Abstract
Study Design
Retrospective chart review.
Objective
Socioeconomic status (SES) greatly impacts one’s health status and the type of trauma that a patient experiences due to increased risk of exposure and varying availability of resources to treat emergent conditions. There is a need for large-scale databases of pediatric facial trauma to identify discrepancies in occurrence and identify risk factors.
Methods
This retrospective examination uses a multi-center database to evaluate pediatric facial trauma patients (n = 644) visiting Atrium Heath Wake Forest Baptist (AHWFB) hospital from 2020 to 2022. Data collected included demographic information, past medical and surgical history, trauma history, interventions, and long-term outcomes such as scarring, deformities, and sensory or motor deficits. The number of incidents for each zip code surrounding AHWFB was compared with SES data including unemployment rate, mean household income, and poverty level.
Results
Thirty-five percent of patients sustained a high-energy injury, and 65% sustained a low-energy injury. Within the surrounding counties of AHWFB, there were more incidents of pediatric facial trauma in areas with greater rates of poverty (P = 0.006). Additionally, there were more incidents due to high-energy injuries in areas with lower income (P = 0.044) and more poverty (P = 0.002). Specifically, motor vehicle accidents were more common in areas with lower income (P = 0.017) and more poverty (P = 0.001).
Conclusions
These findings in the central Piedmont region of North Carolina are consistent with previous research of SES’s effect on health inequalities and serve as evidence of the need to take steps to prevent pediatric facial trauma in areas of low SES.
Keywords: socioeconomic status, pediatric, facial trauma
Introduction
Pediatric Facial Trauma Database
Pediatric trauma causes 12 000 deaths each year in the United States, making it the leading cause of morbidity of pediatric patients. 1 Additionally, the incidence of pediatric facial trauma is more common than adult facial trauma. 1 Health systems would greatly benefit from having a pediatric facial trauma database with organized records and analysis to improve patient care with minimal additional resources. Additionally, statistics and benchmarks can be compared with past and future data to track health system success, apply for funding, and support or refute current or future policy.2,3
More specifically, creating a database for pediatric patients is important for analysis because children are different from adults in terms of facial trauma. First, children’s facial anatomy and bone structure are more resistant to fracture because of their increased elasticity and children have more prominent foreheads and smaller, flatter faces, which grow forward as the child ages. 4 Furthermore, children do not have some facial features that adults do, such as paranasal sinuses, and children have more adipose tissue, which can affect treatment decisions and follow-up care. 4 These differences cause various mechanisms of trauma to be more or less common and deleterious for children of various ages. For example, older children are more likely to sustain high-energy injuries, such as sports injuries or car accidents, whereas younger children are more likely to sustain low-energy injuries, such as low falls/drops, because of the nature of their activities and the presence of adult supervision. 4 Second, treating pediatric facial trauma is more difficult because the pediatric facial skeleton and skull are still growing, so treatment intervention has the potential to interfere with the natural growth and shape of a child’s facial structure. 5
This database serves as 1 of few large-volume databases of pediatric facial trauma, adding valuable data including specific pediatric facial trauma patient demographics, injuries, treatments, and outcomes. Examples of more general databases mined for studies of pediatric facial trauma include the National Trauma Data Bank6,7 and the National Electronic Injury Surveillance System. 8 The specificity and detail of the data compiled in this database can help answer a wide variety of research questions that will benefit future patients and assist health care providers.
Socioeconomic Status and Pediatric Facial Trauma
According to the World Health Organization (WHO), “social determinants of health (SDH) are the non-medical factors that influence health outcomes”. 9 Social determinants of health are the factors that make up an individual’s socioeconomic status (SES) and examples of SDH include income, education, unemployment, food insecurity, and access to affordable health services. 10 It has been noted that SDH accounts for 30%–55% of an individual’s health outcomes. 9 Additionally, SDH is “increasingly acknowledged as 1 of the most critical health determinants, and the non-genetic components are estimated as a significant (70%) contributor to individuals’ health”. 11 And among the various social determinants of health, neighborhood, and therefore on a larger scale zip code, has been identified as a fundamental factor for explaining how discrepancies of SDH are permanently fixed into inequalities of health. 11 By acknowledging the impact of SES on health, steps can be taken to improve the equality of SES across communities. By analyzing the relationship between SES and pediatric facial trauma, this study can serve as evidence of the geographical discrepancies of SES and that these discrepancies may correlate to the number and causes of pediatric facial trauma incidents.
The central Piedmont region of North Carolina and more specifically the greater Winston-Salem area represents a unique area to analyze the effects of SES on pediatric facial trauma because of its large socioeconomic diversity. In 2021, Winston-Salem was ranked in the top half of most economic class diversity in the country based on data from the U.S. Census Bureau. 12 This economic diversity has the most potential to clearly show the effect SES has had on the quantity, mechanism, and treatment of pediatric facial trauma cases at Atrium Health Wake Forest Baptist (AHWFB). The aim of this study is to determine the relationship between SES and the number of pediatric facial trauma incidents in order to identify and potentially improve preventative measures for varying SES patients, as well as highlight any discrepancies in exposure to dangerous situations in regard to pediatric facial trauma.
Materials and Methods
Database Creation
648 incidents from 644 charts of pediatric patients less than 18 years of age who sustained a facial fracture from January 1, 2020 to December 31, 2022 and were cared for at Atrium Health Wake Forest Baptist in Winston Salem, North Carolina were included in the database. Four patients each had 2 separate facial trauma incidents documented. There were 1046 documented incidents with the ICD-10 code of S02 (Fracture of Skull and Facial Bones) during 2020-2022, but 398 were excluded due to a lack of recorded facial trauma or because care took place at a location other than AHWFB (Table 1). Data was obtained from AHWFB’s Epic system.
Table 1.
Number of Incidents Before and After Application of Inclusion Criteria.
| 2020 | 2021 | 2022 | |
| Number of ICD-10 S02 Incidents | 362 | 373 | 311 |
| Number of Excluded Incidents | 145 | 128 | 125 |
| Number of Incidents Included in Database | 217 | 245 | 186 |
Variables of interest included demographic information, past medical and surgical history, trauma history, interventions, and long-term outcomes such as scarring, deformities, and sensory or motor deficits (Supplemental Information A). Mechanism of trauma was differentiated into high-energy vs low-energy. High-energy mechanism of injury included motor vehicle accidents (MVA) greater than 25 mile/h, penetrating injuries, significant blunt force trauma (hit with a metal object, trapped under a large object) significant assault (fights, attacks), and falls from ≥10 feet for ages ≥6 years or ≥5 feet for ages <6 years. The type (bone, soft tissue, dental, brain, etc.) and anatomical location of trauma, concomitant injuries, and, if applicable, complications and follow-up appointments were also recorded.
Study data was collected and managed using REDCap (Research Electronic Data Capture) software hosted at Wake Forest University School of Medicine. REDCap “is a secure, web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources.”13,14
Data Analysis
An institutional review board-approved retrospective analysis was conducted in which the number of visits to AHWFB for pediatric facial trauma for each zip code in North Carolina (n = 133) was recorded and compared with data from the 2021 American Community Survey from the US Census Bureau. 15 Included statistics were the percentage of unemployment, mean household income (dollars), and percentage of people whose income in the past 12 months was below the poverty level for each zip code (n = 131) (Supplemental Information B). Two zip codes were excluded due to a lack of available SES data. This data was inputted into IBM’s SPSS software for statistical analysis. 16 Bivariate correlation analysis was ran between: number of incidents per zip code and unemployment percentage; number of incidents per zip code and mean household income; number of incidents per zip code and percentage below the poverty level. Correlations were computed for all zip codes (n = 131) as well as only the zip codes for Forsyth County (the county housing AHWFB) and surrounding counties (Stokes, Yadkin, Davie, Davidson, Guilford, Surry, and Rockingham) (n = 58) in the central Piedmont region of North Carolina. Figure 1 below shows a geographical representation of the counties. 17 Then, incidents due to high-energy injuries from Forsyth and surrounding counties were further broken down to analyze the distribution of specific high-energy incidents across varying socioeconomic statuses.
Figure 1.
Map of the Counties of North Carolina. Red dot represents Forsyth County, the county in which AHWFB resides.
Results
The sample of patients seen at AHWFB for pediatric facial trauma contained 648 incidents. The average age was 7.85 years (SD = 6.39). Sixty-three percent were male, 63.1% were White/Caucasian, 18.5% were Black/African American, and 13.1% were Hispanic/Latino. Seventeen percent required a social worker and 6% required a translator.
Thirty-five percent of cases required transfer from another hospital for advanced care and the average length of hospital stay for initial treatment was 2.65 days (SD = 8.82). Thirty-five percent of patients sustained a high-energy mechanism of injury, and 65% sustained a low-energy mechanism of injury. Of the cases of high-energy injuries, 40.8% were involved in a high-speed (>25 mile/h) MVA, 19.3% sustained significant blunt force trauma, 18.4% sustained a fall, 11.4% sustained a penetrating injury, 8.8% of cases were due to a pedestrian being struck, and 3.1% were a victim of significant assault/non-accidental trauma. Of the cases of low-energy injuries, 48.2% sustained a fall, 34.4% were due to minor-moderated blunt force, 13.3% were due to assault/non-accidental trauma, and 7.4% were involved in a low-speed (<25 mile/h) MVA. The percentages of specific low and high-energy injuries total more than 100% because some incidents comprised more than 1 mechanism of injury. For example, a patient sustaining a penetrating injury from a windshield during a high-speed car accident would be categorized under both a high-speed MVA and a penetrating injury. Of all MVAs, 16.2% had inappropriate or no seatbelt use, 8.8% of children were not in a proper car seat, and 8.1% included airbag deployment.
Seventy-five percent of patients sustained solely facial fractures and the average number of facial fractures sustained per patient was 1.63 (SD = 1.53); the other 25% sustained either no facial fracture or a facial fracture in addition to an injury of the soft tissue, teeth, eye, ear, togue, brain, or cervical spine. Thirty-four percent of patients required surgical intervention and 34.3% were admitted to the ICU. Post-trauma, 35% of patients had known complications, such as facial deformity (any difference in facial appearance compared to before the trauma) (24.7%), concussion (22%), scarring (16.3%), airway/nasal airway obstruction (13.2%), headaches (12.8%), and seizures (11.5%). Seventy-one percent of patients attended follow-up appointments, whereas 10.8% were lost to follow-up. Less than 1% of traumas were due to a suicide attempt and 1.7% of traumas resulted in mortality.
Of the 644 patients who visited AHWFB for pediatric facial trauma during the years of 2020-2022, 610 (94.7%) of the incidents occurred to patients residing in a North Carolina zip code. Of the 610 incidents, 444 occurred to patients residing in the home county of AHWFB and surrounding counties. These counties comprised 68.9% of the total incidents recorded and 130 (29.3%) of these were due to a high-energy injury. The correlations between the number of incidents per zip code and SES factor for all zip codes are shown in Table 2, with correlations closer to −1 and 1 representing a stronger relationship. When all zip codes were analyzed, there were no significant correlations between the number of incidents and unemployment, income, or poverty.
Table 2.
Correlations of all zip codes (n=131) of pediatric facial trauma incidents with SES.
| % Unemployed | Mean Household Income | % Below Poverty | |
|---|---|---|---|
| # Incidents | 0.107 (P = 0.225) | 0.019 (P = 0.825) | 0.139 (P = 0.113) |
When the geographical area of residence was narrowed to the home county of AHWFB and surrounding counties, it was found that there were significantly more incidents of pediatric facial trauma in areas with more poverty (P < 0.01) (Table 3). There were more incidents due to high-energy injuries in areas with lower income (P < 0.05) and areas with more poverty (P < 0.01) (Table 3).
Table 3.
Correlations of the zip codes (n=58) in the counties surrounding and including Forsyth County with SES.
| % Unemployed | Mean Household Income | % Below Poverty | |
|---|---|---|---|
| # Incidents | 0.213 (P = 0.108) | −0.176 (P = 0.185) | 0.357** (P = 0.006) |
| # High-energy incidents | 0.231 (P = 0.081) | −0.266* (P = 0.044) | 0.403** (P = 0.002) |
*Correlation is significant at the 0.05 level (2-tailed). **Correlation is significant at the 0.01 level (2-tailed).
Correlations of factors of socioeconomic status with specific high-energy mechanisms are shown in Table 4. The category of penetrating injuries was separated into dog attacks and gunshot wounds (GSW). All-terrain vehicle (ATV) accidents were separated as a distinct category from motor vehicle accidents, which pertained to cars. It was found that motor vehicle accidents were more common in areas with lower income (P < 0.05) and more poverty (P < 0.01). No other significant correlations were found between SES and a specific high-energy mechanism of injury.
Table 4.
Correlations of high-energy incidents (n=37) with SES from zip codes (n=58) of Forsyth and surrounding counties.
| % Unemployed | Mean Household Income | % Below Poverty | |
|---|---|---|---|
| MVA | 0.247 (P = 0.141) | −0.392* (P = 0.017) | 0.518** (P = 0.001) |
| Fall 6-17yo | −0.229 (P = 0.173) | −0.048 (P = 0.776) | −0.018 (P = 0.914) |
| Blunt force trauma | 0.120 (P = 0.479) | −0.304 (P = 0.067) | 0.304 (P = 0.067) |
| Pedestrian struck | −0.051 (P = 0.763) | −0.167 (P = 0.322) | −0.165 (P = 0.329) |
| Assault/NAT | 0.160 (P = 0.343) | 0.106 (P = 0.533) | 0.032 (P = 0.851) |
| Fall 0-5yo | 0.070 (P = 0.681) | 0.103 (P = 0.543) | −0.089 (P = 0.602) |
| Dog attack | −0.059 (P = 0.730) | 0.066 (P = 0.699) | −0.112 (P = 0.511) |
| GSW | −0.151 (P = 0.372) | 0.240 (P = 0.153) | −0.031 (P = 0.856) |
| ATV accident | 0.125 (P = 0.463) | −0.146 (P = 0.388) | 0.182 (P = 0.282) |
*Correlation is significant at the 0.05 level (2-tailed). **Correlation is significant at the 0.01 level (2-tailed).
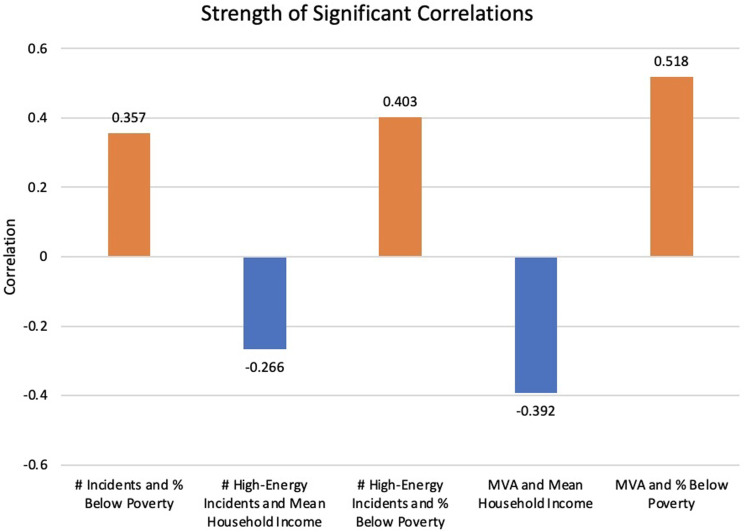
Significant correlations are summarized in Figure 2. The strongest relationship exists between MVAs and poverty compared to total number of incidents and all mechanisms of high-energy incidents.
Figure 2.
Strength of Significant Correlations. Correlations between number of incidents, high-energy incidents, MVAs, income, and poverty are shown. Orange bars represent correlations with p < 0.01 and blue bars represent correlations with p < 0.05.
Discussion
Socioeconomic status can affect the type of trauma that a patient experiences because of the increased risk of exposure and the availability of resources to treat emergent conditions. For example, SES can influence an individual’s level of exposure to dangerous or trauma-inducing events. 18 People with a lower SES may be more likely to experience trauma due to living in high-crime neighborhoods (violence is more common in low SES areas5,19), working in trauma-susceptible manual labor occupations, or having less access to protective resources. In relation to children, parents may not have the resources to provide protection that may prevent or deter facial trauma, such as AAP (American Academy of Pediatrics) recommended car seats, helmets, or adequate adult supervision.20-22 Alternatively, individuals with a higher SES may be less likely to experience these mechanisms of trauma-inducing events.
This study set out to identify a potential relationship between SES and the incidence of pediatric facial trauma in the central Piedmont region of North Carolina. Previous research has theorized that socioeconomic status greatly impacts one’s health status.9,11 This study supports this theory because the results show that within the surrounding counties of AHWFB, there are significantly more incidents of pediatric facial trauma, especially due to high-energy injuries such as motor vehicle accidents, in areas with higher levels of poverty. While motor vehicle accidents were found to predominate in areas with higher poverty levels and lower income, no other high-energy mechanism of injury was significantly correlated to SES. The results align with previous claims that areas of lower SES predispose individuals to trauma-evoking situations, 18 such as those precipitated by the lack of protective motor vehicle safety devices. 20
Analyzing the socioeconomic data by place of residence best shows the distribution of areas where improvement of health maintenance is most needed. 20 Knowing which zip codes have the most pediatric residents incurring facial trauma identifies the need to work to decrease health inequalities. The results highlight discrepancies in exposure to injury-provoking situations to direct efforts to improve preventative measures in areas with more pediatric facial trauma. These results could also shape future budgets and policy to focus attention to the SES distribution so as to not further the divide of health inequality across central North Carolina. For example, as injuries caused by high-speed motor vehicle accidents are more common in areas with increased poverty (P < 0.01) and decreased mean household income (P < 0.05), steps should be taken to prevent these injuries. Proactive steps could include increasing education of the importance of AAP-recommended car seats for each age and offering them at discounted or no cost, and also emphasizing the importance of seatbelts. Large-scale initiatives could include reevaluating the speed limits, traffic signs, and traffic laws to further prevent accidents. Pediatric providers would have the opportunity to address safety issues early on knowing that a patient’s place of residence could put them at a higher risk of facial trauma. During routine health visits for children from areas with greater poverty, educating children and parents about the importance of seatbelts and car seats could help prevent future pediatric facial trauma. Identifying specific areas to concentrate preventative efforts allows for more targeted approaches that can produce the greatest effects. Focusing on providing aid for preventative measures in low SES areas could alter the cycle of lower income/higher poverty areas having to pay additional medical expenses for pediatric facial trauma.
The epidemiological findings of this study are similar to those of others, which shows that this study population may be representative of other geographical areas, even given the smaller sample size. The male/female ratio of the study population (1.7:1) is similar to previous studies which have found that pediatric facial trauma is more common in males.23-25 Other studies investigating the causes of pediatric facial trauma found the most common cause to be falls.23,25 Although this study breaks down the causes by high and low-energy mechanism, overall the most common cause was falls, followed by blunt force trauma and MVAs. These similarities of patient demographics and injury mechanisms may increase the external validity of the data and the results as they align with previous studies.
This study was limited by the number of patients who fit the criteria of pediatric facial trauma in central North Carolina. This study provides guidelines and steps that other hospitals can implement to determine similar findings in their patient population. While this study focuses on pediatric patients, future studies could analyze the relationship between SES and adult patients. The timeframe or anatomical location of injury could also be expanded to include a greater number of patients. The database created and used for this study has the potential to answer many other research questions about demographic variables, treatment, and follow-up care due to the extent of recorded information.
In conclusion, mean household income and poverty levels affect the incidence of pediatric facial trauma in central North Carolina. High-speed motor vehicle accidents are the only high energy mechanism of trauma that correlate with income and poverty. These findings are consistent with previous research of SES’s effect on health inequalities and serve as evidence of the need to take steps to prevent pediatric facial trauma in areas of low SES.
Supplemental Material
Supplemental Material for The Impact of Socioeconomic Status on Pediatric Facial Trauma by Avery Wright, Madison Hinson, Amelia Davidson, Caitrin Curtis, and Christopher Runyan in Craniomaxillofacial Trauma & Reconstruction
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online
ORCID iDs
Avery Wright https://orcid.org/0000-0002-6453-6272
Madison Hinson https://orcid.org/0000-0001-6992-2909
References
- 1.Andrew TW, Morbia R, Lorenz HP. Pediatric facial trauma. Clin Plast Surg. 2018;46(2):239-247. [DOI] [PubMed] [Google Scholar]
- 2.Flynn-O'Brien KT, Fallat ME, Rice TB. et al. Pediatric trauma assessment and management database: leveraging existing data systems to predict mortality and functional status after pediatric injury. J Am Coll Surg. 2017;224(5):933-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tew K, You J, Pircher S. Validation of patient demographic data, Northern Territory hospitals, 2008. Health Gains Planning, DHF. 2008. [Google Scholar]
- 4.Ryan ML, Thorson CM, Otero CA. et al. Pediatric facial trauma: a review of guidelines for assessment, evaluation, and management in the emergency department. J Craniofac Surg. 2011;22(4):1183-1189. [DOI] [PubMed] [Google Scholar]
- 5.Alcalá-Galiano A, Arribas-García IJ, Martín-Pérez MA, Romance A, Montalvo-Moreno JJ, Juncos JM. Pediatric facial fractures: children are not just small adults. Radiographics. 2008;28(2):441-461. [DOI] [PubMed] [Google Scholar]
- 6.Imahara SD, Hopper RA, Wang J, Rivara FP, Klein MB. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg. 2008;207(5):710-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braun TL, Xue AS, Maricevich RS. Differences in the management of pediatric facial trauma. Semin Plast Surg. 2017;31(2):118-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Svider PF, Bobian M, Hojjat H. et al. A chilling reminder: pediatric facial trauma from recreational winter activities. Int J Pediatr Otorhinolaryngol. 2016;87:78-82. doi: 10.1016/j.ijporl.2016.05.025 [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . (nd) Social Determinants of Health. World Health Organization. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 [Google Scholar]
- 10.Centers for Disease Control and Prevention . NCHHSTP Social Determinants of Health. Centers for Disease Control and Prevention; 2019. https://www.cdc.gov/nchhstp/socialdeterminants/faq.html#:∼:text=An_individual%27s_socioeconomic_position_can,the_communities_they_interact_wit [Google Scholar]
- 11.Shin EK, Mahajan R, Akbilgic O, Shaban-Nejad A. Sociomarkers and biomarkers: predictive modeling in identifying pediatric asthma patients at risk of hospital revisits. NPJ Digit Med. 2018;1:50. doi: 10.1038/s41746-018-0056-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCann A. Cities with most & least economic class diversity. WalletHub. 2021. from. https://wallethub.com/edu/cities-with-the-most-least-economic-class-diversity/10321. Retrieved January 8, 2023. [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Minor BL, REDCap Consortium et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.U.S. Census Bureau . DP03: selected economic characteristics. 2022. Retrieved from. https://data.census.gov/table?t=Employment
- 16.IBM Corp. Released . IBM SPSS Statistics for Macintosh, Version 28.0. Armonk, NY: IBM Corp; 2021. [Google Scholar]
- 17.Rudersdorf A. NC County Maps. Government & Heritage Library, State Library of North Carolina; 2010. [Google Scholar]
- 18.Chen P, Voisin DR, Jacobson KC. Community violence exposure and adolescent delinquency: examining a spectrum of promotive factors. Youth Soc. 2016;48(1):33-57. doi: 10.1177/0044118x13475827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Psychological Association . (nd). Violence & Socioeconomic Status. American Psychological Association. Retrieved January 10, 2023, from. https://www.apa.org/pi/ses/resources/publications/violence#:∼:text=Interpersonal_Violence,suffering_from_detrimental_future_outcomes [Google Scholar]
- 20.Hletko PJ, Hletko JD, Shelness AM, Robin SS. Demographic predictors of infant car seat use. Am J Dis Child. 1983;137(11):1061-1063. doi: 10.1001/archpedi.1983.02140370023008 [DOI] [PubMed] [Google Scholar]
- 21.Webman R, Dultz LA, Simon RJ. et al. Helmet use is associated with safer bicycling behaviors and reduced hospital resource use following injury. J Trauma Acute Care Surg. 2013;75(5):877-881. doi: 10.1097/ta.0b013e3182a85f97 [DOI] [PubMed] [Google Scholar]
- 22.Li X, Feigelman S, Stanton B. Perceived parental monitoring and health risk behaviors among urban low-income African-American children and adolescents. J Adolesc Health. 2000;27(1):43-48. doi: 10.1016/s1054-139x(99)00077-4 [DOI] [PubMed] [Google Scholar]
- 23.Li Z, Li Z-B. Characteristic changes of pediatric maxillofacial fractures in China during the past 20 Years. J Oral Maxillofac Surg. 2008;66(11):2239-2242. doi: 10.1016/j.joms.2007.12.032 [DOI] [PubMed] [Google Scholar]
- 24.Gassner R, Tuli T, Hächl O, Moreira R, Ulmer H. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg. 2004;62(4):399-407. doi: 10.1016/j.joms.2003.05.013 [DOI] [PubMed] [Google Scholar]
- 25.Boffano P, Roccia F, Zavattero E. et al. European maxillofacial trauma (EURMAT) project: a multicentre and prospective study. J Cranio-Maxillo-Fac Surg. 2015;43(1):62-70. doi: 10.1016/j.jcms.2014.10.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for The Impact of Socioeconomic Status on Pediatric Facial Trauma by Avery Wright, Madison Hinson, Amelia Davidson, Caitrin Curtis, and Christopher Runyan in Craniomaxillofacial Trauma & Reconstruction