Abstract
Background
Physiotherapy is effective to reduce pain and improve the quality of life of people living with chronic pain. To offer high-quality physiotherapy services, these services must be patient-centred and respond to patients’ needs. However, few studies seem to target patients’ perceived needs, whereas more studies tend to focus on needs assessed by healthcare experts, which are not always in line with patients’ perceived needs. In addition, people living with chronic pain are often faced with several health inequities and may have varied perceived needs depending on their personal conditions. To offer services that truly meet patients’ needs, it is therefore crucial to understand these needs. This scoping review aims to identify and map the perceived needs of people living with chronic pain towards physiotherapy services.
Methods
To conduct this review, we followed the six stages framework proposed by Arksey and O’Malley. We searched four databases (Medline, Embase, CINHAL and APA PsycINFO) as well as the grey literature. We included all studies describing the needs, demands, preferences or expectations of adults living with chronic pain towards physiotherapy. We then performed an inductive thematic analysis of the results and discussion sections of these studies to identify the perceived needs. Once those needs were identified, we mapped them into the seven dimensions of the patient-centred healthcare delivery framework.
Results
Our review included 96 studies. Various perceived needs were identified through the thematic analysis, such as the needs for an empathetic relationship; for a clear, adapted and supervised exercise program; and for personalized treatment. Our mapping into the patient-centred healthcare delivery framework showed that most studies reported needs associated with the dimensions of interpersonal care, individualized healthcare and professional care. Needs associated with the other dimensions of the framework (access; coordination and continuity; services and facilities; data and information) were less frequently mentioned.
Conclusions
The results of this review have enabled us to identify and better understand multiple needs perceived by people living with chronic pain regarding physiotherapy services. The perceived needs identified through this scoping review were mapped within the seven dimensions of the Patient-centred healthcare delivery framework.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-11805-3.
Keywords: Perceived needs, Physiotherapy, Chronic pain
Background
Chronic pain affects approximately 20% of the population worldwide [1, 2]. Now recognized as a disease in itself, chronic pain is generally defined as pain lasting longer than the normal expected healing time of tissues (about 3 to 6 months) [3]. Beyond the pain itself, many physical, psychological and social factors are associated with the experience of chronic pain that negatively impact people’s lives [3]. On top of this enormous personal burden, chronic pain generates significant costs for healthcare systems. In 2010, the total yearly cost of pain in the United States ranged from $560 to $635 billion, which is more than the costs of other major diagnoses such as cardiovascular diseases ($309 billion), cancer ($243 billion), and diabetes ($188 billion) [4].
Physiotherapy is among the most frequently used non-pharmacological approaches for chronic pain in the United States [1]. Interventions provided by physiotherapists have been found to be effective in reducing pain intensity and improving the quality of life of people living with chronic pain, among other outcomes [5, 6].
Following recent guidance on patient-centred care [7–9], physiotherapists are encouraged to collaborate with patients and to consider them as unique, while respecting and incorporating their preferences, values and needs in their interventions [10–12]. Despite patients’ needs being a key element to patient-centred care, the term “need” remains a complex and poorly defined term [13–15]. Results of a recent scoping review concluded that studies in the field of rehabilitation, conducted until now, have mainly targeted health related needs based on what was assessed and valued by healthcare representatives and experts, at the expense of needs perceived and expressed by patients [16]. Such attention to the needs evaluated by experts raises many concerns. Focusing on expert-evaluated needs reinforces the presence of a latent paternalism in healthcare frequently decried by many [17]. This paternalism has deleterious effects on patients, thereby limiting their autonomy and freedom to express their own choices and preferences [17]. Moreover, experts’ opinions on the best available interventions are prone to various cognitive biases which can lead to decision-making that dismisses and diverges from patients’ needs [18]. For example, clinicians having sunken cost bias may be tempted to choose an intervention that is not desired by patients, to financially recoup the cost of recently completed training or purchased equipment [18]. Hence, patients’ needs are not always congruent with professionals’ opinions on healthcare needs [19, 20]. In addition to raising ethical issues overlooking the patients’ voice and needs contributes to poor clinical outcomes and low satisfaction with care [21].
Living with chronic pain can be highly challenging. Because chronic pain is invisible and unpredictable [22], people living with this condition often feel misunderstood and stigmatized by healthcare professionals and those around them [23–25]. Their participation in work and social activities can also be greatly affected by their pain [26], and they often end up feeling socially isolated [27]. Moreover, people living with chronic pain often face different types of health inequities [28]. For example, in the United States, non-Caucasian women from lower socio-economic background living in rural areas have been shown to be more prone to have chronic pain [29] and these women’s characteristics were associated with lower use of physiotherapy services in various countries [30]. Several articles also have described the very lengthy and highly limited access to physiotherapy services for people living with chronic pain more generally [31–33]. The multiplicity of challenges faced by people living with chronic pain certainly informs a diversity of perceived needs that are strongly tied to each person’s physical, social, financial, geographical, and psychological condition. Although listening to people living with chronic pain to better respond to their perceived needs is now a prerequisite to offering high quality physiotherapy services, to date, no study has examined the extent and variety of these needs. This scoping review is therefore necessary in order to better identify and understand the diversity of perceived needs of people living with chronic pain with regard to physiotherapy services. Hence, the principal objective of this study was to identify and map the perceived needs of people living with chronic pain towards physiotherapy services.
Methods
The protocol for this scoping review was previously published [34] and registered on Open Science Framework (registration DOI: 10.17605/OSF.IO/6D8P3). Few modifications have been made since this protocol was published. The exact methodology used to carry out this scoping review is reported here.
We followed the six stages framework for conducting a scoping review proposed by Arksey and O’Malley [35] and enhanced by Levac et al. [36], Daudt et al. [37] and Peters et al. [38]. We also used the Preferred Reporting Items for Systematic reviews and Meta-Analysis-extension for Scoping Reviews checklist (PRISMA-ScR) to guide the reporting of the review (see Appendix 1).
Stage 1: identifying the research questions
After consultation with all team members, our primary research question asked: What are the perceived needs of people living with chronic pain towards physiotherapy services? Our secondary research question asked: Where are the gaps in the literature on this topic?
Stage 2: identifying relevant studies
Two librarians helped develop the search strategy. We searched four databases: Medline, Embase, CINHAL and APA PsycINFO (see Appendix 2). No filters were used to limit the results. We also searched the grey literature using Google Scholar, OpenGrey [39] and ProQuest Dissertation & Theses Global (PQDTGlobal) [40]. We then performed a hand search of the reference lists of all the selected full texts to find other relevant references.
All studies presenting or describing the perceived needs of patients with chronic pain towards physiotherapy, regardless of their methodology were included, as well as all studies published in English and French, regardless of their publication date. Conference abstracts were excluded, as they do not provide a sufficient description of patients’ needs in physiotherapy Although reviews were excluded, we examined them to identify and retrieve any studies that had not been previously identified by our search.
Definitions of key terms used in the search strategy
Patient
The term “patient” in this review related to any adult (18 years old or older) who benefited or who could benefit from physiotherapy services. The term included individuals who wanted to consult in physiotherapy, but who were unable to due to accessibility barriers.
Perceived needs
We defined “Perceived needs” as any demands, preferences or expectations from patients towards physiotherapy services, based on their experiences, beliefs and values. We chose this definition because patients’ perceived needs are often associated with patients’ expectations and preferences [41], but there is no established consensus on the definition of the term “needs” regarding physiotherapy or healthcare.
Chronic pain
Based on the 11th edition of the International Classification of Diseases (ICD-11) we defined “chronic pain” as a pain lasting longer than 3 months, accompanied by important emotional distress or physical disability [3, 42]. We included studies that discussed any type of chronic pain (chronic primary pain, chronic cancer pain, chronic postsurgical and posttraumatic pain, chronic neuropathic pain, chronic headache and orofacial pain, chronic visceral pain and chronic musculoskeletal pain) [43] to allow to identify a broad range of needs related to physiotherapy services.
Physiotherapy services
We included articles describing all the services provided by physiotherapists in any type of healthcare setting (e.g., private clinics; rehabilitation centres, community health centre, home care rehabilitation, etc.). We also included descriptions of patients’ needs regarding any type of interventions in physiotherapy (e.g. clinical treatments in a clinic, YouTube videos, wearable technology, etc.) as long as these were delivered by physiotherapists. We included studies discussing healthcare services other than physiotherapy (e.g., occupational therapy, medicine, psychology, etc.), if patients’ perceived needs regarding physiotherapy were also specifically described. However, we excluded studies describing needs related to multiple healthcare services that did not specifically report on physiotherapy services.
Stage 3: study selection
We uploaded all identified articles and sources into Covidence, a software specifically designed to manage the conduct of reviews and their study selection (https://www.covidence.org/home). We removed all duplicates and then screened based on titles and abstracts. Two independent reviewers (JGH and AF) first examined a random sample of 50 references to assess the agreement between them and to ensure that the eligibility criteria were relevant and clearly defined. Following this pilot screening, the same two persons reviewed all remaining titles and abstracts. They recorded all the reasons for exclusion. Any discrepancies between reviewers were resolved through discussion. For the second stage of the screening process (full text review), one of the reviewers of the first stage (JGH) and two other independent reviewers (GJ and RB) assessed the remaining studies. Disagreements were also resolved through discussion. One reviewer (GJ) went through all the reviews (systematic or other types of reviews) identified during our literature search to retrieve all studies included in these reviews and relevant to our review that could have been missed. As we wanted to analyse the full scope of results on the topic and aligned with our research questions, all studies meeting the inclusion criteria were included regardless of their quality. The methodological quality or risk of bias of the included studies was not assessed because the purpose of our review was to identify and map the perceived needs in order to outline the breadth of the literature in this field, rather than to evaluate its rigour and reliability [44–46].
Stage 4: charting the data
Two students (MAC and NL) developed the demographic data extraction sheet using Microsoft Excel (version 16.80). For each study included, the extraction sheet allowed to extract these specific elements: the study characteristics (e.g. title, author’s name, publication date study design, study objectives, etc.), participants’ types of chronic pain (e.g. low back pain, rheumatoid arthritis, knee osteoarthritis, etc.) and the seven dimensions of the “Patient-centred healthcare delivery framework” (see “Stage 5: Collating, summarizing and reporting the results”) discussed in the included studies.
The extraction sheet was then pretested by the same two reviewers (MAC and NL). They extracted the data from two of the included studies using the Excel sheet to ensure the feasibility and quality of the extraction process. In case of disparities, they met to discuss and ensure concordance. They then met with two other reviewers involved in the project (GJ and RB) as well as the first and the senior authors (JGH and AH) to discuss extraction. Minor changes were made to the extraction form.
Following this test, the same four reviewers (GJ, MAC, NL and RB) randomly and equally shared the remaining included articles and extracted their data. Throughout the extraction process, any questions from the reviewers were addressed through discussion or by consulting other members of the team.
Stage 5: collating, summarising and reporting the results
Since the vast majority of the included studies did not explicitly report and name patients’ perceived needs, we first performed an inductive thematic analysis [47] of the included studies. To do this, we imported the text of the results and discussion sections of the included studies into the QDA miner software [48] and used this software to inductively code these sections. Therefore, segments of the text were associated to a code representing a need. This analysis enabled us to generate perceived needs, as defined above, based on the experiences, expectations and preferences mentioned by the participants of the included studies and/or reported by the authors.
For quantitative studies and the quantitative section of the mixed methods studies, we only analysed the ‘textual’ content from the results and discussion sections, notwithstanding the statistical or numerical components of the results. Once these inductive codes were created, we then used a deductive qualitative approach to coding [49] where we mapped the inductive codes representing patients’ perceived needs to the seven dimensions of the “Patient-centred healthcare delivery framework” proposed by Mühlbacher [50]. This framework was developed to help organize healthcare around patients’ needs [50]. Initially known as the ‘Model of Needs Dimensions’ [51], this conceptual framework encompasses seven dimensions deemed relevant by patients and healthcare providers to offer person-centred care. These dimensions are grouped into three different levels of healthcare delivery: individual level, process level and organizational level.
The seven dimensions of the Patient-centred healthcare delivery framework are presented in Table 1.
Table 1.
Patient-centred healthcare delivery framework from Mühlbacher et al. 2015
| Level | Dimensions | |
|---|---|---|
| Individual | 1. Interpersonal Care | This dimension includes all elements of the patient-physiotherapist relationship, such as respect, attentiveness, and shared decision-making. |
| 2. Individualised Healthcare | This dimension involves the use of personalized care interventions based on patient’s needs and context. | |
| Process | 3. Coordination and Continuity | This dimension relates to the long-term planning of care, including the collaboration and transitions among and between health care providers and services. |
| 4. Professional Care | This dimension refers to all aspects of the clinical care, such as patient education, expertise of the healthcare professional and treatment guidelines. | |
| Organizational | 5. Data and Information | This dimension refers to the content and the ways in which health information is shared to patients. It also encompasses elements related to the availability, security and transparency of “patient data”, as well as the availability and quality of performance indicators. |
| 6. Service and Facilities | This dimension refers to the staff within the facilities and to the ‘structural’ aspect of these facilities. More precisely, it includes all aspects related to accessibility and how user-friendly it is, as well as the equipment and furniture inside the facility. The ‘atmosphere’ and ambiance associated within the service are also part of that dimension. | |
| 7. Access | This dimension encompasses both geographical and timely access to services, as well as the costs related to the services. | |
This analysis was performed by four team members (MAC, NL, GJ, RB) supervised by the first author of the review (JGH). A meeting with the first and the senior authors (JGH and AH) was organized after all the reviewers had each analysed five articles to discuss the analysis process.
Stage 6: consultation with stakeholders
Our research team included two women living with chronic pain who previously used physiotherapy services (CC, FL). They were recruited from two different associations of persons living with chronic pain in the province of Quebec, Canada. They were both involved in the development of the research protocol for this scoping review, including the elaboration of the specific objectives and research questions. They also participated in the discussions on the analysis process, including the identification and codification of the perceived needs. Their involvement enabled the rest of the team to better understand the reality and lived experience of people living with chronic pain in physiotherapy. Their opinions enriched reflections and analysis of the results, enabling to better identify the perceived needs arising from patients’ experiences, expectations and preferences reported in the included studies.
Results
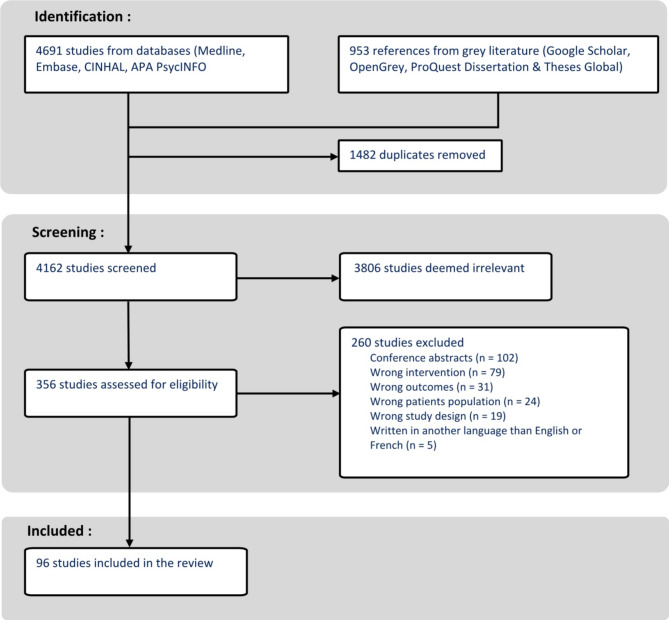
The search in the databases and grey literature resulted in the identification of 5644 studies. After removing duplicates, we screened 4163 studies, of which 96 met the eligibility criteria. These 96 studies where formally included in the final sample and analyzed. Figure 1 shows the detailed study selection flow chart.
Fig. 1.
Study selection flow chart
Characteristics of the included studies
Most of the included studies were recently published: 68 of the 96 were published within the last 10 years and only one study was published before 2000. Studies were mainly from Europe (n = 62), America (n = 17) and Oceania (n = 15). Seventy-seven studies used a qualitative design, 7 a quantitative design, 12 a mixed methods design. Although all studies addressed patients’ experiences in physiotherapy and results aligning with our definition of patient’s perceived needs, only five studies specifically mentioned targeting patient’s needs [52–56]. Most studies included participants living with chronic musculoskeletal pain, including all types of arthritis (n = 78), but some included participants with a diagnosis of fibromyalgia (n = 4), chronic regional pain syndrome (n = 1), vulvodynia (n = 1), multiple sclerosis (n = 1), cancer-related pain (n = 1) and spinal cord injury (n = 1). Five studies included participants with mixed diagnoses and four studies had participants with chronic pain without any other specific diagnosis. Characteristics of all the included studies are available in Appendix 3.
Perceived needs of people living with chronic pain regarding physiotherapy services
Our analysis allowed us to identify the perceived needs of people living with chronic pain towards physiotherapy services and to map them to the seven dimensions of the Patient-centred healthcare delivery framework [50]. Most of the codes (perceived needs) resulting from our analysis were mapped into three of those seven dimensions, which are Interpersonal care, Individualised healthcare and Professional care, whereas less codes were mapped into the four other dimensions (Coordination and continuity; Data and information; Service and facilities and Access).
Each of these seven dimensions are presented in the following sections with the perceived needs identified by our inductive coding analysis. These results are summarized in Table 2.
Table 2.
Seven dimensions of the patient-centred healthcare delivery framework with the corresponding identified perceived needs
| Levels of healthcare delivery | Dimensions | Identified perceived needs for/to |
|---|---|---|
| Individual Level | Interpersonal Care |
• An empathetic relationship [54, 57–83] • Be understood, respected and validated [54, 58, 63, 77, 78, 80, 81, 83–92] • Be considered as full human being in an egalitarian relationship [57, 68, 83, 93–95] • A trusting relationship [56, 57, 61, 64, 68, 70, 72–74, 76, 80, 82, 87, 93, 95–99] • An honest physiotherapist with great communication skills [57, 59, 61, 65, 69, 73, 76, 77, 80, 83, 86, 100] • Support and encouragement [52, 56, 58, 59, 62–64, 66, 67, 69, 74, 77–85, 89, 91–93, 97, 99–112] • Be reassured [52, 56, 57, 61, 67, 69, 72, 76, 77, 84, 85, 87, 97, 100, 106, 110, 113–115] • Collaborate and be actively involved in their rehabilitation [56, 59, 69, 73, 75, 82, 87, 94, 116, 117] |
| Individualised Healthcare |
• An approach that considers their beliefs, expectations and past experiences in physiotherapy [62, 70, 72, 74, 82, 86, 87, 98, 99, 108, 118–120] • An approach that could help them accept their pain [63, 75, 84, 85, 121] • Autonomy and self-management [52, 61–63, 72, 75, 76, 83–86, 89, 91, 93, 100, 105, 113, 122, 123] • Personalized treatment and objectives [52, 54, 56–59, 63, 65–68, 70, 71, 73–75, 77, 79–85, 87, 89, 91, 92, 94, 97–102, 104, 105, 108–112, 115, 117–120, 122–134] • Social support [62–66, 68, 69, 72, 73, 75, 77, 79–81, 85, 86, 89, 91, 92, 94, 96, 99–101, 104–108, 110–113, 118–120, 135, 136] |
|
| Process Level | Coordination and Continuity |
• More physiotherapy treatments and follow-up [52, 56, 64–66, 68–70, 72, 77, 80, 84, 87, 92, 99, 111, 118, 121, 123, 126, 130, 135] • Concordant advice and opinion from health professionals [67, 69, 71, 72, 77, 86, 88, 117, 119, 121, 123, 128, 137] • Continuity in physiotherapy and between healthcare professionals [65, 77, 80, 90, 129] • Well-coordinated services [57, 58, 65, 68, 81, 99, 114, 137–140] • Information to be shared between healthcare professionals [69, 70, 97] |
| Professional Care |
• An expert physiotherapist [54, 56, 57, 63, 65, 70, 72, 73, 76, 78, 82, 84, 86, 87, 91, 105, 109, 112, 114, 123, 125, 126, 139] • A physiotherapist driven by caring intentions [57] • A mindful physiotherapist generous with his time [65, 87, 137, 139] • A proper diagnosis and to know what is “cause of their pain” [52, 56, 58, 61, 67, 70, 81, 85–87, 114, 121, 131, 134, 139] • Education and advice to better understand and manage the pain [52, 53, 56–59, 61–65, 67–73, 75–77, 79–81, 84–87, 89–92, 94, 97–100, 102, 110–112, 114, 115, 117, 119–123, 126, 127, 130, 133, 135–138, 141, 142] • Information on physiotherapy treatments and its possible outcomes [55, 59, 65, 67, 70, 81, 82, 87, 88, 97, 103, 112, 114, 119, 121–123, 126, 128, 143] • A clear, adapted and supervised exercise program [52, 53, 56, 59, 63, 64, 67, 73–77, 79–82, 84, 85, 87, 91, 92, 97–111, 116, 119, 121, 123–125, 127, 129–135, 142, 143] • Regular feedback [71, 72, 74, 98, 102, 109, 110, 120, 125] • Passive intervention such as manual therapy or other analgesic modalities [60, 63, 67, 72, 82, 87, 88, 115, 123, 129, 130, 134, 141, 143] • Information and advice related to psychosocial health [62, 72, 119, 120, 129, 142] • Pain relief and sustainable outcomes from physiotherapy interventions [58, 62–64, 67, 68, 70, 72, 74, 76, 77, 79, 80, 82, 85, 86, 88, 90, 93, 96, 99–105, 107, 110, 111, 114, 115, 118, 120, 134, 135, 137, 138] |
|
| Organizational Level | Data and Information |
• Information on direct access to physiotherapy and reimbursement opportunities [97, 143] • Information on complementary services and on sensitive topics [53, 62, 75, 110, 133] |
| Services and Facilities |
• Simple, convenient and efficient in-clinic services [52, 57, 65, 68, 69, 74, 76, 77, 82, 84, 90, 92, 93, 100, 102, 105, 110, 112, 125, 135] • Easy to use telerehabilitation services and adequate home installations [74, 88, 93, 97, 100–102, 105, 110, 125, 134, 135, 139, 144–146] • Face-to-face appointments [52, 93, 112, 131, 134, 144, 146] • Complementary services and infrastructures [52, 54, 62, 79, 80, 92, 104, 107, 108, 110, 112, 133, 138] |
|
| Access |
• Easy access to nearby physiotherapy services [58, 62, 63, 74, 77, 82, 92, 93, 104, 110, 123, 137–140, 147] • Quick and flexible appointments [52, 58, 62, 65, 68–70, 76, 82, 90, 99, 110, 112, 121, 133, 137, 140] • Low-cost physiotherapy services [54, 55, 58, 69, 72, 74, 80, 82, 88, 97, 100, 103, 111, 112, 117, 122, 123, 130, 134, 135, 137–140, 143, 144] • Transportation, accommodation and being accompanied [68, 79, 137, 140, 144] |
Dimension 1: interpersonal care (individual level)
This dimension relates to elements of the patient-physiotherapist relationship. Sixty-four of the 96 studies reported patients’ perceived needs associated with this dimension of the framework.
One of the frequently discussed needs was the need for participants to establish an empathetic relationship with their physiotherapist [54, 57–83]. Many participants expressed the need to be understood, respected and validated by their therapists throughout their rehabilitation [54, 58, 63, 77, 78, 80, 81, 83–86]. Regardless of their age [87], their condition [83, 88–90], their life experience [81, 84, 91, 92] or their choice of medication [81], they wanted to be respected and recognized as full human beings [83, 93] within an egalitarian relationship [57, 68, 93–95]. Another often evoked need related to the patient-physiotherapist relationship was the need for a therapeutic relationship based on trust [56, 57, 61, 64, 68, 70, 72–74, 76, 80, 82, 88, 93, 94, 96–99]. To foster such an empathetic and trusting relationship, many studies reported the need for the participants to have an honest physiotherapist [57, 73, 76] with great communication skills [59, 61, 65, 69, 73, 76, 77, 80, 83, 86, 100].
The needs to be supported and encouraged [52, 56, 58, 59, 62–64, 66, 67, 69, 74, 77–85, 89, 90, 92, 94, 97, 99–112] and to be reassured by their physiotherapists [52, 56, 57, 61, 67, 69, 72, 76, 77, 84, 85, 88, 97, 100, 106, 110, 113–115] were also commonly found in the included studies. Being reassured helped some participants to better manage their exercises in relation to pain, i.e. to know when to stop or progress their exercises [77], to diminish their fear and to increase their motivation [85, 97, 110].
Finally, in many studies, participants highlighted the need to collaborate and be actively involved in their rehabilitation [56, 59, 69, 73, 75, 82, 88, 95, 116]. Participants were willing to collaborate if they had treatment options to choose from and if their opinion was truly considered by the physiotherapist [56, 117].
Dimension 2: individualized healthcare (individual level)
This dimension includes the personalization of care to respect patients’ context and answer their needs. Seventy-eight studies reported needs related to this dimension.
Many studies highlighted the need for participants to have a physiotherapist that considered their beliefs, expectations and past experiences, as these elements could influence their experience in physiotherapy [62, 70, 72, 74, 82, 86, 88, 98, 99, 108, 118–120]. Some participants also expressed the need to accept their pain and how physiotherapy interventions could help them in this regard [63, 75, 84, 85, 121].
Various studies reported a perceived need for participants to be given or informed of strategies and advice to enhance the self-management of their condition [52, 61–63, 72, 75, 76, 83–86, 89, 92, 94, 100, 105, 113, 122, 123]. Participants in the studies sought empowerment [57, 76, 124], independence [57, 63, 66, 106] self-investment [63, 70, 99, 100, 118, 120], self-accomplishment [102, 104], self-consciousness [84, 86, 93, 96, 109] and control over their life and condition [57, 63, 86, 105, 109]. All these elements contributed to enhance their need for autonomy and self-management.
Moreover, several included studies reported that participants wished to feel unique [54, 57, 58, 66, 69, 71, 74, 100, 125], which made them search for personalized treatments. Indeed, many participants reported that they did not want a one-size-fits-all approach to care [56, 66, 68, 70, 73, 80, 82, 83, 85, 109, 126]. According to participants in several studies, physiotherapy services needed to be adapted to their physical capabilities [57, 65, 68, 71, 74, 111]; their language [57, 97]; their literacy level [100]; their culture [57]; their financial constraints [52]; their employment status [112]; their busy schedule [77, 90, 101, 102, 105, 110, 112, 113, 122]; and their levels of energy [67, 75, 112, 113, 115, 127]. Other participants wanted the length and frequency of the sessions adapted to their preferences [109, 128]. Some studies also discussed the need for participants to be involved throughout the whole process of treatment planning and objectives setting [56, 63, 82, 88, 95, 117, 129]. Few participants specifically asked for meaningful objectives [66, 81, 119], both short and long-term [80], that respected their preferences and limits [57, 68].
In a large amount of studies, participants reported the need to receive personalized exercises [52, 54, 58, 59, 63, 65, 66, 71, 74, 77, 80, 81, 83–85, 88, 89, 92, 95, 97–100, 102, 104, 105, 108–112, 115, 117, 118, 120, 123, 124, 127, 128, 130–135]. More precisely, it was important for the participants to have exercises adapted to their lifestyle [59, 74, 80, 85, 97, 108, 123, 132] and easy to integrate in their daily routine [52, 65, 71, 74, 80, 99, 100, 110, 111, 115, 117, 120, 127]. The complexity [63, 74, 100, 102, 110, 127], pace [95, 105], quantity [110, 124, 134], duration [97, 110, 123, 124], amount of required supervision [80] and level of difficulty [77, 80, 84, 92, 110] were among the most important aspects that needed personalization for the participants. Some also needed exercises that were well-adapted to the variability of their pain [68, 79, 108, 111, 124, 130, 131] and that did not increase their pain [68, 77, 84, 98, 99, 110].
Several studies mentioned the need for participants to be supported by their close ones [63, 69, 72, 75, 77, 80, 81, 86, 89, 100, 105, 108, 110–112, 118] and to participate in exercise and support groups [62, 64–66, 68, 69, 72, 73, 77, 79–81, 85, 89, 90, 92, 95, 96, 99–101, 104–108, 110–113, 119, 120, 136, 137]. Among other things, being in a group was seen as a great source of motivation [62, 64, 66, 69, 80, 81, 92, 96, 104, 105], and allowed them to feel understood and accepted by others [66, 69, 73, 89, 92, 99, 107, 136]. However, some participants preferred individual sessions [65, 79, 80, 112, 136].
Dimension 3: coordination and continuity (process level)
This dimension involves elements related to the long-term planning of care and the collaboration between healthcare professionals. Twenty-nine of the 96 included studies reported perceived needs associated with it.
Several studies highlighted the need for participants to receive more physiotherapy treatments (more frequently, longer sessions and for a longer term) [65, 68–70, 72, 77, 84, 88, 111, 118, 121, 128, 132]. Some participants expressed the need to have a follow-up with their physiotherapist after finishing their episode of care [52, 56, 64, 66, 69, 80, 90, 99, 123, 136].
In numerous studies, participants mentioned their need to receive concordant advice and opinion from the various health professionals consulted [67, 69, 71, 72, 77, 86, 87, 117, 119, 121, 123, 125, 130]. Some participants also perceived a need for continuity among the physiotherapists they consulted, as they wanted to be able to see the same therapist between treatments or episodes [65, 77, 80, 91, 131]. Another frequently reported need was for well-coordinated services, especially to be referred to the right professional at the right time [57, 58, 68, 81, 99, 114, 138]. When possible, patients also liked to see all their healthcare professionals on the same day [68, 125, 139, 140].
In two studies, some participants mentioned the need for the physiotherapists working within the service to have good communication between them and with the administrative staff to ensure the appointments are well organised [65, 139].
Some participants also perceived a need for information related to their medical history, their reasons for consulting in physiotherapy and their medical imagery results between healthcare professionals [69, 70, 97].
Dimension 4: professional care (process level)
This dimension includes all aspects of clinical care such as patient education, expertise of the physiotherapist and interventions used. This dimension was the most discussed among the seven dimensions of the framework, as 87 of the studies presented needs associated with professional care.
A great number of studies reported that participants wished to be treated by an expert and competent physiotherapist [54, 56, 57, 63, 65, 70, 72, 73, 76, 78, 82, 84, 86, 88, 92, 105, 109, 112, 114, 123, 127, 128, 139]. As some studies mentioned, this expertise increases participants’ confidence [65, 76, 78, 112] and gives them a feeling of safety as they feel they are being treated by someone who truly knows what he or she is doing [70, 73, 76, 92, 109, 112].
One study mentioned the importance for participants to have a physiotherapist that is driven by caring intentions, and not by primarily making money or fulfilling requirements for a third party [57]. In addition, few studies raised participants’ need for a mindful therapist [65] that is generous of his or her time to decently answer their questions [88, 125, 139].
Some participants also expressed the need to receive a proper diagnosis [58, 67, 70, 81, 85, 121, 135, 139] and to know what is the “cause of their pain” [56, 61, 88, 98, 133]. This search for a diagnosis also led some participants to perceive the need to undergo medical imagery to be able to “see” their condition and what is problematic in their body [52, 70, 81, 86, 114].
Numerous studies showed that participants needed education [52, 53, 56–59, 61–65, 67, 69–73, 76, 77, 79–81, 84, 85, 89–91, 95, 97–100, 102, 110, 112, 114, 115, 119, 121–123, 125, 128, 129, 132, 137, 138, 141] as well as advice to better understand and manage their pain [52, 58, 61, 65, 67–69, 72, 75, 76, 80, 84–86, 88–92, 95, 100, 110–112, 114, 115, 117, 120, 121, 132, 134, 136, 141, 142]. In several studies, participants also said they wished to receive explanations regarding their treatments and their possible outcomes [55, 59, 65, 67, 70, 81, 87, 88, 97, 112, 114, 119, 121, 123, 128, 130, 143]. Some participants also said they wanted to better understand how physiotherapists can help them compared to other healthcare professionals [82, 103, 122].
The need for participants to have an exercise program was frequently mentioned in the included studies [52, 56, 59, 63, 67, 73, 75, 77, 80–82, 84, 85, 88, 92, 97, 100, 104, 106, 110, 116, 121, 126, 131–133, 135, 142, 143]. When taught the exercises, participants said they liked clear instructions supported by physiotherapist’s demonstrations [59, 63, 64, 67, 74, 76, 77, 80, 84, 89, 90, 100, 103, 107, 110, 123, 124, 127, 133, 134, 136]. They also needed to be supervised [73, 79, 80, 85, 92, 101, 102, 105, 109–111, 119, 124, 127, 134, 136]. As mentioned in some studies, participants needed to receive regular feedback while performing the exercises [71, 74, 102, 109, 110, 120, 127] or to have access to tools to monitor themselves and provide them with feedback, without the physiotherapist being present [72, 98]. Other participants also needed a program to help them to progressively return to their activities, especially if it allowed them to reach short-term goals and to gradually progress their skills [79, 80, 99, 119, 121, 129, 133]. In many studies, participants wanted the exercises to be adapted to their pain level [80, 97, 98, 100, 108, 110, 111, 121, 127, 131, 143].
On the other hand, several participants of the studies mentioned the need to receive passive interventions such as manual therapy [63, 67, 72, 88, 115, 123, 131, 132, 135, 141, 143] or other analgesic modalities like transcutaneous electrical nerve stimulation (TENS) [87], taping [82] and subdermal needling [60].
Other than needs related to their physical wellbeing, some of the studies highlighted the need for participants to receive information and advice regarding their psychological health [72, 119, 131]. To that extend, other participants expressed the need to learn more about mindfulness and/or emotional management techniques to help them accept and live with their pain condition [62, 72, 120, 142].
Finally, several studies highlighted the need for participants to experience pain relief with physiotherapy sessions [58, 62, 67, 68, 70, 72, 74, 76, 79, 80, 82, 85–87, 91, 94, 99–104, 110, 114, 115, 118, 120, 125, 135, 136, 138] or a halt in the deterioration of symptoms [63, 77]. In addition to pain relief, depending on their limitations and conditions, some participants mentioned that they needed to see improvements regarding their balance [63, 96], muscle strength [74, 82, 104, 105, 107], mobility [70, 96, 104, 111], cardiovascular endurance [120] and well-being [64, 87], as well as a decrease in their fear of movement [101]. Improved quality of life, function and return to meaningful activities were also described as desirable outcomes of physiotherapy treatment [94, 102, 111].
Dimension 5: data and information (organizational level)
This dimension refers to the content and the way in which health information is shared to patients. Seven of the included studies addressed perceived needs related to this dimension.
In one study, participants mentioned the need to be informed of direct access in physiotherapy, i.e. access without a medical reference [143], whereas another study reported the need of participants to receive information on reimbursement opportunities for healthcare services such as physiotherapy [97]. In few other included studies, participants expressed the needs to receive information on complementary services, such as aqua gym [62, 134] and on health via online resources such as websites [110] or books [75]. As for sensitive topics such as sexuality, some participants wanted to have access to information to read or watch, such as pamphlets, rather than discussing it directly with their physiotherapist [53].
Dimension 6: services and facilities (organizational level)
This dimension of the Patient-centred healthcare delivery framework includes the structural (physical) aspects of the facilities, the user-friendliness of the services and the helpfulness of the employees. Thirty-eight of the included studies mentioned needs associated with this dimension.
Several of the included studies reported that participants needed simple, convenient and efficient clinic services [57, 65, 68, 69, 76, 82, 84, 91, 94, 105, 110, 136]. Participants wanted to be able to book their appointments online [69, 76, 110] and to be able to easily modify an appointment [65]. Some also appreciated being able to access several healthcare services at the same place [82] and to discuss with the clinic’s administrative staff in order to rapidly book an appointment in the case of an urgent and/or acute situation [69, 110]. To help them remember their appointments, some participants mentioned they wanted to receive reminders [90, 100, 102, 105, 110, 127]. Participants of a few studies also wanted to be able to use phone calls [52, 74, 77, 110, 112] or to send text messaging [77] or emails [77] to reach their physiotherapists when needed. Once arriving at the facility, some participants mentioned that they needed to have easy physical access to the facility where physiotherapy was provided with parking spots [68, 94, 136] or bus stops [68] available close by. Inside the facility, some participants mentioned they appreciated a clean and calm environment [57], with enough space or installations to do their exercises [84, 105], and that provided enough individual resources such as bedsheets to ensure a clean and healthy environment [91].
Several studies reported the need for participants to receive telerehabilitation physiotherapy services [74, 87, 94, 97, 100–102, 105, 110, 127, 135, 136, 139, 144–146], although some preferred to have face-to-face appointments [52, 94, 112, 133, 135, 144, 146]. To take full advantage of telerehabilitation, participants raised the need to have an adequate internet access [94, 135, 146] and a camera [74, 135], as well as to be comfortable using these technologies [94, 101]. They also needed to possess enough space and equipment to properly perform their exercises [87, 97, 100, 102, 105, 110, 127, 135, 136, 146].
To complete prescribed activities or exercises, people living with chronic pain expressed the need to have access to facilities such as gyms, recreational centers and swimming pools [52, 54, 62, 79, 80, 90, 104, 107, 108, 112, 134, 138]. As some gyms could feel intimidating [80], some participants said they could initially need support to get familiarized and increase their confidence to access these facilities [112]. Finally, when using these facilities, participants also perceived the need to be supervised by well trained professionals to select and tailor the exercises to their condition [110, 134].
Dimension 7: access (organizational level)
This last dimension relates to geographical and timely access as well as costs related to the services offered. Forty-four of the included studies reported perceived needs related to access to physiotherapy services.
Many studies mentioned the need for participants to access services close to their home [58, 62, 74, 77, 82, 90, 94, 104, 125, 138–140], to receive home-based physiotherapy services [63, 77, 110, 147] or to have access to outpatient physiotherapy services at the hospital [123]. In addition, some participants also needed to have quick access for physiotherapy services, as they frequently said that they faced long delays and waiting lists to obtain such services [58, 62, 65, 68–70, 110, 121, 125, 140]. Others wanted to get access to physiotherapy services when needed, without the need to consult a doctor first for a reference [52, 76]. Many participants also expressed the need for allowing flexibility in scheduling appointments to better accommodate their lifestyle [62, 69, 70, 76, 82, 91, 99, 112, 134, 140].
Participants of several of the included studies perceived a need for affordable services [54, 58, 72, 82, 100, 103, 111, 112, 117, 122, 125, 135, 136, 138, 140, 144] or services covered by insurances [55, 58, 69, 72, 80, 87, 97, 123, 132, 138, 143]. In this way, some participants expressed the need to reduce the indirect costs related to their physiotherapy appointment, such as a drop in income due to repetitive absences from work [80, 112, 138, 140], babysitting costs [111, 112, 135] or costs related to transportation [74, 125, 135, 139, 140, 144]. To this end, some participants perceived a need for transportation such as public transport, adapted transport (i.e. paratransit) or transport provided by community services to get to their appointment [79, 125, 140, 144]. Others also said they needed to be accompanied to travel to their physiotherapy treatments [68, 79, 125, 140] or to have accommodation because the physiotherapy services were situated too far from their homes, which meant spending a night away [140].
Discussion
To explore the perceived needs of people living with chronic pain towards physiotherapy services, we conducted a scoping review of 96 studies. Most of them were studies of qualitative design and included participants living with chronic musculoskeletal pain.
The use of the patient-centred framework to map the perceived needs identified showed that most studies reported needs associated with the dimensions of interpersonal care and individualized healthcare (both at the Individual Level), as well as professional care (Process Level). Studies mentioning needs related to the dimensions of access (Organizational Level); coordination and continuity (Process Level); or services and facilities (Organizational Level) were less frequent, while very few studies mentioned needs associated with the dimensions of data and information (Organizational Level).
The interpersonal aspect of the care relationship was commonly present in the studies we analyzed. Our results show that participants perceived important needs associated with respect, understanding, empathy, honesty and communication skills of physiotherapists. These results are closely linked to the qualities of a “good” physiotherapist recently identified by Kleiner et al. in an integrative review of 27 qualitative studies [148]. According to their results, patients and physiotherapists consider a “good” physiotherapist to be responsive, ethical, communicative, caring, competent and collaborative [148]. For example, according to the authors, participants defined a “good” physiotherapist as someone who is attentive, a good listener, reassuring, understanding, empathetic, humble, honest and respectful. A “good” physiotherapist must also communicate clearly, foster collaboration and have the appropriate knowledge and practical skills. The authors concluded that “a ‘good’ physiotherapist balances technical competence with a human way of being when interacting with patients” (p.107) [148]. This balance between technical and interpersonal skills is also at the heart of the consensus-based competency profile for pain management recently proposed by a Delphi study involving representatives from Canadian university physiotherapy programs, clinical educators and individuals living with chronic pain [149]. This interesting conclusion shows that patients’ perceived needs toward physiotherapy services and the qualities of a “good” physiotherapist are well-aligned, as the perceived needs identified in our review were mainly mapped into the dimensions of “interpersonal care” and “professional care”.
For people living with chronic pain, the need for a healthy therapeutic relationship, based on listening and empathy, may stem from a perceived lack of understanding on the part of those around them. Indeed, often feeling stigmatized by family, friends and even by some healthcare professionals, people living with chronic pain might seek recognition and empathy from their physiotherapist [25, 81, 150].
Furthermore, many of the perceived needs identified in our review are in line with the findings of recent reviews on patients’ perceptions of healthcare services. In a 2020 overview of reviews on patients’ perceptions regarding their experiences with healthcare services, Chi-Lun-Chiao et al. identified the elements deemed important for people with musculoskeletal disorders [151]. Similar to our results, the authors underlined the importance of communication and interpersonal relationships as patients desired a physiotherapist who understood and respected them and communicated clearly. They also mentioned patients’ expectations to be educated about their condition, to be involved in decision-making surrounding their rehabilitation, and to receive individualized interventions. The participants in the analyzed reviews also considered as important the competencies and technical skills of healthcare providers. Finally, the authors reported various patients’ preferences with regards to the organization of healthcare. For example, they mentioned the need for continuity and coordination of care, as well as the need for access to care and to have flexible appointment times. Although the results of this study and our own show these many similarities, Chi-Lun-Chiao et al. reported elements associated with receiving care in a safe environment and issues about the complexity of paperwork related to healthcare, which were not raised by our review.
Perceived needs related to organizational aspects were less addressed in the studies included in our review. Although some of the studies we analyzed mentioned perceived needs related to access to physiotherapy, we might have expected more studies on the subject, given that unmet needs related to access to healthcare services for people living with chronic pain (including access to physiotherapy) are often discussed in the literature, especially from an experts’ evaluation perspective [152–156]. It is also surprising that few of the included studies mentioned needs related to the physical environment given that several published studies have discussed how such organizational factors can influence patients’ experiences in healthcare [157–163]. Furthermore, some of these organizational factors are directly related to certain perceived needs identified in our review, such as needs concerning communication and interpersonal relationships. In a 2016 systematic review on factors perceived by patients and physiotherapists as influencing their interactions, O’Keeffe et al. [162] mentioned the importance of appointment length and flexibility when booking appointments. Patients appreciated having more time with therapists to talk and were grateful when therapists could adjust the timing of their appointments to suit their needs [162]. In another study, Morera-Balaguer et al. also mentioned how organizational factors such as the lack of coordination between healthcare professionals and a privacy-free environment could affect the therapeutic relationship in physiotherapy [163]. The impact on teamwork and communication of the design of medical facilities was also addressed in Gharaveis et al.’s 2018 systematic review [159]. The results of this review emphasized the impact of aspects of environmental design, such as spatial layout, furnishing, size, space and privacy of rooms, on physicians and nurses’ interactions, as well as communication with patients. The authors also mentioned how room lighting influences interactions in healthcare facilities, as dim lighting resulted in a sensation of calmness for patients and helped facilitate longer conversations. More recently, Zaniboni et al. studied the lighting conditions in physiotherapy facilities and showed that natural day light was associated with higher satisfaction from patients and therapists [160].
Beyond the influence of the environmental design on satisfaction and interactions in healthcare facilities, the environment of physiotherapy services could have some insidious and negative influence on patients’ experiences in physiotherapy. Indeed, some studies explored the influence of physiotherapy services physical environment on power relations between physiotherapists and patients [164, 165]. The authors of these studies argue that the medical look of the décor (e.g. white walls with anatomical posters) and the equipment present in physiotherapy clinics (particularly the treatment bed) suggest a biomedical approach of physiotherapy where the person is reduced to a body and the physiotherapist takes on an expert posture. Thus, as soon as the person enters the waiting room of the physiotherapy clinic, he or she transitions into a potentially “inferior” posture compared to the expert physiotherapist [164]. Such a power imbalance can affect the relationship between physiotherapists and patients, and hinder their collaboration [166]. It might thus be more uncomfortable for patients to express their preferences regarding the organizational elements of healthcare. They may also not see the links between these elements and their lived experience during care. These reasons could potentially explain the lack of perceived needs related to the organizational aspects of physiotherapy services found in the articles included in our review. It is thus essential that more research explores and considers the perceived needs of patients in relation to organizational elements such as environmental design.
Other than the perceived needs identified by our review, an interesting finding is that although meeting patients’ needs are regularly put forward by researchers and healthcare experts, only five of the 96 included studies directly named addressing people’s needs. That is, only five studies explicitly used the term “needs” in the study title or objectives. Although all the other studies revealed elements that enabled us to identify perceived needs according to the definition of such needs retained for the review, these studies used terms such as expectations, preferences, and so on. Moreover, the only study that directly addressed patients’ needs did not provide a definition of what a need is. This may not be surprising because a need is complex and ill-defined.
This finding reinforces existing questions about the use and distinctions between the terms “needs” and “expectations” or “desire”. For some authors, expectations (or wants/demands/desire) and needs should be considered as two different constructs [15, 167, 168]. Expectations seemed more accepted to talk about a person’s demand or desires [168], whereas a need was often linked to a moral obligation to do everything possible to meet it [169]. Therefore, making a distinction between an expectation and a need based on someone’s demand could serve as justifications for physiotherapists and health professionals to attribute less importance to a person’s demand, framing it as a preference or an expectation of that person, and not a need that should be met. However, as Brock [169] illustrated when talking about Internet access, the distinction between a need and a desire is sometimes very thin and can evolve over time. Initially perceived as a desire, the Internet is now more widely accepted in society than ever before and thus, recognized as a need.
Nonetheless, to avoid any confusion or temptation to distinguish an expectation from a need, or more precisely from a perceived need, it is crucial to pursue efforts to more clearly define “perceived needs”. In this respect, Schweighart et al. [170] have recently proposed a definition of “needs and wishes” that could inform what a perceived need should be: “Any desire or craving that the person subjectively feels within him- or herself, whether this is material or immaterial, for change or preservation, already fulfilled or still unfulfilled, realistic or unrealistic, current or future, more or less urgent. The fulfillment of this desire causes a positive effect within the person. This positive effect can be related to the quality of life, satisfaction, self-image, autonomy, and any other aspect of the person’s life.” (p.2). Recognizing that a person’s demands, preferences and expectations can all be defined as a perceived need is certainly a key element for physiotherapists to better recognize and respond to their patients’ needs.
Strengths and limitations
One of the potential challenges of this study concerns the inclusion criteria and keywords used in our research strategy surrounding perceived needs. Since there is no clear and universally accepted definition of the term “perceived needs”, we decided to include interrelated constructs such as demands, preferences and expectations, as described previously. Although this methodological choice may be seen as a limitation of our study, we also believe it can be seen as a strength. Indeed, by including articles dealing with demands, preferences, expectations and lived experiences, we gathered a large sample of studies, the vast majority of which would not have been included if we had only used the keyword “perceived needs”. To this end, we created a comprehensive research strategy with the help of two librarians from two different universities. However, by limiting our research to physiotherapy services, it is likely that some perceived needs, possibly applicable to physiotherapy services but presented in the literature as related to other health services for persons experiencing chronic pain, may have been missed. For example, few needs associated with the multidisciplinary aspect of care were identified by our analysis, even though it is promoted as a key element in rehabilitation for people living with chronic pain [171, 172].
Methodological quality or risk of bias of the studies included was not assessed in our review. This decision aligns with the recommendations for conducting a scoping review [44, 173, 174] and was taken in the light of the fact that our review aims to draw up an exhaustive list of the needs perceived in the literature in order to understand their scope. Consequently, while some perceived needs identified in our review are more frequent than others in the literature, our review does not enable us to draw conclusions about the relative importance of any specific needs.
This review aimed to identify and assess the extent of the perceived needs related to chronic pain, without focusing on specific types of chronic pain, physiotherapy interventions, or geographic regions. As a result, no comparative analysis was conducted.
The active involvement of two patient-partners throughout this review is also a strength of our study. Their input during the analysis process enabled us to ensure the completeness and accuracy of the needs identified and formulated, often based on patients’ preferences or lived experiences described in the included studies. All methodological decisions made during this research were also recorded in a logbook to ensure our entire methodological process was rigorous and transparent.
Conclusion
A better understanding of the perceived needs of people living with chronic pain in regards of physiotherapy services is a key step towards better considering and respecting these needs in physiotherapy. The findings of this review highlight the diverse and heterogeneous nature of perceived needs. Indeed, the perceived needs identified through the scoping review were mapped within the seven dimensions of the Patient-centred healthcare delivery framework. Future research is also needed to obtain a consensus definition of a perceived need, and to explore in more detail patients’ perceived needs with regards to organizational elements of care, such as the physical environment. Finally, although our review targeted the perceived needs related to physiotherapy services for people living with chronic pain, it is likely that some of our findings are relevant to other healthcare services or conditions. Indeed, beyond being treated by a knowledgeable person, what patients say they need is to feel respected, understood and included as full human beings throughout their care.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank Virginie Paquet, librarian at Université de Montréal, and Martine Gagnon, librarian at Université Laval, for their advice concerning our research strategy.
Authors’ contributions
JGH, AF, KP, IG, THW, CC, FL, RB, MAC, GJ, NL and AH contributed to the conception and the design of this review. JGH ran the literature searches. JGH and AF performed the titles and abstracts study selection. RB and GJ did the full-text review. MAC and NL developed the demographic data extraction sheet. RB, MAC, GJ and NL extracted the data and analyzed the included studies. AH and JGH supervised the extraction and analysis processes. AF, KP, IG, THW, CC and FL reviewed and contributed significantly to the interpretation of the results. JGH drafted the manuscript and prepared the tables and figures. AH and KP made substantial revisions. All authors reviewed and approved the submitted version of the manuscript.
Funding
JGH received financial support for the publication of this scoping review from the Quebec Population Health Research Network.
JGH also received doctoral training scholarships from the Canadian Institutes of Health Research, the Fonds de recherche du Québec – Santé, the Faculty of Medicine and the School of Rehabilitation of the Université of Montréal, the Ordre professionnel de la physiothérapie du Québec and the Quebec Rehabilitation Research Network.
AH is supported by a junior 1 career salary award from Fonds de recherche du Québec – Santé (Chercheur-Boursier Junior 1) and startup funds from the Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal (CRIR) and the School of Rehabilitation of the Université of Montréal.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to particpate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yong RJ, Mullins PM, Bhattacharyya N. Prevalence of chronic pain among adults in the United States. Pain. 2022;163(2):e328–32. [DOI] [PubMed] [Google Scholar]
- 2.Harker J, Reid KJ, Bekkering GE, Kellen E, Bala MM, Riemsma R, et al. Epidemiology of chronic pain in Denmark and Sweden. Pain Res Treat. 2012;2012:371248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicholas M, Vlaeyen JWS, Rief W, Barke A, Aziz Q, Benoliel R, et al. The IASP classification of chronic pain for ICD-11: chronic primary pain. Pain. 2019;160(1):28–37. [DOI] [PubMed] [Google Scholar]
- 4.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–24. [DOI] [PubMed] [Google Scholar]
- 5.Rice D, McNair P, Huysmans E, Letzen J, Finan P. Best evidence rehabilitation for chronic pain part 5: osteoarthritis. J Clin Med. 2019;8(11):1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marris D, Theophanous K, Cabezon P, Dunlap Z, Donaldson M. The impact of combining pain education strategies with physical therapy interventions for patients with chronic pain: a systematic review and meta-analysis of randomized controlled trials. Physiother Theory Pract. 2021;37(4):461–72. [DOI] [PubMed] [Google Scholar]
- 7.Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79–86. [DOI] [PubMed] [Google Scholar]
- 8.Cook CE, Denninger T, Lewis J, Diener I, Thigpen C. Providing value-based care as a physiotherapist. Archives Physiotherapy. 2021;11(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Health Canada. An action plan for pain in Canada: Canadian Pain Task Force. 2021. https://www.canada.ca/content/dam/hc-sc/documents/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2021-rapport/report-rapport-2021-eng.pdf. Accessed 24 Nov 2023.
- 10.Birgitte A, Eivind E, David N, Anne Marit M. The singular patient in patient-centred care: physiotherapists’ accounts of treatment of patients with chronic muscle pain. Med Humanit. 2020;46(3):226–33. [DOI] [PubMed] [Google Scholar]
- 11.Naylor J, Killingback C, Green A. What are the views of musculoskeletal physiotherapists and patients on person-centred practice? A systematic review of qualitative studies. Disabil Rehabil. 2023;45(6):950–61. [DOI] [PubMed] [Google Scholar]
- 12.Wijma AJ, Bletterman AN, Clark JR, Vervoort SCJM, Beetsma A, Keizer D, et al. Patient-centeredness in physiotherapy: what does it entail? A systematic review of qualitative studies. Physiother Theory Pract. 2017;33(11):825–40. [DOI] [PubMed] [Google Scholar]
- 13.Asadi-Lari M, Packham C, Gray D. Need for redefining needs. Health Qual Life Outcomes. 2003;1(34):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asadi-Lari M, Tamburini M, Gray D. Patients’ needs, satisfaction, and health related quality of life: towards a comprehensive model. Health Qual Life Outcomes. 2004;2(32):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harrison JD, Young JM, Butow PN, Solomon MJ. Needs in health care: what beast is that? Int J Health Serv. 2013;43(3):567–85. [DOI] [PubMed] [Google Scholar]
- 16.Kamenov K, Mills JA, Chatterji S, Cieza A. Needs and unmet needs for rehabilitation services: a scoping review. Disabil Rehabil. 2019;41(10):1227–37. [DOI] [PubMed] [Google Scholar]
- 17.Filleul A, Drolet M-J, Hudon A. Démasquer Le Paternalisme latent en santé: apports du philosophe Ruwen Ogien. Can J Bioeth / Revue canadienne de bioéthique. 2023;6(2):107–19. [Google Scholar]
- 18.Scott IA, Soon J, Elshaug AG, Lindner R. Countering cognitive biases in minimising low value care. Med J Aust. 2017;206(9):407–11. [DOI] [PubMed] [Google Scholar]
- 19.Kersten P, George S, McLellan L, Smith JA, Mullee MA. Disabled people and professionals differ in their perceptions of rehabilitation needs. J Public Health. 2000;22(3):393–9. [DOI] [PubMed] [Google Scholar]
- 20.Mühlbacher A, Juhnke C. Patient preferences Versus Physicians’ judgement: does it make a difference in Healthcare decision making? Appl Health Econ Health Policy. 2013;11:163–80. [DOI] [PubMed] [Google Scholar]
- 21.Ng JY, Ntoumanis N, Thøgersen-Ntoumani C, Deci EL, Ryan RM, Duda JL, et al. Self-determination theory Applied to Health contexts: a Meta-analysis. Perspect Psychol Sci. 2012;7(4):325–40. [DOI] [PubMed] [Google Scholar]
- 22.Crowe M, Whitehead L, Seaton P, Jordan J, Mccall C, Maskill V, et al. Qualitative meta-synthesis: the experience of chronic pain across conditions. J Adv Nurs. 2017;73(5):1004–16. [DOI] [PubMed] [Google Scholar]
- 23.Wallace B, Varcoe C, Holmes C, Moosa-Mitha M, Moor G, Hudspith M, et al. Towards health equity for people experiencing chronic pain and social marginalization. Int J Equity Health. 2021;20(53):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hadi MA, Alldred DP, Briggs M, Marczewski K, Closs SJ. Treated as a number, not treated as a person’: a qualitative exploration of the perceived barriers to effective pain management of patients with chronic pain. BMJ Open. 2017;7(6):e016454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Synnott A, O’Keeffe M, Bunzli S, Dankaerts W, O’Sullivan P, O’Sullivan K. Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: a systematic review. J Physiotherapy. 2015;61(2):68–76. [DOI] [PubMed] [Google Scholar]
- 26.Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457–67. [DOI] [PMC free article] [PubMed]
- 27.Smith JA, Osborn M. Pain as an assault on the self: an interpretative phenomenological analysis of the psychological impact of chronic benign low back pain. Psychol Health. 2007;22(5):517–34. [Google Scholar]
- 28.Macgregor C, Walumbe J, Tulle E, Seenan C, Blane DN. Intersectionality as a theoretical framework for researching health inequities in chronic pain. Br J Pain. 2023;0(0):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, et al. Prevalence of Chronic Pain and High-Impact Chronic Pain among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(36):1001–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Braaten AD, Hanebuth C, McPherson H, Smallwood D, Kaplan S, Basirico D, et al. Social determinants of health are associated with physical therapy use: a systematic review. Br J Sports Med. 2021;55(22):1293–300. [DOI] [PubMed] [Google Scholar]
- 31.Deslauriers S, Raymond M-H, Laliberté M, Lavoie A, Desmeules F, Feldman DE, et al. Access to publicly funded outpatient physiotherapy services in Quebec: waiting lists and management strategies. Disabil Rehabil. 2017;39(26):2648–56. [DOI] [PubMed] [Google Scholar]
- 32.Fashler SR, Cooper LK, Oosenbrug ED, Burns LC, Razavi S, Goldberg L, et al. Systematic review of multidisciplinary chronic pain treatment facilities. Pain Res Manage. 2016;2016:5960987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hogg MN, Gibson S, Helou A, DeGabriele J, Farrell MJ. Waiting in pain: a systematic investigation into the provision of persistent pain services in Australia. Med J Aust. 2012;196(6):386–90. [DOI] [PubMed] [Google Scholar]
- 34.Gervais-Hupé J, Filleul A, Perreault K, Gaboury I, Wideman TH, Charbonneau C, et al. What are the perceived needs of people living with chronic pain regarding physiotherapy services? A scoping review protocol. PLoS ONE. 2023;18(2):e0274730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 36.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13(48):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2021;19(1):3–10. [DOI] [PubMed] [Google Scholar]
- 39.Data archiving and networked services (DANS). OpenGrey. https://easy.dans.knaw.nl/ui/datasets/id/easy-dataset:200362/tab/2. Accessed 12 July 2022.
- 40.ProQuest. ProQuest Dissertation & Theses Global https://www.proquest.com. Accessed 12 July 2022.
- 41.Papandony MC, Chou L, Seneviwickrama M, Cicuttini FM, Lasserre K, Teichtahl AJ, et al. Patients’ perceived health service needs for osteoarthritis (OA) care: a scoping systematic review. Osteoarthr Cartil. 2017;25(7):1010–25. [DOI] [PubMed] [Google Scholar]
- 42.Perrot S, Cohen M, Barke A, Korwisi B, Rief W, Treede R-D, et al. The IASP classification of chronic pain for ICD-11: chronic secondary musculoskeletal pain. Pain. 2019;160(1):77–82. [DOI] [PubMed] [Google Scholar]
- 43.Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khalil H, Peters MDJ, Tricco AC, Pollock D, Alexander L, McInerney P, et al. Conducting high quality scoping reviews-challenges and solutions. J Clin Epidemiol. 2021;130:156–60. [DOI] [PubMed] [Google Scholar]
- 45.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peters MDJ, Godfrey C, McInerney P, Khalil H, Larsen P, Marnie C, et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI Evid Synth. 2022;20(4):953–68. [DOI] [PubMed]
- 47.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 48.Provalis Research. QDA Miner 2023. https://provalisresearch.com/products/qualitative-data-analysis-software/. Accessed 24 Nov 2023.
- 49.Miles MB, Huberman AM, Saldaña J. Qualitative data analysis: a methods Sourcebook. SAGE; 2020. [Google Scholar]
- 50.Mühlbacher AC, Bethge S. Patients preferences. In: Amelung V, Stein V, Goodwin N, Balicer R, Nolte E, Suter E, editors. Handbook integrated care. Springer; 2021. pp. 39–52. [Google Scholar]
- 51.Juhnke C, Mühlbacher AC. Patient-centredness in integrated healthcare delivery systems - needs, expectations and priorities for organised healthcare systems. Int J Integr Care. 2013;13:e051–e. [PMC free article] [PubMed] [Google Scholar]
- 52.Cooper K, Smith BH, Hancock E. Patients’ perceptions of self-management of chronic low back pain: evidence for enhancing patient education and support. Physiotherapy. 2009;95(1):43–50. [DOI] [PubMed] [Google Scholar]
- 53.Josefsson KA, Gard G. Sexual health in patients with rheumatoid arthritis: experiences, needs and communication with health care professionals. Musculoskelet. 2012;10(2):76–89. [DOI] [PubMed] [Google Scholar]
- 54.Kemp LA. Charting a parallel course: meeting the community service needs of persons with spinal injuries. Ann Arbor: University of Western Sydney (Australia); 1999. [Google Scholar]
- 55.LePage K, Selk A. What do patients want? A needs Assessment of Vulvodynia patients attending a Vulvar diseases Clinic. Sex. 2016;4(4):e242–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stenner R, Swinkels A, Mitchell T, Palmer S. Exercise prescription for non-specific chronic low back pain (NSCLBP): a qualitative study of patients’ experiences of involvement in decision making. Physiotherapy. 2016;102(4):339–44. [DOI] [PubMed] [Google Scholar]
- 57.Bastemeijer CM, van Ewijk JP, Hazelzet JA, Voogt LP. Patient values in physiotherapy practice, a qualitative study. Physiotherapy Res Int. 2021;26(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bath B, Janzen B. Patient and referring health care provider satisfaction with a physiotherapy spinal triage assessment service. J Multidiscip Healthc. 2012;5:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Battista S, Manoni M, Dell’Isola A, Englund M, Palese A, Testa M. Giving an account of patients’ experience: a qualitative study on the care process of hip and knee osteoarthritis. Health Expectations: Int J Public Participation Health care Health Policy. 2022;25:1140–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bibby P. The management of chronic neck pain -- a retrospective survey of the patient journey using in-depth semi-structured interviews. J Orthop Nurs. 2006;10(1):25–32. [Google Scholar]
- 61.Bunzli S, McEvoy S, Dankaerts W, O’Sullivan P, O’Sullivan K. Patient perspectives on participation in cognitive functional therapy for chronic low back Pain. Phys Ther. 2016;96(9):1397–407. [DOI] [PubMed] [Google Scholar]
- 62.Carmona-Teres V, Moix-Queralto J, Pujol-Ribera E, Lumillo-Gutierrez I, Mas X, Batlle-Gualda E, et al. Understanding knee osteoarthritis from the patients’ perspective: a qualitative study. BMC Musculoskelet Disord. 2017;18(1):225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cederbom S, Nortvedt L, Lillekroken D. The perceptions of older adults living with chronic musculoskeletal pain about participating in an intervention based on a behavioral medicine approach to physical therapy. Physiother Theory Pract. 2020;36(10):1118–29. [DOI] [PubMed] [Google Scholar]
- 64.Cook FM, Hassenkamp A-M. Active rehabilitation for chronic low back pain: the patients’ perspective. Physiotherapy. 2000;86(2):61–8. [Google Scholar]
- 65.Cooper K, Smith BH, Hancock E. Patient-centredness in physiotherapy from the perspective of the chronic low back pain patient. Physiotherapy. 2008;94(3):244–52. [Google Scholar]
- 66.Corey JJ, Shirazipour CH, Fricke M, Evans B. Physiotherapists’ role in physical activity promotion: qualitative reflections of patients and providers. Physiother Theory Pract. 2022;9015520:1–13. [DOI] [PubMed] [Google Scholar]
- 67.Feldman R, Nudelman Y, Haleva-Amir S, Ben Ami N. Patients’ prior perceptions and expectations of the enhanced transtheoretical model intervention for chronic low back pain: a qualitative study. Musculoskelet. 2021;20:371–82. [DOI] [PubMed] [Google Scholar]
- 68.Furness PJ, Shelton T, Haywood-Small S, Taylor SJ, Ashe S, Lawson K. A qualitative exploration of experiences of physiotherapy among people with fibromyalgia in the United Kingdom. Pain Rehabil J Physiother Pain Assoc. 2020;2020(48):37–47.
- 69.Goldsmith LJ, Suryaprakash N, Randall E, Shum J, MacDonald V, Sawatzky R, et al. The importance of informational, clinical and personal support in patient experience with total knee replacement: a qualitative investigation. BMC Musculoskelet Disord. 2017;18(1):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hills R, Kitchen S. Satisfaction with outpatient physiotherapy: focus groups to explore the views of patients with acute and chronic musculoskeletal conditions. Physiother Theory Pract. 2007;23(1):1–20. [DOI] [PubMed] [Google Scholar]
- 71.Hinman RS, Delany CM, Campbell PK, Gale J, Bennell KL. Physical therapists, telephone coaches, and patients with knee osteoarthritis: qualitative study about working together to promote exercise adherence. Phys Ther. 2016;96(4):479–93. [DOI] [PubMed] [Google Scholar]
- 72.Holopainen R, Vuoskoski P, Piirainen A, Karppinen J, O’Sullivan P. Patients’ conceptions of undergoing physiotherapy for persistent low back pain delivered in Finnish primary healthcare by physiotherapists who had participated in brief training in cognitive functional therapy. Disabil Rehabil. 2022;44(14):3388–99. [DOI] [PubMed] [Google Scholar]
- 73.Jensen RK, Jakobsen S, Gundersen SV, Andersen MF, Kongsgaard M, Thomsen JL, et al. Patients’ expectations of physiotherapeutic treatment for long-term side effects after cancer: a qualitative study. Cancer Control. 2021;28:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lawford BJ, Delany C, Bennell KL, Hinman RS. "I was really sceptical...But it worked really well": a qualitative study of patient perceptions of telephone-delivered exercise therapy by physiotherapists for people with knee osteoarthritis. Osteoarthritis and cartilage. 2018;26(6):741−50 [DOI] [PubMed]
- 75.May S. Patients’ attitudes and beliefs about back pain and its management after physiotherapy for low back pain. Physiotherapy Res Int. 2007;12(3):126–35. [DOI] [PubMed] [Google Scholar]
- 76.May S. Part 2: an explorative, qualitative study into patient’s satisfaction with physiotherapy. Physiotherapy. 2001;87(1):10–20. [Google Scholar]
- 77.Moore AJ, Holden MA, Foster NE, Jinks C. Therapeutic alliance facilitates adherence to physiotherapy-led exercise and physical activity for older adults with knee pain: a longitudinal qualitative study. J Physiotherapy (Elsevier). 2020;66(1):45–53. [DOI] [PubMed] [Google Scholar]
- 78.Øien AM, Steihaug S, Iversen S, Råheim M. Communication as negotiation processes in long-term physiotherapy: a qualitative study. Scand J Caring Sci. 2011;25(1):53–61. [DOI] [PubMed] [Google Scholar]
- 79.Petursdottir U, Arnadottir SA, Halldorsdottir S. Facilitators and barriers to exercising among people with osteoarthritis: a phenomenological study. Phys Ther. 2010;90(7):1014–25. [DOI] [PubMed] [Google Scholar]
- 80.Slade SC, Molloy E, Keating JL. People with non-specific chronic low back pain who have participated in exercise programs have preferences about exercise: a qualitative study. Aust J Physiother. 2009;55(2):115–21. [DOI] [PubMed] [Google Scholar]
- 81.Slade SC, Molloy E, Keating JL. Stigma experienced by people with nonspecific chronic low back pain: a qualitative study. Pain Med (Malden Mass). 2009;10(1):143–54. [DOI] [PubMed] [Google Scholar]
- 82.Teo PL, Bennell KL, Lawford B, Egerton T, Dziedzic K, Hinman RS. Patient experiences with physiotherapy for knee osteoarthritis in Australia-a qualitative study. BMJ open. 2021;11(3):e043689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Thorne S, McGuinness L, McPherson G, Con A, Cunningham M, Harris SR. Health care communication issues in fibromyalgia: an interpretive description. Physiotherapy Can. 2004;56(1):31–8. [DOI] [PubMed] [Google Scholar]
- 84.Calner T, Isaksson G, Michaelson P. Physiotherapy treatment experiences of persons with persistent musculoskeletal pain: a qualitative study. Physiother Theory Pract. 2021;37(1):28–37. [DOI] [PubMed] [Google Scholar]
- 85.Liddle SD, Baxter GD, Gracey JH. Chronic low back pain: patients’ experiences, opinions and expectations for clinical management. Disabil Rehabil. 2007;29(24):1899–909. [DOI] [PubMed] [Google Scholar]
- 86.Wijma AJ, Speksnijder CM, Crom-Ottens AF, Knulst-Verlaan JMC, Keizer D, Nijs J, et al. What is important in transdisciplinary pain neuroscience education? A qualitative study. Disabil Rehabil. 2018;40(18):2181–91. [DOI] [PubMed] [Google Scholar]
- 87.Davis GC, Hiemenz ML, White TL. Barriers to managing chronic pain of older adults with arthritis. J Nurs Scholarsh. 2002;34(2):121–6. [DOI] [PubMed] [Google Scholar]
- 88.Calner T, Isaksson G, Michaelson P. I know what I want but I’m not sure how to get it-expectations of physiotherapy treatment of persons with persistent pain. Physiother Theory Pract. 2017;33(3):198–205. [DOI] [PubMed] [Google Scholar]
- 89.Joyce C, Keysor J, Stevans J, Ready K, Roseen EJ, Saper RB. Beyond the pain: a qualitative study exploring the physical therapy experience in patients with chronic low back pain. Physiother Theory Pract. 2022;9015520:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Swardh E, Nordgren B, Opava CH, Demmelmaier I. A necessary investment in future health: perceptions of physical activity maintenance among people with rheumatoid arthritis. Phys Ther. 2020;100(12):2144–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Odole AC, Ayodeji A, Adolo B, Alumona CJ, Adandom H, Mbada CE et al. Patients’ satisfaction with physiotherapy management of chronic mechanical neck pain in physiotherapy departments of public hospitals in Ibadan, Nigeria: A mixed-method study. Physiother Theory Pract. 2023;39(9):1896–905. [DOI] [PubMed]
- 92.Swardh E, Biguet G, Opava CH. Views on exercise maintenance: variations among patients with rheumatoid arthritis. Phys Ther. 2008;88(9):1049–60. [DOI] [PubMed] [Google Scholar]
- 93.Wilson S, Chaloner N, Osborn M, Gauntlett-Gilbert J. Psychologically informed physiotherapy for chronic pain: patient experiences of treatment and therapeutic process. Physiotherapy. 2017;103(1):98–105. [DOI] [PubMed] [Google Scholar]
- 94.Hinman RS, Nelligan RK, Bennell KL, Delany C. Sounds a bit crazy, but it was almost more personal: a qualitative study of patient and clinician experiences of physical therapist-prescribed exercise for knee osteoarthritis via skype. Arthritis Care Res (Hoboken). 2017;69(12):1834–44. [DOI] [PubMed] [Google Scholar]
- 95.Martensson L, Dahlin-Ivanoff S. Experiences of a primary health care rehabilitation programme. A focus group study of persons with chronic pain. Disabil Rehabil. 2006;28(16):985–95. [DOI] [PubMed] [Google Scholar]
- 96.Bravo CPPT, Skjaerven LHMPT, Guitard Sein-Echaluce LPNR, Catalan-Matamoros DPTMPHMBAP. Experiences from group basic body awareness therapy by patients suffering from fibromyalgia: a qualitative study. Physiother Theory Pract. 2020;36(8):933–45. [DOI] [PubMed] [Google Scholar]
- 97.Spitaels D, Vankrunkelsven P, Desfosses J, Luyten F, Verschueren S, Van Assche D, et al. Barriers for guideline adherence in knee osteoarthritis care: a qualitative study from the patients’ perspective. J Eval Clin Pract. 2017;23(1):165–72. [DOI] [PubMed] [Google Scholar]
- 98.Stephens G, O’Neill S, Mottershead C, Hawthorn C, Yeowell G, Littlewood C. It’s just like a needle going into my hip, basically all of the time. The experiences and perceptions of patients with Greater Trochanteric Pain syndrome in the UK National Health Service. Musculoskelet Sci Pract. 2020;47(101692753):102175. [DOI] [PubMed] [Google Scholar]
- 99.Willett M, Greig C, Fenton S, Rogers D, Duda J, Rushton A. Utilising the perspectives of patients with lower-limb osteoarthritis on prescribed physical activity to develop a theoretically informed physiotherapy intervention. BMC Musculoskelet Disord. 2021;22(1):155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Che Hasan MK, Stanmore E, Todd C. Perspectives of ESCAPE-Pain Programme for older people with knee osteoarthritis in the community setting. Front Public Health. 2020;8(101616579):612413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ezzat A, Bell E, Kemp JL, O’Halloran P, Russell T, Wallis J, et al. Much better than I thought it was going to be: Telehealth delivered group-based education and exercise was perceived as acceptable among people with knee osteoarthritis. Osteoarthr Cartil Open. 2022;4(3):100271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cronstrom A, Dahlberg LE, Nero H, Ericson J, Hammarlund CS. I would never have done it if it hadn’t been digital’: a qualitative study on patients’ experiences of a digital management programme for hip and knee osteoarthritis in Sweden. BMJ open. 2019;9(5):e028388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Joelsson M, Bernhardsson S, Larsson MEH. Patients with chronic pain may need extra support when prescribed physical activity in primary care: a qualitative study. Scand J Prim Health Care. 2017;35(1):64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Larmer P, Dangan J, Kersten P. Patient reported benefits of hydrotherapy for arthritis. New Z J Physiotherapy. 2014;42(2):89–93. [Google Scholar]
- 105.Ledingham A, Cohn ES, Baker KR, Keysor JJ. Exercise adherence: beliefs of adults with knee osteoarthritis over 2 years. Physiother Theory Pract. 2020;36(12):1363–78. [DOI] [PubMed] [Google Scholar]
- 106.Louw A, Zimney K, Cox T, O’Hotto C, Wassinger CA. The experiences and beliefs of patients with complex regional pain syndrome: an exploratory survey study. Chronic Illn. 2018;14(2):104–18. [DOI] [PubMed] [Google Scholar]
- 107.Mannerkorpi K, Gard G. Physiotherapy group treatment for patients with fibromyalgia -- an embodied learning process. Disabil Rehabil. 2003;25(24):1372–80. [DOI] [PubMed] [Google Scholar]
- 108.Medina-Mirapeix F, Escolar-Reina P, Gascon-Canovas JJ, Montilla-Herrador J, Collins SM. Personal characteristics influencing patients’ adherence to home exercise during chronic pain: a qualitative study. J Rehabil Med. 2009;41(5):347–52. [DOI] [PubMed] [Google Scholar]
- 109.Mengshoel AM, Bjorbaekmo WS, Sallinen M, Wahl AK. It takes time, but recovering makes it worthwhile’- A qualitative study of long-term users’ experiences of physiotherapy in primary health care. Physiother Theory Pract. 2021;37(1):6–16. [DOI] [PubMed] [Google Scholar]
- 110.Palazzo C, Klinger E, Dorner V, Kadri A, Thierry O, Boumenir Y, et al. Barriers to home-based exercise program adherence with chronic low back pain: patient expectations regarding new technologies. Annals Phys Rehabilitation Med. 2016;59(2):107–13. [DOI] [PubMed] [Google Scholar]
- 111.Selten EM, Vriezekolk JE, Geenen R, van der Laan WH, van der Meulen-Dilling RG, Nijhof MW, et al. Reasons for treatment choices in knee and hip osteoarthritis: a qualitative study. Arthritis Care Res (Hoboken). 2016;68(9):1260–7. [DOI] [PubMed] [Google Scholar]
- 112.Withall J, Haase AM, Walsh NE, Young A, Cramp F. Physical activity engagement in early rheumatoid arthritis: a qualitative study to inform intervention development. Physiotherapy. 2016;102(3):264–71. [DOI] [PubMed] [Google Scholar]
- 113.Benjaminsson O, Biguet G, Arvidsson I, Nilsson-Wikmar L. Recurrent low back pain: relapse from a patient perspective. J Rehabil Med. 2007;39(8):640–5. [DOI] [PubMed] [Google Scholar]
- 114.Kamper SJ, Haanstra TM, Simmons K, Kay M, Ingram TGJ, Byrne J, et al. What do patients with chronic spinal pain expect from their physiotherapist? Physiother Can. 2018;70(1):36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Plank A, Rushton A, Ping Y, Mei R, Falla D, Heneghan NR. Exploring expectations and perceptions of different manual therapy techniques in chronic low back pain: a qualitative study. BMC Musculoskelet Disord. 2021;22(444):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Veenhof C, van Hasselt TJ, Koke AJ, Dekker J, Bijlsma JW, van den Ende CH. Active involvement and long-term goals influence long-term adherence to behavioural graded activity in patients with osteoarthritis: a qualitative study. Aust J Physiother. 2006;52(4):273–8. [DOI] [PubMed] [Google Scholar]
- 117.Nost TH, Steinsbekk A. A lifebuoy’ and ‘a waste of time’: patients’ varying experiences of multidisciplinary pain centre treatment- a qualitative study. BMC Health Serv Res. 2019;19(1015):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Campbell R, Evans M, Tucker M, Quilty B, Dieppe P, Donovan JL. Why don’t patients do their exercises? Understanding non-compliance with physiotherapy in patients with osteoarthritis of the knee. J Epidemiol Commun Health. 2001;55(2):132–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Toye F, Barker K. I can’t see any reason for stopping doing anything, but I might have to do it differently’--restoring hope to patients with persistent non-specific low back pain–a qualitative study. Disabil Rehabil. 2012;34(11):894–903. [DOI] [PubMed] [Google Scholar]
- 120.Wallis JA, Webster KE, Levinger P, Singh PJ, Fong C, Taylor NF. Perceptions about participation in a 12-week walking program for people with severe knee osteoarthritis: a qualitative analysis. Disabil Rehabil. 2019;41(7):779–85. [DOI] [PubMed] [Google Scholar]
- 121.Maki D, Lempp H, Critchley DJ. An exploration of experiences and beliefs about low back pain with arab muslim patients. Disabil Rehabil. 2021;44(18):5171–83. [DOI] [PubMed] [Google Scholar]
- 122.Churchill L, Lukacs MJ, Pinto R, Macdonald SJ, Giffin JR, Laliberte Rudman D, et al. A qualitative dominant mixed methods exploration of novel educational material for patients considering total knee arthroplasty. Disabil Rehabil. 2020;44(13):3054–61. [DOI] [PubMed]
- 123.Di Winter J, Juma S, Kennedy D, Dickson P, Denis S, Robarts S, et al. Patients’ perceptions of navigating the system for arthritis management: are they able to follow our recommendations? Physiother Can. 2014;66(3):264–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Larsson J, Westergren H, Haggman-Henrikson B, Ilgunas A, Wanman A, Malmstrom E-M. The feasibility of gym-based exercise therapy for patients with persistent neck pain. Scand J Pain. 2019;20(2):261–72. [DOI] [PubMed] [Google Scholar]
- 125.Gillis K, Augruso A, Coe T, O’Neill A, Radford L, Gibson BE, et al. Physiotherapy extended-role practitioner for individuals with hip and knee arthritis: patient perspectives of a rural/urban partnership. Physiother Can. 2014;66(1):25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cooper K, Schofield P, Klein S, Smith BH, Jehu LM. Exploring peer-mentoring for community dwelling older adults with chronic low back pain: a qualitative study. Physiotherapy. 2017;103(2):138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Escolar-Reina P, Medina-Mirapeix F, Gascón-Cánovas JJ, Montilla-Herrador J, Jimeno-Serrano FJ, de Oliveira Sousa SL, et al. How do care-provider and home exercise program characteristics affect patient adherence in chronic neck and back pain: a qualitative study. BMC Health Serv Res. 2010;10(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hilberdink B, van der Giesen F, Vliet Vlieland T, van Gaalen F, van Weely S. Supervised group exercise in axial spondyloarthritis: patients’ satisfaction and perspective on evidence-based enhancements. Arthritis Care Res (Hoboken). 2020;72(6):829–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Antcliff D, Keenan A-M, Keeley P, Woby S, McGowan L. Pacing does help you get your life back: the acceptability of a newly developed activity pacing framework for chronic pain/fatigue. Musculoskelet. 2022;20(1):99–110. [DOI] [PubMed] [Google Scholar]
- 130.Battista S, Dell’Isola A, Manoni M, Englund M, Palese A, Testa M. Experience of the COVID-19 pandemic as lived by patients with hip and knee osteoarthritis: an Italian qualitative study. BMJ open. 2021;11(10):e053194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bee P, McBeth J, MacFarlane GJ, Lovell K. Managing chronic widespread pain in primary care: a qualitative study of patient perspectives and implications for treatment delivery. BMC Musculoskelet Disord. 2016;17(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bin Sheeha B, Williams A, Johnson DS, Granat M, Jones R. Patients’ experiences and satisfaction at one year following primary total knee arthroplasty: a focus-group discussion. Musculoskelet. 2020;18(4):434–49. [DOI] [PubMed] [Google Scholar]
- 133.Geuens J, Geurts L, Swinnen TW, Westhovens R, Vanden Abeele V. Mobile health features supporting self-management behavior in patients with chronic arthritis: mixed-methods approach on patient preferences. JMIR mHealth uHealth. 2019;7(3):e12535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Moffat F, Paul L. Barriers and solutions to participation in exercise for moderately disabled people with multiple sclerosis not currently exercising: a consensus development study using nominal group technique. Disabil Rehabil. 2019;41(23):2775–83. [DOI] [PubMed] [Google Scholar]
- 135.Skolasky RL, Kimball ER, Galyean P, Minick KI, Brennan G, McGee T, et al. Identifying perceptions, experiences, and recommendations of telehealth physical therapy for patients with chronic low back pain: a mixed methods survey. Arch Phys Med Rehabil. 2022;103:1935–43. [DOI] [PubMed] [Google Scholar]
- 136.Daulat A. A pragmatic randomized controlled trial to compare a novel group physiotherapy programme with a standard group exercise programme for managing chronic low back pain in primary care. Int Musculoskelet Med. 2016;38(3/4):97–108. [Google Scholar]
- 137.Nees TA, Riewe E, Waschke D, Schiltenwolf M, Neubauer E, Wang H. Multidisciplinary pain management of chronic back pain: helpful treatments from the patients’ perspective. J Clin Med. 2020;9(1):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ackerman IN, Livingston JA, Osborne RH. Personal perspectives on enablers and barriers to Accessing Care for hip and knee osteoarthritis. Phys Ther. 2016;96(1):26–36. [DOI] [PubMed] [Google Scholar]
- 139.Lovo S, Harrison L, O’Connell ME, Trask C, Bath B. Experience of patients and practitioners with a team and technology approach to chronic back disorder management. J Multidiscip Healthc. 2019;12(101512691):855–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Nair BV, Schuler R, Stewart S, Taylor-Gjevre RM. Self-reported barriers to Healthcare Access for Rheumatoid Arthritis patients in Rural and Northern Saskatchewan: a mixed methods study. Musculoskelet. 2016;14(4):243–51. [DOI] [PubMed] [Google Scholar]
- 141.Mengshoel AM, Robinson HS. Clinical significance of specific spinal mobilization for patients with ankylosing spondylitis evaluated by quantitative assessments and patient interviews. Disabil Rehabil. 2008;30(5):355–64. [DOI] [PubMed] [Google Scholar]
- 142.Oien AM, Iversen S, Stensland P. Narratives of embodied experiences - therapy processes in Norwegian psychomotor physiotherapy. Adv Physiotherapy. 2007;9(1):31–9. [Google Scholar]
- 143.Reid DA, Potts G, Burnett M, Konings B. Physiotherapy management of knee and hip osteoarthritis: a survey of patient and medicai practitioners’ expectations, experiences and perceptions of effectiveness of treatment. New Z J Physiotherapy. 2014;42(3):118–25. [Google Scholar]
- 144.Brown J, Doherty D, Claus AP, Gilbert K, Nielsen M. In a pandemic that limits contact, can Videoconferencing enable Interdisciplinary Persistent Pain services and what are the patient’s perspectives? Arch Phys Med Rehabil. 2022;103(3):418–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lawford BJ, Bennell KL, Hinman RS. Consumer perceptions of and willingness to use remotely delivered service models for exercise management of knee and hip osteoarthritis: a cross-sectional survey. Arthritis Care Res (Hoboken). 2017;69(5):667–76. [DOI] [PubMed] [Google Scholar]
- 146.Fritz JM, Lane E, Minick KI, Bardsley T, Brennan G, Hunter SJ, et al. Perceptions of Telehealth Physical Therapy among patients with chronic low back Pain. Telemedicine Rep. 2021;2(1):258–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Cederbom S. The importance of a daily rhythm in a supportive environment – promoting ability in activities in everyday life among older women living alone with chronic pain. Disabil Rehabil. 2014;36(24):2050–8. [DOI] [PubMed] [Google Scholar]
- 148.Kleiner MJ, Kinsella EA, Miciak M, Teachman G, McCabe E, Walton DM. An integrative review of the qualities of a ‘good’physiotherapist. Physiother Theory Pract. 2023;39(1):89–116. [DOI] [PubMed] [Google Scholar]
- 149.Augeard N, Bostick G, Miller J, Walton D, Tousignant-Laflamme Y, Hudon A, et al. Development of a national pain management competency profile to guide entry-level physiotherapy education in Canada. Can J Pain. 2022;6(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. Pain. 2016;157(8):1607–10. [DOI] [PubMed] [Google Scholar]
- 151.Chi-Lun-Chiao A, Chehata M, Broeker K, Gates B, Ledbetter L, Cook C, et al. Patients’ perceptions with musculoskeletal disorders regarding their experience with healthcare providers and health services: an overview of reviews. Archives Physiotherapy. 2020;10(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Deslauriers S, Raymond MH, Laliberte M, Lavoie A, Desmeules F, Feldman DE, et al. Access to publicly funded outpatient physiotherapy services in Quebec: waiting lists and management strategies. Disabil Rehabil. 2017;39(26):2648–56. [DOI] [PubMed] [Google Scholar]
- 153.Deslauriers S, Roy J-S, Bernatsky S, Blanchard N, Feldman DE, Pinard AM, et al. The burden of waiting to access pain clinic services: perceptions and experiences of patients with rheumatic conditions. BMC Health Serv Res. 2021;21(160):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Dupuis F, Déry J, De Lucas FC, Pecora AT, Gagnon R, Harding K, et al. Strategies to reduce waiting times in outpatient rehabilitation services for adults with physical disabilities: a systematic literature review. J Health Serv Res Policy. 2022;27(2):157–67. [DOI] [PubMed] [Google Scholar]
- 155.May C, Brcic V, Lau B. Characteristics and complexity of chronic pain patients referred to a community-based multidisciplinary chronic pain clinic. Can J Pain. 2018;2(1):125–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Nguyen M, Ugarte C, Fuller I, Haas G, Portenoy RK. Access to care for chronic pain: racial and ethnic differences. J Pain. 2005;6(5):301–14. [DOI] [PubMed] [Google Scholar]
- 157.Martin D, Nettleton S, Buse C, Prior L, Twigg J. Architecture and health care: a place for sociology. Sociol Health Illn. 2015;37(7):1007–22. [DOI] [PubMed] [Google Scholar]
- 158.Okken V, Van Rompay T, Pruyn A. Exploring space in the consultation room: environmental influences during patient–physician interaction. J Health Communication. 2012;17(4):397–412. [DOI] [PubMed] [Google Scholar]
- 159.Gharaveis A, Hamilton DK, Pati D. The impact of environmental design on teamwork and communication in healthcare facilities: a systematic literature review. HERD: Health Environ Res Des J. 2018;11(1):119–37. [DOI] [PubMed] [Google Scholar]
- 160.Zaniboni L, Sarey Khanie M, Pernigotto G, Toftum J, Gasparella A, Olesen B. Lighting conditions in physiotherapy centres: a comparative field study. Lighting Res Technol. 2022;54(4):377–408. [Google Scholar]
- 161.Buse C, Martin D, Nettleton S. Conceptualising ‘materialities of care’: making visible mundane material culture in health and social care contexts. Sociol Health Illn. 2018;40(2):243–55. [DOI] [PubMed] [Google Scholar]
- 162.O’Keeffe M, Cullinane P, Hurley J, Leahy I, Bunzli S, O’Sullivan PB, et al. What influences patient-therapist interactions in musculoskeletal physical therapy? Qualitative systematic review and meta-synthesis. Phys Ther. 2016;96(5):609–22. [DOI] [PubMed] [Google Scholar]
- 163.Morera-Balaguer J, Botella-Rico JM, Catalán-Matamoros D, Martínez-Segura O-R, Leal-Clavel M, Rodríguez-Nogueira Ó. Patients’ experience regarding therapeutic person-centered relationships in physiotherapy services: a qualitative study. Physiother Theory Pract. 2019;37(1):17–27. [DOI] [PubMed] [Google Scholar]
- 164.Praestegaard J, Gard G, Glasdam S. Physiotherapy as a disciplinary institution in modern society – a foucauldian perspective on physiotherapy in Danish private practice. Physiother Theory Pract. 2015;31(1):17–28. [DOI] [PubMed] [Google Scholar]
- 165.Nicholls DA. Foucault and physiotherapy. Physiother Theory Pract. 2012;28(6):447–53. [DOI] [PubMed] [Google Scholar]
- 166.Mescouto K, Olson RE, Hodges PW, Costa N, Patton MA, Evans K, et al. Physiotherapists both reproduce and resist biomedical dominance when working with people with low back pain: a qualitative study towards new praxis. Qual Health Res. 2022;32(6):902–15. [DOI] [PubMed] [Google Scholar]
- 167.McGregor JA, Camfield L, Woodcock A, Needs. Wants and goals: Wellbeing, Quality of Life and Public Policy. Appl Res Qual Life. 2009;4(2):135–54. [Google Scholar]
- 168.Brock G, Hassoun N, Needs. The International Encyclopedia of Ethics. 2013.
- 169.Brock G, Miller D. Needs in moral and political philosophy. 2019.
- 170.Schweighart R, O’Sullivan JL, Klemmt M, Teti A, Neuderth S. Wishes and needs of nursing home residents: a scoping review. Healthcare. 2022;10(5):854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Malfliet A, Ickmans K, Huysmans E, Coppieters I, Willaert W, Van Bogaert W, et al. Best evidence rehabilitation for chronic pain part 3: low back pain. J Clin Med. 2019;8(7):1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Sterling M, de Zoete RM, Coppieters I, Farrell SF. Best evidence rehabilitation for chronic pain part 4: neck pain. J Clin Med. 2019;8(8):1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 174.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evid Implement. 2015;13(3):141–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.