Abstract
Children’s eating behaviors are dependent on childhood food experiences, which involve their parental feeding practices, home food environments, and modeling of eating behavior. Intuitive eating (IE) promotes eating based on internal hunger and satiety cues. IE has been associated with improvements in mental and physical health. There has been increasing interest in exploring the association between parent and child IE. The aim of this scoping review was to synthesize current literature reporting on parent and child IE associations. Four databases (MEDLINE, EMBASE, Web of Science and CINAHL) were searched using keywords focusing on IE, parents, and children. Inclusion criteria were reporting on parental and/or child IE, and reporting on parent–child relationships. After screening, 15 studies were retained. From these, 3 main correlations were described. Parental IE was associated with child feeding, child weight concerns, and the home food environment. As well, environmental factors (i.e., family cohesion, food security) were associated with components of child IE. Moreover, IE was directly correlated between parents and children. Overall, this study highlights how child IE behaviors may be shaped by both parental IE and the broader environments that they are raised within. Additional high-quality studies are required to verify these findings.
Keywords: parent, child, intuitive eating, review
“All of family cohesion, encouraging diet diversity, healthy eating guidance, and positive parental coping mechanism/low parental stress were positively associated with child IE.”
Introduction
The desire to eat can be traced back to the influence of motivators such as emotions, external contexts (i.e., food sight or odor), or physical hunger cues. 1 People who practice intuitive eating (IE), which involves eating based on physiological hunger and satiety cues, experience numerous health benefits. 2 IE describes a weight-inclusive eating pattern subdivided into four primary eating behaviors: unconditional permission to eat (UPE), eating for physical rather than emotional reasons (EPR), reliance on hunger and satiety cues (RHSC), and body-food choice congruence (B-FCC). 3 Adults who adhere to IE have a variety of adaptive benefits including increased self-efficacy, self-esteem, optimism, and life satisfaction.1,4-6 IE is also associated with a decreased risk of disordered eating and body dysmorphia. 4 IE interventions for eating disorders have led to a decrease in the number of individuals meeting diagnostic criteria for eating disorders and a decrease in binge eating frequency. 3
The ability to regulate one’s hunger based on internal signals is innate to human behavior. This enables young children to attain the proper nutritional intake to facilitate their development. 7 As children age, their eating behaviors become heavily influenced by childhood food experiences, which include their parental feeding practices, home food environments, and parental modeling of eating behavior. 7 Children can develop maladaptive eating patterns through the influence of each of these factors, which predisposes them to the development of physical and mental ailments.
Parental feeding practices have been evaluated with two main modalities: the Satter Division of Responsibility (sDOR) and the Child Feeding Questionnaire (CFQ). The sDOR stresses the importance of the parent-child relationship and the interplay between their respective responsibilities as the feeder and the eater. 8 Within this model, the child’s eating behavior is described as a learned process that is actively shaped by parental feeding practices. 8 In contrast, the CFQ describes parental feeding practices as methods used to correct child eating behaviors that are considered inappropriate. Although both models have produced valuable insight into parental feeding practices, the current study will focus on the latter.
The CFQ describes the feeding behaviors parents exhibit to obtain a desired eating behavior from their child. 9 Each of the three subscales of the CFQ (restriction, pressure to eat, and monitoring 10 ) have been associated with different eating behaviors in children. Restrictive feeding has been associated with uninhibited eating and excessive weight gain in children.11,12 Parental pressure to eat has been associated with lower fruit and vegetable consumption, higher fat intake, and lower responsiveness to internal hunger cues in children.13-16 In particular, pressure to eat was associated with dietary restraint in young girls, which has implications for the development of eating disorders.16,17 In contrast, parental monitoring of their child’s food intake was protective against emotional eating in children. 18 Overall, there is substantial evidence that parental feeding practices influence both the diet quality and eating patterns of their children.
Children’s dietary habits are also influenced by the food environment in which they are brought up. Those with greater access to fruits and vegetables have both a greater intake in their diet and a greater preference for healthy foods.19-3 As parents and guardians largely determine the home food landscape, their dietary patterns influence those of their children. Children’s intake is directly correlated with the amount of food presented in front of them. Children offered larger meal portions consume more energy than those offered smaller portions. 24 As parents portion meals based on the amount of food that they personally consume, children’s food intake is indirectly related to parental eating behaviors. 25
It is well-established that children learn via social modeling which involves learning a behavior through the observation of another individual or model. Children’s eating behaviors are modeled after the behavioral patterns of their parental figures. Parents who model healthy diets, such as consuming fruits and vegetables, have children who abide by similar diets.22,23,26-30 Mothers who practice eating behaviors such as emotional eating, eating for external reasons, or restrained eating are more likely to have children who demonstrate the same eating behaviors. 31 If parents model IE, their children may also participate in this eating style.
Parents and guardians aim to provide children with the resources, knowledge, and skills to develop into healthy adults. Promoting IE could lead to adaptive benefits for children. To promote IE in children, it is important to understand the factors that facilitate this eating behavior. There has been increasing interest in exploring the association between parental and child IE. While it is known that parental feeding, home food environments and social modeling influence children’s eating patterns, the specific relationships between parental and child IE have yet to be summarized in a review. The aim of this scoping review was to amalgamate the current literature regarding the influences of parental IE on their children, as well as parental factors that contribute to children’s IE.
Methods
The PRISMA-ScR protocol for scoping reviews was followed and the reporting guideline for the manuscript was the PRISMA Extension for Scoping Reviews. 32 The protocol was registered on Open Science Framework (OSF: https://osf.io/uk36b).
Eligibility Criteria
In this scoping review, literature was included that reported on the association between parent and child IE. More specifically, included literature either reported the effect of parental IE on children, or reported parental influences of children’s IE. Inclusion criteria were reporting on parental and/or child IE using a validated model of IE, and reporting on parent–child relationships. No age restriction for children was included to ensure that both prospective studies and retrospective studies reporting on childhood food experiences were included. Inclusion criteria were publication in English in a peer-reviewed journal. Studies were not restricted based on date, geographical location or study design. Grey literature and unpublished literature were excluded.
Information Sources and Search Strategy
After a preliminary review of current literature on IE for parents and children, a search strategy was developed using keywords focusing on IE, parents and children. An example search of MEDLINE is provided in the Supplemental Material (Table S1). The databases included in the search were MEDLINE, EMBASE, Web of Science and CINAHL.
Study Screening
Literature retrieved through searching databases was uploaded to Covidence. After removing duplicates, 2 reviewers screened studies based on their titles and abstracts. To ensure a common understanding of eligibility criteria, a pilot trial was run with both reviewers assessing ten studies together. Afterward, both reviewers independently screened all remaining studies. Full-text screening followed the same process with a pilot trial of 5 studies.
Data Extraction
An Excel spreadsheet was used to extract data from the included studies. Two reviewers extracted data from 2 studies together. Then, they each extracted data from half the remaining studies. Both reviewers verified the data extraction of the other reviewer. Specific data extracted included demographics of parents and children, parents’ eating or feeding behavior, children’s eating behavior, the effects of parental IE on children, parental influences on children’s IE, and other outcomes related to parents or children (e.g., mental health, etc.). Both patient-reported and observer-reported outcomes were presented. Missing data was noted.
Synthesis and Presentation of Results
Data was summarized individually and synthesized. First, associations between parent IE and child feeding behaviors and home food environment were summarized. Then, parental influences on children’s IE were described. If sufficient data was retrieved, a synthesis of results of IE interventions for parents or families would be presented.
Results
Summary
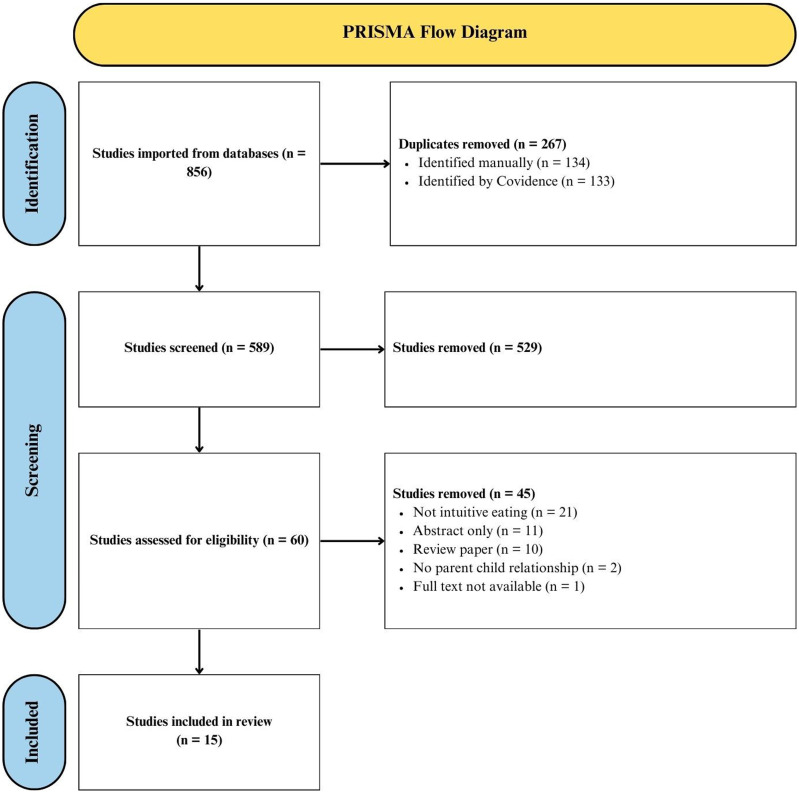
Through the aforementioned selection process, 15 papers were retained for further analysis and data extraction. A PRISMA flow diagram depicting study selection is presented (Figure 1). Of the 15 identified studies, 2 were population-based cross-sectional longitudinal studies,33,34 6 were cross-sectional studies,35-40 6 were retrospective cross-sectional studies,41-46 and 1 was a retrospective chart review. 47 Included studies were published from 2010 to 2024 with most (n = 9) of the studies being completed during or after 2020.33-35,37,40,43,45-47 A total of 11 studies were completed in the United States,33-39,42-44,47 while 1 study was completed in each of Canada, 46 China, 40 and Poland. 45 The last study involved a portion of its sample from both the United States and United Kingdom. 41 IE was reported using the full 21-item Intuitive Eating Scale (IES 4 ) by 5 studies,38,39,41,42,44 the full 23-item Intuitive Eating Scale 2 (IES-2 47 ) by 6 studies,36,40,43,45-47 a modified version of IES by 3 studies,33-35 and a modified version of IES-2 by 1 study. 37 A few of these papers reported on outcomes unrelated to IE. These outcomes were excluded for the purpose of this report. Findings pertaining to IE are highlighted below.
Figure 1.
PRISMA flow diagram.
Effect of Parental IE on Child Feeding Behaviors and Food Environment
Five studies investigated the influence of parental IE on child feeding behaviors and food environment (Table 1).36-39,47 In total, the studies analyzed the responses of 1358 parents of which 1045 (76.95%) identified as mothers and 313 (23.05%) as fathers. Child ages ranged from 8.8 ± 2.0 months, 36 to 15.4 ± 1.43 years. 47 Overall, both total parent IE scores and the subcategories of IE were associated with the food environment and feeding patterns of children.
Table 1.
The Impact of Parental IES on Child Feeding Behaviors, Food Environment, and Eating Patterns.
| Parental Intuitive Eating | |||||||
|---|---|---|---|---|---|---|---|
| Study | Parent Characteristics | Child Characteristics | Total | UPE | EPR | RHSC | B-FCC |
| Khalsa et al, 2019 | N = 201 | Age: 8.8 ± 2.0 mo | / | Neg: Restrictive feeding style | / | Pos: Responsive feeding style | Pos: Restrictive feeding styles |
| Age: 27.2 ± 5.7 | Female: 50% | ||||||
| Mother: 90% | Male: 50% | Pos: Laissez-faire feeding style and indulgent feeding style | |||||
| Father: 9.5% | BMI z score 0.35 ± 1.08 | ||||||
| Nelson et al, 2023 | N = 47 | N = 47 | / | / | Pos: Weight gain in eating disorder treatment | Neg: Adolescent weight concern, shape concern, and eating disorder behavior | Neg: Adolescent weight concern, shape concern, and eating disorder behavior |
| Mother: 72.3% | Age: 15.4 ± 1.43 | ||||||
| Father: 10.6% | Female: 87.2% | ||||||
| Other: 2.4% | Male: 12.8% | ||||||
| BMI: 18.9 ± 2.3 | |||||||
| Rodgers et al, 2022 | N = 750 | Age reported by mothers: 5.1 ± 3.4 | Neg: Salty snacks and soda pop in home (mothers) | / | / | / | / |
| Mother age: 31.3 ± 1.5 | |||||||
| Father age: 31.5 ± 1.4 | Age reported by fathers: 4.0 ± 2.9 | Pos: Availability of fruits and vegetables in the home (mothers), fruit served at meals (mothers), and vegetables served at dinner (both) | |||||
| Mother: 62.7% | |||||||
| Father: 37.3% | |||||||
| Tylka & Kroon Van Diest, 2013 48 | N = 180 | Age: 3.40 ± 0.98 | / | Neg: Restrictive feeding | Pos: Monitoring child food intake | / | / |
| Age: 34.31 ± 6.05 | |||||||
| Mothers: 100% | |||||||
| BMI: 26.41 ± 6.74 | |||||||
| Tylka et al., 2015 | N = 180 | Age: 3.40 ± 0.98 | / | No influence on relationship between child weight concern and restrictive feeding | Child weight concern Pos. to restrictive feeding parents with low or average EPR, no association parents with high EPR | Child weight concern Pos. to restrictive feeding parents with low or average RHSC, no association parents with high RHSC | / |
| Age: 34.31 ± 6.05 | |||||||
| Mothers: 100% | |||||||
| BMI: 26.41 ± 6.74 | |||||||
IES-2 = intuitive eating scale; UPE = unconditional permission to eat; EPR = eating for physical rather than emotional reasons; RHSC = reliance on hunger and satiety cues; B-FCC = body-food choice congruence; Neg = negative association; Pos = positive association.
Three studies specifically analyzed the influence of parental IE subscales on child feeding practices.36,38,39 Two studies found a negative correlation between parental UPE scores and the use of a restrictive feeding style.36,38 Additionally, the study by Tylka, Lumeng and Eneli found that EPR and RHSC moderated the interaction between parental concern about their child’s weight and restrictive feeding. 39 Indeed, in parents with high levels of EPR and RHSC, weight concern and restrictive feeding were unrelated. However, in parents with low or average EPR and RHSC, there was an association between concern about their child’s weight and restrictive feeding. 39 In contrast, restrictive feeding styles were positively correlated with parental B-FCC. 36 In addition to these findings, different parental IE behaviors increased the prevalence of other feeding behaviors. For instance, UPE was positively correlated to both laissez-faire and indulgent feeding styles, and RHSC was directly correlated to a responsive feeding style. 36 There was also a positive association between EPR and monitoring a child’s food intake. 38 Altogether, the different subcategories of parental IE have differing impacts on feeding behaviors.
The work by Rodgers and colleagues 37 examined the relationship between parental total IES-2 scores and the food environment in the home. They demonstrated that maternal IE was associated with many aspects of home food availability and meal experiences. In particular, maternal IE was negatively correlated with the availability of salty foods and soft drinks in the house, and positively correlated to the availability of fruits and vegetables in the home and serving them with meals. Although paternal IE was not associated with the home food environment, they found that fathers with higher IE tended to serve more vegetables at dinner. Together these findings suggest that parental total IE facilitates a healthier food environment.
Nelson and colleagues 47 assessed parental IE as it pertains to facilitating their child’s weight restoration during eating disorder treatment. From this research, they demonstrated that both parental RHSC and B-FCC were negatively correlated to the child’s eating disorder behavior, weight concern, and shape concern. Moreover, a higher parent EPR was associated with increased child beneficial weight gain following the treatment regimen. This finding indicates that parental IE may have the potential to foster healthy eating behaviors in children with eating disorders to uphold their physical health.
Parental Factors Contributing to Child Total IE and IE Subscales
Ten papers reported on parental influences of children’s intuitive eating (Table 2).33-35,40-46 Altogether, these papers include 6766 children and 3631 parents. Five studies did not report on the number of parents included or demographic characteristics.33,40,43-45 Two studies collected data from adolescents.33,34 All ten studies included retrospective reports from adults of childhood influences on eating behavior. Of the children participants, 3843 (56.8%) were female, 2910 (43.0%) were male, 10 (0.1%) identified as another gender, and 3 (0.01%) were unreported. A total of 2386 (65.7%) of parents identified as female/mothers and 1009 (27.8%) identified as males/fathers. The rest of the parents identified as another parental figure or were unreported. Overall, children’s total IE and IE subscales were influenced by several parental factors.
Table 2.
Parental Factors Contributing to Child Total IES and IES Subscales.
| Child Intuitive Eating | |||||||
|---|---|---|---|---|---|---|---|
| Parent Characteristics | Child Characteristics | Total | UPE | EPR | RHSC | B-FCC | |
| Burnette et al, 2023 “Is intuitive eating…” | Not reported | N = 1372 | Neg: Food insecurity in adolescence and early adulthood | / | / | / | / |
| Age: 14.4 ± 2.0 (baseline); 22.0 ± 2.0 (follow-up) | |||||||
| Female: 53.1% | |||||||
| Male: 46.9% | |||||||
| Burnette et al, 2023 “How parental feeding…” | N = 2136 | N = 1383 | Neg: Restrictive feeding, especially with low parental weight concern | / | / | / | / |
| Female age: 41.6 ± 7.8 | Age: 14.4 ± 2.0 (baseline); 22.0 ± 2.0 (follow-up) | Neg: Pressure to eat (adolescent males; emerging adult at low parental weight concern) | |||||
| Male age: 44.8 ± 8.4 | Female: 52.7% | Pos: Pressure to eat (adolescent females; emerging adult at high parental weight concern) | |||||
| Female: 60.6% | Male: 47.3% | ||||||
| Male: 39.4% | |||||||
| Burnette et al, 2022 | N = 891 | N = 891 | Neg: Perceiving the child to be overweight (parent and child) | / | / | / | / |
| Age: 50.4 ± 8.0 | Age: Other: 0.7%22.0 ± 2.0 | Pos: Perceiving weight to be “about right” | |||||
| Mother: 74.2% father: 18.4% | Female: 53.1% male: 45.8% | ||||||
| Ellis et al, 2016 | N = 170 | N = 170 | Neg: Pressure to eat during childhood (female students with higher BMI) | / | / | / | / |
| Age: 48.26 ± 5.87 | Age: 19.75 ± 1.99 | ||||||
| BMI: 27.71 ± 8.87 | Female: 71.2% | ||||||
| Male: 28.8% | |||||||
| BMI: 23.95 ± 4.66 | |||||||
| Galloway et al, 2010 | N = 98 | N = 98 | / | / | Neg: parental monitoring of eating (especially female children) | / | / |
| Age: 38-58 | Age: 17-23 | Neg: Restrictive feeding (female children only) | |||||
| Mother: 97% | Female: 72.4% | ||||||
| Male: 27.6% | |||||||
| Ge et al, 2024 | Primary caregiver = Mother: 94.7% | N = 941 | Pos: Healthful foods at home | Neg: Healthful foods at home (male children only) | Pos: Healthful foods at home | Pos: Healthful foods at home (female children only) | Pos: Healthful foods at home |
| Father: 53.7% | Age: 44.35 ± 13.15 | Pos: Encouraging diet diversity (female children only) | Pos: Honoring children’s hunger and satiety feelings (male children only) | Pos: Encouraging diet diversity (female children only) | Pos: Encouraging diet diversity | Pos: Encouraging diet diversity (female children only) | |
| Female: 53.2% | Pos: Honoring children’s hunger and satiety feelings (male children only) | Pos: Honoring children’s hunger and satiety (male children only) | |||||
| Male: 46.4% | Pos: Considering child’s taste preference (male children only) | ||||||
| Other: 0.4% | |||||||
| Kroon Van Diest & Tylka, 2010 | Not reported | N = 238 | Neg: Restrictive/critical eating messages | / | / | / | / |
| Age: 20.87 ± 3.92 | |||||||
| Female: 67.2% | |||||||
| Male: 32.8% | |||||||
| Malachowska & Jezewska-Zychowicz, 2023 | Not reported | N = 708 | / | Neg: Restrictive feeding style | Neg: Restrictive feeding style (especially female children) | Neg: Restrictive feeding style (especially female children) | / |
| Age: 36.9 ± 11.5 | Neg: Pressure, food reward | Pos: Healthy eating guidance | |||||
| Female: 67.4% | Pos: Healthy eating guidance | ||||||
| Male: 32.6% | Pos: child control of feeding (male children only) | ||||||
| Roberts et al, 2020 | N = 336 | N = 263 | Neg: Maternal BMI (female children only) | / | / | / | / |
| Age: 56.62 ± 8.81 | Age: 29.13 ± 6.65 | None: Feeding practices (restriction, monitoring, etc.) | |||||
| Mother: 100% | Female: 100% | ||||||
| BMI: 26.86 ± 5.30 | BMI: 24.89 ± 5.30 | ||||||
| Yang et al, 2023 | Not reported | N = 702 | Pos: Family cohesion and positive coping styles (mediated by perceived stress) | / | / | / | / |
| Age: 21.12 ± 1.48 | |||||||
| Female: 45.4% | |||||||
| Male: 54.6% | |||||||
| BMI: 20.49 ± 2.69 | |||||||
IES-2 = intuitive eating scale; UPE = unconditional permission to eat; EPR = eating for physical rather than emotional reasons; RHSC = reliance on hunger and satiety cues; B-FCC = body-food choice congruence; Neg = negative association; Pos = positive association.
Familial factors negatively associated with children’s total IE were parent and child perceptions that the child was overweight, 35 and maternal body mass index (BMI) for female children. 46 As well, food insecurity in childhood was associated with lower IE in adolescence and early adulthood. 33 The availability of healthful foods at home was negatively associated with the subscale of UPE for male children. 43 Finally, parental monitoring of eating was negatively associated with the subscale of EPR. 42
Four papers found a negative association between parental restrictive feeding and children’s IE in one or more subscales.34,42,44,45 Restrictive feeding was associated with lower total IE score,34,44 especially when parents were not concerned about their children’s weight. 34 Restrictive feeding was negatively associated with the subscale of EPR, especially in female children.42,45 Additional subscales negatively associated with restrictive feeding were UPE and RHSC. 45 One paper found no association between restrictive feeding and children’s total IE scores. 46
Three studies found a negative association between parental pressure to eat and children’s IE. One study found that pressure to eat was negatively associated with total IE scores in females with higher BMI. 41 Another found a negative association between food reward and the subscale of children’s EPR. Total IE scores were negatively associated with pressure to eat in both adolescent males and emerging adults whose parents were not concerned about their weight. 34 Contrarily, 1 study found that pressure to eat was positively associated with IE in adolescent females and emerging adults whose parents had high concern about their weight. 34
Other factors positively associated with children’s total IE scores were perceiving the child’s weight to be adequate, 35 family cohesion and positive coping styles, 40 and the availability of healthful foods at home. 43 Additionally, encouraging diet diversity and honoring children’s hunger and satiety were positively associated with total IE for females and male children, respectively. 43 The availability of healthful foods at home, encouraging diet diversity, and healthy eating guidance were generally positively associated with subscales of IE including EPR, RHSC, and B-FCC.43,45
The Association Parent IE & Child IE Behaviors
Two studies analyzed the direct association between parent and child IE.35,47 Nelson and colleagues 47 found that parent RHSC and child total IE were positively associated. Moreover, parent and child B-FCC were positively correlated. Similarly, Burnette and colleagues 35 found that 52.9% of parent–child dyads had concordant eating behaviors. Specifically, 31.2% of dyads were both IE, while 21.7% were both non-IE. The smallest category was of dyads wherein the child engaged in IE but the parent did not. Altogether, these findings illustrate direct associations between parent and child IE.
Discussion
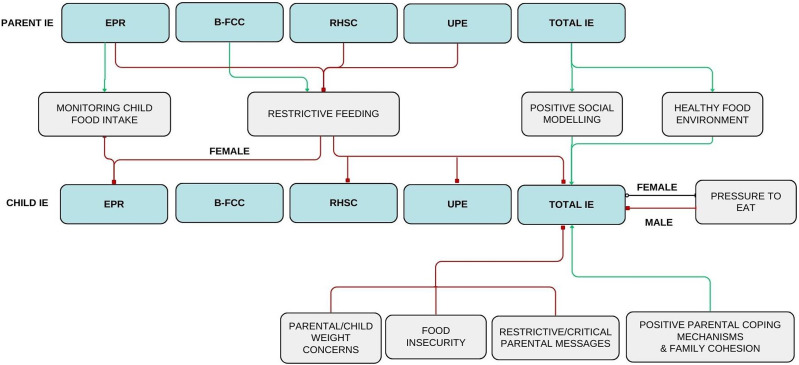
The current review evaluated the association between parent and child IE. The results suggest that parental IE may both directly and indirectly facilitate IE in children. This study found associations between numerous parental behaviors and child IE. These results confirm that parents have a substantial influence on the development of eating behaviors in their children. A summary of connections between parental and child IE is presented (Figure 2).
Figure 2.
The direct and indirect pathways in parental facilitation of child intuitive eating. After analysis of the 15 retained studies, correlations between parental IE and child IE were extracted and variables mediating child IE were identified (gray boxes). The described variables were found to have a positive (green line) or negative (red line) association with a child’s tendency to exhibit IE behaviors. Some correlations only pertain to male or female children and are designated as such. The correlation between pressuring a female child to eat and said child’s total IE was conflicting in the literature; consequently, it is denoted with a black line. IE = intuitive eating; UPE = unconditional permission to eat; EPR = eating for physical rather than emotional reasons; RHSC = reliance on hunger and satiety cues; B-FCC = body-food choice congruence.
Parental IE indirectly facilitates child IE through three main variables: parental feeding practices, weight concerns for their children, and the home food environment. First, high parental IE scores, specifically in the subdomain of UPE, were negatively associated with restrictive feeding practices.36,38 As well, parental use of restrictive feeding decreased child IE behaviors.34,42,44,45 Previous literature has established a link between restrictive feeding practices and both uninhibited eating and excessive weight gain in children.11,12 From the results of this study, a model can be proposed wherein parents who do not engage in IE may be more inclined to turn to restrictive feeding than those who do. Subsequently, this may lead to a lower probability that their child will practice IE.
High parental EPR scores were positively associated with monitoring their child’s food intake. 38 Interestingly, this feeding practice was correlated with a decrease in daughter’s EPR score. 42 This finding contradicts a previous study which found that parental monitoring was linked to lower emotional eating in children. 18 Perhaps this finding is related to children’s reliance on their guardians to select the timing and contents of their meals. Although monitoring did not encourage child IE, it does have beneficial implications on the child’s diet. Indeed, a previous study found that parental monitoring increased the chances that children would eat the recommended daily amounts of fruits, grains, dairy, and vegetables. 49
The second manner by which parental IE is indirectly associated with child IE is through child weight concerns. As per the study completed by Tylka, Lumeng and Eneli, it was found that parental EPR and RHSC moderated the association between parental concern about their child’s weight and the use of restrictive feeding. 39 Parents with higher IE scores in EPR and RHSC were less likely to use restrictive feeding in response to concern over their child’s weight. 39 Moreover, Burnette and colleagues 35 explained a negative correlation between child weight concerns and child total IE. It can be proposed that parents with higher IE are less likely to implement restrictive feeding in the context of concern for their child’s weight, which therefore promotes the development of IE behaviors in their child.
Parental IE may also increase child IE by influencing the food landscape of the home. Parents with higher total IE scores were more likely to have fruits and vegetables available in the household and less likely to bring salty snacks or soda into the home. 37 When healthy foods were accessible to children, they were more likely to engage in IE. 43 These two findings link parental IE to an increase in child IE. Additionally, other literature has reported that children with greater accessibility to healthy foods (i.e., fruits, vegetables, dairy) are more likely to develop a preference for said foods and incorporate them more frequently into their diet.19-23 Therefore, not only does parental IE promote children’s health by increasing their likelihood of practicing IE, but it also supports a well-rounded nutritious diet as well.
The current review also highlighted several parent-involved factors that influence child IE. All of family cohesion, encouraging diet diversity, healthy eating guidance, and positive parental coping mechanism/low parental stress were positively associated with child IE. Both food insecurity and critical parental messages directed to their child were negatively correlated with child IE. Of note, the implications of parental pressure to eat were conflicting. While two studies reported that pressure to eat was negatively correlated with IE in sons, the literature was not consistent for daughters.34,45 Two studies reported that pressure to eat was linked to decreased IE behaviors in daughters,41,45 whereas another study reported the opposite to be true. 34 This finding is echoed in the broader literature that describes diverse outcomes of pressure to eat. Pressuring a child to eat has been associated with a lower consumption of fruits and vegetables, more snacking, and a higher fat intake.3,13,14,16,17 As well, pressure to eat has been associated with disordered eating behaviors in daughters including dietary restraint. 17 Other studies have indicated the opposite, describing a decrease in snacking behavior and healthy eating patterns with pressure to eat. 50 As such, the implications of pressuring a child to eat on their tendency to engage in IE and on eating behaviors in general requires further investigations.
Two studies demonstrated direct associations between parent and child IE.35,47 In particular, high parental scores of RHSC and B-FCC were positively associated with total child IE scores and child B-FCC scores, respectively. 47 These findings are consistent with the well-established theory of social modeling. Previous literature has demonstrated that children who observe their parents select nutritious food are more likely to do so themselves, and that children often mimic the eating behaviors practiced by their parents.22,23,26-31
The results of this review could be applied in the development of family-based interventions aimed at increasing the overall health and well-being of children and youth. Past literature has shown IE to be an effective method of upholding an individual’s health. 2 Directly promoting IE to youth via education or reinforcement may improve their future health outcomes. Interventions should simultaneously focus on the behaviors of the parents and guardians of these children. Education should be given to families on the importance of maintaining a healthy home food environment, the benefits/drawbacks of the different feeding practices, and the importance of social modeling. As well, interventions should look at each family unit holistically and consider addressing underlying causes of food insecurity or family unrest that may impede children from developing IE habits.
The importance of lifestyle medicine, especially with regards to the pediatric population, is a rapidly developing area of interest. To date, there are no known studies which synthesize the literature pertaining to the effects of parental IE on their children. Instead, other authors have focused on the effects of other parental eating behaviors such as eating disorders or mindful eating/parenting.7,51,52 This is likely due to the novelty of research on IE, which is reflected in the fact that most of the literature included in this report was published from 2020 to 2024. This review summarizes current literature to provide novel insight into the associations of specific subdomains of IE (i.e., UPE, EPR, RHSC, and B-FCC) between parents and children. Specific parental factors can be targeted to facilitate the development of child IE.
A limitation of this study is that, due to the novelty of research in this field, only 15 studies were included in this scoping review. As well, studies were included regardless of children’s age. This could complicate data interpretation as children become more independent in their feeding choices as they age. Studies were only included if they clearly demonstrated a relationship between IE amongst parents and children. However, there may be other parentally influenced variables that have yet to be directly correlated to child IE. For instance, higher screen use both during and outside mealtimes results in lower IE in the adult population.53,54 Correspondingly, children who spend more time on screens have poorer dietary patterns55-58; however, published literature has not described the influence of screen time specifically on child IE. As primary caregivers greatly influence their children’s screen time, 59 this may be another means by which parents influence their child’s IE behaviors. Therefore, it is plausible that other variables were not described in this review due to the lack of direct correlations in the current literature.
Additionally, none of the studies referenced in this review were randomized control trials or interventional studies, rather the results concluded here were from retrospective reports and cross-sectional analyses. Consequently, causative conclusions cannot be drawn from the work currently available. It is also important to note that 11 of the 15 studies were published in the United States, so it is possible that the associations depicted in this paper may only be applicable to certain geographical locations. Further research in different countries is required to verify the results of the current review.
Nonetheless, the findings from the current review suggest that parental IE directly increases the likelihood of children developing IE. Parental IE may also indirectly increase child IE through the pathways of parental feeding practices, and the home food environment. Moreover, additional factors such as food security, family cohesion, parental weight concern, and feeding practices all impact eating behaviors in children. Additional high-quality studies are required to verify these findings.
Supplemental Material
Supplemental Material for Association of Parent and Child Intuitive Eating: A Scoping Review by Michaela L. Dowling, Madeline E. Hubbard, and Richa Agnihotri in American Journal of Lifestyle Medicine
Acknowledgments
The authors would like to thank Seddiq Weera for providing information on research methodology.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
Ethical Approval and Informed Consent Statements
As this was a review paper with no human or animal subjects, no ethical approval or informed consent was required.
ORCID iD
Michaela L. Dowling https://orcid.org/0009-0008-2413-1909
Madeline E. Hubbard https://orcid.org/0009-0006-3858-9123
Data Availability Statement
The raw data extraction table is available upon request to the corresponding author.*
References
- 1.Denny KN, Loth K, Eisenberg ME, Neumark-Sztainer D. Intuitive eating in young adults. Who is doing it, and how is it related to disordered eating behaviors? Appetite. 2013;60:13-19. doi: 10.1016/j.appet.2012.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Babbott KM, Cavadino A, Brenton-Peters J, Consedine NS, Roberts M. Outcomes of intuitive eating interventions: A systematic review and meta-analysis. Eat Disord. 2023;31(1):33-63. doi: 10.1080/10640266.2022.2030124 [DOI] [PubMed] [Google Scholar]
- 3.Ramón Barrada J, Cativiela B, van Strien T, Cebolla A. Intuitive eating: a novel eating style? Evidence from a Spanish sample. Eur J Psychol Assess. 2020;36(1):19-31. doi: 10.1027/1015-5759/a000482 [DOI] [Google Scholar]
- 4.Tylka TL. Development and psychometric evaluation of a measure of intuitive eating. J Counsel Psychol. 2006;53(2):226-240. doi: 10.1037/0022-0167.53.2.226 [DOI] [Google Scholar]
- 5.Bacon L, Aphramor L. Weight science: Evaluating the evidence for a paradigm shift. Nutr J. 2011;10(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janet P, Pete HC. Undieting: A program to help people stop dieting. Int J Eat Disord. 1992;11(3):261-268. doi: [DOI] [Google Scholar]
- 7.Brantley C, Knol LL, Douglas JW. Parental mindful eating practices and mindful eating interventions are associated with child emotional eating. Nutr Res. 2023;111:34-43. doi: 10.1016/j.nutres.2022.11.001 [DOI] [PubMed] [Google Scholar]
- 8.Satter E. The feeding relationship: problems and interventions. J Pediatr. 1990;117:S181-189. doi: 10.1016/s0022-3476(05)80017-4 [DOI] [PubMed] [Google Scholar]
- 9.Shloim N, Edelson LR, Martin N, Hetherington MM. Parenting styles, feeding styles, feeding practices, and weight status in 4-12 year-old children: a systematic review of the literature. Front Psychol. 2015;6:1849. doi: 10.3389/fpsyg.2015.01849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Costa A, Oliveira A. Parental feeding practices and children’s eating behaviors: An overview of their complex relationship. Healthcare. 2023;11(3):400. doi: 10.3390/healthcare11030400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birch LL, Zimmerman SI, Hind H. The influence of social-affective context on preschool children’s food preferences. Child Dev. 1980;51:856-861. doi: 10.2307/1129474 [DOI] [Google Scholar]
- 12.Birch LL, Fisher JO. Mothers' child-feeding practices influence daughters' eating and weight. Am J Clin Nutr. 2000;71:1054-1061. doi: 10.1093/ajcn/71.5.1054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fisher JO, Mitchell DC, Smiciklas-Wright H, Birch LL. Parental influences on young girls' fruit and vegetable, micronutrient, and fat intakes. J Am Diet Assoc. 2002;102(1):58-64. doi: 10.1016/s0002-8223(02)90017-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee Y, Birch LL. Diet quality, nutrient intake, weight status, and feeding environments of girls meeting or exceeding the American Academy of Pediatrics recommendations for total dietary fat. An Pediatr. 2002;54(3):179-186. doi: 10.1542/peds.107.6.e95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown KA, Ogden J, Vögele C, Gibson EL. The role of parental control practices in explaining children’s diet and BMI. Appetite. 2008;2(3):252-259. doi: 10.1016/j.appet.2007.07.010 [DOI] [PubMed] [Google Scholar]
- 16.Carper JL, Orlet Fisher J, Birch LL. Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 2000;2:121-129. doi: 10.1006/appe.2000.0343 [DOI] [PubMed] [Google Scholar]
- 17.Galloway AT, Fiorito LM, Francis LA, Birch LL. Finish your soup’: Counterproductive effects of pressuring children to eat on intake and effect. Appetite. 2006;3:318-323. doi: 10.1016/j.appet.2006.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farrow CV. Do parental feeding practices moderate the relationships between impulsivity and eating in children? Eat Behav. 2012;2:150-153. doi: 10.1016/j.eatbeh.2011.11.015 [DOI] [PubMed] [Google Scholar]
- 19.Cullen KW, Baranowski T, Owens E, Marsh T, Rittenberry L, de Moor C. Availability, accessibility, and preferences for fruit, 100% fruit juice, and vegetables influence children's dietary behavior. Health Educ Behav. 2003;30(5):615-626. https://www.jstor.org/stable/45055578 [DOI] [PubMed] [Google Scholar]
- 20.Kratt P, Reynolds K, Shewchuk R. The role of availability as a moderator of family fruit and vegetable consumption. Health Educ Behav. 2000;27(4):471-482. doi: 10.1177/109019810002700409 [DOI] [PubMed] [Google Scholar]
- 21.Fisher JO, Mitchell DC, Smiciklas-Wright H, Mannino ML, Birch LL. Meeting calcium recommendations during middle childhood reflects mother-daughter beverage choices and predicts bone mineral status. Am J Clin Nutr. 2004;79(4):698-706. doi: 10.1093/ajcn/79.4.698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wind M, de Bourdeaudhuij I, te Velde SJ. et al. Correlates of fruit and vegetable consumption among 11-year-old Belgian-Flemish and Dutch schoolchildren. J Nutr Educ Behav. 2006;4:211-221. doi: 10.1016/j.jneb.2006.02.011 [DOI] [PubMed] [Google Scholar]
- 23.Reinaerts E, de Nooijer J, Candel M, de Vries N. Explaining school children’s fruit and vegetable consumption: The contributions of availability, accessibility, exposure, parental consumption and habit in addition to psychosocial factors. Appetite. 2007;2:248-258. doi: 10.1016/j.appet.2006.09.007 [DOI] [PubMed] [Google Scholar]
- 24.Fisher JO, Rolls RJ, Birch LL. Children's bite size and intake of an entrée are greater with large portions than with age-appropriate or self-selected portions. Am J Clin Nutr. 2003;77(5):1164-1170. doi: 10.1093/ajcn/77.5.1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Acolatse L, Pourshahidi LK, Logue C, McCann MT, Kerr MA. Child food portion sizes in the home environment: How do parents decide? Proc Nutr Soc. 2023;82(3):386-393. doi: 10.1017/S0029665123000071 [DOI] [PubMed] [Google Scholar]
- 26.Birch LL. Effects of peer models' food choices and eating behaviors on preschoolers' food preference. Child Dev. 1980;51:489-496. doi: 10.2307/1129283 [DOI] [Google Scholar]
- 27.Lee S, Reicks M. Environmental and behavioral factors are associated with the calcium intake of low-income adolescent girls. J Am Diet Assoc. 2003;103(11):1526-1529. doi: 10.1016/j.jada.2003.08.020 [DOI] [PubMed] [Google Scholar]
- 28.Young EM, Fors SW, Hayes DM. Associations between perceived parent behaviors and middle school student fruit and vegetable consumption. J Nutr Educ Behav. 2004;36(1):2-8. doi: 10.1016/S1499-4046(06)60122-X [DOI] [PubMed] [Google Scholar]
- 29.Cullen KW, Baranowski T, Rittenberry L, Cosart C, Hebert D, de Moor C. Child-reported family and peer influences on fruit, juice and vegetable consumption: reliability and validity of measures. Health Educ Res. 2001;16(2):187-200. doi: 10.1093/her/16.2.187 [DOI] [PubMed] [Google Scholar]
- 30.Draxten M, Fulkerson JA, Friend S, Flattum CF, Schow R. Parental role modeling of fruits and vegetables at meals and snacks is associated with children’s adequate consumption. Appetite. 2014;78:1-7. doi: 10.1016/j.appet.2014.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zarychta K, Kulis E, Gan Y, Chan CKY, Horodyska K, Luszczynska A. Why are you eating mom? Maternal emotional, restrained, and external eating explaining children’s eating styles. Appetite. 2019;141:104335. doi: 10.1016/j.appet.2019.104335 [DOI] [PubMed] [Google Scholar]
- 32.Tricco AC, Lillie E, Zarin W. et al. PRISMA extension for scoping reviews (PRISMAScR): Checklist and explanation. Ann Intern Med. 2018;169:467-473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 33.Burnette CB, Hazzard VM, Larson N, Hahn SL, Eisenberg ME, Neumark-Sztainer D. Is intuitive eating a privileged approach? Cross-sectional and longitudinal associations between food insecurity and intuitive eating. Publ Health Nutr. 2023;26(7):1358-1367. doi: 10.1017/S1368980023000460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burnette CB, Hazzard VM, Linardon J, Rodgers RF, Loth KA, Neumark-Sztainer D. How parental feeding practices relate to young people's intuitive eating: cross-sectional and longitudinal associations by gender and weight concern. J Adolesc Health. 2023;73(6):1145-1152. doi: 10.1016/j.jadohealth.2023.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burnette CB, Hazzard VM, Hahn SL, Larson N, Neumark-Sztainer D. Like parent, like child? Intuitive eating among emerging adults. Appetite. 2022;176:106132. doi: 10.1016/j.appet.2022.106132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khalsa AS, Woo JG, Kharofa RY, Geraghty SR, DeWitt TG, Copeland KA. Parental intuitive eating behaviors and their association with infant feeding styles among low-income families. Eat Behav. 2019;32:78-84. doi: 10.1016/j.eatbeh.2019.01.001 [DOI] [PubMed] [Google Scholar]
- 37.Rodgers RF, Hazzard VM, Franko DL, Loth KA, Larson N, Neumark-Sztainer D. Intuitive eating among parents: Associations with the home food and meal environment. J Acad Nutr Diet. 2022;122(7):1336-1344. doi: 10.1016/j.jand.2022.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tylka TL, Eneli IU, Kroon Van Diest AM, Lumeng JC. Which adaptive maternal eating behaviors predict child feeding practices? An examination with mothers of 2- to 5-year-old children. Eat Behav. 2013;14(1):57-63. doi: 10.1016/j.eatbeh.2012.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tylka TL, Lumeng JC, Eneli IU. Maternal intuitive eating as a moderator of the association between concern about child weight and restrictive child feeding. Appetite. 2015;95:158-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang C, Wen H, Zhou Y, Wang Y, Sun Y, Yuan F. Family cohesion and intuitive eating in Chinese college students: A serial mediation model. Appetite. 2023;190:107021. doi: 10.1016/j.appet.2023.107021 [DOI] [PubMed] [Google Scholar]
- 41.Ellis JM, Galloway AT, Webb RM, Martz DM, Farrow CV. Recollections of pressure to eat during childhood, but not picky eating, predict young adult eating behavior. Appetite. 2016;97:58-63. doi: 10.1016/j.appet.2015.11.020 [DOI] [PubMed] [Google Scholar]
- 42.Galloway AT, Farrow CV, Martz DM. Retrospective reports of child feeding practices, current eating behaviors, and BMI in college students. Obesity. 2010;18:1330-1335. doi: 10.1038/oby.2009.393 [DOI] [PubMed] [Google Scholar]
- 43.Ge L, Byrd K, Giang MT. Positive feeding practices during childhood are associated with higher intuitive eating in adulthood. Am J Health Educ. 2024;55(2):127-136. doi: 10.1080/19325037.2023.2297282 [DOI] [Google Scholar]
- 44.Kroon Van Diest AM, Tylka TL. The caregiver eating messages scale: development and psychometric investigation. Body Image. 2010;7(4):317-326. doi: 10.1016/j.bodyim.2010.06.002 [DOI] [PubMed] [Google Scholar]
- 45.Malachowska A, Jezewska-Zychowicz M. Retrospective reports of parental feeding practices and current eating styles in Polish adults. Nutrients. 2023;15(19):4217. doi: 10.3390/nu15194217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roberts LT, Carbonneau N, Goodman LC, Musher-Eizenman DR. Retrospective reports of childhood feeding in mother-daughter dyads. Appetite. 2020;149:104613. doi: 10.1016/j.appet.2020.104613 [DOI] [PubMed] [Google Scholar]
- 47.Nelson JD, Trojanowski PJ, Aarnio-Peterson CM, Fischer S, Adams L, Matthews A. Caregiver and adolescent intuitive eating behavior: associations with weight change during family-based treatment for anorexia nervosa. Eat Weight Disord. 2023;28(1):32. doi: 10.1007/s40519-023-01557-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tylka TL, Kroon Van Diest AM. The Intuitive Eating Scale–2: item refinement and psychometric evaluation with college women and men. J Counsel Psychol. 2013;60(1):137-153. doi: 10.1037/a0030893 [DOI] [PubMed] [Google Scholar]
- 49.Ardakani A, Monroe-Lord L. Monitoring is an effective parenting practice to encourage adolescents to meet the dietary guidelines for Americans. J Nutr Educ Behav. 2023;55(7):10-11. doi: 10.1016/j.jneb.2023.05.024 [DOI] [Google Scholar]
- 50.Sleddens EFC, Kremers SPJ, De Vries NK, Thijs C. Relationship between parental feeding styles and eating behaviors of Dutch children aged 6-7. Appetite. 2010;54(1):30-36. doi: 10.1016/j.appet.2009.09.002 [DOI] [PubMed] [Google Scholar]
- 51.Gouveia MJ, Canavarro MC, Moreira H. How can mindful parenting be related to emotional eating and overeating in childhood and adolescence? The mediating role of parenting stress and parental child-feeding practices. Appetite. 2019;138:102-114. doi: 10.1016/j.appet.2019.03.021 [DOI] [PubMed] [Google Scholar]
- 52.Martini MG, Barona-Martinez M, Micali N. Eating disorders mothers and their children: a systematic review of the literature. Arch Womens Ment Health. 2020;23:449-467. doi: 10.1007/s00737-020-01019-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.He J, Wang Z, Fu Y. et al. Associations between screen use while eating and eating disorder symptomatology: exploring the roles of mindfulness and intuitive eating. Appeptite. 2024;197:107320. doi: 10.1016/j.appet.2024.107320 [DOI] [PubMed] [Google Scholar]
- 54.Hazzard VM, Burnette CB, Hooper L, Larson N, Eisenberg ME, Neumark-Sztainer D. Lifestyle health behavior correlates of intuitive eating in a population-based sample of men and women. Eat Behav. 2022;46:101644. doi: 10.1016/j.eatbeh.2022.101644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tambalis KD, Panagiotakos DB, Psarra G, Sidossis LS. Screen time and its effect on dietary habits and lifestyle among schoolchildren. Cent Eur J Publ Health. 2020;28(4):260-266. doi: 10.21101/cejph.a6097 [DOI] [PubMed] [Google Scholar]
- 56.Semar R, Bakshi N. Correlation of screen time with eating behavior among school-going children aged 8 to 10 years in East Delhi, India. J Indian Assoc Child Adolesc Ment Health. 2023;18(4). [Google Scholar]
- 57.Jusienė R, Urbonas V, Laurinaitytė I. et al. Screen use during meals among young children: Exploration of associated variables. Medicina. 2019;55(10):688. doi: 10.3390/medicina55100688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lopez RB, Heatherton TF, Wagner DD. Media multitasking is associated with higher risk for obesity and increased responsiveness to rewarding food stimuli. Brain Imaging Behav. 2020;14:1050-1061. doi: 10.1007/s11682-019-00056-0 [DOI] [PubMed] [Google Scholar]
- 59.Sanders W, Parent J, Forehand R. Parenting to reduce child screen time: A feasibility pilot study. J Dev Behav Pediatr. 2018;39(1):46-54. doi: 10.1097/DBP.0000000000000501 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Association of Parent and Child Intuitive Eating: A Scoping Review by Michaela L. Dowling, Madeline E. Hubbard, and Richa Agnihotri in American Journal of Lifestyle Medicine
Data Availability Statement
The raw data extraction table is available upon request to the corresponding author.*