Analysis of nationally representative survey data reveals the existence of systemic disparities in the mental health experiences and outcomes of U.S. adults living with chronic pain.
Supplemental Digital Content is Available in the Text.
Keywords: Chronic pain, Mental health, Anxiety, Depression, Screening, GAD-7, PHQ-8, Treatment access, Treatment use, Treatment quality, Health disparities
Abstract
Previous research suggests that individuals with mental health needs and chronic pain may be less likely to use mental health treatment compared with those with mental health needs only. Yet, few studies have investigated the existence of population-level differences in mental health treatment use. We analyzed data from the National Health Interview Survey (n = 31,997) to address this question. We found that chronic pain was associated with end-to-end disparities in the mental health journeys of U.S. adults: (1) Those living with chronic pain are overrepresented among U.S. adults with mental health needs; (2) among U.S. adults with mental health needs, those living with chronic pain had a lower prevalence of mental health treatment use; (3) among U.S. adults who used mental health treatment, those living with chronic pain had a higher prevalence of screening positive for unremitted anxiety or depression; (4) among U.S. adults living with both chronic pain and mental health needs, suboptimal mental health experiences were more common than otherwise—just 44.4% of those living with mental health needs and co-occurring chronic pain reported use of mental health treatment and screened negative for unremitted anxiety and depression, compared with 71.5% among those with mental health needs only. Overall, our results suggest that U.S. adults with chronic pain constitute an underrecognized majority of those living with unremitted anxiety/depression symptoms and that the U.S. healthcare system is not yet adequately equipped to educate, screen, navigate to care, and successfully address their unmet mental health needs.
1. Introduction
The co-occurrence of chronic pain with anxiety and/or depression has been extensively documented in clinical and population-based studies.14,24,26,30,33,39,44,45,74,76,78,85,93,96 Our recent study found that co-occurring chronic pain and clinically significant anxiety or depression symptoms are experienced by approximately 4.9% of the U.S. adult population, that U.S. adults living with chronic pain are approximately 5 times more likely to have clinically significant unremitted anxiety or depression compared with those not living with chronic pain, and that U.S. adults living with chronic pain comprise the majority (55.5%) of those with unremitted anxiety or depression symptoms.31 These findings raised the possibility of whether U.S. adults with chronic pain may meaningfully differ from others in the prevalence of mental health treatment use.
Previous research suggests that patients with chronic pain may use mental health treatment less frequently or more reluctantly than others.10,16,17,29,40,41,82,97 Yet, in reviewing the literature, we observed that few population-level analyses have examined patterns of mental health treatment use among U.S. adults with chronic pain. Thus, our objective in this study was to determine whether population-level differences in mental health treatment utilization are detectable between those who have and do not have co-occurring chronic pain. We used nationally representative survey data from the National Health Interview Survey (NHIS). The NHIS has been identified as the best single survey for monitoring the epidemiology of chronic pain in the United States.34 National Health Interview Survey data have been used to estimate the prevalence of chronic pain,27,66,107 highlight disparities in chronic pain,4,5,83,104–106 and understand pain treatment strategies used by the general population.5,67 National Health Interview Survey data are also routinely used to assess national patterns of mental health and mental health treatment use,21,23,43,58,90,102 including examination of mental health treatment use disparities associated with racial and ethnic status,8,19,91 sex/gender,13,58 age,90,99 sexual orientation,22,42 rurality,68 and cancer survivorship.6,7,47
2. Methods
2.1. Study design and analysis plan
In this study, we empirically examine potential differences in patterns of mental health treatment among those with and without chronic pain. However, because the prevalence of anxiety and depression are substantially elevated among individuals with chronic pain, unstandardized rates of mental health treatment are not directly comparable. To support the comparison of rates, we first defined the universe of those for whom mental health would be a relevant treatment consideration, and, using this universe as the denominator, identified the proportion who reported the past 12-month use of mental health treatment. The results of this first analysis, which sorted the U.S. adult population with mental health needs into 3 mutually exclusive and exhaustive categories, were grouped by presence or absence of chronic pain.
In a second analysis, we represent the data from a different perspective, as a “cascade of care” from (1) mental health need, to (2) mental health treatment use, and to (3) negative screening for anxiety/depression. Cascade-of-care analysis is an established approach in health services research used to identify vulnerabilities and gaps between healthcare systems and population needs.3,38,46,49,51,53,63,77,86,88,100,101 We used the cascade to examine potential disparities in the distribution of mental health cascade of care for U.S. adults with mental health needs with and without co-occurring chronic pain.
Finally, to ensure these disparities are not due to statistical confounding, we regressed the past 12-month mental health treatment on insurance status, age, sex, race/ethnicity, presence of a cancer diagnosis, presence of functional limitations in daily living, and presence of chronic pain (Supplemental Table 2, http://links.lww.com/PAIN/C97). Among those reporting the past 12-month use of mental health treatment, we also regressed the presence of unremitted symptoms on the same factors (Supplemental Table 3, http://links.lww.com/PAIN/C97).
2.2. Data source
The NHIS is a nationally representative survey of the U.S. adult general population; it has been used in the surveillance of U.S. population health since 1957. This survey, conducted continuously by the National Center for Health Statistics, is used to report national prevalence estimates, track trends in population health, and measure progress toward public health benchmarks, including healthcare access, treatment utilization, and a wide variety of population health outcomes of interest to policymakers and researchers.69–72 The survey design is stratified, clustered, and weighted to accurately represent the U.S. population and mitigate sampling and nonresponse bias. Additional information on the survey design and implementation is publicly available on the National Health Interview Survey website.70
The 2019 NHIS interview schedule for adults was the first103 NHIS adult survey to include validated screening and diagnostic scales for clinically significant anxiety and depression symptoms.56,87 These scales and the chronic pain module will next appear together in the 2025 adult data set; the data will be released to the public in 2026. The 2019 data set contains 31,997 U.S. adults, sampled and weighted to represent 244.6 million U.S. adults in the noninstitutionalized U.S. population (95% CI: 237.7-252.4 million). The sample adult response rate was 59.1%.70
2.3. Chronic pain
Chronic Pain was measured using the NHIS survey item “In the past 3 months, how often did you have pain? Response measures included: Would you say never, some days, most days, or every day?” Those who answered “Most Days” or “Every Day” to this survey item were considered to have chronic pain, while those selecting “Never” or “Some Days” were considered not to have chronic pain. This operationalization is consistent with the International Association for the Study of Pain (IASP) definition of chronic pain as implemented in the International Classification of Disease (ICD-11).92
2.4. Unremitted anxiety and/or depression symptoms
The 2019 NHIS adult data set was the first to include widely used validated clinical screening and diagnostic scales for symptoms of anxiety and depression: (1) the General Anxiety Disorder-7 (GAD-7), a validated scale used to screen for and diagnose anxiety, and (2) the Patient Health Questionnaire-8 (PHQ-8), a validated scale used to screen for and diagnose depression. The GAD-7 uses summative scoring to categorize anxiety symptoms over the past 2 weeks as follows: none (0-4), mild (5-9), moderate (10-14), and severe (15-21). We operationalized clinically significant unremitted anxiety symptoms in line with the standard cut-point; respondents who scored 10 or higher on the GAD-7 were considered to have unremitted anxiety.87 The PHQ-8 also uses summative scoring in the categorization of depression symptoms over the past 2 weeks: none/minimal (0-4), mild (5-9), moderate (10-14), and severe (15-24). We operationalized clinically significant unremitted depression symptoms in line with the standard clinical cut-point; respondents who scored greater than or equal to 10 on the PHQ-8 were considered to have unremitted depression.56 Survey respondents were coded as having anxiety and/or depression (A/D) symptoms if they scored greater than or equal to 10 on the PHQ-8, the GAD-7, or both. Most respondents reporting co-occurring chronic pain and mental health symptoms had clinically significant symptoms of both anxiety and depression.
It is useful to note that not all people who have anxiety and/or depression as clinical diagnoses will screen positive for clinically significant symptoms. Individuals who utilize mental health treatment and for whom mental health treatment has been effective would likely not display the clinically significant symptoms that warranted the initial diagnoses of anxiety or depression. In other words, the use of mental health treatment in the absence of unremitted anxiety/depression symptoms does not suggest the absence of an ongoing mental health need.
2.5. Use of mental health treatment
The use of mental health treatment is operationalized using a combination of NHIS survey items. Respondents were asked, “How often do you feel worried, nervous, or anxious?” Those who responded daily, weekly, monthly, or a few times a year, were asked, “Do you take prescription medication for these feelings?” with response choices Yes or No. All respondents were asked, “How often do you feel depressed?” Those who responded daily, weekly, monthly, or a few times a year, were asked, “Do you take prescription medication for these feelings?” with response choices Yes or No. All respondents were also asked, “During the past 12 months, did you take prescription medication to help you with any other emotions or with your concentration, behavior, or mental health? Participants who took medication for anxiety, depression, or any other mental/behavioral health reason during the past 12 months were considered to have taken mental health medication.” Respondents were asked, “During the past 12 months, did you receive counseling or therapy from a mental health professional such as a psychiatrist, psychologist, psychiatric nurse, or clinical social worker?” with response choices Yes or No. Respondents were considered to have used counseling or therapy if they answered yes to this question. Respondents were considered to have used mental health treatment in the past 12 months, if they had taken mental health medication, received mental health counseling or therapy, or received both. This is the standard operationalization used by the National Center for Health Statistics.90
2.6. Use of mental health treatment and negative screening for unremitted anxiety or depression
The National Health Interview Survey provides intent-to-treat information for most survey respondents who reported the past 12-month use of mental health treatment. Respondents who used medication as part of their mental health treatment approach were directly asked whether they take prescription medicine for depression or anxiety. Owing to the design of the survey, the National Health Interview Survey does not provide equivalent intent-to-treat information for respondents who used counseling or therapy and did not use any mental health medication as part of their treatment. For those respondents, the best available data about intent to treat comes from 2 survey items that ask “Have you ever been told by a doctor or other health professional that you have any type of depression?,” and “Have you ever been told by a doctor or other health professional that you have any type of anxiety?” We considered an affirmative response to these survey items to be suggestive of an intent-to-treat anxiety or depression.
2.7. Use of mental health treatment and positive screening for unremitted anxiety or depression
As part of routine behavioral health practice, every mental health services provider (of substance use counseling, medication for opioid use disorder, management of attention deficit hyperactivity disorder, providers of family or couples therapy, etc) is expected to routinely assess for the possibility of unmet mental health needs; anxiety and depression are among the most frequent unmet needs to address. Therefore, this study considers that the past 12-month use of mental health treatment in combination with a positive screening for unremitted anxiety and depression is indicative of a suboptimal mental health treatment experience.
2.8. Existence of mental health treatment need
Using the available data, we operationalized “mental health treatment need” as follows: survey respondents who did not report any past 12-month use of mental health treatment and did not report clinically significant anxiety or depression symptoms were coded as “Does not have a mental health treatment need.” The remaining respondents were coded as “Has a mental health treatment need”; this analytic category included those who screened positive for clinically significant unremitted A/D symptoms, those who reported past 12-month use of mental health treatment, and those for whom both were true. These mutually exclusive and exhaustive analytic categories are summarized in Table 1.
Table 1.
Four mental health experience categories reflecting different combinations of mental health treatment use and anxiety/depression symptoms.
| MH experiences | Operationalization | |
|---|---|---|
| No MH treatment need | Tx not used, A/D (−) | Did not use any mental health treatment in the past 12 mo, and Screened negative A/D (−) for clinically significant anxiety/depression symptoms |
| MH treatment need | Tx used, A/D (−) |
Used mental health treatment in the past 12 mo, and Screened negative A/D (−) for clinically significant anxiety/depression symptoms |
| Tx used, A/D (+) |
Used mental health treatment in the past 12 mo, and Screened positive A/D (+) for clinically significant anxiety/depression symptoms |
|
| Tx not used, A/D (+) | Did not use mental health treatment in the past 12 mo, and Screened positive A/D (+) for clinically significant anxiety/depression symptoms |
A/D, anxiety/depression; MH, mental health; Tx, treatment.
2.9. Social, demographic, and functional variables
2.9.1. Sex
Response options concerning respondent sex assigned at birth include male, female, or not ascertained. The NHIS adult survey does not collect data on respondent gender.
2.9.2. Race/ethnicity
Survey response options for race/ethnicity include “Hispanic,” “Non-Hispanic White Only,” “Non-Hispanic Black/African-American only,” “Non-Hispanic Asian only,” “Non-Hispanic AIAN only,” “Non-Hispanic AIAN and any other group,” and “Other single and multiple races.”
2.9.3. Age
Age in years was categorized to facilitate interpretation. Categories included 18 to 24, 25 to 34, 35 to 44, 45 to 54, 55 to 64, 65 to 74 to 75 to 84, and 85+.
2.9.4. History of cancer diagnosis
Receipt of a cancer diagnosis was assessed using a binary yes/no survey item that asked “Have you EVER been told by a doctor or other health professional that you had cancer or a malignancy of any kind?”
2.9.5. Health insurance coverage status
Adults were considered to not have insurance coverage if they did not have any of the following: private health insurance, Medicare, Medicaid, State Children's Health Insurance Program (CHIP), a state-sponsored health plan, other government programs, or a military health plan. Coverage status is binary; respondents are considered either “covered” or “not covered.”
2.9.6. Functional limitations in daily living
The presence of functional limitation in activities of daily living was assessed using a survey item that asked “Because of a physical, mental, or emotional condition, do you have difficulty doing errands alone such as visiting a doctor's office or shopping?” Individuals who responded that they have “no difficulty” were considered to not have functional limitations in daily activities; those who selected “some difficulty,” “a lot of difficulty,” or “cannot do at all” were considered to have functional limitations in daily activities.
2.10. Analysis details
Estimates and percentages presented in this report account for the stratification, clustering, and weighting procedures of the complex NHIS survey design70 and were calculated with SAS statistical software (Version 9.4). Disparities in the distribution of mental health experiences for those with and without chronic pain were assessed using adjusted Rao–Scott χ2 test statistics; graphics were generated using R software. Logistic regression analyses were completed to assess the degree to which these disparities could be explained by statistical confounding. Intent-to-treat analysis was conducted among those who reported the past 12-month use of mental health treatment and screened negative for unremitted anxiety and depression, to assess the degree to which mental health treatment was used with intent to treat anxiety or depression in this group.
2.11. Missing data
Responses recorded as “Refused,” “Don't Know,” or “Not Ascertained” in responses to questions used for the above measures were considered missing and were excluded from analyses. Missing data for questions used to operationalize chronic pain, A/D symptoms, and past 12-month use of mental health treatment included a total of 900 observations, representing 2.8% of overall data. In the first supplemental logistic regression analysis, 38 participants (0.5%) of 7476 participants with mental health needs were excluded due to missing data across the predictors. Similarly, in the second supplemental logistic regression analysis, 88 participants (1.4%) of 6490 participants were excluded. Complete case analysis was used in light of the small amount of missing data (<3%), the robust sample size, and the resultant expectation of minimal precision and bias loss57 in the context of odds ratio and prevalence estimation with observational data.65 In light of the aforementioned study data characteristics, any deviations from the missing at random (MAR) assumption are unlikely to affect the validity of the estimates.59 Nevertheless, we evaluated patterns of missingness; consistent mean values supported the expectation that missingness is unlikely to be related to the variables under study and that the MAR assumption is justifiable.
3. Results
3.1. Disparities in the distribution of mental health experiences
Individuals living with chronic pain represent approximately 20.4% of the U.S. adult population,107 yet make up an estimated 39.1% of U.S. adults with a mental health treatment need (21.5 million of 55.1 million = 39.1%) (P < 0.001). Confidence intervals for population proportions as well as prevalence estimates in millions of people are presented in Table 2.
Table 2.
Mental health experiences among U.S. adults with a mental health treatment need, by presence/absence of chronic pain.
| U.S. adults with a mental health treatment need 55.1 million [52.9, 57.3] |
||||
|---|---|---|---|---|
|
No chronic pain 33.6 million [32.0, 35.1] |
Living with chronic pain 21.5 million [20.3, 22.8] |
|||
| N [95 CI] | % [95 CI] | N [95 CI] | % [95 CI] | |
| Tx used, A/D (−) | 24.0 million [22.7, 25.3] | 71.5% [69.8, 73.2] | 9.5 million [8.9, 10.2] | 44.4% [42.2, 46.6] |
| Tx used, A/D (+) | 5.1 million [4.6, 5.6] | 15.2% [13.9, 15.4] | 8.0 million [7.3, 8.7] | 37.2% [35.0, 39.4] |
| Tx not used, A/D (+) | 4.5 million [4.0, 5.0] | 13.3% [12.0, 14.7] | 4.0 million [3.5, 4.4] | 18.4% [16.6, 20.2] |
Data source: National Center for Health Statistics, National Health Interview Survey, 2019.
N = national prevalence, reported in millions of U.S. adults, grouped by presence/absence of chronic pain.
% = prevalence as a proportion of U.S. adults, grouped by presence/absence of chronic pain.
Tx used, A/D (−) = used mental health treatment in the past 12 months, screened negative for unremitted anxiety or depression.
Tx used, A/D (+) = used mental health treatment in the past 12 months, screened positive for unremitted anxiety or depression.
Tx not used, A/D (+) = did not use mental health treatment in the past 12 months, screened positive for unremitted anxiety or depression.
To visualize the distribution of mental health experiences among those with mental health treatment needs, we generated an alluvial plot showing the distribution of U.S. adults to the 3 mental health experience categories, grouped by presence/absence of chronic pain (Fig. 1).
Figure 1.
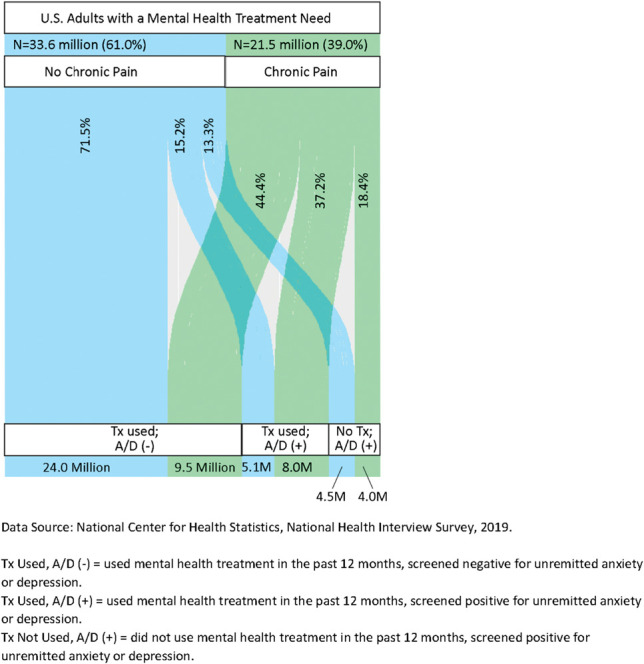
Use of mental health treatment (Tx) and status of anxiety/depression (A/D) screening, among all U.S. adults with a mental health treatment need, grouped by presence/absence of chronic pain.
3.1.1. Mental health treatment used and screened negative for anxiety and depression
Among U.S. adults with a mental health treatment need, those with chronic pain were substantially less likely than others to report the past 12-month use of MH treatment and screen negative for unremitted anxiety and depression. Only 44.4% of those living with chronic pain, an estimated 9.5 million people, used mental health treatment and screened negative for unremitted anxiety/depression symptoms, compared with 71.5% of those without chronic pain, an estimated 24.0 million people (P < 0.001) (Fig. 1, Table 2).
Among those who used mental health treatment and screened negative for unremitted anxiety and depression, direct measurement of intent-to-treat anxiety or depression is available for 76.4% of those without chronic pain and 87.0% of those with chronic pain. In medication-only users, 91.8% with chronic pain had intended to treat anxiety or depression compared with 84.4% of those without chronic pain; among those using both therapy and medication, 87.2% of those with chronic pain intended to treat anxiety or depression compared with 85.8% among those without chronic pain. Direct measurement of intent-to-treat analysis was not available for the 20.6% who did not use medication as part of mental health treatment. For these individuals, we considered having ever been told by a health professional they have anxiety or depression to be suggestive of intent to treat. Among all U.S. adults who used mental health treatment and screened negative for anxiety and depression, we estimated that treatment was likely intended to address anxiety or depression in at least 71.4% of U.S. adults without chronic pain and at least 83.8% of those with chronic pain. Full intent-to-treat analysis details are reported in Supplemental Table 1, http://links.lww.com/PAIN/C97.
3.1.2. Mental health treatment used and screened positive for anxiety or depression
Among U.S. adults with a mental health treatment need, those with chronic pain were more than twice as likely as those without chronic pain to report the past 12-month use of mental health treatment and screen positive for unremitted anxiety/depression. Approximately 37.2% of those living with chronic pain, an estimated 8.0 million people, used mental health treatment and screened positive for unremitted clinically significant anxiety/depression symptoms, compared with 15.2% of those without chronic pain, an estimated 5.1 million people (P < 0.001). U.S. adults with chronic pain are more than twice as likely as others to experience unremitted anxiety symptoms when mental health treatment is used. U.S. adults with chronic pain make up 61.1% (8.0 million of 13.1 million) of those who used mental health treatment and screened positive for unremitted clinically significant anxiety/depression symptoms (Fig. 1, Table 2).
3.1.3. Mental health treatment not used and screened positive for anxiety or depression
Among U.S. adults with a mental health treatment need, 18.4% of those living with chronic pain, an estimated 4.0 million people, did not use mental health treatment during the past 12 months and screened positive for unremitted anxiety/depression, compared with 13.3% of those without chronic pain, an estimated 4.4 million people (P < 0.001). U.S. adults with chronic pain are significantly more likely than others to experience untreated anxiety or depression symptoms (Fig. 1, Table 2).
3.2. Disparities in the mental health cascade of care
Figure 2 demonstrates differences in mental health benefits across 3 inflection points in the mental health cascade of care. Mental health treatment need is substantially more prevalent among U.S. adults living with chronic pain than among those without chronic pain (P < 0.001). Specifically, 43.2% of U.S. adults living with chronic pain had a mental health need, corresponding to an estimated 21.5 million U.S. adults, compared with 17.4% of those without chronic pain, corresponding to an estimated 33.6 million people (Fig. 2, Table 3). A hypothetical (perfectly functioning) health system would have a slope of 0—all people with a mental health treatment need would use treatment and all people who used treatment would screen negative for symptoms. In real-world healthcare systems, there is always some unmet need, and the steepness of this slope, or the size of the stepdown between bars in Figure 2, shows the magnitude of the gaps in healthcare system performance.
Figure 2.
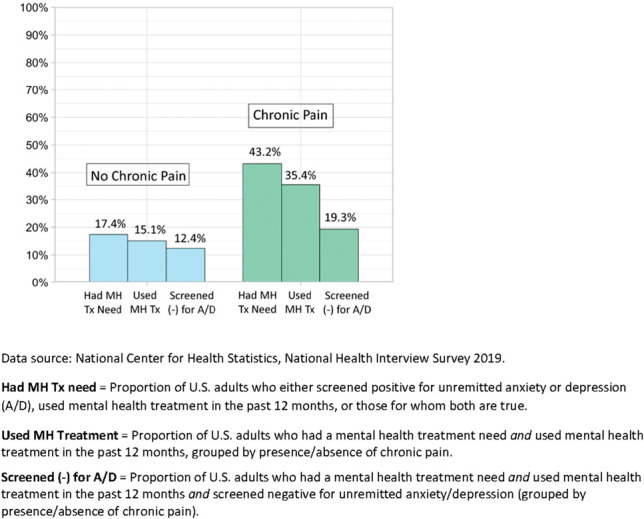
Visualizing the cascade to mental health benefit: comparing U.S. adults living with chronic pain (N = 49.8 million) to others (N = 193.1 million).
Table 3.
Cascade to mental health benefit, by presence/absence of chronic pain.
| U.S. adults without chronic pain | U.S. adults with chronic pain | |||||||
|---|---|---|---|---|---|---|---|---|
| N [95 CI] | % [95 CI] | % of MH need [95 CI] | % of used MH Tx [95 CI] | N [95 CI] | % [95 CI] | % of MH need [95 CI] | % of used MH Tx [95 CI] | |
| Had MH Tx need | 33.6 million [32.0, 35.1] | 17.4% [16.8, 18.0] | N/A | N/A | 21.5 million [20.3, 22.7] | 43.2% [41.7, 44.7] | N/A | N/A |
| Had MH Tx need and used MH Tx | 29.1 million [27.6, 30.6] | 15.1% [14.5, 15.7] | 86.7% [85.3, 88.0] | N/A | 17.6 million [16.5, 18.6] | 35.4% [33.8, 36.7] | 81.6% [79.8, 83.4] | N/A |
| Had MH Tx need and used MH Tx and screened (−) for A/D | 24.0 million [22.7, 25.3] | 12.4% [11.9, 13.0] | 71.5% [69.8, 73.2] | 82.5% [81.0, 84.0] | 9.5 million [8.9, 10.2] | 19.2% [18.0, 20.3] | 44.4% [42.2, 46.6] | 54.4% [51.9, 56.8] |
Data source: National Center for Health Statistics, National Health Interview Survey, 2019.
N = national prevalence, reported in millions of U.S. adults, grouped by presence/absence of chronic pain.
% = prevalence as a proportion of all U.S. adults, grouped by presence/absence of chronic pain.
% MH need = prevalence as a proportion of U.S. adults with mental health need, grouped by presence/absence of chronic pain.
% of Used MH Tx = prevalence as a proportion of U.S. adults who used mental health treatment in the past 12 months, grouped by presence/absence of chronic pain.
A/D, anxiety/depression; MH, mental health; Tx, treatment.
Among all U.S. adults with mental health treatment needs, 81.6% of those with chronic pain used mental health treatment, compared with 86.7% of others (Table 3). Among U.S. adults who used mental health treatment in the past 12 months, those with chronic pain less often screened negative for anxiety/depression symptoms than those without chronic pain (P < 0.001). Among all U.S. adults who used mental health treatment in the past 12 months, only 54.4% of those living with chronic pain, an estimated 9.5 million people, screened negative for unremitted anxiety/depression, compared with 82.5% of those without chronic pain, an estimated 24.0 million people. U.S. adults with chronic pain make up 28.3% (9.5 million out of 33.5 million) of U.S. adults who used mental health treatment and screened negative for unremitted anxiety/depression.
The chronic pain-associated disparities in mental health treatment use and in the presence of unremitted symptoms among those who used treatment remained statistically and substantively significant in logistic regression models controlling for potential confounds including health insurance status, age, sex, race/ethnicity, presence/absence of a cancer diagnosis, and presence/absence of functional limitation in daily life. Among those with a mental health treatment need, chronic pain was associated with a 40.3% reduction in odds of using mental health treatment (unadjusted odds ratio = 0.684 P < 0.001; adjusted odds ratio = 0.597 P < 0.001). Complete logistic regression results on the use of mental health treatment (universe = U.S. adults with a mental health need) are presented in Supplemental Table 2, http://links.lww.com/PAIN/C97. Among those who reported the past 12-month use of mental health treatment, chronic pain was associated with 270% times the odds of screening positive for anxiety or depression (unadjusted odds ratio = 3.961 P < 0.001; adjusted odds ratio = 3.696 P < 0.001). Complete logistic regression results on unremitted anxiety and depression symptoms (universe = U.S. adults who reported past 12-month use of mental health treatment) are presented in Supplemental Table 3, http://links.lww.com/PAIN/C97.
4. Discussion
Our cascade-of-care analyses detected chronic pain-associated disparities at 3 distinct inflection points: (1) disproportionately frequent need for mental health treatment, (2) disproportionately infrequent past 12-month use of mental health treatment, and (3) disproportionately infrequent negative screening for anxiety/depression when past 12-month use of mental health treatment was reported. At every point, U.S. adults living with chronic pain were underserved. The association between chronic pain and suboptimal mental health experiences persisted in size and statistical significance when controlling for the influence of health insurance status, age, sex, race/ethnicity, presence/absence of a cancer diagnosis, and presence of functional limitations in daily life. Our intent-to-treat analysis found that differences in intention to treat anxiety or depression vs some other behavioral or mental concerns appear unlikely to drive these disparities.
Our findings are consistent with previous patient-centered and provider-centered studies that suggest the existence of chronic pain-specific barriers to meeting the mental health needs of those living with chronic pain. Those living with chronic pain may have several reasons for the use of mental health care, eg, addressing sleep difficulty. Thus, the fact that U.S. adults with chronic pain access mental health care at lower rates than others with mental health needs is indicative of a meaningful treatment gap. Further research is needed to identify the mechanisms driving these disparities and design interventions capable of addressing the suboptimal mental health experiences of U.S. adults with chronic pain—including the study of the role of specific pain syndromes and subclassifications in relation to these disparities. We outline several possibilities that could plausibly exert a chronic pain-specific influence on the U.S. mental health system cascade of care and may be worthy of further exploration.
4.1. Low awareness of the rationale for mental health treatment in the context of chronic pain
Patients/providers may (inaccurately) assume that mental health treatment is only indicated for anxiety and depressive symptoms that are incongruent with an individual's perceived quality of life. If anxiety and depression are secondary to chronic pain, patients/providers may inaccurately assume that relief from anxiety and depression is possible only through relief from chronic pain. Yet, in fact, mental health treatment is a first-line treatment that can meaningfully reduce mental and emotional suffering and improve the quality of life of people whose lives are impacted by chronic pain.18,29,36,54,89
4.2. Ineffective identification of mental health treatment need
Providers treating patients for chronic pain have little training in mental health and may not initially recognize mood symptoms as such; instead, significant anxiety or depression symptoms may be understood as pertaining to the aversiveness of pain alone.41 A typical experience in seeking treatment for chronic pain is a full workup with imaging and laboratory test results, searching for biological explanations for chronic pain. In many cases, mental health is only discussed after all biomedical investigation is exhausted without a positive finding. Some patients are being discharged from care when they are first advised that mental healthcare might help.50 Clinical workflows that approach pain and mental health dualistically (either/or) may communicate or reinforce the inaccurate belief that mental health treatment is a last-line treatment for “psychogenic” pain that has no verifiable basis.25,84 Primary and family care providers prescribe most prescriptions for anxiety/depression in the United States37 and are usually the first-line clinical encounter related to acute and chronic pain.20,64 This workforce may be an intervention target associated with high dividends at scale.41
4.3. Low patient receptivity to discussing mental health treatment
In clinical encounters, the possibility of mental or behavioral health concerns may interact with the lived experience of chronic pain in complicated ways. Patients often feel stigmatized and invalidated by family, friends, coworkers, and previous healthcare interactions by the time they present at pain clinics.11,15,48 Some patients may interpret mental health screening as potentially discrediting perhaps reflecting provider's doubts as to the legitimacy of self-reported pain.32,62,75,79 Patients may also fear that acknowledging mental health comorbidity will reduce the likelihood of being prescribed opioids. The heightened mental health treatment stigma experienced by patients with chronic pain may lead many patients to resist the conceptualization of their chronic pain as having any emotional or mental components.11,32,73
4.4. Low accessibility and feasibility of mental health treatment
For U.S. adults living with chronic pain who acknowledge mental health symptoms and are theoretically amenable to treatment, accessibility may still present some challenges. People living with chronic pain may have numerous medical appointments and medications that must be managed, yet time and disposable finances available for the pursuit of healthcare are finite. Secondly, mobility limitations associated with chronic pain may form a barrier to in-person mental health care visits. Finally, chronic pain may be more prevalent in rural and underserved communities,108 which also disproportionately experience shortages of mental health providers,35 health providers trained in pain management,80 and lack access to integrated models of care.28
4.5. Low engagement and retention in mental health treatment
Few mental health providers are trained in chronic pain,9,28,41 potentially limiting the mental health treatment engagement and retention of those living with chronic pain. Patients may be willing to try mental health treatment but experience that the care is not responsive to their needs. Achieving culturally and linguistically appropriate mental health treatment may be more challenging, without providers trained in culturally and linguistically appropriate pain care.55,98 Providers may experience that patients living with chronic pain are among their most interpersonally challenging patients.61,94,95 Owing to low confidence and/or competency to address physical pain,28 mental health providers may disproportionately fail to perceive treatment benefits or more often discontinue mental health treatment of patients living with chronic pain.
4.6. Incomplete implementation of effective mental health treatments
Randomized controlled trials support the effectiveness of psychiatric medication protocols and psychological interventions tailored specifically for those with chronic pain.28,41 However, only a small proportion of U.S. adults living with chronic pain likely receive mental health treatment that is designed to address the needs of those with chronic pain.
4.7. Issues in the assessment of anxiety and depression
Studies suggest that overlapping symptoms between chronic pain and anxiety/depression could lead to an inflated rate of positive screens for depression and anxiety among patients with high-impact chronic pain seeking pain specialist treatment.1,52 Further research should investigate whether these issues might also influence the measurement of anxiety and depression among those living with chronic pain in the U.S. adult general population.
Chronic pain is an aversive experience, and chronic pain is known to contribute to the development or exacerbation of anxiety or depression. Logically, it follows that fully eliminating the mental health disparities between those with and without chronic pain may not be realistically attainable. Still, the question remains open as to whether the bleak portrait presented above represents the best mental health outcomes possible for those living with chronic pain.
5. Limitations
The data used in this analysis are cross-sectional and no inferences can be made about directional causality. The NHIS does not include persons with no permanent address, active-duty military personnel, persons in long-term care or correctional facilities, or U.S. expatriates; noninstitutional homeless shelters and group homes are included.70 While our measurement is identical to the clinical definitions for ICD-11 classification of chronic pain, and the GAD-7 and PHQ-8 are diagnostic screeners widely used in clinical settings, it is possible that the self-reported diagnostic data could be less accurate when collected by the National Health Interview Survey vs a clinician. The data set allowed direct assessment of treatment intentions for survey respondents who used mental health medication; for those who used only nonpharmacological mental health treatment approaches, indirect intent-to-treat measurement was used.
6. Conclusion
To summarize, this study found that the U.S. mental health care and social services system does not equitably address the mental health needs of U.S. adults living with chronic pain and is not fully equipped to educate, screen, successfully navigate to care, and adequately address their needs. In the United States, there is a consensus view that the number of individuals with unremitted anxiety and depression is unacceptably high: elected officials, policymakers, and advocates often refer to the worsening mental health among U.S. adults as a crisis warranting urgent action.2,12,60,81 This study found that chronic pain is an experience shared by an underrecognized majority of all U.S. adults experiencing clinically significant unremitted anxiety and depression symptoms. Among those with unmet mental health needs, co-occurring chronic pain is not the exception, it is the rule. Yet, chronic pain remains infrequently included in the national mental health conversation. We suggest that meaningful engagement with the mental health experiences and outcomes of those living with chronic pain should become a cornerstone of mental health policy going forward; furthermore, a concerted examination of the role chronic pain plays in our national mental health crisis represents a potentially transformative scientific and policy opportunity. Building the U.S. healthcare system's capacity to address co-occurring chronic pain and mental health challenges holds promise for interrupting preventable progressions to high-impact chronic pain, new or exacerbated substance use disorders, and, potentially, the morbidity and mortality associated with the use of opioids.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Appendix A. Supplemental digital content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/C97.
Supplemental video content
A video abstract associated with this article can be found on the PAIN Web site.
Supplementary Material
Acknowledgements
Funding for this study was provided by the Comprehensive Center for Pain & Addiction, University of Arizona Health Sciences.
Data availability: No original data sets were generated over the course of this research; this is a secondary analysis of survey data. All data used in this study are publicly available on the National Health Interview Survey website.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painjournalonline.com).
Contributor Information
Mohab M. Ibrahim, Email: mohab@arizona.edu.
Alicia M. Allen, Email: aliciaallen@arizona.edu.
References
- [1].Aagaard A, Ravn SL, Andersen TE, Vaegter HB. Interpretation of the patient health questionnaire 9 in high-impact chronic pain: do we measure depressive symptoms the way we think? Clin J Pain 2023;39:501–15. [DOI] [PubMed] [Google Scholar]
- [2].Alegría M, Frank RG, Hansen HB, Sharfstein JM, Shim RS, Tierney M. Transforming mental health and addiction services. Health Aff (Millwood) 2021;40:226–34. [DOI] [PubMed] [Google Scholar]
- [3].Ali MK, Bullard KM, Gregg EW, Del Rio C. A cascade of care for diabetes in the United States: visualizing the gaps. Ann Intern Med 2014;161:681–9. [DOI] [PubMed] [Google Scholar]
- [4].Allen B, Nolan ML, Paone D. Underutilization of medications to treat opioid use disorder: what role does stigma play? Substance Abuse 2019;40:459–65. [DOI] [PubMed] [Google Scholar]
- [5].Allen-Watts K, Sims AM, Buchanan TL, DeJesus DJB, Quinn TL, Buford TW, Goodin BR, Rumble DD. Sociodemographic differences in pain medication usage and healthcare provider utilization among adults with chronic low back pain. Front Pain Res (Lausanne, Switzerland) 2021;2:806310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Andrykowski MA, Goedendorp MM. Distress and mental health care and medication use among survivors of multiple primary cancer diagnoses: findings from the 2016 National Health Interview Survey. J Psychosom Res 2020;134:110137. [DOI] [PubMed] [Google Scholar]
- [7].Arega MA, Dee EC, Muralidhar V, Nguyen PL, Franco I, Mahal BA, Sanford NN. Psychological distress and access to mental health services among cancer survivors: a national health interview survey analysis. J Gen Intern Med 2021;36:3243–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Balaraman KK, Dan S, Ortega N, Srinivasan M, Palaniappan L, Singh J, Chung S, Joshi SV. Psychological distress and mental health service utilization disparities in disaggregated Asian American populations, 2006–2018. Asian Am J Psychol 2023;14:239–49. [Google Scholar]
- [9].Balon R, Morreale MK, Coverdale JH, Brenner A, Louie AK, Beresin EV, Guerrero APS, Roberts LW. The role of psychiatric education in pain management. Acad Psychiatry 2018;42:587–91. [DOI] [PubMed] [Google Scholar]
- [10].Bao Y, Sturm R, Croghan TW. A national study of the effect of chronic pain on the use of health care by depressed persons. Psychiatr Serv 2003;54:693–7. [DOI] [PubMed] [Google Scholar]
- [11].Bean DJ, Dryland A, Rashid U, Tuck NL. The determinants and effects of chronic pain stigma: a mixed methods study and the development of a model. J Pain 2022;23:1749–64. [DOI] [PubMed] [Google Scholar]
- [12].Becerra X, Palm A, Haffajee RL, Contreras J, Barkoff A, O'Connell D, Valdez RO, Walensky RP, Brooks-LaSure C, Califf RM, Johnson C, Tso R, Tabak LA, Levine RL, Tripathi M, Delphin-Rittmon M, Murthy VH. Addressing the nation's behavioral health crisis: an HHS roadmap to integrate behavioral health. Health Aff Forefr. 2022. Available at: https://www.healthaffairs.org/content/forefront/addressing-nations-behavioral-health-crisis-hhs-roadmap-integrate-behavioral-health
- [13].Blumberg SJ. Racial and Ethnic Disparities in Men's Use of Mental Health Treatments, 2015. [PubMed] [Google Scholar]
- [14].Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: a prevalence study. PAIN 2001;89:127–34. [DOI] [PubMed] [Google Scholar]
- [15].Boring BL, Walsh KT, Nanavaty N, Mathur VA. Shame mediates the relationship between pain invalidation and depression. Front Psychol 2021;12:743584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Borkan J, Reis S, Hermoni D, Biderman A. Talking about the pain: a patient-centered study of low back pain in primary care. Soc Sci Med 1995;40:977–88. [DOI] [PubMed] [Google Scholar]
- [17].Braden JB, Zhang L, Fan M-Y, Unützer J, Edlund MJ, Sullivan MD. Mental health service use by older adults: the role of chronic pain. Am J Geriatr Psychiatry 2008;16:156–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bushnell MC, Čeko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci 2013;14:502–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Caraballo C, Massey D, Mahajan S, Lu Y, Annapureddy AR, Roy B, Riley C, Murugiah K, Valero-Elizondo J, Onuma O, Nunez-Smith M, Forman HP, Nasir K, Herrin J, Krumholz HM. Racial and ethnic disparities in access to health care among adults in the United States: a 20-year national health interview survey analysis, 1999–2018. JAMA 2021;326:637–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Carnago L, O'Regan A, Hughes JM. Diagnosing and treating chronic pain: are we doing this right? J Prim Care Commun Health 2021;12:21501327211008055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chaudhry MM, Banta JE, McCleary K, Mataya R, Banta JM. Psychological distress, structural barriers, and health services utilization among U.S. adults: national Health interview survey, 2011–2017. Int J Ment Health 2022;52:452–72. [Google Scholar]
- [22].Cochran SD, Björkenstam C, Mays VM. Sexual orientation differences in functional limitations, disability, and mental health services use: results from the 2013–2014 National Health Interview Survey. J Consult Clin Psychol 2017;85:1111–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Coombs NC, Meriwether WE, Caringi J, Newcomer SR. Barriers to healthcare access among U.S. adults with mental health challenges: a population-based study. SSM Popul Health 2021;15:100847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Csupak B, Sommer JL, Jacobsohn E, El-Gabalawy R. A population-based examination of the co-occurrence and functional correlates of chronic pain and generalized anxiety disorder. J Anxiety Disord 2018;56:74–80. [DOI] [PubMed] [Google Scholar]
- [25].Cunningham R, Imlach F, Haitana T, Every-Palmer S, Lacey C, Lockett H, Peterson D. It's not in my head: a qualitative analysis of experiences of discrimination in people with mental health and substance use conditions seeking physical healthcare. Front Psychiatry 2023;14:1285431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Currie SR, Wang J. Chronic back pain and major depression in the general Canadian population. PAIN 2004;107:54–60. [DOI] [PubMed] [Google Scholar]
- [27].Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, Kerns R, Von Korff M, Porter L, Helmick C. Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. MMWR Morbid Mortal Weekly Report 2018;67:1001–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Darnall BD, Scheman J, Davin S, Burns JW, Murphy JL, Wilson AC, Kerns RD, Mackey SC. Pain psychology: a global needs assessment and national call to action. Pain Med 2016;17:250–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Darnall B. To treat pain, study people in all their complexity. Nature 2018;557:7–8. [DOI] [PubMed] [Google Scholar]
- [30].de Heer EW, Gerrits MMJG, Beekman ATF, Dekker J, van Marwijk HWJ, de Waal MWM, Spinhoven P, Penninx BWJH, van der Feltz-Cornelis CM. The association of depression and anxiety with pain: a study from NESDA. PLoS One 2014;9:e106907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].De La Rosa JS, Brady BR, Ibrahim MM, Herder KE, Wallace JS, Padilla AR, Vanderah TW. Co-occurrence of chronic pain and anxiety/depression symptoms in U.S. adults: prevalence, functional impacts, and opportunities. PAIN 2024;165:666–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. PAIN 2016;157:1607–10. [DOI] [PubMed] [Google Scholar]
- [33].Demyttenaere K, Bruffaerts R, Lee S, Posada-Villa J, Kovess V, Angermeyer MC, Levinson D, de Girolamo G, Nakane H, Mneimneh Z, Lara C, de Graaf R, Scott KM, Gureje O, Stein DJ, Haro JM, Bromet EJ, Kessler RC, Alonso J, Von Korff M. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. PAIN 2007;129:332–42. [DOI] [PubMed] [Google Scholar]
- [34].Duca LM, Helmick CG, Barbour KE, Nahin RL, Von Korff M, Murphy LB, Theis K, Guglielmo D, Dahlhamer J, Porter L, Falasinnu T, Mackey S. A review of potential national chronic pain surveillance systems in the United States. J Pain 2022;23:1492–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Eaton LH, Langford DJ, Meins AR, Rue T, Tauben DJ, Doorenbos AZ. Use of self-management interventions for chronic pain management: a comparison between rural and nonrural residents. Pain Manag Nurs 2018;19:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA, Maher CG, Lancet Low Back Pain Series Working Group, Hartvigsen J, Cherkin D, Foster NE, Maher CG, Underwood M, Tulder Mvan, Anema JR, Chou R, Cohen SP, Costa LM, Croft P, Ferreira M, Ferreira PH, Fritz JM, Genevay S, Gross DP, Hancock MJ, Hoy D, Karppinen J, Koes BW, Kongsted A, Louw Q, Öberg B, Peul WC, Pransky G, Schoene M, Sieper J, Smeets RJ, Turner JA, Woolf A. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet (London, England) 2018;391:2368–83. [DOI] [PubMed] [Google Scholar]
- [37].Frank RG, Huskamp HA, Pincus HA. Aligning incentives in the treatment of depression in primary care with evidence-based practice. Psychiatr Serv 2003;54:682–7. [DOI] [PubMed] [Google Scholar]
- [38].Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis 2011;52:793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Gerrits MMJG, Vogelzangs N, van Oppen P, van Marwijk HWJ, van der Horst H, Penninx BWJH. Impact of pain on the course of depressive and anxiety disorders. PAIN 2012;153:429–36. [DOI] [PubMed] [Google Scholar]
- [40].Glenton C. Chronic back pain sufferers—striving for the sick role. Soc Sci Med 2003;57:2243–52. [DOI] [PubMed] [Google Scholar]
- [41].Goesling J, Lin LA, Clauw DJ. Psychiatry and pain management: at the intersection of chronic pain and mental health. Curr Psychiatry Rep 2018;20:12. [DOI] [PubMed] [Google Scholar]
- [42].Gonzales G, Przedworski J, Henning-Smith C. Comparison of health and health risk factors between lesbian, gay, and bisexual adults and heterosexual adults in the United States: results from the national health interview survey. JAMA Intern Med 2016;176:1344–51. [DOI] [PubMed] [Google Scholar]
- [43].Gu JK, Charles LE, Allison P, Violanti JM, Andrew ME. Mental health treatment reported by US workers before and during the COVID-19 pandemic: United States (2019–2020). Int J Environ Res Public Health 2022;20:651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: a world health organization study in primary care. JAMA 1998;280:147–51. [DOI] [PubMed] [Google Scholar]
- [45].Gureje O, Von Korff M, Kola L, Demyttenaere K, He Y, Posada-Villa J, Lepine JP, Angermeyer MC, Levinson D, de Girolamo G, Iwata N, Karam A, Guimaraes Borges GL, de Graaf R, Browne MO, Stein DJ, Haro JM, Bromet EJ, Kessler RC, Alonso J. The relation between multiple pains and mental disorders: results from the World Mental Health Surveys. PAIN 2008;135:82–91. [DOI] [PubMed] [Google Scholar]
- [46].Haber N, Pillay D, Porter K, Bärnighausen T. Constructing the cascade of HIV care: methods for measurement. Curr Opin HIV AIDS 2016;11:102–8. [DOI] [PubMed] [Google Scholar]
- [47].Hewitt M, Rowland JH. Mental health service use among adult cancer survivors: analyses of the national health interview survey. J Clin Oncol 2002;20:4581–90. [DOI] [PubMed] [Google Scholar]
- [48].Holloway I, Sofaer-Bennett B, Walker J. The stigmatisation of people with chronic back pain. Disabil Rehabil 2007;29:1456–64. [DOI] [PubMed] [Google Scholar]
- [49].Johnson K, Williams AR, Chalk M. Making the opioid use disorder cascade of care A reality, despite data limitations. Health Aff Forefr. 2018. Available at: https://www.healthaffairs.org/content/forefront/making-opioid-use-disorder-cascade-care-reality-despite-data-limitations
- [50].Jones LP. Anxiety, as experienced by chronic pain patients. J Relig Health 1985;24:209–17. [DOI] [PubMed] [Google Scholar]
- [51].Kay ES, Batey DS, Mugavero MJ. The HIV treatment cascade and care continuum: updates, goals, and recommendations for the future. AIDS Res Ther 2016;13:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Kha TV, Stenager E, Hoang H, Bruun-Plesner K, Fuglsang KS, Søgaard la Cour B, Handberg G, Vaegter HB. Preliminary validity and test–retest reliability of two depression questionnaires compared with a diagnostic interview in 99 patients with chronic pain seeking specialist pain treatment. Scand J Pain 2020;20:717–26. [DOI] [PubMed] [Google Scholar]
- [53].Khalid L, Cunningham CO, Deng Y, Masyukova M, Bumol J, Valle A, Zhang C, Lu T. Cascade of care for office-based buprenorphine treatment in Bronx community clinics. J Subst Abuse Treat 2022;139:108778. [DOI] [PubMed] [Google Scholar]
- [54].Kirsh KL. Differentiating and managing common psychiatric comorbidities seen in chronic pain patients. J Pain Palliat Care Pharmacother 2010;24:39–47. [DOI] [PubMed] [Google Scholar]
- [55].Kohrt BA, Griffith JL, Patel V. Chronic pain and mental health: integrated solutions for global problems. PAIN 2018;159(suppl 1):S85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord 2009;114:163–73. [DOI] [PubMed] [Google Scholar]
- [57].Lee KJ, Tilling KM, Cornish RP, Little RJA, Bell ML, Goetghebeur E, Hogan JW, Carpenter JR, STRATOS initiative. Framework for the treatment and reporting of missing data in observational studies: the Treatment and Reporting of Missing data in Observational Studies framework. J Clin Epidemiol 2021;134:79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Lee YJ, Palmer J, Cline AC, Lee H. Factors influencing the health care utilization among people with depression and/or anxiety symptoms. J Am Psychiatr Nurses Assoc 2023:10783903231197655. doi: 10.1177/10783903231197655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Little RJA, Rubin DB. Statistical analysis with missing data. 3rd ed. Hoboken, NJ: Wiley, 2019. [Google Scholar]
- [60].Lopes L, Kirzinger A, Sparks G, Stokes M, Published MB. KFF/CNN mental health in America survey—findings—10015. KFF, 2022. Available at: https://www.kff.org/report-section/kff-cnn-mental-health-in-america-survey-findings/. Accessed January 30, 2024. [Google Scholar]
- [61].Matthias MS, Parpart AL, Nyland KA, Huffman MA, Stubbs DL, Sargent C, Bair MJ. The patient–provider relationship in chronic pain care: providers' perspectives. Pain Med 2010;11:1688–97. [DOI] [PubMed] [Google Scholar]
- [62].McManimen S, McClellan D, Stoothoff J, Gleason K, Jason LA. Dismissing chronic illness: a qualitative analysis of negative health care experiences. Health Care Women Int 2019;40:241–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Meyerson BE, Russell DM, Downer M, Alfar A, Garnett I, Lowther J, Lutz R, Mahoney A, Moore J, Nuñez G, Samorano S, Brady BR, Bentele KG, Granillo B, Arizona Drug Policy Research & Advocacy Board. Opportunities and challenges: hepatitis C testing and treatment access experiences among people in methadone and buprenorphine treatment during COVID-19, Arizona, 2021. AJPM Focus 2022;2:100047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Mills S, Torrance N, Smith BH. Identification and management of chronic pain in primary care: a review. Curr Psychiatry Rep 2016;18:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Mukaka M, White SA, Terlouw DJ, Mwapasa V, Kalilani-Phiri L, Faragher EB. Is using multiple imputation better than complete case analysis for estimating a prevalence (risk) difference in randomized controlled trials when binary outcome observations are missing? Trials 2016;17:341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain 2015;16:769–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Nahin RL. Use of multimodal multidisciplinary pain management in the US. JAMA Netw Open 2022;5:e2240620. [DOI] [PubMed] [Google Scholar]
- [68].Narcisse M-R, Andersen JA, Felix HC, Hayes CJ, Eswaran H, McElfish PA. Factors associated with telehealth use among adults in the United States: findings from the 2020 national health interview survey. J Telemed Telecare 2022:1357633X221113192. Available at: https://journals.sagepub.com/doi/full/10.1177/1357633X221113192. Accessed October 4, 2023. [DOI] [PubMed] [Google Scholar]
- [69].National Center for Health Statistics. National health interview survey English brochure, 2019. Available at: https://www.cdc.gov/nchs/nhis/participants/survey-brochure.htm. Accessed July 7, 2023. [Google Scholar]
- [70].National Center for Health Statistics. Survey description, national health interview survey, 2019. Hyattsville, MD: National Center for Health Statistics, 2020. [Google Scholar]
- [71].National Center for Health Statistics. National health interview survey, 2019. Public-use data file and documentation. Available at: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm.2020. Accessed January 10, 2023. [Google Scholar]
- [72].National Health Interview Survey. (NHIS)—healthy people 2030; health.gov. Available at: https://health.gov/healthypeople/objectives-and-data/data-sources-and-methods/data-sources/national-health-interview-survey-nhis. Accessed October 4, 2023. [Google Scholar]
- [73].Naushad N, Dunn LB, Muñoz RF, Leykin Y. Depression increases subjective stigma of chronic pain. J Affect Disord 2018;229:456–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Nekovarova T, Yamamotova A, Vales K, Stuchlik A, Fricova J, Rokyta R. Common mechanisms of pain and depression: are antidepressants also analgesics? Front Behav Neurosci 2014;8:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Newton BJ, Southall JL, Raphael JH, Ashford RL, LeMarchand K. A narrative review of the impact of disbelief in chronic pain. Pain Manag Nurs 2013;14:161–71. [DOI] [PubMed] [Google Scholar]
- [76].Nissen A, Hynek KA, Scales D, Hilden PK, Straiton M. Chronic pain, mental health and functional impairment in adult refugees from Syria resettled in Norway: a cross-sectional study. BMC Psychiatry 2022;22:571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].O'Donnell M, Mathema B. Expanding the tuberculosis cascade of care to treat undiagnosed and subclinical tuberculosis in high-burden settings. Am J Respir Crit Care Med 2022;205:149–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Onwumere J, Stubbs B, Stirling M, Shiers D, Gaughran F, Rice ASC, C de C Williams A, Scott W, Scott W. Pain management in people with severe mental illness: an agenda for progress. PAIN 2022;163:1653–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Osborn M, Rodham K. Insights into pain: a review of qualitative research. Rev Pain 2010;4:2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Reichert A, Jacobs R. The impact of waiting time on patient outcomes: evidence from early intervention in psychosis services in England. Health Econ 2018;27:1772–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Reinert M, Fritze D, Nguyen T. The state of mental health in America. Alexandria, VA: Mental Health America, 2022. [Google Scholar]
- [82].Rhodes LA, McPhillips-Tangum CA, Markham C, Klenk R. The power of the visible: the meaning of diagnostic tests in chronic back pain. Soc Sci Med 1999;48:1189–203. [DOI] [PubMed] [Google Scholar]
- [83].Shavers VL, Bakos A, Sheppard VB. Race, ethnicity, and pain among the U.S. adult population. J Health Care Poor Underserved 2010;21:177–220. [DOI] [PubMed] [Google Scholar]
- [84].Siqueira JLD, Morete MC. Psychological assessment of chronic pain patients: when, how and why refer? Revista Dor 2014;15:51–4. [Google Scholar]
- [85].Smit T, Rogers AH, Garey L, Allan NP, Viana AG, Zvolensky MJ. Anxiety sensitivity and pain intensity independently predict opioid misuse and dependence in chronic pain patients. Psychiatry Res 2020;294:113523. [DOI] [PubMed] [Google Scholar]
- [86].Socías ME, Volkow N, Wood E. Adopting the ‘cascade of care’ framework: an opportunity to close the implementation gap in addiction care? Addiction (Abingdon, England) 2016;111:2079–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. [DOI] [PubMed] [Google Scholar]
- [88].Subbaraman R, Nathavitharana RR, Mayer KH, Satyanarayana S, Chadha VK, Arinaminpathy N, Pai M. Constructing care cascades for active tuberculosis: a strategy for program monitoring and identifying gaps in quality of care. PLoS Med 2019;16:e1002754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Teh CF, Zaslavsky AM, Reynolds CFI, Cleary PD. Effect of depression treatment on chronic pain outcomes. Psychosom Med 2010;72:61–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Terlizzi EPNT. Mental health treatment among adults: United States, 2020. Hyattsville, MD: National Center for Health Statistics, 2021. Available at: https://www.cdc.gov/nchs/data/databriefs/db419.pdf. Accessed August 21, 2023. [Google Scholar]
- [91].Thomeer MB, Moody MD, Yahirun J. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J Racial Ethn Health Disparities 2023;10:961–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA, Kaasa S, Korwisi B, Kosek E, Lavand’homme P, Nicholas M, Perrot S, Scholz J, Schug S, Smith BH, Svensson P, Vlaeyen JWS, Wang S-J. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11). PAIN 2019;160:19–27. [DOI] [PubMed] [Google Scholar]
- [93].Tunks ER, Crook J, Weir R. Epidemiology of chronic pain with psychological comorbidity: prevalence, risk, course, and prognosis. Can J Psychiatry 2008;53:224–34. [DOI] [PubMed] [Google Scholar]
- [94].Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med 2006;21:652–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Upshur CC, Bacigalupe G, Luckmann R. “They don't want anything to do with you”: patient views of primary care management of chronic pain. Pain Med 2010;11:1791–8. [DOI] [PubMed] [Google Scholar]
- [96].Von Korff M, Crane P, Lane M, Miglioretti DL, Simon G, Saunders K, Stang P, Brandenburg N, Kessler R. Chronic spinal pain and physical–mental comorbidity in the United States: results from the national comorbidity survey replication. PAIN 2005;113:331–9. [DOI] [PubMed] [Google Scholar]
- [97].Walker J, Holloway I, Sofaer B. In the system: the lived experience of chronic back pain from the perspectives of those seeking help from pain clinics. PAIN 1999;80:621–8. [DOI] [PubMed] [Google Scholar]
- [98].Wallace B, Varcoe C, Holmes C, Moosa-Mitha M, Moor G, Hudspith M, Craig KD. Towards health equity for people experiencing chronic pain and social marginalization. Int J Equity Health 2021;20:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Watkins DC, Johnson NC. Age and gender differences in psychological distress among African Americans and Whites: findings from the 2016 national health interview survey. Healthcare 2018;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Williams AR, Nunes EV, Bisaga A, Levin FR, Olfson M. Development of a Cascade of Care for responding to the opioid epidemic. Am J Drug Alcohol Abuse 2019;45:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Yehia BR, Schranz AJ, Umscheid CA, Lo Re V. The treatment cascade for chronic hepatitis C virus infection in the United States: a systematic review and meta-analysis. PLoS One 2014;9:e101554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Zablotsky B, Terlizzi EP. Mental health treatment among children aged 5-17 years: United States, 2019. NCHS data brief no. 381. National Center for Health Statistics, 2020. Available at: https://eric.ed.gov/?id=ED612069. Accessed October 4, 2023. [PubMed] [Google Scholar]
- [103].Zablotsky B, Weeks JD, Terlizzi EP, Madans JH, Blumberg SJ. Assessing anxiety and depression: a comparison of national health interview survey measures. Hyattsville, MD: National Center for Health Statistics, 2022. Available at: 10.15620/cdc:117491. Accessed January 10, 2023. [DOI] [PubMed] [Google Scholar]
- [104].Zajacova A, Grol-Prokopczyk H, Zimmer Z. Sociology of chronic pain. J Health Soc Behav 2021;62:302–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Zajacova A, Grol-Prokopczyk H, Fillingim R. Beyond Black vs White: racial/ethnic disparities in chronic pain including Hispanic, Asian, Native American, and multiracial US adults. PAIN 2022;163:1688–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Zajacova A, Grol-Prokopczyk H, Liu H, Reczek R, Nahin RL. Chronic pain among U.S. sexual minority adults who identify as gay, lesbian, bisexual, or “something else”. PAIN 2023;164:1942–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Zelaya C, Dahlhamer J, Lucas J, Connor E. Chronic pain and high-impact chronic pain among U.S. adults, 2019. Hyattsville, MD: National Center for Health Statistics, 2020. Available at: https://www.cdc.gov/nchs/data/databriefs/db390-H.pdf. Accessed February 25, 2023. [Google Scholar]
- [108].Zelaya CE, Dahlhamer JM, Lucas JW, Connor EricM. Chronic pain and high-impact chronic pain among U.S. adults, 2019. NCHS data brief no 390; 2020. Available at: https://stacks.cdc.gov/view/cdc/97308. Accessed March 28, 2024. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/C97.
A video abstract associated with this article can be found on the PAIN Web site.


