Abstract
Introduction
The main goal of this scoping review is to highlight the clinical features of subjects with rotator cuff calcific tendinopathy (RCCT), in order to identify and map this condition clinical criteria, and thus to be able to hypothesize such pathology before imaging investigations.
Methods
Four databases were consulted up to January 2023. The obtained results were reported following the PRISMA-ScR and the Joanna Briggs Institute reviewer's manual was used as guideline for conducting the review. No time and geographical restrictions were applied.
Results
A total of 851 records have been identified, with 50 studies meeting the inclusion criteria. Subjects with RCCT mostly reported nightly, acute and severe pain with spontaneous onset. Symptoms were mostly unilateral. Subjects were mostly women aged between 30 and 60. Deficit in active and passive range of motion was reported, mainly during abduction and forward flexion. Endocrine and metabolic disorders were described as comorbidity, in particular diabetes and thyroid disorders.
Conclusion
In this scoping review, the most relevant RCCT clinical features were detected. These clinical criteria, predictive for shoulder RCCT, can be crucial to help all clinicians suspect this musculoskeletal disease early and with certainty, thus allowing for an appropriate and prompt diagnosis path.
Level of evidence
III.
Keywords: calcific tendinopathy, clinical features, scoping review, shoulder
Highlights
Subjects with rotator cuff calcific tendinopathy often reported nightly, acute, unilateral and severe pain with spontaneous onset
Subjects complaining rotator cuff calcific tendinopathy were often female aged between 30 and 60
Subjects often reported deficit in active and passive range of motion, mainly in abduction and flexion
Endocrine and metabolic disorders were often described as ccomorbidity
Background
Rotator cuff calcific tendinopathy (RCCT) is a clinical condition characterized by the presence of calcific deposits in the rotator cuff tendons, 1 which led to shoulder pain and functional limitations.2,3 The calcium deposits are most commonly located at the level of the supraspinatus tendon1,2,4–8 and in about 10% of individuals the deposits are found bilaterally.1,4,5,7 Notably, in 20% of cases, the subjects are asymptomatic.1,7,8
According to the literature, RCCT etiology remains unclear; probably, endocrine disorders play an important role in its development, but the effect of this process is still unknown.3,9 As far as its pathogenesis is concerned, various theories have been described in the literature; the most accredited one is the reactive calcification theory proposed by Uthoff in 1997, 10 which consists in a three-stages process: pre-calcific, calcific, and post-calcific stage. During the pre-calcific stage, tenocytes undergo a metaplastic transformation into chondrocytes1,4,10 within the site where the calcium deposits will subsequently form. The calcific stage is further divided into three different phases: the formative phase, in which calcium deposits increase in size,4,10 the resting phase, characterized by the presence of calcium deposits in the rotator cuff, 8 and finally, the resorptive phase, during which the calcium deposits are gradually eliminated through macrophages phagocytosis.8,10 During the last post-calcific phase, the tendon seems to undergo a remodeling process and it gradually returns to its prior physiological conditions.4,10 This theory emphasizes the fact that calcium deposits are characterized by spontaneous formation and remission and therefore RCCT should not be considered a degenerative process. 1
As for RCCT diagnosis, the majority of the studies focused on imaging screening investigations,1,4,5,11 rather than on the subjects’ clinical presentation. X-ray, ultrasonography1,4,5,11 and, optionally, computed tomography6,12 and magnetic resonance imaging being described as the main diagnostic tools used to identify where calcium deposits are located and to inspect their morphology, dimension and evolution.7,12,13
To date there is a lack of knowledge of relevant clinical criteria for hypothesizing RCCT in subjects with painful shoulder, therefore a scoping review would seem to be the most appropriate study for investigating these aspects.
The aim of this scoping review is to highlight the clinical features of RCCT in subjects affected by shoulder pain, in order to identify, map and summarize useful and relevant clinical criteria, which could led clinicians to an early RCCT diagnostic hypothesis, before imaging testing.
Review question
The review question is the following: what clinically relevant features are useful to hypothesize the clinical entity of RCCT.
Materials and methods
In this scoping review, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR checklist) 14 was used for reporting and the Joanna Briggs Institute reviewer's manual was used as guideline for conducting the review. 15
Inclusion and exclusion criteria
As far as the eligibility of the studies to be included in the study is concerned, the population, concept and context (PCC) criteria appeared to be the most appropriate. 16 Therefore, in order to be included, articles had to meet the following criteria:
Population: Symptomatic subjects diagnosed with RCCT
Concepts: Any study reporting the RCCT clinical presentation
Context: Any context.
In this scoping review, no restrictions regarding study design, publication type and time and geographical restriction have been applied. Therefore, studies which do not meet all the inclusion criteria included in PCC were excluded.
Search strategies
The search process to identify the studies to be included in this scoping review began on 28 July 2022, and the following databases were searched: PubMed, PEDro, and Cochrane Library. The articles obtained were subsequently screened for title and abstract, after the duplicates removal (28 records). Google Scholar has been consulted in order to identify any additional study and eventual grey literature. The full search strategy for PubMed and Google Scholar are available in Appendix 1. In January 2023, the search strategy was updated in order to include all articles published in 2022 as well.
Studies selection
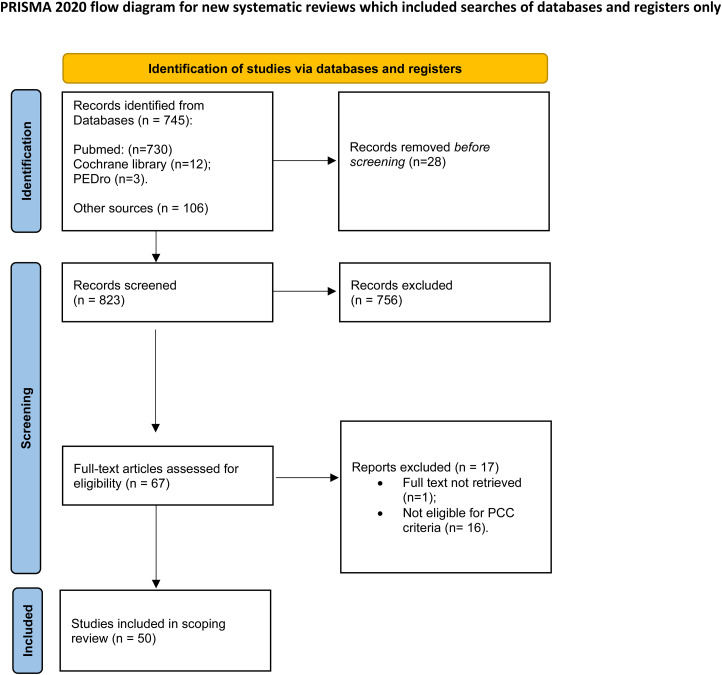
The studies analysis was conducted by two independent authors (FG, ADS), who are physiotherapists specialized in shoulder musculoskeletal disorders. The studies selection was conducted using the Rayyan QCRI web application 17 ; during this process both (a) a title and abstract and (b) a full-text screening was performed. A third independent author (DV) contributed to solve any disagreement. The PRISMA-ScR flow-chart shows the studies selection process (Figure 1); a detailed list of excluded studies, with their reason for exclusion, is provided in Appendix 2.
Figure 1.
PRISMA 2020 flow diagram.
Data charting process
For data extraction we used a standard Excel file which follows the PCC. Two authors (FG and DV) filled the Excel, with mutual check. Disagreements were solved by a third author (FB). In this file, the following items have been included: title of the study, first author, year of publication, study type, and clinical presentation. In the “Clinical presentation” section, the subjects’ most relevant features were reported—such as age, sex, pain characteristics, functional limitation, and possible comorbidities.
Data synthesis
As a scoping review, it was not necessary to perform a quality assessment of the included studies. 18 The results have been presented quantitatively and thematically:
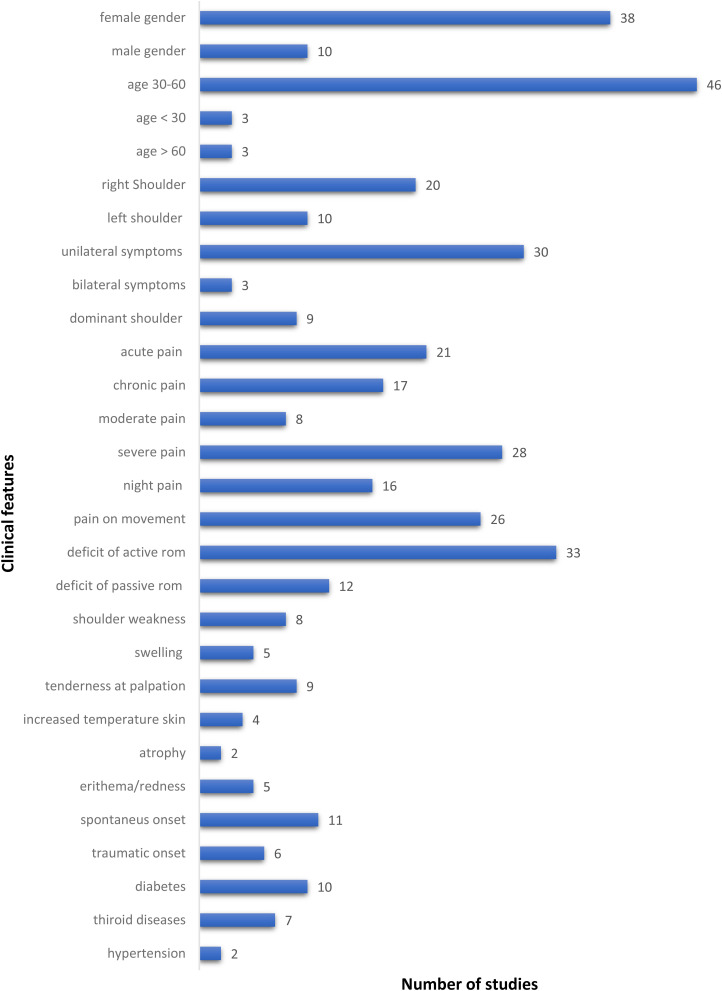
The quantitative results have been represented through a histogram (Figure 2), showing all the clinical features found in the analyzed studies. This quantitative representation provides a mapping of the clinical criteria that were found in subjects affected by RCCT: age, sex, pain characteristics (acute, chronic, onset type, intensity), functional limitation, signs (tenderness, erythema, increased temperature skin, etc.), comorbidities, lifestyle, and occupation type (manual workers, sedentary jobs, etc.) with the number of studies reporting such features.
Thematic analysis was performed to discuss and summarize the existing literature on the clinical characteristics of RCCT subjects, based on the quantitative results reported in this scoping review.
Figure 2.
Clinical findings of rotator cuff calcific tendinopathy.
Results
Characteristics of the included studies
The search on the aforementioned databases was conducted at the end of January 2023 and led to the collection of 851 articles. Firstly, all duplicates were removed (n = 28). Subsequently, the selection by title and abstract of each of the 823 remaining studies was conducted, leading to 756 articles being deleted at the end of this analysis. An article was not retrieved for full text evaluation. The full text analysis was conducted on the 66 remaining articles and 16 articles were excluded (the reasons for exclusion are detailed in Appendix 2). Therefore, at the end of the study selection, 50 articles were finally included (Figure 1). The report of included studies can be found in Appendix 3.
The 50 included studies were: case reports (n = 14),19–32 narrative reviews (n = 11),1–3,6–8,33–37 randomized clinical trials (n = 4),38–41 clinical trials (n = 4),42–45 retrospective studies (n = 5),9,46–49 case series (n = 3),50–52 prospective studies (n = 2),53,54 concise reviews (n = 2),4,55 cross sectional study (n = 1), 56 comparative study (n = 1), 57 prognostic study (n = 1), 58 diagnostic clinical study (n = 1), 59 clinical commentary (n = 1). 60 Three articles were declared as case reports; however, Gimblett et al. 50 reported two clinical cases in his study, Takahashi et al. 51 described four clinical cases in his article, and Lehmer et al. 52 reported three RCCT case reports. Indeed, 14 case reports and 3 case series were included, together with 23 RCCT single reports.
Most of the included studies were conducted after 2010 (32/50), 10 studies were conducted between 2000 and 2010 and 8 before 2000. Moreover, 24 of the included studies were European, while the others came from USA (13/50), Japan (3/50), Republic of China (2/50) Australia (1/50), Canada (2/50), Nepal (1/50), Egypt (1/50), Korea (1/50), Pakistan (1/50), and only in one study (1/50) the (geographical) origin of the data was not specified.
Clinical findings
As previously pointed out, the study included 50 articles and each article was fully reviewed in order to bring out all relevant clinic data. A mapping of the data is provided by the histogram in Figure 2.
In the majority of the articles included, female subjects were the most affected (>75%)1,2,4,6–9,19,21,23,25,28–30,32,33,36–39,42–56,58,59 and the subjects’ age was reported between 30 and 60 years of age (>85%).1–4,6–9,19–22,27–30,33,34,36–40,42–56,58,59 Only in six studies, the individuals’ age fell outside this range, with two children,23,24 three subjects who were over sixty28,30,32 and one 29-year-old individual. 31
In 30 studies, the reported symptoms were unilateral (20 right shoulders)7,19–22,24,26,31,32,39,44,46,49–53,56 and 10 left shoulders,23,25,27–30,44,49,50,52 and in three studies the symptoms were present bilaterally.34,36,44 Nine of them specified that the subjects’ dominant shoulder was affected.8,20,22,26,31,42,46,47
Pain was mostly defined as acute, recent, severe,2,4,6,8,19,23,24,26,28,29,31,33,35–37,42,43,49,51–53,55 with a spontaneous and sudden onset20–23,27–32,50,51 and which occurred during the night.1,2,4,20,22,26,31,32,35,42,44,48,51 However, in some articles, the subjects’ pain was described as chronic4,22,30,32,33,36,39–44,46,48,50,51,55 and moderate1,36,38,43,51.
Another RCCT important clinical sign seems to be linked to the subject's limited range of motion (ROM). Indeed, in thirty-three studies1,2,4,6–8,19–21,23–36,38,40,48–51,55 an active ROM deficit was reported, and in twelve studies2,19,20,24,26,28,30,36,40,44,50,51 a passive ROM deficit was reported; this suggested that RCCT may indeed frequently cause a functional movement restriction in affected subjects. Specifically, the restricted glenohumeral movements were reported in case of: forward flexion (17 studies),4,19,20,23,26,27,29,31,48,50,51 abduction (15 studies),8,19,20,23,26,29–31,33,50,51 internal rotation (11 studies),19,20,27,28,33,50,51 external rotation (8 studies),19,20,27–29,33,51 adduction (5 studies)19,51 and extension (5 studies).19,31,51
Others clinical features reported by subjects affected by RCCT were tenderness upon palpation of greater tuberosity,2,6,29,50 deltoid,24,50 bicipital groove, 50 acromial process area 20 and coracoid process. 32 Moreover, local erythema or redness,2,4,23,34,37 swelling;21,23,32,37,60 muscle atrophy20,33; increased skin temperature4,20,34,51 were reported. Shoulder weakness was reported in 4 studies,20,22,33,48 specifically, strength deficit during abduction (3 studies),20,22,33 external rotation (3 studies)20,22,33 and internal rotation (2 studies)20,33 were described; pain upon movement was reported in 14 studies2,20,22–24,26,29,30,33,37,44,48,50,51 and in particular glenohumeral movements contributed to exacerbate the subject's pain: abduction (7 studies),23,29,30,33,37,50 forward flexion (6 studies),2,20,23,29,48,50 internal rotation (3 studies),29,33,50 overhead activity (3 studies),22,26,37 external rotation (2 studies)29,33 and extension (1 study). 20 Furthermore, two studies24,51 reported that all shoulder movements worsened the subject's pain, in one study 22 running was also described as a painful activity for the RCCT subject.
As far as comorbidities are concerned, endocrine and metabolic disorders have been reported. In particular, ten studies reported diabetes2–4,9,29,33,36,37,46,49 and seven studies reported thyroid disorders.2,3,9,33,36,37,49 Hypertension was also reported as comorbidity in subjects with RCCT in two studies.3,29
Discussion
In the present study, the main RCCT clinical findings were the following: predominantly female-related condition, subjects aged between thirty and sixty, sudden onset of severe pain, night pain, active and passive ROM deficit, pain upon movement and presence of metabolic or endocrine comorbidities.
The aim of this scoping review is to highlight the RCCT clinical features reported in literature, in order to profile the clinical diagnostic criteria of this musculoskeletal condition. The scoping review study typology was chosen since no other reviews have been conducted on this topic. In fact, most of the RCCT diagnostic studies which can be found in the literature were based on imaging1,4,5,11 and little consideration was given to RCCT clinical features or to functional impairments. Detecting RCCT clinical features would be crucial and beneficial for both the scientific literature and the subjects, since it would imply that clinicians could hypothesize RCCT cases earlier; consequently, they could offer their subjects a targeted therapeutic treatment immediately, in order to intervene promptly; moreover, this would help cutting costs for the subjects, who would resort less to imaging investigations and would perform only those strictly necessary for their own clinical condition.
The present study showed that the most common RCCT symptom is unilateral pain, mostly acute, severe and occurring at night, which has a sudden onset and strongly impairs the subject's movements.2,20,22–24,26,29,30,33,37,44,48,50,51 It is likely that subjects with a sudden onset of these severe clinical features are in their resorptive RCCT stage2,3,10,37 – which is generally described as the most painful and disabling stage1,4,7,10,33,37 – whereas subjects who are experiencing a chronic moderate pain are more likely to be in their RCCT formative stage.2,10,33,37
Our review revealed an active and passive ROM deficit; in particular, forward flexion and abduction were the most restricted movements. This can be due to calcium deposits occurring more often in the supraspinatus tendon insertion, near the greater tuberosity.2,4 Indeed, Kim et al. 4 reported that 63% of calcification occurs in the supraspinatus tendon, 20% in both supraspinatus and subscapularis tendons, 7% in both the infraspinatus tendons and subacromial bursa and 3% in the subscapularis tendon. Notably, all of these muscles play a predominant role in the active abduction of the shoulder61–64 and during the elevation on the scapular and sagittal plane. 65 Furthermore, the distance between the acromion and the humeral greater tuberosity during abduction and flexion on the scapular plane is minimal between 36 and 72 degrees of movement 66 ; therefore, the presence of calcium deposits at the supraspinatus insertion site could furtherly contribute to narrowing this space, resulting in pain upon movement, since the supraspinatus tendon and the calcified mass end up caught between the acromion and humeral head. 37
However, RCCT shows some clinical features that could be found in other shoulder pathologies as well and the present study could not rigorously delineate and isolate the clinical diagnostic criteria for symptomatic RCCT. For example, passive and active ROM deficit on different planes of movement, associated with night pain, is typically found in subjects with frozen shoulder, 67 therefore they cannot be considered discriminating RCCT criteria.
However, the sudden onset of severe pain found in RCCT subjects deserves to be assessed more in-depth. Generally, subjects affected by frozen shoulder or rotator cuff tendinopathies report a gradual onset of their symptoms, which tend to worsen over time. 68 Furthermore, in most cases, acute shoulder pain due to a rotator cuff tear is associated with a traumatic event 69 and their onset is generally spontaneous and sudden. In this review, the majority of the included studies reported pain characterized by a sudden onset, which could compromise all active and passive shoulder movements. For example, Takahashi et al. 51 described two case reports in which symptoms began at midnight and, subsequently, all active and passive shoulder movements were impossible due to the subject's pain; Spivey et al. 29 described the case of a 37-year-old woman, who reported pain lasting for 5 days, without notion of trauma; in this case, both internal and external rotation were impossible due to the pain. Fong et al. 24 described a case report of a 7-year-old boy with acute RCCT mimicking humeral great tuberosity fracture for the intensity of his pain and the severity of his functional impairment. These studies highlight both RCCT symptoms severity and its rapid flair up, which would indeed represent RCCT clinical peculiarities. Therefore, clinicians should consider these features during their first subject's assessment, in case of acute and severe shoulder pain, especially when subjects report a sudden onset of their symptoms, associated to other signs, such as tenderness upon shoulder palpation,2,6,20,24,29,32,34,50 swelling21,23,32,37,60 and erythema2.,4,23,34,37
Another important aspect which clinicians should take into consideration is the presence of endocrine conditions in the subjects’ medical history. Indeed, Robinson et al. 2 reported that the typical RCCT subject profile is that of a female subject, aged between forty and sixty; moreover, RCCT suspicion should increase in case of factors such as diabetes or thyroid diseases.2,3 Harvie et al. 9 showed a high prevalence of endocrine and metabolic diseases in their cohort and described a female predisposition for RCCT, with a peak prevalence during the fifth decade. Moreover, Bechay et al. 33 reported that hormonal disorders, such as diabetes and hypothyroidism, and metabolic disorders have to be considered as risk factors for RCCT. Greis et al. 3 reported ischemic heart disease, hypertension, diabetes and thyroid conditions as clinical findings potentially linked to the development of RCCT. Considering all the data discussed above, it is indeed very likely that endocrine and hormonal disorders could actually play a key role in calcium deposits formation in RCCT subjects, however, this mechanism is not yet fully understood.3,9
Implications for clinical practice
This scoping review was conducted in order to highlight the main clinical characteristics of subjects affected by RCCT, since beforehand the only diagnostic criteria were mainly based on imaging investigations.
Therefore, in order to be able to suspect (and subsequently detect) RCCT during an early stage of their clinical evaluation, clinicians must remember that subjects affected by RCCT frequently report a sudden onset of their symptoms, which are characterized by severe and disabling pain; in case of RCCT, the subjects’ symptomatology may led to the restriction of all their glenohumeral movements; furthermore, it should be remembered that RCCT predominantly affects women aged between thirty and sixty.
Lastly, it would be important to ask the subject if they have ever suffered from endocrine or metabolic disorders, as these could represent further risk factors of RCCT.2,3,33
Early suspicion of RCCT could be beneficial for the affected subject that should be referred for a prompt and definitive diagnosis by imaging, cutting costs for health services and saving from ineffective pharmacotherapy and/or physiotherapy.
Implications for research
This scoping review has provided a summary of RCCT clinical findings, since no other review has been ever conducted on this topic. Indeed, no systematic reviews about this specific area has emerged during our study selection, and this implies that the literature would certainly profit from more in-depth studies regarding RCCT clinical criteria.
Strengths and limitations
This scoping review followed the PRISMA-ScR checklist for the correct reporting of the study. The methods have been reported and the search strategy has been specified in Appendix 1. No time, language and geographical areas restrictions have been applied.
However, as a scoping review, no methodological quality assessment of the included studies was performed. Moreover, our search strings, even if as comprehensive as possible, could still have missed some paper of interest. Nevertheless, being a scoping review, the present study carries its methodological limitations and, therefore, it aims to provide useful information in order to allow for the development of subsequent better-quality research.
Conclusion
The most relevant RCCT clinical findings detected in this scoping review were predominantly female-related condition, subjects aged between 30 and 60, sudden onset of severe pain, night pain, active and passive ROM deficit, specifically during forward flexion and abduction, pain upon movement, and presence of metabolic or endocrine comorbidities. These clinical criteria, predictive for shoulder RCCT, can be crucial to help all clinicians to confidently suspect this musculoskeletal disease early, thus allowing for an appropriate and prompt diagnosis path. In this way, clinicians could refer the subjects to perform the most appropriate imaging examination for RCCT (x-ray) and, subsequently, start the proper therapeutic treatment.
Supplemental Material
Supplemental material, sj-docx-1-sel-10.1177_17585732241244515 for Clinical features in rotator cuff calcific tendinopathy: A scoping review by Federico Guido, Davide Venturin, Andrea De Santis, Giuseppe Giovannico and Fabrizio Brindisino in Shoulder & Elbow
Supplemental material, sj-docx-2-sel-10.1177_17585732241244515 for Clinical features in rotator cuff calcific tendinopathy: A scoping review by Federico Guido, Davide Venturin, Andrea De Santis, Giuseppe Giovannico and Fabrizio Brindisino in Shoulder & Elbow
Supplemental material, sj-docx-3-sel-10.1177_17585732241244515 for Clinical features in rotator cuff calcific tendinopathy: A scoping review by Federico Guido, Davide Venturin, Andrea De Santis, Giuseppe Giovannico and Fabrizio Brindisino in Shoulder & Elbow
Abbreviations
- RCCT
rotator cuff calcific tendinopathy
- PCC
population, concept, and context
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews
Footnotes
Contributorship: Concept/Idea: DV and FB. Research Design: DV, FB, and FG. Writing: FG, DV, and FB. Data Collection: FG and ADS. Data Analysis: FG, ADS, and GG. Project Management: FB and DV. Consultation (including review of manuscript before submitting): FG, DV, ADS, GG, and FB. Final approval of the Manuscript: FG, DV, ADS, GG, and FB.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Guarantor: Fabrizio Brindisino.
ORCID iD: Fabrizio Brindisino https://orcid.org/0000-0001-8950-8203
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Chianca V, Albano D, Messina C, et al. Rotator cuff calcific tendinopathy from diagnosis to treatment. Acta Biomed 2018; 89: 186–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robinson DM, Schowalter S, McInnis KC. Update on evaluation and management of calcific tendinopathy. Curr Med Phys Rehabil Rep 2021; 9: 57–69. [Google Scholar]
- 3.Greis AC, Derrington SM, McAuliffe M. Evaluation and nonsurgical management of rotator cuff calcific tendinopathy. Orthop Clin North Am 2015; 46: 293–302. [DOI] [PubMed] [Google Scholar]
- 4.Kim M-S, Kim I-W, Lee Set al. et al. Diagnosis and treatment of calcific tendinitis of the shoulder. Clin Shoulder Elb 2020; 23: 210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sansone V, Maiorano E, Galluzzo Aet al. et al. Calcific tendinopathy of the shoulder: clinical perspectives into the mechanisms, pathogenesis, and treatment. Orthop Res Rev 2018; 10: 63–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ElShewy MT. Calcific tendinitis of the rotator cuff. World J Orthop 2016; 7: 55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merolla G, Singh S, Paladini Pet al. et al. Calcific tendinitis of the rotator cuff: state of the art in diagnosis and treatment. J Orthop Traumatol 2016; 17: 7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bureau N. Calcific tendinopathy of the shoulder. Semin Musculoskelet Radiol 2013; 17: 80–84. [DOI] [PubMed] [Google Scholar]
- 9.Harvie P, Pollard TCB, Carr AJ. Calcific tendinitis: natural history and association with endocrine disorders. J Shoulder Elbow Surg 2007; 16: 169–173. [DOI] [PubMed] [Google Scholar]
- 10.Uthoff HK, Loehr JW. Calcific tendinopathy of the rotator cuff: pathogenesis, diagnosis and management. J Am Acad Orthop Surg 1997; 5: 183–191. [DOI] [PubMed] [Google Scholar]
- 11.Ogon P, Suedkamp NP, Jaeger M, et al. Prognostic factors in nonoperative therapy for chronic symptomatic calcific tendinitis of the shoulder. Arthritis Rheum 2009; 60: 2978–2984. [DOI] [PubMed] [Google Scholar]
- 12.Draghi F, Cocco G, Lomoro P, et al. Non-rotator cuff calcific tendinopathy: ultrasonographic diagnosis and treatment. J Ultrasound 2020; 23: 301–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loew M, Sabo D, Wehrle Met al. et al. Relationship between calcifying tendinitis and subacromial impingement: a prospective radiography and magnetic resonance imaging study. J Shoulder Elbow Surg 1996; 5: 314–319. [DOI] [PubMed] [Google Scholar]
- 14.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169: 467–473. [DOI] [PubMed] [Google Scholar]
- 15.Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z, editors. JBI manual for evidence synthesis. JBI. 2024. https://synthesismanual.jbi.global.
- 16.Peters MDJ, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015; 13: 141–146. [DOI] [PubMed] [Google Scholar]
- 17.Ouzzani M, Hammady H, Fedorowicz Zet al. et al. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016; 5: 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018; 18: 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Polastri M, Cantagalli S. Massive calcific shoulder tendinitis. Am J Phys Med Rehabil 2020; 99: e126–e127. [DOI] [PubMed] [Google Scholar]
- 20.Wainner MAJRS, Hasz M. Management of acute calcific tendinitis of the shoulder. J Orthop Sports Phys Ther 1998; 27: 231–237. [DOI] [PubMed] [Google Scholar]
- 21.Prato N, Banderali A, Neumaier CE, et al. Calcific tendinitis of the rotator cuff as a cause of drooping shoulder. Skeletal Radiol 2003; 32: 82–85. [DOI] [PubMed] [Google Scholar]
- 22.Chan R, Kim DH, Millett PJet al. et al. Calcifying tendinitis of the rotator cuff with cortical bone erosion. Skeletal Radiol 2004; 33: 596–599. [DOI] [PubMed] [Google Scholar]
- 23.Bittmann S. Calcific tendinitis of the supraspinatus tendon in children. Klin Padiatr 2006; 218: 45–46. [DOI] [PubMed] [Google Scholar]
- 24.Fong CM. Calcific tendinitis of the supraspinatus tendon in a 7-year-old boy: diagnostic challenges. Hong Kong Med J 2011; 17: 414–416. [PubMed] [Google Scholar]
- 25.Slavin JD, Levine GM, Spencer RP. Calcification in the supraspinatus tendon detected on bone scan. Clin Nucl Med 1989; 14: 921–922. [DOI] [PubMed] [Google Scholar]
- 26.Berg E. Calcific tendinitis of the shoulder. Orthop Nurs 1997; 16: 68–69. [PubMed] [Google Scholar]
- 27.Gotoh M, Higuchi F, Suzuki Ret al. et al. Progression from calcifying tendinitis to rotator cuff tear. Skeletal Radiol 2003; 32: 86–89. [DOI] [PubMed] [Google Scholar]
- 28.Lecoq B, Levasseur R, Fournier L, et al. Atypical pattern of acute severe shoulder pain: contribution of sonography. Joint Bone Spine 2004; 71: 592–594. [DOI] [PubMed] [Google Scholar]
- 29.Spivey JL, Carrell TM. Severe pain in the shoulder with no history of trauma. JAAPA 2009; 22: 59–60. [DOI] [PubMed] [Google Scholar]
- 30.Hutchinson JL, Gusberti D, Saab G. Changing appearance of intraosseous calcific tendinitis in the shoulder with time: a case report. Radiol Case Rep 2019; 14: 1267–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Skyler W, Jeffrey L. A closer look at a case of calcific tendonitis of the shoulder. Curr Sports Med Rep 2022; 21: 318–321. [DOI] [PubMed] [Google Scholar]
- 32.Layfer LF. Painful anterior shoulder mass with calcification. IMJ III Med J 1978; 154: 22–23. [PubMed] [Google Scholar]
- 33.Bechay J, Lawrence C, Namdari S. Calcific tendinopathy of the rotator cuff: a review of operative versus nonoperative management. Phys Sportsmed 2020; 48: 241–246. [DOI] [PubMed] [Google Scholar]
- 34.Garcia GM, McCord GC, Kumar R. Hydroxyapatite crystal deposition disease. Semin Musculoskelet Radiol 2003; 7: 187–193. [DOI] [PubMed] [Google Scholar]
- 35.Ricci V, Mezian K, Chang K-Vet al. et al. Clinical/sonographic assessment and management of calcific tendinopathy of the shoulder: a narrative review. Diagnostics (Basel) 2022; 12: 3097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beckmann NM. Calcium apatite deposition disease: diagnosis and treatment. Radiol Res Pract 2016; 2016: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Catapano M, Robinson DM, Schowalter Set al. et al. Clinical evaluation and management of calcific tendinopathy: an evidence-based review. J Osteopath Med 2022; 122: 141–151. [DOI] [PubMed] [Google Scholar]
- 38.Pieber K, Grim-Stieger M, Kainberger F, et al. Long-term course of shoulders after ultrasound therapy for calcific tendinitis: results of the 10-year follow-up of a randomized controlled trial. Am J Phys Med Rehabil 2018; 97: 651–658. [DOI] [PubMed] [Google Scholar]
- 39.Rompe JD, Zoellner J, Nafe B. Shock wave therapy versus conventional surgery in the treatment of calcifying tendinitis of the shoulder. Clin Orthop Relat Res 2001; 387: 72–82. [DOI] [PubMed] [Google Scholar]
- 40.Fatima A, Ahmad A, Gilani SA, et al. Effects of high-energy extracorporeal shockwave therapy on pain, functional disability, quality of life, and ultrasonographic changes in patients with calcified rotator cuff tendinopathy. Biomed Res Int 2022; 2022: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Verstraelen F, Verhagen S, Giesberts A, et al. Needle aspiration of calcific deposits versus shock wave therapy for conservative therapy resistant calcifying tendinitis of the shoulder: protocol of a randomized, controlled trial. BMC Musculoskelet Disord 2022; 23: 308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Le Goff B, Berthelot J-M, Guillot P, et al. Assessment of calcific tendonitis of rotator cuff by ultrasonography: comparison between symptomatic and asymptomatic shoulders. Joint Bone Spine 2010; 77: 258–263. [DOI] [PubMed] [Google Scholar]
- 43.Chiou H-J, Hung S-C, Lin S-Y, et al. Correlations among mineral components, progressive calcification process and clinical symptoms of calcific tendonitis. Rheumatology (Oxford) 2010; 49: 548–555. [DOI] [PubMed] [Google Scholar]
- 44.Pfister J, Gerber H. Chronic calcifying tendinitis of the shoulder-therapy by percutaneous needle aspiration and lavage prospective open study of 62 shoulders. Clin Rheumatol 1997; 16: 269–274. [DOI] [PubMed] [Google Scholar]
- 45.Fusaro I, Orsini S, Diani S, et al. Functional results in calcific tendinitis of the shoulder treated with rehabilitation after ultrasonic- guided approach. Musculoskelet Surg 2011; 95: 31–36. [DOI] [PubMed] [Google Scholar]
- 46.Louwerens JKG, Sierevelt IN, van Hove RP, et al. Prevalence of calcific deposits within the rotator cuff tendons in adults with and without subacromial pain syndrome: clinical and radiologic analysis of 1219 patients. J Shoulder Elbow Surg 2015; 24: 1588–1593. [DOI] [PubMed] [Google Scholar]
- 47.Compagnoni R, Menon A, Radaelli S, et al. Long-term evolution of calcific tendinitis of the rotator cuff: clinical and radiological evaluation 10 years after diagnosis. J Orthop Traumatol 2021; 22: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oudelaar BW, Schepers-Bok R, Ooms EM, et al. Needle aspiration of calcific deposits (NACD) for calcific tendinitis is safe and effective: six months follow-up of clinical results and complications in a series of 431 patients. Eur J Radiol 2016; 85: 689–694. [DOI] [PubMed] [Google Scholar]
- 49.Furuhata R, Matsumura N, Yoshiyama A, et al. Seasonal variation in the onset of acute calcific tendinitis of rotator cuff. BMC Musculoskelet Disord 2020; 21: 741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gimblett PA, Saville J, Ebrall P. A conservative management protocol for calcific tendinitis of the shoulder. J Manipulative Physiol Ther 1999; 22: 622–627. [DOI] [PubMed] [Google Scholar]
- 51.Takahashi M, Ogawa K. Calcific tendinitis of the rotator cuff showing a contracted state of abduction: a report of four cases. J Shoulder Elbow Surg 1997; 6: 72–76. [DOI] [PubMed] [Google Scholar]
- 52.Lehmer LM, Ragsdale BD. Calcific periarthritis: more than a shoulder problem. A series of fifteen cases. J Bone Joint Surg Am 2012; 94: e157. [DOI] [PubMed] [Google Scholar]
- 53.Sanjel Chhetri R, Khatri KP, Khanal Jet al. et al. Outcome of needle fenestration, subacromial steroid and diclofenac phonophoresis in acute calcific tendinitis of shoulder. J Nepal Med Assoc 2017; 56: 357–361. [PubMed] [Google Scholar]
- 54.Vassalou EE, Klontzas ME, Plagou APet al. et al. Ultrasound-guided percutaneous irrigation of calcific tendinopathy: redefining predictors of treatment outcome. Eur Radiol 2021; 31: 2634–2643. [DOI] [PubMed] [Google Scholar]
- 55.Merolla G, Bhat MG, Paladini Pet al. et al. Complications of calcific tendinitis of the shoulder: a concise review. J Orthop Traumatol 2015; 16: 175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sansone V, Consonni O, Maiorano E, et al. Calcific tendinopathy of the rotator cuff: the correlation between pain and imaging features in symptomatic and asymptomatic female shoulders. Skeletal Radiol 2016; 45: 49–55. [DOI] [PubMed] [Google Scholar]
- 57.Maier M, Stäbler A, Schmitz C, et al. On the impact of calcific deposits within the rotator cuff tendons in shoulders of patients with shoulder pain and dysfunction. Arch Orthop Trauma Surg 2001; 121: 371–378. [DOI] [PubMed] [Google Scholar]
- 58.Sansone VC, Meroni R, Boria P, et al. Are occupational repetitive movements of the upper arm associated with rotator cuff calcific tendinopathies? Rheumatol Int 2015; 35: 273–280. [DOI] [PubMed] [Google Scholar]
- 59.Kircher J, Morhard M, Patzer T, et al. Do anatomic variants of the acromion shape in the frontal plane influence pain and function in calcifying tendinitis of the shoulder? Knee Surg Sports Traumatol Arthrosc 2012; 20: 368–372. [DOI] [PubMed] [Google Scholar]
- 60.Swannell AJ, Dixon AS. Extra-articular calcification mimicking acute arthritis. Ann Rheum Dis 1969; 28: 678–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Otis JC, Jiang CC, Wickiewicz TL, et al. Changes in the moment arms of the rotator cuff and deltoid muscles with abduction and rotation. J Bone Joint Surg Am 1994; 76: 667–676. [DOI] [PubMed] [Google Scholar]
- 62.Morag Y, Jamadar DA, Miller B, et al. The subscapularis: anatomy, injury, and imaging. Skeletal Radiol 2011; 40: 255–269. [DOI] [PubMed] [Google Scholar]
- 63.Halder A, Zobitz ME, Schultz Fet al. et al. Structural properties of the subscapularis tendon. J Orthop Res 2000; 18: 829–834. [DOI] [PubMed] [Google Scholar]
- 64.Gerber C, Blumenthal S, Curt Aet al. et al. Effect of selective experimental suprascapular nerve block on abduction and external rotation strength of the shoulder. J Shoulder Elbow Surg 2007; 16: 815–820. [DOI] [PubMed] [Google Scholar]
- 65.Hawkes DH, Khaiyat OA, Howard AJ, et al. Patterns of muscle coordination during dynamic glenohumeral joint elevation: an EMG study. PLoS One 2019; 14: e0211800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Giphart JE, van der Meijden OAJ, Millett PJ. The effects of arm elevation on the 3-dimensional acromiohumeral distance: a biplane fluoroscopy study with normative data. J Shoulder Elbow Surg 2012; 21: 1593–1600. [DOI] [PubMed] [Google Scholar]
- 67.Abrassart S, Kolo F, Piotton S, et al. ‘Frozen shoulder’ is ill-defined. How can it be described better? EFORT Open Rev 2020; 5: 273–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kelley MJ, Shaffer MA, Kuhn JE, et al. Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther 2013; 43: A1–A31. [DOI] [PubMed] [Google Scholar]
- 69.Osborne JD, Gowda AL, Wiater Bet al. et al. Rotator cuff rehabilitation: current theories and practice. Phys Sportsmed 2016; 44: 85–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sel-10.1177_17585732241244515 for Clinical features in rotator cuff calcific tendinopathy: A scoping review by Federico Guido, Davide Venturin, Andrea De Santis, Giuseppe Giovannico and Fabrizio Brindisino in Shoulder & Elbow
Supplemental material, sj-docx-2-sel-10.1177_17585732241244515 for Clinical features in rotator cuff calcific tendinopathy: A scoping review by Federico Guido, Davide Venturin, Andrea De Santis, Giuseppe Giovannico and Fabrizio Brindisino in Shoulder & Elbow
Supplemental material, sj-docx-3-sel-10.1177_17585732241244515 for Clinical features in rotator cuff calcific tendinopathy: A scoping review by Federico Guido, Davide Venturin, Andrea De Santis, Giuseppe Giovannico and Fabrizio Brindisino in Shoulder & Elbow