Abstract
International spread of polio continues to be a Public Health Emergency of International Concern since its declaration by the World Health Organization in 2014 and its reiteration in 2024. In 2023 and 2024, two countries remained endemic for wild poliovirus (WPV) but 20 countries reported polio outbreaks due to vaccine-derived polioviruses (VDPVs) in 2023 and 10 countries in 2024 (up to mid-June). Guidelines from various agencies recommend polio vaccination before travelling to or from polio-affected countries, or attending mass gatherings anywhere in the world, particularly if the crowd is international. Immunity protects against polio paralysis but not against poliovirus re-infection, irrespective of which vaccine was involved – live attenuated oral polio vaccine (OPV) or inactivated poliovirus vaccine (IPV). Infection with WPV or circulating VDPV in the vast majority of non-immune individuals (first infection) is asymptomatic, while they are efficient virus transmitters. Re-infections in immune individuals are always asymptomatic, but they are also infectious and may act as source for further transmission, although less efficiently than the former. Thus, travellers can become transmission vectors, illustrated by many episodes of importations of WPV or VDPVs into polio-free countries in recent years. The route of poliovirus transmission remains controversial, with many believing it to be faecal-oral, but epidemiological analysis is consistent with respiratory route and not faecal-oral. Transmission occurs person-to-person during social contact. Travellers must ensure they are adequately immunised to avoid polio, and becoming vectors of virus importation. The vaccine efficacy (VE) of OPV is highly variable – high in temperate climate countries, particularly rich countries, but low or very low in tropical low-income countries. On the other hand, VE of IPV is excellent everywhere irrespective of geography.
Keywords: public health emergency of international concern, vaccine-derived polio virus, vaccine-associated paralytic polio, Global Polio Eradication Programme, pilgrims, refugees, migrants
Introduction
Global travel is an integral part of human civilisation, cultural exchange and development. At the same time, it carries with it the risk of seeding a new pathogen in a new population in a new territory. The unprecedented and sudden closure of international borders and mass gatherings during the Coronavirus Disease (COVID-19) pandemic highlights the important relationship between travel and disease control. 1
Poliovirus infection can lead to polio paralysis which is irreversible. The polio eradication efforts were initiated 36 years ago by the World Health Organization (WHO) in 1988. 2 On 5 May 2014 the international spread of poliovirus was declared by the WHO as a Public Health Emergency of International Concern (PHEIC). 3 Under the 2005 International Health Regulations (IHR), countries/states have a legal duty to respond promptly to a PHEIC. In the latest (thirty-seventh) meeting of the Emergency Committee under IHR, held in December 2023, it was reaffirmed that the risk of international spread of polio remains a PHEIC. 4
This article presents a perspective on the complexities of the current eradication efforts of polio and how best to provide a world safe from polio, for all international travellers.
Vaccines available against polio
Polio is completely preventable with immunisation. Two vaccines have been available for over half a century – Inactivated Poliovirus Vaccine (IPV) and Oral Poliovirus Vaccine (OPV). IPV, an injectable vaccine, is highly protective with a minimum of two doses at 8 weeks interval, offering nearly 100% protection against polio disease, irrespective of the geographic conditions. IPV is not associated with any serious adverse event following immunisation (sAEFI) and is completely safe. 5
Though easy to administer, OPV has serious disadvantages of low efficacy, especially in tropical countries, and risk of rare sAEFI. One such sAEFI is vaccine-associated paralytic poliomyelitis (VAPP) in the vaccine-recipient or in close contact. It is estimated that over 17,000 cases of VAPP could have been caused by OPV, globally, during the past 23 years. 6 The other sAEFI is polio paralysis caused by vaccine-derived polioviruses (VDPVs). VDPVs emerge due to genetic reversion to neurovirulence of vaccine virus strains of the OPV, if the strains undergo a few generations of transmission. Another property regained by VDPV during spread is its transmission efficiency, like that of WPV. When VDPV spreads it is called circulating VDPV (cVDPV). Therefore cVDPVs cause polio outbreaks in the community, just like WPV. 6
Polio presents as lower motor neuron muscle paralysis due to spinal cord motor neuron infection and neuronal death. Therefore, neither VAPP nor polio due to VDPV can be clinically differentiated from polio due to WPV. Virological tests differentiate the cause as WPV, vaccine virus or VDPV/cVDPV. However, unlike paralysis due to VDPV, VAPP is not officially recorded in the polio surveillance reports of the Global Polio Eradication Initiative (GPEI). 6
OPV being a live vaccine is contraindicated in the B-cell immunocompromised host, whereas IPV can be safely administered in the immunocompromised. IPV is contraindicated in persons with hypersensitivity to a previous dose of the vaccine or to any of the vaccine components, including formaldehyde and 2-phenoxyethanol. The GPEI, led by the WHO, has used OPV as the principal tool for polio eradication, mainly due to its low cost and convenience of administration. GPEI managers had another reason to rely predominantly on OPV: They argue that infection by vaccine viruses induces intestinal immunity for inhibiting infection by WPV or VDPV when exposed. So, trivalent OPV (tOPV) containing vaccine virus types 1, 2 and 3 was used exclusively from 1988 to 2016. 7
Because of low vaccine efficacy (VE) of OPV in tropical low-income countries, GPEI supplemented routine doses (3 or 4 during infancy) with many rounds of community-wide or country-wide campaigns – even house-to-house campaigns in some countries. Concurrently, there was a worldwide increase in cases due to cVDPV type 2 (cVDPV-2). Among the three vaccine virus types, the most transmissible is type 2. Polio due to cVDPV-2 was reported from 2000 onwards, first in small numbers, but later as outbreaks from 2005/2006 onwards, and gradually increased in international spread also. Realising that the widespread use of type 2 vaccine virus was leading to the emergence of new lineages of cVDPV-2, a decision was made by GPEI to discontinue type 2 virus from tOPV. It was implemented by globally synchronous tOPV to bOPV switch, in April–May of 2016. Only types 1 and 3 vaccine viruses are present in bivalent OPV (bOPV). Yet cVDPV lineages have continued to emerge from silently spreading vaccine virus type 2; in the post-switch years, monovalent type-2 continued to be used by GPEI to control cVDPV-2 polio outbreaks in some countries, which has resulted in the generation of new lineages of cVDPV-2. During the last quarter of 2001 and first quarter of 2022 such lineages had reached Israel, the United Kingdom (UK) and the United States of America (USA), imported from some such sources that remained unknown. 8
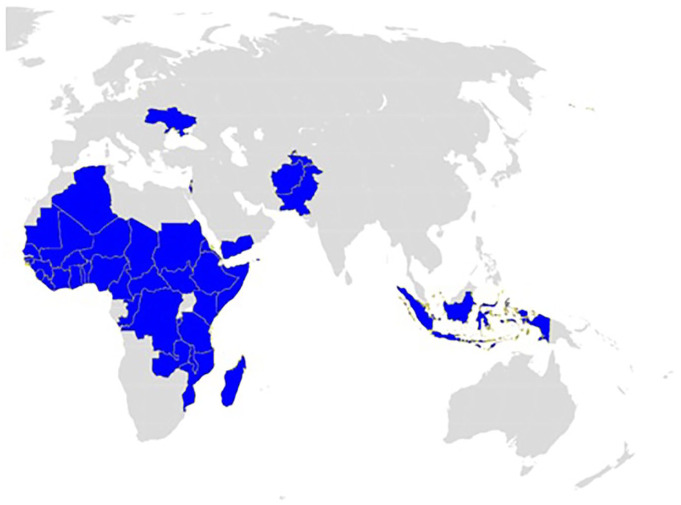
In 2023, just two countries, Afghanistan and Pakistan, continued to remain endemic for WPV-1, but 20 countries reported polio due to cVDPVs. Of these, 17 countries are in Africa, with the remaining three being Yemen, Israel and Indonesia. 9 Many of the countries that reported VDPV polio in recent years are very popular tourist destinations. The United Nations Tourism dashboard reported inbound travel into the African continent of over 60 million tourists in the year 2023 alone. 10 The map below shows countries in Africa and Eurasia reporting polio due to WPV or cVDPV in the past 3 years (Figure 1).
Figure 1.
Countries in Africa and Eurasia Continents (shaded in blue) that reported polio due to WPV and/or cVDPV in past 3 years (2021–2023).
cVDPV, circulating vaccine-derived poliovirus; WPV, wild poliovirus.
Risk of polio in the traveller
Immunity induced by past WPV infection or successful OPV immunisation is protective against polio paralysis for life. As for IPV, if immunity is primed by 2 or 3 doses and boosted at least once, protection is also life-long. However, in case a traveller is unimmunised and fully susceptible, they are at risk of developing polio if infected with WPV or VDPV when travelling in endemic countries. Even if infected, the probability of polio paralysis is low, as the case-to-infection ratio is <0.01. During the episodes of importation of cVDPV into Israel and in New York, a few unimmunised individuals – only children in Israel but one adult in New York, developed polio paralysis in 2022. 8
Those who had been immunised with OPV have to be aware that its VE varies widely – while a recommended course of 3 or 4 doses of tOPV or bOPV may have induced immunity in all subjects in temperate zone countries, it may not have induced immunity in all in tropical and sub-tropical zone countries, where OPV’s VE may be low, or even very low.10,11 Those born in such countries before 1990 might have acquired natural immunity from WPV infection. However, for travel preparation, additional doses are prudent in everyone, to be sure of immunity. 12 A booster with IPV would provide personal protection against the disease to the traveller and also reduce the chances of re-infection. 12
The USA Centers for Disease Control and Prevention (CDC) has therefore given recommendations to vaccinate against polio before international travel to polio-affected countries (see below). 12
This protection is due to systemic immunity but it often does not protect from re-infection.13,14 Such re-infection is confined to mucosal tissues and asymptomatic. Therefore there is risk of acquiring polio infection during travel, especially to endemic countries for a traveller and/or family (including children). 12
In the pre-OPV era the transmission of WPVs was believed to be directly person-to-person, highly contagious, and by inhalation of virus shed in oral droplets/aerosol, shed most often by silently infected persons. 15 Once WPV infection was discovered to be pharyngeal and intestinal, shed in the throat and in faeces, opinions of experts changed to transmission by faecal-oral route. The main argument to persist with OPV for polio prevention, control and eradication, despite its geographic variations of VE is the belief that transmission is faecal-oral. 11 However, epidemiological studies point towards a respiratory route: in all low-income countries, the age distribution of polio resembled that of measles, diphtheria and pertussis – all respiratory transmitted.11,16,17 Polio-affected even exclusively breastfed infants, and the median age was in the range of 12–15 months – typical of respiratory-transmitted infectious diseases.11,18 Where the water supply got contaminated by sewage, many outbreaks of faecal-orally transmitted infectious diseases such as typhoid fever, dysentery, cholera and hepatitis A/E have occurred but never polio outbreaks. In the pre-vaccine era, polio was equally prevalent in rich and low-income countries. 11 Large outbreaks occurred in the 19th century despite the sanitation movement across Europe and America, which had significantly reduced water-borne infectious diseases but not polio. Therefore, simple measures such as safe drinking water or eating hygienic food, while very important for personal well-being, cannot be equally useful against poliovirus infection, where it is still endemic/prevalent.
The not-so-infrequent long-distance importations of WPV or cVDPV, to polio-free countries, are most likely through asymptomatically re-infected travellers, mostly adults. 19 However, many respiratory-transmitted viruses are shed in faeces, such as Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV2) and Middle East Respiratory Syndrome. Therefore faecal collections in aircraft during long-haul international flights are being considered as an option to detect poliovirus shed by air travellers. 20
Risk of importation of polio in polio-free countries
An infected traveller can carry the virus into the countries being visited. In Bulgaria, WPV-1 was carried by sailors and the imported virus caused a polio outbreak in children in the port region. 21 It is estimated that an additional 1.15 billion US dollars were spent for outbreak control alone, for 191 documented polio importations, during 2003–2014, which resulted in 3763 polio cases in polio-free countries. 22 In 2008, Burkina Faso had WPV-1 importation from Nigeria, resulting in an outbreak despite 99% infant vaccination coverage with three doses of OPV. 23 The investigation of imported WPV-1 from Afghanistan to Tajikistan in April 2010, resulting in 120 cases of paralysis and 10 deaths in children, found that over 45% of victims had received over 4 doses of OPV. 24 A mathematical model estimated 665 polio exportations from nine polio-infected countries in the year 2014 of which over 99% were by asymptomatic travellers. 21
The clear failure of protection by OPV despite good vaccination coverage in these affected countries is concerning. 11 There is a pressing need for a more secure strategy by every country to protect itself from polio re-infections and onward transmissions.
Poliovirus spread during gatherings and travel
Despite the high sanitation standards in USA and UK, sustained transmission of the poliovirus was detected in these IPV-using populations in the year 2022. This has raised intense debates in the media, among the scientific community and policymakers about the alleged failure of IPV to contain the transmission of poliovirus and the need for re-introduction of OPV in the form of novel OPV (nOPV) in these countries.25,26 The nOPV has been designed to avoid genetic reversion to neurovirulence but disappointingly has been recently reported to have evolved into cVDPV. 27 Also nOPV does not improve the problem of low efficacy of OPV in the tropical countries. 28
The case study of the unimmunised adult paralysed with VDPV-2 in Rockland County, New York, in July 2022 and detection of VDPV in wastewater in the USA has highlighted that even resource-rich countries can face the consequences of polio importation. Investigations by CDC revealed that IPV immunisation coverage had dipped post-COVID-pandemic to as low as 37.3% in the region of zip code covering Rockland County. 29 Therefore, the claim by some experts and the media that the virus transmission was due to the inability of IPV immunity to contain transmission was false: It was due to failure to keep up vaccination coverage. Once vaccination coverage with IPV was improved, the transmission died out. The adult polio victim had never been vaccinated against polio (apparently due to religious belief). The New York City Department of Health and Mental Hygiene had declared that there was no possibility of contamination of drinking water with sewage, 29 thus making the transmission theory of faecal-oral route not plausible.8,17
We have reviewed the epidemiology of the short-term and geographically restricted spread of cVDPV-2 in London and New York State and concluded that its transmission was respiratory and not faecal-oral.8,17,30 Moreover, the note of “the long distance spread by air travel of cVDPV2 between Israel, the UK and the USA” by WHO in its report of the thirty-seventh meeting of the Emergency Committee, 4 is consistent with the route of cVDPV-2 transmission as respiratory.
The unvaccinated adult in New York had attended a gathering in the city, 8 days prior to the onset of symptoms. Incubation period of polio ranges between 1 and 4 weeks. The most likely sequence was that he got infected during social contact, hence through respiratory transmission, from another individual who was already infected without any symptoms.
CDC recommendations for travellers to polio-affected countries
The US CDC recommends that all infants and children in the US ought to have been given four doses of IPV at 2 months, 4 months, 6–18 months and 4–6 years before departure to countries with any risk of polio exposure. 12 An optional accelerated course can be provided before departure as first dose at 6 weeks, with second and third doses at one-month intervals from previous doses and the fourth dose at least 6 months interval from the third dose. In case the accelerated course could not be completed before departure, the pending doses need to be taken while in the country travelled to. In case of unvaccinated adults, the recommendation is three doses of IPV with second and third at least 1 month and 6 months from the 1st dose respectively. An accelerated schedule for adults includes three doses of IPV with at least one-month intervals from previous doses. Adults who are incompletely vaccinated with only one or two doses of polio should receive the remaining 1 or 2 doses of IPV (at minimum 4 weeks interval) before departure. 12 Fully vaccinated adults should receive a one-time booster of IPV before travelling to countries with increased risk of exposure to poliovirus. 12
Large gatherings and polio vaccine recommendations
Kumbh Mela in India is probably the world’s largest congregation of religious pilgrims and is celebrated four times over a course of 12 years. Health advisory for attending the Kumbh Mela states mandatory vaccination against poliomyelitis. 31
Although India eliminated WPV polio in January 2011 (certified so in March 2014), it continues to remain at risk of polio importation. The Government of India requires polio vaccination certification at least 4 weeks before departure to India from polio-endemic countries, countries with poliovirus circulation following importation, and countries with cVDPV during the last 3 years. 32
Hajj pilgrimage is a requirement for Muslims, to be carried out at least once in their lifetime. Annually millions gather in Mecca (Saudi Arabia) for this sacred pilgrimage. For Hajj pilgrims and Umrah performers, proof of polio vaccination with either OPV or IPV is required at least 6 weeks prior to the application for entry visa to Saudi Arabia. 33 All visitors under 15 years, irrespective of immunisation status, will receive 1 dose of OPV at border points. Saudi Arabia protects its children against polio using IPV combined with other injected childhood vaccines. 34
Opposition by religious fundamentalists has been described as a major cause of failure of immunisation programmes against polio in countries such as Pakistan, Nigeria and Afghanistan. 35 “Fatwas” were issued by the Taliban against oral polio vaccination as an alleged American conspiracy to sterilise the Muslim populations. Hundreds of polio vaccinators in these countries have been either kidnapped or killed during the last decade. Engagement of religious leaders as champions of polio eradication is a critical strategy to encourage vaccination against polio. 36 OPV is technically easy to administer and therefore it is easy to recruit an army of volunteers for mass vaccination in countries where only OPV is available. 37 At the same time, in conflict areas and highly sensitive areas, it is wiser to offer a vaccine that will provide higher protection with minimum doses such as IPV than to use a vaccine such as OPV, which requires repeated doses through mass campaigns. Repeated campaigns not only add to the cost but also reduce the confidence of the community, leading to misinformation by religious and political leaders as well as vulnerability of health workers to violent attacks.
Polio protection for refugees and migrants
Countries face a high risk of polio importation from migrant and refugee populations. At the same time, these migrant populations are highly vulnerable to all vaccine-preventable diseases. Language barriers, lack of knowledge, lack of trust, underserved and marginalised populations, inaccessibility of convenient services, and discrimination by health care providers are important challenges in these populations, leading to low vaccination coverage. 36 Increased efforts are needed by the host countries to reach these vulnerable populations, integrate them into the country’s health system and improve awareness through education about important vaccinations, including polio.
Summary and conclusion
As long as there is poliovirus infection anywhere, there is always a risk of importation during travel. Poliovirus importations, especially into polio-free countries, reverse the progress made for global polio eradication.
Compared to IPV, OPV needs maintenance of higher vaccination coverage and must avoid even the smallest immunity gaps. 8 Also, OPV due to its lower efficacy, does not guarantee protection from wild poliovirus in much of the so-called developing world. 11 Children have developed polio despite receiving even 20–28 doses of OPV. 38 At the same time its continued use is leading to further seeding of vaccine polio viruses even in previously polio-free countries, with the risk of emergence of VDPVs. The advantage that OPV can be administered by volunteers does not mitigate these disadvantages. 11
In our opinion, the world needs to move to the exclusive use of IPV immunisation in every country, with subsequent withdrawal of all OPVs.6,8,11,17,19,39 There appears to be no better alternative strategy. 28 Using injectable vaccines, the world eradicated smallpox and has decades of successful experience eliminating neonatal tetanus as a public health problem from all but a dozen countries and implementing wide age-range mass campaigns against measles and coronavirus. There should be no deterrence in using IPV despite its parenteral route or higher per-dose vaccine costs. As a more heat-stable vaccine than OPV, IPV has additional operational advantages, especially in tropical climates. The higher efficacy and safety of IPV makes it a desirable option for protection irrespective of geography. Therefore, in our perspective, an individual traveller will be relieved of inconvenience and concern related to polio in future if there is a uniform shift to an exclusive IPV strategy globally in the primary series of immunisation. The early completion and certification of global polio eradication will be beneficial to everyone in the world.
Acknowledgments
None.
Footnotes
ORCID iD: Dhanya Dharmapalan  https://orcid.org/0000-0002-6691-1435
https://orcid.org/0000-0002-6691-1435
Contributor Information
Dhanya Dharmapalan, Apollo Hospitals, CBD Belapur, Navi Mumbai 400614, India.
Thekkekara Jacob John, Christian Medical College, Vellore, Tamil Nadu, India.
Robert Steinglass, Independent Consultant, Marshall, NC, USA.
Norbert Hirschhorn, Independent Consultant, Minneapolis, MN, USA.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Author contributions: Dhanya Dharmapalan: Conceptualisation; Data curation; Writing – original draft; Writing – review & editing.
Thekkekara Jacob John: Writing – original draft; Writing – review & editing.
Robert Steinglass: Writing – original draft; Writing – review & editing.
Norbert Hirschhorn: Writing – original draft; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
Competing interests: The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1. Gössling S, Scott D, Hall CM. Pandemics, tourism and global change: a rapid assessment of COVID-19. J Sustain Tourism 2020; 29(1): 1–20. [Google Scholar]
- 2. World Health Assembly. Forty-first world health assembly, Geneva, 2–13 May 1988. WHA41.28. Global eradication of poliomyelitis by the year 2000. https://iris.who.int/handle/10665/164197 (accessed 12 January 2024).
- 3. Global Polio Eradication Initiative. Public Health Emergency status, http://polioeradication.org/polio-today/polio-now/public-health-emergency-status, (2014, accessed 02 January 2024).
- 4. WHO. Statement following the Thirty-seventh meeting of the IHR emergency committee for polio, https://www.who.int/news/item/22-12-2023-statement-following-the-thirty-seventh-meeting-of-the-ihr-emergency-committee-for-polio (2023, accessed 12 January 2024).
- 5. Global polio Eradication Initiative. IPV, https://polioeradication.org/about-polio/the-vaccines/ipv/ (accessed 16 August 2024).
- 6. John TJ, Dharmapalan D, Hirschhorn N, et al. How to avoid causing polio in the name of its eradication. Lancet 2023; 402(10397): 179–180. [DOI] [PubMed] [Google Scholar]
- 7. Hampton LM, Farrell M, Ramirez-Gonzalez A, et al. ; Immunization systems management group of the global polio eradication initiative. Cessation of trivalent oral poliovirus vaccine and introduction of inactivated poliovirus vaccine - worldwide, 2016. MMWR Morb Mortal Wkly Rep 2016; 65(35): 934–938. [DOI] [PubMed] [Google Scholar]
- 8. John TJ, Dharmapalan D. Lessons from vaccine-related poliovirus in Israel, UK and USA. Vaccines (Basel) 2022; 10(11): 1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization. 25_Polio weekly update. Geneva, Switzerland: WHO, 2024. [Google Scholar]
- 10. UNTWO. Global and regional tourism performance, https://www.unwto.org/tourism-data/global-and-regional-tourism-p (accessed 22 December 2024).
- 11. John TJ, Dharmapalan D. Challenges en route to polio eradication. Lancet 2022; 400(10350): 428–429. [DOI] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention. Polio: for travelers, https://www.cdc.gov/polio/vaccines/international-travelers.html (2024, accessed 25 January 2024).
- 13. Grassly NC, Jafari H, Bahl S, et al. Waning intestinal immunity after vaccination with oral poliovirus vaccines in India. J Infect Dis 2012; 205(10): 1554–1561. [DOI] [PubMed] [Google Scholar]
- 14. Mach O, Verma H, Khandait DW, et al. Prevalence of asymptomatic poliovirus infection in older children and adults in northern India: analysis of contact and enhanced community surveillance, 2009. J Infect Dis 2014; 210(Suppl. 1): S252–S258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stanfield JP. Immunization: current major issues. In: Jelliffee DB, Jelliffe EFP. (eds). Advances in international maternal and child health. New York: Oxford University Press, 1981, pp. 1–23. [Google Scholar]
- 16. Anderson RM. Directly transmitted viral and bacterial infections of man. In: Anderson RM. (ed). The population dynamics of infectious diseases: theory and applications. London: Chapman and Hall, 1982, pp. 1–37. [Google Scholar]
- 17. John TJ, Dharmapalan D, Steinglass R, et al. The respiratory route of transmission of virulent polioviruses. Infect Dis (Lond) 2024; 56: 918–924. [DOI] [PubMed] [Google Scholar]
- 18. Soudarssanane MB, Rotti SB, Srinivasa DK, et al. Paralytic poliomyelitis in children under 6 years in Pondicherry: a community survey. J Epidemiol Community Health 1993; 47: 210–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. John TJ, Dharmapalan D, Steinglass R, et al. The role of adults in poliovirus transmission to infants and children. Glob Health Sci Pract 2024; 12(2): e2300363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Newey S. The new mile-high club: Why airline toilets could give early warning of the next pandemic. The Telegraph [Internet], https://www.telegraph.co.uk/global-health/science-and-disease/airline-toilets-early-warning-of-the-next-pandemic/ (2024, accessed 10 Feb 2024).
- 21. Kojouharova K, Zuber PLF, Gyuroa S, et al. Importation and circulation of poliovirus in Bulgaria in 2001. Bull WHO 2003; 81(7): 476–481. [PMC free article] [PubMed] [Google Scholar]
- 22. Wilder-Smith A, Leong WY, Lopez LF, et al. Potential for international spread of wild poliovirus via travelers. BMC Med 2015; 13: 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. CDC. Wild poliovirus Type 1 and Type 3 importations - 15 countries, Africa, 2008–2009. MMWR 2009: 58(14); 357–362. [PubMed] [Google Scholar]
- 24. WHO. Disease outbreak news, https://www.who.int/emergencies/disease-outbreak-news/item/2010_04_23-en (2010, accessed 15 February 2024).
- 25. Schwalbe N, Varma JK. The US needs to prepare to introduce the novel oral polio vaccine. BMJ 2022; 379: 2388. [DOI] [PubMed] [Google Scholar]
- 26. Kimball S. CDC is discussing using oral polio vaccine for first time in 20 years to stop New York outbreak. CNBC [Internet], https://www.cnbc.com/2022/10/21/cdc-is-discussing-using-oral-polio-vaccine-for-first-time-in-20-years-to-stop-new-york-outbreak (2022, accessed 10 January 2024).
- 27. GPEI. GPEI Statement on cVDPV2 detections in Burundi and Democratic Republic of the Congo, https://polioeradication.org/news-post/gpei-statement-on-cvdpv2-detections-in-burundi-and-democratic-republic-of-the-congo/(2023, accessed 12 January 2024).
- 28. John TJ, Dharmapalan D, Steinglass R, et al. Novel OPV is still not the right tool for polio eradication. Indian Pediatr 2024; 61(4): 387. [PubMed] [Google Scholar]
- 29. Link-Gelles R, Lutterloh E, Ruppert SP, et al. ; 2022 U.S. Poliovirus Response Team. Public health response to a case of paralytic poliomyelitis in an unvaccinated person and detection of poliovirus in wastewater - New York, June-August 2022. MMWR Morb Mortal Wkly Rep 2022; 71(33): 1065–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kum D. USA Today [Internet], https://www.usatoday.com/story/news/factcheck/2022/08/26/fact-check-polio-detected-new-york-city-sewage-not-tap-water/10357330002/ (2022, accessed 29 January 2024).
- 31. Directorate General Health Services. Health advisory for international travellers visiting India for Kumbh Mela, https://dghs.gov.in/WriteReadData/News/201812310545124501329CCF12312018.pdf (2019, accessed 20 January 2024).
- 32. The Embassy of the kingdom of Saudi Arabia. Hajj and Umrah health requirements, https://www.saudiembassy.net/hajj-and-umrah-health-requirements (2016, accessed 22 January 2024).
- 33. WHO. Vaccine schedule for Saudi Arabia, https://immunizationdata.who.int/pages/schedule-by-country/sau.html (accessed 22 January 2024).
- 34. Warraich HJ. Religious opposition to polio vaccination. Emerg Infect Dis 2009; 15(6): 978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. GPEI. Religious leaders fuelling demand for polio vaccines and health services In Nigeria, https://polioeradication.org/news-post/religious-leaders-fuelling-demand-for-polio-vaccines-and-health-services-in-nigeria/(2018, accessed 15 January 2024).
- 36. Nasiri A, Farshidi H, Rezaei F, et al. Perceived barriers of migrants and refugees to vaccinate their children against Measles and polio: a study in Iran. Int J Equity Health 2023; 22(1): 253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. WHO. History of polio vaccination, https://www.who.int/news-room/spotlight/history-of-vaccination/history-of-polio-vaccination# (accessed 4 September 2024). [DOI] [PMC free article] [PubMed]
- 38. Independent Monitoring Board. Closing in on zero. Twenty second report, https://polioeradication.org/wp-content/uploads/2023/09/22nd-Report-of-The-Independent-Monitoring-Board-IMB.pdf (2023, accessed 02 February 2024).
- 39. John TJ, Dharmapalan D, Hirschhorn N. Intestinal mucosal immunity is unimportant for polio eradication: the failure of oral polio vaccination. Infect Dis 2024; 56(8): 669–677. [DOI] [PubMed] [Google Scholar]