Abstract
Venous sinus stenting for dural venous sinus outflow obstruction due to an intrinsic filling obstruction or extrinsic stenosis is an increasingly popular treatment strategy for idiopathic intracranial hypertension (IIH) and isolated pulsatile tinnitus (PT). The most common site of stenosis is the lateral venous sinus at the transverse-sigmoid junction. Approximately 10% of the population has a persistent occipital venous sinus (OVS), a variant that may be the dominant venous drainage pathway in the setting of a hypoplastic or aplastic transverse sinus. OVS stenosis has been rarely associated with IIH and isolated PT with only a handful published cases. We herein report a retrospective series of OVS stenting in five patients, four of whom presented with non-IIH PT and one with IIH.
Keywords: Occipital sinus, dural venous sinus stenting, pulsatile tinnitus, idiopathic intracranial hypertension
Introduction
Venous sinus stenting (VSS) for dural venous sinus outflow obstruction due to an intrinsic filling obstruction or extrinsic stenosis is an increasingly popular treatment strategy for idiopathic intracranial hypertension (IIH) and isolated pulsatile tinnitus (PT).1–3 The most common site of stenosis is the lateral venous sinus at the transverse-sigmoid junction (TSJ).2,3 There may also be an associated post-stenotic venous aneurysm amenable to embolization. 3
Approximately 10% of the population has a persistent occipital venous sinus (OVS), a variant that may be the dominant venous drainage pathway in the setting of a hypoplastic or aplastic transverse sinus (TS).4–6 The OVS typically functions as a venous outflow pathway between the confluence of the sinuses, the vertebral venous plexus, and/or the marginal sinus around the foramen magnum. 7
OVS stenosis has been rarely associated with IIH and isolated PT. VSS for OVS stenosis has been sparsely reported in the literature with only a handful published cases.6,8,9 We herein report a retrospective series of OVS stenting in five patients, four of whom presented with non-IIH PT and one with IIH. To our knowledge, this is the largest case series describing OVS stenting reported in the literature.
Methods
The authors retrospectively reviewed the records of five consecutive patients who underwent OVS stenting performed by the senior author (AP) at a single institution between July 2020 and July 2023. A prior approval was obtained from the Institutional Review Board. Preoperative symptoms, prior medical management, dural sinus anatomy, venous manometry, and post-operative outcomes were noted. All patients were evaluated with catheter cerebral venogram and manometry from the superior sagittal sinus (SSS) to the jugular bulb under local anesthesia as previously reported by the senior author. 3 A minimum gradient of at least 4 mm Hg was required for stenting. The aim of VSS is to alleviate the trans-stenosis pressure gradient by increasing the luminal diameter of the affected sinus according to Hagen–Poiseuille's law. 8
Results
Five patients with a stenotic OVS, one that presented with IIH and four with isolated PT, underwent VSS between July 2020 to July 2023 (Table 1). Three patients were female and two were male. Median age at stenting was 45.2 years (range 35 years to 61 years). The patient with IIH presented with debilitating headache but did not present with papilledema on fundoscopy. Lumbar puncture (LP) opening pressure was 35 cmH2O. The patient was prescribed acetazolamide prior to the procedure. Of the four patients with isolated PT, two had unilateral right-sided PT (50%) and two had unilateral left-sided PT (50%). Three out of four (75%) described relief with neck pressure or manipulation.
Table 1.
Patient demographics and symptomatology for all six venous stenting patients with dominant occipital sinuses.
| Case | Age, sex | PT side (R/L) | PT relieved with neck pressure (Y/N) | Papilledema (Y/N) | Venous aneurysm (Y/N) | CSF OP (cm H2O) | OVS side (R/L) |
|---|---|---|---|---|---|---|---|
| Pulsatile tinnitus | |||||||
| 2 a (Figure 2) | 35F | R | Y | N | Y | N/A | R |
| 3 (Figure 3(a) and (b)) | 30F | R | N/A | N | Y | N/A | R |
| 4 (Figure 3(c) and (d)) | 61F | L | Y | N | Y | N/A | L |
| 5 (Figure 3(e) and (f)) | 61M | L | Y | N | Y | N/A | L |
| Idiopathic intracranial hypertension | |||||||
| 1 a (Figure 1) | 39M | None | N/A | N | N | 35 | R |
PT: pulsatile tinnitus; R: right; L: left; Y: yes; N: no; CSF: cerebrospinal fluid; OP: opening pressure; OVS: occipital sinus; F: female; N/A: not available; M: male.
Case 2.
Case 1.
On catheter venography, all patients exhibited a persistent OVS as the dominant venous sinus drainage pathway (Figures 1(a), 2(a), 3(a), (c), (e) and (g)). It is performed under local anesthesia. Out of the four patients with PT, two had a right-sided OVS. All four patients had a hypoplastic (50%) or completely absent (50%) ipsilateral TS. Notably, patient number 4 had bilateral hypoplastic TSs. Moreover, all four isolated PT patients were found to have a post-stenotic venous aneurysm. Intravenous manometry was used to assess the pressure gradient across the OVS stenosis; the median stenotic gradient before stenting was 8 mm Hg (range 7 mm Hg to 11 mm Hg). The IIH patient had a right-sided OVS also had hypoplastic bilateral transverse venous sinuses. The pre-stent stenotic gradient as measured by manometry in this patient was also 8 mm Hg (Table 2).
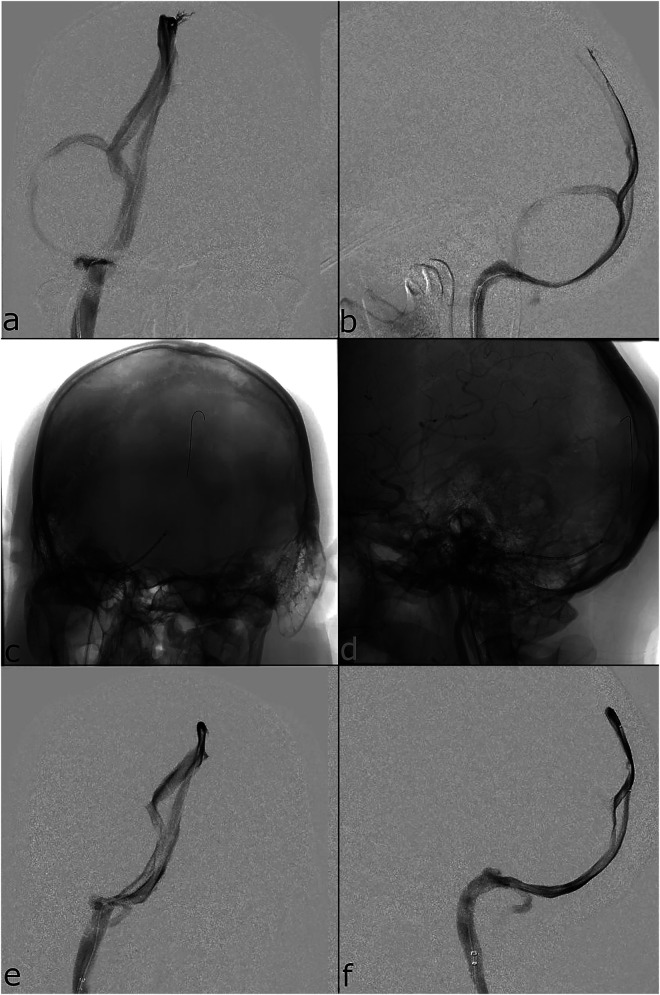
Figure 1.
Catheter cerebral venogram superior sagittal sinus injection (a, b) frontal and lateral views before stenting showing the right-sided dominant occipital sinus and hypoplastic transverse sinus; (c, d) unsubtracted frontal and lateral views showing stent placement; and (e, f) superior sagittal sinus injection frontal and lateral views after stenting showing a larger occipital sinus caliber which drains the entirety of venous outflow into the jugular bulb, without contribution from the transverse sinus as seen previously.
Figure 2.
Catheter cerebral venogram superior sagittal sinus injection (a, b) frontal and lateral views before stenting showing the right-sided dominant occipital sinus, post-stenotic venous aneurysm (white arrow), and hypoplastic transverse sinus; (c, d) unsubtracted frontal and lateral views showing transverse-sigmoid junction stent placement; (e, f) unsubtracted frontal and lateral views occipital sinus stent placement; (g, h) right common carotid artery injection frontal and lateral views after stenting showing larger occipital and lateral sinus calibers.
Figure 3.
(a, c, e) catheter cerebral venogram superior sagittal sinus injection frontal views showing pre-stent dominant stenotic occipital sinuses; post-stent (b and d) cerebral angiogram vertebral artery injections and (f and g) venogram superior sagittal sinus injections showing increased sinus calibers.
Table 2.
Stenosis gradients as measured by venous manometry, stent characteristics, and follow-up data for all six venous stenting patients with dominant occipital sinuses.
| Case | Pre-stent trans-stenotic OVS gradient (mm Hg) | Post-stent trans-stenotic OVS gradient (mm Hg) | OVS stent size | TSJ stent size | Aneurysm coiling (Y/N) | 1-month follow-up symptoms | Last follow-up (months) |
|---|---|---|---|---|---|---|---|
| PT | |||||||
| 2 | 7 | 0 | 7 × 40 mm | 6 × 40 mm (TSS) | N | Complete resolution | Asymptomatic (26) |
| 3 | 8 | 1 | 6 × 40 mm | N/A | Y | Complete resolution | Asymptomatic (9) |
| 4 | 7 | 1 | 6 × 40 mm | 6 × 30 mm (TS) | Y | Complete resolution | Asymptomatic (1) |
| 5 | 11 | 1 | 5 × 40 mm | N/A | N | Complete resolution | Asymptomatic (1) |
| IIH | |||||||
| 1 | 7 | 1 | 6 × 40 mm | N/A | N | Headaches improved | Headaches improved (13) |
PT: pulsatile tinnitus; R: right; L: left; Y: yes; N: no; CSF: cerebrospinal fluid; OP: opening pressure; OVS: occipital sinus; F: female; N/A: not available; M: male; IIH: idiopathic intracranial hypertension; TSJ: transverse-sigmoid junction.
Case 2.
Case 1.
All stents were Precise Pro (Cordis, Hialeah, FL, USA) ranging in size from 5 × 40 mm to 7 × 40 mm. Two patients with TSJ stenosis had additional Precise Pro stents (6 × 30 mm, 6 × 40 mm) placed across the TSJ (Table 2). Two of the four venous aneurysms were coiled (50%). All post-stenting runs showed patent venous sinus outflow (Figures 1(e), 2(g), 3(b), (d), (f) and (g)) without stenosis. The median post-stenting pressure gradient across the previously stenotic segment was 1 mm Hg (range 0 mm Hg to 1 mm Hg).
No patients had any peri-procedural or post-procedural complications. All patients were discharged after a few hours of observation. All patients were continued on dual antiplatelet therapy (asprin 81 mg and Plavix 75 mg) for 1 month postoperatively except one patient who had an allergy to aspirin and was maintained on monotherapy.
At 1-month follow-up, all five patients reported improvement in symptoms, with all four PT patients reporting complete resolution of PT and the IIH patient reporting improvement in headache. At most recent follow-up, all five patients reported improvement of their symptoms (median clinical follow-up 10 months, range 1 month to 26 months).
Case example 1: occipital venous Sinus stenting for idiopathic intracranial hypertension
A 39-year-old male presented with a 3-year history of headaches secondary to IIH, which was diagnosed after LP revealed an opening pressure of 35 cm H2O. Cerebral angiogram was performed at an outside institution at the time of diagnosis which showed stenosis of the right TS and a persistent OVS. The patient experienced medication intolerance to both acetazolamide and topiramate, and eventually presented to our institution for further evaluation and potential VSS. Repeat computed tomography venography and magnetic resonance imaging were obtained which showed bilateral transverse venous sinuses stenosis without thrombosis. Fundoscopic exam was negative for papilledema.
The patient was premedicated with aspirin 81 mg and clopidogrel 75 mg for 5 days. Cerebral venogram was performed which showed an aplastic left tranverse venous sinus, hypoplastic right TS, and venous outflow from the SSS to a dominant right OVS and jugular bulb (Figure 1(a) and (b)). There was moderate appearing stenosis at the distal aspect of the OVS. Venous manometry was performed showing a trans-stenotic gradient of 7 mm Hg between the torcula and right jugular bulb and trans-stenotic gradient of 5 mm Hg between the right transverse and sigmoid venous sinuses (Table 3a). After discussion at follow-up, the patient wished to move forward with VSS.
Table 3.
Case 1 pre- and post-stenting venous sinus pressure measurements.
| Manometry pre-stenting | Pressure (mm Hg) |
|---|---|
| Superior sagittal sinus | 15 |
| Right proximal transverse sinus | 14 |
| Right distal transverse sinus | 14 |
| Right proximal sigmoid sinus | 9 |
| Right distal sigmoid sinus | 9 |
| Right jugular bulb | 8 |
| Manometry post-stenting | |
| Superior sagittal sinus | 23 |
| Right proximal occipital sinus (pre-stent) | 23 |
| In-stent occipital sinus | 23 |
| Distal occipital sinus (post-stent) | 22 |
Under general anesthesia, cerebral angiogram was first performed via right radial puncture which showed no concomitant arterial pathology. The right common femoral vein was accessed. A Ballast guide catheter (Balt, Montmorency, France) was advanced into the right internal jugular vein. A Headway 27 microcatheter (MicroVention, Aliso Viejo, CA, USA) was then advanced over a Synchro 2 microwire (Stryker, Kalamazoo, MI, USA) into the SSS. An Esperance 071 intermediate catheter (Wallaby Medical, Laguna Hills, CA, USA) was advanced over a Synchro 2 microwire and the Headway 27 into the proximal OVS. The Synchro 2 microwire was exchanged for a balanced heavy weight 0.014” microwire positioned into the SSS, and a Precise Pro 6 × 40 mm stent (Cordis, Hialeah, FL, USA) was advanced into the right OVS and deployed without complications (Figure 1(c) and (d)). Post-stent venogram showed good flow into the patent right OVS stent construct and manometry demonstrated a decreased trans-stenotic gradient of 1 mm Hg (Figure 1(e) and (f); Table 3b). The patient awoke without neurological deficits and was discharged home same day.
At 1-month follow-up, the patient self-reported decreased headache intensity. Three-month routine follow-up MRV demonstrated stent patency (Figure 4). By 1-year follow-up, he reported continued significant improvement of headaches related to intracranial hypertension.
Figure 4.
Magnetic resonance venography showing patent stent in the right occipital sinus (arrow).
Case example 2: occipital venous Sinus stenting for isolated pulsatile tinnitus
A 35-year-old female presented with a chief complaint of right-sided PT described as a whooshing sound synchronous with her heartbeat. Turning her head to the right and gentle pressure on the right neck provided relief. She additionally reported headaches of 8/10 intensity approximately once per week. Acetazolamide was ineffective at treating her symptoms. Ophthalmology exam was negative for papilledema. Outside imaging showed evidence of a prominent OVS with severe stenosis and associated sigmoid sinus aneurysm.
The patient was premedicated with aspirin 81 mg and clopidogrel 75 mg for 5 days. Under local anesthesia, the right common femoral vein was accessed. An Envoy guide catheter (Codman Neuro, Raynham, MA, USA) was advanced into the right internal jugular vein. A Headway 27 microcatheter (MicroVention, Aliso Viejo, CA, USA) was then advanced over a Synchro 2 soft microwire (Stryker, Kalamazoo, MI, USA) into the SSS via the aberrant OVS and the microwire was removed. SSS injection confirmed a dominant right OVS with severe distal stenosis, a post-stenotic venous aneurysm, and bilateral hypoplastic TSs with severe stenosis at the right TSJ (Figure 2(a) and (b)). Venous manometry was preformed revealed a trans-stenotic gradient of 7 mm Hg between the proximal occipital sinus and the jugular bulb (Table 4a).
Table 4.
Case 2 pre- and post-stenting venous sinus pressure measurements.
| Manometry pre-stenting | Pressure (mm Hg) |
|---|---|
| Superior sagittal sinus | 19 |
| Right proximal occipital sinus | 18 |
| Right jugular bulb | 11 |
| Manometry post-stenting | |
| Superior sagittal sinus | 15 |
| Right proximal occipital sinus | 15 |
| Right occipital in-stent pressure | 15 |
| Right jugular bulb | 15 |
The patient was then placed under general anesthesia and arterial access was then obtained via the right radial artery. Cerebral angiogram demonstrated no arterial pathology. An Infinity guide catheter was then navigated to the right jugular vein (Stryker, Kalamazoo, MI, USA). A Navien 072 intermediate catheter (Medtronic, Minneapolis, MN, USA) was advanced over a Headway 27 (MicroVention, Aliso Viejo, CA, USA) and Synchro 2 microwire (Stryker, Kalamazoo, MI, USA) into the proximal right TS. The Headway 27 was positioned in the SSS. The Synchro 2 microwire was exchanged for a balanced heavy weight 0.014” microwire positioned into the SSS. A Precise Pro 6 × 40 mm stent (Cordis, Hialeah, FL, USA) was advanced into the right TS and deployed across the TSJ without complications (Figure 2(c) and (d)). The Navien intermediate catheter was then repositioned into the OVS and a Precise Pro 7 × 40 mm stent (Cordis, Hialeah, FL, USA) was deployed across the OVS stenosis and the neck of the distal venous (Figure 2(e) and (f)). Post-stent venogram showed good flow through both stent constructs without residual aneurysm filling and manometry confirmed a diminished trans-stenotic gradient of 0 mm Hg (Figure 2(g) and (h); Table 4b). Angiogram confirmed good flow throughout the venous system without residual stenosis. On awakening, the patient reported immediate relief of tinnitus and was discharged home the same day. At 15-month follow-up, MRV showed patent stent constructs without new stenosis and the patient reported persistent complete resolution of her PT (Figure 5).
Figure 5.
Magnetic resonance venography showing patent stent in the right occipital sinus (arrow).
Discussion
VSS has been previously shown to be an effective treatment modality as a stand-alone treatment for PT and IIH.2,3 PT and IIH are suspected to share an underlying mechanism involving venous sinus stenosis, especially in the setting of aberrant dural venous sinus pathology. In PT patients, the pulsatile sound is thought to be caused by the turbulent flow of blood through the stenotic segment of the involved dural venous sinus, usually the TS, and also through the post-stenotic vessel dilatation, which is then transmitted to the cochlea via bone conduction. 3 In IIH patients, it is hypothesized that dural venous sinus stenosis is a consequence of extrinsic compression from increased intracranial pressure, which, in turn, further contributes to elevated intracranial pressure by diminishing overall venous outflow in a positive feedback loop. 10 OVS stenting in either IIH or PT patients has been rarely described in the literature, and to our knowledge, this series represents the largest experience to date.
Embryologically, the OVS is derived from small venous channels around the primitive torcula and medial portions of TSs. It is most prominent during the fifth month of gestation and progressively regresses by the age of two. 5 It terminates at the level of the occipital protuberance at the level of the confluence of sinuses. 11 Previous studies have reported an incidence of persistent OVS in less than 10% of adults. 11 In 77.8% of cases where the OVS is persistent, the TSs are hypoplastic or absent. 11 In our series, all five patients presented with hypoplastic or absent TSs. Given its rarity, pathologies associated with the OVS can be easily overlooked, and only a few cases of OVS stenting have been described in the literature.6,8,9 In all of our five patients, the OVS was the main pathway of venous outflow and the area of stenosis was identified near or at the junction of the OVS to the ipsilateral jugular bulb.
In a prospective trial of isolated PT patients with dural venous sinus stenosis with or without associated aneurysms, VSS was shown to completely resolve symptoms in 93% of patients, and 5% of patients experienced near-complete resolution. 3 No recurrence was noted at follow-up. In this case series, all four patients with PT experienced complete symptom resolution without recurrence.
In IIH patients, dural venous sinus stenosis is commonly associated with intrinsic or extrinsic stenosis related to thrombotic dysregulation, arachnoid granulations, or aberrant anatomy associated with venous hypertension leading to impaired resorption of cerebrospinal fluid (CSF).1,12 In medically refractory or fulminant IIH patients with venous sinus stenosis, VSS can potentially improve symptoms without the need for surgical CSF diversion. A recent meta-analysis of 781 total VSS procedures in 694 patients showed 76% reduction in papilledema, 73% reduction in headaches, 65% improvement in visual acuity, and 43% reduction in tinnitus. 12 Complication rate was low at 0.9%. Studies have also shown significant decreases in CSF opening pressure after VSS. 3
In both IIH and non-IIH PT associated with venous sinus pathology, aberrant venous sinus anatomy can be present in the setting of stenosis. Stenosis of the persistent OVS variant itself directly contributed to the pathology of our five patients, as was supported by elevated trans-stenotic pressure gradients on venous manometry that normalized after OVS stenting. A previously published single report of VSS for distal stenosis of a dominant OVS in a patient with IIH showed successful resolution of papilledema and headaches after stenting. 6 This prior case coupled with our experience highlight the importance of studying the dural sinus anatomy in patients with IIH and PT in order to reveal potential targets for endovascular therapy.
Conclusions
Dural venous sinus stenosis is a common finding in patients with IIH and non-IIH PT. Regardless of whether a cause or a consequence, the stenosis can be targeted and treated with stenting for symptomatic relief. In some patients, the site of stenosis may be within an anatomical variant, such as a persistent OVS, that comprises the dominant drainage pathway, and stenting in these cases seems to still be beneficial. In our experience, OVS stenting is a safe and effective endovascular treatment for IIH and PT in the presence of this uncommon variant. Nonetheless, this is a limited retrospective case series from a single institution and further validation of these findings in larger, prospective datasets remains warranted.
Corrections (October 2024): In the published version of the article, errors were noted on pages 2 and 3. These errors have been corrected in the updated version of the article. For complete details, refer to the correction notice available here: [Include the complete DOI of the corrigendum]
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: This work is approved by the Ethical Comity of North Shore University Hospital.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article,
ORCID iDs: Kyriakos Papadimitriou https://orcid.org/0000-0002-6025-1755
Timothy G White https://orcid.org/0000-0002-3604-4334
Danielle Golub https://orcid.org/0000-0001-8732-796X
Justin Turpin https://orcid.org/0000-0002-3686-2695
Kevin Shah https://orcid.org/0000-0003-0896-2266
Patient consent: An informed consent was obtained prior to this work.
References
- 1.Leishangthem L, SirDeshpande P, Dua D, et al. Dural venous sinus stenting for idiopathic intracranial hypertension: an updated review. J Neuroradiol 2019; 46: 148–154. [DOI] [PubMed] [Google Scholar]
- 2.Patsalides A, Oliveira C, Wilcox J, et al. Venous sinus stenting lowers the intracranial pressure in patients with idiopathic intracranial hypertension. J Neurointerv Surg 2019; 11: 175–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patsalides A, Santillan A, Sundararajan SH, et al. Venous sinus stenting for the treatment of isolated pulsatile tinnitus: results of a prospective trial. Interv Neuroradiol 2021; 27: 266–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goyal G, Singh R, Bansal N, et al. Anatomical variations of cerebral MR venography: is gender matter? Neurointervention 2016; 11: 92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Satyarthee GD, Moscote-Salazar LR, Agrawal A. Persistent enlarged occipital sinus with absent unilateral transverse sinus. J Neurosci Rural Pract 2019; 10: 519–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al Balushi A, Oliveira C, Patsalides A. Idiopathic intracranial hypertension with stenosis of a solitary occipital venous sinus treated with stenting. Interv Neuroradiol 2020; 26: 664–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Inui T, Shibuya M, Miyabayashi T, et al. Two cases of persistent falcine and occipital sinuses. Brain Dev 2021; 43: 170–173. [DOI] [PubMed] [Google Scholar]
- 8.Buell TJ, Raper DMS, Ding D, et al. Concurrent venous stenting of the transverse and occipito-marginal sinuses: an analogy with parallel hemodynamic circuits. J Neurosci Rural Pract 2019; 10: 334–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alvarado AM, Nalluri P, Alvarado AM, et al. Unique variant of idiopathic intracranial hypertension dural sinus stenting. Int J Neurosci 2021; 131: 196–198. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed RM, Wilkinson M, Parker GD, et al. Transverse sinus stenting for idiopathic intracranial hypertension: a review of 52 patients and of model predictions. Am J Neuroradiol 2011; 32: 1408–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Widjaja E, Griffiths PD. Intracranial MR venography in children: normal anatomy and variations. Am J Neuroradiol 2004; 25: 1557–1562. [PMC free article] [PubMed] [Google Scholar]
- 12.Lim J, Monteiro A, Kuo CC, et al. Stenting for venous sinus stenosis in patients with idiopathic intracranial hypertension: an updated systematic review and meta-analysis of the literature. Neurosurgery 2024; 94: 648–656. doi: 10.1227/neu.0000000000002718. [DOI] [PubMed] [Google Scholar]