Abstract
Introduction and importance
A hydatid cyst is a parasitic disease caused by the development of the larval form of Echinococcus granulosus (1). The liver and lungs are the most frequent locations, while pancreatic involvement is unusual (<1 %), even in countries where hydatid disease is endemic (2). We report a rare case of a hydatid cyst of the pancreas, revealed by acute pancreatitis. Through this observation and a review of the literature, we discuss the diagnostic and therapeutic challenges of this rare localization of a hydatid cyst.
Case presentation
A 60-year-old man from rural southwestern Tunisia, with a medical history of cardiac conduction disorder such as atrioventricular block treated with a pacemaker and type II diabetes for 10 years, presented with epigastric pain and periodic episodes of vomiting for the past 2 years. The patient noticed a recent exacerbation of the pain over the last 3 months. On physical examination, there was no jaundice or fever. Mild tenderness of the entire supramesocolic region of the abdomen was revealed, and no palpable mass was evident. Biological tests showed an elevation of lipase to 5 times the normal level and an increased leukocyte count of 12,000/dL. Liver function tests were normal. The CT scan indicated pancreatitis, Balthazar grade E, with cystic formation in the tail of the pancreas extending into the dilated Wirsung duct. The echinococcal immunological test (ELISA) was positive, and tumor markers (CEA, CA 19–9) were negative. The diagnosis of a pancreatic hydatid cyst with pancreatitis was considered. The patient underwent surgery 2 months after the onset of pancreatitis. A left splenopancreatectomy was performed. Histopathological examination confirmed the presence of a hydatid cyst. Following an uneventful postoperative period, the patient was discharged on the 7th postoperative day. The patient was treated with Penicillin V (Oracillin®) 2 million IU per day for 2 years and Albendazole 800 mg per day for 2 months after surgery. At 1 year post-surgery, no hydatid recurrence was detected, and hydatid serology was negative.
Clinical discussion
Finally, We reported the case of a rare observation of hydatid cyst of the pancreas revealed by acute pancreatitis.
Conclusion
We highlighted the necessity to consider the hydatid origin when evaluating complicated cystic pancreatic tumors, especially in endemic regions.
Keywords: Pancreas, Hydatid cyst, Echinococcosis, Surgery
Highlights
-
•
When faced with a cystic formation of the pancreas, it is important to consider the hydatid origin, especially in an endemic endemic country and perform hydatid serology
-
•
The benefits of combining CT scan and MRI in the etiological assessment of pancreatic cystic lesions.
-
•
The treatment of Hydatid cysts of the pancreas is surgical.
1. Introduction
Hydatid cyst is a parasitic disease caused by the larval form of Echinococcus granulosus [1]. This zoonosis affects every country worldwide, with varying incidence rates. It remains prevalent and poses a significant public health challenge in highly endemic regions such as the Middle East, South America, and Mediterranean countries [1]. Hepatic and pulmonary locations are the most common, while pancreatic involvement is rare (<1 %), even in endemic countries [2]. We present a rare case of a pancreatic hydatid cyst diagnosed due to acute pancreatitis. Through this case and a literature review, we discuss the diagnostic and therapeutic challenges associated with this uncommon localization of a hydatid cyst.
2. Case presentation
A 60-year-old man from rural southwestern Tunisia, with a history of atrioventricular block treated with a pacemaker and type II diabetes for 10 years, presented with epigastric pain and recurrent vomiting over the past 2 years, worsening significantly in the last 3 months. Physical examination revealed no jaundice or fever. Mild tenderness was noted in the upper abdomen, with no palpable mass. Laboratory tests showed elevated lipase (5 times normal) and leukocytosis (12,000/dL), while liver function tests were normal. An emergency abdominal ultrasound indicated an enlarged pancreas with a 40 mm cystic formation in the pancreatic tail and an 8 mm dilated Wirsung duct. A subsequent CT scan performed after 72 h revealed a globally enlarged pancreas with homogeneous enhancement post-contrast, infiltration of the peripancreatic region, and three acute necrotic collections in the lesser sac and splenopancreatic region. The Wirsung duct remained dilated at 8 mm, communicating with the cystic formation in the peripherally enhanced pancreatic tail measuring 3.7 × 2.5 cm. Abundant intraperitoneal fluid effusion was also observed. (See Fig. 1, Fig. 2.)
Fig. 1.
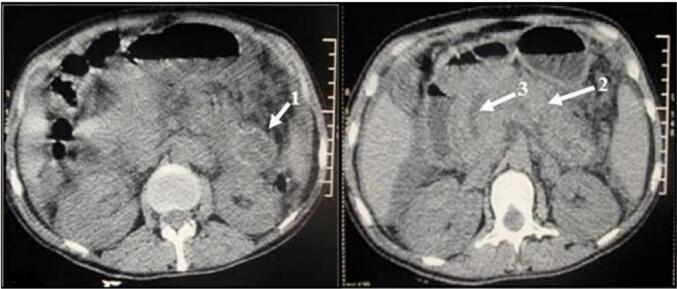
Non-contrast abdominopelvic CT scan showing a cystic formation in the pancreatic tail (1), an enlarged pancreas (2), and a dilated Wirsung duct (3).
Fig. 2.
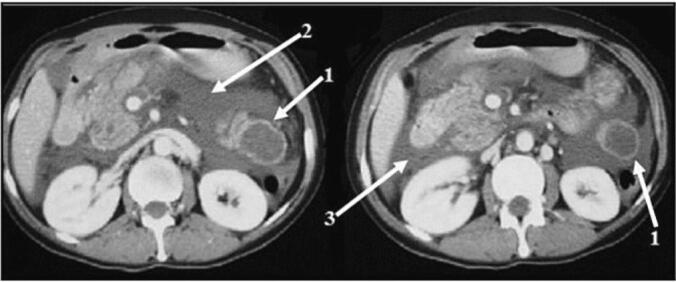
Abdomino-pelvic CT scan with contrast injection showing cystic formation in the pancreatic tail (1), necrotic cast in the lesser sac (2) and intraperitoneal effusion (3).
MRI was not performed due to the patient's pacemaker. Echinococcal immunological test (ELISA) was positive, while tumor markers (ACE, CA 19-9) were negative. The diagnosis of pancreatic hydatid cyst complicated by pancreatitis was made. The patient responded well to medical management of pancreatitis. Surgical intervention was scheduled 2 months later. During surgery, a cystic mass of the pancreatic tail, confirmed as hydatid in nature, was found. A left splenopancreatectomy was performed (Fig. 3).
Fig. 3.
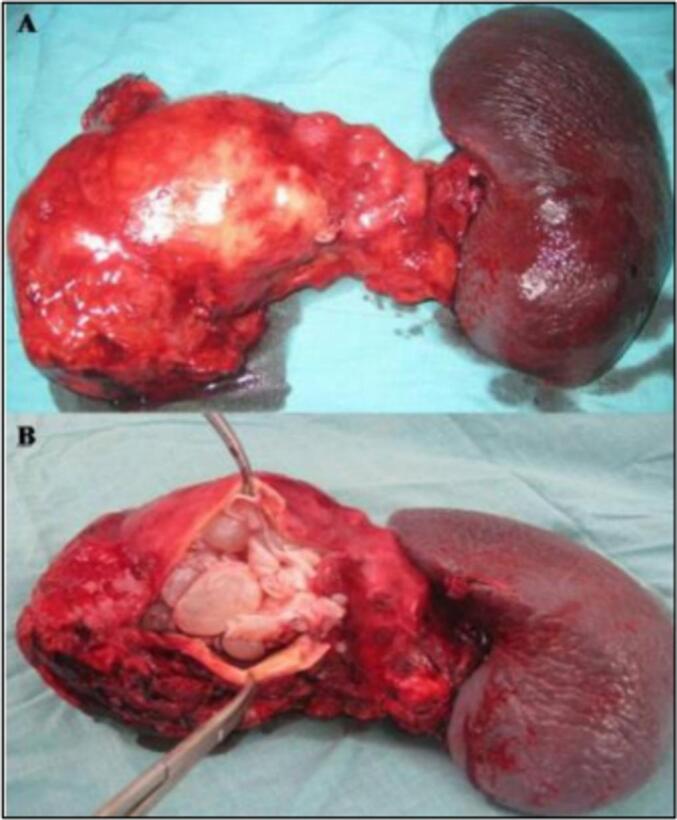
Specimen from Spleno-pancreatectomy (A-before cyst opening; B-after cyst opening).
Histopathological examination confirmed the presence of a hydatid cyst. The patient had an uneventful postoperative recovery and was discharged on the 7th day post-surgery. Postoperatively, the patient received Penicillin V (Oracillin®) 2 million IU/day for 2 years and Albendazole 800 mg/day for 2 months. At the 1-year follow-up, no recurrence was detected, and hydatid serology was negative, although insulin was started for diabetes management.
This work has been reported in line with the SCARE criteria [3].
3. Discussion
Pancreatic hydatid cysts are extremely rare, comprising only 0.2 % of all abdominal hydatid locations [4]. Various aspects including natural history, diagnosis, and management of pancreatic hydatid cysts have been described. The primary mode of pancreatic infestation by hydatid disease is typically hematogenous dissemination [5], although other modes such as local spread through bile or pancreatic ducts and retroperitoneal dissemination have been reported [6]. In 91 % of cases, pancreatic hydatid cysts are solitary [7], with preferential localization in the head (50 %), body (24–34 %), and tail (16–19 %) of the pancreas [8,9].
-
1)
Clinical Manifestations:
Symptoms often develop insidiously over time and depend on cyst location, size, and complications [10]. Cysts in the pancreatic head may present with obstructive jaundice due to bile duct compression, mimicking choledochal cysts [11]. Those in the body may remain asymptomatic until they grow large enough to cause abdominal discomfort or compress neighboring organs, such as the stomach, leading to nausea, vomiting, and early satiety [12]. Cysts in the pancreatic tail can compress the splenic vein, resulting in splenomegaly and portal hypertension [13]. Rare complications include cholangitis, biliary or peritoneal rupture, pancreatic fistula, or abscess formation have been reported [4].
In our case, we reported a rare complication of pancreatic hydatid cyst presenting as acute pancreatitis. A literature review by Akbulut et al. in 2014 documented acute pancreatitis in 6 out of 54 cases of pancreatic hydatidosis, suggesting possible mechanisms including pancreatic duct compression or obstruction by hydatid scolex migration [14,15]. Such lesions can lead to recurrent acute or chronic obstructive pancreatitis, with potential complications like Wirsungorrhage [4].
-
2)
Diagnostic Modalities:
Diagnosis relies heavily on radiological imaging, though it remains challenging. Epidemiological context and hydatid serology aid in diagnosis, but negative serology does not exclude a hydatid cyst since it can be positive in only 54 % of cases [4]. Ultrasound is effective for detecting pancreatic cystic lesions, but specific diagnosis of a hydatid cyst is difficult. MRI is valuable, revealing characteristic features like a peripheral hypo-intense crown on T2-weighted sequences due to fibrous tissue [16]. MRI also aids in assessing pancreatic duct-cyst fistulas. The role of diagnostic aspiration cytology is debated due to risks of intra-abdominal dissemination, pancreatitis, hemorrhage, or cyst infection [17].
-
3)
Differential diagnosis:
In our case, CT scan findings suggested differential diagnoses like serous cystadenoma or hydatid cyst of the pancreatic tail:
-
➢
serous cystadenoma (CS) and mucinous cystadenoma (CM): Classically, the radiological appearance of these tumors is characterized by the the presence of partitions within the cystic mass, which are enhanced after contrast medium, whereas in pancreatic hydatid cyst, the presence of arciform calcifications of the cyst wall that does not enhance after injection of contrast and the presence of daughter cysts are strong arguments in favour of the hydatid nature [18]. However, this is not a constant feature, and arciform calcifications may be found in CM and central calcifications in CS with partitions partitions whose contrast is not always very clear [19].
-
➢
pseudocyst presents with a thick, enhancing wall and T1 hyper-intensity, indicative of hemorrhage and necrosis, with T1 hypo-intensity suggesting pancreatitis.
-
4)
Treatment:
Given potential complications, all pancreatic hydatid cysts require treatment. Surgery remains the mainstay, although medical treatment may be considered. Medical treatment of hydatid cyst is based on oral Albendazole. The usual dosage is 12 to 15 mg/kg/day. Medical treatment alone should be reserved for malignant disseminated hydatidosis. Albendazole is used primarily for disseminated or high-risk cases and to prevent intraoperative dissemination.
Medical treatment is not useful in cases of calcified hydatid cyst, and under no circumstances should delay surgery.
The use of medical treatment one week before surgery and 2 months postoperative period is increasingly recommended to avoid any recurrences. In our case, albendazole was used postoperatively for 2 months [20,21].
Furthermore, the treatment of hydatid cyst of the pancreas is surgical. Surgery involves radical or conservative approaches based on cyst location and presence of pancreatic duct fistulas. In a literature review published in 2017, Dziri el al [22], the authors outlined a surgical treatment strategy for pancreatic hydatid cysts as follows:
Pancreatic head: Conservative surgery is preferred. If there is no fistula with the pancreatic duct, resection of the protruding dome with omentoplasty is recommended. If a fistula is present, anastomosis between the cyst and the digestive tract may be necessary. In rare cases, duodenopancreatectomy is considered.
Pancreatic body: Radical surgery tends to be favored. If there is a fistula between the pancreatic duct and the cyst, central pancreatectomy or anastomosis with the digestive tract is indicated. In the absence of a fistula, resection of the protruding dome with omentoplasty is recommended.
Tail of the pancreas: Radical surgery, specifically distal pancreatectomy with or without splenectomy, is typically recommended. If there is a fistula between the pancreatic duct and the cyst, distal pancreatectomy is performed. If no fistula is present, options include distal pancreatectomy or resection of the protruding dome with omentoplasty.
4. Conclusion
Pancreatic hydatid cysts are exceedingly rare (<1 % of all hydatid locations) and pose diagnostic and therapeutic challenges due to their unusual presentation and potential complications. Consideration of hydatid origin is crucial when evaluating cystic pancreatic tumors, especially in endemic regions. Clinical manifestations vary widely, making differential diagnosis difficult. A multimodal diagnostic approach using CT scan and MRI is essential. Surgical intervention remains the cornerstone of treatment for pancreatic hydatid cysts.
Patient consent
Written informed consent was obtained from the patient for publication of this case report.
Ethical approval
Ethics clearance was not necessary because of the nature of the research that not involve any sensitive data that could potentially harm individual. Besides, the authors have been transparent about the ethical consideration of the study. The authors ensure consent for the data used from the patient, and they declare no potential conflicts of interest.
Funding
No funding was received to conduct this study.
Author contribution
Chaouech MA: Study concept, Methodology, Software. Touzi MA: Data collection, Writing- Original draft preparation. Jalleli M: Supervision and Validation. Noomen F: Reviewing and Editing.
Guarantor
Dr. Touzi Mohamed Aziz.
Research registration number
This is a study about one case report, it's not necessary to be registered.
Declaration of competing interest
None declared.
References
- 1.Moro P., Schantz P.M. Echinococcosis: a review. Int J Infect Dis. Mars. 2009;13(2):125–133. doi: 10.1016/j.ijid.2008.03.037. [DOI] [PubMed] [Google Scholar]
- 2.Bedioui H., Chebbi F., Ayadi S., Daghfous A., Bakhtri M., Jouini M., et al. Kyste hydatique primitif du pancréas: diagnostic et modalités chirurgicales. À propos de trois cas. Gastroenterol. Clin. Biol. 2008;32(1):102–106. doi: 10.1016/j.gcb.2007.12.014. 1 janv. [DOI] [PubMed] [Google Scholar]
- 3.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akbulut S., Yavuz R., Sogutcu N., Kaya B., Hatipoglu S., Senol A., et al. Hydatid cyst of the pancreas: report of an undiagnosed case of pancreatic hydatid cyst and brief literature review. World J Gastrointest Surg. 2014;6(10):190–200. doi: 10.4240/wjgs.v6.i10.190. 27 oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rayate A., Prabhu R., Kantharia C., Supe A. Isolated pancreatic hydatid cyst: Preoperative prediction on contrast-enhanced computed tomography case report and review of literature. Med J Dr Patil Univ. 2012;5(1):66. 1 janv. [Google Scholar]
- 6.Javed A., Agarwal G., Ps A., Manipadam J., Puri S., Agarwal A. Hydatid cyst of the pancreas: a diagnostic dilemma. Trop. Gastroenterol. 2020 [Google Scholar]
- 7.Khiari A., Mzali R., Ouali M., Kharrat M., Kechaou M.S., Beyrouti M.I. Hydatid cyst of the pancreas. Apropos of 7 cases. Ann Gastroenterol Hepatol (Paris) 1994;30(3):87–91. [PubMed] [Google Scholar]
- 8.Soin P., Sharma P., Kochar P.S. Pancreatic echinococcosis. Proc. (Baylor Univ. Med. Cent.) 2019;32(1):85–87. doi: 10.1080/08998280.2018.1512359. 7 janv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lada P.E., Termengo D., Cáceres G., Sanchez Tacone C., Caballero F., Sonzini Astudillo P. Primary hydatid cyst of the pancreas. Rev Fac Cienc Medicas Cordoba Argent. 2017;74(1):33–36. [PubMed] [Google Scholar]
- 10.Barrera M.C., Villanua J., Barrena J.E., Nogues A. Pancreatic hydatid disease. Pediatr. Radiol. 1995;25(1):S169–S170. 1 nov. Références Page II. [PubMed] [Google Scholar]
- 11.Agrawal S., Parag P. Hydatid cyst of head of pancreas mimicking choledochal cyst. BMJ Case Rep. 2011;2011 doi: 10.1136/bcr.04.2011.4087. 30 juin. bcr0420114087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trigui A., Rejab H., Guirat A., Mizouni A., Ben Amar M., Mzali R., et al. Hydatid cyst of the pancreas. About 12 cases. Ann. Ital. Chir. 2013;84(2):165–170. [PubMed] [Google Scholar]
- 13.Szanto P., Goian I., Al Hajjar N., Badea R., Seicean A., Manciula D., et al. Hydatid cyst of the pancreas causing portal hypertension. Maedica. 2010;5(2):139–141. 1 avr. [PMC free article] [PubMed] [Google Scholar]
- 14.Ozmen M.M., Moran M., Karakahya M., Coskun F. Recurrent acute pancreatitis due to a hydatid cyst of the pancreatic head: a case report and review of the literature. JOP. 2005;6(4):354–358. 1 juill. [PubMed] [Google Scholar]
- 15.Diop S.P., Costi R., Le Bian A., Carloni A., Meduri B., Smadja C. Acute pancreatitis associated with a pancreatic hydatid cyst: understanding the mechanism by EUS. Gastrointest. Endosc. 2010;72(6):1312–1314. doi: 10.1016/j.gie.2010.04.051. 1 déc. [DOI] [PubMed] [Google Scholar]
- 16.Macari M., Lee T., Kim S., Jacobs S., Megibow A.J., Hajdu C., et al. Is gadolinium necessary for MRI follow-up evaluation of cystic lesions in the pancréas? Preliminary results. AJR Am. J. Roentgenol. 2009;192(1):159–164. doi: 10.2214/AJR.08.1068. janv. [DOI] [PubMed] [Google Scholar]
- 17.Faucompret S., Farthouat P., Sainton T., Breda Y. Kyste hydatique du pancréas compliqué après cytoponction. Ann. Chir. 2001;126(5):491–492. doi: 10.1016/s0003-3944(01)00536-3. 1 juin. [DOI] [PubMed] [Google Scholar]
- 18.Arnaud A., Jc S., Belkhodja C., Larabi B. 1991. Kyste hydatique du pancréas: a propos de deux observations. [PubMed] [Google Scholar]
- 19.Mohamed H., Azza S., Chrif A., Karim S., Adnen C. Kyste hydatique du pancréas révélé par une pancréatite aigüe: à propos d’un cas. Pan Afr Med J. 2015;22:166. doi: 10.11604/pamj.2015.22.166.6242. 21 oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turkaçapar A.G., Ersoz S., Gungor C., et al. Surgical treatment of hepatic hydatidosis combined with perioperative treatment with albendazole. Eur. J. Surg. 1997;163:923–928. [PubMed] [Google Scholar]
- 21.Dziri C., Haouet K., Fingerhut A. Treatment of hydatid cyst of the liver: where is the evidence? World J. Surg. 2004;28:731–736. doi: 10.1007/s00268-004-7516-z. [DOI] [PubMed] [Google Scholar]
- 22.Dziri C., Dougaz W., Bouasker I. Surgery of the pancreatic cystic echinococcosis: systematic review. Transl Gastroenterol Hepatol. 2017;2:105. doi: 10.21037/tgh.2017.11.13. 8 déc. [DOI] [PMC free article] [PubMed] [Google Scholar]


