Abstract
Background:
The 2 primary surgical approaches for proximal interphalangeal joint (PIPJ) arthroplasty, dorsal or volar, have been extensively described in the literature. However, the ongoing debate regarding which approach offers superior results or is associated with fewer complications persists. This systematic review aims to compare the outcomes of PIPJ arthroplasty between the dorsal and volar approaches.
Methods:
A comprehensive search of multiple databases was conducted, and studies meeting predetermined criteria were included. Data extraction, assessment of bias risk, and statistical analysis were performed to compare treatment modalities. Outcome measures included range of motion (ROM), patient-reported outcome measures (PROMs), revisions, and reported complications.
Results:
Among 368 screened articles, 5 studies involving 302 patients (310 implants) were eligible for final review. No significant differences were observed between the 2 approaches regarding postoperative ROM (mean difference [MD] 2.24; 95% confidence interval [CI] −3.83, 8.32; P = .47) and PROMs (standardized mean difference [SMD] 0.18; 95% CI −0.12, 0.48; P = .25). Complication rates, including revision/fusion, persistent pain, stiffness, infection, and dislocation, did not significantly differ between the approaches. Notably, dorsal approach was associated with higher risk of swan-neck deformity (9 out of 82 implants), while no such cases were reported in the volar approach (0 out of 101 implants).
Conclusion:
Despite limitations and heterogeneity in the literature, both dorsal and volar approaches for PIPJ arthroplasty appear to yield equivalent outcomes for patients.
Level of Evidence:
II, therapeutic.
Keywords: digits, arthroplasty, arthritis, osteoarthritis, outcomes, surgery
Introduction
Arthritis affecting the proximal interphalangeal joint (PIPJ) is a prevalent condition, with reported population-based studies estimating its incidence at around 18% to 20%, while symptomatic cases range from 0.7% to 6%.1 -3 Typically, patients can manage their symptoms through activity modification and medication such as analgesics or anti-inflammatories. In cases of exacerbation, intra-articular steroid injections may provide relief. However, as symptoms progress, surgical intervention becomes necessary.
Traditionally, arthrodesis of the PIPJ has been the standard surgical approach, particularly for achieving stability and strength in pinch and grip, notably in the index and middle fingers. However, this procedure can be disabling for the ring and little fingers, which require flexion for better function. 4 Joint replacement has emerged as an alternative, aiming to alleviate pain while preserving or enhancing mobility. 5 Over the past 4 decades, various PIPJ replacement implants have been developed, ranging from flexible silastic hinges to constrained hinges and recently, Pyrocarbon anatomical surface replacements.5 -7
The 2 primary surgical approaches for PIPJ replacement, dorsal and volar, have been extensively described, along with variations to facilitate exposure and protect soft tissue stabilizers. The dorsal approach provides wide exposure and access to the joint, with potential for rebalancing the extensor mechanism. However, it carries a risk of joint contracture due to extensor tendon adhesion and possible extension lag. In contrast, the volar approach maintains the integrity of the extensor mechanism and allows for early postoperative rehabilitation.8,9 While the lateral approach has been mentioned in the literature, its outcomes remain uncertain due to limited reported data.10,11
Despite the growing popularity of PIPJ replacement, the evidence base remains limited, primarily consisting of retrospective case series with small sample sizes. A meta-analysis by Adams et al 12 in 2012 highlighted the lack of established effectiveness for PIPJ replacement due to study design and outcome reporting heterogeneity. Subsequently, Yamamoto et al in 2017 conducted a systematic review on surgical approaches and implants in PIPJ replacement but focused solely on descriptive analysis without direct comparative analysis. 9
Given the gaps in current literature, the purpose of this systematic review was to evaluate the available literature on the 2 common surgical approaches for PIPJ replacement. We aim to perform statistical analyses to compare the patients’ outcomes and complications rates between the 2 approaches in PIPJ replacement.
Methods
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement (Supplemental Appendix 1). 13
Protocol Setting
We systematically included all comparative studies directly contrasting dorsal and volar approaches for PIPJ replacement in our search. This encompassed randomized controlled trials (RCTs), as well as prospective and retrospective observational studies and series. Only studies available in English or with a translation were considered eligible for inclusion. Our criteria dictated that participants must be over 18 years old, diagnosed with primary PIPJ arthritis, and have undergone PIPJ replacement. We excluded studies focusing on individuals with PIPJ arthritis secondary to trauma or cancer, as well as those investigating revision PIPJ replacement.
The primary outcome of interest revolved around patient-reported outcome measures (PROMs), such as the Disabilities of the Arm, Shoulder, and Hand score (DASH/QuickDASH), Michigan Hand Outcomes Questionnaire (MHQ), and Patient-Rated Wrist/Hand Evaluation (PRWHE). Additionally, we analyzed secondary outcomes, including data comparing range of motion (ROM), revision rates, and complications.
Identification of Studies
The search strategy of our literature search is detailed in Supplemental Appendix 2. We conducted searches in Medline, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) from their inception to August 2023. Additionally, we reviewed the reference lists of identified studies and previous systematic reviews to identify any relevant studies for potential inclusion.
Selection of Studies
The screening and selection of studies were performed by 3 authors (GM, EA, and EG), and any disagreements were resolved by the fourth author (SD). Initially, articles obtained from the searches underwent screening based on a review of their titles and abstracts, followed by a thorough assessment of the full texts.
Risk of Bias Assessment
Three authors (GM, EA, and EG) independently evaluated each study for risk of bias using the Cochrane Risk of Bias in Non-randomized Studies—of Interventions (ROBINS-I) tool. 14 Any discrepancies were resolved through discussion with fourth authors (SD) to achieve consensus. The findings were visually depicted through traffic light plots and summary plots using the robvis online tool. 15
Data Extraction
Data were extracted from the included studies and collated into a standardized proforma. The extracted data, comparing the 2 approaches, encompassed study characteristics, patient demographics, implant types, PROMs, ROM, implant revisions, complications, and duration of follow up.
Data Synthesis and Statistical Analysis
We utilized Cochrane Review Manager (RevMan) v5.4 for conducting meta-analysis calculations and generating forest plots. In cases where data extracted from the included studies were incomplete, efforts were made to reach out to the original corresponding authors for any missing information.
For the meta-analysis of PROMs, we employed the standardized mean difference (SMD) and 95% confidence intervals (CIs) to enable the pooling of various reported outcomes. Mean difference (MD) was employed for analyzing ROM, while relative risk (RR) was used to analyze categorical data for revision and complications. In each analysis, a random-effect model was applied. Statistical significance was defined as P < .05.
To evaluate study heterogeneity, we utilized the I2 statistic. An I2 value of zero indicated perfect homogeneity among the data from the included studies, while an I2 closer to 100% indicated significant heterogeneity among the studies.
Results
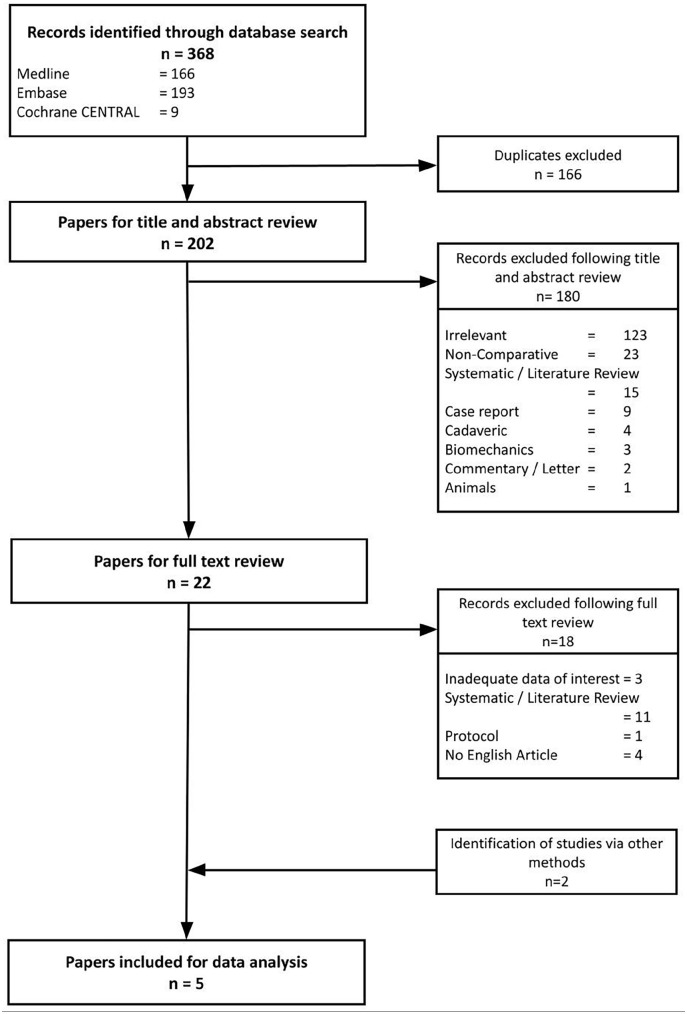
Following the initial literature search and removal of duplicate results, we identified 202 individual studies. After applying our eligibility criteria, conducting title and abstract screening, and completing the final full-text review, 5 studies were deemed eligible for inclusion in this study.16 -20 The process is illustrated in the PRISMA flowchart, depicted in Figure 1.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart.
Table 1 delineates the particulars of each study. In total, 302 patients (310 implants) were included, with sample sizes varying from 32 to 100 patients, and follow-up durations ranging from 1 month to 5 years.
Table 1.
Characteristics of the Included Studies.
| Study / method | Age (years) | Total patients, n= | Type of approach | Total implant, n = | Type of implants | Reported outcome of interest | Follow up |
|---|---|---|---|---|---|---|---|
| Heren 19 Prospective | 65.7 (51-79) | 38 | Volar | 38 | Swanson Silicone | ROM | 28.2 months (SD 16.1) |
| 65 (49-75) | Dorsal | 21 | 51.4 months (SD 22.4) | ||||
| Natera 17 Retrospective | 56 | 66 | Volar | 8 | Avanta Silicone | ROM | 29 months |
| Dorsal (Lluch modification of Chamay) | 14 | ||||||
| Van Nuffel 20 Retrospective | 59.5 (39-80) | 32 | Volar | 17 | Swanson Silicone | DASH, ROM | Not specified |
| 60 (45-71) | Dorsal (Chamay) | 24 | Ascension PyroCarbon | ||||
| Bodmer 18 Prospective | 66 (SD 11) | 100 | Volar | 42 | CapFlex-PIP Metal-on-poly | MHQ, ROM | 2 years |
| Dorsal (Chamay) | 37 | ||||||
| Dorsal (Tendon splitting) | 21 | ||||||
| Tranchida 16 Retrospective | 64.2 (SD 11.8) | 66 | Volar | 45 | Silicone, Pyrocarbon, Metal-on-poly | ROM | 132 days (30-365) |
| Dorsal | 43 | Silicone, Pyrocarbon |
Data are presented as n, mean (range) or mean (SD) unless otherwise indicated.
Abbreviations: DASH, disabilities of arm, shoulder and hand; MHQ, Michigan Hand Questionnaire; ROM, range of motion.
Risk of Bias
The authors’ judgment assessing studies’ quality and risk of bias is demonstrated in Supplemental Appendix 3. In summary, 4 studies were classified as having a low risk of bias, while the remaining one was categorized as moderate risk.
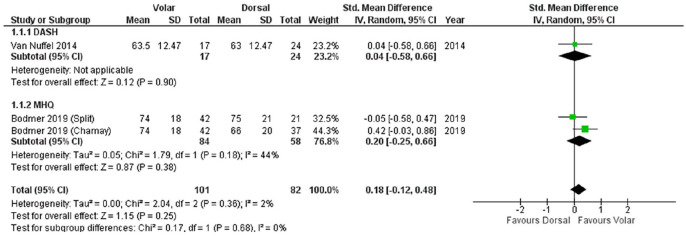
PROMs
Two studies, Van Nuffel 2014 and Bodmer 2019, utilized PROMs as their outcome measures, specifically the DASH score and MHQ, respectively.18,20 Postoperatively, no significant differences between the 2 approaches were observed (SMD 0.18; 95% CI −0.12, 0.48; P = .25; I2 2%), as illustrated in Figure 2.
Figure 2.
Forest plot of the comparison between 2 approaches for PROMs.
DASH, Disabilities of the Arm, Shoulder, and Hand; MHQ, Michigan Hand Outcomes Questionnaire; PROMs, patient reported outcome measures.
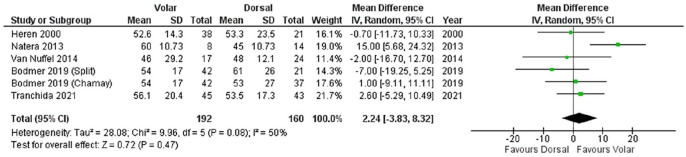
ROM
ROM was assessed as an outcome measure in 5 studies.16 -20 Postoperatively, no significant differences between the 2 approaches were found (MD 2.24; 95% CI −3.83, 8.32; P = .47; I2 50%) (Figure 3).
Figure 3.
Forest plot of the comparison between 2 approaches for ROM.
ROM, range of motion.
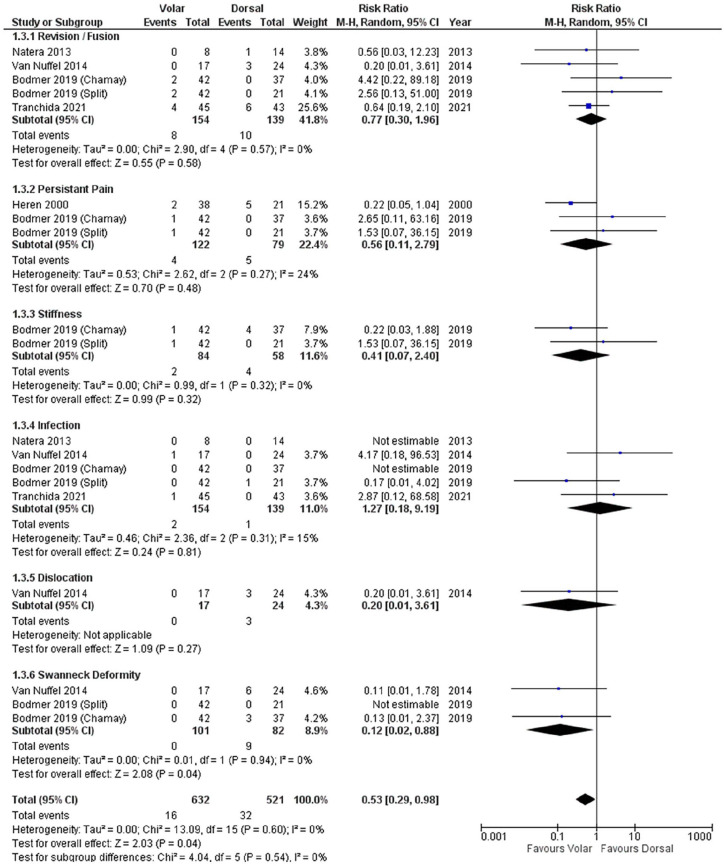
Revision and Complication
Four studies provided data on the revision of implants to either new implants or arthrodesis.16 -18,20 There was no difference in relative risk between the 2 approaches (RR 0.77; 95% CI 0.30, 1.96; P = .58; I2 0%).
We analyzed 5 common complications reported by the included studies, namely persistent pain, stiffness, infection, dislocation, and swan-neck deformity. There were no statistically significant differences in relative risk between both approaches regarding persistent pain, stiffness, infection, and dislocation postoperatively. Dorsal approach was shown to have higher risk of developing swan-neck deformity (9 out of 82 implants) postoperatively compared to volar approach (0 out of 101 implants) (RR 0.12; 95% CI 0.02, 0.88; P = .04; I2 0%) (Figure 4).
Figure 4.
Forest plot of the comparison between 2 approaches for revision and complications.
Discussion
Our study aimed to assess the outcomes of PIPJ replacement, specifically comparing the dorsal and volar approaches. Our analysis revealed no significant differences between the 2 approaches in terms of PROMs, ROM, revision rates, and common postoperative complications. However, it is noteworthy that the dorsal approach exhibited a slightly higher risk of developing swan-neck deformity compared to the volar approach.
The dorsal approach remains the predominant technique for PIPJ replacement, primarily due to its technical simplicity and favorable access to the joint. Furthermore, the majority of current implant instrumentation systems are designed to facilitate this approach. 8 However, recent publications have highlighted the promising outcomes associated with the volar approach.21 -23 Advocates of the volar approach suggest that it preserves the extensor mechanism, enabling early postoperative rehabilitation to prevent complications such as adhesions, extensor lag, and joint contracture.8,9 Despite these theoretical advantages, our meta-analysis did not detect a statistically significant difference in postoperative range of motion between the 2 approaches. This may be attributed to advancements in surgical techniques, implant designs, and tailored rehabilitation strategies for each approach.
Yamamoto et al 9 conducted a systematic review examining various implants and approaches for PIPJ replacement. Their analysis of 40 studies suggested that silicone implants with the volar approach yielded the best ROM outcomes with fewer complications compared to other implant designs and surgical approaches. Although their review provided valuable insights, limitations such as limited data and inability to perform meta-analysis for each subcategory combination of implant and approach were acknowledged. In contrast, our study focused specifically on comparing the dorsal and volar approaches, allowing for a more detailed and focused analysis. Our findings complement Yamamoto et al's work by providing additional evidence regarding the comparative effectiveness and safety profiles of these 2 approaches.
The findings of this systematic review provide essential insights for surgeons performing PIPJ replacement. Both dorsal and volar approaches demonstrate comparable safety and efficacy in terms of surgical complications and functional outcomes, which underscores the importance of a personalized approach in surgical planning. Surgeons can confidently select the approach based on individual patient anatomy, specific details of the joint pathology, and their own surgical experience without compromising the outcomes.
Our study is not without limitations. Firstly, the retrospective nature of the included studies introduces inherent biases that may impact the reliability of our results. Additionally, the heterogeneity among the studies, including variations in patient populations, preoperative deformities, surgical techniques, surgeon experience, implant usage, and reported outcome measures, may limit the comparability of our findings. Furthermore, the relatively short follow-up durations in some patients may not capture long-term outcomes and complications associated with PIPJ replacement. Lastly, the limited number of studies available for inclusion may restrict the breadth of our analysis and the generalizability of our findings. These limitations underscore the need for further prospective studies with standardized protocols to elucidate the optimal approach for PIPJ replacement.
Conclusion
Our comparative analysis of dorsal and volar approaches for PIPJ replacement revealed no significant differences in patient’s outcome. To validate these findings and overcome the limitations of our study, it is imperative to conduct prospective studies with standardized protocols and extended follow-up periods. Future research should prioritize examining outcomes beyond the immediate postoperative phase and investigating how various implant designs and surgical techniques influence long-term functional outcomes and complication rates. Establishing a national registry database and fostering collaboration among medical centers could facilitate this endeavor.
Supplemental Material
Supplemental material, sj-docx-1-han-10.1177_15589447241284670 for Dorsal and Volar Approaches for Proximal Interphalangeal Joint Replacement: Comparing Outcomes Through Systematic Review and Meta-Analysis by Gagandeep Mahi, Eric Ansong, Eugene Gan, Sasan Dehbozorgi and Han Hong Chong in HAND
Supplemental material, sj-docx-2-han-10.1177_15589447241284670 for Dorsal and Volar Approaches for Proximal Interphalangeal Joint Replacement: Comparing Outcomes Through Systematic Review and Meta-Analysis by Gagandeep Mahi, Eric Ansong, Eugene Gan, Sasan Dehbozorgi and Han Hong Chong in HAND
Supplemental material, sj-tif-1-han-10.1177_15589447241284670 for Dorsal and Volar Approaches for Proximal Interphalangeal Joint Replacement: Comparing Outcomes Through Systematic Review and Meta-Analysis by Gagandeep Mahi, Eric Ansong, Eugene Gan, Sasan Dehbozorgi and Han Hong Chong in HAND
Supplemental material, sj-tif-2-han-10.1177_15589447241284670 for Dorsal and Volar Approaches for Proximal Interphalangeal Joint Replacement: Comparing Outcomes Through Systematic Review and Meta-Analysis by Gagandeep Mahi, Eric Ansong, Eugene Gan, Sasan Dehbozorgi and Han Hong Chong in HAND
Acknowledgments
The authors would like to thank Pip Divall, Clinical Librarian of University Hospital of Leicester NHS Trust, United Kingdom for her assistance in conducting literature search for this meta-analysis.
Footnotes
Ethical Approval: Ethical approval is not required for this article.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent is not required for this article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Gagandeep Mahi  https://orcid.org/0000-0001-6487-4805
https://orcid.org/0000-0001-6487-4805
Han Hong Chong  https://orcid.org/0000-0003-0102-2167
https://orcid.org/0000-0003-0102-2167
Supplemental material is available in the online version of the article.
References
- 1. Dahaghin S, Bierma-Zeinstra SMA, Ginai AZ, Pols HAP, Hazes JMW, Koes BW. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study). Ann Rheum Dis. 2005;64(5):682-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Snyder EA, Alvarez C, Golightly YM, Renner JB, Jordan JM, Nelson AE. Incidence and progression of hand osteoarthritis in a large community-based cohort: the Johnston County osteoarthritis project. Osteoarthritis Cartilage. 2020;28(4):446-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eaton CB, Schaefer LF, Duryea J, et al. Prevalence, incidence, and progression of radiographic and symptomatic hand osteoarthritis: the osteoarthritis initiative. Arthritis Rheumatol. 2022;74(6):992-1000. [DOI] [PubMed] [Google Scholar]
- 4. Pellegrini VD, Burton RI. Osteoarthritis of the proximal interphalangeal joint of the hand: arthroplasty or fusion? J Hand Surg Am. 1990;15(2):194-209. [DOI] [PubMed] [Google Scholar]
- 5. Murray PM. Prosthetic replacement of the proximal interphalangeal joint. Hand Clin. 2006;22(2):201-206. [DOI] [PubMed] [Google Scholar]
- 6. Swanson AB. Silicone rubber implants for replacement of arthritis or destroyed joints in the hand. Surg Clin North Am. 1968;48(5):1113-1127. [DOI] [PubMed] [Google Scholar]
- 7. Cook SD, Beckenbaugh RD, Redondo J, Popich LS, Klawitter JJ, Linscheid RL. Long-term follow-up of pyrolytic carbon metacarpophalangeal implants. J Bone Joint Surg Am. 1999;81(5):635-648. [DOI] [PubMed] [Google Scholar]
- 8. Renfree KJ. Surgical approaches for proximal interphalangeal joint arthroplasty. Bone Joint J. 2022;104-B(12):1329-1333. [DOI] [PubMed] [Google Scholar]
- 9. Yamamoto M, Malay S, Fujihara Y, Zhong L, Chung KC. A systematic review of different implants and approaches for proximal interphalangeal joint arthroplasty. Plast Reconstr Surg. 2017;139(5):1139e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Merle M, Villani F, Lallemand B, Vaienti L. Proximal interphalangeal joint arthroplasty with silicone implants (NeuFlex) by a lateral approach: a series of 51 cases. J Hand Surg Eur Vol. 2012;37(1):50-55. [DOI] [PubMed] [Google Scholar]
- 11. Hage JJ, Yoe EPD, Zevering JP, De Groot PJM. Proximal interphalangeal joint silicone arthroplasty for posttraumatic arthritis. J Hand Surg Am. 1999;24(1):73-77. [DOI] [PubMed] [Google Scholar]
- 12. Adams J, Ryall C, Pandyan A, et al. Proximal interphalangeal joint replacement in patients with arthritis of the hand: a meta-analysis. J Bone Joint Surg Br. 2012;94(10):1305-1312. [DOI] [PubMed] [Google Scholar]
- 13. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Higgins J, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions 6.4. Cochrane, 2023. [Google Scholar]
- 15. McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55-61. [DOI] [PubMed] [Google Scholar]
- 16. Tranchida GV, Allen ST, Moen SM, Erickson LO, Ward CM. Comparison of volar and dorsal approach for PIP arthroplasty. Hand (N Y). 2021;16(3):348-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Natera L, Moya-Gómez E, Lamas-Gómez C, Proubasta I. Proximal interphalangeal joint replacement: a comparison between the volar and dorsal approach. Rev Esp Cir Ortop Traumatol. 2014;58(5):303-308. [DOI] [PubMed] [Google Scholar]
- 18. Bodmer E, Marks M, Hensler S, Schindele S, Herren DB. Comparison of outcomes of three surgical approaches for proximal interphalangeal joint arthroplasty using a surface-replacing implant. J Hand Surg Eur Vol. 2020;45(6):608-614. [DOI] [PubMed] [Google Scholar]
- 19. Herren DB, Simmen BR. Palmar approach in flexible implant arthroplasty of the proximal interphalangeal joint. Clin Orthop Relat Res. 2000;371(371):131-135. [DOI] [PubMed] [Google Scholar]
- 20. Van Nuffel M, Degreef I, Willems S, De Smet L. Proximal interphalangeal joint replacement: resurfacing pyrocarbon versus silicone arthroplasty. Acta Orthop Belg. 2014;80(2):190-195. [PubMed] [Google Scholar]
- 21. Proubasta IR, Lamas CG, Natera L, Millan A. Silicone proximal interphalangeal joint arthroplasty for primary osteoarthritis using a volar approach. J Hand Surg Am. 2014;39(6):1075-1081. [DOI] [PubMed] [Google Scholar]
- 22. Lautenbach M, Kim S, Berndsen M, Eisenschenk A. The palmar approach for PIP-arthroplasty according to Simmen: results after 8 years follow-up. J Orthop Sci. 2014;19(5):722-728. [DOI] [PubMed] [Google Scholar]
- 23. Bouacida S, Lazerges C, Coulet B, Chammas M. Proximal interphalangeal joint arthroplasty with Neuflex® implants: relevance of the volar approach and early rehabilitation. Chir Main. 2014;33(5):350-355. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-han-10.1177_15589447241284670 for Dorsal and Volar Approaches for Proximal Interphalangeal Joint Replacement: Comparing Outcomes Through Systematic Review and Meta-Analysis by Gagandeep Mahi, Eric Ansong, Eugene Gan, Sasan Dehbozorgi and Han Hong Chong in HAND
Supplemental material, sj-docx-2-han-10.1177_15589447241284670 for Dorsal and Volar Approaches for Proximal Interphalangeal Joint Replacement: Comparing Outcomes Through Systematic Review and Meta-Analysis by Gagandeep Mahi, Eric Ansong, Eugene Gan, Sasan Dehbozorgi and Han Hong Chong in HAND
Supplemental material, sj-tif-1-han-10.1177_15589447241284670 for Dorsal and Volar Approaches for Proximal Interphalangeal Joint Replacement: Comparing Outcomes Through Systematic Review and Meta-Analysis by Gagandeep Mahi, Eric Ansong, Eugene Gan, Sasan Dehbozorgi and Han Hong Chong in HAND
Supplemental material, sj-tif-2-han-10.1177_15589447241284670 for Dorsal and Volar Approaches for Proximal Interphalangeal Joint Replacement: Comparing Outcomes Through Systematic Review and Meta-Analysis by Gagandeep Mahi, Eric Ansong, Eugene Gan, Sasan Dehbozorgi and Han Hong Chong in HAND