Abstract
Study Design
Retrospective case series study.
Objectives
This study aimed to evaluate the clinical efficacy of TARP technique for treating IAAD caused by old odontoid fracture and assess the outcomes of patients who underwent TARP technique over 2 years of follow-up.
Methods
Between January 2005 and September 2017, 56 patients with IAAD caused by old odontoid fractures were treated with TARP technique. Patients’ clinical, radiological, and surgical data were retrospectively analyzed. Radiological parameters included the atlantodental interval (ADI) and the space available for the spinal cord (SAC) were measured. Occipitocervical pain levels and neurologic status were evaluated with Visual Analog Scale (VAS) and Japanese Orthopaedic Association (JOA) score respectively. Degree of cervical dysfunction was assessed by Neck Disability Index (NDI). Fusion status was evaluated by images during the follow-ups.
Results
Surgeries for 56 cases were performed successfully with no injury to the spinal cord, nerve, or blood vessels. All patients achieved satisfactory reduction and fixation. Clinical symptomatic relief was obtained in all cases (100%). Patients were followed up for an average of 33.9 ± 9.6 months (ranged 24-60 months). Improvements in the postoperative ADI, SAC, VAS, JOA score and NDI were significant (P < .05). Besides, Bone fusion was observed in all patients. No hardware failure or re-dislocation occurred during the follow-up period.
Conclusions
TARP technique is an effective procedure for the treatment of IAAD caused by old odontoid fracture, which can achieve complete release, satisfactory decompression, reduction and fixation, and reliable bone fusion through a single transoral approach.
Keywords: transoral approach, atlantoaxial dislocation, old odontoid fracture, arthrodesis, internal fixation, spinal fusion
Introduction
Odontoid fractures can destroy the stability of the atlantoaxial complex and lead to atlantoaxial dislocation. Moreover, scar and osteophyte formation after odontoid fracture can lead to irreducible atlantoaxial dislocation (IAAD). In clinical situations, anterior release, followed by posterior atlantoaxial fixation, has been commonly performed for this disease.1,2 Although the combined anterior-posterior approach can achieve satisfactory reduction and cord decompression, it will increase surgical injuries and operative time. Additionally, the risk of spinal cord injury is increased when performing posture conversion with an extremely unstable atlantoaxial joint after anterior release. 3 Transoral atlantoaxial reduction plate (TARP) technique, as a simple anterior approach procedure, retains the previous functionality of anterior tissue release and posterior fixation while reducing the steps of changing positions and incisions. Therefore, in order to investigate the clinical effect of TARP operation in the treatment of IAAD caused by odontoid fractures, we performed 56 cases using this technique through a single transoral approach, then collected and analyzed the relevant data of these cases.
Patients and Methods
Patients
From January 2005 to September 2017, 56 patients (26 men and 30 women) with IAAD caused by old odontoid fractures were included. The average age was 41.8 ± 10.2 years and the average injured history was 24.7 ± 13.7 months. The causes of injury include fall injury (28 cases), sports-related injury (9 cases), and motor vehicle accident (19 cases). All patients were followed up for at least 2 years (range 24-60 months). Our study received ethical approval from our hospital’s ethics committee (2024012), and all patients provided informed consent. Detailed information on all 56 patients presented in the supplemented Table. We categorized old odontoid fractures according to the classification system of Anderson and D’Alonzo. 4 The detailed patient characteristics are summarized in Table 1. The clinical presentations of all 56 subjects admitted to our hospital are presented in Table 2.
Table 1.
Demographic and Clinical Data.
| Demographics | |
|---|---|
| Gender (male/Female) | 26/30 |
| Age (Years) | 41.8 ± 10.2 |
| Cause of injury | |
| Fall injury | 28 |
| Sports related injury | 9 |
| Motor vehicle accident | 19 |
| Type of odontoid fracture | |
| Type Ⅱ a | 24 |
| Type Ⅲ a | 32 |
| Instability (Yes/No) | 56/0 |
| Neurological deficit (Yes/No) | 56/0 |
| Operative time (min) | 205.3 ± 37.1 |
| Blood loss | 89.9 ± 28.6 |
| Follow-up (months) | 33.9 ± 9.6 |
| Bony fusion (months) | 5.9 ± 2.3 |
| Complications | |
| Pulmonary infection | 2 |
| Pharyngeal foreign body sensation | 5 |
| Screw misplacement | 3 |
aType of odontoid fracture according to the classification system of Anderson and D’Alonzo.
Table 2.
Pre-and Postoperative Clinical Symptoms.
| Clinical Symptoms | Preoperative No. (%) | Postoperative Improvement No. (%) |
|---|---|---|
| Occipitocervical pain | 56 (100%) | 56 (100%) |
| Extremity numbness | 44 (78.6%) | 38 (86.4%) |
| Extremity weakness | 36 (64.3%) | 33 (91.7%) |
| Unsteady gait | 20 (35.7%) | 20 (100%) |
| Hemiparalysis | 7 (12.5%) | 7 (100%) |
Each patient may have 1 or more symptoms.
Indications of Surgical Choice
All of the patients underwent skull traction of 4-12 kg for 1 week preoperatively, even under general anesthesia during surgery. The atlantoaxial longitudinal dislocation of all cases reduced less than 50% after traction. Combined with preoperative X-rays and CT scans, these were used as the diagnostic basis for IAAD. 5 Preoperative examination excluded any patient who had contraindications to the transoral approach such as oral infection. During this period, the above indications were strictly used to select surgical procedures with no selection bias in our department.
Surgical Techniques
Preoperative Examinations
Standard anteroposterior and lateral X-rays plus flexion and extension films, three-dimensional computed tomography (CT), and magnetic resonance imaging (MRI) were performed on the upper cervical spine of all patients, showing that every case had a history of odontoid fracture, forward displacement of the odontoid processes and atlas, retained facet joint, whereas no bone fusion exists. Extension views suggested no signs of atlantoaxial reduction for all cases. MRI showed obvious ventral spinal cord compression in all cases. After undergoing skull traction in a hyperextended position for 1 week, all patients had no signs of atlantoaxial reduction. The preoperative imaging parameters and evaluation indexes are shown in Table 3.
Table 3.
Pre-and Postoperative Assessment Data.
| Preoperative Value | Postoperative Value a | Final Follow-Up Value | P1 b | P2 b | P3 b | |
|---|---|---|---|---|---|---|
| ADI (mm) | 8.8 ± 1.8 | 1.6 ± 1.0 | / | 0.000 | / | / |
| SAC (mm) | 9.2 ± 1.5 | 15.5 ± 1.6 | 15.4 ± 1.6 | 0.000 | 0.000 | 0.567 |
| JOA score | 11.8 ± 1.8 | 14.3 ± 1.6 | 16.1 ± 1.1 | 0.000 | 0.000 | 0.000 |
| VAS score | 3.8 ± 1.0 | 1.5 ± 0.6 | 0.2 ± 0.4 | 0.000 | 0.000 | 0.000 |
| NDI (%) | 44.8 ± 15.9 | 31.1 ± 12.7 | 6.5 ± 5.7 | 0.000 | 0.000 | 0.000 |
Abbreviations: ADI, atlantodental interval; SAC, space available for the spinal cord; JOA, Japanese Orthopaedic Association; VAS, visual analog scale; NDI, Neck Disability Index.
P1, comparison of preoperative and postoperative values; P2, comparison of preoperative and final follow-up values; P3, comparison of postoperative and final follow-up values.
adata at 1 week after surgery.
bPaired-sample t test.
Surgical Procedure
The surgical technique has been described in detail by Yin et al.6-8 The main points are outlined here.
Preoperative preparations: An oral examination and dental cleaning were performed before surgery. 0.02% vinegar chlorhexidine was applied for oral cleaning 3-6 times per day for 3 days before surgery. Broad-spectrum antibiotics were administered intravenously 30 min before surgery.
Surgical techniques: The patient was placed in supine position with skull traction after undergoing general anesthesia with nasotracheal intubation. When we incised the posterior pharyngeal wall before, the oral cavity was washed and sterilized 3 times with hydrogen peroxide, iodophor disinfectant and normal saline. Then the posterior pharyngeal wall was incised, and the longus capitis and longus colli were separated to expose the anterior structure of the C1-C2. To release the atlantoaxial joint, hyperplastic scar tissue between the anterior arch of the atlas and odontoid process, osteotylus at the odontoid fracture gap, articular capsule and articular cartilage were resected (Figures 1A, 2A-2D and 3A). The distance between the entry points of the C1 lateral mass screw was measured to select an appropriate size TARP. Then, 2 screws were implanted bilaterally to the lateral mass of C1 to fix the TARP to the anterior surface of the atlas. A temporary reduction screw was inserted into the C2 vertebral body through the open slip section in the central part of the TARP (Figures 1B, 2E and 2F and 3B). The upper arm of a reduction forceps was installed to hold the crossbar of the TARP and the inferior arm hold the temporary reduction screw (Figures 1C, 2G and 3C). Lengthways reduction was performed by distraction of reduction forceps (Figure 1D and 1E), and the nut on top of the upper arm was turned to push the C1 backwards relative to C2 (Figure 1F and 1G, 2H and 3D), so the odontoid fracture was also reduced. After the reduction was confirmed to be satisfactory on intraoperative radiographs, retropedicle screws or vertebral screws were placed into C2 to solidly fix the TARP (Figures 1H, 2I and 3E). Then, the reduction forceps and temporary screw were removed (Figures 1I, 2J and 3F). After reducing and locking the TARP plate, we processed the autogenous bone taken from the anterior superior iliac spine into bone particles for grafting. Then bone particles were placed laterally on both sides of the lateral mass joint and atlantodont space (Figures 1J and 2K and 2L). Finally, the wound was closed in 2 layers: the muscular layer and the mucosal layer.
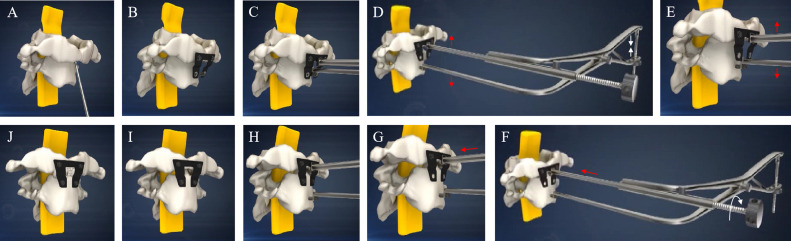
Figure 1.
Diagram of TARP technique. (A) Hyperplastic scar tissue and osteotylus were released. (B) A TARP plate was fixed on C1 using 2 anterior lateral mass screws, and then a temporary reduction screw was inserted into the C2 vertebral body. (C) A reduction forceps was installed to hold the crossbar of the plate and the temporary reduction screw. (D and E) The reduction forceps were distracted to upraise the C1. (F and G) The nut on top of the upper arm was turned to push the C1 backwards. (H) C2 screws were implanted. (I) The reduction forceps and a temporary reduction screw were removed. (J) Finally, bone grafting was performed.
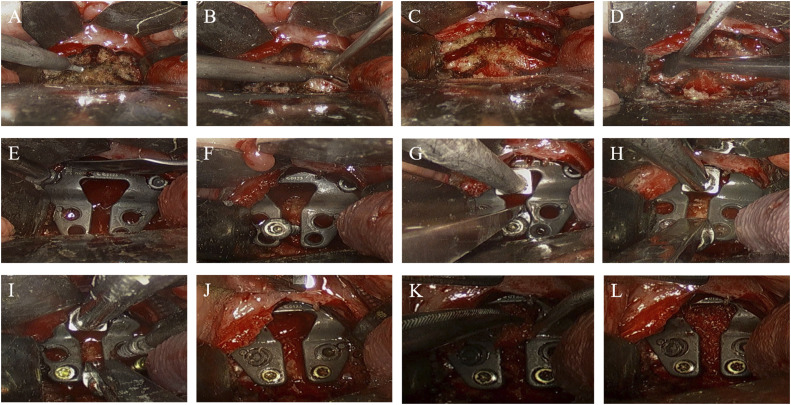
Figure 2.
Intraoperative TARP operation. (A) Hyperplastic scar tissue and osteotylus were released. (B and C) Articular capsule and articular cartilage of lateral mass joints were resected. (D) Lateral mass joints were levered to confirm complete release. (E) A TARP plate was fixed on C1 using 2 anterior lateral mass screws. (F) A temporary reduction screw was inserted into the C2 vertebral body. (G) A pair of reduction forceps was installed to hold the crossbar of the plate and the temporary reduction screw. (H) The reduction forceps were handled to upraise the C1 and push the C1 backwards. (I) Four C2 screws were placed to the fixed plate. (J) The reduction forceps and a temporary reduction screw were removed. (K and L) Autogenous bone was grafted in lateral mass joints and atlantodont space.
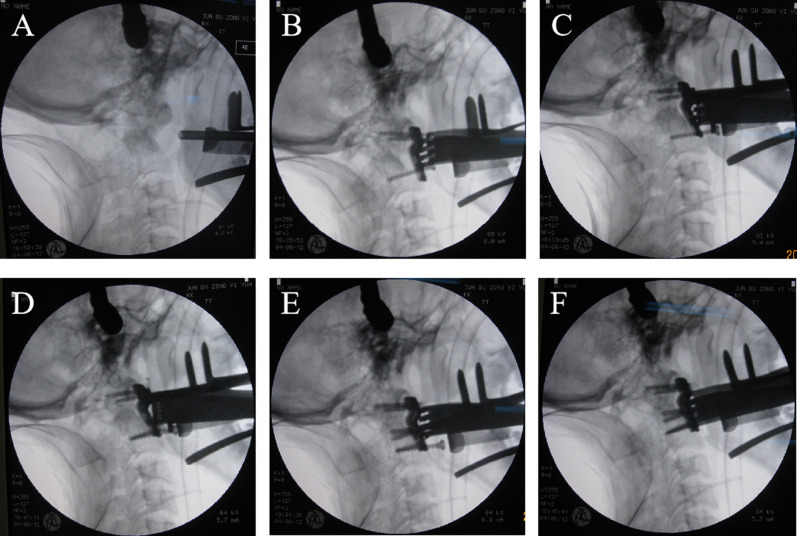
Figure 3.
Intraoperative fluoroscopy of TARP procedure. (A) Atlantoaxial dislocation was shown. (B) A TARP plate was fixed on C1 and a temporary reduction screw was inserted into the C2 vertebral body. (C and D) A pair of reduction forceps was installed to hold the crossbar of the plate and the temporary reduction screw, and the C1-C2 joint was reset after reduction procedure. (E) Four C2 screws were placed and the reduction forceps were removed. (F) The temporary reduction screw was pulled out.
Postoperative Management and Follow-up
The nasal trachea cannula was removed in 24-48 h postoperatively, and the nasogastric tube was removed according to the healing condition of the incision as determined by electronic laryngoscopy, as appropriate. Ultrasonic nebulisation and 0.02% chlorhexidine acetate gargling were performed 3-6 times per day for 7 days. Broad-spectrum antibiotics and anti-anaerobic drugs were administered introvenously for 3 consecutive days. The X-ray, CT scan and MRI scan were performed postoperatively. The ADI and SAC were measured after operation and during the follow-up. Neurologic function was evaluated based on the JOA scoring system, and the level of cervico-occipital pain was assessed by VAS score. The degree of cervical dysfunction was evaluated by NDIs. Redislocation, internal fixation failure and all possible complications such as neurovascular injury, infection, cerebrospinal fluid leak, pharyngeal foreign body sensation, and swallowing difficulty were recorded after surgery and during the follow-up. Bone fusion was confirmed by bone bridge formation on CT scan. All patients were asked to wear a rigid cervical collar for 3 months and were followed up at 3, 6, 9 and 12 months and then once per year or whenever needed (Figure 4).
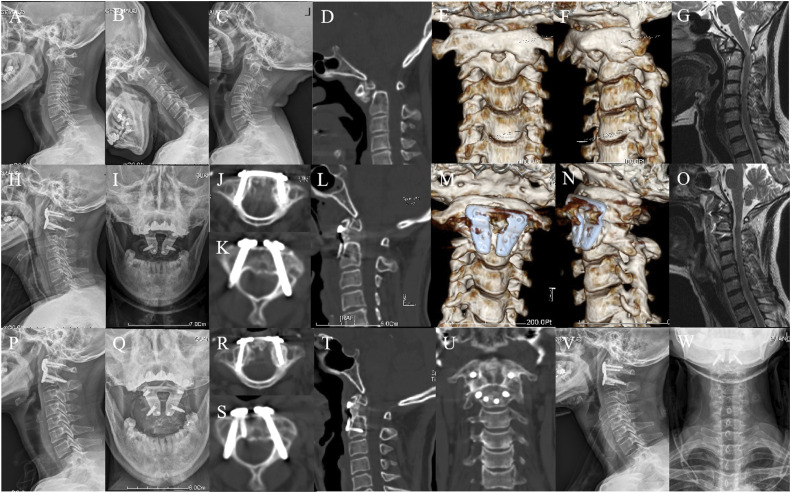
Figure 4.
A 51-year-old woman was diagnosed with atlantoaxial dislocation caused by old odontoid fracture. (A and C) Preoperative X-rays showed evidence of atlantoaxial dislocation. (D and F) CT scans and three-dimensional reconstruction showed atlantoaxial dislocation caused by old odontoid fracture, and osteotylus was formed between the anterior arch and the odontoid process. (G) MRI showed severe spinal cord compression. (H and I) Postoperative X-rays revealed satisfactory reduction of C1-C2 joint. (J-N) Postoperative CT scans and 3D reconstruction showed good screw placement and plate position. (O) Complete spinal decompression was found on postoperative MRI. (P-U) X-rays and CT scan from the 6 month follow-up showed stable internal fixation and bone fusion. (V and W) X-rays at the last follow-up showed good cervical spine sequences without recurrent dislocation or internal fixation failure.
Statistical Analysis
Statistical analysis was performed using the SPSS 23.0 software (IBM, Armonk, NY, USA). All data were subject to normal distribution based on K-S test and expressed as the mean and standard deviation. Student’s paired t test was used for statistical comparison of the data. A P value <.05 was considered statistically significant.
Results
The TARP technique was performed successfully in all 56 cases. The mean time of the procedure was 205.3 ± 37.1 minutes, with an average intraoperative blood loss of 89.9 ± 28.6 mL. Clinical symptoms were alleviated in all patients (Table 2).
Radiographic and Clinical Parameters
Postoperative X-rays, CT scans and MRI showed that anatomical atlantoaxial reduction and adequate spinal cord decompression were obtained in all patients. The preoperative ADI was significantly reduced postoperatively while the SAC was larger (P < .05). Both postoperative JOA score and NDIs were significantly higher compared to the preoperative scores (P < .05). In contrast, patients’ VAS scores were lower after surgery (P < .05). The average follow-up time was 33.9 ± 9.6 months. Compared with the preoperative score, the JOA score and NDIs were also higher while VAS score decreased significantly at final follow-up (P < .05). According to the equation: improvement rate in neurologic function = (postoperative JOA score - preoperative JOA score)/(17 - preoperative JOA score), the average improvement rate in neurologic function was 86.7% (ranged 62.5%-100%). Except ASC, all parameters at the last follow-up showed significant changes compared with the postoperative values, among which JOA score and NDIs increased, while VAS decreased (P < .05; Table 3).
Healing and Complication Status
All 56 patients received successful surgeries without incision infection complications. With postoperative pain relief interventions, extracorporeal drainage volume monitoring, and prophylactic antibiotics (routinely used in transoral surgery), patients recovered well after surgery. No complications related to the potential donor site were found during the follow-up period. Bone fusion was found in all patients on CT imaging at 3-9 months postoperatively as X-ray showed that there was a continuous bone bridge between C1 and C2. Two patients had pulmonary infections 1 week after surgery and were cured after anti-infection. Pharyngeal foreign body sensation occurred in 5 patients and disappeared 2 months after operation. CT scan revealed that 2 transoral C2 retropedicle screws and 1 anterior C1 lateral mass screw invaded the vertebral canal or foramen of the transverse process in 3 patients (Table 1). No redislocation, internal fixation failure or any other complication occurred during the perioperative and follow-up periods.
Discussion
IAAD Caused by Odontoid Fracture
Atlantoaxial dislocation commonly results in spinal cord compression, which can cause severe neurological impairment. Surgical management is often necessary for atlantoaxial dislocation, and reduction is the key event, especially for IAAD.9,10 Historically, surgical treatment of IAAD was usually performed through a single posterior approach which provides adequate stabilization but frequently incomplete reduction. Presently, it is generally believed that anterior or posterior release of C1-C2 joint is often necessary before reduction and fixation for IAAD.11-13
In our case series, all patients had a history of failed non-surgical therapy. They were externally immobilized just by rigid cervical collars or cephalo-cervico-thoracic orthoses. Because of the forward displacement of the skull, with the motion of cervical vertebra, the distal part of the odontoid fractures and atlas slide forward and down, thus forming atlantoaxial dislocation and spinal cord compression. 2 After the contracture of the anterior muscles, ligaments, and capsules of atlantoaxial joint, and the formation of scar and osteophytes, atlantoaxial dislocation becomes irreversible, which makes reduction difficult. The principal element affecting the reduction of these patients was the complete release of the callus such as the malunited odontoid process and facet joint. However, posterior procedure can not remove the anterior hyperplasia tissue and touch the odontoid fracture, thereby suggesting that, for the IAAD caused by odontoid fracture, anterior release is more advantageous than the posterior approach. Some scholars reported an anterior submandibular retropharyngeal approach for the release of C1-C2 joint. 1 However, this method can not fully reveal the atlantoaxial joint in a deeper location owing to obstruction of the lower jaw, 14 easily leading to inadequate release. Currently, the transoral approach is the most common approach used for anterior release in IAAD, because it can provide excellent exposure of the C1 and C2 segments and adequate release.7,15
Posterior Fixation vs TARP
Posterior atlantoaxial fixation was commonly performed after transoral release for IAAD in previous researches.2,11,12,15 In the cases of this study, spinal cord compression was mainly derived from the posterior margin of the fractured C2 body and the posterior arch of the C1. One shortcoming of the posterior approach is that it requires flexing the head during surgery to obtain adequate exposure to C1-C2, thereby risking more severe compression and fatal injury to the spinal cord. 2 Furthermore, the spinal cord might have been injured while in the transforming operative position after transoral release when the atlantoaxial joint was extremely unstable. 3
The transoral atlantoaxial reduction plate (TARP) system, designed by our institution in 2004, can perform direct anterior atlantoaxial fixation and fusion after transoral release, which can avoid additional posterior fixation, thus reducing surgical trauma, operative time and risk of spinal cord injury for IAAD.6,8 Moreover, compared with previous anterior atlantoaxial plates, TARP system has an advantage of intraoperative reduction mechanism, which can restore the physiological position of C1-C2.16,17 In our study, 56 patients with IAAD caused by old odontoid fracture were treated with TARP operation and were followed up to assess the efficacy of this technique. Imaging parameters such as ADI and SAC values during perioperative and the follow-up periods were significantly improved compared with those before operation. For clinical evaluation indicators as JOA score, VAS and NDI, there was also a similar trend of improvement. All patients achieved satisfactory reduction, decompression, fixation and fusion through a single transoral approach.
The atlantoaxial region has a high risk of screw placement due to its special structure and proximity to the high spinal cord and vertebral artery. In TARP operation, C1 is commonly fixed with anterior lateral mass screws. In the early stage, the C2 was fixed with a vertebral screw, which had poor fixation strength and was prone to internal fixation loosening. With the improvement of TARP strategies, for cases without pedicle variation or high-riding vertebral artery, transoral C2 retropedicle screws were applied, 18 which improved fixation strength but increased technical difficulty. Two transoral C2 retropedicle screws and 1 anterior C1 lateral mass screw in 3 patients appeared to be out of position in this study. Because these patients did not present any corresponding clinical symptoms, no intervention was performed.
A disadvantage of TARP operation is that transoral plate fixation increases the risk of wound infection. However, according to our experience of the application of this technique from 2004 to now, with proper preoperative preparation and postoperative care, the occurrence of this complication can be effectively prevented.8,19 Before the surgery, a detailed oral examination and repeated dental cleaning were performed to prevent infection. Intraoperatively, before the posterior pharyngeal wall was incised, the oral cavity was repeatedly and carefully sterilized to reduce local bacterial concentrations. Postoperative nasogastric tube feeding can reduce the contact of food and oral bacteria with the wound. Postoperative prophylactic application of broad-spectrum antibiotics and anti-anaerobic drugs can prevent infections. Continuous perioperative oral cleansing with 0.02% chlorhexidine vinegar (3 days preoperatively and 7 days postoperatively) changes the intraoral microenvironment and reduces the concentrations of pathogenic bacteria. The wound healing condition was checked by electronic laryngoscope at any time. These measures together form a defense barrier which significantly reduces the incidence of postoperative infection. None of the patients developed wound infection in current study. Although the foreign body sensation occurred in 5 patients and the pulmonary infection in 2 cases, those complications were eliminated by expectant treatment. No signs and symptoms of other surgery-related complications were found in this case series during the follow-up.
Limitations
Several limitations still exist in the current study. First, the present study is retrospective in nature and the grade of evidence needs to be improved; future prospective studies may better control for follow-up timing intervals and may have the potential to include more standardized outcome measures. Second, the sample size is still small, and research with a larger number of cases is needed in the future. In addition, due to the lack of a control group, it is difficult to demonstrate the superiority of the TARP technique over the prevalent posterior screw-rod fixation technique. Randomized controlled trials with control groups must be needed in the future to further evaluate this technique comprehensively.
Conclusions
The TARP operation is an effective, reliable, and safe operation for the treatment of IAAD caused by odontoid fracture. This technique can provide immediate reduction, fixation and fusion after release through a single transoral approach without the need for a posterior operation.
Supplemental Material
Supplemental Material for Transoral Atlantoaxial Reduction Plate (TARP) Technique for Treatment of Irreducible Atlantoaxial Dislocation (IAAD) Caused by Xiaobao Zou, Mandi Cai, Hanzhi Yang, Shuang Zhang, Chenfu Deng, Junlin Chen, Rencai Ma, Zexing Chen, Hong Xia, and Xiangyang Ma in Global Spine Journal
Author Contributions: Conceptualization: Xiangyang Ma, Xiaobao Zou, Hong Xia. Formal Analysis: Xiaobao Zou, Mandi Cai, Haozhi Yang, Shuang Zhang. Investigation: Xiaobao Zou, Mandi Cai, Rencai Ma, Junlin Chen, Zexing Chen. Methodology: Xiangyang Ma, Hong Xia, Xiaobao Zou, Mandi Cai, Chenfu Deng. Funding acquisitiony: Xiangyang Ma, Xiaobao Zou. Project Administration: Hong Xia, Xiangyang Ma. Writing – Original Draft: Xiaobao Zou, Mandi Cai. Writing – Review & Editing: Hong Xia, Xiangyang Ma, Xiaobao Zou, Mandi Cai.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funds from the National Natural Science Foundation of China (82272582) and the Natural Science Foundation of Guangdong Province (2023A1515011857).
Supplemental Material: Supplemental material for this article is available online.
Ethical Statement
Our institution certifies that this clinical retrospective study entitled “Computed Tomography Based Analysis of Anterior Fixations in Patients with Basilar Invagination”, performed by Xiaobao Zou, Mandi Cai et al had been examined by Ethical Review Committee of General Hospital of Southern Theatre Command of Peoples Liberation Army, People’s Republic of China (2024012).
ORCID iDs
Mandi Cai https://orcid.org/0000-0003-2581-4353
Hong Xia https://orcid.org/0000-0002-5324-9278
Xiangyang Ma https://orcid.org/0000-0001-7708-0246
References
- 1.Li C, Duan JZ, Li L. Anterior submandibular retropharyngeal odontoid osteotomy and posterior atlantoaxial fusion for irreducible atlantoaxial dislocation associated with odontoid fracture malunion. Eur Spine J. 2018;27(Suppl 3):292-297. [DOI] [PubMed] [Google Scholar]
- 2.Xu ZW, Liu TJ, He BR, Guo H, Zheng YH, Hao DJ. Transoral anterior release, odontoid partial resection, and reduction with posterior fusion for the treatment of irreducible atlantoaxial dislocation caused by odontoid fracture malunion. Eur Spine J. 2015;24(4):694-701. [DOI] [PubMed] [Google Scholar]
- 3.Yang JC, Ma XY, Xia H, Wu ZH, Ai FZ, Yin QS. Transoral anterior revision surgeries for basilar invagination with irreducible atlantoaxial dislocation after posterior decompression: a retrospective study of 30 cases. Eur Spine J. 2014;23(5):1099-1108. [DOI] [PubMed] [Google Scholar]
- 4.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56(8):1663-1674. [PubMed] [Google Scholar]
- 5.Wang SL, Wang C, Yan M, Zhou HT, Dang GT. Novel surgical classification and treatment strategy for atlantoaxial dislocations. Spine (Phila Pa 1976). 2013;38(21):E1348-E1356. [DOI] [PubMed] [Google Scholar]
- 6.Yin QS, Ai FZ, Zhang K, et al. Irreducible anterior atlantoaxial dislocation: one-stage treatment with a transoral atlantoaxial reduction plate fixation and fusion. Report of 5 cases and review of the literature. Spine (Phila Pa 1976). 2005;30(13):E375-E381. [DOI] [PubMed] [Google Scholar]
- 7.Yin QS, Ai FZ, Zhang K, Mai XH, Xia H, Wu ZH. Transoral atlantoaxial reduction plate internal fixation for the treatment of irreducible atlantoaxial dislocation: a 2- to 4-year follow-up. Orthop Surg. 2010;2(2):149-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yin QS, Li XS, Bai ZH, et al. An 11-year review of the TARP procedure in the treatment of atlantoaxial dislocation. Spine (Phila Pa 1976). 2016;41(19):E1151-E1158. [DOI] [PubMed] [Google Scholar]
- 9.Xu JJ, Yin QS, Xia H, et al. New clinical classification system for atlantoaxial dislocation. Orthopedics. 2013;36(1):E95-E100. [DOI] [PubMed] [Google Scholar]
- 10.Yin QS, Wang JH. Current trends in management of atlantoaxial dislocation. Orthop Surg. 2015;7(3):189-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laheri V, Chaudhary K, Rathod A, Bapat M. Anterior transoral atlantoaxial release and posterior instrumented fusion for irreducible congenital basilar invagination. Eur Spine J. 2015;24(12):2977-2985. [DOI] [PubMed] [Google Scholar]
- 12.Wang C, Yan M, Zhou HT, Wang SL, Dang GT. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine (Phila Pa 1976). 2006;31(11):E306-E313. [DOI] [PubMed] [Google Scholar]
- 13.Yin YH, Tong HY, Qiao GY, Yu XG. Posterior reduction of fixed atlantoaxial dislocation and basilar invagination by atlantoaxial facet joint release and fixation: a modified technique with 174 cases. Neurosurgery. 2016;78(3):391-400; discussion 400. [DOI] [PubMed] [Google Scholar]
- 14.Zou XB, Yang HZ, Ge S, et al. Anterior transoral débridement combined with posterior fixation and fusion for atlantoaxial tuberculosis. World Neurosurg. 2020;138:E275-E281. [DOI] [PubMed] [Google Scholar]
- 15.Wang QD, Mao KZ, Wang CL, Mei W. Transoral atlantoaxial release and posterior reduction by occipitocervical plate fixation for the treatment of basilar invagination with irreducible atlantoaxial dislocation. J Neurol Surg A Cent Eur Neurosurg. 2017;78(4):313-320. [DOI] [PubMed] [Google Scholar]
- 16.Wei GJ, Wang ZY, Ai FZ, et al. Treatment of basilar invagination with Klippel-Feil syndrome: atlantoaxial joint distraction and fixation with transoral atlantoaxial reduction plate. Neurosurgery. 2016;78(4):492-498. [DOI] [PubMed] [Google Scholar]
- 17.Xia H, Yin QS, Ai FZ, et al. Treatment of basilar invagination with atlantoaxial dislocation: atlantoaxial joint distraction and fixation with transoral atlantoaxial reduction plate (TARP) without odontoidectomy. Eur Spine J. 2014;23(8):1648-1655. [DOI] [PubMed] [Google Scholar]
- 18.Li XS, Ai FZ, Xia H, Wu ZH, Ma XY, Yin QS. Radiographic and clinical assessment on the accuracy and complications of C1 anterior lateral mass and C2 anterior pedicle screw placement in the TARP-III procedure: a study of 106 patients. Eur Spine J. 2014;23(8):1712-1719. [DOI] [PubMed] [Google Scholar]
- 19.Yin QS, Xia H, Wu ZH, et al. Surgical site infections following the transoral approach: a review of 172 consecutive cases. Clin Spine Surg. 2016;29(10):E502-E508. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Transoral Atlantoaxial Reduction Plate (TARP) Technique for Treatment of Irreducible Atlantoaxial Dislocation (IAAD) Caused by Xiaobao Zou, Mandi Cai, Hanzhi Yang, Shuang Zhang, Chenfu Deng, Junlin Chen, Rencai Ma, Zexing Chen, Hong Xia, and Xiangyang Ma in Global Spine Journal