 months. A multivariable logistic regression model was used to measure the associations between CWT and meeting the minimally clinically important difference (MCID) for the Oswestry Disability Index (ODI) score at 12 months post-operatively.
Results
A total of 2281 patients were included in the study cohort. The average age was 59.4 years (SD 14.8). The median CWT was 43.1 weeks (IQR 17.8 – 60.6) and only 30.9% had treatment within 6 months. Patients were more likely achieve the MCID for the ODI at 12 months post-operatively if they had surgery within 6 months of referral from primary care (OR 1.22; 95% CI 1.11 – 1.34). This relationship was also found at a benchmark CWT time of 3 months (OR 1.33; 95% CI 1.15 – 1.54) though not at 12 months (OR 1.08; 95% CI 0.97 – 1.20).
Conclusions
Patients who received operative treatment within a 3- and 6-month benchmark between referral and surgery were more likely to experience noticeable improvement in post-operative function.
Keywords: wait times, lumbar spine surgery, epidemiology, surgical outcomes, access to care
Introduction
Degenerative lumbar conditions (DLC) cause significant pain and are a leading cause of physical disability, mental health issues, and poor quality of life amongst adults globally.1,2 In some patients, elective non-urgent surgery including lumbar decompression with or without fusion may be required for pain relief and to regain function.3–5 Wait times for surgical management of musculoskeletal conditions are a major area of concern for clinicians, policy makers and affected patients in a single payer health care system. 6 Reasons for long wait times in elective surgical care in public health care systems often include low number of specialists to the population, poor hospital operating room resource allocation, a high volume of patient referrals, and the prioritization of urgent cases over elective procedures.6,7 Those specialities which treat DLCs, orthopaedic surgery and neurosurgery, have the longest average wait times for consultation of any surgical specialty in Canada.6,7 For patients waiting for spinal assessment and surgery, symptoms may worsen, triggering pursuit of alternative health services leading to increased public spending and/or out-of-pocket costs.8–10
Wait time information in Canada is reported by the Canadian Institute for Health Information (CIHI) among other agencies. A goal of treatment by 6 months has been established as an indicator for access for hip and knee replacement; however, no national benchmark has been established for DLCs. 11 In other jurisdictions, elective wait time targets vary between 3 and 6 months, however direct comparisons are challenging given different definitions of wait times.6,12 These metrics of wait time reporting are traditionally based on the time from surgical booking to the date that surgical intervention is performed, defined as the Wait 2 time.13,14 However this may be a significant underestimate of patients’ experience waiting for surgery as there are lengthy periods of time prior to specialist consultation where patients wait for referral, or are sent for updated/additional investigations.
A cumulative wait time (CWT) includes the entire period of investigation and treatment from primary care referral to surgical management and is a more accurate representation of the experience of waiting patients but is not currently reported in Canada. 15 The objective of this study is to determine whether different CWT benchmarks wait times (3-, 6-, and 12 months) are associated with achieving clinically meaningful improvements in post-operative patient reported outcomes (PROs) for measuring disability among adult patients receiving surgical management for DLC. Our hypothesis was that patients would be less likely to reach meaningful improvement in PROs if their waits exceeded longer benchmark wait times. This study aims to provide insights to clinicians, decision makers and insurers regarding how the wait time from primary care referral to surgery can influence self-reported post-operative outcomes.
Methods
Study Design and Study Sample
This study was a retrospective analysis of a cohort of patients enrolled in the Canadian Spine Outcomes Research Network (CSORN). The network includes over 60 self-selected neurosurgical and orthopaedic spine surgeons from provinces across Canada (including Newfoundland, New Brunswick, Nova Scotia, Quebec, Ontario, Manitoba, Alberta, and British Columbia). All patients provided written informed consent to participate. Ethics approval was obtained for this study through the University of British Columbia Clinical Research Ethics board (REB# H22-00534).
Patients diagnosed with DLC requiring elective surgical management were prospectively enrolled in the cohort from January 2015 to December 2020, if they were over the age of 18 and could read and write in English or French. Additional inclusion criteria included: having all referral data (including dates for primary care referral, surgical consult, surgical booking, and the surgical procedure) and had postoperatively completed 12-month patient-report outcomes surveys. Patients were excluded from the study if they were identified as having had a revision surgery, an active workers-compensation claim, involved in legal action or required urgent/emergency surgery such as cauda equina syndrome. Demographic, clinical, and outcome data was prospectively collected from all enrolled patients.
Wait Time Variables
The CSORN Database collects dates for initial referral, first spinal surgeon consultation, surgical booking, and the surgery itself. CWT was defined as the date from initial referral to the date of surgery. Each participant’s CWT was calculated in weeks and a dichotomous variable was defined by whether the CWT was less or greater than the 3-, 6-, or 12 months benchmark. This wait time was selected given that patient outcomes and associated health care costs have been shown to be equivalent between DLC and hip or knee replacements, which have an established benchmark target time of 6 months by CIHI and Ontario Health.16,17
Wait 1 was defined as the difference between the date of referral from a primary care provider to the date of first clinical assessment by a spinal surgeon. Wait 2 is the difference between the date of surgical booking to the date of the procedure.
Primary Outcome Variable
The Oswestry Disability Index (ODI) is a validated, reliable PRO measure developed for use among people with DLCs. 18 This score is a self-administered questionnaire that is commonly used to assess the limitations of various activities of daily living for patients with lumbar pathology. Each item is scored between 0 and 5, with higher scores representing increased disability. The summed score is then converted to a value out of 100.
The minimally clinically important difference (MCID) is a concept that evaluates the change required in the PRO’s values for the patient to be likely to report a meaningful change, not just a statistical one, in their quality of life. The MCID of the ODI for lumbar pathology has been found to be a change of 12.8 points based on the total score. 19 The primary outcome of this study was defined as whether the patient achieved the MCID based on the change in their reported ODI values between preoperative baseline and 12-month post-operative follow-up. Prior work has identified that 12 months is a sufficient follow up time to measure meaningful change from surgical management in lumbar spine surgery. 20
Patient Reported Outcomes (PROs)
Additional PROs were also collected at baseline, including the Numeric Rating Scale (NRS) for back and leg pain which measures participant’s self-reported average pain on a scale that ranges between 0 and 10. 21 The SF-12 physical component scores (PCS) were used to assess patients’ general physical health; each domain’s scores ranged between 0 and 100, with higher scores indicating better function and a total domain score was used. 22 Finally, the Patient Health Questionnaire-8 (PHQ-8) is an eight-item instrument used to measure symptoms of depression that the patient has had in the past 2 weeks. The instrument’s items measure the frequency of depressive symptoms, ranging from 0 (not at all) to 3 (nearly every day) where lower values correspond with fewer symptoms.23,24
Variable Selection
A multivariable model was constructed with covariates and potential confounders identified from prior subject knowledge from the literature.25–33 The variables included were age, sex, BMI, comorbidity count, lumbar degenerative diagnosis, smoking status (smoker or non-smoker), education level (post-secondary education vs high school or less education), surgical procedure type (fusion and decompression vs decompression alone), number of levels operated on, and baseline PROs (including baseline NRS back and leg pain, baseline ODI score, PHQ-8 and SF-12 PCS).
Statistical Analyses
Patients’ demographics, clinical, and PRO’s data were summarized and stratified by the 3-, 6-and 12-month CWT benchmark. Differences were evaluated using t-tests for continuous variables and chi-square tests for categorical variables. Statistical significance was evaluated at 5 percent level of significance.
A multivariable logistic regression model was constructed to determine whether the probability of achieving the MCID for the ODI was associated with the CWT benchmark of 3, 6 and 12 months individually. The model was adjusted for clinical, demographic, and baseline PRO data as defined above as well as an indicator variable for geographic location by province, and no selection process was utilized as all variables were deemed important for inclusion in the model. Missing data was addressed using multiple imputations by chained equations (MICE) 34 and 10 imputations were used. Pooled standard errors for the outcome and covariates included in the final model were calculated using Rubin’s rule for multiple imputations. Model fit was assessed using the area under the receiver operating curve (AUC) and by visually inspecting residual plots. All statistical analyses were performed using SAS v9.4. 35
To further investigate the association between different wait time definitions and achieving the MCID for ODI, sensitivity analyses using the same multivariable logistic regression models was performed to evaluate 3-, 6-, and 12-months benchmarks for Wait 1, and Wait 2 times.
Results
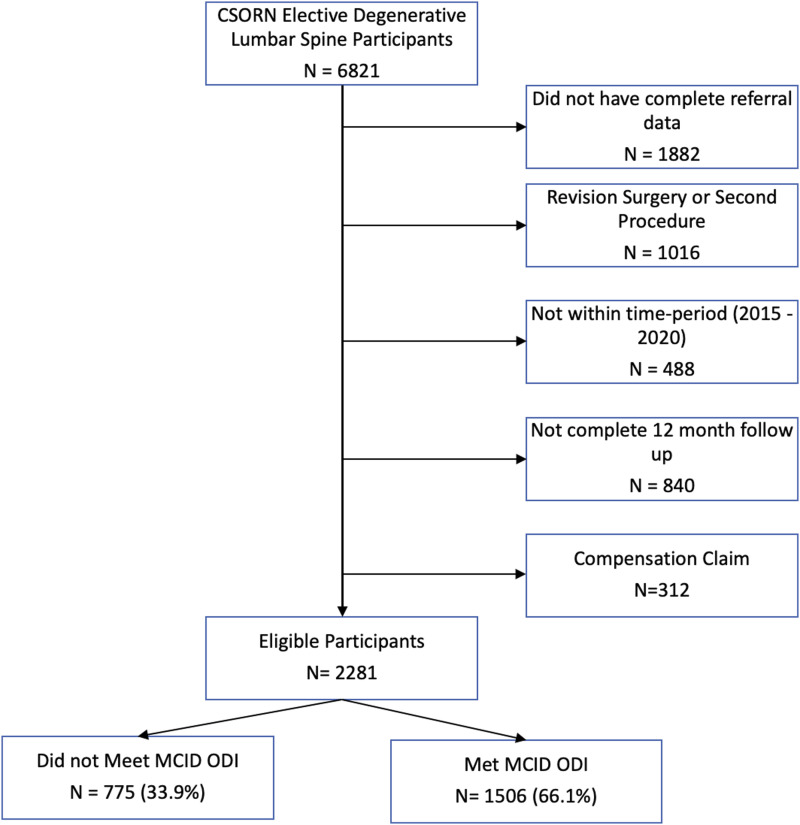
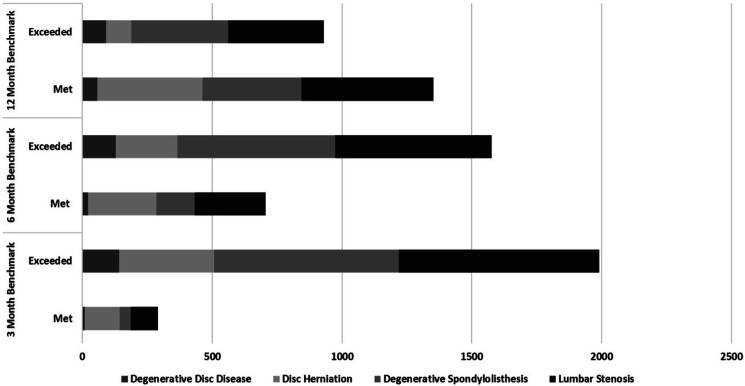
A total of 2281 patients were identified as having DLCs that were managed surgically and were eligible for inclusion in the study (See Figure 1). The average age of participants was 59.4 years (SD 14.8) and 1150 (50.4%) were female. The most common diagnosis was lumbar spinal stenosis (38.4%), followed by degenerative spondylolisthesis (33.1%), disc herniation (22.0%) and degenerative disc disease (3.3%), Figure 2 shows the breakdown of diagnosis based on 3-, 6-, and 12-month CWT benchmarks. The median CWT was 43.1 weeks (IQR 21.8, 76.8), Wait 1 was 14.1 weeks (IQR 5.6, 33.6), and Wait 2 was 14.0 weeks (IQR 6.3, 24.2). There was missing covariate data for 206 (9.0%) patients. (See Table 1 for details) At the 3-month CWT only 12.7% of patients met the benchmark wait time, at 6-months this increased to 30.9%, and finally at 12-months 59.2% achieved the target time.
Figure 1.
Flow diagram inclusion of patients for inclusion in study.
Figure 2.
Lumbar Degenerative diagnosis stratified by 3-, 6-, and 12 month CWT benchmark and whether or not the target wait time was met or exceeded.
Table 1.
Demographic and Clinical Data Stratified by 6 months Benchmark Cumulative Wait Time Dichotomization (3-, 6-, and 12 months).
| Overall | ≤3 months | >3 months | P-value | ≤6 months | >6 months | P-value | ≤12 months | >12 months | P-value | |
|---|---|---|---|---|---|---|---|---|---|---|
| N | 2281 | 290 | 1991 | 706 | 1575 | 1351 | 930 | |||
| Age (SD) | 59.4 (14.8) | 56.1 (16.4) | 59.9 (14.5) | <0.001 | 57.6 (15.9) | 60.2 (14.1) | <0.001 | 58.9 (15.4) | 60.3 (13.7) | 0.019 |
| Female (%) | 1150 (50.4) | 135 (46.5) | 1014 (50.9) | 0.163 | 337 (47.7) | 812 (51.6) | 0.092 | 659 (48.7) | 490 (52.7) | <0.001 |
| BMI (SD) | 28.9 (5.8) | 28.4 (5.9) | 29.0 (5.7) | 0.124 | 28.7 (5.7) | 29.0 (5.8) | 0.115 | 28.8 (5.6) | 29.1 (5.9) | 0.223 |
| Comorbidities (SD) | 2.8 (1.8) | 2.4 (1.7) | 2.9 (1.8) | <0.001 | 2.5 (1.8) | 2.9 (1.8) | <0.001 | 2.6 (1.8) | 3.0 (1.8) | <0.001 |
| Smokers (%) | 268 (11.8) | 36 (12.5) | 232 (11.2) | 0.694 | 88 (12.6) | 180 (11.5) | 0.462 | 156 (11.6) | 112 (12.1) | 0.745 |
| Post-secondary education (%) | 1359 (61.1) | 180 (62.9) | 1178 (60.8) | 0.485 | 436 (63.4) | 922 (60.0) | 0.120 | 836 (63.3) | 522 (57.7) | 0.065 |
| Decompression alone (%) | 993 (43.5) | 134 (46.2) | 859 (43.1) | <0.001 | 366 (51.8) | 627 (39.8) | <0.001 | 634 (46.9) | 359 (38.6) | <0.001 |
| Number of levels (SD) | 1.3 (0.6) | 1.2 (0.5) | 1.4 (0.6) | <0.001 | 1.3 (0.6) | 1.4 (0.6) | 0.006 | 1.3 (0.6) | 1.4 (0.6) | 0.002 |
| Diagnosis (%) | <0.001 | <0.001 | <0.001 | |||||||
| Disc herniation | 502 (22.0) | 136 (46.9) | 366 (18.4) | 265 (37.5) | 237 (15.0) | 404 (29.9) | 98 (10.5) | |||
| Spondylolisthesis | 755 (33.1) | 43 (14.8) | 712 (35.7) | 146 (20.7) | 609 (38.7) | 382 (28.3) | 373 (40.1) | |||
| Degenerative disc disease | 149 (6.5) | 8 (2.7) | 141 (7.1) | 21 (3.0) | 128 (8.1) | 58 (4.3) | 91 (9.8) | |||
| Spinal stenosis | 875 (38.4) | 103 (35.5) | 772 (38.7) | 274 (38.8) | 601 (38.1) | 507 (37.5) | 368 (39.5) | |||
| Median wait times in weeks (IQR) | ||||||||||
| Wait 1 | 14.1 (5.6, 33.5) | 2.4 (1.0, 4.4) | 17.3 (8.3, 39.4) | <0.001 | 5.0 (2.0, 9.8) | 23.3 (11.1, 48.8)) | <0.001 | 8.4 (3.7, 15.4) | 41.6 (18.3, 71.0) | <0.001 |
| Wait 2 | 14.0 (6.2, 24.3) | 3.7 (1.9, 5.3) | 16.4 (8.7, 26.3) | <0.001 | 5.8 (3.1, 9.5) | 19.4 (11.5, 30.0) | <0.001 | 9.4 (4.7, 17.8) | 21.8 (12.7, 36.1) | <0.001 |
| Cumulative wait time | 43.1 (21.8, 76.8) | 7.8 (4.8, 10.0) | 49.4 (28.5, 84.0) | <0.001 | 14.7 (8.7, 20.3) | 60.1 (41.3, 95.0) | <0.001 | 25.1 (14.1, 37.4) | 86.8 (66.7, 122.1) | <0.001 |
| Province | <0.001 | <0.001 | <0.001 | |||||||
| Newfoundland | 35 (1.5) | 5 (1.7) | 30 (1.5) | 6 (0.8) | 29 (1.9) | 24 (1.8) | 11 (1.2) | |||
| Nova Scotia | 18 (0.8) | 1 (0.3) | 17 (0.8) | 5 (0.7) | 13 (0.8) | 10 (0.7) | 8 (0.86) | |||
| New Brunswick | 327 (14.3) | 30 (10.3) | 297 (14.9) | 80 (11.3) | 247 (15.9) | 202 (14.9) | 125 (13.4) | |||
| Quebec | 254 (11.1) | 64 (22.1) | 190 (9.5) | 137 (19.4) | 99 (6.4) | 195 (14.4) | 59 (6.3) | |||
| Ontario | 263 (11.5) | 40 (13.8) | 223 (11.2) | 102 (14.5) | 161 (10.3) | 169 (12.5) | 94 (10.1) | |||
| Manitoba | 332 (14.6) | 73 (25.2) | 259 (13.0) | 135 (19.2) | 197 (12.6) | 229 (16.9) | 1.3 (11.0) | |||
| Alberta | 861 (37.7) | 69 (23.8) | 792 (39.8) | 201 (28.5) | 660 (42.3) | 429 (31.7) | 432 (46.4) | |||
| British Columbia | 191 (8.3) | 8 (2.7) | 183 (9.1) | 39 (5.5) | 152 (9.8) | 93 (6.9) | 98 (10.5 | |||
| Baseline patient reported outcomes (SD) | ||||||||||
| NRS back pain | 6.7 (2.4) | 6.6 (2.8) | 6.7 (2.3) | 0.585 | 6.6 (2.6) | 6.7 (2.3) | 0.765 | 6.6 (2.5) | 6.7 (2.3) | 0.399 |
| NRS leg pain | 7.2 (2.2) | 7.5 (2.1) | 7.1 (2.2) | 0.006 | 7.5 (2.1) | 7.1 (2.3) | <0.001 | 7.3 (2.2) | 7.0 (2.3) | 0.003 |
| SF12 - physical component score | 29.4 (8.0) | 28.2 (7.9) | 29.5 (8.0) | 0.008 | 28.7 (7.5) | 29.6 (8.1) | 0.020 | 29.1 (7.7) | 29.6 (8.5) | 0.128 |
| PHQ-9 score | 9.1 (6.1) | 9.7 (6.3) | 9.0 (6.0) | 0.073 | 9.7 (6.3) | 8.8 (5.9) | 0.001 | 9.2 (6.1) | 8.9 (5.9) | 0.165 |
| Baseline ODI score (SD) | 45.0 (15.3) | 51.8 (17.1) | 44.0 (14.7) | <0.001 | 48.6 (15.9) | 43.4 (14.7) | <0.001 | 46.0 (15.7) | 43.6 (14.6) | <0.001 |
Bold text indicates statistical significance.
There was a significant improvement in all participant’s average ODI score between baseline and 12-month postoperative follow-up (preoperative mean: 45.0, and postoperative mean: 23.9, P < 0.001). The average 12-month post-operative scores for ODI were lower (or better functional outcomes) for those who achieved benchmark wait times at 3- and 6-months compared to those who exceeded the benchmark time, however this was not significant at the 12-month CWT. Overall, at 12 months post-operatively 1506 (66.1%) of patients reached the MCID for change in ODI score from baseline. The proportion of patients who achieved the MCID for ODI was greater than those who did not at the 3-, 6-, and 12- month CWT benchmark was 79.6%, 74.9%, and 68.6% respectively (P < 0.001). (See Table 2 for details).
Table 2.
ODI Scores at Baseline, 12-Month Follow-Up, ODI Change, and Number Who Reached 12-Month Post-operative MCID at 3, 6, and 12 months for CWT Benchmark.
| 3 Month Benchmark | 6 Month Benchmark | 12 Month Benchmark | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ≤3 months | >3 months | P-value | ≤6 months | >6 months | P-value | ≤12 months | >12 months | P-value | |
| N | 290 | 1991 | 706 | 1575 | 1351 | 930 | |||
| Baseline ODI (SD) | 51.8 (17.1) | 44.0 (14.7) | <0.001 | 48.6 (15.9) | 43.4 (14.7) | <0.001 | 46.0 (15.7) | 43.6 (14.6) | <0.001 |
| 12-month ODI (SD) | 20.5 (17.7) | 24.3 (19.0) | 0.001 | 22.0 (18.5) | 24.6 (19.0) | 0.002 | 23.3 (18.8) | 24.6 (19.0) | 0.096 |
| ODI change (SD) | −31.0 (21.2) | −19.6 (18.4) | <0.001 | −26.5 (20.9) | −18.6 (17.8) | <0.001 | −22.6 (20.0) | −18.9 (17.7) | <0.001 |
| Reached MCID (%) | 231 (79.6) | 1275 (64.4) | <0.001 | 529 (74.9) | 977 (62.0) | <0.001 | 927 (68.6) | 579 (62.2) | 0.002 |
Bold text indicates statistical significance.
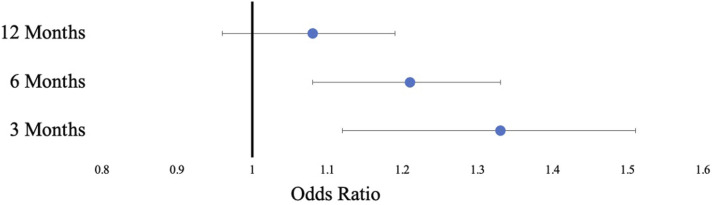
From multivariable logistic regression after adjusting for clinical, demographic and baseline PROs differences between groups, the patients who had a CWT less than or equal to 6 months had 1.26 times the odds of achieving the MCID for post-operative ODI score (95% CI 1.13 - 1.42, P < 0.001). The model had an average AUC of 0.697. Further analysis demonstrated that using a 3-month CWT had greater odds of achieving the MCID for ODI (OR 1.33, 95% CI 1.13 – 1.57, P < 0.001, AUC = 0.692). The relationship at the 12-month CWT did not achieve statistical significance (OR 1.10, 95% CI 0.99 – 1.22, P = 0.053, AUC = 0.695). (See Figure 3 and Table 3 for full model results).
Figure 3.
Odds ratios for achieving the minimally clinical important difference (MCID) for post-operative ODI at 12 months for CWT at 3, 6, and 12 month benchmarks on multivariable logistic regression.
Table 3.
Full Multivariable Logistic Regression Model for Meeting the Minimally Clinically Important Difference of the One-Year Post-operative ODI at the 3-, 6-, and 12-Month Benchmark for CWT.
| 3 Month Benchmark | 6 Month Benchmark | 12 Month Benchmark | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | Confidence interval | P-value | OR | Confidence interval | P-value | OR | Confidence interval | P-value | |
| Intercept | 0.80 | 0.28 – 2.29 | 0.672 | 0.70 | 0.25 – 2.00 | 0.508 | 0.62 | 0.22 – 1.75 | 0.362 |
| Achieving MCID | 1.33 | 1.13 – 1.57 | <0.001 | 1.26 | 1.13 - 1.42 | <0.001 | 1.10 | 0.99 – 1.22 | 0.053 |
| Not achieving MCID | Ref | Ref | Ref | ||||||
| Age | 0.98 | 0.98 – 0.99 | <0.001 | 0.99 | 0.98 – 0.99 | <0.001 | 0.98 | 0.98 – 0.99 | <0.001 |
| BMI | 1.00 | 0.98 – 1.01 | 0.565 | 1.00 | 0.98 - 1.01 | 0.584 | 1.00 | 0.98 – 1.01 | 0.570 |
| Comorbidities | 0.87 | 0.82 – 0.91 | <0.001 | 0.87 | 0.82 – 0.92 | <0.001 | 0.87 | 0.82 – 0.92 | <0.001 |
| Number of levels | 0.89 | 0.77 – 1.05 | 0.164 | 0.89 | 0.76 – 1.04 | 0.140 | 0.89 | 0.76 – 1.04 | 0.131 |
| Female | 0.90 | 0.81 – 0.99 | 0.030 | 0.90 | 0.81 – 0.99 | 0.029 | 0.89 | 0.81 – 0.99 | 0.025 |
| Male | Ref | Ref | Ref | ||||||
| Diagnosis | |||||||||
| Disc herniation | 0.90 | 0.72 – 1.12 | 0.353 | 0.88 | 0.71 – 1.10 | 0.272 | 0.92 | 0.74 – 1.15 | 0.473 |
| Spondylolisthesis | 1.15 | 0.95 – 1.38 | 0.145 | 1.15 | 0.95 – 1.38 | 0.143 | 1.12 | 0.98 – 1.34 | 0.231 |
| Degenerative disc disease | 1.13 | 0.83 – 1.52 | 0.442 | 1.15 | 0.85 – 1.56 | 0.364 | 1.13 | 0.83 – 1.53 | 0.439 |
| Spinal stenosis | Ref | Ref | Ref | ||||||
| Non smoker | 1.18 | 1.01 – 1.36 | 0.031 | 1.17 | 1.01 - 1.34 | 0.034 | 1.18 | 1.02 – 1.37 | 0.026 |
| Smoker | Ref | Ref | Ref | ||||||
| Post-secondary education | 1.10 | 1.00 – 1.22 | 0.049 | 1.10 | 0.99 - 1.21 | 0.063 | 1.10 | 0.99 – 1.21 | 0.065 |
| High school only | Ref | Ref | Ref | ||||||
| Decompression alone | 1.04 | 0.94 – 1.17 | 0.435 | 1.03 | 0.92 – 1.14 | 0.656 | 1.03 | 0.93 – 1.15 | 0.543 |
| Fusion | Ref | Ref | Ref | ||||||
| Baseline PRO scores | |||||||||
| ODI | 1.05 | 1.04 – 1.06 | <0.001 | 1.05 | 1.04 – 1.06 | <0.001 | 1.05 | 1.04 – 1.06 | <0.001 |
| NRS leg pain | 1.05 | 1.01 – 1.11 | 0.030 | 1.05 | 1.00 - 1.10 | 0.042 | 1.05 | 1.00 – 1.10 | 0.033 |
| NRS back pain | 0.97 | 0.93 – 1.02 | 0.285 | 0.97 | 0.93 – 1.02 | 0.272 | 0.97 | 0.93 – 1.02 | 0.233 |
| SF-12 PCS | 1.02 | 1.00 – 1.03 | 0.021 | 1.02 | 1.00 - 1.03 | 0.018 | 1.02 | 1.00 – 1.03 | 0.019 |
| PHQ-9 | 0.98 | 0.96 – 1.00 | 0.039 | 0.98 | 0.96 – 1.00 | 0.025 | 0.98 | 0.96 – 1.00 | 0.022 |
| Province | |||||||||
| Newfoundland | 0.98 | 0.49 – 1.95 | 0.954 | 1.03 | 0.52 – 2.04 | 0.938 | 0.96 | 0.48 – 1.90 | 0.903 |
| Nova Scotia | 1.56 | 0.59 – 4.14 | 0.368 | 1.52 | 0.57 – 4.05 | 0.400 | 1.58 | 0.59 – 4.21 | 0.358 |
| New Brunswick | 1.04 | 0.78 – 1.38 | 0.797 | 1.05 | 0.79 – 1.40 | 0.724 | 1.01 | 0.76 – 1.34 | 0.945 |
| Quebec | 0.97 | 0.71 – 1.34 | 0.867 | 0.92 | 0.67 – 1.27 | 0.622 | 0.99 | 0.72 – 1.37 | 0.974 |
| British Columbia | 1.09 | 0.78 – 1.53 | 0.605 | 1.11 | 0.79 – 1.56 | 0.533 | 1.09 | 0.77 – 1.53 | 0.632 |
| Manitoba | 0.56 | 0.42 – 0.74 | <0.001 | 0.56 | 0.42 – 0.74 | <0.001 | 0.57 | 0.43 – 0.76 | <0.001 |
| Alberta | 1.14 | 0.90 – 1.43 | 0.270 | 1.15 | 0.92 – 1.45 | 0.223 | 1.14 | 0.90 – 1.43 | 0.280 |
| Ontario | Ref | Ref | Ref | ||||||
Bold text indicates statistical significance.
Sensitivity analysis using Wait 1 and Wait 2 times instead of CWT demonstrated that patients treated within the shorter benchmark time were more likely to achieve the MCID for ODI. However, this relationship was not statistically significant using Wait 1 time at the 6-month and 12-month benchmark time. (See Appendix 1)
Discussion
This study found that patients who were surgically treated within 3 or 6 months of referral from their primary care provider for DLC were more likely to experience clinically meaningful improvement in their function post-operatively. Thus, patients who suffer from DLC and who are surgical candidates, are more likely to have clinically important improvements with earlier surgical management. Results from this study also further emphasized the long wait times for DLC in Canada, a single payer health care system. Overall, only 12.7% and 30.9% of patients were meeting the 3- and 6-month CWT benchmark for surgical management respectively.
This paper demonstrates that the average CWT for elective lumbar degenerative surgery, with a median of 43.1 weeks, is much higher than the ideal 6-month benchmark for other orthopaedic conditions established in Canada. In 2004, the National Health Services in the United Kingdom recognized that reporting only Wait 2 times was insufficient and introduced the concept of referral-to-treatment (RTT) which was the time from primary care referral to treatment by specialists in hospital. 36 The CWT that was constructed in this paper is the same value as the RTT and is used to define a more comprehensive evaluation of the patient experience waiting for elective lumbar degenerative surgery.
Prior elective lumbar spine surgery literature has demonstrated conflicting findings with whether longer wait times negatively influenced functional outcomes, quality of life, and recovery during the first year after surgery.37,38 There are few studies that evaluate the association between wait times and outcomes; several Canadian studies have demonstrated that those with longer wait times were less likely to be satisfied, had delays in recovery during first year after surgery and had worse post-operative outcomes.9,10 However, these studies were limited to single centres with small sample sizes and only considered the differences in absolute values in patient scores without evaluating the clinical significance of these changes with the MCID. Similar research using the CSORN database found that patients with spinal stenosis who had symptoms for greater than 1-year were less likely to achieve the MCID and more likely to experience equivalent or worse disability post-operatively. 29 A recent study by Rampersaud et al., (2024) sought to evaluate the effect of wait times on surgical outcomes in lumbar spinal stenosis specifically, and found that by using MCID values for the ODI, longer wait times were less likely to achieve a clinically meaningful difference. 39 This study provides further evidence to the literature that there are more likely to be clinically meaningful gains for patients who receive timely access to spine surgical care for elective DLC.
Interestingly, at all benchmark time points the baseline ODI scores were higher in the groups who met the benchmark suggesting that patients who had more severe symptoms had been treated earlier. Further, patients who were treated within benchmark times, using the CWT, had greater change in ODI score, better average post operative ODI scores, and were more likely to reach the MCID for ODI at 12 months suggesting greater improvements in disability and function if treated earlier. Although these cases were all categorized as elective procedures, surgeons likely will place priority for patients who have more significant pain and disability based on clinical reviews and a combination of physical examination and imaging findings. 40 In the context of spine surgery, worsening severity of symptoms can often lead to significant deterioration of function and result in emergency interventions. A recent review by Dandurand et al, 41 (2023) noted that patients requiring urgent surgery for DLC have worse perioperative outcomes compared to those with elective surgery. Other possible reasons for these findings are that as patients wait for care they have increasing pain and reductions in mobility making them less likely to engage in exercise or physical therapy both prior to and after surgical management. This lack of engagement in appropriate rehabilitation before and after surgery has been shown to be detrimental to post-operative outcomes. 42 Also patients waiting for longer periods of time prior to treatment experience worsening mental health, including anxiety and depression, which can greatly impact satisfaction with surgery and post-operative outcomes.15,25,43 Clearly, as patients wait for elective surgical treatments they have significant declines in function, from both a physical and mental perspective and need to be monitored closely for worsening. It is thus important to consider the whole waiting period from initial referral to surgical management when evaluating post-operative outcomes and thus it is the CWT that is more representative of the true wait and patient experience. By decreasing the time from referral to surgical management it can reduce further burden on patients and health care systems by improving outcomes, and decreasing the need for urgent surgical management.
Lumbar pain due to degenerative conditions is one of the top reasons patients present for treatment and evaluation by orthopaedic and neurosurgical specialists but long wait times often represent a significant barrier to care.44,45 It is estimated that in the Canadian province of Ontario the costs of non-trauma related spinal care has exceeded US$170 million per year and responsible for 890 000 primary care visits. 46 This paper adds further evidence that if patients access surgical care within 3 or 6 months there is up to a 30% increase in the odds that they will achieve clinically significant improvements in their symptoms compared to those who wait longer for treatment. Given the significant burden of DLCs and improvements made by timely access to care, public health systems should prioritize standardized measuring, defining, and meeting targets for surgical management. There have been a number of strategies have been studied that have helped to reduce wait times for consultation and surgical management including multi-disciplinary teams, advanced practice clinicians, and the use of centralized referral systems.47–49 In Ontario, a large triage service has been established for low back pain and need for spine surgery and has been a tremendously successful program, reducing wait times, unnecessary imaging investigations, and streamlining the process from initial referral to surgical management. 50 In Saskatchewan, the advent of a multidisciplinary program for low back pain has achieved similar goals and improved patient satisfaction and outcomes.47,51 These programs have not been adopted or standardized in most jurisdictions where spinal care is provided but should be considered by governments and policy makers given the significant burden caused by degenerative lumbar spinal pathology on patients and the health care systems.
Strengths and Limitations
This study includes data from the largest multi-centre Canadian sample of patients who have received surgical management for DLC with a robust sample size. The sample likely represents a diverse collection of patient experiences from a number of different clinical practices and settings throughout Canada, increasing the generalizability of the results. However, there are limitations to this study. First, the CSORN dataset represents mostly academic centres and may not reflect the wait times of community spinal specialists. Second, many Canadians do not have timely access to a family physician so the wait times prior to seeing a primary care provider may be considerable and were not evaluated in this study. 52 This has the potential to introduce lead-time bias, where great variations in time to presentation to primary care can influence the effectiveness of the surgical treatment and influence results. Previous CSORN work has looked at self-reported symptom duration, and found that it influences outcomes, however this study did not utilize this information due to limitations with recall bias. 28 Third, this study found that baseline ODI scores were higher among those who met the benchmark at all times points, likely representing the fact that surgeons treated patient with more severe symptoms earlier. This suggests confounding by indication; however baseline ODI score was controlled for in all regression models. Finally, CSORN does not collect PROs during the waiting period so there is a paucity of information on the change in PROs prior to surgical management, this could have potential implications on how symptom severity alters during the waiting period and influence post-operative results. Future research should focus on obtaining additional data throughout the waiting experience to evaluate the change in patients’ condition over time and determine its relationship with post-operative outcomes.
Conclusion
This study found that among Canadian patients waiting for elective lumbar degenerative surgical management, timely access to care and treatment is associated with improved post-operative outcomes. There is a pressing need for the consideration of policy interventions that are targeted at reducing wait times for DLC given its prevalence in the population and costliness to taxpayers in a public health system. Future research should focus on evaluating the efficacy of standardized methods to reduce wait times for surgical care including centralized wait lists, and triage clinics. Additionally, research should evaluate the role that PROs can play in providing a way to monitor patient symptoms during the pre-operative period and whether these can be used in the triaging process. This research is essential to ascertain the most effective approaches for expediting referrals and reducing wait times, ultimately improving the quality of life for patients enduring pain and disability due to lumbar degenerative disease.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Michael Bond https://orcid.org/0000-0001-9923-3573
Raphaële Charest-Morin https://orcid.org/0000-0002-7689-1087
Jerome Paquet https://orcid.org/0000-0003-1390-2428
Appendix 1.
ODI scores at baseline, 12-month follow-Up, ODI change, and number Who reached MCID along and Adjusted OR for meeting MCID at 3, 6, and 12 months for Wait 1, and Wait 2.
| 3 months wait | 6 months wait | 12 months wait | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ≤3 months | >3 months | P-value | ≤6 months | >6 months | P-value | ≤12 months | >12 months | P-value | |
| Wait 2 time | |||||||||
| N | 1066 | 1215 | 1774 | 507 | 2178 | 103 | |||
| Baseline ODI (SD) | 46.9 (15.9) | 43.4 (14.5) | <0.001 | 45.2 (15.4) | 44.4 (14.8) | 0.295 | 45.0 (15.3) | 45.4 (14.6) | 0.920 |
| 12 month ODI (SD) | 22.8 (18.4) | 24.7 (19.3) | 0.016 | 22.9 (18.6) | 27.1 (19.6) | <0.001 | 23.6 (18.8) | 29.3 (20.5) | 0.002 |
| ODI change (SD) | −24.0 (20.0) | −18.5 (18.0) | <0.001 | −22.2 (19.6) | −17.1 (17.1) | <0.001 | −21.3 (19.2) | −15.5 (17.1) | 0.003 |
| Reached MCID (%) | 763 (71.6) | 743 (61.1) | <0.001 | 1206 (68.0) | 300 (59.0) | <0.001 | 1452 (66.7) | 54 (51.9) | 0.002 |
| Adjusted OR (CI) | 1.20 (1.08 – 1.32) | Ref | <0.001 | 1.14 (1.02 – 1.28) | Ref | 0.022 | 1.28 (1.03 – 1.58) | Ref | 0.026 |
| Wait 1 time | |||||||||
| N | 1063 | 1218 | 1562 | 719 | 1911 | 370 | |||
| Baseline ODI (SD) | 46.3 (16.0) | 43.9 (14.6) | <0.001 | 45.9 (15.5) | 43.1 (14.8) | <0.001 | 45.4 (15.5) | 43.3 (14.5) | 0.020 |
| 12 month ODI (SD) | 22.8 (18.7) | 24.7 (19.0) | 0.016 | 23.7 (18.8) | 24.2 (19.0) | 0.558 | 23.7 (18.9) | 24.7 (19.0) | 0.317 |
| ODI change (SD) | −23.3 (20.11) | −19.1 (18.1) | <0.001 | −22.1 (19.8) | −18.9 (17.3) | <0.001 | −21.6 (19.5) | −18.6 (16.7) | 0.006 |
| Reached MCID (%) | 742 (69.8) | 764 (62.7) | <0.001 | 1054 (67.5) | 452 (62.8) | 0.028 | 1282 (67.1) | 224 (60.4) | 0.013 |
| Adjusted OR (CI) | 1.12 (1.01 – 1.23) | Ref | 0.024 | 1.05 (0.95 – 1.17) | Ref | 0.343 | 1.12 (0.99 – 1.27) | Ref | 0.078 |
Bold text indicates statistical significance.
References
- 1.Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028-2037. doi: 10.1002/art.34347 [DOI] [PubMed] [Google Scholar]
- 2.Buchbinder R, van Tulder M, Öberg B, et al. Low back pain: a call for action. Lancet. 2018;391(10137). [DOI] [PubMed] [Google Scholar]
- 3.Eismont FJ, Norton RP, Hirsch BP. Surgical management of lumbar degenerative spondylolisthesis. J Am Acad Orthop Surg. 2014;22(4):203-213. doi: 10.5435/JAAOS-22-04-203 [DOI] [PubMed] [Google Scholar]
- 4.Madigan L, Vaccaro AR, Spector LR, Milam RA. Management of symptomatic lumbar degenerative disk disease. J Am Acad Orthop Surg. 2009;17(2):102-111. doi: 10.5435/00124635-200902000-00006 [DOI] [PubMed] [Google Scholar]
- 5.Issack PS, Cunningham ME, Pumberger M, Hughes AP, Cammisa FP. Degenerative lumbar spinal stenosis: evaluation and management. J Am Acad Orthop Surg. 2012;20(8):527-535. doi: 10.5435/JAAOS-20-08-527 [DOI] [PubMed] [Google Scholar]
- 6.Siciliani L, Moran V, Borowitz M. Measuring and comparing health care waiting times in OECD countries. Health Pol. 2014;118(3):292-303. doi: 10.1016/j.healthpol.2014.08.011 [DOI] [PubMed] [Google Scholar]
- 7.Liddy C, Moroz I, Affleck E, et al. How long are Canadians waiting to access specialty care? Retrospective study from a primary care perspective. Can Fam Physician. 2020;66(6):434-444. [PMC free article] [PubMed] [Google Scholar]
- 8.Quan H, Lafreniere R, Johnson D. Health service costs for patients on the waiting list. Can J Surg. 2002;45(1):34-42. [PMC free article] [PubMed] [Google Scholar]
- 9.Braybrooke J, Ahn H, Gallant A, et al. The impact of surgical wait time on patient-based outcomes in posterior lumbar spinal surgery. Eur Spine J. 2007;16(11):1832-1839. doi: 10.1007/s00586-007-0452-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bailey C, Gurr K, Bailey S, et al. Does the wait for lumbar degenerative spinal stenosis surgery have a detrimental effect on patient outcomes? A prospective observational study. 2016;4(2):E185-E193. doi: 10.9778/cmajo.20150001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Canadian Institute for Health Information . Wait times for priority procedures in Canada. https://www.cihi.ca/en/wait-times-for-priority-procedures-in-canada. Accessed 9 November 2022.
- 12.OECD . Waiting times for health services: next in line. Paris: OECD; 2020. [Google Scholar]
- 13.Glauser W. What about the wait times Canada isn’t tracking? CMAJ (Can Med Assoc J). 2020;192(37):E1081-E1082. doi: 10.1503/CMAJ.1095896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Segall RE, Takata JL, Urbach DR. Wait-time reporting systems for elective surgery in Canada: a content analysis of provincial and territorial initiatives. Canadian Medical Association Open Access Journal. 2020;8(4):E844-E851. doi: 10.9778/CMAJO.20200033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiseman SM, Crump T, Cadesky E, Sutherland JM. Addressing the mental health of Canadians waiting for elective surgery: a potential positive post-pandemic legacy. Can J Surg. 2020;63(5):E393-E394. doi: 10.1503/CJS.014120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rampersaud YR, Tso P, Walker KR, et al. Comparative outcomes and cost-utility following surgical treatment of focal lumbar spinal stenosis compared with osteoarthritis of the hip or knee: Part 2 - estimated lifetime incremental cost-utility ratios. Spine J. 2014;14(2):244-254. doi: 10.1016/j.spinee.2013.11.011 [DOI] [PubMed] [Google Scholar]
- 17.Rampersaud YR, Lewis SJ, Davey JR, Gandhi R, Mahomed NN. Comparative outcomes and cost-utility after surgical treatment of focal lumbar spinal stenosis compared with osteoarthritis of the hip or knee - Part 1: long-term change in health-related quality of life. Spine J. 2014;14(2):234-243. doi: 10.1016/j.spinee.2013.12.010 [DOI] [PubMed] [Google Scholar]
- 18.Fairbank JCT, Pynsent PB. The oswestry disability index. Spine. 2000;25(22):2940-2953. doi: 10.1097/00007632-200011150-00017 [DOI] [PubMed] [Google Scholar]
- 19.Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J. 2008;8(6):968-974. doi: 10.1016/J.SPINEE.2007.11.006 [DOI] [PubMed] [Google Scholar]
- 20.Ayling OGS, Ailon T, McIntosh G, et al. Clinical outcomes research in spine surgery: what are appropriate follow-up times? J Neurosurg Spine. 2019;30(3):397-404. doi: 10.3171/2018.8.SPINE18715 [DOI] [PubMed] [Google Scholar]
- 21.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine. 2005;30(11):1331-1334. doi: 10.1097/01.BRS.0000164099.92112.29 [DOI] [PubMed] [Google Scholar]
- 22.Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220-233. doi: 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1-3):163-173. doi: 10.1016/J.JAD.2008.06.026 [DOI] [PubMed] [Google Scholar]
- 24.Wu Y, Levis B, Riehm KE, et al. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: a systematic review and individual participant data meta-analysis. Psychol Med. 2020;50(8):1368-1380. doi: 10.1017/S0033291719001314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cushnie D, Fisher C, Hall H, et al. Mental health improvements after elective spine surgery: a Canadian Spine Outcome Research Network (CSORN) study. Spine J. 2021;21(8):1332-1339. doi: 10.1016/j.spinee.2021.03.032 [DOI] [PubMed] [Google Scholar]
- 26.Cushnie D, Soroceanu A, Stratton A, et al. Outcome of spine surgery in patients with depressed mental states: a Canadian spine outcome research network study. Spine J. 2022;22(10):1700-1707. doi: 10.1016/J.SPINEE.2022.05.012 [DOI] [PubMed] [Google Scholar]
- 27.Deyo R, Cherkin D, Loeser J, Bigos S, Ciol M. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am 1992;74(4):536-543. https://europepmc.org/article/med/1583048. Accessed 16 October 2021. [PubMed] [Google Scholar]
- 28.Fleming J, Glassman SD, Miller A. et al. The effect of symptom duration on outcomes after fusion for degenerative spondylolisthesis. Global Spine J. 2018;9(5):487-491. doi: 10.1177/2192568218804557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cushnie D, Thomas K, Jacobs WB, et al. Effect of preoperative symptom duration on outcome in lumbar spinal stenosis: a Canadian Spine Outcomes and Research Network registry study. Spine J. 2019;19(9):1470-1477. doi: 10.1016/j.spinee.2019.05.008 [DOI] [PubMed] [Google Scholar]
- 30.Bond M, Evaniew N, Bailey CS, et al. Back pain in surgically treated degenerative lumbar spondylolisthesis: what can we tell our patients? Spine J. 2020;20(12):1940-1947. doi: 10.1016/j.spinee.2020.08.009 [DOI] [PubMed] [Google Scholar]
- 31.Iorio-Morin C, Fisher CG, Abraham E, et al. Low-back pain after lumbar discectomy for disc herniation: what can you tell your patient? J Neurosurg Spine. 2021;35(6):715-721. doi: 10.3171/2021.2.SPINE201625 [DOI] [PubMed] [Google Scholar]
- 32.Rajesh N, Moudgil-Joshi J, Kaliaperumal C. Smoking and degenerative spinal disease: a systematic review. Brain & Spine. 2022;2:100916. doi: 10.1016/J.BAS.2022.100916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MacLean MA, Touchette CJ, Han JH, Christie SD, Pickett GE. Gender differences in the surgical management of lumbar degenerative disease: a scoping review. J Neurosurg Spine. 2020;32(6):799-816. doi: 10.3171/2019.11.SPINE19896 [DOI] [PubMed] [Google Scholar]
- 34.Sterne JAC, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338(7713):157-160. doi: 10.1136/BMJ.B2393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yuan Y. Multiple imputation using SAS software. J Stat Software. 2011;45(6):1-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wood RM. Unravelling the dynamics of referral-to-treatment in the NHS. Health Systems. 2021;10(2):131-137. doi: 10.1080/20476965.2019.1700764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aalto TJ, Malmivaara A, Kovacs F, et al. Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine. 2006;31(18). [DOI] [PubMed] [Google Scholar]
- 38.Athiviraham A, Wali ZA, Yen D. Predictive factors influencing clinical outcome with operative management of lumbar spinal stenosis. Spine J. 2011;11(7):613-617. doi: 10.1016/J.SPINEE.2011.03.008 [DOI] [PubMed] [Google Scholar]
- 39.Jentzsch T, Sundararajan K, Rampersaud YR. The clinical course of symptoms during wait time for lumbar spinal stenosis surgery and its effect on postoperative outcome: a retrospective cohort study. Spine J. 2024;24(4):644-649. doi: 10.1016/J.SPINEE.2023.11.006 [DOI] [PubMed] [Google Scholar]
- 40.Wiebe K, Kelley S, Kirsch RE. Revisiting the concept of urgency in surgical prioritization and addressing backlogs in elective surgery provision. CMAJ (Can Med Assoc J). 2022;194(29):E1037-E1039. doi: 10.1503/CMAJ.220420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dandurand C, Hindi MN, Laghaei PF, et al. Degenerative spinal conditions requiring emergency surgery: an evolving crisis in a publicly funded health care system. Can J Surg. 2023;66(3):E274-E281. doi: 10.1503/CJS.012122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hébert JJ, Abraham E, Wedderkopp N, et al. Preoperative factors predict postoperative trajectories of pain and disability following surgery for degenerative lumbar spinal stenosis. Spine. 2020;45(21):E1421. doi: 10.1097/BRS.0000000000003587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sutherland JM, Crump RT, Chan A, Liu G, Yue E, Bair M. Health of patients on the waiting list: opportunity to improve health in Canada? Health Pol. 2016;120(7):749-757. doi: 10.1016/J.HEALTHPOL.2016.04.017 [DOI] [PubMed] [Google Scholar]
- 44.Mclntosh G, Hall H, Melles T. The incidence of spinal surgery in Canada. Can J Surg. 1998;41(1):59-66. [PMC free article] [PubMed] [Google Scholar]
- 45.Comeau P. Crisis in orthopedic care: surgeon and resource shortage. 2004;171(3):223. doi: 10.1503/cmaj.1041073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rampersaud YR, Power JD, Perruccio Av., et al. Healthcare utilization and costs for spinal conditions in Ontario, Canada - opportunities for funding high-value care: a retrospective cohort study. Spine J. 2020;20(6):874-881. doi: 10.1016/J.SPINEE.2020.01.013 [DOI] [PubMed] [Google Scholar]
- 47.Fourney DR, Dettori JR, Hall H, Härtl R, McGirt MJ, Daubs MD. A systematic review of clinical pathways for lower back pain and introduction of the Saskatchewan spine pathway. Spine. 2011;36(21 SUPPL). [DOI] [PubMed] [Google Scholar]
- 48.Robarts S, Stratford P, Kennedy D, Malcolm B, Finkelstein J. Evaluation of an advanced-practice physiotherapist in triaging patients with lumbar spine pain: surgeon–physiotherapist level of agreement and patient satisfaction. Can J Surg. 2017;60(4):266. doi: 10.1503/CJS.013416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McAlister CN. Centralized referral systems can both shorten wait times and preserve patient autonomy. CMAJ (Can Med Assoc J). 2020;192(24):E659. doi: 10.1503/CMAJ.75698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zarrabian M, Bidos A, Fanti C, et al. Improving spine surgical access, appropriateness and efficiency in metropolitan, urban and rural settings. Can J Surg. 2017;60(5):342-348. doi: 10.1503/cjs.016116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnston G. Saskatchewan’s successful strategy for surgical waitlist reduction. Healthc Q. 2018;21(3):51-56. [DOI] [PubMed] [Google Scholar]
- 52.Kiran T. Keeping the front door open: ensuring access to primary care for all in Canada. CMAJ (Can Med Assoc J). 2022;194(48):E1655-E1656. doi: 10.1503/CMAJ.221563 [DOI] [PMC free article] [PubMed] [Google Scholar]