Abstract
In this narrative review, we summarized evidence from peer-reviewed articles, published before February 2024, that investigated lifestyle behaviors among children (≤12 years) and adolescents (13-18 years) representing different geographic descents. These behaviors included dietary patterns, screen time, physical activity, smoking, alcohol consumption, oral hygiene, unsafe sex, and sleep duration and quality. We documented the significant impacts of parental, school, and sociodemographic factors on the adoption of numerous lifestyle behaviors in this age category. Several health consequences could be attributed to unhealthy lifestyle behaviors during childhood and adolescence. For example, poor dietary habits can lead to a higher risk of obesity and cardiovascular disease. Physical inactivity contributes to the development of musculoskeletal and psychological disorders. Excessive screen time is associated with visual acuity problems, poor sleep, and psychological and behavioral problems. Tobacco use poses a significant risk for severe respiratory and cardiovascular diseases. Risky sexual behaviors are related to sexually transmitted infections and exposure to violence. Short sleep duration is associated with a lack of physical fitness and poor cognitive function. However, potential interventions, such as school-based health programs, community outreach initiatives, and national health policies and regulations, can improve lifestyle behaviors among children and adolescents.
Keywords: diet, physical activity, smoking, oral health, children, adolescents
“Inadequate sleep may have disruptive effects on the cognitive function and learning capacity of children and adolescents.”
Introduction
Childhood and adolescence represent critical developmental periods when habits and behaviors are established, laying the foundation for future health trajectories. The impact of lifestyle factors during these formative years can extend into adulthood, affecting long-term health outcomes.1,2
The modern era has witnessed a substantial increase in the prevalence of chronic diseases, especially those of non-communicable origin, among children and adolescents.3,4 Unhealthy lifestyle behaviors have emerged as a significant contributing factor to this alarming trend.5,6 Lifestyle factors, such as dietary patterns, screen time, physical activity, smoking, alcohol consumption, oral hygiene, unsafe sex, and sleep duration and quality, can play a crucial role in shaping the health outcomes of young individuals.5,6
Investigating the contributing factors, health consequences, and potential interventions related to lifestyle behaviors is of paramount importance for promoting healthy living and preventing chronic diseases in this vulnerable population.7-9 Thus, we conducted this review to provide an overview of the lifestyle factors prevalent among children and adolescents. We explored factors that influence lifestyle behaviors in this age group, including societal, environmental, and familial determinants. Additionally, we described potential health consequences associated with unhealthy lifestyle choices during childhood and adolescence, such as obesity, cardiovascular disease (CVD), and mental health disorders. We also highlighted potential interventions and strategies that can be applied to promote positive lifestyle modifications among children and adolescents. Elucidating the effectiveness and feasibility of different interventions may provide insights and guidance to policymakers, health care professionals, parents, and teachers regarding their efforts to improve the health and well-being of the younger generation.
Methods
In this narrative review, we briefly presented contributing factors, health consequences, and potential interventions for certain lifestyle behaviors during childhood and adolescence. We collected evidence from 164 epidemiological studies, published in the Scopus and Web of Science databases before February 2024. The obtained studies investigated dietary patterns, screen time, physical activity, smoking behaviors, alcohol consumption, oral hygiene, unsafe sex, and sleep habits during childhood and adolescence. The age limits for childhood and adolescence were set based on the age limits of the reviewed studies (≤12 years for childhood and 10-12 to 18-20 years for adolescence). The publication time of the included studies ranged between 1986 and 2024 and was distributed as follows: before 2010: 11.6%, 2010-2015: 20.1%, 2016-2020: 32.3%, and after 2020: 36.0%. To reach generalizable conclusions, we included study populations representing different geographic descendants as follows: reviews, systematic reviews, meta-analyses, and cross-continental studies: 35.5%, North America: 15.9%, South America: 5.5%, Europe: 14.6%, Africa: 7.3%, West and Central Asia: 7.3%, East Asia: 11.6%, and Oceania: 4.3%.
Of note, we did not systematically obtain all related studies. Unpublished and non-peer-reviewed reports and studies published in languages other than English were not included.
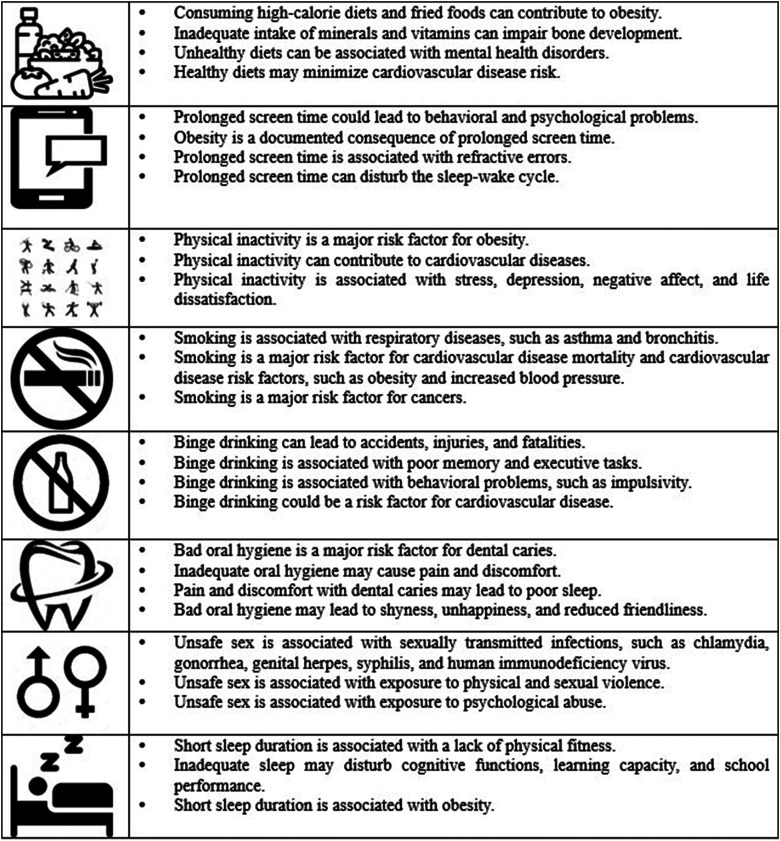
In (Table 1), we briefly summarized the contributing factors, health consequences, and potential interventions for different lifestyle behaviors among children and adolescents. More details about health consequences (Figure 1) and a summary of the main characteristics and findings of the included studies (Supplemental File 1) were provided as well.
Table 1.
Contributing Factors, Health Consequences, and Potential Interventions of Different Lifestyle Behaviors Among Children and Adolescents.
| Lifestyle | Contributing Factors | Health Consequences | Potential Interventions |
|---|---|---|---|
| Dietary pattern | Parental influence.10-12 | Obesity.17-19 | Nutrition education and awareness programs.28,29 |
| School environment.13,14 | Poor bone health.20,21 | Improving school food policies. 30 | |
| Media influence. 15 | Behavioral and mental health issues. 22-24 | Regulating food marketing and production.31,32 | |
| Socioeconomic status. 16 | Cardiovascular disease.25-27 | ||
| Screen time | Parental influence.33,34 | Behavioral and psychological issues.37-40 | Parental education. 53 |
| Sociodemographic factors.35,36 | Obesity.41-43 | Behavior substitution. 54 | |
| Vision problems.44-46 | |||
| Sleep disturbance.47,48 | |||
| Musculoskeletal problems.49-52 | |||
| Physical activity | Parental influence.55-57 | Obesity.60-62 | Behavioral change.68,69 |
| Access to facilities.58,59 | Cardiovascular disease.63-65 | Providing places for physical activity.70,71 | |
| Psychological problems.66,67 | |||
| Smoking | Parental and peer influence.72-74 | Respiratory disorders.79-81 | Cognitive-based approaches.88-91 |
| Media and marketing influence.75-77 | Cardiovascular disease.82-84 | Pharmaceutical approaches.91-93 | |
| Access to tobacco. 78 | Cancer.85-87 | Restricting access to tobacco. 94 | |
| Alcohol consumption | Parental and peer influence.95-97 | Accidents.104-107 | School-based interventions.113-115 |
| Media and marketing influence.98-101 | Cognitive, neurological, and behavioral problems.108-111 | Family-based interventions. 114 | |
| Access to alcohol.102,103 | Cardiovascular disease. 112 | Restricting access to alcohol.116,117 | |
| Oral hygiene | Parental factors.118-122 | Dental caries.128-130 | School-based educational programs.136,137 |
| Dietary behaviors.123-127 | Poor sleep.131,132 | Community-based initiatives and programs.138-140 | |
| Psychological and behavioral problems.133,135 | |||
| Unsafe sex | Personal factors.141-145 | Sexually transmitted infections.146-148 | Sex education.153,154 |
| Family factors.141-145 | Exposure to violence.149-151 | Parental involvement.155,156 | |
| Community factors.141-145 | Unwanted pregnancies. 152 | ||
| Sleep | Excessive screen use.47,48,157 | Lack of physical fitness.163,164 | Behavioral interventions.168-170 |
| Lack of consistent sleep habits.158-160 | Poor cognitive functions. 165 | Pharmaceutical interventions.171,172 | |
| Sociodemographic factors.161,162 | Obesity.166,167 |
Figure 1.
Main lifestyle behaviors and their associated health consequences in children and adolescents.
Lifestyle Behaviors: Contributing Factors, Health Consequences, and Potential Interventions
Dietary Patterns
Contributing Factors
Parental Influence
Parents play a vital role in providing healthy meals, setting an example through their eating behaviors, and creating a positive food environment at home. In the ToyBox Study, among 5185 European parents of preschool children (3-5 years), being permissive about unhealthy snacking and acceding to child demands for unhealthy snacks were associated with a greater intake of unhealthy snacks by children. 10 Parents with better nutritional knowledge of snack food recommendations were more likely to have children consuming healthy snacks. 10 Additionally, the family food environment can play an essential role in shaping food consumption at a young age. In a study including 9686 Chinese students (grades 3-12) and their parents, family food availability, parents’ nutritional literacy, meal practices, and food rules were associated with healthier food consumption. 11 Shared family meals are pointedly related to nutritional health in children and adolescents. A meta-analysis of 17 studies showed that children and adolescents who shared family meals ≥3 times/week were more likely to have healthier dietary patterns and were less likely to engage in disordered eating. 12
School Environment
Schools can influence children’s dietary intake by offering healthy meal options, implementing nutrition education programs, and promoting a supportive food environment. In a study including 1010 US students (12-13 years) from the Military Teenagers Environments, Exercise, and Nutrition Study (M-TEENS), unhealthy item availability at school was associated with purchasing sweets, snacks, and sugar-sweetened beverages. 13 A study of 812 Canadian students (10-11 years) showed that children exposed to unhealthy food outlets around the school had lower diet quality and consumed fewer fruits and vegetables. 14
Media Influence
The marketing of unhealthy foods and beverages to children and adolescents can influence their dietary preferences, purchases, and consumption. Various marketing strategies, especially those aimed at a younger audience, can shape their perceptions and choices related to food and drinks. Appealing packaging and design, advertising on children’s media and video games, promotions and contests, and celebrity endorsements are among these strategies. 15 A systematic review of 26 studies showed that unhealthy food and beverage marketing, especially through social media (6 studies) and advergaming (20 studies), can negatively impact children’s food choices and intake. 15
Socioeconomic Status
Socioeconomic status can play an essential role in determining the quality of the food consumed. A systematic review of 40 studies showed that parental education and family income were inversely associated with unhealthy dietary patterns, especially in developing countries. 16
Health Consequences
Obesity
The association between dietary patterns and obesity in children and adolescents is profound, with studies consistently demonstrating that diets high in processed foods and sugary beverages significantly contribute to the rising prevalence of childhood obesity. Conversely, adopting a balanced and nutrient-dense diet, rich in fruits, vegetables, and whole grains, plays a crucial role in mitigating the risk of obesity and promoting overall health in children. 17 The IDEFICS (Identification and prevention of Dietary- and lifestyle-induced health EFfects In Children and infantS) study analyzed data from 8341 children (2-9 years) representing 8 European countries and concluded that processed dietary pattern or changing to a sweet pattern were associated with increased body mass index, waist circumference, and fat mass 2 years later. 18 A study investigating 487 urban-dwelling children and adolescents (9-15 years) from 24 schools in Ghana showed that energy-dense dietary patterns, characterized by processed meat, fried foods, and sugary foods, were associated with overweight/obesity, while dietary patterns including starchy root staples and vegetables were associated with decreased overweight/obesity. 19 A systematic review and meta-analysis of 60 studies reported that a higher intake of sugar-sweetened beverages, fast food, meat, and refined grains was associated with a higher risk of overweight/obesity, while a higher intake of whole grains was associated with a decreased risk of overweight/obesity. 17
Poor Bone Health
The relationship between diet patterns and poor bone health in children is evident, as inadequate intake of essential nutrients such as calcium and vitamin D can compromise bone development later in life. 20 A prospective cohort study of 2850 Dutch children showed that infant dietary patterns at the age of 13 months, characterized by high intakes of dairy, whole grains, and eggs, were associated with increased bone mineral content at the age of 6 years. 20 A recent systematic review involving 7130 children and adolescents (3-17.9 years) showed a significant association between healthy dietary patterns and bone health markers in 7 studies. 21
Behavioral and Mental Health Issues
Unhealthy dietary patterns can be associated with an increased risk of mental health disorders. A study including Australian children (n = 1367; 5-10 years) and adolescents (n = 1277; 11-15 years) showed that those who met vegetable, fruit, and discretionary food intake guidelines were less likely to develop emotional, behavioral, and social problems. 22 Among 7114 adolescents (10-14 years) from the Australian Healthy Neighbourhoods Study, healthy diets, defined as having a daily breakfast and consuming low-fat dairy, 2 servings of fruit, and 4 servings of vegetables every day, were associated with a lower risk of depression. 23 In a study involving 71 553 Brazilian adolescents (12-17 years), healthy dietary patterns, having breakfast, and sharing meals with family were associated with better mental health. 24
Cardiovascular Disease
Healthy diets may minimize CVD risk by preventing its risk factors. A prospective cohort study of 116 430 female US nurses from the Nurses’ Health Study II (NHSII) showed that frequent consumption of fruits, vegetables, and whole grains during high school was associated with a lower risk of hypercholesterolemia and hypertension during adulthood. 25 In a study of 435 German children and adolescents (4-18 years), the intake of fruits and vegetables was associated with reduced blood pressure in the pre-puberty group, while salt intake was associated with elevated blood pressure in the puberty group. 26 Among 232 Brazilian children and adolescents with congenital heart disease (median age = 10 years), the excessive intake of ultra-processed foods was associated with high CVD risk defined as central adiposity, elevated high-sensitivity C-reactive protein, and subclinical atherosclerosis. 27
Potential Interventions
Nutrition Education and Awareness Programs
Providing nutrition education in schools and community settings can empower children and adolescents to make informed food choices and develop lifelong healthy eating habits. Besides, educating parents and caregivers about the importance of healthy diets and providing them with resources and guidance on meal planning and preparation can positively influence children’s eating habits.28,29 A study of 1535 Japanese adults revealed that those who received nutrition education at elementary and middle schools had better attitudes towards nutrition education during adulthood. 28 Additionally, family conversations on diet during elementary school years had a positive impact on consuming nutritionally balanced diets during adulthood. 28 A statewide program serving low-income US children (≤5 years) showed that enacting policies promoting healthy foods and educating parents about healthy diets were associated with increased consumption of fruits and lean proteins. 29
Improving School Food Policies
Implementing policies that promote nutritious school meals and ensure food safety standards can have a significant impact on children’s dietary behaviors. A meta-analysis of 91 interventions, aiming to modify school food environment policies, showed that direct provision policies, which mainly targeted fruits and vegetables, and competitive food/beverage standards, which mainly targeted sugar-sweetened beverages, were effective in improving the nutritional knowledge and behaviors of students. 30
Regulating Food Marketing and Production
Regulating food marketing and using economic incentives to promote healthier food choices, such as introducing taxes on sugary beverages and unhealthy snacks, while offering subsidies for fruits and vegetables, should be attempted. Still, more evidence is needed to explore the effectiveness of these interventions.31,32
Screen Time
Contributing Factors
Parental Influence
Parental behavior and attitudes towards screen use can impact screen time among children. A study of 489 Malaysian children (<5 years) showed that prolonged parental screen time and the positive perception of parents towards the influence of screen time on a child’s cognitive health were positively associated with screen time among their children. 33 Using screen devices as discipline tools was also associated with increased screen time in a study of 3141 Lebanese children (7-11 years). 34
Sociodemographic Factors
Sociodemographic factors may affect children’s screen time. Two studies including children and adolescents from Colombia (n = 16 459; 3-17 years) and Iran (n = 14 880; 6-18 years) showed that children and adolescents who came from wealthier families or were living in urban areas had more screen time.35,36
Health Consequences
Behavioral and Psychological Issues
Prolonged screen time could lead to serious behavioral and psychological problems among children and adolescents, emphasizing the importance of mindful screen use in maintaining optimal mental well-being. In the Adolescent Brain Cognitive Development study, 11 875 US children (9-10 years) and their parents showed increased rates of rule-breaking and aggressive behaviors and social and thought problems among children who reported greater screen time. 37 Among 101 350 US children and adolescents (≤17 years) from the 2018-2020 National Survey of Children’s Health (NSCH), prolonged screen time was associated with developmental delay, speech disorder, learning disability, behavioral and conduct problems, autism spectrum disorders (ASD), and attention deficit hyperactivity disorder. 38 A study investigating 1140 Palestinian adolescents (16-17 years) showed that using electronic devices (smartphones, laptops, tablets, and video game players) for a long time was associated with depression and anxiety. 39 Additionally, a study from Egypt, including 560 preschool children from 10 nurseries and their mothers, showed a positive correlation between the duration of media exposure and experiencing learning problems, hyperactivity, impulsivity, conduct problems, anxiety, and psychosomatic problems. 40
Obesity
Obesity is a documented consequence of prolonged screen time. 41 Displacing time that could be spent practicing physical activity, food advertising, and eating while viewing can explain this association. 41 Previous meta-analyses indicated positive associations between screen time and overweight/obesity among children and adolescents.42,43
Vision Problems
Screen time is a near-work activity associated with several visual problems. A study of 1508 students (8-14 years) from Hong Kong detected a dose-response association between smartphone use and digital eye strain. 44 Among 469 Egyptian students (12-14 years), screen time was positively associated with refractive errors (myopia, hyperopia, and astigmatism). 45 In a study involving 7497 Spanish children (5-7 years), children who reported more screen hours were more likely to develop myopia. 46
Sleep Disturbance
Prolonged screen time has a potentially disturbing impact on children’s sleep-wake cycles. In a study including 314 caregivers of Korean children (4-7 years), the frequency of smartphone screen use was associated with bedtime resistance, nighttime awakening, and daytime sleepiness. 47 A systematic review of 109 studies investigating children and adolescents in Western countries showed that prolonged screen time was associated with difficulty falling asleep, short sleep duration, poor sleep quality, and daytime tiredness. 48
Musculoskeletal Problems
Prolonged screen time, particularly when accompanied by poor ergonomics and improper posture, can contribute to musculoskeletal problems. A study including 200 adolescents (10-14 years) from Hong Kong showed that increased computer use was associated with trunk asymmetry, undermining the health-related quality of life. 49 Another study including 1022 adolescents (11-15 years) from the Nordic countries showed a positive association between screen time and physical complaints. 50 A systematic review of 9 Brazilian studies showed a positive association between screen time and non-specific low back pain in adolescents (6-19 years) exposed to screen time for ≥ 3 hours/day. 51 In a dose-response meta-analysis of 9 studies investigating adolescents (11-19 years), there was a positive correlation between daily computer time, daily mobile phone time, daily TV watching, and the risk of low back pain, separately. 52
Potential Interventions
Parental Education
Promoting digital literacy among parents could be effective in minimizing screen time among children and adolescents. A meta-analysis of 204 studies showed that educating parents about the potential dangers of screen time helped them monitor their children’s screen use and minimize their screen time. 53 Intervention strategies with clear goals, feedback, and planning behavioral techniques were noticeably effective. Yet, the effectiveness of most interventions was short-term. 53
Behavior Substitution
Replacing screen use with healthier habits, such as practicing physical activity, is a promising approach. A meta-analysis of 7 randomized controlled trials showed that behavior substitution could effectively reduce screen time. 54
Physical Activity
Contributing Factors
Parental Influence
Parental support and involvement play a crucial role in promoting physical activity among children. A study of 102 Canadian children (3-5 years) showed that children who received greater parental support for physical activity were almost 6 times more likely to be physically active. 55 In a study investigating 717 Japanese children (8-9 years), direct parental assistance for physical activity encouraged children to engage in moderate-to-vigorous physical activity. 56 Another study including 651 adolescents (grade 10) from Bosnia showed that maternal and paternal education was associated with higher physical activity levels among their children. 57
Access to Facilities
The physical environment in which children live, play, and attend school can influence their physical activity levels. A study of 136 US children (2-5 years) showed that the provision of sufficient outdoor active play, using portable play equipment, the presence of a variety of fixed play equipment, and having a suitable indoor play space were associated with higher levels of physical activity. 58 In a systematic review of 14 studies investigating Pacific Island Countries and Territories with Non-European, Non-Asian ancestry children and adolescents, community barriers to physical activity included minimal indoor facilities for physical activity, inadequate footpaths/cycle paths, distance for active transport, and safety issues. 59
Health Consequences
Obesity
Childhood lower physical activity levels are strongly associated with obesity. A study of 1266 Indian children and adolescents (6-17 years) showed that the lack of physical activity, in the form of passive transport to school, not playing during lunch breaks, and not participating in household work, was associated with obesity. 60 Besides, among 1090 South African primary schoolchildren (mean age = 8.3 years), lower moderate-to-vigorous physical activity was associated with overweight/obesity and higher relative body fat. 61 In a study investigating 688 children and adolescents (6-16 years) from Saudi Arabia, lack of physical activity was associated with overweight and obesity. 62
Cardiovascular Disease
The lack of physical activity is a risk factor for CVD. A 30-year cohort study of 5115 US young adults, registered in the Coronary Artery Risk Development in Young Adults (CARDIA) study, showed that lower physical activity levels during younger age were associated with future risk of coronary heart disease, heart failure, and stroke. 63 A study from Poland including 568 children and adolescents with intellectual disabilities (7-18 years) showed that the risk of hypertension was greater among those who reported lower levels of physical activity. 64 A study of 1961 Finnish children and adolescents (3-18 years) showed that physical activity was associated with a lower risk of major CVD risk factors, including obesity, high triglyceride, low high-density lipoprotein cholesterol, and insulin and glucose concentrations, during adulthood. 65
Psychological Problems
Physical activity can support the current and future mental health of children and adolescents. A meta-analysis of 114 studies investigating children and adolescents showed that physical activity was positively associated with psychological well-being, life satisfaction, happiness, and self-image, but negatively associated with stress, depression, negative affect, and psychological distress. 66 A meta-analysis of 31 studies showed that the administration of physical activity, compared to a control group, led to moderate improvements in ASD and depression among children and adolescents. 67
Potential Interventions
Behavioral Change
Promoting physical activity for schoolchildren and adolescents via interventional programs that educate parents, teachers, and schoolchildren about the health impacts of physical activity is important. Freely chosen and unstructured physical activity at schools was shown in a systematic review to have the potential to promote physical activity. 68 A meta-analysis of 57 controlled trials showed that interventions with both school and family or community involvement promoted physical activity among children and adolescents. 69 Multicomponent interventions that aimed to promote physical activity among other healthy lifestyle behaviors were particularly effective. 69
Providing Places for Physical Activity
Providing indoor and outdoor spaces may help children and adolescents engage in physical activity. A study including 179 Chinese children and adolescents (6-14 years) showed that the availability of playgrounds and open green spaces was associated with higher levels of physical activity. 70 Providing enough indoor spaces for 496 preschool US children resulted in greater involvement in physical activity. 71 These findings highlight the need for considering several environmental factors, such as the availability of safe play spaces, walkability, and access to sports and recreational facilities and programs.
Smoking
Contributing Factors
Parental and Peer Influence
Adolescents with parents or peers who smoke are more likely to start smoking due to exposure to and normalization of smoking behaviors. In a prospective cohort study including 8944 UK adolescents (13-15 years) who had never smoked tobacco, having parents or peers with smoking behaviors more than doubled the risk of smoking among those adolescents 2 or 3 years later. 72 Besides, Ethiopian students in rural and urban secondary schools (10-19 years; n = 341) who reported smoking were more likely to have parents, friends, or classmates who were current smokers. 73 In a study including 5705 US parents and their children (9-16 years), parent-youth connectedness and parental monitoring and punishment for smoking significantly decreased the odds of smoking initiation. 74
Media and Marketing Influence
Media and marketing campaigns that encourage or normalize smoking among adolescents have negative impacts. Additionally, the visibility of tobacco products in marketing and advertising can contribute to the perception that they are easy to obtain. The more prevalent and accessible these products appear in media and promotional materials, the more likely adolescents may perceive them as readily available.75-77 A one-year follow-up study of 11 279 US adolescents (12-18 years), registered in the PATH (Population Assessment of Tobacco and Health) study, showed that exposure to and interactions with social media presenting tobacco content were associated with their tobacco use. 75 Among 4332 Nigerian students in rural and urban secondary schools (10-19 years), exposure to tobacco smoking-related media was associated with current smoking. 76 Using data from adolescents (mean age = 14.3 years) from the Global Youth Tobacco Surveys (GYTS) (2014-2017) for Cameroon, Gabon, Comoros, Seychelles, Mauritius, Tanzania, Gambia, Ghana, and Sierra Leone, tobacco marketing was closely associated with smoking initiation. 77
Access to Tobacco
Easy access to tobacco is also a risk factor for smoking. The perception among adolescents that tobacco products are easy to obtain is considered a risk factor for smoking initiation and progression. This perception can contribute to a more permissive attitude toward tobacco use, making it seem more accessible and socially acceptable. 78 A meta-analysis of 11 studies showed a significant association between tobacco outlet density around homes and adolescents’ past-month smoking behavior. 78
Health Consequences
Respiratory Disorders
Smoking during adolescence has negative health impacts on the respiratory system. A study including 2295 Swedish adolescents (16 years) showed that smoking was associated with reduced forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) ratio and increased peripheral airway resistance. 79 Smoking was also associated with a higher risk of chronic bronchitis among 3108 high school students (15-19 years) from Poland. 80 A prospective cohort study including 2609 US students (4-7 grades) showed that smoking ≥ 7 cigarettes/day was associated with an increased risk of asthma. 81
Cardiovascular Disease
Smoking is a major risk factor for CVD, even in young individuals. A Greek study of 238 adolescents (12-15 years) showed that those who reported smoking had a higher prevalence of CVD risk factors, such as obesity and increased blood pressure. 82 In the Harvard Alumni Health Study, cigarette smoking from adolescence to middle age was positively associated with CVD mortality among 5785 US men. 83 In a study including 236 Aboriginal Canadian youths (10-19 years), smoking ≥ 6 cigarettes/day increased CVD risk profile consisting of a higher mean systolic blood pressure and homocysteine level and a lower mean serum folate level. 84
Cancer
Smoking during adolescence significantly increases the risk of developing various types of cancers later in life. A study of 102 098 Kenyan and Nigerian women showed that women who started smoking during their teenage and continued to smoke for 20 years or more had a higher risk of breast cancer compared to those who did not smoke or those who initiated smoking later in age. 85 Similarly, starting smoking at a young age was associated with an increased risk of breast cancer among 102 927 UK women from the Generations Study. 86 A prospective cohort study including 40 897 Japanese middle-aged and older adults showed that those who started smoking before the age of 17 years had significantly a higher risk of lung cancer than those who started smoking after the age of 20 years. 87
Potential Interventions
Cognitive-Based Approaches
Cognitive-based approaches for smoking cessation among adolescents focus on teaching skills to manage withdrawal symptoms and prevent relapse using self-monitoring, coping skills, and positive reinforcement for abstinence. 88 However, previous interventions from the US (n = 407; mean age = 16 years) 89 and France (n = 1814; mean age = 16.9 years) 90 showed that these approaches had minimal impacts. A meta-analysis of interventions showed a modest effect for group counseling, but no effect for individual counseling, mixed delivery methods, or computer or messaging interventions. 91
Pharmaceutical Approaches
Nicotine replacement therapy is a widely used pharmacotherapy for smoking cessation. Previous interventions performed on Dutch adolescents (n = 257; mean age = 16.7 years) showed that nicotine replacement therapy slightly promoted abstinence rates in the short run only.92,93 A meta-analysis of pharmaceutical interventions failed to detect significant impacts of nicotine replacement therapy or other medications on smoking cessation. 91
Restricting Access to Tobacco
Several policies could be attempted to limit youth access and exposure to tobacco, such as increasing the minimum age of sale, limiting the number or type of tobacco outlets, and banning the display of tobacco products. 94 However, limited evidence is available about the effectiveness of these interventions. 94
Alcohol Consumption
Contributing Factors
Parental and Peer Influence
Parents with permissive attitudes toward alcohol can increase the likelihood of adolescent drinking. Peers also have a significant influence because adolescents may feel pressured to drink to fit in, be accepted, or conform to social norms. A study of 3017 US students (6-12 grades) showed that parental and peer drinking behaviors were associated with moderate or heavy drinking among adolescents. 95 Using data from 1183 Taiwanese children (10-11 years) registered in the Child and Adolescent Behaviors in Long-term Evolution (CABLE) study, having parents who both used alcohol, less parental support, and more family conflict were significant predictors of first alcohol use in the following year. 96 Another study including 413 adolescents (16-19 years) in a rural community in Thailand showed that having close friends consuming alcohol increased the likelihood of current drinking. 97
Media and Marketing Influence
The portrayal of alcohol in the media, including movies and advertisements, can glamorize drinking and create a perception that it is a normative behavior for adolescents. Previous systematic reviews detected that the exposure of adolescents to alcohol-related content on the internet, media, and commercials was associated with their subsequent alcohol consumption.98-101
Access to Alcohol
Adolescents who live near alcohol outlets tend to consume more alcohol, despite laws prohibiting alcohol purchases. In a study including Australian adolescents (n = 44 897 from urban settings and 23 311 from regional settings; age = 12-17 years), higher densities of general, on- and off-premises outlets in the immediate neighborhood were associated with a higher likelihood of alcohol consumption. 102 Another study including 1388 sixth-grade US students and their parents showed that accessibility of alcohol at home was associated with significant increases in the trajectories of young adolescent alcohol use and intentions. 103
Health Consequences
Accidents
Underage drinkers are more likely to engage in risky behaviors such as driving under the influence of alcohol, which can lead to accidents, injuries, and fatalities. Alcohol impairs judgment, coordination, and reaction time, making it particularly dangerous for drivers.104,105 A study of 4021 US young adults who reported alcohol drinking showed that those who started drinking at an age <21 years were more likely to get involved in motor vehicle crashes and unintentional injuries compared with individuals who started drinking at the age of 21 years. 106 Starting drinking at an age <14 years increased the odds of motor vehicle crashes by 6 times and unintentional injuries by 4 and a half times. 106 In a study investigating 4729 injured adolescents visiting 6 emergency departments in South Korea, motorcycle-related injuries were strongly associated with alcohol use. 107
Cognitive, Neurological, and Behavioral Problems
Alcohol consumption during adolescence has several cognitive and neural consequences. A study of 89 university students (mean age = 18.8 years) from Brazil showed that participants with a persistent binge drinking trajectory over 2 years performed poorer in memory and executive tasks than those who gave up their pattern of consumption and non-binge drinkers. 108 A longitudinal analysis of 548 US adolescents (12-21 years) showed that those who initiated alcohol drinking were more likely to show MRI-documented disturbed cerebellar growth, suggesting they would experience coordination, imbalance, and gait disorders later in life. 109 Another study including 116 US adolescents (10-19 years) showed a positive association between binge drinking and impulsivity. 110 A study including 828 Norwegian tertiary school students (15-20 years) showed more depressive and psychosomatic complaints and problems with parents and peers among those who reported alcohol intoxication. 111
Cardiovascular Disease
Adolescent binge alcohol consumption is a risk factor for CVD. A study including 1266 UK adolescents (17 years), registered in the Avon Longitudinal Study of Parents and Children (ALSPAC), showed vascular damage attributed to high-intensity alcohol drinking; carotid to femoral pulse wave velocity (PWV) was higher among heavy drinkers, and this effect was augmented among smokers. 112
Potential Interventions
School-Based Interventions
School-based interventions to minimize alcohol misuse among adolescents include a constellation of programs, such as educational programs, life skills training, social norms campaigns, peer-led interventions, and parental involvement programs. Schools may offer screening and counseling services and enhance alternative activities. Previous systematic reviews showed varying effects for these programs.113-115 Interventions characterized by combining more than 1 program and involving parents were more likely to be effective.113-115
Family-Based Interventions
It is important to work with the entire family to address underlying issues that may contribute to alcohol misuse among adolescents. Parental involvement, modeling, dynamics, and communication patterns may influence the behavior of young individuals, including their relationship with alcohol. 114 Parenting skills training, family education programs, and promoting positive interactions and active communication between parents and adolescents were shown in previous systematic reviews to be effective. 114
Restricting Access to Alcohol
Policy strategies aiming at increasing the minimum legal drinking age, reducing the commercial and social access of adolescents to alcohol, enforcing retailer compliance, and controlling the density of alcohol outlets may be useful.116,117 However, effective underage drinking prevention typically involves a combination of these strategies, tailored to the specific cultural and legal context of a given region. Collaborations among government agencies, law enforcement, educators, parents, and community organizations are keys to implementing and enforcing these policies successfully.116,117
Oral Hygiene
Contributing Factors
Parental Factors
Parental socioeconomic status and behaviors can significantly influence the oral hygiene of their children. A study including 2338 parents of children from 167 kindergartens in Poland showed that parental education, income, health literacy, and oral hygiene practices were associated with better oral hygiene among their children. 118 Among 791 Libyan children (12 years), 213 Indonesian children (<12 years), and 400 Indian children (5 years), lower parental education was associated with dental caries.119-121 A systematic review of 14 studies detected that parental tooth brushing behavior, educational and occupational levels, dietary patterns, dental visits, snacking frequency, psychological status, and knowledge of oral health were associated with dental caries among their children. 122
Dietary Behaviors
There is abundant evidence that certain dietary behaviors are risk factors for dental caries. A study of 8647 Portuguese children (4 years) and their mothers showed that children who consumed energy-dense foods and multiple snacks were more likely to develop severe dental caries 3 years later. 123 Among 495 Australian children (5-10 years), chocolate consumption was associated with primary dentition caries. 124 A study investigating 247 preschool children (mean age = 4.1 years) from Saudi Arabia showed a higher risk of dental caries among children who consumed sweetened milk, soft drinks, and sweets. 125 In a study including 698 Iranian children (10-12 years), children who consumed fizzy soft beverages and sweet biscuits > once/day were more likely to have dental caries. 126 A systematic review of ten longitudinal studies showed that the intake of candy, 100% juice, and soft and sweet drinks at bedtime was associated with dental caries in children. 127
Health Consequences
Dental Caries
Bad oral hygiene is a major risk factor for dental caries. Previous studies from the UK (n = 1450; 1.5-4.5 years), Iraq (n = 342; 6 years), and Palestinian refugee camps in Jordan, Lebanon, Syria, Gaza Strip, and West Bank (n = 2781; 12 years) showed that infrequent tooth brushing was associated with dental caries.128-130
Poor Sleep
Bad oral hygiene and dental caries may cause pain and discomfort; factors that can result in poor sleep. A study investigating 332 Japanese preschoolers (3-6 years) showed that children with dental caries slept significantly shorter periods. 131 Having untreated dental caries was associated with trouble sleeping among 1589 students (8-10 years) from Brazil. 132
Psychological and Behavioral Problems
Dental health may also affect psychosocial well-being. Among 793 Brazilian children (8-10 years), cavitated carious lesions were associated with general anxiety. 133 A study of 40 752 US children and adolescents (6-17 years) showed that dental problems were associated with shyness, unhappiness, feelings of worthlessness, and reduced friendliness, especially among those between 15-17 years. 134 In a study including 713 713 Korean adolescents (12-18 years), experiencing oral symptoms was associated with increased suicide ideations and attempts and feelings of sadness and despair. 135
Potential Interventions
School-Based Educational Programs
Raising children’s awareness of oral health, including proper brushing techniques, flossing, and regular dental checkups, should begin in kindergartens and schools. Interventions given by various aids, such as lectures and presentations, flipcharts, drawings, leaflets, albums, models, E-programs, and games were shown in a meta-analysis of 7 trials to be effective in improving oral hygiene and reducing dental caries among school students (5-16 years). 136 Another meta-analysis of 12 trials showed that school-based educational interventions in developing countries could improve oral health knowledge, attitudes, and behaviors. 137
Community-Based Initiatives and Programs
Several community-based initiatives were launched to improve the dental health of children by applying free or low-cost dental diagnostic, preventive, restorative, prosthodontic, and endodontic services, such as dental examinations, cleaning, X-rays, fillings, extractions, and oral surgeries. Other initiatives included oral health educational activities, supervised toothbrushing programs, and motivational interviewing. Besides, community outreach and awareness campaigns targeting parents were shown to be essential for promoting the oral health of their children. These campaigns involved distributing educational materials, organizing workshops, and promoting healthy dental habits.138-140
Unsafe Sex
Contributing Factors
Starting sexual activity at a young age, having a high-risk partner or multiple sex partners, and engaging in unprotected sex are common risky sexual behaviors during adolescence. A systematic review of 16 studies showed that several personal, family, peer, and community factors can contribute to risky sexual behaviors. These factors interact in a way that they could not be described solely, and most studies investigated them together. 141 A study investigating 659 Ethiopian adolescents (15-19 years) showed that poor social support, living out of the family, experiencing parental neglect, and drinking alcohol were associated with risky sexual behaviors. 142 Among 397 adolescents from Thailand (10-19 years), risky sexual behaviors were positively associated with age, male sex, having a boyfriend/girlfriend, uninvolved parenting style, parental approval of sex, perceived peer norms, neighborhood disorganization, and community norms, but negatively associated with religious beliefs and practices, parental monitoring, and neighborhood social cohesion. 143 Another study including 6167 high school and vocational students (mean age = 15.6 years) from Thailand showed that smoking cigarettes, using cannabis, gambling, and experiencing childhood sex abuse were associated with risky sex behaviors. 144 Using data from 1200 Australian adolescents (13-17 years) registered in the Western Australian Pregnancy Cohort [Raine] Study, internalizing (e.g., anxious/depressed, withdrawn) and externalizing (e.g., delinquent, aggressive) behavior problems were associated with earlier first sexual intercourse. 145
Health Consequences
Sexually Transmitted Infections
Chlamydia, gonorrhea, genital herpes, human papillomavirus (HPV), syphilis, and human immunodeficiency virus (HIV) are among the most frequent sexually transmitted infections (STIs) affecting adolescents. In a study including 196 Brazilian adolescents (14-19 years) treated at a family planning outpatient clinic in the western Amazon, 32% had at least 1 STI, with the most prevalent being chlamydia (23%), trichomoniasis (5.6%), herpes simplex (4.6%), and gonorrhea (3.1%). 146 A study including 317 Spanish adolescents (10-19 years) who were referred to an STI clinic in Madrid put the prevalence of gonorrhea, chlamydia, syphilis, and HIV at 21.7%, 17.1%, 4.8%, and 2.4%, respectively. 147 The study also showed that having first sexual relations at a young age was associated with STI. 147 Among 4389 US adolescents (14-20 years) presenting to an Emergency Department, 10% reported a previous history of STIs, and risky sex behaviors were associated with increased odds of STIs history. 148
Exposure to Violence
Adolescents who engage in unsafe sex are more likely to be physically or psychologically victimized. Among 517 sexually active adolescent girls (<18 years) who presented for contraceptive care in the US, experiencing violence was associated with early initiation of sex, having sex with strangers, having multiple partners, or having a partner with multiple partners. 149 A study of 563 African US students (13-19 years) showed a significant association between risky sex behaviors and exposure to community violence. 150 Another study including 179 adolescent girls (mean age = 18.9 years) recruited from social service agencies in the US showed that risky sexual behaviors were associated with both physical assault and sexual victimization. 151
Unwanted Pregnancies
Unwanted pregnancies and abortions are common among female adolescents engaging in unsafe sex. Among sexually active female street-involved adolescents (10-19 years) in Nigeria, 63.7% reported having had sex and 23.7% had a history of pregnancy, of which 59.4% gave a history of induced abortion of the last pregnancy. 152
Potential Interventions
Sex Education
Implementing evidence-based, age-appropriate, and culturally sensitive sex education programs in schools is important. These programs should cover topics like reproductive health, contraception, STIs, consent, and healthy relationships. Providing accurate information empowers adolescents to make informed decisions.153,154
Parental Involvement
Encouraging parents and caregivers to engage in open and non-judgmental conversations about sexuality and relationships is important. Supportive parental involvement can positively influence the decisions of adolescents.155,156
Sleep
Contributing Factors
Excessive Screen Use
Screen time is closely associated with sleep duration and quality. In a study including 314 caregivers of Korean children (4-7 years), the frequency of smartphone screen use was associated with bedtime resistance, sleep duration, nighttime awakening, and daytime sleepiness. 47 Among 11 878 US children (9-10 years), greater screen time was associated with decreased sleep duration and increased sleep onset latency, excessive sleepiness, insomnia, and overall sleep disturbance symptom severity. 157 A systematic review of 49 studies investigating children and adolescents (≤15 years) showed that electronic media use was associated with delayed bedtime and poor sleep quality in children (6-12 years). 48
Lack of Consistent Sleep Habits
Good sleep habits include a consistent sleep routine, avoidance of active and stimulating activities before sleep, utilizing only the bed for sleeping, and adhering to consistent sleep and wake-up times. 158 Having a consistent bedtime routine is often recommended to parents of young children. A study of 405 US mothers and their infants (n = 206; .5-1.5 years) or toddlers (n = 199; 1.5-3 years) showed that having a bedtime routine resulted in significant reductions in problematic sleep behaviors for infants and toddlers. 159 Another study investigating mothers of 10 085 children (≤5 years) from 14 countries showed that having a consistent bedtime routine was associated with better sleep outcomes, including earlier bedtimes, shorter sleep onset latency, reduced night wakings, and increased sleep duration. 160
Sociodemographic and Environmental Factors
Several sociodemographic and environmental factors can affect sleep quality. A study including 855 children (4-9 years) and 1047 adolescents (10-17 years) from Germany showed that lower socioeconomic standard was associated with bedtime resistance, sleep onset delay, sleep-related anxiety, night waking, and parasomnia. 161 Another study of 6728 German adolescents (11-17 years) showed that living with a single parent, having siblings, and residing in provincial, urban, or metropolitan areas were associated with more sleep problems. 162
Health Consequences
Lack of Physical Fitness
Sleep duration and quality may also affect physical fitness. Among 21 857 Chinese children (3-6 years), abnormal sleep duration was associated with low physical fitness. 163 A systematic review of 6 studies investigating 5797 children and adolescents (6-19 years) from 11 countries showed that shorter periods of sleep and worse sleep quality were associated with lower levels of physical fitness. 164
Poor Cognitive Functions
Inadequate sleep may have disruptive effects on the cognitive function and learning capacity of children and adolescents. In a large meta-analysis of 86 studies investigating 35 936 children (5-12 years), sleep duration was positively associated with cognitive performance, especially executive functioning, performance on tasks that address multiple cognitive domains, and school performance, but negatively associated with both internalizing and externalizing behavioral problems. 165
Obesity
Sleep duration may also be associated with obesity. A meta-analysis of 33 articles, involving 57 848 children and adolescents, revealed statistically significant associations between short sleep duration and obesity. In dose-response meta-analyses, short sleep duration increased the risk of obesity in toddlers (1-2 years) by 20%, in preschool-aged children (3-5 years) by 58%, and in school-aged children (6-13 years) by 82%. 166 A meta-analysis of 25 prospective cohort studies including 56 584 children and adolescents showed that short sleep duration was associated with obesity and weight gain during follow-up. 167
Potential Interventions
Behavioral Interventions
Several behavioral changes could improve sleep in children and adolescents, such as establishing a regular sleep routine by setting a consistent bedtime and wake-up time, limiting screen time before bed, creating a sleep-friendly environment by keeping the room dark, quiet, and at a comfortable temperature, encouraging regular physical activity, and limiting caffeine and sugar intake, especially in the late afternoon and evening.168-170
Pharmaceutical Interventions
Melatonin, antihistamines, benzodiazepines, and alpha agonists are the most commonly prescribed medications for the management of sleep disorders in children and adolescents. However, evidence of their long-term safety and efficacy is not robust.171,172
Conclusion
This review highlighted various lifestyle behaviors that play a pivotal role in shaping the overall health of children and adolescents, including dietary patterns, screen time, physical activity, smoking, alcohol consumption, oral hygiene, unsafe sex, and sleep duration. Identifying the factors influencing these behaviors allows for a better understanding of the complex interplay between individual, familial, societal, and environmental determinants. Additionally, we described the health consequences of unhealthy lifestyle behaviors and potential interventions that may revert these behaviors or mitigate their effects. We believe that this review can serve as a resource for policymakers, health care professionals, parents, and teachers, emphasizing the need for collective efforts in enhancing healthy lifestyle behaviors among children and adolescents.
Supplemental Material
Supplemental Material for Lifestyle Behaviors of Childhood and Adolescence: Contributing Factors, Health Consequences, and Potential Interventions by Ahmed Arafa, Yuka Yasui, Yoshihiro Kokubo, Yuka Kato, Chisa Matsumoto, Masayuki Teramoto, Saya Nosaka, and Miho Kogirima in American Journal of Lifestyle Medicine
Acknowledgments
We would like to thank Dr Rena Kashima.
Appendix
Abbreviations
- ALSPAC
Avon Longitudinal Study of Parents and Children
- ASD
Autism spectrum disorders
- CARDIA
Coronary Artery Risk Development in Young Adults
- CVD
Cardiovascular disease
- FEV1
Forced expiratory volume in one second
- FVC
Forced vital capacity
- GYTS
Global Youth Tobacco Surveys
- HIV
Human immunodeficiency virus
- HPV
Human papillomavirus
- IDEFICS
Identification and prevention of Dietary- and lifestyle-induced health EFfects In Children and infantS
- M-TEENS
Military Teenagers Environments, Exercise, and Nutrition Study
- NHSII
Nurses’ Health Study II
- NSCH
National Survey of Children’s Health
- PATH
Population Assessment of Tobacco and Health
- PWV
Pulse wave velocity
- STI
Sexually transmitted infections
Authors’ Contributions: A. A. (conceptualization, literature review, and manuscript drafting), Y. K. (conceptualization, funding acquisition, and supervision), and all authors (revision and editing).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Intramural Research Fund for the cardiovascular diseases of the National Cerebral and Cardiovascular Center (20-4-9, 23-B-9), the JH Young Researcher Grant, the Health and Labour Sciences Research Grants of the Ministry of Health, Labour, and Welfare of Japan, AMED (21dk0207053h0001), the Japan Science and Technology Agency (JPMJPF2018), and the Cross-ministerial Strategic Innovation Promotion Program (SIP) “Building a Resilient and Nourishing Food Chain for a Sustainable Future.” From the Bio-oriented Technology Research Advancement Institution (JP J012287).
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Ahmed Arafa https://orcid.org/0000-0002-3335-2243
Saya Nosaka https://orcid.org/0009-0002-5730-6759
References
- 1.Lioret S, Campbell KJ, McNaughton SA, et al. Lifestyle patterns begin in early childhood, persist and are socioeconomically patterned, confirming the importance of early life interventions. Nutrients. 2020;12(3):724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yan Y, Mi J. Noncommunicable chronic disease prevention should start from childhood. Pediatr Investig. 2021;5(1):3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wijlaars LP, Gilbert R, Hardelid P. Chronic conditions in children and young people: learning from administrative data. Arch Dis Child. 2016;101(10):881-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Armocida B, Monasta L, Sawyer S, et al. Burden of non-communicable diseases among adolescents aged 10-24 years in the EU, 1990-2019: a systematic analysis of the Global Burden of Diseases Study 2019. Lancet Child Adolesc Health. 2022;6(6):367-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mayne SL, Virudachalam S, Fiks AG. Clustering of unhealthy behaviors in a nationally representative sample of U.S. children and adolescents. Prev Med. 2020;130:105892. [DOI] [PubMed] [Google Scholar]
- 6.Shurney D, Gustafson PA. Lifestyle medicine in children. Am J Lifestyle Med. 2019;14(1):54-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim AR, Lee S, Park JH. An analysis of the factors affecting children and adolescent lifestyle in South Korea: a cross-sectional study with KCYPS 2018. PLoS One. 2022;17(2):e0263923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marconcin P, Matos MG, Ihle A, et al. Trends of healthy lifestyles among adolescents: an analysis of more than half a million participants from 32 countries between 2006 and 2014. Front Pediatr. 2021;9:645074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pigaiani Y, Zoccante L, Zocca A, et al. Adolescent lifestyle behaviors, coping strategies and subjective wellbeing during the COVID-19 pandemic: an online student survey. Healthcare (Basel). 2020;8(4):472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gibson EL, Androutsos O, Moreno L, et al. Influences of parental snacking-related attitudes, behaviours and nutritional knowledge on young children's healthy and unhealthy snacking: the ToyBox Study. Nutrients. 2020;12(2):432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang R, Yu X, Yu Y, et al. Family food environments and their association with primary and secondary students' food consumption in Beijing, China: a cross-sectional study. Nutrients. 2022;14(9):1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hammons AJ, Fiese BH. Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics. 2011;127(6):e1565-1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richardson AS, Nicosia N, Ghosh-Dastidar MB, Datar A. School food and beverage availability and children's diet, purchasing, and obesity: evidence from a natural experiment. J Adolesc Health. 2020;67(6):804-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sim S, Veugelers PJ, Prowse R, Nykiforuk CI, Maximova K. Unhealthy food options in the school environment are associated with diet quality and body weights of elementary school children in Canada. Public Health Nutr. 2021;24(14):4572-4581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mc Carthy CM, de Vries R, Mackenbach JD. The influence of unhealthy food and beverage marketing through social media and advergaming on diet-related outcomes in children-a systematic review. Obes Rev. 2022;23(6):e13441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinnig PF, Monteiro JS, de Assis MAA, et al. Dietary patterns of children and adolescents from high, medium and low human development countries and associated socioeconomic factors: a systematic review. Nutrients. 2018;10(4):436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jakobsen DD, Brader L, Bruun JM. Association between food, beverages and overweight/obesity in children and adolescents-a systematic review and meta-analysis of observational studies. Nutrients. 2023;15(3):764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fernández-Alvira JM, Bammann K, Eiben G, et al. Prospective associations between dietary patterns and body composition changes in European children: the IDEFICS study. Public Health Nutr. 2017;20(18):3257-3265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ogum Alangea D, Aryeetey RN, Gray HL, Laar AK, Adanu RMK. Dietary patterns and associated risk factors among school age children in urban Ghana. BMC Nutr. 2018;4:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van den Hooven EH, Heppe DH, Kiefte-de Jong JC, et al. Infant dietary patterns and bone mass in childhood: the Generation R Study. Osteoporos Int. 2015;26(5):1595-1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suhett LG, Filgueiras MS, de Novaes JF, Sukumar D. Role of diet quality in bone health in children and adolescents: a systematic review. Nutr Rev. 2023;82(1):47-59. [DOI] [PubMed] [Google Scholar]
- 22.Thomas MM, Gugusheff J, Baldwin HJ, Gale J, Boylan S, Mihrshahi S. Healthy lifestyle behaviours are associated with children's psychological health: a cross-sectional study. Int J Environ Res Publ Health. 2020;17(20):7509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacka FN, Kremer PJ, Leslie ER, et al. Associations between diet quality and depressed mood in adolescents: results from the Australian Healthy Neighbourhoods Study. Aust N Z J Psychiatr. 2010;44(5):435-442. [DOI] [PubMed] [Google Scholar]
- 24.Gratão LHA, Pessoa MC, Rodrigues da Silva TP, et al. Dietary patterns, breakfast consumption, meals with family and associations with common mental disorders in adolescents: a school-based cross-sectional study. BMC Publ Health. 2022;22(1):980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dahm CC, Chomistek AK, Jakobsen MU, et al. Adolescent diet quality and cardiovascular disease risk factors and incident cardiovascular disease in middle-aged women. J Am Heart Assoc. 2016;5(12):e003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shi L, Krupp D, Remer T. Salt, fruit and vegetable consumption and blood pressure development: a longitudinal investigation in healthy children. Br J Nutr. 2014;111(4):662-671. [DOI] [PubMed] [Google Scholar]
- 27.Honicky M, Cardoso SM, Kunradi Vieira FG, Hinnig PF, Back IC, Moreno YMF. Ultra-processed food intake is associated with children and adolescents with congenital heart disease clustered by high cardiovascular risk factors. Br J Nutr. 2023;129(7):1163-1171. [DOI] [PubMed] [Google Scholar]
- 28.Kuwahara M, Eum W. Effects of childhood nutrition education from school and family on eating habits of Japanese adults. Nutrients. 2022;14(12):2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zaltz DA, Hecht AA, Neff RA, et al. Healthy eating policy improves children's diet quality in early care and education in South Carolina. Nutrients. 2020;12(6):1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Micha R, Karageorgou D, Bakogianni I, et al. Effectiveness of school food environment policies on children's dietary behaviors: a systematic review and meta-analysis. PLoS One. 2018;13(3):e0194555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kelly B, Backholer K, Boyland E, et al. Contemporary approaches for monitoring food marketing to children to progress policy actions. Curr Nutr Rep. 2023;12(1):14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sacks G, Kwon J, Backholer K. Do taxes on unhealthy foods and beverages influence food purchases? Curr Nutr Rep. 2021;10(3):179-187. [DOI] [PubMed] [Google Scholar]
- 33.Raj D, Mohd Zulkefli N, Mohd Shariff Z, Ahmad N. Determinants of excessive screen time among children under five years old in Selangor, Malaysia: a cross-sectional study. Int J Environ Res Publ Health. 2022;19(6):3560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hawi NS, Rupert MS. Impact of e-Discipline on children's screen time. Cyberpsychol, Behav Soc Netw. 2015;18(6):337-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.González SA, Sarmiento OL, Florez-Pregonero A, Katzmarzyk PT, Chaput JP, Tremblay MS. Prevalence and associated factors of excessive recreational screen time among Colombian children and adolescents. Int J Public Health. 2022;67:1604217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mozafarian N, Motlagh ME, Heshmat R, et al. Factors Associated with screen time in Iranian children and adolescents: the CASPIAN-IV Study. Int J Prev Med. 2017;8:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guerrero MD, Barnes JD, Chaput JP, Tremblay MS. Screen time and problem behaviors in children: exploring the mediating role of sleep duration. Int J Behav Nutr Phys Activ. 2019;16(1):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qu G, Hu W, Meng J, et al. Association between screen time and developmental and behavioral problems among children in the United States: evidence from 2018 to 2020 NSCH. J Psychiatr Res. 2023;161:140-149. [DOI] [PubMed] [Google Scholar]
- 39.Hamshari S, Yaseen S, Zayed M, Dalasha A, Maraqa B, Nazzal Z. Adolescents' electronic devices use during the COVID-19 pandemic and its relationship to anxiety and depression levels: a cross-sectional study. BMC Psychiatr. 2024;24(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zoromba MA, Abdelgawad D, Hashem S, El-Gazar H, Abd El Aziz MA. Association between media exposure and behavioral problems among preschool children. Front Psychol. 2023;14:1080550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Robinson TN, Banda JA, Hale L, et al. Screen media exposure and obesity in children and adolescents. Pediatrics. 2017;140(Suppl 2):S97-S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wu Y, Amirfakhraei A, Ebrahimzadeh F, Jahangiry L, Abbasalizad-Farhangi M. Screen time and body mass index among children and adolescents: a systematic review and meta-analysis. Front Pediatr. 2022;10:822108. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 43.Haghjoo P, Siri G, Soleimani E, Farhangi MA, Alesaeidi S. Screen time increases overweight and obesity risk among adolescents: a systematic review and dose-response meta-analysis. BMC Prim Care. 2022;23(1):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chu GCH, Chan LYL, Do CW, et al. Association between time spent on smartphones and digital eye strain: a 1-year prospective observational study among Hong Kong children and adolescents. Environ Sci Pollut Res Int. 2023;30(20):58428-58435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arafa AEED, Ewis AAE, Mahran WM, Mohamed AAE, El-Shabrawy EM. Prevalence and risk factors of refractive errors among preparatory school students in Beni-Suef, Egypt. J Public Health. 2019;27:43-47. [Google Scholar]
- 46.Alvarez-Peregrina C, Sánchez-Tena MÁ, Martinez-Perez C, Villa-Collar C. The relationship between screen and outdoor time with rates of myopia in Spanish children. Front Public Health. 2020;8:560378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee S, Kim S, Yang S, Shin Y. Effects of frequent smartphone use on sleep problems in children under 7 years of age in Korea: a 4-year longitudinal study. Int J Environ Res Publ Health. 2022;19(16):10252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lund L, Sølvhøj IN, Danielsen D, Andersen S. Electronic media use and sleep in children and adolescents in Western countries: a systematic review. BMC Publ Health. 2021;21(1):1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cheung MC, Lai JSK, Yip J, Cheung JPY. Increased computer use is associated with trunk asymmetry that negatively impacts health-related quality of life in early adolescents. Patient Prefer Adherence. 2021;15:2289-2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Torsheim T, Eriksson L, Schnohr CW, Hansen F, Bjarnason T, Välimaa R. Screen-based activities and physical complaints among adolescents from the Nordic countries. BMC Publ Health. 2010;10:324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guerra PH, Martelo R, da Silva MN, de Andrade GF, Christofaro DGD, Loch MR. Screen time and low back pain in children and adolescents: a systematic review of Brazilian studies. Rev Paul Pediatr. 2023;41:e2021342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yue C, Wenyao G, Xudong Y, et al. Dose-response relationship between daily screen time and the risk of low back pain among children and adolescents: a meta-analysis of 57831 participants. Environ Health Prev Med. 2023;28:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jones A, Armstrong B, Weaver RG, Parker H, von Klinggraeff L, Beets MW. Identifying effective intervention strategies to reduce children's screen time: a systematic review and meta-analysis. Int J Behav Nutr Phys Activ. 2021;18(1):126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lewis L, Povey R, Rose S, et al. What behavior change techniques are associated with effective interventions to reduce screen time in 0-5 year olds? A narrative systematic review. Prev Med Rep. 2021;23:101429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zecevic CA, Tremblay L, Lovsin T, Michel L. Parental influence on young children's physical activity. Int J Pediatr. 2010;2010:468526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hosokawa R, Fujimoto M, Katsura T. Parental support for physical activity and children's physical activities: a cross-sectional study. BMC Sports Sci Med Rehabil. 2023;15(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Maric D, Kvesic I, Lujan IK, et al. Parental and familial factors influencing physical activity levels in early adolescence: a prospective study. Healthcare (Basel). 2020;8(4):532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gunter KB, Rice KR, Ward DS, Trost SG. Factors associated with physical activity in children attending family child care homes. Prev Med. 2012;54(2):131-133. [DOI] [PubMed] [Google Scholar]
- 59.Peralta LR, Cinelli RL, Cotton W, Morris S, Galy O, Caillaud C. The barriers to and facilitators of physical activity and sport for Oceania with Non-European, Non-Asian (ONENA) ancestry children and adolescents: a mixed studies systematic review. Int J Environ Res Publ Health. 2022;19(18):11554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bhargava M, Kandpal SD, Aggarwal P. Physical activity correlates of overweight and obesity in school-going children of Dehradun, Uttarakhand. J Fam Med Prim Care. 2016;5(3):564-568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gerber M, Lang C, Beckmann J, et al. Physical activity, sedentary behaviour, weight status, and body composition among South African primary schoolchildren. Int J Environ Res Publ Health. 2022;19(18):11836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Almaqhawi A, Alkhateeb A, AlHussain AK, Alqahtani KS, Aldrweesh AK, Aljarri SA. Prevalence and associated risk factors of childhood obesity in the Eastern Province of Saudi Arabia. Cureus. 2022;14(10):e30015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nagata JM, Vittinghoff E, Gabriel KP, et al. Physical activity from young adulthood to middle age and premature cardiovascular disease events: a 30-year population-based cohort study. Int J Behav Nutr Phys Activ. 2022;19(1):123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wyszyńska J, Podgórska-Bednarz J, Dereń K, Mazur A. The relationship between physical activity and screen time with the risk of hypertension in children and adolescents with intellectual disability. BioMed Res Int. 2017;2017:1940602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kallio P, Pahkala K, Heinonen OJ, et al. Physical inactivity from youth to adulthood and adult cardiometabolic risk profile. Prev Med. 2021;145:106433. [DOI] [PubMed] [Google Scholar]
- 66.Rodriguez-Ayllon M, Cadenas-Sánchez C, Estévez-López F, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 2019;49(9):1383-1410. [DOI] [PubMed] [Google Scholar]
- 67.Peng S, Fang Y, Othman AT, Liang J. Meta-analysis and systematic review of physical activity on neurodevelopment disorders, depression, and obesity among children and adolescents. Front Psychol. 2022;13:940977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Johnstone A, Hughes AR, Martin A, Reilly JJ. Utilising active play interventions to promote physical activity and improve fundamental movement skills in children: a systematic review and meta-analysis. BMC Publ Health. 2018;18(1):789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007;335(7622):703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ma M, Adeney M, Chen W, Deng D, Tan S. To create a safe and healthy place for children: the associations of green open space characteristics with children's use. Front Public Health. 2022;9:813976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Neshteruk CD, Mazzucca S, Østbye T, Ward DS. The physical environment in family childcare homes and children's physical activity. Child Care Health Dev. 2018;44(5):746-752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vrinten C, Parnham JC, Filippidis FT, Hopkinson NS, Laverty AA. Risk factors for adolescent smoking uptake: analysis of prospective data from the UK Millennium Cohort Study. Tob Induc Dis. 2022;20:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Roble AK, Osman MO, Lathwal OP, Aden AA. Prevalence of cigarette smoking and associated factors among adolescents in Eastern Ethiopia, 2020. Subst Abuse Rehabil. 2021;12:73-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mahabee-Gittens EM, Xiao Y, Gordon JS, Khoury JC. The dynamic role of parental influences in preventing adolescent smoking initiation. Addict Behav. 2013;38(4):1905-1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cavazos-Rehg P, Li X, Kasson E, et al. Exploring how social media exposure and interactions are associated with ENDS and tobacco use in adolescents from the PATH Study. Nicotine Tob Res. 2021;23(3):487-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Itanyi IU, Onwasigwe CN, Ossip D, et al. Predictors of current tobacco smoking by adolescents in Nigeria: interaction between school location and socioeconomic status. Tob Induc Dis. 2020;18:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chido-Amajuoyi OG, Fueta P, Mantey D. Age at smoking initiation and prevalence of cigarette use among youths in Sub-Saharan Africa, 2014-2017. JAMA Netw Open. 2021;4(5):e218060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Finan LJ, Lipperman-Kreda S, Abadi M, et al. Tobacco outlet density and adolescents' cigarette smoking: a meta-analysis. Tob Control. 2019;28(1):27-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Thacher JD, Schultz ES, Hallberg J, et al. Tobacco smoke exposure in early life and adolescence in relation to lung function. Eur Respir J. 2018;51(6):1702111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Saracen A. Cigarette smoking and respiratory system diseases in adolescents. Adv Exp Med Biol. 2017;944:81-85. [DOI] [PubMed] [Google Scholar]
- 81.Gilliland FD, Islam T, Berhane K, et al. Regular smoking and asthma incidence in adolescents. Am J Respir Crit Care Med. 2006;174(10):1094-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Flouris AD, Faught BE, Klentrou P. Cardiovascular disease risk in adolescent smokers: evidence of a 'smoker lifestyle. J Child Health Care. 2008;12(3):221-231. [DOI] [PubMed] [Google Scholar]
- 83.Whitley E, Lee IM, Sesso HD, Batty GD. Association of cigarette smoking from adolescence to middle-age with later total and cardiovascular disease mortality: the Harvard Alumni Health Study. J Am Coll Cardiol. 2012;60(18):1839-1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Retnakaran R, Hanley AJ, Connelly PW, Harris SB, Zinman B. Cigarette smoking and cardiovascular risk factors among Aboriginal Canadian youths. CMAJ (Can Med Assoc J). 2005;173(8):885-889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Odiase EJ. Risk of breast cancer amongst women who start smoking as teenagers. Breast Cancer Res. 2009;11(Suppl 1):P12. [Google Scholar]
- 86.Jones ME, Schoemaker MJ, Wright LB, Ashworth A, Swerdlow AJ. Smoking and risk of breast cancer in the Generations Study cohort. Breast Cancer Res. 2017;19(1):118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hara M, Inoue M, Shimazu T, Yamamoto S, Tsugane S, Japan Public Health Center-based Prospective Study Group . The association between cancer risk and age at onset of smoking in Japanese. J Epidemiol. 2010;20(2):128-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Simon P, Kong G, Cavallo DA, Krishnan-Sarin S. Update of adolescent smoking cessation interventions: 2009-2014. Curr Addict Rep. 2015;2(1):15-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Joffe A, McNeely C, Colantuoni E, An MW, Wang W, Scharfstein D. Evaluation of school-based smoking-cessation interventions for self-described adolescent smokers. Pediatrics. 2009;124(2):e187-194. [DOI] [PubMed] [Google Scholar]
- 90.Minary L, Cambon L, Martini H, et al. Efficacy of a smoking cessation program in a population of adolescent smokers in vocational schools: a public health evaluative controlled study. BMC Publ Health. 2013;13:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fanshawe TR, Halliwell W, Lindson N, Aveyard P, Livingstone-Banks J, Hartmann-Boyce J. Tobacco cessation interventions for young people. Cochrane Database Syst Rev. 2017;11(11):CD003289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Scherphof CS, van den Eijnden RJ, Engels RC, Vollebergh WA. Short-term efficacy of nicotine replacement therapy for smoking cessation in adolescents: a randomized controlled trial. J Subst Abuse Treat. 2014;46(2):120-127. [DOI] [PubMed] [Google Scholar]
- 93.Scherphof CS, van den Eijnden RJ, Engels RC, Vollebergh WA. Long-term efficacy of nicotine replacement therapy for smoking cessation in adolescents: a randomized controlled trial. Drug Alcohol Depend. 2014;140:217-220. [DOI] [PubMed] [Google Scholar]
- 94.Kuijpers TG, Kunst AE, Willemsen MC. Policies that limit youth access and exposure to tobacco: a scientific neglect of the first stages of the policy process. BMC Publ Health. 2019;19(1):825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Forney MA, Forney PD, Ripley WK. Predictor variables of adolescent drinking. Adv Alcohol Subst Abuse. 1989;8(2):97-117. [DOI] [PubMed] [Google Scholar]
- 96.Hung CC, Yen LL, Wu WC. Association of parents' alcohol use and family interaction with the initiation of alcohol use by sixth graders: a preliminary study in Taiwan. BMC Publ Health. 2009;9:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pramaunururut P, Anuntakulnathee P, Wangroongsarb P, et al. Alcohol consumption and its associated factors among adolescents in a rural community in central Thailand: a mixed-methods study. Sci Rep. 2022;12(1):19605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Finan LJ, Lipperman-Kreda S, Grube JW, Balassone A, Kaner E. Alcohol marketing and adolescent and young adult alcohol use behaviors: a systematic review of cross-sectional studies. J Stud Alcohol Drugs Suppl. 2020;19(Suppl 19):42-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Smith LA, Foxcroft DR. The effect of alcohol advertising, marketing and portrayal on drinking behaviour in young people: systematic review of prospective cohort studies. BMC Publ Health. 2009;9:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gupta H, Pettigrew S, Lam T, Tait RJ. A systematic review of the impact of exposure to internet-based alcohol-related content on young people's alcohol use behaviours. Alcohol Alcohol. 2016;51(6):763-771. [DOI] [PubMed] [Google Scholar]
- 101.Anderson P, de Bruijn A, Angus K, Gordon R, Hastings G. Impact of alcohol advertising and media exposure on adolescent alcohol use: a systematic review of longitudinal studies. Alcohol Alcohol. 2009;44(3):229-243. [DOI] [PubMed] [Google Scholar]
- 102.Azar D, White V, Coomber K, et al. The association between alcohol outlet density and alcohol use among urban and regional Australian adolescents. Addiction. 2016;111(1):65-72. [DOI] [PubMed] [Google Scholar]
- 103.Komro KA, Maldonado-Molina MM, Tobler AL, Bonds JR, Muller KE. Effects of home access and availability of alcohol on young adolescents' alcohol use. Addiction. 2007;102(10):1597-1608. [DOI] [PubMed] [Google Scholar]
- 104.Haegerich TM, Shults RA, Oman RF, Vesely SK. The predictive influence of youth assets on drinking and driving behaviors in adolescence and young adulthood. J Prim Prev. 2016;37(3):231-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mayhew DR, Donelson AC, Beirness DJ, Simpson HM. Youth, alcohol and relative risk of crash involvement. Accid Anal Prev. 1986;18(4):273-287. [DOI] [PubMed] [Google Scholar]
- 106.Hingson RW, Edwards EM, Heeren T, Rosenbloom D. Age of drinking onset and injuries, motor vehicle crashes, and physical fights after drinking and when not drinking. Alcohol Clin Exp Res. 2009;33(5):783-790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Noh H, Jung KY, Park HS, Cheon YJ. Characteristics of alcohol-related injuries in adolescents visiting the emergency department. J Korean Med Sci. 2011;26(3):431-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mota N, Parada M, Crego A, et al. Binge drinking trajectory and neuropsychological functioning among university students: a longitudinal study. Drug Alcohol Depend. 2013;133(1):108-114. [DOI] [PubMed] [Google Scholar]
- 109.Sullivan EV, Brumback T, Tapert SF, et al. Disturbed cerebellar growth trajectories in adolescents who initiate alcohol drinking. Biol Psychiatr. 2020;87(7):632-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jones SA, Steele JS, Nagel BJ. Binge drinking and family history of alcoholism are associated with an altered developmental trajectory of impulsive choice across adolescence. Addiction. 2017;112(7):1184-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hoel S, Eriksen BM, Breidablik HJ, Meland E. Adolescent alcohol use, psychological health, and social integration. Scand J Publ Health. 2004;32(5):361-367. [DOI] [PubMed] [Google Scholar]
- 112.Charakida M, Georgiopoulos G, Dangardt F, et al. Early vascular damage from smoking and alcohol in teenage years: the ALSPAC study. Eur Heart J. 2019;40(4):345-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Strøm HK, Adolfsen F, Fossum S, Kaiser S, Martinussen M. Effectiveness of school-based preventive interventions on adolescent alcohol use: a meta-analysis of randomized controlled trials. Subst Abuse Treat Prev Pol. 2014;9:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Das JK, Salam RA, Arshad A, Finkelstein Y, Bhutta ZA. Interventions for adolescent substance abuse: an overview of systematic reviews. J Adolesc Health. 2016;59(4S):S61-S75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hennessy EA, Tanner-Smith EE. Effectiveness of brief school-based interventions for adolescents: a meta-analysis of alcohol use prevention programs. Prev Sci. 2015;16(3):463-474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Komro KA, Toomey TL. Strategies to prevent underage drinking. Alcohol Res Health. 2002;26(1):5-14. [PMC free article] [PubMed] [Google Scholar]
- 117.Harding FM, Hingson RW, Klitzner M, et al. Underage drinking: a review of trends and prevention strategies. Am J Prev Med. 2016;51(4 Suppl 2):S148-S157. [DOI] [PubMed] [Google Scholar]
- 118.Chawłowska E, Karasiewicz M, Lipiak A, et al. Exploring the relationships between children's oral health and parents' oral health knowledge, literacy, behaviours and adherence to recommendations: a cross-sectional survey. Int J Environ Res Publ Health. 2022;19(18):11288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Huew R, Waterhouse PJ, Moynihan PJ, Maguire A. Prevalence and severity of dental caries in Libyan schoolchildren. Int Dent J. 2011;61(4):217-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Bramantoro T, Setijanto RD, Palupi R, Aghazy AZ, Irmalia WR. Dental caries and associated factors among primary school children in metropolitan city with the largest Javanese race population: a crosssectional study. Contemp Clin Dent. 2019;10(2):274-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sujlana A, Pannu PK. Family related factors associated with caries prevalence in the primary dentition of five-year-old children. J Indian Soc Pedod Prev Dent. 2015;33(2):83-87. [DOI] [PubMed] [Google Scholar]
- 122.Anwar DS, Mohd Yusof MYP, Ahmad MS, Md Sabri BA. Family influences on the dental caries status of children with special health care needs: a systematic review. Children. 2022;9(12):1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Carvalho Silva C, Gavinha S, Vilela S, et al. Dietary patterns and oral health behaviours associated with caries development from 4 to 7 years of age. Life. 2021;11(7):609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Arora A, Manohar N, John JR. Factors associated with dental caries in primary dentition in a non-fluoridated rural community of New South Wales, Australia. Int J Environ Res Publ Health. 2017;14(12):1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.al Ghanim NA, Adenubi JO, Wyne AA, Khan NB. Caries prediction model in pre-school children in Riyadh, Saudi Arabia. Int J Paediatr Dent. 1998;8(2):115-122. [DOI] [PubMed] [Google Scholar]
- 126.Almasi A, Rahimiforoushani A, Eshraghian MR, et al. Effect of nutritional habits on dental caries in permanent dentition among schoolchildren aged 10-12 years: a zero-inflated generalized Poisson regression model approach. Iran J Public Health. 2016;45(3):353-361. [PMC free article] [PubMed] [Google Scholar]
- 127.Mahboobi Z, Pakdaman A, Yazdani R, Azadbakht L, Montazeri A. Dietary free sugar and dental caries in children: a systematic review on longitudinal studies. Health Promot Perspect. 2021;11(3):271-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gibson S, Williams S. Dental caries in pre-school children: associations with social class, toothbrushing habit and consumption of sugars and sugar-containing foods. Further analysis of data from the National Diet and Nutrition Survey of children aged 1.5-4.5 years. Caries Res. 1999;33(2):101-113. [DOI] [PubMed] [Google Scholar]
- 129.Al-Mendalawi MD, Karam NT. Risk factors associated with deciduous tooth decay in Iraqi preschool children. Avicenna J Med. 2014;4(1):5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Biscaglia L, di Caccamo P, Terrenato I, et al. Oral health status and caries trend among 12-year old Palestine refugee students: results from the UNRWA's oral health surveys 2011 and 2016. BMC Oral Health. 2019;19(1):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ogawa M, Ogi H, Nakamura D, Nakamura T, Izawa KP. Association between insufficient sleep and dental caries among preschoolers in Japan: a cross-sectional multicentre study. Eur J Investig Health Psychol Educ. 2021;12(1):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Moro J, Santos P, Giacomin A, Cardoso M, Bolan M. Association between trouble sleeping and oral conditions among schoolchildren. Rev Paul Pediatr. 2020;39:e2019342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.de Lima LCM, Bernardino VMM, Leal TR, Granja GL, Paiva SM, Granville-Garcia AF. Sleep disorders, anxiety and obesity associated with untreated dental caries in children eight to ten years of age. J Publ Health Dent. 2024;84(1):13-20. [DOI] [PubMed] [Google Scholar]
- 134.Guarnizo-Herreño CC, Wehby GL. Children's dental health, school performance, and psychosocial well-being. J Pediatr. 2012;161(6):1153-1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lee KH, Lee WK, Jung ES, Choi YY. Associations between mental health and oral health among Korean adolescents: analysis of the national surveys (2008-2017). Int J Environ Res Publ Health. 2021;18(20):10660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gurav KM, Shetty V, Vinay V, Bhor K, Jain C, Divekar P. Effectiveness of oral health educational methods among school children aged 5-16 years in improving their oral health status: a meta-analysis. Int J Clin Pediatr Dent. 2022;15(3):338-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Dadipoor S, Akbarizadeh F, Ghaffari M, Alipour A, Safari-Moradabadi A. Educational intervention of improve student's oral health: a systematic review and meta-analysis school-based. Iran J Public Health. 2023;52(3):500-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rowan-Legg A, Canadian Paediatric Society, Community Paediatrics Committee . Oral health care for children - a call for action. Paediatr Child Health. 2013;18(1):37-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.de Silva AM, Hegde S, Akudo Nwagbara B, et al. Community-based population-level interventions for promoting child oral health. Cochrane Database Syst Rev. 2016;9(9):CD009837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Cruz S, Chi DL, Huebner CE. Oral health services within community-based organizations for young children with special health care needs. Spec Care Dentist. 2016;36(5):243-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Alimoradi Z, Kariman N, Simbar M, Ahmadi F. Contributing factors to high-risk sexual behaviors among Iranian adolescent girls: a systematic review. Int J Community Based Nurs Midwifery. 2017;5(1):2-12. [PMC free article] [PubMed] [Google Scholar]
- 142.Srahbzu M, Tirfeneh E. Risky sexual behavior and associated factors among adolescents aged 15-19 years at governmental high schools in Aksum Town, Tigray, Ethiopia, 2019: an institution-based, cross-sectional study. BioMed Res Int. 2020;2020:3719845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Settheekul S, Fongkaew W, Viseskul N, Boonchieng W, Voss JG. Factors influencing sexual risk behaviors among adolescents: a community-based participatory study. Nurs Health Sci. 2019;21(2):186-197. [DOI] [PubMed] [Google Scholar]
- 144.Thepthien BO. Celyn. Risky sexual behavior and associated factors among sexually-experienced adolescents in Bangkok, Thailand: findings from a school web-based survey. Reprod Health. 2022;19(1):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Skinner SR, Robinson M, Smith MA, et al. Childhood behavior problems and age at first sexual intercourse: a prospective birth cohort study. Pediatrics. 2015;135(2):255-263. [DOI] [PubMed] [Google Scholar]
- 146.Monteiro IP, Azzi CFG, Bilibio JP, Monteiro PS, Braga GC, Nitz N. Prevalence of sexually transmissible infections in adolescents treated in a family planning outpatient clinic for adolescents in the western Amazon. PLoS One. 2023;18(6):e0287633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ayerdi Aguirrebengoa O, Vera Garcia M, Rueda Sanchez M, et al. Risk factors associated with sexually transmitted infections and HIV among adolescents in a reference clinic in Madrid. PLoS One. 2020;15(3):e0228998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bonar EE, Walton MA, Caldwell MT, Whiteside LK, Barry KL, Cunningham RM. Sexually transmitted infection history among adolescents presenting to the Emergency Department. J Emerg Med. 2015;49(5):613-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Berenson AB, Wiemann CM, McCombs S. Exposure to violence and associated health-risk behaviors among adolescent girls. Arch Pediatr Adolesc Med. 2001;155(11):1238-1242. [DOI] [PubMed] [Google Scholar]
- 150.Voisin DR, Hotton A, Neilands T. Exposure to community violence and sexual behaviors among African American youth: testing multiple pathways. Behav Med. 2018;44(1):19-27. [DOI] [PubMed] [Google Scholar]
- 151.Hill DC, Stein LAR, Rossi JS, Magill M, Clarke JG. Intimate violence as it relates to risky sexual behavior among at-risk females. Psychol Trauma. 2018;10(6):619-627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Obiyan MO, Olaleye AO, Oyinlola FF, Folayan MO. Factors associated with pregnancy and induced abortion among street-involved female adolescents in two Nigerian urban cities: a mixed-method study. BMC Health Serv Res. 2023;23(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lameiras-Fernández M, Martínez-Román R, Carrera-Fernández MV, Rodríguez-Castro Y. Sex education in the spotlight: what is working? systematic review. Int J Environ Res Publ Health. 2021;18(5):2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Betit AL, Kennedy C. The need for earlier implementation of comprehensive sexual education within a formal classroom setting and beyond based on the influences of technology. Cureus. 2022;14(8):e28552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Aventin Á, Gough A, McShane T, et al. Engaging parents in digital sexual and reproductive health education: evidence from the JACK trial. Reprod Health. 2020;17(1):132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Nghipondoka-Lukolo LN, Charles KL. Parents' participation in the sexuality education of their children in Namibia: a framework and an educational programme for enhanced action. Global J Health Sci. 2015;8(4):172-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hisler GC, Hasler BP, Franzen PL, Clark DB, Twenge JM. Screen media use and sleep disturbance symptom severity in children. Sleep Health. 2020;6(6):731-742. [DOI] [PubMed] [Google Scholar]
- 158.Fadzil A. Factors affecting the quality of sleep in children. Children. 2021;8(2):122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mindell JA, Telofski LS, Wiegand B, Kurtz ES. A nightly bedtime routine: impact on sleep in young children and maternal mood. Sleep. 2009;32(5):599-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Mindell JA, Li AM, Sadeh A, Kwon R, Goh DY. Bedtime routines for young children: a dose-dependent association with sleep outcomes. Sleep. 2015;38(5):717-722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lewien C, Genuneit J, Meigen C, Kiess W, Poulain T. Sleep-related difficulties in healthy children and adolescents. BMC Pediatr. 2021;21(1):82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kolip P, Kuhnert R, Saß AC. Social, health-related, and environmental factors influencing sleep problems of children, adolescents and young adults. J Health Monit. 2022;7(Suppl 2):2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Xiong X, Cui Y, Zhang W, et al. Association between sleep duration and physical fitness in children aged 3-6 years: a cross-sectional study from China. Int J Environ Res Publ Health. 2022;19(11):6902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Fonseca APLM, de Azevedo CVM, Santos RMR. Sleep and health-related physical fitness in children and adolescents: a systematic review. Sleep Sci. 2021;14(4):357-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Astill RG, Van der Heijden KB, Van Ijzendoorn MH, Van Someren EJ. Sleep, cognition, and behavioral problems in school-age children: a century of research meta-analyzed. Psychol Bull. 2012;138(6):1109-1138. [DOI] [PubMed] [Google Scholar]
- 166.Deng X, He M, He D, Zhu Y, Zhang Z, Niu W. Sleep duration and obesity in children and adolescents: evidence from an updated and dose-response meta-analysis. Sleep Med. 2021;78:169-181. [DOI] [PubMed] [Google Scholar]
- 167.Ruan H, Xun P, Cai W, He K, Tang Q. Habitual sleep duration and risk of childhood obesity: systematic review and dose-response meta-analysis of prospective cohort studies. Sci Rep. 2015;5:16160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kitsaras G, Goodwin M, Allan J, Kelly MP, Pretty IA. Bedtime routines child wellbeing & development. BMC Publ Health. 2018;18(1):386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Meltzer LJ, Williamson AA, Mindell JA. Pediatric sleep health: it matters, and so does how we define it. Sleep Med Rev. 2021;57:101425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Galland BC, Mitchell EA. Helping children sleep. Arch Dis Child. 2010;95(10):850-853. [DOI] [PubMed] [Google Scholar]
- 171.Cummings C, Canadian Paediatric Society, Community Paediatrics Committee . Melatonin for the management of sleep disorders in children and adolescents. Paediatr Child Health. 2012;17(6):331-336. [PMC free article] [PubMed] [Google Scholar]
- 172.Felt BT, Chervin RD. Medications for sleep disturbances in children. Neurol Clin Pract. 2014;4(1):82-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Lifestyle Behaviors of Childhood and Adolescence: Contributing Factors, Health Consequences, and Potential Interventions by Ahmed Arafa, Yuka Yasui, Yoshihiro Kokubo, Yuka Kato, Chisa Matsumoto, Masayuki Teramoto, Saya Nosaka, and Miho Kogirima in American Journal of Lifestyle Medicine