Abstract
Background:
Cannabinoids are a diverse group of compounds under investigation for various medical purposes, including analgesia. Given the evolving landscape of cannabinoid use, we aimed to analyze their prevalence and effect in pain management among urban orthopedic hand patients.
Methods:
An electronic survey was administered to 122 new patients presenting to the orthopedic hand clinic of a major urban academic hospital. Demographic data, numerical rating scale pain scores, cannabinoid usage, and other concomitant pain regimens were recorded.
Results:
Approximately half of the new patients were dissatisfied with current pain management for their hand pathology. Prescription (Rx) and over-the-counter (OTC) pain medications were used by 58% (71/122) of patients, while cannabinoids were used by 15% (18/122) of patients. Compared with pre-usage pain scores, both cannabinoids and Rx/OTC medications induced significant reductions in pain associated with patients’ hand pathologies (Cannabinoid: Δ4.4, P = .002; Rx/OTC: Δ3.0, P < .001). Cannabinoids induced a larger analgesic effect, but this difference was not statistically or clinically significant (P = .06). Subjectively, cannabinoid users either preferred their cannabinoid over Rx/OTC medications or liked both equally. Opioid use was higher among cannabinoid users (22.2% vs 12.5%), although this was not statistically significant (P = .28).
Conclusion:
Approximately 15% of new urban hand patients use cannabinoids for pain control, and these compounds have similar analgesic efficacy in hand pathologies as Rx/OTC medications. Cannabinoids are equally liked or preferred relative to traditional medications in this cohort, and they may play an important role in pain management for hand patients.
Keywords: opioid, cannabinoid, CBD, THC, marijuana, orthopedic, hand, hand surgery, pain, pain control, pain management, pain score
Introduction
Cannabis refers to all products derived from the plants Cannabis sativa. 1 Among these, cannabinoids are a diverse group of compounds that bind to the cannabinoid receptors of the body. 2 The main cannabinoids found in cannabis products are cannabidiol (CBD) and tetrahydrocannabinol (THC); however, more than 100 other cannabinoids have been identified. 1 While cannabinoid products have been used medically and recreationally for millennia, they have only become officially recognized for their medicinal indications in parts of the United States since 1996. 3 Chiefly, cannabinoids have been proven as effective analgesic,4,5 antiemetic,4,6 antispasmodic, 7 and anti-inflammatory 8 medications. Similarly, their effects on increasing appetite9 -12 and reducing seizures13,14 have been investigated for clinical utility.
While California was the first state to legalize medicinal cannabinoids, 38 other states and the District of Columbia have now passed laws legalizing medicinal marijuana as of December 2023. 15 Outside of medical uses, cannabinoid use has also progressed more broadly. In the most recent National Survey on Drug Use and Health conducted in 2022, lifetime marijuana use was estimated at around 46.9% of all people aged 12 or older. 16 Given the medicinal benefits, high rates of lifetime consumption among the population, and relatively widespread legalization, it would be reasonable to suspect that cannabinoid use may be occurring among patients with orthopedic hand pathologies.
Previous research on this subject has shown that around 10% to 34% of orthopedic patients may be using marijuana for pain control.17 -19 This research is especially salient in light of the opioid crisis of the last 3 decades, which stemmed from initial over-prescription of opioids and resulting increases in opioid use disorder.20 -22 In response to this crisis, more energy and research has been dedicated to the diversification of pain control methods. Recent research substantiates the idea that multimodal analgesia is effective and safer for patients, and efforts have been made to transition to personalized and varied pain control regimens.23,24 Among the various classes of medications, cannabinoids have been considered as potential supplementary analgesics due to greater evidence establishing their efficacy and safety profile and growing public acceptance of these compounds.25 -27
Considering the cannabinoid landscape and the relative paucity of literature on its use among orthopedic hand patients, the objective of this study is to characterize the prevalence and effect of cannabinoid use within this population by analyzing demographic characteristics, current pain control modalities, and pain scores between cannabinoid and non-cannabinoid cohorts.
Materials and Methods
Institutional Review Board Statement
This study was classified as human subjects research and was approved by our university’s institutional review board (IRB), IRB protocol no. 20-1885. All procedures followed were in accordance with the ethical standards of the relevant institutional and national committee on human experimentation, with the ethical guidelines of the 1975 Declaration of Helsinki as most recently revised in 2013, and with the regulatory requirements laid down in U.S. Code of Federal Regulations, Title 45 Department of Health and Human Services Part 46, Protection of Human Subjects.
Survey Design
We designed a one-time survey for new patients presenting to our orthopedic hand clinic that covered demographics, mental health status at the time of survey administration, current symptoms, diagnosis received, pain intensity, and data regarding analgesic use specifically for their hand pathology; this included prescription (Rx)/over-the-counter (OTC) medication use, cannabinoid use, non-medication pain control, and pain management preferences. Sex, age, and body mass index (BMI) were collected as demographic characteristics. Patients less than age 18 were excluded from participation. Pain intensity was measured using a traditional 11-point numerical rating scale (NRS), with 0 representing no pain at all and 10 representing the highest level of pain. The use of common OTC and prescription pain medications was recorded. Cannabinoid use was assessed in several ways: prescription status, prescribing provider, type of cannabinoid, method of consumption, method of purchase, and frequency of use. Both medical and recreational cannabinoid use is legal in the state where the study was conducted. Numerical rating scales of pain pre- and post-consumption were used to assess the patient-perceived efficacy of Rx/OTC pain medications and cannabinoids specifically for pain related to their hand pathology.
Survey Administration
From July 2021 to January 2022, new patients presenting to our orthopedic hand clinic were approached to participate in the one-time electronic survey. Informed consent was obtained in accordance with our IRB protocol. The survey was administered electronically with a tablet, and study data was aggregated and de-identified using REDCap electronic data capture tools. 28
Statistical Analysis
Shapiro-Wilk test was used to assess the normality of all data sets collected. 29 Comparison of characteristics, prescription/OTC drug usage, and opioid usage between cannabinoid and non-cannabinoid cohorts was conducted using Mann-Whitney U test for continuous non-parametric variables and Fisher’s exact test for categorical variables (Table 1). Fisher’s exact test was used to account for the small sample size. 30 Numerical rating scale pain score data was also non-parametric. Wilcoxon signed-rank test was used to assess the paired data of pain scores before and after analgesic usage, while Mann-Whitney U test was used to assess the non-paired data comparing analgesic effect between Rx/OTC medications and cannabinoids.29,31,32 Statistical significance was set to an alpha of 0.05. All primary data is available on request.
Table 1.
Demographics and Comparison of Cannabinoid Versus Non-Cannabinoid Cohort.
| Characteristic | Cannabinoid cohort (n = 18) | Non-cannabinoid cohort (n = 104) | Total (n = 122) | P-value |
|---|---|---|---|---|
| Average age (y) | 42.2 | 49.9 | 48.8 | N/A |
| Sex | 0.31 | |||
| Female | 13 (72.2) | 61 (58.7) | 74 (60.7) | |
| Male | 5 (27.8) | 43 (41.3) | 48 (39.3) | |
| BMI (n = 83) a | 0.04* | |||
| <18.5 (Underweight) | 1 (7.7) | 0 | 1 (1.2) | |
| 18.5 to <25 (Healthy) | 5 (38.5) | 15 (21.4) | 20 (24.1) | |
| 25 to <30 (Overweight) | 1 (7.7) | 23 (32.9) | 24 (28.9) | |
| 30 to <35 (Obese Class 1) | 6 (46.2) | 14 (20.0) | 20 (24.1) | |
| 35 to <40 (Obese Class 2) | 0 | 4 (5.71) | 4 (4.8) | |
| 40+ (Obese Class 3) | 0 | 14 (20.0) | 14 (16.9) | |
| Average BMI per person | 25.85 | 31.74 | 30.81 | |
| Presence of mental health diagnosis (n = 122) | 0.01* | |||
| None | 8 (44.4) | 72 (69.2) | 80 (65.6) | |
| 1 Diagnosis | 2 (11.1) | 19 (18.3) | 21 (17.2) | |
| 2 Diagnoses | 6 (33.3) | 10 (9.6) | 16 (13.1) | |
| 3 Diagnoses | 1 (5.56) | 3 (2.9) | 4 (3.3) | |
| 4+ Diagnoses | 1 (5.56) | 0 | 1 (0.8) | |
| Average number of diagnoses per person | 1.17 | 0.46 | 0.57 | |
| Mental health diagnosis (n = 69) b | N/A | |||
| Anxiety | 9 (50.0) | 20 (41.7) | 29 (42.0) | |
| Depression | 7 (38.9) | 18 (37.5) | 25 (36.2) | |
| Bipolar disorder | 1 (5.56) | 4 (8.3) | 5 (7.2) | |
| Substance use disorder | 2 (11.1) | 2 (4.2) | 4 (5.8) | |
| PTSD | 2 (11.1) | 0 | 2 (2.9) | |
| OCD | 0 | 1 (2.1) | 1 (1.4) | |
| ADHD | 0 | 1 (2.1) | 1 (1.4) | |
| Other | 0 | 2 (4.2) | 2 (2.9) | |
| Number of prescription/OTC medications used | 0.15 | |||
| 0 | 6 (33.3) | 46 (44.2) | 52 (42.6) | |
| 1 | 4 (22.2) | 37 (35.6) | 41 (33.6) | |
| 2 | 6 (33.3) | 11 (10.6) | 17 (13.9) | |
| 3+ | 2 (11.1) | 10 (9.6) | 12 (9.8) | |
| Average number used per person | 1.22 | 0.86 | 0.91 | |
| Opioid use | 0.28 | |||
| Yes | 4 (22.2) | 3 (12.5) | 7 (13.9) | |
| No | 14 (77.8) | 91 (87.5) | 105 (86.1) | |
Note. Values in parentheses indicate percentages. N/A = not applicable; BMI = body mass index; PTSD = post-traumatic stress disorder; OCD = obsessive-compulsive disorder; ADHD = attention-deficit hyperactivity disorder; OTC = over-the-counter.
Discrepancy between cohort size and number of responses is due to incomplete survey completion by participants.
Answer frequency may not equal the number of subject responses because patients could indicate more than 1 answer per response.
Asterisk (*) indicates statistical significance.
Results
One hundred and twenty-two patients were recruited and completed the survey. These patients had an average age of 49 years old, with a range of 18 to 84 years. Female patients represented 61% of the total cohort (74/122). Patients using cannabinoid products were more likely to have an established mental health diagnosis at the time of survey administration (1.17 diagnoses vs 0.46 diagnoses; P = .01). Full demographic characteristics are provided in Table 1.
Eighteen patients (14.8%) reported cannabinoid use for managing pain associated with their hand pathology, either exclusively (6/18; 33.3%) or in conjunction with Rx/OTC medications (12/18; 66.7%). Most of the cannabinoid cohort reported using recreational cannabinoid products (15/18, 83.3%), most commonly in the form of smoking (10/13, 76.9%) or vaping (3/13, 23.1%). The complete set of responses to the cannabinoid questions is provided in Table 2.
Table 2.
Cannabinoid Consumption Characteristics.
| Characteristic | Frequency (percent) |
|---|---|
| Cannabinoid use (n = 122) | |
| Yes | 18 (14.8) |
| No | 104 (85.2) |
| Prescription cannabinoid (n = 18) | |
| Yes | 3 (16.7) |
| No | 15 (83.3) |
| Prescribing physician (n = 3) | |
| Oncologist | 1 (33.3) |
| Nephrologist | 1 (33.3) |
| Pain management specialist | 1 (33.3) |
| Type of cannabinoid (n = 13) a | |
| Nonmedicinal marijuana | 7 (53.8) |
| Medicinal marijuana | 5 (38.5) |
| CBD oil | 3 (23.1) |
| Method of consumption (n = 13) a | |
| Smoke | 10 (76.9) |
| Vape | 3 (23.1) |
| Eat or drink | 3 (23.1) |
| Pill | 1 (7.7) |
| Topical | 1 (7.7) |
| Sublingual | 1 (7.7) |
| Method of purchase (n = 13) | |
| Dispensary or retail location | 8 (61.5) |
| Unlicensed supplier | 3 (23.1) |
| Both | 2 (15.4) |
| Frequency of use (n = 13) | |
| Every day | 9 (69.2) |
| 2-3 times per week | 1 (7.7) |
| Once per week | 1 (7.7) |
| Twice per month | 1 (7.7) |
| Once per month | 1 (7.7) |
Note. CBD = cannabidiol.
Answer frequency may not equal the number of subject responses because patients could indicate more than 1 answer per response.
Prescription/OTC pain medication use was common among patients presenting to the clinic; approximately 58% of all patients surveyed (71/122) reported some form of medication use for pain control. The types of non-cannabinoid pain medications most commonly used were nonsteroidal anti-inflammatory drugs (NSAIDs; 61.4%), acetaminophen (54.3%), opioids (28.6%), and gabapentin (8.6%).
Patients were frequently dissatisfied with their current pain management when they presented to clinic. Among all patients, including patients not taking any analgesics for their hand pathology, 44% (54/122) reported unsatisfactory current pain management. When divided into cohorts, the non-cannabinoid cohort reported dissatisfaction rates of 44% (46/104), with further subcategorization yielding 35% (16/45) dissatisfaction for patients with no current analgesic intake and 51% (30/59) dissatisfaction for patients with exclusive Rx/OTC pain regimens. The cannabinoid cohort reported dissatisfaction rates of 44% (8/18), with further subcategorization yielding 50% (6/12) dissatisfaction for patients with combined Rx/OTC + cannabinoid regimens and 33% (2/6) dissatisfaction for patients with exclusive cannabinoid regimens.
Of the patients who used cannabinoids alongside Rx/OTC medications for hand pathology analgesia and reported their preferences, all of them preferred either the cannabinoid (7/11, 63.6%) or both equally (4/11, 36.4%). None preferred prescription/OTC pain medications alone. Full pain and medication characteristic data are provided in Table 3.
Table 3.
Pain and medication characteristics.
| Characteristic | Frequency (percent) |
|---|---|
| Medication use for pain management (n = 122) | |
| Yes | 71 (58.2) |
| No | 51 (41.8) |
| Dissatisfaction with current pain management | |
| Entire study population (n = 122) | 54 (44.3) |
| Non-cannabinoid cohort (n = 104) | 46 (44.2) |
| Patients with no analgesic use (n = 45) | 16 (35.6) |
| Patients with exclusive Rx/OTC use (n = 59) | 30 (50.8) |
| Cannabinoid cohort (n = 18) | 8 (44.4) |
| Patients with Rx/OTC + cannabinoid use (n = 12) | 6 (50) |
| Patients with exclusive cannabinoid use (n = 6) | 2 (33.3) |
| Type of non-cannabinoid pain medications (n = 70) a | |
| NSAIDs | 43 (61.4) |
| Acetaminophen | 32 (54.3) |
| Opioids | 20 (28.6) |
| Gabapentin | 6 (8.6) |
| Other | 10 (14.3) |
| Pain control preference (n = 11) | |
| Prescription/OTC pain medication | 0 (0) |
| Cannabinoid | 7 (63.6) |
| Both equally | 4 (36.4) |
Note. Rx = prescription; OTC = over-the-counter; NSAIDs = nonsteroidal anti-inflammatory drugs.
Answer frequency may not equal the number of patient responses because patients could indicate more than 1 answer per response.
Comparison data between cannabinoid and non-cannabinoid cohort is shown in Table 1. There was a lower average age in the cannabinoid cohort (42.2 vs 49.9 years), as well as a higher percentage of female patients (72.2% vs 58.7%). There was a greater number of patients in the cannabinoid cohort that used 2 or more Rx/OTC medication (44.4% vs 20.2%), and opioid use was higher among cannabinoid users (22.2% vs 12.5%), although this was not statistically significant when analyzed with Fisher’s exact test (P = .28).
In our entire patient dataset, including both cannabinoid and non-cannabinoid cohorts, 67 full sets of pain scores secondary to hand pathology were reported for prescription/OTC medications and 13 full sets of pain scores were reported for cannabinoids. Data were analyzed in this fashion to capture all pain score data, as some patients in the cannabinoid cohort used both Rx/OTC and cannabinoid medications and reported pain scores for both. The average pain score from hand pathologies before use of cannabinoids and Rx/OTC pain medications was similar, rating 7.3 for both. The average pain score after analgesic use varied, with cannabinoids inducing a lower average pain score after use than Rx/OTC medications: 2.9 versus 4.3, respectively (Figure 1). This corresponds with an average pain reduction for cannabinoids of 4.4 (Z = −3, P = .002) while Rx/OTC medications elicited a drop of 3.0 (Z = −6.5, P < .001). When comparing pain reduction between analgesic modalities, Figure 2 demonstrates that cannabinoids reduced pain by 1.38 more relative to prescription/Rx; this approached significance (P = .06).
Figure 1.
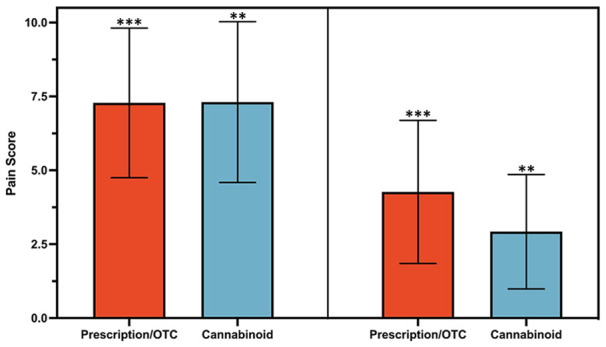
Numerical pain scores before and after analgesic use.
Note. Clustered bar graph illustrating the numerical pain scores of prescription/OTC and cannabinoid analgesics. Error bars represent ± 1 standard deviation. Pain scores were collected for each of these categories both before and after ingestion for comparison. OTC = over-the-counter.
**P ≤ .01. ***P ≤ .001.
Figure 2.
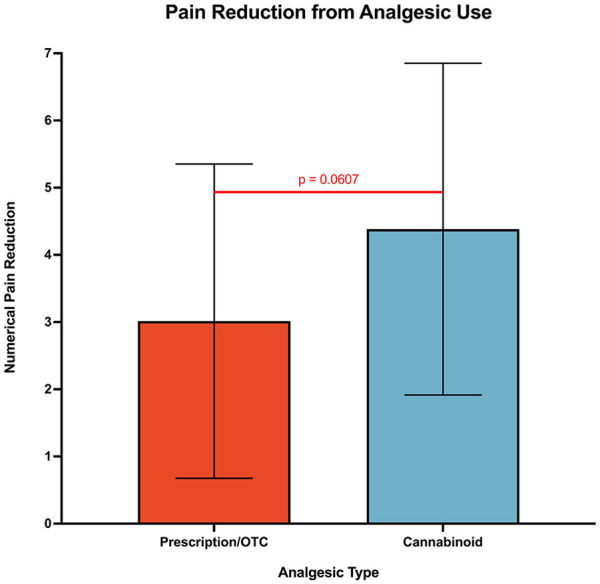
Average pain reduction from analgesic use.
Note. Bar graph illustrating the total reduction in numerical pain scores from baseline before ingestion to after ingestion for both prescription/OTC and cannabinoid analgesics. Error bars represent ± 1 standard deviation. In this graph, higher values indicate a greater reduction in pain and more effective pain control. OTC = over-the-counter.
Discussion
Pain management is a critical step in the continuum of orthopedic care. Our survey asked new patients presenting to our orthopedic hand clinic how they were managing pain associated with their hand pathology and what role cannabinoids played in that process.
First, our results show that this research is relevant to our patients, given that nearly half of them expressed dissatisfaction with their current pain management at the time of presentation. While most of our study population were using some form of analgesic for pain control, 44% (54/122) expressed that their current pain regimen was insufficient for managing pain associated with their hand pathology. When broken down further into subcohorts, patients with exclusive Rx/OTC regimens and combined Rx/OTC + cannabinoid regimens expressed the highest level of current dissatisfaction at 51% and 50%, respectively. While the reasoning behind regimen dissatisfaction was not captured, this difference may reflect more painful baseline hand pathologies or higher baseline pain sensitivity, as these types of patients are more likely to have pursued an analgesic regimen before arriving to clinic and are less likely to find these regimens helpful. This hypothesis is supported through comparison to the dissatisfaction rates among patients with no current analgesic intake (35%) and those solely on cannabinoids (33%), which may reflect patients with less painful pathologies or higher pain tolerance. However, we cannot make definitive conclusions with these data, and this relationship deserves further evaluation in future studies. Among the medications used, OTC medications such as NSAIDs and acetaminophen were most commonly used, followed by prescription medications such as opioids and gabapentin.
Second, a substantial portion of surveyed patients used cannabinoids as a singular or adjunct analgesic for hand pathology pain. Approximately 15% (18/122) of patients reported cannabinoid use, and most indicated daily use of their cannabinoid (69%, 9/13). This substantiates prior research estimating that cannabinoid use among hand patients is approximately 10% to 34%.17 -19 As cannabinoids become legal across the country and their analgesic applications become more popular, hand surgeons can expect that cannabinoid use will increase among their patients. 33 Indeed, recent research indicates that 81% of patients would consider using medical cannabis for orthopedic-related chronic pain. 17 Interestingly, despite medical and recreational marijuana being legal in Illinois, 38% (5/13) of patients reported purchasing cannabinoids from an unlicensed supplier, indicating that legality may only be one factor among many behind the rise in cannabinoid use. Hand surgeons should be aware of these trends and should counsel their patients appropriately.
Aside from prevalence, the value of cannabinoids in pain management was also assessed individually and relative to traditional medications. Pain score data shows that patients used cannabinoids and prescription/OTC pain medications when their pain reached similar levels (7.3 in each group). However, reported pain reduction was greater with cannabinoids relative to Rx/OTC medications (Δ4.4 vs Δ3.0 on NRS scale), although this difference did not reach statistical significance (P = .06). Recent systematic reviews of the minimal clinically important difference (MCID) in mean change of acute and chronic pain scores were shown to have a median of 23% and 32%, respectively.34,35 Using these statistics and the baseline pain score of 7.3, our cohort has an acute pain MCID of 1.68 and a chronic pain MCID of 2.34. Both cannabinoids and prescription/OTC pain medications surpass these thresholds independently, indicating clinically meaningful reductions in acute and chronic pain. When comparing the 2 modalities, the difference in pain reduction was 1.4, which is less than the MCID for acute and chronic pain. Therefore, neither of these analgesics provides a statistically or clinically significant advantage in pain reduction over the other. Importantly, MCID is variable between pathologies and people; therefore, it is difficult to fully determine the clinical advantage of these analgesics relative to each other. In addition, traditional pain medications are limited by dosage and pill numbers, while cannabinoids do not have similar limitations; this may play a role in the efficacy of pain reduction when comparing the 2 modalities.
While the difference in pain reduction based on NRS pain scores is not completely clear, the subjective preference of the cannabinoid cohort was heavily weighted toward cannabinoids versus traditional medications. Cannabinoids were preferred over Rx/OTC medications by 64% of the cannabinoid cohort, and no respondents preferred traditional medications over cannabinoids. Taken together, these results indicate that among our cohort, cannabinoids are effective at managing pain associated with hand pathologies, and those who use cannabinoids place high value on them as part of their pain control regimen.
Given the recent attention on the risks of opioid analgesics, we examined whether cannabinoid use influenced concurrent opioid use for pain control. Usage rates for Rx/OTC pain medications and opioids were assessed for cannabinoid and non-cannabinoid cohorts. A greater number of patients in the cannabinoid cohort used 2 or more Rx/OTC medications (44.4% vs 20.2%), and opioid use was also increased among cannabinoid users (22.2% vs 12.5%), although this was not statistically significant (P = 0.28). This result aligns with previous literature indicating that opioid use may be increased among cannabinoid users,19,36,37 although there also exists evidence showing both no link 38 and decreased opioid use among cannabinoid users.39,40 There are many potential reasons for this relationship, but our data is not strong enough to make an assertion either way; the current body of literature supports the idea that the relationship between cannabinoids and opioids is variable.
This study design has some limitations. Selection bias may be present, as the survey could only be administered when the research assistant was present. The voluntary survey questions were not fully completed by all participants, producing some partially incomplete datasets. The number of patients who were noted to use cannabinoids was relatively small, restricting the generalizability of these findings. Due to our small sample size, this study may have been underpowered to detect statistically significant differences, even among the analyses that approached or produced a P-value < .05, including BMI, presence of mental health diagnoses, number of medications used, opioid use, and pain reduction. Although information was provided that the results would be analyzed in aggregate, patients may have been hesitant to share information on cannabinoid usage, despite medical and recreational legality in the state where this study was conducted, thus underestimating the actual prevalence. We grouped all cannabinoids under a single umbrella term despite significant variability among cannabinoid products; this may not capture nuances between cannabinoid types, ingestion methods, and potencies. Among prescription cannabinoid users, the 3 cannabinoid prescribers were not directly within the hand surgery realm (oncologist, nephrologist, and pain management specialist), indicating potential confounding diagnoses for some patients that may be motivating cannabinoid use for pain management beyond their hand pathology. Indeed, while our survey specified that our questions relate to cannabinoid use specifically for patients’ current hand pathology, some patients may have counted cannabinoid use for pain management of other pathologies while completing the survey. We did not account for the difference in established mental health diagnoses at the time of survey administration as a confounding factor in the prevalence or efficacy of either Rx/OTC medications or cannabinoids. Finally, the survey was only conducted in a single large urban academic medical center, therefore external validity and generalizability of the data may be limited.
Although this is a small-scale study, these findings support the idea that cannabinoids are used regularly and are effective for pain control in orthopedic hand patients. Given the variety of cannabinoids among patients surveyed, future directions include examining the formulations, ingestion methods, and potencies that most improve pain from hand pathologies. Orthopedic surgeons should continue working with their patients to find successful, safe, and personalized ways to achieve adequate pain control.
Footnotes
Ethical Approval: This study was classified as human subjects research and was approved by our university’s Institutional Review Board, IRB protocol no. 20-1885.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the relevant institutional and national committees on human experimentation, with the ethical guidelines of the 1975 Declaration of Helsinki as most recently revised in 2013, and with the regulatory requirements laid down in U.S. Code of Federal Regulations, Title 45 Department of Health and Human Services Part 46, Protection of Human Subjects.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Marc G. Sleiman  https://orcid.org/0000-0002-9291-9596
https://orcid.org/0000-0002-9291-9596
Jeffrey G. Stepan  https://orcid.org/0000-0002-6595-9752
https://orcid.org/0000-0002-6595-9752
References
- 1. National Center For Complementary and Alternative Medicine. Cannabis (marijuana) and cannabinoids: what you need to know. Accessed May 15, 2022. https://www.nccih.nih.gov/health/cannabis-marijuana-and-cannabinoids-what-you-need-to-know
- 2. Zou S, Kumar U. Cannabinoid receptors and the endocannabinoid system: signaling and function in the central nervous system. Int J Mol Sci. 2018;19(3):833. doi: 10.3390/ijms19030833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bridgeman MB, Abazia DT. Medicinal cannabis: history, pharmacology, and implications for the acute care setting. P T. 2017;42(3):180-188. [PMC free article] [PubMed] [Google Scholar]
- 4. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473. doi: 10.1001/jama.2015.6358 [DOI] [PubMed] [Google Scholar]
- 5. Lynch ME, Campbell F. Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials. Br J Clin Pharmacol. 2011;72(5):735-744. doi: 10.1111/j.1365-2125.2011.03970.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Smith LA, Azariah F, Lavender VTC, et al. Cannabinoids for nausea and vomiting in adults with cancer receiving chemotherapy. Cochrane Database Syst Rev. 2015;11:CD009464. doi: 10.1002/14651858.CD009464.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Corey-Bloom J, Wolfson T, Gamst A, et al. Smoked cannabis for spasticity in multiple sclerosis: a randomized, placebo-controlled trial. CMAJ Can Med Assoc J. 2012;184(10):1143-1150. doi: 10.1503/cmaj.110837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nagarkatti P, Pandey R, Rieder SA, et al. Cannabinoids as novel anti-inflammatory drugs. Future Med Chem. 2009;1(7):1333-1349. doi: 10.4155/fmc.09.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Andries A, Frystyk J, Flyvbjerg A, et al. Dronabinol in severe, enduring anorexia nervosa: a randomized controlled trial. Int J Eat Disord. 2014;47(1):18-23. doi: 10.1002/eat.22173 [DOI] [PubMed] [Google Scholar]
- 10. Soria-Gómez E, Bellocchio L, Reguero L, et al. The endocannabinoid system controls food intake via olfactory processes. Nat Neurosci. 2014;17(3):407-415. doi: 10.1038/nn.3647 [DOI] [PubMed] [Google Scholar]
- 11. Farokhnia M, McDiarmid GR, Newmeyer MN, et al. Effects of oral, smoked, and vaporized cannabis on endocrine pathways related to appetite and metabolism: a randomized, double-blind, placebo-controlled, human laboratory study. Transl Psychiatry. 2020;10(1):1-11. doi: 10.1038/s41398-020-0756-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kirkham TC. Cannabinoids and appetite: food craving and food pleasure. Int Rev Psychiatry. 2009;21(2):163-171. doi: 10.1080/09540260902782810 [DOI] [PubMed] [Google Scholar]
- 13. Zaheer S, Kumar D, Khan MT, et al. Epilepsy and cannabis: a literature review. Cureus. 2018;10(9):e3278. doi: 10.7759/cureus.3278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Perucca E. Cannabinoids in the treatment of epilepsy: hard evidence at last? J Epilepsy Res. 2017;7(2):61-76. doi: 10.14581/jer.17012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. National Conference of State Legislatures. State medical cannabis laws. Published June 22, 2023. Accessed December 26, 2023. https://www.ncsl.org/health/state-medical-cannabis-laws
- 16. Substance Abuse and Mental Health Services Administration. Section 1: illicit drug use/misuse tables. Results from the 2022 national survey on drug use and health: detailed tables, SAMHSA. Published November 13, 2023. Accessed December 26, 2023. https://www.samhsa.gov/data/sites/default/files/reports/rpt42728/NSDUHDetailedTabs2022/NSDUHDetailedTabs2022/NSDUHDetTabsSect1pe2022.htm
- 17. Fones L, Townsend C, Hoyen H, et al. Hand surgery patient perspectives on medical cannabis: a survey of over 600 patients. J Hand Surg Glob Online. 2022;5:102-107. doi: 10.1016/j.jhsg.2022.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Carney JJ, Hwang A, Heckmann N, et al. Characteristics of marijuana use among orthopedic patients. Orthopedics. 2020;43(2):108-112. doi: 10.3928/01477447-20191212-07 [DOI] [PubMed] [Google Scholar]
- 19. Denduluri SK, Woolson ST, Indelli PF, et al. Cannabinoid and opioid use among total joint arthroplasty patients: a 6-year, single-institution study. Orthopedics. 2021;44(1):e101-e106. doi: 10.3928/01477447-20200928-02 [DOI] [PubMed] [Google Scholar]
- 20. Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 1. Pain Physician. 2017;20(2S):S93-S109. [PubMed] [Google Scholar]
- 21. Azadfard M, Huecker MR, Leaming JM. Opioid Addiction. StatPearls Publishing; 2022. Accessed June 12, 2022. https://www.ncbi.nlm.nih.gov/books/NBK448203/ [PubMed] [Google Scholar]
- 22. Jones MR, Viswanath O, Peck J, et al. A brief history of the opioid epidemic and strategies for pain medicine. Pain Ther. 2018;7(1):13-21. doi: 10.1007/s40122-018-0097-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152(7):691-697. doi: 10.1001/jamasurg.2017.0898 [DOI] [PubMed] [Google Scholar]
- 24. Schwenk ES, Mariano ER. Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J Anesthesiol. 2018;71(5):345-352. doi: 10.4097/kja.d.18.00217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. A summary of reviews of evidence on the efficacy and safety of medical use of cannabis and cannabinoids. Accessed September 18, 2022. https://www.emcdda.europa.eu/publications/technical-reports/summary-reviews-evidence-efficacy-and-safety-medical-use-cannabis-and-cannabinoids_en
- 26. Aviram J, Samuelly-Leichtag G. Efficacy of cannabis-based medicines for pain management: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2017;20(6):E755-E796. [PubMed] [Google Scholar]
- 27. Green TV. Americans Overwhelmingly Say Marijuana Should Be Legal for Medical or Recreational Use. Pew Research Center. Accessed September 18, 2022. https://www.pewresearch.org/fact-tank/2021/04/16/americans-overwhelmingly-say-marijuana-should-be-legal-for-recreational-or-medical-use/ [Google Scholar]
- 28. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nair AS, Diwan S. Pain scores and statistical analysis—the conundrum. Ain-Shams J Anesthesiol. 2020;12(1):35. doi: 10.1186/s42077-020-00085-8 [DOI] [Google Scholar]
- 30. Kim HY. Statistical notes for clinical researchers: sample size calculation 2. Comparison of two independent proportions. Restor Dent Endod. 2016;41(2):154-156. doi: 10.5395/rde.2016.41.2.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kim TK. Practical statistics in pain research. Korean J Pain. 2017;30(4):243-249. doi: 10.3344/kjp.2017.30.4.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Scheff SW. Fundamental Statistical Principles for the Neurobiologist: A Survival Guide. Elsevier; 2016. [Google Scholar]
- 33. Hasin D, Walsh C. Trends over time in adult cannabis use: a review of recent findings. Curr Opin Psychol. 2021;38:80-85. doi: 10.1016/j.copsyc.2021.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Olsen MF, Bjerre E, Hansen MD, et al. Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Med. 2017;15(1):35. doi: 10.1186/s12916-016-0775-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Olsen MF, Bjerre E, Hansen MD, et al. Minimum clinically important differences in chronic pain vary considerably by baseline pain and methodological factors: systematic review of empirical studies. J Clin Epidemiol. 2018;101:87-106.e2. doi: 10.1016/j.jclinepi.2018.05.007 [DOI] [PubMed] [Google Scholar]
- 36. Salottolo K, Peck L, Tanner A, II, et al. The grass is not always greener: a multi-institutional pilot study of marijuana use and acute pain management following traumatic injury. Patient Saf Surg. 2018;12(1):16. doi: 10.1186/s13037-018-0163-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Olfson M, Wall MM, Liu SM, et al. Cannabis use and risk of prescription opioid use disorder in the United States. Am J Psychiatry. 2018;175(1):47-53. doi: 10.1176/appi.ajp.2017.17040413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jennings JM, McNabb DC, Johnson RM, et al. Use of cannabis does not decrease opioid consumption in patients who underwent total joint arthroplasty. Arthroplast Today. 2022; 15:141-146. doi: 10.1016/j.artd.2022.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lake S, Walsh Z, Kerr T, et al. Frequency of cannabis and illicit opioid use among people who use drugs and report chronic pain: a longitudinal analysis. PLoS Med. 2019;16(11): e1002967. doi: 10.1371/journal.pmed.1002967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vivace BJ, Sanders AN, Glassman SD, et al. Cannabinoids and orthopedic surgery: a systematic review of therapeutic studies. J Orthop Surg. 2021;16(1):57. doi: 10.1186/s13018-021-02205-y [DOI] [PMC free article] [PubMed] [Google Scholar]


