Abstract
Introduction
Bladder leiomyomas (LM) are uncommon, non-cancerous growths that originate from the smooth muscle cells of the bladder and constitute 0.5% of bladder tumor cases. This review aims to compile existing data and present a summary of bladder leiomyomas’ characteristics, management, and related outcomes.
Method
We conducted systematic review of studies that investigated bladder leiomyoma. Case studies or series describing individuals with bladder leiomyoma who underwent surgery and the outcomes were included. Four databases were used in our literature search, which was carried out until January 2024: PubMed, Proquest, EBSCOHost, and Google Scholar. We utilized MeSH terms such as “leiomyoma,” “urinary bladder,” and looked for synonyms of “bladder leiomyoma” in free text.
Results
A total of 99 studies with 119 patients were included. Most reported bladder leiomyoma cases were female, accounting for 79.0% of all cases. While symptomatic patients primarily presented with lower urinary tract symptoms (LUTS) (59.7%), hematuria (24.4%), acute urine retention (11.8%), and about 16.8% of cases were incidentally detected. Storage-related symptoms were the most common LUTS (37.0%). Different diagnostic techniques were used, frequently combining CT (Computed Tomography), MRI (Magnetic Resonance Imaging), USG (Ultrasonography), and/or cystoscopy. Bladder leiomyomas were commonly found on the left lateral wall (26.9%) and the bladder neck (17.6%). In more than half of the cases (52.1%) the treatment techniques used were transurethral resection (TURBt/TUR). Fifteen out of 119 cases (12.6%) had recurrence or remain symptomatic. Symptomatic symptoms at first presentation and extended location are frequently found among recurrent or symptomatic cases after first management.
Conclusion
Management of bladder leiomyoma should focus on the relief of symptoms and recurrence and be personalized based on the tumor characteristics, patient symptoms, and surgeon’s expertise. Further investigation is necessary to fully understand the best course of treatment and long-term results for bladder leiomyomas. In particular, prospective trials with bigger participant pools and meticulously controlled factors should be the main emphasis of this research.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12894-024-01624-3.
Keywords: Bladder leiomyoma, Bladder neoplasm, Clinical characteristics, Management, Outcome of treatment
Introduction
Bladder leiomyomas (LM) are uncommon, benign tumors that develop from the smooth muscle cells of the bladder wall and constitute less than 0.5% of bladder tumour [1, 2]. Despite being benign, these tumors have the potential to restrict the bladder outlet if located near bladder outlet or neck, which can result in symptoms and consequences related to the urinary tract, including sensation of incomplete emptying, weak stream, urine retention, recurrent urinary tract infections, and renal impairment [3–5], . The symptoms vary according to the size and location of the tumor. Bladder LM may present as irritative symptoms, hematuria, and flank pain. Bladder tumor may cause disorganized contraction of bladder leading to lower urinary tract symptoms. Tumor near ureteral orifice might cause obstruction leading to ureteral colic, flank pain, and obstructive uropathy. There were also a few patients who had no symptoms at all [6].
Bladder LMs have been treated with a variety of modalities; they include transurethral resection, open surgical excision, and minimally invasive methods like laparoscopy and robotic-assisted surgery [6–8]. However, opinions on the best course of action for diagnosis and management are diverse. Furthermore, the majority of the literature on bladder LM therapy consists of case reports and short case series, which makes it challenging to draw definitive conclusions about the features and results of various treatment approaches.
As such, single case reports and small case series are excellent sources for understanding the subtleties of the clinical presentation and therapeutic strategies for this rare illness. To summarize the existing data and offer insights into the characteristics, approaches to treatment, and outcomes related to bladder LMs, a thorough analysis of case reports and case series is necessary. This study aims to better understand the clinical presentation, diagnostic strategy, treatment methods, and results of bladder LMs by methodically locating and examining published cases. This will help guide future research directions and support clinical decision-making.
Method
This systematic review was performed based on Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines and registered on PROSPERO (CRD42024506575).
Eligibility criteria
Research studies may be eligible for inclusion if they explore or document cases of patients diagnosed with bladder LM who underwent surgical management with reported post-management outcomes. The literature should be in the form of a case report or case series. Additionally, letters or correspondences providing information about bladder LM, with adequate details, will also be incorporated to prevent overlooking crucial information on this uncommon occurrence. Reports from the same health center and demographic will be excluded to ensure the avoidance of duplicate patient inclusions. Studies that were not reporting bladder LM or no management data were also excluded. Pediatric cases were also excluded due to the rarity in children. No year of publication was applied for identifying studies, however, only studies published in 2000 and over were included. We only included studies using English or Indonesian.
Search strategy
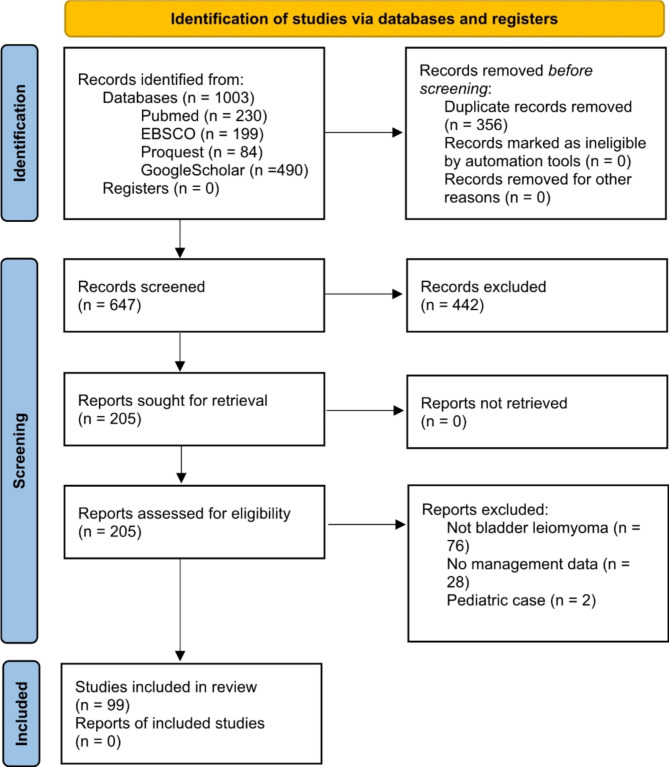
We employed four databases—PubMed, Proquest, EBSCOHost, and Google Scholar to conduct a literature search up to January 2024. Our search utilized the MeSH term (“urinary bladder” AND “leiomyoma”) OR free text word of “bladder leiomyoma” and its word variants (listed in Supplementary File 1). Two authors (AH and SKL) independently screened research titles to exclude studies that did not meet eligibility criteria, and subsequently, selected studies underwent abstract and full-text reviews (Fig. 1). Any disagreements between the two authors were resolved through discussion with a third and fourth author (JCP and SPH).
Fig. 1.
PRISMA flow diagram 2020
Data selection, collection, and extraction
The data were extracted by two independent co‑authors and double‑checked by the third author to ensure the data were matched and organized. The following information was extracted from the selected studies: author, study year, country, study design, duration of follow-up, number of patient(s), age, complaints, diagnostic data, location of the tumor, size of the tumor, presence of comorbidity, management, and outcome of the patient (quality of life, residual symptoms, urodynamic studies, and complications).
Quality assessment
We used The Joanna Briggs Institute (JBI) critical appraisal checklist designed for case series and case reports to assess the quality of the studies.
Results
A total of 1003 studies were retrieved from four databases and screened independently by two co-authors resulting in 99 studies eventually included in this review (Fig. 1) [2, 3, 5–101]. All included cases are shown in Table 1. The total number of patients included in this review is 119 patients, with ages ranging from 22 to 75 years (median 43) (Table 2).
Table 1.
Characteristics of included studies
| Author | Country | Year | Patient No. | Age | Sex | Symptoms | Imaging | Location | Size | Management | Follow-up | LOS | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gaynor-Krupnick, et al. | US | 2004 | 1 | 50 | F | LUTS (storage) | CT, MRI, Cystoscopy, VCUG | Bladder Neck | 3.0 cm (d) | TURBt/TUR | NR | NR | NR |
| Ninan et al. | US | 2005 | 1 | 61 | M | Incidental | CT, Cystoscopy | Ureteric Orifice (right) | 1.0 cm (d) | Cystoscopic enucleation | 6 months | NR | Symptom-free |
| Sawada et al. | Japan | 2005 | 1 | 47 | M | Incidental | CT, MRI, USG, Cystoscopy | Anterolateral Wall (left) | 2.0 × 2.0 cm | TURBt/TUR | 13 months | NR | Symptom-free & no recurrence |
| Chung et al. | Taiwan | 2006 | 1 | 47 | F | LUTS (storage), Hematuria | CT, USG, Cystoscopy | Dome | 5.0 × 3.5 × 3.0 cm | TURBt/TUR, Partial Cystectomy (Laparoscopic)* | NR | 10 days | Persistent symptoms after first procedure, but symptom-free after the second procedure. |
| Lee et al. | Taiwan | 2006 | 1 | 53 | F | Flank Pain, Fever | CT, Cystoscopy, IVP | Not Specified | 8.0 cm (d) | Cystostomy (Open) | 1 month | NR | Symptoms-free & no recurrence |
| Lin et al. | Taiwan | 2006 | 1 | 35 | F | LUTS, Abdominal Pain | CT, MRI, Cystoscopy, VCUG | Anterior Bladder Wall | 8.0 cm (d) | Partial Cystectomy (Open) | 3 months | NR | Small capacity of the bladder (240 mL) with right VUR (grade 2) at 1 month |
| Horton et al. | US | 2007 | 1 | 73 | F | LUTS (storage) | MRI | Dome | 2.6 × 2.3 × 2.1 cm | TURBt/TUR | 1 year | NR | Symptoms-free & no recurrence |
| Metzdorf et al. | US | 2007 | 1 | 59 | F | LUTS (voiding), Abdominal Pain | CT, Cystoscopy | Anterolateral Wall (left) | 3.0 cm (d) | Open Local Excision | NR | NR | NR |
| Bai et al. | South Korea | 2007 | 1 | 55 | F | LUTS | USG | Posterolateral Wall (right) | 4.0 cm (d) | TURBt/TUR | NR | NR | No recurrence |
| Chatzigeorgiou et al. | Germany | 2008 | 1 | 36 | F | LUTS (storage), Flank Pain | CT, USG, Cystoscopy | Lateral Wall (left) | 5.5 × 5.0 × 3.2 cm | Open Local Excision | 3 months | NR | Symptom-free |
| Sudhakar et al. | Bahrain | 2008 | 1 | 45 | F | LUTS | CT, USG, Cystoscopy, IVP | Lateral Wall (left) | 10.0 × 8.0 × 7.0 cm | Partial Cystectomy (Open) | NR | NR | NR |
| Bhuiyan et al. | Malaysia | 2008 | 1 | 30 | F | LUTS, Hematuria | USG, CT | Posterior Floor | NR | Partial Cystectomy (Open) | NR | NR | NR |
| Farouk et al. | Pakistan | 2008 | 1 | 65 | M | LUTS (storage), Hematuria | CT, USG, Cystoscopy, Plain Abdominal X-ray | Lateral Wall (left) | 4.2 × 1.9 cm and 1.7 × 2.2 cm | TURBt/TUR | 3 month | NR | NR |
| Castillo, et al. | Chile | 2008 | 1 | 38 | M | Pelvic Pain | CT | Anterolateral Wall (left) | 2.0 cm (d) | Partial Cystectomy (Laparoscopic) | NR | NR | NR |
| Hong et al. | South Korea | 2009 | 1 | 45 | F | LUTS (storage), Palpable Mass | USG | Dome | 7.0 × 7.0 cm | Laparoscopic Enucleation | 4 months | 3 days | Symptom-free |
| Nazir et al. | India | 2009 | 1 | 30 | F | AUR, LUTS (storage), Hematuria | CT, USG, Cystoscopy | Anterior Bladder Wall | NR | Partial Cystectomy (Laparoscopic) | 1 year | NR | Symptom-free |
| Matsushima et al. | Japan | 2010 | 1 | 56 | F | AUR, LUTS | MRI, USG, Cystoscopy | Bladder Neck | 2.7 cm (d) | TURBt/TUR | 1 week | NR | Symptom-free |
| Sellaturay et al. | UK | 2010 | 1 | 63 | F | AUR, Palpable Mass, AUB, Pelvic Pain | MRI, Cystoscopy | Bladder Neck | 3.0 cm (d) | TURBt/TUR | 18 months | NR | Symptom-free |
| Park et al. | South Korea | 2010 | 1 | 42 | F | Hematuria | CT, USG | Lateral Wall (left) | 5.5 cm (d) | TURBt/TUR | 54 months | NR | Reccurence occurred and follow up TUR performed. |
| South Korea | 2010 | 2 | 41 | F | Incidental | CT, USG | Lateral Wall (left) | 3.0 cm (d) | TURBt/TUR | 7 months | NR | No recurrence | |
| South Korea | 2010 | 3 | 47 | F | LUTS (storage) | CT, USG | Trigone | NA | TURBt/TUR | 77 months | NR | Reccurence and treated with Enucleation. | |
| South Korea | 2010 | 4 | 24 | F | LUTS (storage) | CT, USG | Lateral Wall (left) | 7.0 cm (d) | Partial Cystectomy (Laparoscopic) | 38 month | NR | No recurrence | |
| South Korea | 2010 | 5 | 36 | F | LUTS | CT, USG | Bladder Neck | 3.5 cm (d) | Partial Cystectomy (Laparoscopic) | 39 month | NR | No recurrence | |
| South Korea | 2010 | 6 | 65 | F | Incidental | CT, USG | Anterior Bladder Wall | 4.7 cm (d) | TURBt/TUR | 3 month | NR | No recurrence | |
| South Korea | 2010 | 7 | 53 | F | LUTS | CT, USG | Lateral Wall (right) | 4.0 cm (d) | Transvesical Enucleation (Open) | 3 month | NR | No recurrence | |
| South Korea | 2010 | 8 | 34 | F | Incidental | CT, USG | Lateral Wall (right) | 2.4 cm (d) | TURBt/TUR | 1 month | NR | No recurrence | |
| South Korea | 2010 | 9 | 50 | F | LUTS | CT, USG | Ureteric Orifice (left) | 3.2 cm (d) | TURBt/TUR | 14 month | NR | No recurrence | |
| Paul et al. | India | 2010 | 1 | 22 | F | LUTS | USG, Cystoscopy | Not Specified | 7.0 × 5.3 × 3.0 cm | Open Local Excision | NR | 2 days | NR |
| Singh et al. | India | 2011 | 1 | 35 | F | Hematuria | CT, USG, Cystoscopy | Lateral Wall (left) | 5.0 × 4.5 cm | Laparoscopic Enucleation | 1 year | NR | Symptoms-free & no recurrence |
| Bullock et al. | Jamaica | 2011 | 1 | 42 | F | LUTS (voiding) | CT, MRI, USG | Lateral Wall (left) | 4.0 cm (d)\ | TURBt/TUR | NR | NR | Recurrent urinary tract infection, patient was planned for complete excision |
| Fang et al. | Taiwan | 2011 | 1 | 51 | M | LUTS (storage) | CT, MRI, Cystoscopy, Plain Abdominal X-ray | Lateral Wall (right) | 6.5 × 6.5 × 6.0 cm | TURBt/TUR | NR | NR | Symptom-free |
| Tupikowski et al. | Poland | 2011 | 1 | 29 | F | AUR | MRI, USG, Cystoscopy | Bladder Neck | 4.5 cm (d) | TURBt/TUR | 6 months | 1 day | No recurrence |
| Kaviani et al. | Iran | 2012 | 1 | 46 | F | Palpable Mass, LUTS (storage) | CT, MRI, USG, Cystoscopy | Bladder Neck | 3.0 × 4.0 cm | Partial Cystectomy (Open) | 2 years | 4 days | No recurrence |
| Erdem et al. | Turkey | 2012 | 1 | 49 | F | Incidental | MRI, USG, Cystoscopy | Lateral Wall (left) | 3.0 × 2.5 × 2 cm | TURBt/TUR | NR | NR | NR |
| Ortiz et al. | Colombia | 2012 | 1 | 71 | F | LUTS (storage) | CT, MRI, USG, Cystoscopy | Anterolateral Wall (right) | 4.0 cm (d) | Partial Cystectomy (Laparoscopic) | 1 year | NR | Improved symptoms |
| Barayan et al. | Saudi Arabia | 2012 | 1 | 62 | F | LUTS (storage) | CT, USG, Cystoscopy | Anterior Bladder Wall | 1.7 × 1.1 × 0.8 cm | Cystoscopic Enucleation | 12 months | NR | Persistent urgency which was controlled by oxybutanin 5 mg twice a day |
| Khater et al. | Beirut | 2013 | 1 | 41 | F | Hematuria, Flank Pain, LUTS (storage) | CT, USG | Lateral Wall (left) | 6.0 × 4.2 cm | TURBt/TUR | NR | NR | NR |
| Ghadian et al. | Iran | 2013 | 1 | 42 | F | Hematuria | CT, Cystoscopy | Trigone and Bladder Neck | Multiple tumor weighted 170 g | TURBt/TUR | NR | NR | NR |
| Agrawal et al. | India | 2014 | 1 | 45 | F | AUR, AUB | USG, Cystoscopy | Bladder Neck | 1.4 cm (d) | TURBt/TUR | 6 months | NR | Symptom-free & no recurrence |
| Jain et al. | India | 2014 | 1 | 42 | F | LUTS (storage), Suprapubic Pain | USG, CT, Cystoscopy | Lateral Wall (left) | 6.0 × 4.0 cm | Open Local Excision | 36 months | NR | Symptom-free & no recurrence |
| India | 2014 | 2 | 46 | F | LUTS, Hematuria | CT, MRI, USG, Cystoscopy | Interureteric ridge | 4.0 × 3.0 × 2.0 cm | TURBt/TUR | 6 months | NR | Symptom-free & no recurrence | |
| Musayev et al. | Azerbaijan | 2014 | 1 | 55 | M | Incidental | CT, USG, Cystoscopy | Lateral Wall (left) | 2.0 × 2.5 × 3.0 cm | Partial Cystectomy (Open) | 25 months | 3 days | Symptom-free |
| Chatterjee et al. | India | 2014 | 1 | 35 | F | Dyspareunia, Palpable Mass | CT, USG, Cystoscopy | Posterior Floor | 6.0 × 4.0 cm | Open Local Excision | 12 months | NR | Symptom-free & no recurrence |
| Dewaele et al. | Belgium | 2014 | 1 | 26 | F | LUTS (storage), Palpable Mass | MRI, USG, Cystoscopy | Lateral Wall (right) | 5.0 cm (d) | Transvesical Enucleation (Open) | 15 months | NR | Symptom-free |
| Rosenblatt et al. | Brazil | 2014 | 1 | 60 | F | LUTS (storage), Pelvic Discomfort | CT, MRI, USG, Cystoscopy | Lateral Wall (left) | 4.0 cm (d) | TURBt/TUR | 7 months | 3 days | Symptom-free & no recurrence |
| Vitagliano et al. | Argentina | 2014 | 1 | 30 | F | Incidental | CT, USG | Lateral Wall (right) | 10.1 cm x 4.9 cm | Cystotomy (Laparoscopic) | NR | 2 days | NR |
| Goktug et al. | Turkey | 2014 | 1 | 27 | M | LUTS (storage) | MRI, USG, Cystoscopy | Anterolateral Wall (left) | 7.0 × 8.0 cm | TURBt/TUR | 1 year | 2 days | No reccurences |
| Dere et al. | Turkey | 2015 | 1 | 41 | M | Incidental | CT, Cystoscopy | Anterolateral Wall (left) | 2.5 × 2.0 × 2.0 cm | Open Local Excision | 3 months | NR | Symptom-free |
| Kalathia et al. | India | 2015 | 1 | 55 | F | LUTS (voiding), Palpable Mass, Abdominal Pain | MRI, USG, Cystoscopy, IVP | Lateral Wall (left) | 6.76 × 5.1 cm | TURBt/TUR | 3 months | 1 day | Symptom-free & no recurrence |
| Gungor et al. | Turkey | 2015 | 1 | 26 | M | Premature Ejaculation | CT, USG, Cystoscopy | Dome | 5.4 × 5.0 cm | TURBt/TUR, Partial Cystectomy (Laparoscopic)* | 1 year | 5 days | Residual tumor after 2 months, then undergo Partial Cystectomy. After followup, patient was symptom-free and has no recurence. |
| Yin et al. | China | 2015 | 1 | 22 | F | Abdominal Pain | CT, USG, Cystoscopy | Bladder Neck | 3.2 × 2.5 cm | Transvaginal Resection | 24 months | NR | Symptom-free |
| Mehta et al. | India | 2015 | 1 | 63 | F | AUR | CT, USG, Cystoscopy | Lateral Wall (left) | 4.3 × 4.0 cm | TURBt/TUR | NR | NR | NR |
| India | 2015 | 2 | 43 | F | AUR, Hematuria | CT, USG, Cystoscopy | Cranial Wall | 5.5 × 5.0 cm | TURBt/TUR | NR | NR | NR | |
| Mendes et al. | Portugal | 2016 | 1 | 22 | F | LUTS (storage), Dyspareunia, Pelvic Discomfort | USG, Cystoscopy | Not Specified | 1.6 × 1.1 × 0.6 cm | TURBt/TUR | NR | NR | Symptom-free |
| Itam et al. | UK | 2016 | 1 | 56 | M | AUR, LUTS (voiding), Hematuria and Palpable Mass | CT, MRI, Cystoscopy | Bladder Neck, Trigone | 9.1 cm (d) | Transvesical Enucleation (Open) | 6 weeks | 6 days | Symptom-free & no recurrence |
| Xin et al. | China | 2016 | 1 | 44 | F | Dyspareunia | CT, USG, Cystoscopy | Trigone | 7.3 × 6.1 × 5.8 cm | Open Local Excision | 8 months | 10 days | Symptom-free & no recurrence |
| Haddad et al. | Jordan | 2016 | 1 | 37 | M | LUTS (storage), Fever | CT, USG, Cystoscopy | Lateral Wall (left) | 5.5 × 4.3 cm | TURBt/TUR | 1 year | NR | Symptom-free |
| Caliskan et al. | Turkey | 2017 | 1 | 39 | M | Hematuria | USG, CT, Cystoscopy | Anterior Bladder Wall | 4.8 × 6.2 cm | TURBt/TUR | 6 months | NR | Symptom-free & no recurrence |
| Vijay et al. | India | 2017 | 1 | 53 | F | AUR, LUTS (storage), Hematuria | CT, USG, Cystoscopy | Lateral Wall (left) | 5.0 × 5.0 cm | TURBt/TUR | 6 months | NR | Symptom-free & no recurrence |
| Ameli et al. | Iran | 2017 | 1 | 75 | F | LUTS (storage), Colicky Pain, Flank Pain | CT, USG | Posterior Floor | 4.0 cm (d) | TURBt/TUR | NR | NR | NR |
| Barlotta et al. | US | 2017 | 1 | 31 | M | Purulent drainage from the umbilicus | CT, Cystoscopy | Lateral Wall (left), Dome | 6.5 cm (d) | Cystotomy (Laparoscopic) | 4 months | 7 days | Symptom-free |
| Chaker et al. | Tunisia | 2017 | 1 | 43 | F | Pelvic Pain | MRI, USG | Trigone | 4.3 × 4.7 cm | Transvesical Enucleation (Open) | 14 months | NR | Symptom-free & no recurrence |
| Dodia et al. | India | 2017 | 1 | 35 | F | LUTS (storage), Hematuria, Dysuria | MRI, USG | Lateral Wall (left) | 3.3 × 4.3 cm | Transvesical Enucleation (Open) | NR | NR | NR |
| Gok et al. | Turkey | 2017 | 1 | 46 | F | LUTS | CT, USG, Cystoscopy | Junction between Bladder Neck dan Lateral Wall (left) | 9.0 × 6.0 cm | TURBt/TUR | 6 month | NR | Residual LUTS (storage) after first surgery. All complaints were resolved after second TURBt |
| Zachoval et al. | Czech Republic | 2017 | 1 | 32 | F | Incidental | USG, MRI | Anterior Bladder Wall | 5.0 cm (d) | Open Local Excision | 1 year | NR | Symptom-free & no recurrence |
| Danacioglu et al. | Turkey | 2018 | 1 | 45 | F | LUTS (storage) | CT, MRI, USG | Bladder Neck | 2.5 × 2.0 × 1.5 cm | TURBt/TUR | NR | 5 days | Symptom-free |
| Izzo et al. | Italy | 2018 | 1 | 51 | F | LUTS (storage) | USG, Cystoscopy | Posterior Floor | 1.5 × 2.0 cm | TURBt/TUR | 30 days | NR | Symptom-free |
| Juraski et al. | Brazil | 2018 | 1 | 50 | F | AUR, LUTS | MRI | Anterior Bladder Wall | 3.7 × 3.7 × 3.1 cm | Partial Cystectomy (Laparoscopic) | 45 days | NR | Symptom-free |
| Ahmed et al. | Iraq | 2018 | 1 | 24 | F | LUTS (storage), Hematuria | USG, Cystoscopy, IVP | Ureteric Orifice (left) | 1.5 × 2.5 cm | TURBt/TUR | NR | NR | NR |
| He et al. | China | 2018 | 1 | 47 | F | LUTS (storage) | CT | Posterolateral Wall (left) | 4.0 cm (d) | Partial Cystectomy (Open) | 8 month | NR | Symptom-free |
| Li et al. | China | 2018 | 1 | 34 | F | Incidental | CT, USG,, Cystoscopy | Lateral Wall (left) | 4.0 cm (d) | TURBt/TUR | 30 month | 2 days | No recurrence |
| China | 2018 | 2 | 55 | F | LUTS (storage) | CT, USG,, Cystoscopy | Trigone | 3.3 cm (d) | TURBt/TUR | 21 month | 2 days | No recurrence | |
| China | 2018 | 3 | 54 | F | Hematuria | CT, USG,, Cystoscopy | Trigone | 5.4 cm (d) | TURBt/TUR | 13 month | 2 days | No recurrence | |
| China | 2018 | 4 | 46 | F | LUTS (storage) | CT, USG,, Cystoscopy | Lateral Wall (left) | 6.7 cm (d) | TURBt/TUR | 12 month | 2 days | No recurrence | |
| China | 2018 | 5 | 45 | F | Incidental | CT, USG,, Cystoscopy | Bladder Neck | 2.4 cm (d) | TURBt/TUR | 11 month | 2 days | No recurrence | |
| China | 2018 | 6 | 67 | M | Incidental | CT, USG,, Cystoscopy | Lateral Wall (left) | 1.8 cm (d) | TURBt/TUR | 2 month | 2 days | No recurrence | |
| Jain et al. | India | 2019 | 1 | 32 | F | LUTS (storage) | MRI, USG | Anterior Bladder Wall | 7.0 × 6.0 cm | Open Local Excision | 2 years | 7 days | Symptom-free |
| Kolukcu et al. | Turkey | 2019 | 1 | 41 | M | Hematuria, Muscle pain and fatigue | CT, Cystoscopy | Lateral Wall (left) | 2.0 cm (d) | TURBt/TUR | 2 years | 3 days | No recurrence |
| Mendoza et al. | Philippines | 2019 | 1 | 50 | M | Incidental | CT, USG, Cystoscopy | Lateral Wall (left) | 4.5 × 3.9 × 4.2 cm | Partial Cystectomy (Open) | 1 month | NR | Symptom-free |
| Yoshioka | Japan | 2019 | 1 | 46 | F | Incidental | MRI, USG, Cystoscopy | Lateral Wall (left) | 7.6 × 7.0 cm | Laparoscopic Enucleation | 18 months | 7 days | Residual urinary frequency but decreasing & no recurrence |
| Elhend et al. | Morocco | 2019 | 1 | 32 | M | LUTS (storage), Flank Pain | CT, USG, Cystoscopy | Trigone | 7.0 cm (d) | Transvesical Enucleation (Open) | NR | NR | NR |
| Morroco | 2019 | 2 | 37 | F | Hematuria, LUTS (storage), Pelvic Pain and Palpable Mass | CT, MRI, USG | Lateral Wall (left) | 6.0 cm (d) | Transvesical Enucleation (Open) | NR | NR | NR | |
| Mitchell et al. | US | 2019 | 1 | 64 | M | Hematuria | CT, MRI, Cystoscopy | Ureteric Orifice (left) | 5.0 × 5.0 × 2.5 cm | TURBt/TUR | 6 months | 4 days | Symptom-free with 1.8 cm of residual tumor was noted. |
| Sodo et al. | Italy | 2019 | 1 | 33 | M | LUTS (storage), Pelvic Pain | CT, MRI, USG | Anterior Bladder Wall | 6.0 × 5.0 × 4.0 cm | Partial Cystectomy (Laparoscopic) | 9 months | 7 days | Improved symptoms |
| Kumar et al. | India | 2019 | 1 | 27 | F | LUTS | MRI, USG, Cystoscopy | Bladder Neck | 2.9 × 2.5 × 2.4 cm | TURBt/TUR | 1 year | 3 days | Symptom-free & no recurrence |
| India | 2019 | 2 | 30 | F | AUR, LUTS (voiding) | CT, USG, Cystoscopy | Bladder Neck | 2.7 × 1.6 × 1.7 cm | TURBt/TUR | 1 year | 3 days | Symptom-free & no recurrence | |
| India | 2019 | 3 | 35 | F | AUR, LUTS (voiding) | MRI, USG, Cystoscopy | Bladder Neck | 3.7 × 2.6 × 3.1 cm | TURBt/TUR | 1 year | 3 days | Symptom-free & no recurrence | |
| Delara et al. | US | 2020 | 1 | 33 | F | LUTS (storage), Abdominal Pain, AUB | MRI, Cystoscopy | Ureteric Orifice (left) | 2.0 × 1.3 × 1.7 cm | TURBt/TUR | NR | 0 day | NR |
| Godlewski et al. | Poland | 2020 | 1 | 30 | F | Incidental | USG, CT | Anterior Bladder Wall | 1.5 × 0.5 × 2.5 cm | Cystotomy (Laparoscopic) | 2 months | NR | Symptom-free |
| Poland | 2020 | 2 | 30 | F | Hematuria | CT, USG | Ureteric Orifice (left) | 3.1 × 3.1 × 2.8 cm | Partial Cystectomy (Laparoscopic) | 10 days | NR | NR | |
| Lu et al. | China | 2020 | 1 | 40 | F | LUTS (storage) | MRI, USG, Cystoscopy | Bladder Neck | 4.0 × 3.4 cm | TURBt/TUR | 6 months | NR | No recurrence |
| Mavridis et al. | Greece | 2020 | 1 | 28 | M | Incidental | CT, Cystoscopy | Lateral Wall (left) | 3.3 × 2.7 × 2.2 cm | Open Retropubic Surgical Exploration | NR | NR | NR |
| Pramod et al. | Indonesia | 2020 | 1 | 43 | F | LUTS (storage), Hematuria, Pyuria | CT, USG | Posterior Floor | 7.0 × 6.5 × 4.0 cm | Open transvesical excision | NR | 3 days | NR |
| Valzacchi et al. | Argentina | 2020 | 1 | 45 | F | AUR, LUTS | MRI, USG, Cystoscopy | Bladder Neck | 3.6 × 4.6 cm | Transvesical Laparascopy | 60 months | 2 days | Symptom-free |
| Zachariou et al. | Greece | 2020 | 1 | 52 | M | LUTS, Hematuria | CT, MRI, Cystoscopy | Trigone | 4.1 × 2.4 cm | TURBt/TUR | 12 month | NR | No recurrence |
| Alkharouf et al. | Ireland | 2021 | 1 | 42 | F | LUTS (storage), Hematuria, Dyspareunia | MRI | Trigone | 4.5 cm (d) | Transvaginal Resection | 3 months | 2 days | Symptom-free |
| Asdemir et al. | Turkey | 2021 | 1 | 53 | F | Abdominal Pain | CT, Cystoscopy | Lateral Wall (left) | 2.6 cm x 2.4 cm | TURBt/TUR | NR | 5 days | NR |
| Wei et al. | China | 2021 | 1 | 62 | F | Incidental | CT, MRI, Cystoscopy | Lateral Wall (left) | 2.9 cm × 2.4 cm | Partial Cystectomy (Laparoscopic) | 6 months | NR | Symptom-free & no recurrence |
| Gorgoraptis et al. | Greece | 2021 | 1 | 61 | F | LUTS (storage) | CT, USG | Bladder Neck | 2.7 cm x 3.1 cm | TURBt/TUR | 3 months | 1 day | Symptom-free & no recurrence |
| Tosun et al. | Turkey | 2021 | 1 | 23 | F | Flank Pain, LUTS (storage) | MRI | Lateral Wall (right) | 15.5 cm x 14.5 cm x 14 cm | Partial Cystectomy (Open) | 8 years | 6 days | Symptom-free & no recurrence |
| Al Solumany et al. | Saudi Arabia | 2021 | 1 | 50 | F | Hematuria | CT, MRI | Anterolateral Wall (left) | 7 × 5 × 3.5 cm | TURBt/TUR | 1 year | 8 days | Symptom-free |
| Moawad et al. | UAE | 2021 | 1 | 33 | F | Hematuria, Abdominal Pain | CT, MRI | Bladder Neck | 7.6 × 7 × 6.5 cm | Open Local Excision | 6 months | 2 week | NR |
| Bangash et al. | Pakistan | 2021 | 1 | 52 | F | LUTS, Abdominal Pain | CT, USG | Anterolateral Wall (left) | 3.2 × 1.6 cm | TURBt/TUR, Intravesical Mitomycin-C | 3 Year | 1 day | Residual tumor with size 3 × 2 cm after 6 months. Re-TURBt was performed. After 3 years of follow-up, patient has no recurrence. |
| Pakistan | 2021 | 2 | 42 | F | LUTS, Hematuria | CT, USG, Cystoscopy | Ureteric Orifice (left) | 2.0 × 3.0 cm | TURBt/TUR and Single Dose Intravesical Mitomycin-C, followed by Partial Cystectomy (laparoscopic)* | 3 year | 1 day | Recurrence of tumor after 2 years sizing 2.0 × 3.0 cm. Partial cystectomy was done. After 1 year, patient was symptom-free & has no recurrence | |
| AlHalak et al. | UAE | 2022 | 1 | 24 | F | LUTS (storage) | MRI, USG | Trigone | 4.0 × 2.8 × 3.2 cm | TURBt/TUR | 2 months | NR | Symptom-free & no recurrence |
| Kashkoush et al. | US | 2022 | 1 | 38 | F | AUR, LUTS (voiding), Suprapubic Pain, Nocturia | MRI, USG, Cystoscopy, CT | Bladder Neck | 3.7 × 3.7 × 4.1 cm | TURBt/TUR | 2 year | NR | LUTS (storage) persist after 1 year with recurrent lesion. Re-TUR was performed, however, residual tumor still persist after 1 more year of follow-up. pattient opted out repeat TUR and her symptoms improved. |
| Nazari et al. | Iran | 2022 | 1 | 50 | F | LUTS, Abdominal Pain, AUB | MRI, USG, Cystoscopy | Posterior Floor to Dome | 7.2 × 5.7 cm | Partial Cystectomy (Open), total abdominal hysterectomy (TAH), bilateral salpingo-oophorectomy (BSO) | 1 year | 3 days | Symptom-free & no recurrence |
| Stanescu et al. | UK | 2022 | 1 | 53 | F | LUTS (storage), Hematuria | CT, USG, Cystoscopy | Bladder Neck | 1.5 cm (d) | TURBt/TUR | NR | NR | Symptom-free |
| AlAmri et al. | Saudi Arabia | 2022 | 1 | 34 | M | LUTS | USG, Cystoscopy | Anterolateral Wall (left) | 1.5 × 1.1 cm | TURBt/TUR | 2 weeks | 5 days | Improved symptoms |
| Manoj et al. | India | 2022 | 1 | 27 | F | Flank Pain, Nausea and Vomitting | CT, MRI, USG, Cystoscopy | Anterolateral Wall (right) | 3.3 × 2.0 cm | Partial Cystectomy (Laparoscopic) | 10 days | 5 days | NR |
| Abou-Bieh et al. | Egypt | 2022 | 1 | 32 | F | Hematuria, Suprapubic Pain | MRI | Bladder Neck | Unspecified | TURBt/TUR | NR | NR | NR |
| Victoria et al. | Philippines | 2022 | 1 | 56 | F | Abdominal Pain, Palpable Mass, Weightloss | CT, USG | Cranial Wall | 11.0 × 9.0 × 7.5 cm | Partial Cystectomy (Open) | NR | 7 days | Symptom-free |
| Baird et al. | US | 2022 | 1 | 30 | M | LUTS | CT, Cystoscopy | Ureteric Orifice (left) | 4.1 × 2.9 × 3.4 cm | Transvesical Excision (laparoscopic) | NR | 3 weeks | Symptom-free |
| Jakus et al. | Croatia | 2023 | 1 | 44 | F | Dyspareunia | CT, USG, Cystoscopy | Trigone | 7.3 × 6.1 × 5.8 cm | TURBt/TUR | 8 months | 10 days | Symptom-free |
| Lamy et al. | Saudi Arabia | 2023 | 1 | 36 | F | LUTS (storage), Abdominal Pain | CT, MRI, Cystoscopy | Lateral Wall (left) | 3.0 × 2.0 cm | Partial Cystectomy (Open) | 26 days | 1 day | Urinary frequency and nocturia with negative urine culture |
| Lim et al. | Australia | 2023 | 1 | 41 | F | LUTS (storage), Anteromedial thigh pain | CT, MRI, USG, Cystoscopy | Lateral Wall (left) | 4.4 × 4.2 × 2.8 cm | Open Local Excision | NR | NR | NR |
| Ali et al. | UK | 2023 | 1 | 51 | F | LUTS (storage), Hematuria | CT | Lateral Wall (left) extending to Bladder Neck | 2 × 2.3 × 2 cm | Robotic-Assisted Transvesical Excision | 14 month | 2 weeks | Symptom-free |
| Taniuchi et al. | Japan | 2023 | 1 | 47 | M | Incidental | CT, MRI | Lateral Wall (left) | 8.7 cm (d) | Partial Cystectomy (Laparoscopic) | 1 year | NR | NR |
| Balawender et al. | Poland | 2023 | 1 | 31 | M | Incidental | MRI, USG, Cystoscopy | Lateral Wall (left) | 2.2 × 2.0 cm | Laparoscopic Resection | NR | NR | NR |
F, female; M, male; LUTS, lower urinary tract symptoms; CT, computed tomography; MRI, magnetic resonance imaging; VCUG, voiding cystourethrography; d, diameter; TURBt, transurethral resection of bladder tumor; TUR, transurethral resection; NR, not reported; US, United States; UK, United Kingdom; UAE, United Arab Emirates; USG, ultrasonography; IVP, intravenous pyelography; AUB, abnormal uterine bleeding
*Second procedure
Table 2.
Patient’s characteristics
| Characteristics | Total | Outcome | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Asymptomatic and no recurrence | Symptomatic or recurrence | ||||||||
| N | % | N | % | N | % | ||||
| Total patients | 119 | 100 | 75 | 100 | 15 | 100 | |||
| Age (range, median) | 22 to 75 years, 43 | 6 to 73 years, 45 | 26 to 64, 46 | ||||||
| Sex | |||||||||
| Male | 25 | 21.0 | 17 | 22.7 | 2 | 13.3 | |||
| Female | 94 | 79.0 | 58 | 77.3 | 13 | 86.7 | |||
| Symptoms | |||||||||
| AUR | 14 | 11.8 | 11 | 14.7 | 1 | 6.7 | |||
| LUTS | 71 | 59.7 | 45 | 60.0 | 11 | 73.3 | |||
| LUTS (predominantly Strorage) | 44 | 37.0 | 28 | 37.3 | 5 | 33.3 | |||
| LUTS (predominatly Voiding) | 7 | 5.9 | 4 | 5.3 | 2 | 13.3 | |||
| Hematuria | 29 | 24.4 | 12 | 16.0 | 5 | 33.3 | |||
| Dyspareunia | 5 | 4.2 | 5 | 6.7 | 0 | 0.0 | |||
| Mass | 9 | 7.6 | 8 | 10.7 | 0 | 0.0 | |||
| Abdominal Pain | 11 | 9.2 | 7 | 9.3 | 3 | 20.0 | |||
| Suprapubic Pain | 3 | 2.5 | 1 | 1.3 | 1 | 6.7 | |||
| Flank Pain | 7 | 5.9 | 3 | 4.0 | 0 | 0.0 | |||
| Pelvic pain/discomfort | 7 | 5.9 | 5 | 6.7 | 0 | 0.0 | |||
| AUB | 4 | 3.4 | 3 | 4.0 | 0 | 0.0 | |||
| Incidental (asymptomatic) | 20 | 16.8 | 14 | 18.7 | 1 | 6.7 | |||
| Others (fever, premature ejaculation, purulent drainage, thigh pain, muscle fatique/pain, pyuria, nocturia and weightloss) | 8 | 6.7 | 5 | 6.7 | 2 | 13.3 | |||
| Diagnostic modalities | |||||||||
| CT Scan | 86 | 72.3 | 50 | 67.7 | 14 | 93.3 | |||
| MRI | 48 | 40.3 | 31 | 41.3 | 6 | 40.0 | |||
| USG | 89 | 74.8 | 58 | 77.3 | 11 | 73.3 | |||
| Cystoscopy | 79 | 66.4 | 51 | 68.0 | 10 | 66.7 | |||
| Others (voiding cystourethrography, plain abdominal x-ray, IVP) | 6 | 5.0 | 3 | 4.0 | 1 | 6.7 | |||
| Tumor Location | |||||||||
| Bladder Neck | 21 | 17.6 | 16 | 21.3 | 1 | 6.7 | |||
| Trigone | 10 | 8.4 | 8 | 10.7 | 1 | 6.7 | |||
| Ureteric orifice (right) | 1 | 0.8 | 1 | 1.3 | 0 | 0.0 | |||
| Ureteric orifice (left) | 7 | 5.9 | 2 | 2.7 | 2 | 13.3 | |||
| Interureteric ridge | 1 | 0.8 | 1 | 1.3 | 0 | 0.0 | |||
| Posterior floor | 5 | 4.2 | 2 | 2.7 | 0 | 0.0 | |||
| Anterolateral wall (right) | 2 | 1.7 | 1 | 1.3 | 0 | 0.0 | |||
| Anterolateral wall (left) | 8 | 6.7 | 5 | 6.7 | 1 | 6.7 | |||
| Lateral wall (right) | 6 | 5.0 | 5 | 6.7 | 0 | 0.0 | |||
| Lateral wall (left) | 32 | 26.9 | 16 | 21.3 | 4 | 26.7 | |||
| Posterolateral Wall (right) | 1 | 0.8 | 1 | 1.3 | 0 | 0.0 | |||
| Posterolateral Wall (left) | 1 | 0.8 | 1 | 1.3 | 0 | 0.0 | |||
| Anterior wall | 10 | 8.4 | 8 | 10.7 | 2 | 13.3 | |||
| Dome | 4 | 3.4 | 2 | 2.7 | 2 | 13.3 | |||
| Cranial wall | 2 | 1.7 | 1 | 1.3 | 0 | 0.0 | |||
| Others (junction between bladder neck and left lateral wall, lateral wall and dome, lateral wall and bladder neck, posterior floor to dome, trigone to bladder neck) | 5 | 4.2 | 3 | 4.0 | 2 | 13.3 | |||
| Not specified | 3 | 2.5 | 1 | 1.3 | 0 | 0.0 | |||
| Management (first intervention) | |||||||||
| TURBt/TUR | 62 | 52.1 | 40 | 53.3 | 10 | 66.7 | |||
| Cystoscopic Enucleation | 2 | 1.7 | 1 | 1.3 | 1 | 6.7 | |||
| Open Local Excision | 11 | 9.2 | 7 | 9.2 | 0 | 0.0 | |||
| Transvesical Enucleation (open) | 7 | 5.9 | 4 | 5.3 | 0 | 0.0 | |||
| Transvesical Excision (open) | 1 | 0.8 | 0 | 0.0 | 0 | 0.0 | |||
| Transvesical Excision (laparoscopic) | 1 | 0.8 | 1 | 1.3 | 1 | 6.7 | |||
| Partial Cystectomy (laparoscopic) | 11 | 9.2 | 7 | 9.3 | 0 | 0.0 | |||
| Partial Cystectomy (open) | 11 | 9.2 | 7 | 9.3 | 2 | 13.3 | |||
| Laparoscopic Enucleation | 3 | 2.5 | 2 | 2.7 | 1 | 6.7 | |||
| Laparoscopic Resection | 1 | 0.8 | 0 | 0.0 | 0 | 0.0 | |||
| Cystostomy (open) | 1 | 0.8 | 1 | 1.3 | 0 | 0.0 | |||
| Cystotomy (laparoscopic) | 3 | 2.5 | 2 | 2.7 | 0 | 0.0 | |||
| Transvaginal Resection | 2 | 1.7 | 2 | 2.7 | 0 | 0.0 | |||
| Transvesical Laparoscopy | 1 | 0.8 | 1 | 1.3 | 0 | 0.0 | |||
| Open Retropubic Surgical Exploration | 1 | 0.8 | 1 | 1.3 | 0 | 0.0 | |||
Most of the reported cases were female, which comprised 79.0% of total cases. A total of 16.8% cases were found incidentally (asymptomatic), while in symptomatic patients, most experienced LUTS (59.7%), followed by hematuria (24.4%), acute urinary retention (11.8%), abdominal pain (9.2%), flank pain (5.9%), palpable mass (7.6%), pelvic pain or discomfort (5.9%), and abnormal uterine bleeding (3.4%). The most common type of LUTS experienced by the patients was predominantly storage type (37.0%).
Diagnostic modalities used in these reported cases were combinations of either USG, CT scan, MRI, or cystoscopy. All cases underwent pathology examination to determine the final diagnosis of bladder LM. There is no mismatch between preliminary biopsy and final pathology results. Some studies that did not undergo preliminary biopsy directly conducted excisional surgery for final pathology. Bladder LM is composed of smooth muscle fibers mixed with connective tissue without mitotic activity, cellular atypia, necrosis, or infiltration. Most of the bladder LMs were found on the left lateral wall (26.9%), bladder neck (17.6%), bladder trigone (8.4%), and anterior wall (8.4%), with a wide range of sizes ranging from 1.0 to 18 cm of the longest dimension (median 4.1 cm). More than half of the reported cases were managed by TURBt/TUR (52.1%), followed by partial cystectomy (18.4%), open local excision (9.2%), open transvesical enucleation (5.9%), laparoscopic enucleation (2.5%), and laparoscopic cystostomy (2.5%).
A total of 15 out of 119 cases had a recurrence or remained symptomatic, 75 patients did not have recurrence or symptoms, and the rest 29 patients did not have reported information regarding the final outcome of the management (Table 2). Most were symptomatic at the beginning, only 6.7% were incidental findings and extending to more than one location. Ten out of 15 cases underwent TURBt/TUR (66.7%) and residual tumors were frequently found.
Discussion
The present systematic review synthesized data from 99 studies encompassing 119 patients diagnosed with bladder LM over the past two decades. Our findings highlight several key characteristics and outcomes pertinent to the management of this rare condition. Even if the precise etiology is still unclear, several important processes have been suggested with most research derived from uterine LM studies [102–104]. The intricate interaction of genetic, hormonal, and environmental variables is responsible for the pathogenesis of LM.
Demographics
Our analysis revealed a predominance of female cases, comprising 79% of the total cohort. The age range of affected individuals varied widely, spanning from 22 to 75 years, with a median age of 43 years. It frequently occurs in middle-aged women and rarely in young men. For pediatric cases, yhe youngest cases were from a 1-year-old boy and 6-year old boy [105, 106].
Diagnosis
Notably, a considerable proportion of cases (16.8%) were incidentally detected. Among symptomatic patients, lower urinary tract symptoms (LUTS) were the most commonly reported clinical presentation, affecting 59.7% of cases (Table 2). Urinary retention occurs usually in bladder outlet tumours or large LMs.
It might be difficult to distinguish bladder LMs from bladder cancer for a variety of reasons. Clinical distinction is challenging since both illnesses frequently present identical symptoms, such as hematuria, lower urinary tract symptoms (LUTS), and pelvic pain. Moreover, mass lesions within the bladder in both entities may be detected by radiological imaging techniques, confounding the diagnosis even more. Thus, diagnostic evaluation typically involves a combination of imaging modalities such as ultrasonography (USG), computed tomography (CT) scan, magnetic resonance imaging (MRI), and cystoscopy to ascertain what lesion the clinicians are dealing with. In the end, histological analysis of tissue taken from a biopsy or surgical resection is required for a definite diagnosis of bladder LMs or bladder cancer, highlighting the significance of careful pathological assessment in clinical decision-making. Unlike uterine LM, bladder LM was never reported to transform into malignant leiomyosarcomas [107].
Urinary bladder usually investigated using USG through transabdominal route. On USG, LM usually characterized as having smooth-walled homogenous hypoechoic solid mass with thin echogenic surface [6]. A LM may show up on a CT scan as a homogeneous, pedunculated mass that lacks distinguishing characteristics from other bladder neoplasms. The visual characteristics of bladder LMs on MRI are determined by the presence of collagen and smooth muscle, just like uterine LMs. They often have variable degrees of dynamic enhancement and a uniform T2-hypointense and T1-hypointense look that resembles muscle tissue [108]. Furthermore, they might exhibit a “T2-weighted black-out” effect, which would show up as low signal intensity regions on diffusion-weighted MRI, hypointense areas on high b-value diffusion-weighted MRI, and hyperintense areas on ADC maps. In urothelial carcinoma, it frequently manifests as a strongly enhancing mass with limited dissemination that arises from the wall of the bladder. Non-muscle-invasive urothelial carcinomas are usually present as sessile or flat lesions that are only visible following a cystoscopy as erythema or anomalies of the mucosa. Interestingly, there is usually no thickening or abnormality in the surrounding bladder wall associated with these lesions. On occasion, papillary frond surfaces can show signs of calcification. Leiomyosarcoma typically appears as big, polypoid masses, usually near the bladder dome. It can be difficult to differentiate from a bladder LM since both lesions usually show low signal intensity on T2-weighted MRI. However, characteristics including poorly defined borders, invasion into neighboring structures, and necrotic patches can help differentiate LM from leiomyosarcoma. As with the distinction between leiomyosarcomas and uterine LMs, testing for diffusion limitation can help separate bladder leiomyosarcomas from bladder LMs. The diagnostic accuracy of bladder LM by any imaging modalities is not known due to rarity of cases, however, investigation by Ozden et al., showed that CT has 100% detection rates for bladder tumor larger than 5 mm, while USG has detection rate ranged from 90 to 100% for tumor larger than 5 mm, except for anterior wall region (with detection rate only 60-66.6%) [109]. Tumors with size less than 5 mm also difficult to be detected with USG (0–75% detection rate) or CT (0-66.6% detection rate). Other than diagnosis, USG can be applied to assess if there is invasion to bladder wall. Diffusion-weighted MR can reach sensitivity 95% and specificity 85% for bladder cancer detection [110].
In practice, USG appearance of malignant tumor or any mass-like benign lesions might be similar, it is difficult to differentiate them [111]. At CT, LM is indistinguishable from other bladder neoplasm [108]. Regardless the result of USG, CT, or MRI, whenever bladder tumor is suspected, cystoscopy and biopsy should be conducted as gold standard diagnostics. If bladder mass is found, the differential diagnoses include urothelial carcinoma, malignant mesenchymal mass (such as leiomyosarcoma, lymphoma of bladder, or angiosarcoma), other benign masses (such as paraganglioma, hemangioma, lymphangioma), inflammatory lesions (such as pseudotumor, poplypoid cystitis) [108].
Treatments
To the best of our knowledge, the lack of established studies identifying a superior treatment can be attributed to the rarity of cases and the variability observed among tumors, including variations in size, location, and accessibility [5]. Transurethral resection of bladder tumor (TURBT) is presently utilized as the primary treatment option, owing to its safety and un-eventful procedure, particularly in small, endovesical tumors that are easily accessible [88]. The genesis of TURBT can be traced back to 1806 [112], with subsequent refinement in 1910 by Beer [113], who introduced the utilization of electrocoagulation for the management of bladder tumors. After these historical developments, TURBT has been deemed sufficient for the management of endovesical tumors when performed by experienced operators, following confirmation through imaging modalities [5, 114].
In cases where tumors exhibit larger dimensions or entail extensive involvement of the bladder wall, the consideration of segmental resection via either open surgical or laparoscopic approaches may be done, ensuring comprehensive lesion eradication beyond submucosal levels [5, 48]. Minimally invasive techniques upon segmental resection, including laparoscopic approaches for managing bladder LMs, have been documented as early as 2002 [115]. Moreover, a transvesical method can be used to enhance visualization and manipulation of the lesion. This approach, augmented by the integration of robotic-assisted techniques and guided imaging on occasion, offers advantages such as improved precision and reduced risk of damage to surrounding structures when executed by a trained surgeon [8, 78].
The TURBT procedure exhibits the shortest duration, however, it is imperative to consider the recurrence rate and its constraints regarding the extent of the lesion [88]. The minimum length of stay ranged from a single day to a maximum of eight days among patients undergoing TURBT, while for open surgery, it extended from one day to two weeks, and for laparoscopic approaches, it varied from 10 days to three weeks across the studies included within our analysis. The duration of stay should not be the main concern, more invasive approach is indeed causing the longest hospitalization. Choosing the exact surgery for complete removal is the most important.
Our study presents the first comprehensive systematic review of case reports concerning to LM of the bladder, encompassing a cohort of 99 studies involving 119 patients across 38 countries. Furthermore, it encompasses essential data concerning precise anatomical localization, dimensional measurements, therapeutic modalities, and symptomatic presentations, with detailed consideration of age and gender demographics on a global scale.
In summary, our thorough review offers a significant understanding of the clinical characteristics, approaches to diagnosis, therapeutic strategies, and results of bladder LMs. Our results highlight the large age range of affected individuals, the preponderance of female cases, and the variety of clinical presentations, with lower urinary tract symptoms being the most frequently reported. MRI, CT scan, ultrasonography, and cystoscopy are among the imaging modalities commonly used in diagnostic evaluation. Nonetheless, a significant percentage of individuals have recurrence or persistent symptoms, emphasizing the necessity of ongoing observation and monitoring. Due to overlapping symptoms and radiological features, differentiating bladder LMs from bladder cancer can be difficult, underscoring the significance of histological investigation for conclusive. Our opinions for surgical management are that it should focus on the patient’s condition and tumour’s characteristics. Smaller lesions could be managed by TURBt, while larger lesions might require open surgery if full tumour removal cannot be achieved.
Several limitations are inherent in our study. Firstly, the studies included in our analysis predominantly consist of case reports or case series, rendering them vulnerable to biases, particularly selection and publication bias. Moreover, the typically small patient sizes inherent in these study designs may constrain the reliability and generalizability of the findings to larger populations with controlled variability. Consequently, the interpretation and utilization of our results within reviews necessitate careful consideration.
Conclusion
For an understanding of the best course of treatment and long-term results for bladder LMs, more investigation is necessary. This should primarily take the form of prospective trials with bigger sample sizes and controlled variability. Good sensitivity imaging and pathology examination should be done to exclude leiomyosarcoma. Since there is no standard intervention, management of bladder LM should focus on the relief of symptoms and recurrence and be personalized based on the surgeon’s experience, the patient’s condition, and tumour characteristics.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
JCP: Resources, Supervision; JCP & AH: Conceptualization, Investigation; AH, SKL, SPH: Data Curation, Methodology, Formal Analysis, Project Administration, Validation, Visualization, Software, Writing – Original Draft, Writing – Review & Editing.
Funding
There is no formal funding for this study, all expenses were personally funded by the authors.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jhaveri PN, Makwana SV, Oza KK, Shah C. A histopathological study of urinary bladder neoplasms. Indian J Pathol Oncol. 2021;8(1):59–63. [Google Scholar]
- 2.He L, Li S, Zheng C, Wang C. Rare symptomatic bladder leiomyoma: case report and literature review. J Int Med Res. 2018;46(4):1678–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsushima M, Asakura H, Sakamoto H, Horinaga M, Nakahira Y, Yanaihara H. Leiomyoma of the bladder presenting as acute urinary retention in a female patient: urodynamic analysis of lower urinary tract symptom; a case report. BMC Urol. 2010;10(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsiao CW, Sun GH, Wu ST, Chang SY, Yu DS. Leiomyoma of the bladder causing ureteral outlet obstruction: a case report and review of the literature. J Med Sci. 2000;20(7):377–82. [Google Scholar]
- 5.Khater N, Sakr G. Bladder leiomyoma: presentation, evaluation and treatment. Arab J Urol. 2013;11(1):54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park JW, Jeong BC, Seo SI, Jeon SS, Kwon GY, Lee HM. Leiomyoma of the urinary bladder: a series of nine cases and review of the literature. Urology. 2010;76(6):1425–9. [DOI] [PubMed] [Google Scholar]
- 7.Kalathia J, Agrawal S, Chipde SS, Agrawal R. Total endoscopic management of a large bladder leiomyoma. Urol Ann. 2015;7(4):527–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ali A, Wilby D, Dossantos J, Robinson R. Robotic assisted transvesical excision of recurrent bladder leiomyoma with intraoperative ultrasound guidance. Uro-Technol J. 2023;7(3):26–9. [Google Scholar]
- 9.Gaynor-Krupnick DM, Kreder KJ. Bladder neck leiomyoma presenting as voiding dysfunction. J Urol. 2004;172(1):249–50. [DOI] [PubMed] [Google Scholar]
- 10.Ninan AC, St Luce S, Kimberl IJ, Petros JA, Issa MM. Endoscopic enucleation of leiomyoma of the bladder. Urol Int. 2005;75(1):8–9. [DOI] [PubMed] [Google Scholar]
- 11.Sawada N, Araki I, Ito S, Kudo S, Nakamura K, Takeda M. A case of asymptomatic submucosal-type leiomyoma of the urinary bladder correctly diagnosed with magnetic resonance imaging (MRI) and successfully treated by transurethral resection. Yamanashi Med J. 2005;20(3):65–7. [Google Scholar]
- 12.Chung SD, Tai HC, Chueh SC. Laparoscopic partial cystectomy for a vesical leiomyoma. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(5):565–6. [DOI] [PubMed] [Google Scholar]
- 13.Lee CY, Wang LJ, Chuang KL, Wu KF, Chuang CK. Bladder leiomyoma with right hydronephrosis. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(2):215–7. [DOI] [PubMed] [Google Scholar]
- 14.Lin HC, Wu WJ, Ke HL, Huang CH. Bladder leiomyoma presenting as voiding dysfunction: a case report. Kaohsiung J Med Sci. 2006;22(3):154–7. [DOI] [PubMed] [Google Scholar]
- 15.Horton ES, Dobin SM, Donner LR. Leiomyoma of the urinary bladder: a cytogenetic study of a case. Cancer Genet Cytogenet. 2007;177(2):147–8. [DOI] [PubMed] [Google Scholar]
- 16.Metzdorf MM, Schmidt JD. Urinary bladder leiomyoma associated with pulmonary lymphangioleiomyomatosis. Urology. 2008;71(4):e7553–4. [DOI] [PubMed] [Google Scholar]
- 17.Bai SW, Jung HJ, Jeon MJ, Jung DJ, Kim SK, Kim JW. Leiomyomas of the female urethra and bladder: a report of five cases and review of the literature. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(8):913–7. [DOI] [PubMed] [Google Scholar]
- 18.Chatzigeorgiou K, Burges A, Becker AJ, Friese K. Intramural bladder leiomyoma appearing as a pelvic tumor: a case report. Eur J Obstet Gynecol Reprod Biol. 2008;137(2):254–5. [DOI] [PubMed] [Google Scholar]
- 19.Sudhakar PJ, Malik N, Malik A. Leiomyoma of bladder. Saudi J Kidney Dis Transpl. 2008;19(2):232–5. [PubMed] [Google Scholar]
- 20.Bhuiyan HU. Urinary bladder leiomyoma: a rare case report. Ibrahim Med Coll J. 2008;2(2):70–1. [Google Scholar]
- 21.Farouk K, Gondal M, Ahmad A, Bano U, Khan A. Leiomyoma of the urinary bladder with bladder stone. J Coll Physicians Surg Pak. 2008;18(9):592–4. [PubMed] [Google Scholar]
- 22.Castillo O, Foneron A, Vitagliano G, Sánchez-Salas R, Díaz M, Fajardo M, et al. Bladder leiomyoma: case report. Arch Esp Urol. 2008;61(1):87–91. [DOI] [PubMed] [Google Scholar]
- 23.Hong SY, Lee TS, Kim JH. Laparoscopic enucleation of a bladder leiomyoma. J Minim Invasive Gynecol. 2009;16(6):772–4. [DOI] [PubMed] [Google Scholar]
- 24.Nazir S, Maqbool A, Khan M. Leiomyoma of the urinary bladder-a case report and brief review of literature. Nephro-Urol Mon. 2009;1(1):72–4. [Google Scholar]
- 25.Sellaturay SV, Brown CT, Poulsen J. Leiomyoma of the bladder neck: transurethral resection in a woman to treat bladder outflow obstruction. Br J Med Surg Urol. 2011;4(4):171–3. [Google Scholar]
- 26.P PG, Aggarwal S, Patil A. Bladder leiomyoma mimicking cervical or vaginal myoma. Gynecol Surg. 2011;8(3):377–3779. [Google Scholar]
- 27.Singh O, Gupta SS, Hastir A. Laparoscopic enucleation of leiomyoma of the urinary bladder: a case report and review of the literature. Urol J. 2011 Spring;8(2):155–8. [PubMed]
- 28.Bullock R, Mayhew R, Gibson T, James M, Didier M, Nebhnani J. Leiomyoma: an unusual bladder neoplasm. BMJ Case Rep. 2011;2011:bcr0120113739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fang SM, Hsiao PJ, Lee SH, Chiang HS, Liao CH. Leiomyoma of the urinary bladder: an unusual cause of lower urinary tract symptoms. Incontinence Pelvic Floor Dysfunct. 2011;5(2):51–2. [Google Scholar]
- 30.Tupikowski K, Szewczyk P, Szydełko T, Hałoń A, Polok M, Dembowski J, et al. Management of bladder neck leiomyoma during pregnancy. Cent Eur J Urol. 2011;64(4):260–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaviani A, Razi A, Mokhtarpour H, Mohammad Mohsen Mazloomfard, Moeini A, Bahrami-Motlagh H. Epitheliod leiomyoma of the bladder: an unusual case of irritative and obstructive voiding symptoms. Case Rep Urol. 2012;759150. [DOI] [PMC free article] [PubMed]
- 32.Erdem H, Yildirim U, Tekin A, Kayikci A, Uzunlar A, Sahiner C. Leiomyoma of the urinary bladder in asymptomatic women. Urol Ann. 2012;4(3):172–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ortiz M, Henao DE, Maya WC, Ceballos MM. Leiomyoma of the urinary bladder: a case report. Int Braz J Urol. 2013;39:432–4. [DOI] [PubMed] [Google Scholar]
- 34.Barayan GA, Nassir AM. Cystoscopic enucleation of bladder leiomyoma. Urol Ann. 2012;4(1):38–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ghadian A, Hoseini SY. Transvesical enucleation of multiple leiomyoma of bladder and urethra. Nephro-Urol Mon. 2013;5(1):709–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agrawal SK, Agrawal P, Paliwal S, Yadav C. Bladder neck leiomyoma presenting with acute retention of urine in an elderly female. J Life Health. 2014;5(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jain SK, Tanwar R, Mitra A. Bladder leiomyoma presenting with LUTS and coexisting bladder and uterine leiomyomata: a review of two cases. Rev Urol. 2014;16(1):50–4. [PMC free article] [PubMed] [Google Scholar]
- 38.Musayev JS, Bagirov AM, Hasanov AB, Mammadov E. An asymptomatic intramural leiomyoma of bladder in male patient. Austin J Urol. 2014;1(2):3. [Google Scholar]
- 39.Chatterjee S, Baksi A, Kumar S. Dyspareunia due to leiomyoma of the urinary bladder: an unusual presentation of a rare bladder neoplasm. Hell J Surg. 2014;86(1):34–6. [Google Scholar]
- 40.Dewaele T, D’Hooghe L, Weyers S, Devisschere P. Leiomyoma of the urinary bladder. J Belg Soc Radiol. 2014;97(4):263. [DOI] [PubMed] [Google Scholar]
- 41.Rosenblatt C, Pompeo ACL, Tomé ALF, Lima ASF, Pompeo LBS. Leiomyoma of the bladder. Case report and literature review. Einstein. 2005;3(4):275–7. [Google Scholar]
- 42.Vitagliano G, Castilla R, Long JF. Giant asymptomatic endovesical bladder leiomyoma laparoscopically excised. CRSLS. e2014.00235.
- 43.Goktug GH, Ozturk U, Sener NC, Tuygun C, Bakirtas H, Imamoglu AM. Transurethral resection of a bladder leiomyoma: a case report. Can Urol Assoc J. 2014;8(1–2):E111–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dere Y, Çelik SY, Ilhan Çelik Ö, Deliktas H, Sahin H. Leiomyoma in a very rare location: bladder. Arch Esp Urol. 2015;68(7):585–6. [PubMed] [Google Scholar]
- 45.Güngör R, Onuk Ö, Hazar Ai, Özkan A, Gezmiş C, Nuhoğlu B. Open surgery following endourological treatment in leiomyoma of the bladder: case report. Turk Klin J Urol. 2015;6(2):45–8. [Google Scholar]
- 46.Yin FF, Wang N, Wang YL, Bi XN, Xu XH, Wang YK. Transvaginal resection of a bladder leiomyoma misdiagnosed with a vaginal mass: a case report and literature review. Case Rep Obstet Gynecol. 2015;2015:981843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mehta N, Rathore RS, Bansal D, Babu M, Pillai B. Leiomyoma of urinary bladder presenting as acute urinary obstruction: report of 2 cases. Austin J Urol. 2015;2(4):1035. [Google Scholar]
- 48.Mendes JE, Ferreira AV, Coelho SA, Gil C. Bladder leiomyoma. Urol Ann. 2017;9(3):275–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Itam S, Elhage O, Khan MS. Large leiomyoma of the bladder masquerading as an enlarged prostate gland. BMJ Case Rep. 2016;2016:bcr2015212800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xin J, Lai HP, Lin SK, Zhang QQ, Shao CX, Jin L, et al. Bladder leiomyoma presenting as dyspareunia: case report and literature review. Med (Baltim). 2016;95(28):e3971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Haddad RG, Murshidi MM, Abu Shahin N, Murshidi MM. Leiomyoma of urinary bladder presenting with febrile urinary tract infection: a case report. Int J Surg Case Rep. 2016;27:180–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Caliskan S, Sungur M. Bladder leiomyoma. J Coll Physicians Surg Pak. 2017;27(3):189–90. [PubMed] [Google Scholar]
- 53.Ganapathy VS, Siddappa S, Saini VA, Keshavamurthy R. Bladder leiomyoma - an unusual cause of acute urinary retention. J Cancer Prev Curr Res. 2017;8(4):00287. [Google Scholar]
- 54.Ameli M, Rahmandoost M. Elderly patient with atypical leiomyoma of the bladder presenting as flank pain: a case report. Arch Ital Urol E Androl. 2017;89(4):327–8. [DOI] [PubMed] [Google Scholar]
- 55.Barlotta R, Edwards DC, McGreen B, Levy J, Xia G, Brennan M, et al. Incidental asymptomatic leiomyoma of the urinary bladder. Urology. 2018;113:6–9. [DOI] [PubMed] [Google Scholar]
- 56.Chaker K, Sellami A, Ouanes Y, Zehani A, Dali KM, Abid K, et al. Endovesical leiomyoma of bladder treated by enucleation: a case report. Urol Case Rep. 2018;16:48–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dodia B, Mahajan A, Amlani D, Bathe S. Leiomyoma of urinary bladder in middle-aged female. J Obstet Gynecol India. 2017;67(2):147–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gok A. Transurethral resection of a large urinary bladder leiomyoma: a rare case Report. Urol J. 2017;14(4):4052–4. [PubMed] [Google Scholar]
- 59.Zachoval R, Dukatova K, Svabik K. Vaginal ultrasound for imaging of a urinary bladder mass and treatment of a large leiomyoma of the urinary bladder in pregnancy. Int Urogynecol J. 2018;29(4):601–2. [DOI] [PubMed] [Google Scholar]
- 60.Danacioğlu Yo, Bülent E, Zerk Pe, Güçlüer B, Yildirim A, Çaşkurlu T. Case report: successful resection of a bladder leiomyoma causing lower urinary tract symptoms. New J Urol. 2018;13(1):49–52. [Google Scholar]
- 61.Izzo L, Izzo S, Codacci Pisanelli M, D’Andrea V, Pugliese F, Izzo P. A rare case of leiomyoma of the bladder. Paripex Indian J Res. 2018;7(7):50. [Google Scholar]
- 62.Mattos TA, de Resende S. Bladder outlet obstruction due to bladder leiomyoma–case report and literature review. J Urol Nephrol. 2018;3(3):000143. [Google Scholar]
- 63.Ahmed SA, Al-Shaheen AJ, Khudher ZS. Leiomyoma of the urinary bladder-a case report and review of literature. Ann Coll Med Mosul. 2018;40(2):74–6. [Google Scholar]
- 64.Li A, Zhang P, Zhang M, Yang T, Yue Y, Chen G, et al. Transurethral enucleation of bladder leiomyoma: a series of six cases and review of the literature. Urol Int. 2019;102(1):102–8. [DOI] [PubMed] [Google Scholar]
- 65.Jain S, Dahiya P, Dahiya K, Kamal H, Jain N. Bladder leiomyoma: a diagnostic challenge. J Gynecol Surg. 2019;35(4):276–8. [Google Scholar]
- 66.Kölükçü E, Parlaktaş BS, Deresoy FA, Beyhan M, Özbek LM. Bladder leiomyoma: a case report and brief review of literature. J Surg Med. 2019;3(5):411–4113. [Google Scholar]
- 67.Mendoza JS, Lavadia AD, Lim SL. A rare case of asymptomatic leiomyoma of the urinary bladder. Philipp J Urol. 2019;29(2):73–6. [Google Scholar]
- 68.Yoshioka T, Kawakita M, Kameoka H. Cystoscope-assisted laparoscopic enucleation of a large progressive bladder leiomyoma. J Endourol Case Rep. 2019;5(3):120–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Elhend SB. Leiomyoma of the bladder: case report and literature review. EAS J Radiol Imaging Technol. 2019;1(1):5–8. [Google Scholar]
- 70.Mitchell K, Barnard J, Luchey A. Locally recurrent leiomyoma of the bladder refractory to visually complete transurethral resection: an indication for cystoprostatectomy. Case Rep Urol. 2019;2019:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sodo M, Spirito L, La Rocca R, Bracale U, Imbimbo C. Partial cystectomy in young male for a urachal tumor masquerading a bladder leiomyoma. Arch Ital Urol Androl. 2019;91(1):51–2. [DOI] [PubMed] [Google Scholar]
- 72.Kumar N, Karthik M, Samyuktha K, Palve S, Agrawal T. Leiomyoma of urinary bladder a rare entity: series of 3 cases and review of literature. J Oncol Res. 2019;1(3):7–12. [Google Scholar]
- 73.Delara R, Wasson M, Khan A. Bladder leiomyoma. J Minim Invasive Gynecol. 2021;28(6):1123–4. [DOI] [PubMed] [Google Scholar]
- 74.Godlewski D, Pszczó\lkowski P, Fedus T, Aebisher D. Bladder leiomyoma: diagnostics, laparoscopy, and treatment. Eur J Clin Exp Med. 2020;18(3):237–41. [Google Scholar]
- 75.Lu Y, Sun J, Wang Y. Acute urinary retention with a missed bladder neck leiomyoma. Int Urogynecol J. 2021;32(5):1321–4. [DOI] [PubMed] [Google Scholar]
- 76.Mavridis C, Georgiadis G, Lagoudaki ED, Skamagkas I, Heretis I, Koutsopoulos AV, et al. Bladder leiomyoma with synchronous solitary fibrous tumor of the pleura. Case Rep Urol. 2020;2020:3717506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pramod SV, Safriadi F, Hernowo BS, Dwiyana RF, Ksatriapraja RA. A large bladder leiomyoma. Urol Case Rep. 2020;32:101211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rey Valzacchi GM, Pavan LI, Bourguignon GA, Cortez JP, Ubertazzi EP, Saadi JM. Transvesical laparoscopy for bladder leiomyoma excision: a novel surgical technique. Int Urogynecol J. 2021;32(9):2543–4. [DOI] [PubMed] [Google Scholar]
- 79.Zachariou A, Filiponi M, Dimitriadis F, Kaltsas A, Sofikitis N. Transurethral resection of a bladder trigone leiomyoma: a rare case report. BMC Urol. 2020;20(1):152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Alkharouf F, Abdelrahman M, Salameh FT, Mc Carthy C, Keogh A, Geary M, et al. A bladder leiomyoma masquerading as a vaginal mass causing dyspareunia. A case report and literature review. EGO Eur Gynecol Obstet. 2021;2021/01:44–7. [Google Scholar]
- 81.Asdemir A, Asdemir TY, Saygin H, Korgali E, Cicek R. A 53-year-old female with bladder leiomyoma: a rare case and review of the literature. Ann Clin Anal Med. 2021;12(8):947–50. [Google Scholar]
- 82.Wei MZ, Yan ZJ, Jiang JH, Jia XL. Atypical granular cell tumor of the urinary bladder: A case report. World J Clin Cases. 2021. Oct 6;9(28):8453–8460. [DOI] [PMC free article] [PubMed]
- 83.Gorgoraptis P, Papaioannou D, Kazanis I, Chondros K. Leiomyoma of the bladder neck. Hell Urol. 2021;33(1):24–7. [Google Scholar]
- 84.Tosun ŞA, Sözen H, Tefik T, Iyibozkurt A, Salihoğlu Y. Giant sized extravesical bladder leiomyoma mimicking uterine cervical leiomyoma: a case report with 8 years’postoperative follow-up and a review of the literature. J Istanb Fac Med. 2021;84(3):448–445. [Google Scholar]
- 85.Al Solumany A, Alobairi Y, Abuzenada M, Sulaiman OA, Fatani M. Open partial cystectomy of intramural bladder leiomyoma with unfavorable position: a rare case report. Cureus. 2021;13(1):e12965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Moawad M, Ghashir NB, Rustum Q, Toussi H. Rare case presentation of leiomyoma of bladder neck with tuberculous pelvic lymphadenitis in a young female patient. Urol Case Rep. 2021;34:101436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bangash M, Faruqui N, Muhammad AUI, Uddin Z. Leiomyoma urinary bladder, mimicking urothelial cancer. J Ayub Med Coll Abbottabad JAMC. 2021;33(4):685–9. [PubMed] [Google Scholar]
- 88.AlHalak R, Alkabbani S, Nasseif H, Oghanna N, Janahi F. Bladder leiomyoma treated with transurethral resection of bladder tumor (TURBT): Case report. Int J Surg Case Rep. 2022;98:107464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kashkoush J, Park A. Bladder leiomyoma presenting as urinary retention: a case report. Urol Case Rep. 2022;45:102253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nazari Z, Pirastehfar Z, Torabizadeh Z. Bladder leiomyoma presenting as uterine pedunculated leiomyoma. SAGE Open Med Case Rep. 2022;10:2050313X221111671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Stanescu A, Smith SF, Ball R, Reddy U, Tsiotras A. A case report of bladder leiomyoma: an unusual bladder tumour. J Surg Case Rep. 2022;2022(12):rjac580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.AlAmri N, Abdullah H, AlIbrahim F, Eid K, AlShehri M. Imaging findings of atypical leiomyoma of urinary bladder simulating ureterocele. J Surg Case Rep. 2022;2022(6):rjac256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Manoj S, Joshi AS. Laparoscopic partial cystectomy for leiomyoma of urinary bladder-a case report with review of literature. Radiology. 2022;7(4):D1–3. [Google Scholar]
- 94.Abou-Bieh E, Abd EM. Leiomyoma of the urinary bladder. Eurorad. 2022 [cited 2024 Jan 25]; https://www.eurorad.org/case/9699
- 95.Victoria CMD, Hilvano-Cabungcal AM, Lopez MPJ, Serrano DP. Leiomyoma of the bladder presenting with an ovarian new growth: a case report and review of literature. Philipp J Urol. 2022;32:1. [Google Scholar]
- 96.Baird BA, Ericson CA, Augustus A, Geldmaker L, Wajswol E, Young PR. Robotic transvesical bladder leiomyoma excision. Urol Case Rep. 2022;43:102054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jakus D, Jurić I, Šitum M. Benign urinary bladder masses: rare entities. Afr J Urol. 2023;29(1):48. [Google Scholar]
- 98.Lamy S, Hadidi MF, Alhamami N, Almutairi MA, Qashgry A. A female with urinary bladder leiomyoma: a case report. Cureus. 2023;15(12):e51326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lim KYY, Morkos K, Levy SM, Davis P. Bladder leiomyoma and the utility of 18F-fluorodeoxyglucose-positron emission tomography - a case report. Bladder San Franc Calif. 2023;10:e21200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Taniuchi M, Yanagi M, Kiriyama T, Akatsuka J, Hasegawa H, Mikami H, et al. Primary leiomyoma of the bladder radiologically mimicking a retroperitoneal tumor - a case report. J Med Investig JMI. 2023;70(34):513–5. [DOI] [PubMed] [Google Scholar]
- 101.Balawender K, Wawrzyniak A, Walocha J, Mazur M, Żytkowski A, Wysiadecki G. Leiomyoma: a case of a rare benign mesenchymal neoplasm of the urinary bladder. Pol Arch Intern Med. 2023;133(2):16381. [DOI] [PubMed] [Google Scholar]
- 102.Kim JJ, Sefton EC. The role of progesterone signaling in the pathogenesis of uterine leiomyoma. Mol Cell Endocrinol. 2012;358(2):223–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Arslan AA, Gold LI, Mittal K, Suen TC, Belitskaya-Levy I, Tang MS, et al. Gene expression studies provide clues to the pathogenesis of uterine leiomyoma: new evidence and a systematic review. Hum Reprod. 2005;20(4):852–63. [DOI] [PubMed] [Google Scholar]
- 104.Islam MS, Ciavattini A, Petraglia F, Castellucci M, Ciarmela P. Extracellular matrix in uterine leiomyoma pathogenesis: a potential target for future therapeutics. Hum Reprod Update. 2018;24(1):59–85. [DOI] [PubMed] [Google Scholar]
- 105.Chen H, Niu ZB, Yang Y. Bladder leiomyoma in a 6-year-old boy. Urology. 2012;79(2):434–6. [DOI] [PubMed] [Google Scholar]
- 106.Hanifi AN, Yaseen R, Hameed S, Shams MU, Riaz S, Khan HA. Leiomyoma of the urinary bladder in one Year Old child: a rare. SMU Med J. 2014;1(2):329–35. [Google Scholar]
- 107.Bharambe, Deshpande KA, Surase SG, Ajmera AP. Malignant transformation of leiomyoma of uterus to leiomyosarcoma with metastasis to ovary. J Obstet Gynaecol India. 2014;64:68–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hoegger MJ, Strnad BS, Ballard DH, Siegel CL, Shetty AS, Weimholt RC, et al. Urinary bladder masses, rare subtypes, and masslike lesions: radiologic-pathologic correlation. Radiographics. 2023;43(1):e220034. [DOI] [PubMed] [Google Scholar]
- 109.Ozden E, Turgut AT, Turkolmez K, Resorlu B, Safak M. Effect of bladder carcinoma location on detection rates by ultrasonography and computed tomography. Urology. 2007;69(5):889–92. [DOI] [PubMed] [Google Scholar]
- 110.Zhai N, Wang YH, Zhu LM, Wang JH, Sun XH, Hu XB, et al. Sensitivity and specificity of diffusion-weighted magnetic resonance imaging in diagnosis of bladder cancers. Clin Invest Med. 2015;38(4):E173–84. [DOI] [PubMed] [Google Scholar]
- 111.Bala KG, Chou YH. Ultrasonography of the urinary bladder. J Med Ultrasound. 2010;18(3):105–14. [Google Scholar]
- 112.Engel RME. Philipp Bozzini–the father of endoscopy. J Endourol. 2003;17(10):859–62. [DOI] [PubMed] [Google Scholar]
- 113.Landmark article EB. May 28, 1910: Removal of neoplasms of the urinary bladder. By Edwin Beer. JAMA. 1983;250(10). [PubMed]
- 114.Khaitan A, Seth A, Dinda AK, Singh I, Talwar M, Bandhu S. Transurethral resection versus open surgery for leiomyoma of urinary bladder–a report of 2 cases. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(4):270–3. [DOI] [PubMed] [Google Scholar]
- 115.Jeschke K, Wakonig J, Winzely M, Henning K. Laparoscopic partial cystectomy for leiomyoma of the bladder wall. J Urol. 2002;168(5):2115–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.