Abstract
A better understanding of how childhood adversity (CA) patterns influence the effectiveness of Trauma Informed Care (TIC) for youth in residential programs is needed. Utilizing a longitudinal design, the study examined how CA patterns influenced aggression and self-injurious behavior during treatment and emotional and conduct outcomes for 1,343 racially diverse adolescents in a TIC residential program. Latent class analysis identified five CA patterns. Subsequent mixed, two-factor ANCOVAs indicated youth from all CA patterns experienced parallel decreases in emotional problems from intake to discharge while changes in conduct problems during this same period differed by CA pattern. Likewise, Hierarchical Linear Modeling revealed that youths’ self-injurious behavior and aggressive behaviors over the first 12 months of the program also differed by CA pattern. Some demographic differences based on sex and race were found, which are discussed in turn. Findings indicate that while the program is functioning as TIC, more tailored support is needed for youth with specific CA patterns and demographics.
Keywords: Residential treatment, Trauma, Emotional problems, Aggression, Self-injurious behavior
An alarmingly high rate of youth in residential care have experienced childhood adversity (CA), with some prevalence rates as high as 92% (Briggs et al., 2012). Rates may be high because CA increases risk for problems for which youth are frequently admitted to residential care, including behavior problems, substance use, and suicidality (Briggs et al., 2012). While in residential care, youth with CA continue to experience functional and clinical impairment and are prone to poor treatment response (Brack et al., 2012; Briggs et al., 2012). Although youth with CA may benefit from trauma-informed care (TIC; Hodgdon et al., 2023), a better understanding of their needs could improve how TIC is approached in residential programs (Tyler et al., 2019, 2021). However, there is limited research on how CA pattern influences treatment response and outcomes (Sheridan et al., 2020). The current study examined how different CA patterns influenced youth’s behavior during a TIC residential program and their subsequent treatment outcomes.
Definition of childhood adversity (CA) and relationship to trauma
CA is “experiences that are likely to require significant adaptation by an average child and that represent a deviation from the expectable environment” and typically includes experiences such abuse, neglect, exposure to violence, and negative familial circumstances (McLaughlin, 2016, p. 363). Trauma is the stress and clinical impairment that result from CA (Felitti et al., 1998). Thus, youth may be exposed to a potentially traumatic event without incurring an acute trauma response, such as intrusive memories and/or clinical impairment (Berliner & Kolko, 2016). However, youth in this study tended to experience severe forms of CA that often generate trauma (Connell et al., 2018). Thus, while CA and trauma are related but different concepts, the terms are used interchangeably in this paper (see Kisiel et al., 2009).
Approaches to studying CA
There are multiple approaches to understanding how CA is linked to negative outcomes. The Cumulative Risk approach suggests that the wider a variety of CA experienced, the larger the negative impact (Evans et al., 2013; Felitti et al., 1998). Greater exposure to CA is consistently linked to greater impairment (Gordon et al., 2022; Tyler et al., 2021) and chronic exposure such as neglect or adverse events can lead to long-standing dysregulation of the stress response system (Shonkoff et al., 2012). CA may be linked to negative outcomes because it disrupts processes of healthy development (Shonkoff et al., 2012). However, the Cumulative Risk approach does not account for the impact of different types of trauma exposure, such as exposure to sexual abuse or neglect. Alternatively, the Dimensional Model of Adversity and Psychopathology posits there are two partially distinct dimensions of trauma exposure – threat and deprivation – that differentially impact development (McLaughlin & Sheridan, 2016). Indeed, CA type, not just quantity, differently predict negative outcomes and impairment (Connell et al., 2018). For example, neglect, which is a form of deprivation, is associated with cognitive deficits, perhaps due to limited sensory and social learning opportunities; alternatively, physical abuse and exposure to violence, which are forms of threat, are associated with increased sensitivity and emotion to threats, perhaps because these responses increase safety in dangerous environments (McLaughlin & Lambert, 2017).
To account for CA type and quantity, person-centered approaches, such as Latent Class Analysis (LCA), have been used to examine patterns of CA exposure. For example, Connell et al. (2018) found four CA subgroups among youth receiving residential care, with youth in high polyvictimization and moderate general polyvictimization groups most likely to report trauma-related stress. This aligns with theorizing that type and amount of CA impact impairment (Gordon et al., 2022). Using a similar LCA approach, Gordon et al. (2022) identified five patterns of CA exposure for youth in residential care: low exposure, familial dysfunction, neglect/emotional abuse, high exposure without sexual abuse, and high exposure with sexual abuse – which were uniquely associated with clinical functioning. For example, youth with high exposure with sexual abuse, but not those with high exposure without sexual abuse, experienced greater trauma symptoms and emotional problems when compared to youth in the low exposure group. This is consistent with previous research suggesting that sexual abuse is particularly harmful given that it is robustly linked to suicide attempts (Ng et al., 2018). Surprisingly, however, minimal research has examined how CA pattern influences response to residential care.
Associations between CA and residential programs outcomes
CA history can impact youth response to residential treatment (Boyer et al., 2009; Brack et al., 2012) and may increase risk for problematic behavior during care (Griffin et al., 2009; Zelechoski et al., 2013). For example, Boyer et al. (2009) found that the greater the variety of CA for a youth, the less likely a youth was to improve in residential treatment and that CA exposure was a stronger predictor of poor treatment response than all other variables, including length of stay and severity at admission. Although CA events can induce fight, flight, freeze, or fawn responses that may be adaptive and survival-oriented while enduring CA, such responses can be problematic when they are generalized to residential care facilities (Griffin et al., 2009). Additionally, how CA exposure impacts behavior while in residential treatment is not well understood. Although Tyler et al. (2019) found that youth with high trauma symptoms engaged in significantly more self-injurious behaviors than youth with low trauma symptoms, youth with high exposure to trauma – that is exposure to multiple CA incidents – unexpectedly engaged in fewer self-injurious behaviors than youth with low trauma exposure during the first month of residential treatment. However, this study did not look at specific types of CA. Research on how subtype of CA impacts behavior in residential treatment is even less clear, with most studies focused on how a history sexual abuse increases risk for problematic sexual behavior (e.g., Zelechoski et al., 2013). Therefore, more research is needed on how CA patterns impact outcomes and behavior in residential care.
Trauma-informed care and treating youth with CA
The need for services for youth with CA has been widely recognized and has resulted in many institutions adopting TIC. According to Substance Abuse and Mental Health Services Administration (SAMHSA), TIC is an approach which realizes the impact of and potential for recovery from trauma, recognizes trauma symptoms, and responds by integrating this knowledge into policies and practices (United States Department of Health and Human Services Substance Abuse and Mental Health Services Administration for Substance Abuse Treatment Center for Behavioral Health Statistics and Quality, 2014). In practice, TIC encompasses an institution-wide treatment approach that prioritizes safety and empowerment for youth and an awareness of how trauma influences wellbeing and behavior (Berliner & Kolko, 2016). TIC is promising for improving treatment outcomes in residential programs (Hodgdon et al., 2023; Tyler et al., 2019); however, there is debate whether TIC principles differ from general principles of good care and substantial heterogeneity with how TIC is implemented (Berliner & Kolko, 2016).
Understanding the influence of CA patterns on treatment is one avenue for more effective TIC. The amount of CA exposure can impact youth response to treatment (e.g., Boyer et al., 2009); however, despite evidence that different types of CA distinctly influence outcomes (e.g., Gordon et al., 2022), research on how specific patterns of CA exposure influence response to treatment is limited. Boyer et al. (2009) found that witnessing community violence was the only type of CA that uniquely predicted residential treatment outcomes, with youth who had witnessed community violence significantly more likely to deteriorate. However, results should be interpreted with caution given only 4.6% of those youth were exposed to community violence. To the authors’ knowledge, no research has examined how CA patterns influence residential treatment outcomes for youth – even though such research could provide valuable insight on how TIC programs could be tailored to address specific types of CA. For example, youth with histories of sexual abuse may require tailored interventions to reduce their risk of suicidality, while youth with histories of neglect may demonstrate unique cognitive functioning impairments and benefit from problem solving interventions (McLaughlin & Lambert, 2017; Ng et al., 2018).
Sex and race may also contribute to treatment response (Brack et al., 2012; Javdani et al., 2023). Girls consistently have more severe clinical problems entering residential treatment (Brack et al., 2012; Hodgdon et al., 2023); however, evidence regarding the impact of sex on treatment effectiveness is mixed, with girls responding worse, better, or just as well as boys to treatment (Brack et al., 2012; Hodgdon et al., 2023; Holtberg et al., 2016). Additionally, Black youth are at increased risk for restraints in residential care (Braun et al., 2020) and Black and Hispanic youth are more likely to be diagnosed with conduct disorder while in residential treatment than White youth (Cameron & Guterman, 2007). However, despite Black, Latinx and Indigenous youth representing approximately 70% of youth in residential care, there is limited research on how patient race influences their treatment (Javdani et al., 2023).
The current study
In sum, the amount and type of CA exposure may influence treatment response and outcomes, with youth who experience more types and more severe CA potentially demonstrating worse outcomes (Boyer et al., 2009; Gordon et al., 2022). Additionally, demographic variables, such as sex and race, may significantly impact how youth with CA exposure respond to residential treatment. While evidence on the impact of sex is mixed (Brack et al., 2012; Hodgdon et al., 2023; Holtberg et al., 2016), youth of color are overrepresented in residential care and more likely to be given a diagnosis of conduct disorder (Cameron & Guterman, 2007; Javdani et al., 2023). A better understanding of how CA pattern influences treatment response and outcomes are needed to improve TIC in youth residential programs. The current study addresses this gap by examining how CA patterns influenced youth’s response to treatment via aggressive and self-injurious behaviors during their first 12 months within a residential program and their emotional and conduct outcomes at the end of treatment. Aligning with our previous research using this sample (Gordon et al., 2022), five patterns of adversity were expected to emerge, including a low exposure CA group and several distinct CA groups characterized by familial dysfunction, maltreatment, sexual abuse, or high levels of overall trauma. It was expected that youth exposed to the most types of CA would demonstrate the most aggressive incidences. Given links between sexual abuse and suicide attempts (Ng et al., 2018), patterns with high levels of sexual abuse were expected to demonstrate the highest level of self-injurious behavior, referring to self-harm and suicidal ideation. It was expected that youth with patterns characterized by high CA and/or sexual abuse to demonstrate the worst treatment outcomes, given previous research on Cumulative Risk (e.g., Briggs et al., 2012; Evans et al., 2013) and sexual abuse (Ng et al., 2018). Given the prior literature on race and sex differences in residential treatment, they were included as covariates to control for the potential influence of these variables.
Materials and methods
Participants and data collection
Archival records were used. The sample included youth entering a midwestern family-style residential program for the first time between January 1, 2013 to August 1, 2020. The study used measures originally collected as part of the program’s routine intake assessments, direct observations of the youth’s behavior while in the residential program, and routine assessments of problem behavior upon exiting the program. The original sample comprised of 2,066 participants. Only participants with program outcome data (i.e., 1343 participants or 65% of the original sample) were included in the present study. Possible reasons for missing outcome data included sudden departures from the program (e.g., a hospitalization or early release from court mandate) or staff errors. An analysis of the demographics between those with and without outcome data (see Table S1 in the supplementary materials) indicated no group differences at admission for age, sex, or baseline emotional or behavioral problems as measured by the corresponding subscales on the Strengths and Difficulties Questionnaire, which is described below. However, those with outcome data tended to have longer program stay (12 months) than those without such data (10 months; [t (1852) = 5.38, p < .001]) and were less likely to be a minority (χ2 (7) 16.54, p = .02, see Table S1).
The sample was 9.11–18.63 years at intake (M = 15.63, SD = 1.53; 65.5% male). The sample was 47.8% White, 24.9% Black or African American, 12.4% Hispanic or Latinx, 9.6% multi-racial, and 5.4% other. Youth were commonly referred to the residential program by the court system (53%), a parent/guardian (36%), or a public social services agency (5%). Top presenting problems were difficulty following instructions of authority figures (85%), verbal aggression (81%), poor anger control (78%), being out of control of parental instruction (77%), relationship problems with peers (72%), and school behavior problems (68%). The average length of stay was 12.88 months (SD = 9.06). The study was approved by the Boys Town National Research Hospital Institutional Review Board (number: 20–17-x).
Program description
All youth received residential services as part of the Boys Town’s Family Home Program (Father Flanagan’s Boys’ Home, 2015). This program implements a modified trauma-informed version of the Teaching-Family Model, in which a married couple, referred to as Family Teachers, and, if applicable, their biological children reside with youth full time in a home (n = 6–8 per home) within a neighborhood full of other similar homes to teach pro-social, motivation, problem-solving, and self-government skills in a family-like environment (Thompson & Daly, 2015). At regular intervals, youth are prescribed tailored coping strategies, such as progressive muscle relaxation, and behavioral goals, such as “0 instances of physical aggression,” to improve behavior and well-being by Family Teachers guided by program Consultants, which were master’s- or doctorate-level professionals with degrees in mental health related fields. A token economy system is used to reinforce youth for demonstrating targeted social skills associated with their treatment objectives. During a typical week youth attend full time school in the program, participate in extracurricular activities, attend a family meeting within their program home, use their points to buy privileges, such as video game time, and may attend individual or group therapy sessions with Master’s and PhD level clinicians. Throughout the program youth may also participate in family therapy and have regular meetings with their primary caregivers outside of the program to discuss treatment progress. Multiple TIC components are implemented within the Family Home Program (see USDHHS, 2014) including an institution-wide emphasis on ensuring youth feel physically and emotionally safe within a calm and nurturing environment. All staff, including therapist, family teachers, behavioral assistants, received training on the multiple types of trauma youth experience, its impact, and appropriate responses to trauma reactions, such as remaining calm and helping youth regulate. Specific strategies implemented by staff include positive reinforcement to youth for using skills within the program both informally and via the token economy system and working with youth and their families to promote their empowerment and their skills related to self-advocacy, conflict resolution, healthy decision-making, stress management skills, and emotional regulation (FFBH, 2015). After completing the program youth either return to residing with a legal guardian or receive a new placement. Youth who age into adulthood during the program participate in transitional programs designed to ease them into career training such as college, trade school, and apprenticeships and independent living.
Measures
Adverse childhood experiences
Exposure to adverse childhood experiences at intake was measured according to 10 items (see Tyler et al., 2019 for detailed procedures) adapted from the Adverse Childhood Experiences study (Felitti et al., 1998). These included emotional, physical, and sexual abuse, one global type of neglect, and six exposures to household dysfunction: domestic violence, household substance use, household mental health issues, parent relationship problems, a criminal household member, and abandonment. At intake, staff indicated whether youth had been exposed to these 10 adverse events (0 = no, 1 = yes) based on the youth records at admission which included their social history, a psychological evaluation, and interviews with the youth and their parent/guardian.
Outcome measures
Conduct and emotional problems: strengths and difficulties questionnaire
Youth conduct and emotional problems at intake and discharge were assessed using the emotional and conduct problem subscales from the Strengths and Difficulties Questionnaire (Goodman et al., 1998). It is a 25-item questionnaire which assesses child behavioral and emotional problems using five subscales composed of five items: emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems, and prosocial behavior. At intake, the youth’s parent/guardian rated each statement on a 3-point Likert-type scale ranging from 0 (not true) to 2 (certainly true). Items from each subscale are summed. Only the emotional problems – which included anxiety and depressive symptoms – and conduct problems – which included behaviors such as fighting, stealing, and lying – subscales were used in the current study. Scores ranging from 5 to 10 for emotional problems and from 4 to 10 for conduct problems are considered clinically significant. At discharge, the measure was completed by the Family-Teachers as they were more familiar with youth daily behavior during that period. The Strengths and Difficulties Questionnaire is a well-established measure with acceptable reliability and validity in children and adolescents (Goodman, 2001).
Self-injurious behavior and aggressive behavior: daily incident report
Direct observation of behaviors gathered from the Daily Incident Report is the principal measure of change while in the program. It is a daily log of all significant events including self-injurious behavior and aggression that occur in the program. Each recorded incident includes a descriptive narrative of the event and at least one behavioral code, such as “self-destructive behavior” or “physical aggression.” Direct-care staff report significant behaviors to their clinical supervisors daily who review it for completeness and accuracy. All direct-care staff receive in-person training and ongoing consultation about reportable behaviors. The narrative description of each incident is assigned one or more pre-defined behavioral codes. Each code has been operationalized via a brief description of the code along with a prototypical example, such as “physical assault [on staff]): youth assaults a staff member.” The entire coded narrative is reviewed by senior clinical supervisors to ensure accuracy. The Daily Incident Report data in this study was not examined for inter-rater reliability, but previous studies indicate that it possesses good to excellent reliability at both the level of reporting and coding the narrative descriptions. For example, Wright (2001) found an 83.5% inter-judge agreement in regards to the “reportability” of behavior between direct-care staff responding to 43 scenarios. Finally, Larzelere (1996) found Kappa coefficients between .66 and .97 for codes assigned to the same incident narratives.
For this study, incident codes were used which were representative of self-injurious and aggressive behavior. Self-injurious behaviors were the sum of three incident codes: (1) self-destructive behavior, such as scratching, cutting self, intentionally walking into traffic, or self-mutilation; (2) suicide ideation, which included any verbalization, such as saying “I wish I were dead,” behavior, such as extreme mood swings or social withdrawal or isolation, gesture, such as pretending to slash throat, and an elevated Suicide Probability Score; and (3) suicide attempt which included when a youth attempted suicide. Aggressive behaviors were the sum of five incident codes: verbal symbolic aggression, physical aggression, property damage, physical assault on adult, physical assault on youth.
Data analytic plan
A latent class analysis (LCA) was performed to identify the CA patterns. To eliminate bias when identifying subgroups with similar exposure to CA, an inclusive LCA method was followed (Bray et al., 2015). See Gordon et al. (2022) for a detailed description of this method. The latent class membership was treated as a manifest categorical variable and conducted a mixed, two-factor Analysis of Covariance (ANCOVA; i.e., time by CA pattern) to explore if CA patterns moderated youth’s emotional problems and aggressive behaviors from intake to discharge. Finally, Hierarchical Linear Modeling (HLM) was performed to explore possible CA pattern differences in the change of self-injurious and aggressive behavior incidents over the first the 12 months of the program. Stata 15 and the LCA Stata Plugin Version 1.2 (Lanza et al., 2015) were used to estimate all LCA models. To aid with model selection, the LCA Bootstrap Stata function was used (Huang et al., 2016) to perform a Bootstrap likelihood ratio test (BLRT). Software packages to conduct LCA are available for download free of charge at http://methodology.psu.edu. SPSS 25 and HLM6 were used to perform the ANOVA and HLM analyses.
Results
Descriptive statistics
Table 1 presents youth demographic, CA frequencies, and mean scores for emotional problems, conduct problems, and self-injurious and aggressive behaviors at intake and discharge. About 8% of youth did not have any CA exposure with 21.6% reporting six or more CA exposures. T-test analyses revealed that youth displayed decreases in emotional problems (Mean Difference = −.93, SE =.08, t[1341] = −11.44, p < .001) and conduct problems (Mean Difference = −.90, SE =.09, t[1341] = −9.72, p < .001) from intake to discharge.
Table 1.
Demographics, CA experiences, and clinical functioning among (masked) youth (N = 1343).
| N | % | ||
|---|---|---|---|
| Sex | Female | 464 | 34.5% |
| Male | 879 | 65.5% | |
| Ethnicity | Black/African American | 334 | 24.9% |
| Asiana | 13 | 1.0% | |
| Hispanic/Latinx | 166 | 12.4% | |
| Multiracial | 129 | 9.6% | |
| Native American | 53 | 4.0% | |
| White | 642 | 47.8% | |
| Unknown | 6 | 0.4% | |
| Cumulative CAs | 1 | 201 | 15.0% |
| 2 | 190 | 14.1% | |
| 3 | 216 | 16.1% | |
| 4 | 205 | 15.3% | |
| 5 | 139 | 10.3% | |
| 6+ | 290 | 21.6% | |
| CA Indicators | Parental Discord | 777 | 58.10% |
| Parental Substance Abuse | 744 | 55.60% | |
| Verbal/Emotional Abuse | 738 | 55.20% | |
| Parental Crime | 473 | 35.40% | |
| Abandonment | 466 | 34.80% | |
| Neglect | 436 | 32.60% | |
| Family Mental Illness | 360 | 26.90% | |
| Physical Abuse | 352 | 26.30% | |
| Domestic Violence | 282 | 21.10% | |
| Sexual Abuse | 215 | 16.10% | |
| Mean | SD | ||
| Age at Admission | 15.62 | 1.53 | |
| Average Daily Incidents Reported in 1st Twelve Months | Self-Injurious Behaviors | .23 | .72 |
| Aggressive Behaviors | 1.21 | 2.18 | |
| Emotional Problems | Admission | 3.82 | 2.52 |
| Discharge | 2.88 | 2.50 | |
| Conduct Problems | Admission | 4.82 | 2.65 |
| Discharge | 3.92 | 2.95 |
Note:
For ethnicity, the Asian category includes Asian and Pacific Islander and Native Hawaiian.
Daily Incident Report
Given that most youth had no incidents on any given day, both self-injurious and aggressive behavior incidents are zero inflated. Thus, they were summed separately by month by youth for the first 12 months in the program. Thus, each youth could have up to 12 monthly self-injurious and aggressive behavior scores. The number of self-injurious behaviors per youth per month ranged from 0 to 13 (M = .16; SD = .72). The number of aggressive behaviors per youth per month ranged from 0 to 44 (M = .96; SD = 2.38). Even after aggregating daily data into monthly, the mode and median for both behaviors were 0. Thus, most youth did not engage in self-injurious or aggressive behaviors for most months.
Latent class analysis (LCA)
An inclusive LCA determined the youth’s CA pattern. In accordance with procedures for fitting an inclusive LCA model using LCA Stata Plugin Version 1.2, records with missing data for the covariates – sex and ethnicity – and clinical functioning, which includes emotional problems, conduct problems, self-injurious behavior, and aggressive behaviors, were eliminated listwise from the analysis. For information relevant for model selection see Table 2. The five-class model was selected because it had the smallest BIC and an Entropy value of .72, which is acceptable based on current recommended standards (see Table 3; Clark, 2010). The overall pattern of item-response probabilities for a particular class was used to inform the choice of label for that latent class. Based on posterior probabilities produced from the inclusive LCA model, the maximum-probability assignment method was used to classify participants into five adversity patterns: (1) low exposure, (2) familial dysfunction, (3) neglect/emotional abuse, which is called neglect for the remainder of the paper, (4) broad exposure, and (5) pervasive exposure. Note that in the original sample the two highest exposure groups were characterized by the absence or presence of sexual abuse (Gordon et al., 2022). Since this was not the case in the current study, the two highest exposure groups were labeled “broad” and “pervasive” based on the new item-response probabilities. See Table 4 for more details.
Table 2.
Summary of information for selecting number of latent classes of childhood adversity (N = 2,066a).
| Number of Latent Classes | Number of Parameters Estimated | G 2 | df | AIC | BIC | aBIC | Entropy | I | BLRT p-value |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 10 | 3526.2 | 1013 | 3446.2 | 3502.3 | 3470.6 | 1.00 | −12437.0 | - |
| 2 | 21 | 1594.1 | 1002 | 1636.1 | 1754.1 | 1687.3 | .71 | −11521.0 | <.001 |
| 3 | 32 | 1316.2 | 991 | 1380.2 | 1560.0 | 1458.3 | .77 | −11382.0 | <.001 |
| 4 | 43 | 1046.9 | 980 | 1132.9 | 1374.4 | 1237.8 | .68 | −11247.4 | <.001 |
| 5 | 54 | 957.8 | 969 | 1065.8 | 1369.2 | 1197.6 | .72 | −11202.8 | .001 |
| 6 | 65 | 895.1 | 958 | 1025.1 | 1390.2 | 1183.7 | .73 | −11171.5 | .001 |
Note: BLRT tested whether an LCA model with (k +1)-class is more adequate than the k-class model in describing the population which a particular sample came from. For example, the significant p-value indicated that the four-class model describes the population better than the three-class model. After conducting 999 bootstrap replications to reduce the random variability of the p-value, as recommended by Huang et al. (2016), we found that the BLRT for the six-class model was still significant (p < .001). However, the Entropy value – or classification error, with higher value (ranging from 0 to 1) indicating better classification (Celeux & Soromenho, 1996) – for the five-class model was 0.72, which is acceptable based on current recommended standards (Clark, 2010). Given the smallest BIC and the acceptable Entropy value, we selected the five-class model as the final model.
In accordance with inclusive LCA method recommended by Bray et al. (2015), BLRT was performed for the original sample of 2066. However, records with missing data for the covariates (sex and ethnicity) and clinical functioning (emotional problems, conduct problems, self-injurious behaviors, and aggressive behaviors) were eliminated listwise from the analysis, so all subsequent analyses are limited to 1343 participants with complete data (65% of the original sample).
Table 3.
Four latent-class Model of childhood adversity (N = 1,343).
| Latent Class Indicator | Class 1 | Class 2 | Class 3 | Class 4 | Class 5 |
|---|---|---|---|---|---|
|
| |||||
| Latent Class Prevalence | (33%) | (23%) | (14%) | (13%) | (16%) |
|
| |||||
| Label | Low Exposure | Familial Dysfunction | Neglect/Emotional Abuse | Broad Exposure | Pervasive Exposure |
| Item-response probabilities corresponding to a YES response a | |||||
| Verbal/Emotional Abuse | 0.34 | 0.52 | 0.61 | 0.64 | 0.91 |
| Physical Abuse | 0.08 | 0.07 | 0.41 | 0.00 | 0.99 |
| Sexual Abuse | 0.06 | 0.08 | 0.19 | 0.17 | 0.44 |
| Domestic Violence | 0.05 | 0.08 | 0.02 | 0.43 | 0.72 |
| Substance Abuse | 0.03 | 1.00 | 0.44 | 0.83 | 0.87 |
| Family Mental Illness | 0.08 | 0.17 | 0.27 | 0.61 | 0.51 |
| Parental Discord | 0.38 | 0.67 | 0.25 | 0.88 | 0.91 |
| Parental Crime | 0.12 | 0.39 | 0.20 | 0.68 | 0.64 |
| Neglect | 0.01 | 0.08 | 0.85 | 0.49 | 0.71 |
| Abandonment | 0.17 | 0.17 | 0.60 | 0.55 | 0.57 |
| Posterior Class Assignment | 32.8% | 25.1% | 13.2% | 12.4% | 16.5% |
| (441) | (337) | (177) | (166) | (222) | |
Note.
Item-response probabilities > .5 in bold to facilitate interpretation.
Table 4.
Mean and standard deviation by trauma profiles (N = 1,343).
| Emotional Problems |
Conduct Problems |
Self-Injurious Behaviors |
Aggression |
|||
|---|---|---|---|---|---|---|
| Intake Mean (SD) | Discharge Mean (SD) | Intake Mean (SD) | Discharge Mean (SD) | 1st Twelve months Mean (SD) | 1st Twelve months Mean (SD) | |
| Trauma Profiles | ||||||
| Low Exposure | 3.55 (2.51) | 2.63 (2.49) | 4.60 (2.75) | 3.60 (3.01) | .25 (.87) | 1.09 (2.17) |
| Familial Dysfunction | 3.64 (2.54) | 2.69 (2.28) | 4.76 (2.59) | 3.89 (2.87) | .20 (.71) | .93 (1.44) |
| Neglect/Emotional Abuse | 3.79 (2.37) | 3.09 (2.61) | 5.11 (2.45) | 4.35 (2.85) | .31 (.87) | 1.54 (2.34) |
| Broad | 3.94 (2.45) | 2.95 (2.49) | 4.63 (2.47) | 4.17 (2.93) | .14 (.30) | 1.43 (2.33) |
| Pervasive | 4.55 (2.54) | 3.48 (2.66) | 5.26 (2.74) | 4.08 (2.98) | .22 (.45) | 1.44 (2.78) |
Mixed two-way analysis of covariance (ANCOVA)
A mixed 2 (Time) by 5 (CA Patterns) ANCOVA was performed with sex, being Black, being Latinx, age at admission, and length of stay entered as covariates.
Emotional problems (Main effects)
For emotional problems, tests of between-subjects effects revealed a significant main effect for CA patterns, F(4, 1332) = 3.46, p = .008, with follow-up pairwise comparisons indicating that the pervasive exposure pattern had significantly higher levels of emotional problems (M = 3.62, SE = .13) than all other groups: low exposure (M = 3.26, SE = .09); familial dysfunction (M = 3.30, SE = .10); neglect (M = 3.36, SE = .14); and broad exposure (M = 3.14, SE = .15). Main effects were also found for sex, F(1, 1332) = 91.95, p < .001, being Black, F(1, 1332) = 65.20, p < .001, being Latinx, F(1, 1332) = 6.18, p = .01, age at admission, F(1, 1332) = 13.21, p < .001, and length of stay, F(1, 1332) = 10.15, p = .001. Follow-up analysis of overall emotional problems reveals that girls (M = 4.13, SE =.09) had higher levels of emotional problems than boys (M = 2.94, SE =.06). Black youth (M = 2.52, SE =.09) and Latinx youth (M = 3.19, SE =.16) had lower levels of emotional problems than other youth (Non-black: M = 3.63, SE = .06; non-Latinx: M = 3.37, SE =.06). Increased age (β = −.10) and longer length of stay were associated with fewer emotional problems (β = −.07).
Emotional Problems (Change Over Time)
There was a significant within-subjects interaction for time by sex, F(1, 1332) = 7.54, p = .006, and time by length of stay, F(1, 1332) = 16.09, p < .001. Follow-up analyses indicated that from intake to discharge girls (Mean difference = −1.26, p < .001) and youth with longer stays in the program (β = −.11, p < .001) demonstrated significantly greater decreases in emotional problems. A time by CA pattern interaction was not found F(4, 1332) = .78, p = .54, indicating the mean difference for emotional problems did not differ by CA pattern.
Conduct problems (Main effects)
For conduct problems, tests of between-subjects effects revealed a significant main effect for CA patterns, F(4, 1332) = 4.29, p = .002, with follow-up pairwise comparisons indicating that – with the exception of the broad exposure pattern (M = 4.31, SE =.17) – the low exposure pattern (M = 4.07, SE = .10) had lower levels of conduct problems than other groups: familial dysfunction (M = 4.48, SE = .12); neglect (M = 4.70, SE =.16); and pervasive exposure (M = 4.66, SE = .14). Main effects were found for sex, F(1, 1332) = 43.67, p = .03, being Latinx, F(1, 1332) = 6.43, p = .01, age at intake F(1, 1332) = 105.30, p < .001, and length of stay, F(1, 1332) = 58.24, p < .001. Follow-up analyses of overall conduct problems revealed boys (M = 4.45, SE =.08) had higher levels of conduct problems than girls (M = 4.22, SE = .10). Further, Latinx youth (M = 4.49, SE = 2.56) had lower levels of conduct problems than Non-Latinx youth (M = 4.87, SE = 2.66). Increased age (β = −.25) and longer length of stay was associated with fewer conduct problems (β = −.16).
Conduct problems (Change over time)
There was a significant within-subjects interaction for time by CA pattern, F(1, 1332) = 3.48, p = .008. Follow-up analyses indicated significant decreases in conduct problems for low exposure (Mean difference = −1.23, p < .001), familial dysfunction (Mean difference = −.89, p <.001), neglect (Mean difference = −.59, p =.02), and pervasive exposure (Mean difference = −1.03, p < .001 but not broad exposure (Mean difference = −.18, p = .48; see Figure 1). Time by sex, F(1, 1332) = 8.33, p =.004, time by race (i.e., being Black), F(1, 1332) = 40.86, p < .001, and time by length of stay, F(1, 1332) = 59.48, p <.001, interactions were found. Follow-up analyses indicated girls (Mean difference = −1.34, p < .001) and youth with longer stays in the program (β = −.20, p < .001) demonstrated greater decreases in conduct problems. The interaction for race revealed non-Black youth demonstrated significant decreases in conduct problems (Mean difference = −1.20, p < .001) while Black youth experienced no change (Mean difference = .02, p = .90). Notably, compared to Black youth, Non-Black youth started with higher conduct scores at intake (β = .85, p < .001) and had lower scores (β = −.38, p < .001) at discharge.
Figure 1.
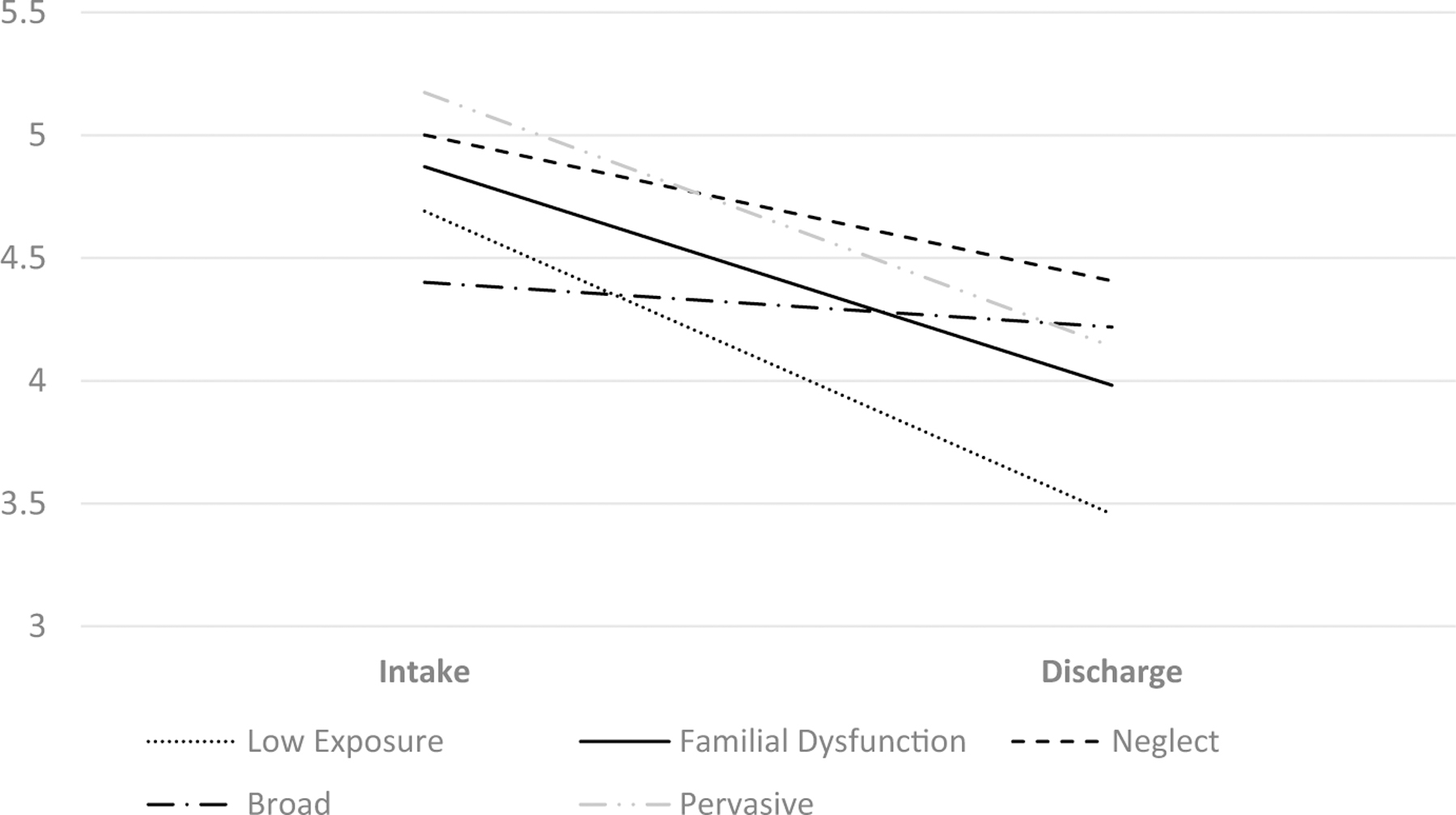
Time by CA pattern for conduct problems.
HLM analysis
Self-injurious behavior: unconditional & level 1 model
Given self-injurious behaviors are count data, a Poisson sampling model with a log link function was used (Raudenbush & Bryk, 2002). Further examination indicated the data would fit better if it was Winsorized to the 99th percentile. Winsorizing is a method of dealing with outliers by making all extreme scores equal, such as values in the 99th percentile, to pull in outliers (Lusk et al., 2011). In this case, 99% of all youth engaged in between zero and three self-injurious behaviors during their first 12 months. As such, the upper end of the self-injurious behaviors range was Winsorized to three. The unconditional model revealed significant variation in self-injurious behaviors (β = −1.86, t (1248) = −40.38, p < .001). For the level 1 model, results indicated the intercept (β = −1.63, t(1248) = −31.81, p < .001) and overall time trend was significant (β = −.056, t(1248) = −8.67, p < .000), indicating that self-injurious behaviors decreased over the first 12 months in the program.
Self-injurious behavior: combined model (levels 1 and 2)
The five Level 2 CA patterns were incorporated into this model: broad, neglect, pervasive, familial, and low exposure (reference group). Covariates included age at admission (grand mean centered = 15.7 years), sex, length of stay in months (grand mean centered = 13.0 months), and race (Black, Latinx, Other [reference group]). At entry into the program (the intercept), those fitting the broad CA pattern engaged in significantly fewer incidents (β = −.588, t(1239) = −2.96, p = .004). Further, females (β = .509, t(1239) = 4.54, p < .001) had significantly more incidents during the first month in care than did males. Conversely, older youth at admission (β = −.159, t(1239) = −4.81, p < .001), longer length of stay in months (β = −.040, t(1239) = −5.33, p < .001), being Black (β = −.609, t(1239) = −4.74, p < .001) or Latinx (β = −.490, t(1239) = −2.85, p < .001) were all associated with fewer self-injurious behaviors during the first month in care.
Regarding the time components (i.e., first 12 months in care) youth with the neglect CA pattern engaged in more self-injurious behaviors during their first 12 months (β = .057, t(1239) = 2.63, p = .009) as did those with the pervasive CA pattern (β = .058, t(1239) = 3.01, p = .003). Females engaged in more self-injurious behaviors (β = .094, t(1239) = 6.76, p < .001) than did males whereas the Black youth engaged in fewer (β = −.06, t(1239) = −2.82, p = .005) than other races. See Figure 2 for a comparison of the self-injurious behavior over time in Black and White girls. See Table 4 for a summary of the models.
Figure 2.
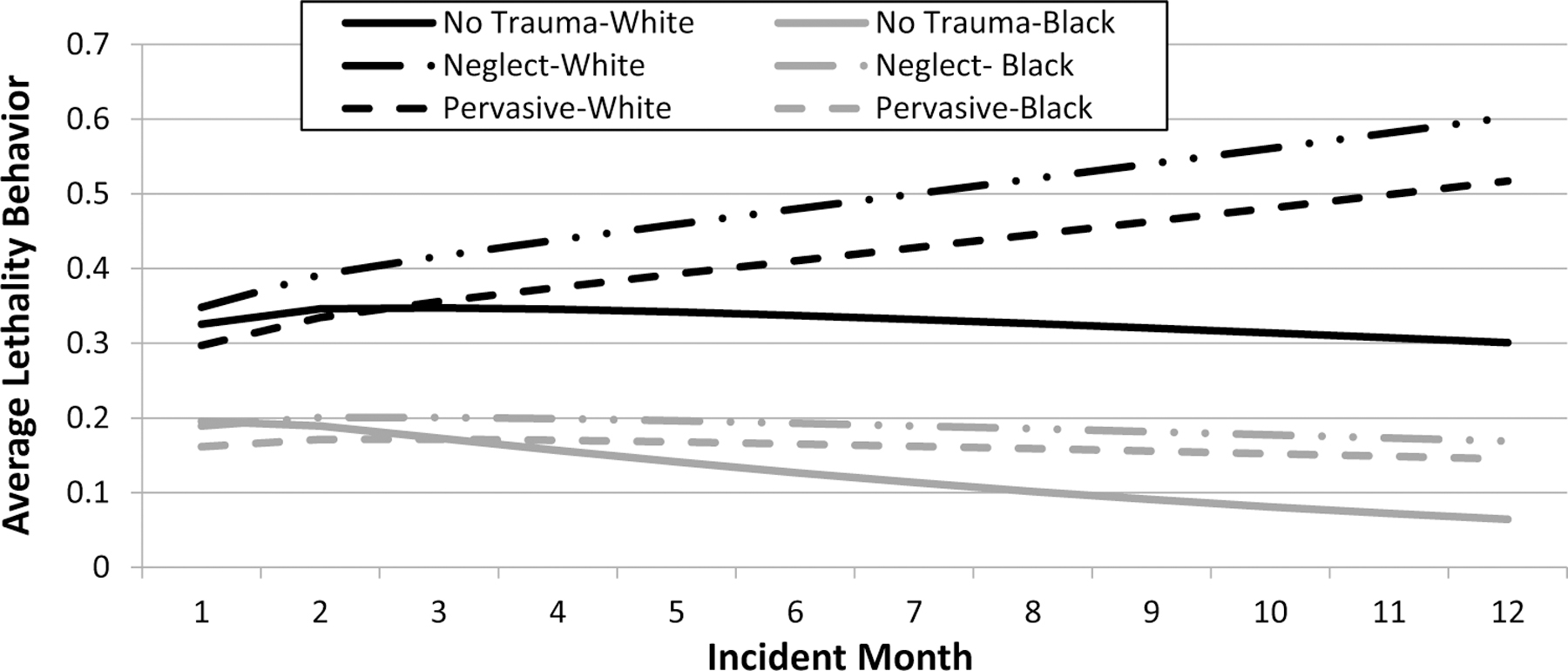
Hierarchical linear modeling of average daily reported self-injurious behaviors in girls within the first 12 program months.
Aggressive behaviors: unconditional & level 1 model
Given that the aggressive behavior variable is count data, a Poisson sampling model with a log link function was used (Raudenbush & Bryk, 2002). The unconditional model revealed significant variation in aggressive behaviors (β = .181, t(1248) = 4.22, p < .001). For the level 1 model, results indicated the intercept (β = .299, t(1248) = 7.20, p < .001) and overall time trend was significant (β = −.042, t(1248) = −7.70, p < .001), indicating that aggressive behaviors decreased over the first 12 months in the program.
Aggressive behaviors: combined model (levels 1 and 2)
The five Level 2 CA patterns were incorporated into this model: broad, neglect, pervasive, familial, and low exposure (reference group). Covariates included age at admission (grand mean centered = 15.7 years), sex, length of stay in months (grand mean centered = 13.0 months), and race (Black, Latinx, Other [reference group]). At entry into the program (the intercept), youth with the neglect (β = .286, t(1239) = 2.39, p = .017) and pervasive (β = .317, t(1239) = 2.47, p = .014) CA patterns engaged in significantly more aggressive behaviors than those with the low exposure pattern. Further, Black youth had significantly more incidents during the first month in care (β = .352, t(1239) = 4.07, p < .001) compared to other races. Additionally, females (β = −.219, t(1239) = −2.41, p = .016), older youth at admission (β = −.326, t(1239) = −14.11, p < .001), and those with longer length of stay in months (β = −.042, t(1239) = −5.98, p < .001), all displayed with fewer aggressive behaviors during their first month in care.
For the time components, youth with the neglect (β = .046, t(1239) = 2.98, p = .003) and broad (β = .046, t(1239) = 2.48, p = .013) CA patterns had significantly more aggressive behaviors than the low exposure group. Conversely, Black youth had significantly fewer aggressive incidents over their first 12 months in care than those in the reference group (β = −.026, t (1239) = −2.13, p = .033). See Figure 3 for a comparison of the aggressive behaviors over time in boys. See Table 5 for a summary of the models.
Figure 3.
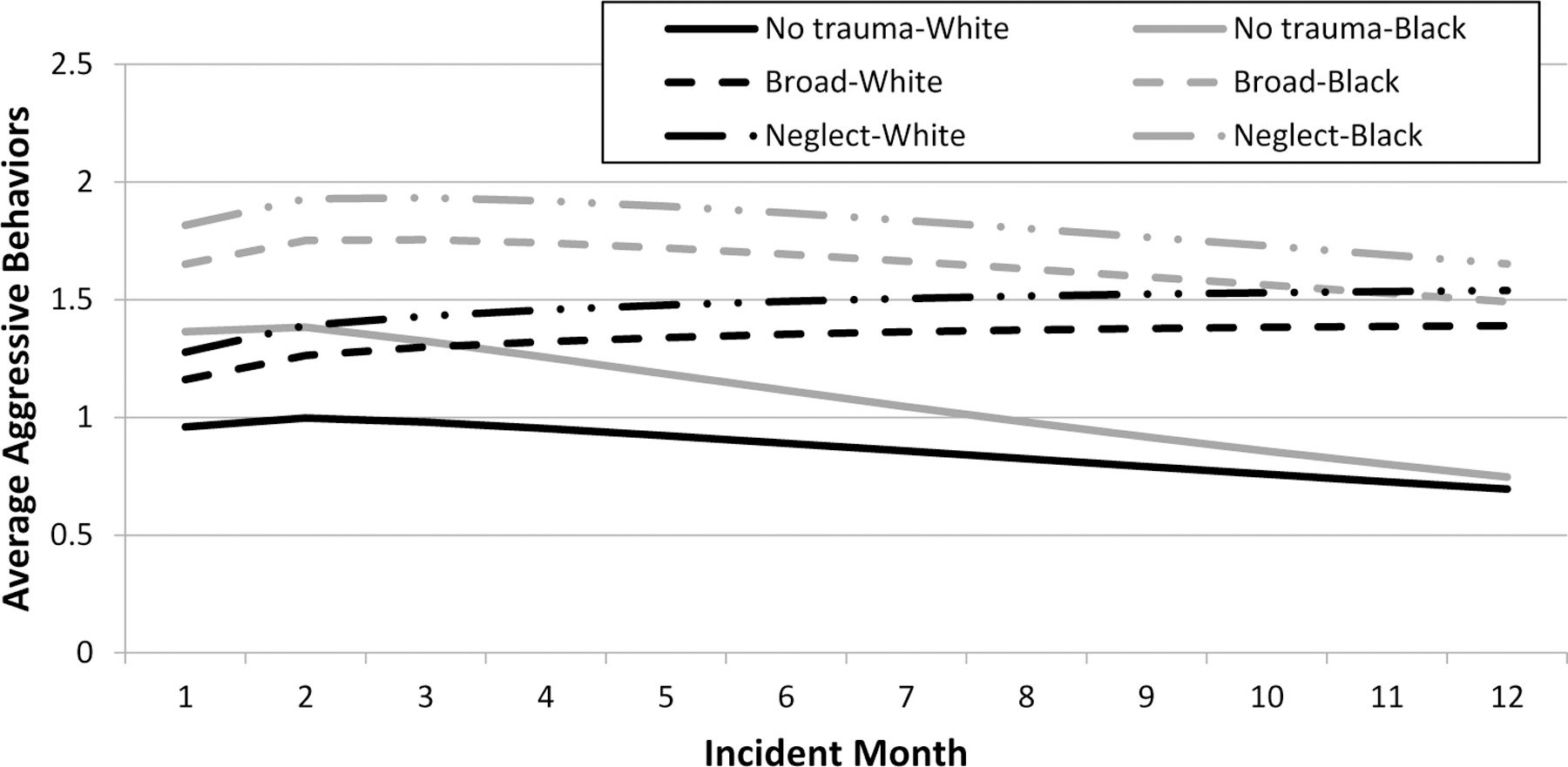
Hierarchical linear modeling of average daily reported aggressive behaviors in boys within the first 12 program months.
Table 5.
HLM combined models: self-injurious and aggressive incidents.
| Self-Injurious Incidents (N = 1249) |
Aggressive Incidents (N = 1249) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | B | SE | t | p | Β | SE | t | p |
| Intercepta | −1.632 | .10 | −15.55 | .000 | −0.042 | .11 | −0.38 | .701 |
| Female | 0.509 | .11 | 4.54 | .000 | −0.219 | .09 | −2.41 | .016 |
| Black | −0.609 | .13 | −4.74 | .000 | 0.352 | .09 | 4.07 | .000 |
| Latinx | −0.490 | .17 | −2.85 | .005 | −0.094 | .13 | −0.71 | .476 |
| Length of Stay (Months) | −0.040 | .01 | −5.33 | .000 | −0.042 | .01 | −5.98 | .000 |
| Mean Admission Age (Years) | −0.159 | .03 | −4.81 | .000 | −0.326 | .02 | −14.11 | .000 |
| Broad | −0.588 | .20 | −2.96 | .004 | 0.191 | .15 | 1.32 | .189 |
| Neglect | 0.067 | .15 | 0.46 | .647 | 0.286 | .12 | 2.39 | .017 |
| Pervasive | −0.091 | .14 | −0.67 | .506 | 0.317 | .13 | 2.47 | .014 |
| Familial | −0.028 | .15 | −0.19 | .851 | 0.166 | .11 | 1.44 | .149 |
| Slope (Month) | −0.131 | .02 | −8.07 | .000 | −0.059 | .01 | −4.27 | .000 |
| Female | 0.094 | .01 | 6.76 | .000 | 0.018 | .01 | 1.47 | .143 |
| Black | −0.060 | .02 | −2.82 | .005 | −0.026 | .01 | −2.13 | .033 |
| Latinx | −0.020 | .02 | −1.08 | .282 | 0.001 | .02 | 0.07 | .948 |
| Length of Stay (Months) | 0.001 | .00 | 1.20 | .229 | 0.001 | .00 | 1.88 | .060 |
| Mean Admission Age (Years) | −0.006 | .00 | −1.31 | .192 | 0.005 | .00 | 1.42 | .156 |
| Broad | 0.039 | .03 | 1.35 | .179 | 0.046 | .02 | 2.48 | .013 |
| Neglect | 0.057 | .02 | 2.63 | .009 | 0.046 | .02 | 2.98 | .003 |
| Pervasive | 0.058 | .02 | 3.01 | .003 | 0.014 | .02 | 0.77 | .439 |
| Familial | 0.023 | .02 | 1.16 | .246 | 0.001 | .02 | 0.08 | .935 |
Notes:
Estimated average of self-injurious or aggressive incidents at Month 1.
Discussion
This study investigated the influence of CA patterns on youth’s response to a residential TIC program. Generally, youth experienced decreases in self-injurious and aggressive behaviors over the first 12 months in the program and decreases in emotional and conduct problems from intake to discharge. Five CA patterns were identified: (1) low exposure, (2) familial dysfunction, (3) neglect, (4) broad exposure, and (5) pervasive exposure. There were parallel decreases in emotional problems across all patterns. Longer program stays were associated with greater decreases in emotional problems. This suggests TIC is associated with improved emotional problems regardless of CA history. It is likely that TIC – which encourages residential staff to be empathetic toward youth and aware of the role of trauma in problem behavior – creates an emotionally and physically safe environment that facilitates improvements in anxiety and depressive symptoms.
In contrast, trends in aggression, conduct problems, and self-injurious behaviors differed by CA pattern. The pervasive group displayed more initial aggressive behavior within the first month of the program and demonstrated higher rates of self-injurious behaviors during their first 12 months relative to the low exposure group, which is consistent with past work indicating youth with the greatest adversity have the most functional impairment in residential care (Briggs et al., 2012). The pervasive group also demonstrated higher levels of emotional problems than all other groups throughout treatment – even though their rate of symptom reduction did not differ from the other CA groups. These results suggest that while TIC is beneficial for this group, they may still benefit from additional services and targeted interventions to help them function on par with their low exposure peers. Problem solving in particular may be an important skill to target for youth with pervasive exposure given that it reduces emotional problems in youth with high trauma symptoms (Tyler et al., 2021). Peer relationships training may also be important for these youth given it has been found to moderate the association between high trauma symptoms and suicide attempts (Tyler et al., 2022).
The neglect group engaged in higher rates of self-injurious behaviors than the low exposure group in the first 12 months of the program. This is consistent with the Dimensional Model of Adversity and Psychopathology framework, which links neglect to poor emotional regulation and problem-solving abilities (McLaughlin & Lambert, 2017). Neglected youth may struggle to adapt to a residential program and resort to self-harm. Consistent with the interpersonal theory of suicide, which indicates thwarted belongingness is linked to suicidal behaviors (Van Orden et al., 2010), neglect may interfere with a youth’s sense of belongingness, increasing their risk for self-injurious behavior.
The neglect, but not the pervasive, group also engaged in higher rates of aggressive behaviors than the low exposure group over their first 12 months in the program. Aligning with the Dimensional Model of Adversity and Psychopathology, links between neglect and aggression may be due to children having fewer opportunities for learning adaptive social skills (Kim & Cicchetti, 2010; McLaughlin & Lambert, 2017). Neglect is also associated with deviant peer affiliation which, in turn, is associated with the development of aggression (Yang et al., 2021). Additionally, neglected youth may encounter adults who more closely monitor their behavior and set more limits than past caregivers when entering a residential program, and may engage in increased aggression in response to this environment. Overall, findings suggest TIC residential programs should consider targeted efforts to help neglected youth best assimilate such as developing adaptive social skills.
The most unexpected findings were for the broad exposure group. Unlike other groups, the broad exposure group was not associated with higher levels of overall conduct problems than the low exposure group. Moreover, the broad exposure group engaged in the fewest incidences of self-injurious behavior in the first month of the program out of all of the groups, including the low exposure group. These findings contrast with studies indicating exposure to multiple CA is associated with increased impairment (e.g., Connell et al., 2018). Also, improvements in externalizing behaviors were less robust for the broad exposure group and those in the broad exposure group did not decrease in conduct problems. They also displayed increases in aggressive behaviors during the first 12 months in the program.
Group-level characteristics may be driving these results. For example, the lower caregiver reported levels of conduct problems for the broad group could be due to underreporting. Alternatively, it could be that because the broad exposure group did not display more internalizing or externalizing problems than other youth, it is possible they were not being referred for additional services such as individual and/or group therapy at a similar rate. The broad exposure group was also characterized by a higher percentage of youth being convicted of a crime than expected – given the group’s size and the proportion of those convicted of a crime in the overall sample (53.6%; χ2 = 10.56; p < .001). Thus, the broad exposure group’s referral to residential care may have been driven by acute behavioral incidents. Alternatively, given their exposure to multiple forms of CA, residential care may have been primarily sought to protect these youth from further CA exposure, and not necessarily because of behavioral problems. Finally, it may be that severity or frequency of the CA experienced by youth have a bigger role in treatment outcomes than the number of CA types.
Youth in the broad exposure group did not make progress on behavioral problems and even demonstrated increased behavioral impairment while in the TIC program, suggesting further changes are needed to meet their needs. For example, Kind et al. (2020) found that youth who demonstrated decreased aggression over approximately 6.5 months reported concurrent improvements in peer relationships, managing school requirements, reductions in substance use, suicidal ideation, and improved perceived self-efficacy – suggesting that having a positive self-image and a sense of control of one’s behavior and environment can inhibit aggressive behavior. TIC programs may better serve youth with broad CA exposure by incorporating additional interventions that improve the youth’s social and school life, including more targeted substance abuse and suicidal/self-injury prevention, and strengthening youth’s self-efficacy. These interventions would also directly benefit youth in the pervasive and neglect groups.
Some differences based on youth’s demographics were found. Compared to boys, girls demonstrated increases in self-injurious behaviors in their first 12 months within the program but also demonstrated greater decreases in emotional and conduct problems from intake to discharge. These findings are consistent with previous research suggesting that, though girls display more suicidal ideation/self-harming behavior while in residential care, they have better overall treatment outcomes than boys (Holtberg et al., 2016). In addition, compared to other races, being Latinx was associated with fewer self-injurious behaviors in the first month of the program. A more in-depth examination of conduct problems among Latinx youth also revealed that they experienced fewer conduct problems at intake (β = −.62, p =.004). Fewer problems at the start of the program among these youth may indicate that the threshold for residential care referrals may be lower for Latinx youth – possibly due to cultural biases (Javdani et al., 2023). Conversely, being Black was associated with more aggressive behaviors during the first month of their stay, but fewer self-injurious and aggressive behaviors over the first 12 months of the program. This may indicate that additional support is needed for Black youth as they transition into this TIC program and highlights the need for Black youth to be given sufficient time to adjust to residential programs before they are terminated for aggressive incidents. Additionally, non-Black youth demonstrated significantly better improvements in conduct problems than Black youth – who demonstrated nonsignificant changes. Black youth had lower reports of conduct problem at intake compared to their non-black counterparts, so there may have been less opportunity for them to improve. Still, there is room for improvement to better serve Black youth. Black youth may face additional stressors in out-of-home care, such as a disruption in positive family and community support, inadequate representation in staff, or poor cultural sensitivity/unconscious bias (FitzGerald & Hurst, 2017; Kruzich et al., 2002). While the percentage of white and Black staff in our intervention closely matched the demographics of the major city in which the program was located (Census Bureau, 2021). For example, 75% of our Family-Teachers were white and 12% were Black. However, Black youth are over-represented in the sample (24.9%) and would likely benefit from increased staff representation. Members of all races can demonstrate unconscious bias (FitzGerald & Hurst, 2017). While the staff received trainings on racism and cultural sensitivity, our organization and residential care more broadly would benefit from more intensive antiracist and cultural sensitivity training (Javdani et al., 2023). A comprehensive framework detailing the role of gender or ethnicity in residential care is absent in the literature and further work is needed to understand these differences.
Limitations
The current study’s limitations provide direction for future research. First, future research would benefit from examining additional CA events such as community violence, CA severity, and CA frequency. Posterior probabilities were used to assign youth into their most likely latent CA profiles, which may introduce potential biases (Bray et al., 2015); future work using different statistical approaches is warranted to evaluate the robustness of results. Third, different raters were used for emotional symptoms and conduct problems throughout the study – future research should examine potential informant effects. Fourth, only 65% of participants in the original sample had outcome data. Compared to the original sample, the current sample included participants with a longer length of stay and fewer minority participants. However, to mitigate the effects of both variables on our main analyses, both length of stay and race/ethnicity were included as covariates. Additionally, while the coding system of the Daily Incident Report has previously demonstrated strong inter-rater reliability (Wright, 2001), its data in this study was not examined for inter-rater reliability. While beyond the scope of the current project, future research would benefit from examining how individual therapy within the program influences treatment. Finally, our study examined a single agency that serves youth from across the U.S. using family-style group home (Thompson & Daly, 2015) and lacked a comparison group. Therefore, results may not generalize to other programs and future work comparing TIC residential treatment to control conditions is warranted (Berliner & Kolko, 2016).
Conclusions and implications
Overall, youth benefitted from the TIC program. Observed decreases in self-injurious behavior and aggression in the first 12 months of treatment for youth across all CA patterns are a testament to the culture of safety within the TIC program as well as youth’s frequent access to resources which may reduce problem behavior in residential care, such as engaging activities, proper nutrition, and access to supportive adults (Sekol, 2013). Universal and parallel decreases in emotional problems across CA patterns suggest that TIC has benefits for youth’s emotional well-being in general.
However, our findings also highlight that youth impairment within a TIC program and their response to treatment can depend on their CA patterns. Youth who have experienced neglect may be at high risk for problematic behaviors and self-injurious behavior in residential programs and may require tailored interventions and increased support, such as social skills training – especially during their first year of care. Likewise, youth in the pervasive group had higher levels of emotional problems than other youth at the end of treatment and may require tiered interventions, such as problem-solving training, to improve their emotional coping. Additionally, the broad group did not demonstrate the same decreases in conduct problems observed in the other CA exposure groups, despite having lower levels of conduct problems overall. More work is needed to explore the mechanisms behind this unusual trajectory and how to best foster their progress within a TIC program. Finally, our findings highlight the importance of considering youth demographics when developing TIC programs. Girls may require additional support and monitoring to reduce risk of self-injurious behavior, while Black youth, given reported increases in aggression during the first month of treatment, may also benefit from tailored interventions and a more culturally supportive environment as they transition into the program. More intensive staff training in cultural sensitivity and bias awareness may facilitate better care for Black youth.
Despite differences in program impairment and treatment response among youth with a history of neglect, broad CA, and pervasive CA, research suggests that TIC programs may better serve youth with all three CA patterns by incorporating interventions that target social development (e.g., Kind et al. 2020). For example, these interventions may focus on teaching adaptive prosocial skills like problem solving and peer relations training (Tyler et al., 2021, 2022), and facilitating environments that reduce negative peer contagion (Huefner & Ringle, 2012). Future research is needed to explore how to best approach and address treatment response differences in youth with different CA patterns.
Supplementary Material
Practice Implications.
Trauma-informed practices are important for improving emotional well-being in residential care.
Tailored interventions for youth with specific trauma histories may help reduce self-injurious behavior and behavior problems.
TIC programs may better serve youth with a variety of trauma histories by incorporating interventions that target social development.
Funding
The work was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health [T32HD101392].
Footnotes
Supplemental data for this article can be accessed online at https://doi.org/10.1080/0886571X.2023.2266987.
Disclosure statement
Dr. Gordon, Mr. Ringle, Ms. Ende, and Dr. Tyler are all researchers at the same institution which houses the evaluated residential program. Several measures were taken to mitigate this potential conflict of interest including utilizing a priori hypotheses and statistical plans, collaborating with colleagues/authors outside of the program institution, and utilizing rigorous statistical techniques based on sound scientific support.
References
- Berliner L, & Kolko DJ (2016). Trauma informed care: A commentary and critique. Child Maltreatment, 21(2), 168–172. 10.1177/1077559516643785 [DOI] [PubMed] [Google Scholar]
- Boyer SN, Hallion LS, Hammell CL, & Button S (2009). Trauma as a predictive indicator of clinical outcome in residential treatment. Residential Treatment for Children & Youth, 26(2), 92–104. 10.1080/08865710902872978 [DOI] [Google Scholar]
- Brack AB, Huefner JC, & Handwerk ML (2012). The impact of abuse and gender on psychopathology, behavioral disturbance, and psychotropic medication count for youth in residential treatment. American Journal of Orthopsychiatry, 82(4), 562–572. 10.1111/j.1939-0025.2012.01177.x [DOI] [PubMed] [Google Scholar]
- Braun MT, Adams NB, O’Grady CE, Miller DL, & Bystrynski J (2020). An exploration of youth physically restrained in mental health residential treatment centers. Children and Youth Services Review, 110, 110. 10.1016/j.childyouth.2020.104826 [DOI] [Google Scholar]
- Bray BC, Lanza ST, & Tan X (2015). Eliminating bias in classify-analyze approaches for latent profile analysis. Structural Equation Modeling, 22(1), 1–11. 10.1080/10705511.2014.935265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs EC, Greeson JK, Layne CM, Fairbank JA, Knoverek AM, & Pynoos RS (2012). Trauma exposure, psychosocial functioning, and treatment needs of youth in residential care: Preliminary findings from the NCTSN core data set. Journal of Child & Adolescent Trauma, 5(1), 1–15. 10.1080/19361521.2012.646413 [DOI] [Google Scholar]
- Cameron M, & Guterman NB (2007). Diagnosing conduct problems of children and adolescents in residential treatment. Child & Youth Care Forum, 36(1), 1–10. 10.1007/s10566-006-9027-6 [DOI] [Google Scholar]
- Celeux G, & Soromenho G (1996). An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification, 13, 195–212. [Google Scholar]
- Census Bureau, U. S. (2021). Quick facts: Retrieved March 26, 2023. https://www.census.gov/quickfacts/omahacitynebraska
- Clark SL (2010). Mixture modeling with behavioral data. Dissertation Abstracts International Section A: Humanities and Social Sciences, 71(4–A), 1183. [Google Scholar]
- Connell CM, Pittenger SL, & Lang JM (2018). Patterns of trauma exposure in childhood and adolescence and their associations with behavioral well-being. Journal of Traumatic Stress, 31(4), 518–528. 10.1002/jts.22315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Li D, & Whipple SS (2013). Cumulative risk and child development. Psychological Bulletin, 139(6), 1342. 10.1037/a0031808 [DOI] [PubMed] [Google Scholar]
- Father Flanagan’s Boys’ Home. (2015). Family home program: Program manual Father Flanagan’s Boys’. [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/s0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- FitzGerald C, & Hurst S (2017). Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics, 18(1), 1–18. 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child & Adolescent Psychiatry, 40(11), 1337–1345. 10.1097/00004583-200111000-00015 [DOI] [PubMed] [Google Scholar]
- Goodman R, Meltzer H, & Bailey V (1998). The strengths and difficulties questionnaire: A pilot study on the validity of the self-report version. European Child & Adolescent Psychiatry, 7(3), 125–130. 10.1007/s007870050057 [DOI] [PubMed] [Google Scholar]
- Gordon C, Nguyen P, Mitchell A, & Tyler P (2022). Profiles of childhood adversity and associated psychopathology in youth entering residential care. Psychological Trauma: Theory, Research, Practice, & Policy, 15(Suppl 1), S82–S91. Advanced online publication. 10.1037/tra0001325 [DOI] [PubMed] [Google Scholar]
- Griffin G, Martinovich Z, Gawron T, & Lyons JS (2009). Strengths moderate the impact of trauma on risk behaviors in child welfare. Residential Treatment for Children & Youth, 26 (2), 105–118. 10.1080/08865710902872994 [DOI] [Google Scholar]
- Hodgdon HB, Lord KA, Suvak MK, Martin L, Briggs EC, & Beserra K (2023). Predictors of symptom severity and change over time among youth in trauma-informed residential care. Child Abuse and Neglect, 137, 106056. 10.1016/j.chiabu.2023.106056. [DOI] [PubMed] [Google Scholar]
- Holtberg T, Olson S, & Brown-Rice K (2016). Adolescent gender differences in residential versus outpatient mental health treatment: A meta-analysis. Journal of Mental Health Counseling, 38(3), 217–232. 10.17744/mehc.38.3.03 [DOI] [Google Scholar]
- Huang L, Dziak JJ, Wagner AT, & Lanza ST (2016). LCA bootstrap stata function users’ guide (version 1.0). University Park: The Methodology Center, Penn State. http://methodology.psu.edu [Google Scholar]
- Huefner JC, & Ringle JL (2012). Examination of negative peer contagion in a residential care setting. Journal of Child and Family Studies, 21(5), 807–815. 10.1007/s10826-011-9540-6 [DOI] [Google Scholar]
- Javdani S, Berezin MN, & April K (2023). A treatment-to-prison-pipeline? Scoping review and multimethod examination of legal consequences of residential treatment among adolescents. Journal of Clinical Child and Adolescent Psychology, 52(3), 376–395. 10.1080/15374416.2023.2178003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51(6), 706–716. 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind N, Bürgin D, Clemens V, Jenkel N, & Schmid M (2020). Disrupting the disruption cycle – a longitudinal analysis of aggression trajectories, quality of life, psychopathology and self-efficacy in closed youth residential care. Children and Youth Services Review, 113, 105015. 10.1016/j.childyouth.2020.105015 [DOI] [Google Scholar]
- Kisiel C, Fehrenbach T, Small L, & Lyons JS (2009). Assessment of complex trauma exposure, responses, and service needs among children and adolescents in child welfare. Journal of Child & Adolescent Trauma, 2, 143–160. [Google Scholar]
- Kruzich JM, Friesen BJ, Williams-Murphy T, & Longley MJ (2002). Voices of African American families: Perspectives on residential treatment. Social Work, 47(4), 461–470. 10.1093/sw/47.4.461 [DOI] [PubMed] [Google Scholar]
- Lanza ST, Dziak JJ, Huang L, Wagner AT, & Collins LM (2015). LCA Stata plugin users’ guide (version 1.2) (Retrieved from methodology.psu.edu). University Park: The Methodology Center, Penn State. [Google Scholar]
- Larzelere RE (1996). Inter-coder reliabilities and construct groupings for some important codes on the daily incident report. Boys Town Press. [Google Scholar]
- Lusk EJ, Halperin M, & Heilig F (2011). A note on power differentials in data preparation between trimming and winsorizing. Business Management Dynamics, 1(2), 23. [Google Scholar]
- McLaughlin KA (2016). Future directions in childhood adversity and youth psychopathology. Journal of Clinical Child & Adolescent Psychology, 45(3), 361–382. 10.1080/15374416.2015.1110823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Lambert HK (2017). Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Current Opinion in Psychology, 14, 29–34. 10.1016/j.copsyc.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science, 25(4), 239–245. 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng QX, Yong BZJ, Ho CYX, Lim DY, & Yeo WS (2018). Early life sexual abuse is associated with increased suicide attempts: An update meta-analysis. Journal of Psychiatric Research, 99, 129–141. 10.1016/j.jpsychires.2018.02.001 [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods (Vol. 1). Sage. [Google Scholar]
- Sekol I (2013). Peer violence in adolescent residential care: A qualitative examination of contextual and peer factors. Children and Youth Services Review, 35(12), 1901–1912. 10.1016/j.childyouth.2013.09.006 [DOI] [Google Scholar]
- Sheridan MA, Shi F, Miller AB, Salhi C, & McLaughlin KA (2020). Network structure reveals clusters of associations between childhood adversities and development outcomes. Developmental Science, 23(5). 10.1111/desc.12934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, & Committee on Early Childhood, Adoption, and Dependent Care. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- Thompson RW, & Daly DL (2015). The family home program: An adaptation of the teaching family model at boys town. In Whittaker JK, Del Valle JF, & Holmes L (Eds.), Therapeutic residential care with children and youth: Developing evidence-based international practice (pp. 113–123). Kingsley. [Google Scholar]
- Tyler PM, Aitken AA, Ringle JL, Stephenson JM, & Mason WA (2021). Evaluating social skills training for youth with trauma symptoms in residential programs. Psychological Trauma: Theory, Research, Practice, & Policy, 13(1), 104. 10.1037/tra0000589 [DOI] [PubMed] [Google Scholar]
- Tyler PM, Hillman MS, & Ringle JL (2022). Peer relations training moderates trauma symptoms and suicide ideation for youth in a residential program. Journal of Child and Family Studies, 31(2), 447–458. 10.1007/s10826-021-02193-x [DOI] [Google Scholar]
- Tyler PM, Patwardan I, Ringle JL, Chmelka MB, & Mason WA (2019). Youth needs at intake into trauma‐informed group homes and response to services: An examination of trauma exposure, symptoms, and clinical impression. American Journal of Community Psychology, 64(3–4), 321–332. 10.1002/ajcp.12364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services Substance Abuse and Mental Health Services Administration for Substance Abuse Treatment Center for Behavioral Health Statistics and Quality. (2014). Trauma-informed care in behavioral health services (SMA Publication No. 14–4816). Available from: https://store.samhsa.gov/shin/content//SMA14-4816/SMA14-4816.pdf
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TE Jr. (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright DJ (2001). The relationship of anxiety and externalizing disorders. Dissertation Abstracts International: Section B: The Sciences & Engineering, 62, 2084B. [Google Scholar]
- Yang B, Xiong C, & Huang J (2021). Parental emotional neglect and left-behind children’s externalizing problem behaviors: The mediating role of deviant peer affiliation and the moderating role of beliefs about adversity. Children and Youth Services Review, 120, 105710. 10.1016/j.childyouth.2020.105710 [DOI] [Google Scholar]
- Zelechoski AD, Sharma R, Beserra K, Miguel JL, DeMarco M, & Spinazzola J (2013). Traumatized youth in residential treatment settings: Prevalence, clinical presentation, treatment, and policy implications. Journal of Family Violence, 28(7), 639–652. 10.1007/s10896-013-9534-9 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


