Abstract
Background:
The cost of endoscopic carpal tunnel release (ECTR) has historically been shown to be significantly higher than the cost of open carpal tunnel release (OCTR). Setting and anesthetic technique drive costs in hand surgery; ambulatory surgical center (ASC) settings demonstrate lower costs when compared to hospital-based settings and local-only anesthetic techniques demonstrate savings over general anesthesia. The purpose of this study is to compare wide awake local-only anesthesia technique (WALANT) to monitored anesthetic care (MAC) for ECTR performed in an ASC setting.
Methods:
This study includes 481 ECTR under WALANT and 405 ECTR under MAC, performed between January 2019 and December 2021 in an ASC. Utilizing previously reported direct operating room costs, overhead, and material costs, we calculated a final cost for each procedure. We also report our complication rates: intraoperative conversion to OCTR and late revision to OCTR.
Results:
Intraoperative times were shortest for ECTR performed under WALANT (22 min) versus ECTR under MAC (25 min). The total cost for ECTR under WALANT was most cost-effective at $1341.28 versus ECTR under MAC at $1634.00. Both techniques demonstrated a low complication profile.
Conclusions:
Our intraoperative process flow, staffing model, and ASC setting resulted in cost savings making ECTR an economically feasible option.
Keywords: endoscopic carpal tunnel release, WALANT, ambulatory surgery center, time-driven activity-based costing
Introduction
Endoscopic carpal tunnel release (ECTR) and open carpal tunnel release (OCTR) have similar long-term patient outcomes. 1 However, ECTR patients return to work sooner, 2 have fewer major and minor complications, 3 and show lower postoperative narcotic utilization. 4 The one demonstrated downside to ECTR is its higher rate of revision surgery. 5 Open carpal tunnel releases are more commonly employed by practitioners; 86% of patients in a large Medicare Advantage cohort had OCTR versus ECTR. 6 At this point, the choice of carpal tunnel release technique is up to the individual practitioner in regard to efficacy and safety.
Cost analyses, on the other hand, have trended toward identifying OCTR as the more cost-effective option. At an academic medical center, ECTR was 43.9% more expensive than OCTR. 7 Kazmers et al found a 12.4- to 16.6-fold greater cost for ECTR under anesthesia (including Bier block, monitored anesthetic care (MAC) or general) relative to OCTR carried out in a procedure room without anesthesia or a tourniquet (wide awake local-only anesthesia technique (WALANT)). 8 An analysis utilizing the New York State All-Payer Database determined the following drivers of higher cost for carpal tunnel releases: general anesthesia, hospital outpatient setting, time in the operating room (OR), and ECTR. 9 In a large database study comparing Medicare and Humana patients, ECTR costs more than OCTR. 3
Koehler et al also identify intraoperative time as a major cost driver, and pose a challenge within its discussion: “In order to achieve cost neutrality between the 2 techniques for CTR, the duration of the endoscopic procedure would have to be decreased by 20.2 min.” 7 Wellington et al demonstrate these abbreviated operative times for ECTR performed utilizing WALANT; patients undergoing WALANT had faster procedure times (10 min ± 2 min), faster OR times (20 ± 3 min), and faster postanesthesia care unit times, resulting in overall faster door-to-door times (95 ± 21 min) than patients receiving anesthesia. 10
In our ambulatory surgical center (ASC) setting, we preferentially performed ECTR for patients with carpal tunnel. We hypothesized that our intraoperative times would meet the challenge posed by Koehler et al, resulting in economically feasible costs for ECTR in the ASC setting. The purpose of this study was to utilize the capacity cost rates and activity time published by Koehler et al, in combination with our institutional intraoperative process map, to approximate the relative cost of ECTR performed utilizing WALANT to ECTR utilizing MAC in an ASC. We monitored complication rates as a balance measure to ensure that technical differences did not result in worse outcomes.
Materials and Methods
We performed all included procedures at a private practice-owned ASC. The average turnover time between cases is 14.6 minutes. All procedures were completed by 1 of 4 fellowship-trained hand surgeons all equally proficient in ECTR, each averaging over 100 ECTRs per year, with a mean clinical experience of 8.75 ± 5.1 years. Either a certified surgical assistant (CSA), physician assistant (PA), or nurse practitioner (NP) participated in the entire intraoperative phase of care as surgical assists. Patients selected between WALANT and MAC anesthesia when no major comorbidities were present; however, elderly patients or those with significant comorbid risk factors were encouraged to have the procedure performed utilizing WALANT. Postoperative protocols did not change by surgical sedation approach.
Study Groups
A retrospective review of ECTR cases performed at the ASC identified 2 independent groups to perform the time-driven activity-based costing (TDABC) analysis. There were 1495 individual ECTR procedures performed between January 2019 and December 2021 as identified by the Current Procedural Terminology code (29848). Patients over the age of 18 were included. Bilateral carpal tunnel releases (n = 541), revision carpal tunnel procedures (n = 8), ECTR performed concurrent to another procedure (n = 41), and patients missing demographic or surgical time data (n = 19) were excluded. Patients with American Society of Anesthesiologist (ASA) score greater than 3 requiring sedation were not candidates for the ASC and were excluded. ASA was not an exclusionary category for surgery under WALANT. Patients on ambulatory oxygen were excluded from having surgery at the ASC. Patients on blood thinners were included; those on warfarin were asked to have an international normalized ratio <2.5 on the date of surgery, and other forms of blood thinners were not discontinued prior to the procedure. Patient characteristics including age, sex assigned at birth, body mass index, tobacco use, and payer class were collected. The final analysis included 481 ECTR under WALANT and 405 ECTR under MAC.
Surgical complications included intraoperative conversion to OCTR or subsequent revision surgery (OCTR at a later date). Conversion to OCTR intraoperatively was abstracted from operative notes. A separate analysis utilizing Current Procedural Terminology code 64721 for OCTR during the study period identified patients with 2 separate surgical dates, one of which was coded as on OCTR, and then a chart review of all patients meeting this criterion was performed.
Process Mapping
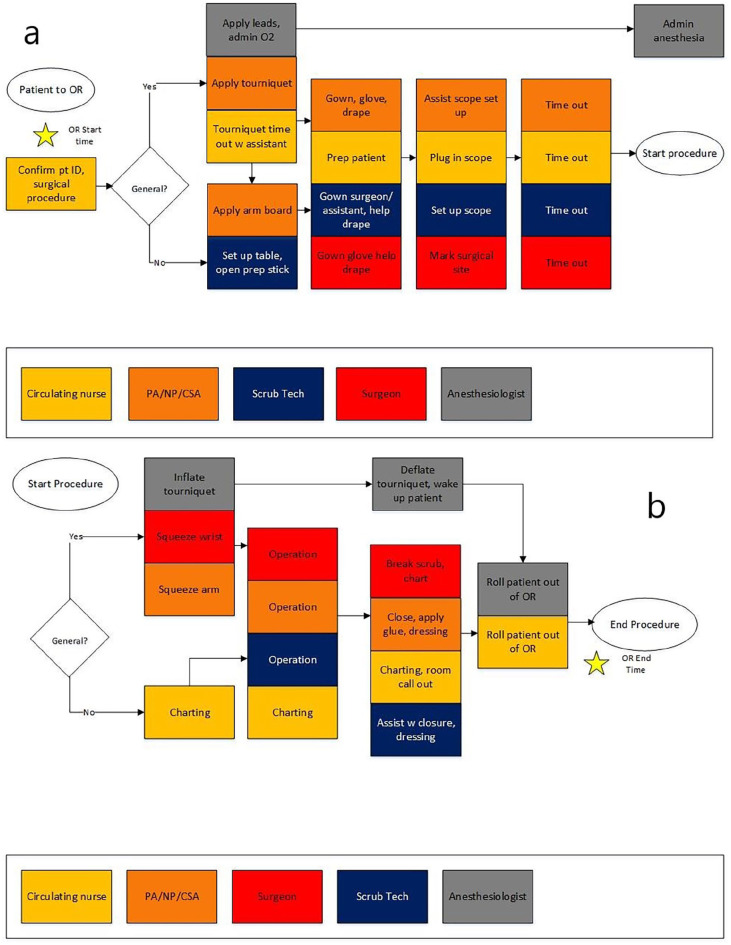
We reviewed the Koehler et al process map in detail and used it as a blueprint to create an intraoperative process map in our ASC. 8 Using the previously established modeling, we identified all regular personnel participating in each process step. Key points of divergence intraoperatively include the composition of staff in the OR (Figure 1). Mid-level providers were substituted for the Resident MD. Since we do not perform Bier blocks, the certified registered nurse anesthetist was omitted from the intraoperative environment. If required, preoperative nurses place the intravenous catheter. We did not include an anesthesiologist for patients in the WALANT group who were not sedated. We do not employ pharmacists, pharmacy techs, or anesthesia techs.
Figure 1.
Process maps delineating intraoperative care pathways between (a) patient enters OR to procedure start and (b) procedure start to end.
Note. Rectangles represent process steps, colors represent staff involved, and diamonds indicate decision nodes; OR, operating room; PA, physician assistant; NP, nurse practitioner; CSA, certified surgical assistant.
Time Estimates and Personnel Costs
To allow for direct comparison to the previously published study, we utilized the personnel costs reported, as opposed to utilizing our specific intuition and region reimbursement standards. Intraoperative times (patient in-room and out-of-room times) were abstracted from ASC charts for all patients included in the study. We obtained the average hourly salary band for our surgical assistants (CSAs/PAs/NP) from Human Resources and utilized this hourly rate to create a modifier compared to the per-minute rate reported for Orthopedic Residents, resulting in a modified Capacity Cost Rate ($/min) of 1.03. All other personnel costs were determined using previously published data.
Direct OR Cost
As per the previously published data, 7 direct OR costs were $12.99/min for ECTR calculated from the reported $582.12 in direct OR cost for ECTR.
Materials and Overhead
The previously published methods did not allow us to perform a comparable calculation of overhead as reported in their results ($1265 ECTR). 7 Instead, a per minute in the OR rate was used based on previously reported values of $28.24/min for ECTR. Material costs, excluding blades, were reported as $65 for ECTR. At our institution, we similarly used the MicroAire Smart Release Endoscopic Carpal Tunnel System (Charlottesville, VA), with our negotiated blade price of $95/blade versus $217/blade as reported. 7
Statistical Analysis
We did not perform a power analysis, as the primary outcome of interest was an economic analysis and no clinically relevant differences were sought. When indicated, student t-tests and ANOVA were used for continuous variables and chi-squared for categorical variables.
This study was approved by the IRB (Protocol #1858830).
Results
After exclusions, 886 procedures were included in the final analysis: 481 ECTR under WALANT and 405 ECTR under MAC (Table 1). There were significant differences between the groups with regard to age, sex, smoking status, and insurance, P < .01 (Table 1). Seven patients were converted intraoperatively from ECTR to OCTR in the WALANT group; 4 were converted to the MAC group. Five patients (2 WALANT and 3 MAC) required a revision OCTR at a later date due to incomplete release (Table 1).
Table 1.
Patient Characteristics and Surgical Complications for ECTR Under WALANT and ECTR Under MAC, Performed in an Ambulatory Surgery Center, 2019-2021 (N = 886).
| ECTR under WALANT (n = 481) |
ECTR under MAC (n = 405) |
P-value b | ||
|---|---|---|---|---|
| Age (M, SD) | 65.7 (14.1) | 54.9 (15.3) | <.001 | |
| Sex (n, %) | Female | 280 (58.2%) | 279 (68.1%) | .002 |
| Male | 201 (41.8%) | 129 (31.9%) | ||
| Body mass index (M, SD) | 31.6 (7.6) | 32.1 (7.1) | .34 | |
| Smoking status | Current | 41 (8.5%) | 62 (15.3%) | .005 |
| (n, %) | Former/never | 423 (87.9%) | 334 (82.5%) | |
| Unknown | 17 (3.5%) | 10 (2.2%) | ||
| Insurance category | Commercial | 130 (26.9%) | 137 (33.4%) | <.001 |
| (n, %) | Medicaid | 44 (9.1%) | 107 (26.1%) | |
| Medicare | 279 (58.0%) | 137 (33.8%) | ||
| Other a | 28 (5.8%) | 26 (6.4%) | ||
| Convert to open intraoperatively (n, %) | 7 (1.5%) | 4 (1.0%) | ||
| Revision due to incomplete release (n, %) | 2 (0.42%) | 3(0.73%) | ||
Note. ECTR, endoscopic carpal tunnel release; WALANT, wide awake local-only anesthetic no tourniquet; MAC, monitored anesthetic care; M, mean; SD, standard deviation; BMI, body mass index.
Includes workers compensation, automobile, and veteran’s administration.
Students t-test: age, BMI; ꭓ2: sex, smoking status, insurance category.
Intraoperative times were significantly shorter for ECTR under WALANT at 22 min (95% confidence interval [95% CI] [10-34]) versus ECTR under MAC at 25 min (95% CI [13-37]), P < .001 (Table 2). Based on the mean minutes spent in the OR, direct OR cost for ECTR under MAC was more expensive at $324.75 versus $285.78 under WALANT.
Table 2.
Average Elapsed Intraoperative Time (in Minutes) for ECTR Under WALANT and ECTR Under MAC in an Ambulatory Surgery Center, 2019-2021 (N = 886).
| ECTR under WALANT (n = 481) |
ECTR under MAC (n = 405) |
P-value | |
|---|---|---|---|
| Intraoperative time (min) (M ± SD) | 22 ± 6 | 25 ± 6 | <.001 a |
Note. ECTR, endoscopic carpal tunnel release; WALANT, wide awake local-only anesthetic no tourniquet; MAC, monitored anesthetic care; M, mean; SD, standard deviation.
Student t-test.
Intraoperatively, our process map identified that all 4 or 5 participating personnel were in the OR for the duration of the procedure given how short the procedure times were. Therefore, the average surgical times for WALANT and MAC were applied across the personnel types (Figure 1). Table 3 compares intraoperative personnel costs for ECTR with WALANT and MAC and the intraoperative results reported previously by Koehler et al. ECTR under WALANT personnel cost is $203.06, compared to ECTR under MAC at $353.25.
Table 3.
Intraoperative Labor Costs for ECTR Under WALANT and ECTR Under MAC Compared to ECTR and OCTR From Koehler et al, 7 Performed in an Ambulatory Surgical Center, 2019-2021 (N = 886).
| Current study groups | Koehler et al 7 comparison a | ||||
|---|---|---|---|---|---|
| Personnel group | Capacity cost rate a ($/min) | ECTR under WALANT (n = 481) | ECTR under MAC (n = 405) |
Cost of ECTR | Cost of OCTR |
| Operative time (min) (M ± SD) | 22 ± 6 | 25 ± 6 | 45 ± 5 | 41 ± 7 | |
| Surgeon | $6.53 | $143.66 | $163.25 | $213.53 | $139.09 |
| Surgeon assist (PA/NP/CSA) | $1.03 | $22.66 | $25.75 | - | - |
| Resident physician | $0.86 | - | - | $49.36 | $45.92 |
| Anesthesiologist | $4.90 | - | $122.50 | $49.00 | $34.30 |
| Circulating nurse | $1.03 | $22.66 | $25.75 | $56.42 | $52.31 |
| Surgical technologist | $0.64 | $14.08 | $16.00 | $32.13 | $29.56 |
| CRNA | $1.03 | - | - | $71.84 | $67.73 |
| Total cost | $203.06 | $353.25 | $472.28 | $368.91 | |
Note. PA, physician assistant; NP, nurse practitioner; CSA, certified surgical assistant; CRNA, certified registered nurse anesthetist; ECTR, endoscopic carpal tunnel release; OCTR, open carpal tunnel release; WALANT, wide awake local-only anesthetic no tourniquet; MAC, monitored anesthetic care; M, mean; SD, standard deviation.
As reported by Koehler et al. 7
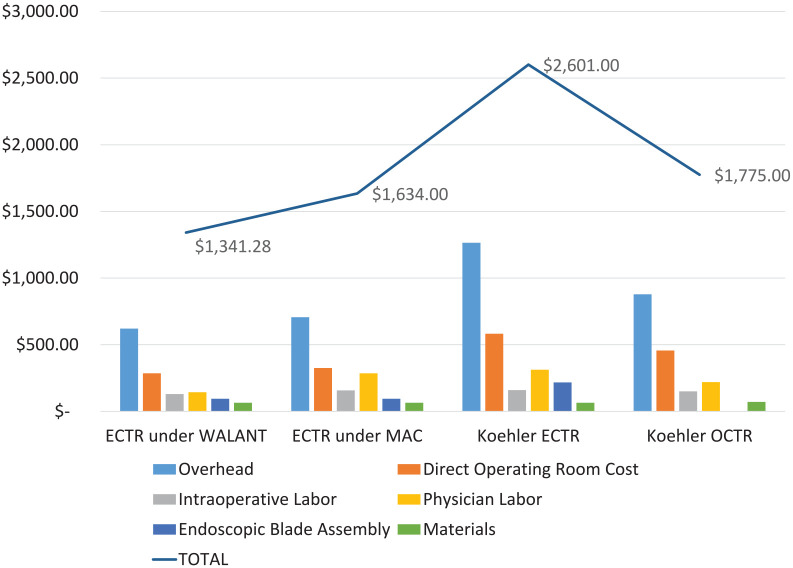
Utilizing previously published data for overhead, materials, and endoscopic blade assembly, final costs were calculated (Table 4, Figure 2). Endoscopic carpal tunnel release under WALANT was the most cost-effective at $1341.28.
Table 4.
Total Costs for ECTR Under WALANT and ECTR Under MAC Compared to ECTR and OCTR From Koehler et al, 7 Performed in an Ambulatory Surgical Center, 2019-2021 (N = 886).
| Costs | ECTR under WALANT | ECTR under MAC | Koehler ECTR | Koehler OCTR |
|---|---|---|---|---|
| Overhead | $621.28 | $706.00 | $1265.00 | $878.00 |
| Direct operating room cost | $286.00 | $325.00 | $582.00 | $457.00 |
| Intraoperative labor | $130.00 | $157.00 | $160.00 | $150.00 |
| Physician labor | $144.00 | $286.00 | $312.00 | $219.00 |
| Endoscopic blade assembly | $95.00 | $95.00 | $217.00 | $0 |
| Materials | $65.00 | $65.00 | $65.00 | $71.00 |
| Total | $1341.28 | $1634.00 | $2601.00 | $1775.00 |
Note. ECTR, endoscopic carpal tunnel release; OCTR, open carpal tunnel release; WALANT, wide awake local-only anesthetic no tourniquet; MAC, monitored anesthetic care.
Figure 2.
Total costs for ECTR under WALANT and ECTR under MAC compared to previously published total cost for ECTR and OCTR from Koehler et al. 7
Note. ECTR, endoscopic carpal tunnel release; WALANT, wide awake local-only anesthetic no tourniquet; MAC, monitored anesthetic care; OCTR, open carpal tunnel release.
Discussion
We realized total cost savings of 18% for ECTR performed utilizing WALANT when compared to ECTR with MAC. Despite 15% fewer patients in the MAC group, the total costs to the group during the 35-month period were $16 614.32 higher than the WALANT ECTR group. Physician labor and time in the OR primarily drove the cost difference between the groups, with the MAC group charged for an anesthesiologist’s time and for an additional 3 min on average in the OR (22 vs 25 min respectively). We report low complication rates (<1% revision rates) for both WALANT and MAC groups, demonstrating that WALANT technique did not increase the need for revision surgery.
Additionally, our process flow, staffing model, ASC environment, and WALANT technique, realized total cost savings for ECTR compared to the prior TDABC report. 7 Endoscopic carpal tunnel release performed utilizing a WALANT technique in an ASC setting represents a 48.4% cost saving over ECTR performed at an academic medical center ($1341.28 vs $2601.00). The primary driver of the cost savings is time in the OR, with an average OR time of 22 min for ECTR performed utilizing WALANT in the ASC versus 44.8 min for ECTR with general in the academic setting. Staffing also contributed to cost savings, with only one physician labor cost and a surgical assistant during the procedure to drive the majority of labor costs in this study. However, directly comparing an academic setting to a private practice omits the time and labor involved in training resident physicians.
Setting is also a major driver of cost when considering reimbursements. ASC facility fees are lower than hospital outpatient department (HOPD) fees. 11 Medicare calculates payments based on both the physician fee schedule and the outpatient prospective payment system. 11 Based on these calculations, ASC payments are lower than HOPD payments from Medicare, or, HOPD is more expensive to the system as a location for CTR. Utilizing the New York Statewide Planning and Research Cooperative System Database, total charges for HOPD were 48.2% higher than ASC charges. 9
The present study has limitations. Primarily, we did not include an OCTR group. We did, on initial analysis, evaluate our OCTR cases, but given our low volume of OCTR cases (<30 during the study period per group), we were unable to perform any meaningful statistical comparisons between the intraoperative times. We also do not currently perform OCTR in a procedure room.
Our study groups were not identical. Patients were older and more likely to be on Medicare for the WALANT group and there were more women in the MAC group. While patients were allowed to self-select the anesthesia technique, older patients and those with comorbidities were encouraged to have the procedure under WALANT. However, we do not believe that these demographic differences directly affect the results of this work.
We did not directly cost our nonpersonnel expenses (eg, draping, institutional OR time cost, blade cost, etc). This was intentional, as we wanted to address costs that are modifiable between institutions. Contract negotiations, regional variability, and availability of materials are not directly comparable. We utilized prior data to estimate our “direct OR costs” again demonstrating significant savings related directly to saving time in the OR. In addition, we utilized the previously published personnel costs. Overhead was an estimate based on OR time, and certainly would be different if calculated directly based on the ASC setting, but it is reasonable to assume that ASC overhead is lower than the hospital setting. We did not specifically examine the added cost of conversion from ECTR to OCTR given the low rate of conversion (1.2%), as this is unavoidable and our rate for conversion was low.
In addition, we focused on our intraoperative process map, as opposed to the entire continuum of care. We chose this focus for 2 important reasons: (1) as stated by Koehler et al, time in the operative suite drives cost; and (2) intraoperative processes are modifiable by the surgeons (techniques and intraoperative personnel) whereas pre- and postoperative processes are deeply embedded in the setting of care and represent less of an opportunity for surgeons to directly implement cost savings at their institution.
Future studies include analysis of the bilateral ECTR, which was excluded from this study in order to allow for direct comparison to previous work. Given the cost savings incurred with our current process, along with the omission of an additional trip to the operating for bilateral ECTR, even more cost savings are likely achieved.
The authors intend this to be a concept paper along with an economic analysis. The results indicate that the ASC setting for ECTR results in a cost comparable to OCTR performed in an OR, regardless of anesthesia type employed (MAC vs WALANT). Having the surgeon perform blocks, limiting personnel in the OR, and achieving a short operating time with an efficient ECTR technique is applicable across settings. Regarding costs, prior studies suggest a specific cost threshold for ECTR to be viable, a threshold that previous work could not substantiate. Our study, encompassing a significant number of cases in an ASC setting, utilizing both MAC and WALANT techniques, successfully met these economic criteria. Our results demonstrate the economic feasibility of ECTR in an ASC setting as outlined in our process map.
Acknowledgments
We thank Kate Spitzley, PhD, for manuscript preparation. We thank Taylor Rezell, Scott Cordell, Hannah Grunwald, and William Potwora for their assistance with data collection.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was not needed from all individual participants included in the study.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
This study was approved by the PeaceHealth System IRB, Eugene, OR, USA (Protocol # 1858830).
ORCID iD: Jenna M. Godfrey  https://orcid.org/0000-0003-0568-7203
https://orcid.org/0000-0003-0568-7203
References
- 1. Hacquebord JH, Chen JS, Rettig ME. Endoscopic carpal tunnel release: techniques, controversies, and comparison to open techniques. J Am Acad Orthop Surg. 2022;30(7):292-301. [DOI] [PubMed] [Google Scholar]
- 2. Miles MR, Shetty PN, Bhayana K, Yousaf IS, Sanghavi KK, Giladi AM. Early outcomes of endoscopic versus open carpal tunnel release. J Hand Surg Am. 2021;46(10):868-876. doi: 10.1016/j.jhsa.2021.04.030 [DOI] [PubMed] [Google Scholar]
- 3. Devana SK, Jensen AR, Yamaguchi KT, et al. Trends and complications in open versus endoscopic carpal tunnel release in private payer and Medicare patient populations. Hand (N Y). 2019;14(4):455-461. doi: 10.1177/1558944717751196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aultman H, Roth CA, Curran J, et al. Prospective evaluation of surgical and anesthetic technique of carpal tunnel release in an orthopedic practice. J Hand Surg Am. 2021;46(1):69.e1-669.e7. doi: 10.1016/j.jhsa.2020.07.023 [DOI] [PubMed] [Google Scholar]
- 5. Carroll TJ, Dussik CM, Clary Z, Hoffman S, Hammert W, Mahmood B. Endoscopic versus open carpal tunnel surgery: risk factors and rates of revision surgery. J Hand Surg Am. 2023;48(8):757-763. doi: 10.1016/j.jhsa.2023.05.002 [DOI] [PubMed] [Google Scholar]
- 6. Zhang S, Vora M, Harris AH, Baker L, Curtin C, Kamal RN. Cost-minimization analysis of open and endoscopic carpal tunnel release. J Bone Joint Surg Am. 2016;98(23):1970-1977. doi: 10.2106/JBJS.16.00121 [DOI] [PubMed] [Google Scholar]
- 7. Koehler DM, Balakrishnan R, Lawler EA, Shah AS. Endoscopic versus open carpal tunnel release: A detailed analysis using time-driven activity-based costing at an academic medical center. J Hand Surg Am. 2019;44(1):62.e1-662.e9. doi: 10.1016/j.jhsa.2018.04.023 [DOI] [PubMed] [Google Scholar]
- 8. Kazmers NH, Presson AP, Xu Y, Howenstein A, Tyser AR. Cost implications of varying the surgical technique, surgical setting, and anesthesia type for carpal tunnel release surgery. J Hand Surg Am. 2018;43(11):971-977.e1. doi: 10.1016/j.jhsa.2018.03.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brodeur PG, Raducha JE, Patel DD, Cruz AI, Jr, Gil JA. Cost drivers in carpal tunnel release surgery: an analysis of 8,717 patients in New York State. J Hand Surg Am. 2022;47(3):258-265.e1. doi: 10.1016/j.jhsa.2021.10.022 [DOI] [PubMed] [Google Scholar]
- 10. Wellington I, Cusano A, Ferreira JV, Parrino A. WALANT technique versus sedation for endoscopic carpal tunnel release. Hand (N Y). 2023;18(2):214-221. doi:15589447211003180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Payment Variations across Outpatient Sites of Service [press release]. American Medical Association. 2023. [Google Scholar]