Abstract
Study Design
This is a retrospective study using the Nationwide Emergency Department Sample.
Objective
Facial laceration repairs are one of the most common procedures performed in the emergency department (ED). The goal of this study was to describe the patient’s characteristics and healthcare cost associated with ED encounters for facial lacerations using the largest nationally representative database in the United States.
Methods
This is a retrospective study using the Nationwide Emergency Department Sample. The data was collected between January and December of 2019. Patients with either a primary or secondary diagnosis of facial laceration were included. The primary outcome was patient characteristics. The secondary outcomes were ED characteristics, number and type of procedures performed and total encounter charges. Diagnoses and procedures were identified using ICD-10 CM codes.
Results
There were 2,548,944 ED encounters for facial lacerations in the United States. Of those, laceration was the chief complaint in 75%. 80% of lacerations were unintentional, 8% were due to assaults, and <1% due to suicidal attempts. The most common laceration location was the scalp (21%) followed by the lip (11%) and eyelid (11%). The mean patient age was 38 years. Most patients were adults (69%), male (62%), Caucasian (64%, African American 14%, Hispanic 14%, Other 4%, Asian 2%), from low income levels ($1–$45,999: 29%, $46,000– $58,999: 24%, $59,000–$78,999: 24%, $79,000 or more: 23%), with private insurance (32%, Medicaid 25%, Medicare 24%, self-pay 12%, other 6%). Most encounters were during summer (June, July, August) at large metropolitan areas with at least 1 million residents (52%, small metropolitan: 30%, micropolitan: 10%, other: 7%) at teaching hospitals (65%) located in the southern region of the United States (37%, Midwest: 23%, west: 21%, northeast: 19%). Almost half of the encounters were at non-trauma-designated hospitals (48%, Level 1 trauma center: 21%, Level 2 trauma center: 17%, Level 3 trauma center: 13%). The number of procedures during each encounter was: none: 4%, one: 17%, two: 23%, three: 11%, four: 11%, five or more: 28%. The most frequent laceration repair was a simple repair of superficial wounds of the face, ears, eyelids, nose, lips, and/or mucous membranes 2.5 cm or less, followed by simple repair of superficial wounds to the scalp, neck, axillae, external genitalia, trunk, and/or extremities 2.5 cm or less. Most emergency department visits were billed as a Level 3 encounter, followed by Level 2 then Level 4. CT scan of the head was the most common imaging modality. Of all patients, <1% were admitted to the hospital and 87% were discharged home. The average total emergency department charges were $5,733.
Conclusions
Facial laceration is a common complaint in the emergency department. It is costly, and disproportionately affects the impoverished. Most lacerations are classified as simple, less than 2.5 cm, involving the scalp, unintentional, with the discharge disposition being home. Thus, exploring pathways to treat facial lacerations outside of the ED can potentially reduce both healthcare cost and ED crowding.
Keywords: laceration, face, emergency department, plastic surgery, incidence, characterization
Introduction
Every year approximately 8 million emergency department visits in the US include evaluation and treatment of lacerations. 1 Of these encounters, almost 30% involve lacerations of the face (Loder RT). 2 The etiology of these injuries can have great variance, with notable causes including motor vehicle collisions, assault, falls, and sports.3,4 As such, prior studies have identified modifiable factors to reduce these risks, especially amongst the pediatric and geriatric populations.5,6 1 study focusing on emergency room visits due to interpersonal violence found a 17% incidence of lacerations, with 61% of these involving the head and neck (Loder RT). 2 Interestingly, Roccia et al 4 found that male to female ratios of patients with facial lacerations varied with regard to traumatic causes, with 1.5:1 for falls, 3:1 for sports, 10:1 for assaults, and 1.7:1 for motor vehicle collisions, respectively. Of note, most facial lacerations are observed over the “T” area, which includes the forehead, upper orbit, nose, lips, and chin.4,7
Recent literature estimates these visits cost over 3 billion US dollars each year, not including the additional cost of subsequent complications and infections that affect up to 5% of patients.8,9 Previous studies have primarily focused on wound characteristics and patient comorbidities, as well as timing and decision making considerations for delayed wound closure.10–12 However, there is a lack of objective data examining secondary factors that can guide treatment. In this study, we sought to characterize facial laceration patient characteristics utilizing the Nationwide Emergency Department Sample (NEDS) to identify emergency department characteristics, amount and type of procedures performed during visits, and total encounter charges and costs.
Methods
Data Source and Study Design
This retrospective observational study draws upon data sourced from the 2019 Nationwide Emergency Department Sample. The NEDS stands as an extensive database crafted and maintained by the Healthcare Cost and Utilization Project. This project constitutes a collaborative endeavor involving partnership between federal, state, and industry entities under the sponsorship of the Agency for Healthcare Research and Quality. 13 Being the most expansive publicly accessible database of its kind in the United States, the NEDS records over 28 million unweighted visits to emergency departments annually, which translates to an estimated 123 million weighted visits. The database is a representative cross-section of the nation and derives its information from both State Inpatient Databases and State Emergency Department Databases. It encompasses details about patients who receive treatment in the emergency department and are either discharged or admitted to the same hospital. In total, 40 states and the District of Columbia contribute to the NEDS, making it a roughly 20% stratified sample of emergency departments owned by hospitals across the United States. Moreover, the NEDS provides insights into primary and secondary diagnoses as well as procedures carried out during the hospital stay. The study received an exemption from the Fox Chase Cancer Center Institutional Review Board approval process (IRB number 23-9926) due to its utilization of de-identified pre-existing data, thereby ensuring the safeguarding of patient privacy and confidentiality.
Study Population
Within this investigation, the study population consisted of individuals with a primary or secondary diagnosis of facial laceration. This analysis did not encompass patients with open wounds, and specifically included lacerations of the face and scalp. The eligible facial laceration patients were selected for using the dedicated ICD-10 CM codes, which are detailed in Appendix A.
Outcomes
The primary emphasis of the investigation revolved around assessing the aggregate number of ED visits for facial laceration repair during the year 2019 utilizing the NEDS database. In conjunction with this principal result, the study also scrutinized various secondary results. These encompassed the rate of admissions within the hospital, the overall costs and charges incurred within the ED, and the prevailing Current Procedural Terminology (CPT) codes most frequently employed in the ED setting. We examined both the overall most common CPT codes as well as laceration-specific repair CPT codes. To ensure precise and comparable evaluations across different time spans, all expenses were appropriately modified for inflation employing the consumer price index.
Study Variables
The dataset encompasses both patient-level and hospital-level characteristics. Patient-level particulars comprise age, sex, insurance provider, discharge disposition, and financial metrics like overall emergency department expenses and duration of hospitalization. Hospital-level data entails hospital teaching classification, urban or rural categorization, and geographical region. Additionally, the NEDS furnishes details about hospital trauma classification, comprehensive emergency department expenses, and the patient’s ethnicity. The in-hospital mortality rate is indicated by the patient’s vital status upon discharge. Total emergency department charges and length of stay are directly documented within the NEDS. The total emergency department charges signify the sum billed by the hospital for the services delivered throughout the patient’s interaction, while the total emergency department costs denote the sum the hospital disbursed for the services provided.
Statistical Analysis
The statistical examination was designed with STATA MP, version 14.0 (STATACorp, College Station, TX). STATA’s svyset and svy commands were employed to accommodate the intricacies of the sampling design, resulting in nationally representative variance estimates, unbiased results, and P-values.
Results
Patient Characteristics
Patient Characteristics
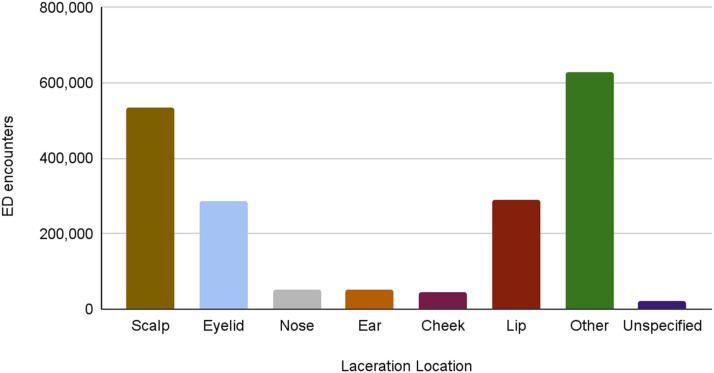
In our cohort, we identified 2,548,944 facial lacerations. The distribution of these lacerations saw 25% categorized as “other,” with the scalp being the most common specified location at 21%. Lacerations on the lip and eyelid each accounted for 11% (Figure 1). The average age of patients was 37 years, with the predominant demographic being Caucasian 64% and males 62%. Patient characteristics are summarized in Table 1. When assessing median income based on patients’ zip codes, the distribution was nearly equal in all income quartiles. Healthcare coverage revealed that half of the patients relied on Medicare (24%) or Medicaid (25%), with private insurance covering 32%. We found that 87% of patients were discharged to their homes post-treatment. Most injuries were primary facial lacerations stemming from unintentional causes, with only 8% resulting from assault (Table 1). Over half of the patients underwent at least 1 procedure in the Emergency Department, and 28% underwent 6 or more procedures. Total cost and charge in ED was $750 and $5733 respectively.
Figure 1.
Facial laceration distribution.
Table 1.
Patient Characteristics.
| Patient Characteristics | % (n) (2,548,944) |
|---|---|
| Age | 37 years (range: 36.9 - 39.1) |
| Female | 38% (964,360) |
| Race | |
| Caucasian | 64% (1,644,069) |
| African American | 14% (359,410) |
| Hispanic | 14% (364,499) |
| Asian | 2% (61,175) |
| Other | 6% (152,937) |
| Median income in the patient’s zip code | |
| $1–$45,999 | 29% (739,194) |
| $46,000– $58,999 | 24% (611,747) |
| $59,000–$78,999 | 24% (606,649) |
| $79,000 or more | 23% (581,159) |
| Primary payer | |
| Medicare | 24% (624,491) |
| Medicaid | 25% (647,432) |
| Private | 32% (823,309) |
| Self-pay | 12% (300,775) |
| Other | 6% (152,937) |
| Weekend encounter | 32% (808,015) |
| Encounter season | |
| Winter | 23% (586,257) |
| Spring | 25% (637,236) |
| Summer | 27% (688,215) |
| Fall | 25% (637,236) |
| Disposition from ED | |
| Discharge home | 87% (2,215,032) |
| Transfer to short-term hospital | 2% (44,861) |
| Other transfers, eg, skilled nursing facility, intermediate care | 2% (46,646) |
| Admitted as an inpatient to this hospital | 8% (209,013) |
| Died in ED | <1% (2266) |
| Against Medical Advice | 1% (23,527) |
| Total charge in ED | $5733 |
| Total cost in ED | $750 |
| Number of ED procedures | |
| 0 | 4% (95,331) |
| 1 | 17% (439,183) |
| 2 | 23% (586,257) |
| 3 | 11% (269,168) |
| 4 | 11% (267,639) |
| 5 | 6% (161,348) |
| 6 or more | 28% (713,704) |
| Adult | 69% (1,758,771) |
| Primary facial laceration | 75% (1,899,983) |
| Secondary facial laceration | 25% (648,961) |
| Intent of Injury | |
| Assault | 8% (199,837) |
| Unintentional | 80% (2,049,351) |
| Intentional | <1% (5863) |
Hospital Characteristics
Of the ED visits, 65% were to large metropolitan teaching hospitals. In terms of governance, 52% of hospitals identified as private non-profit and voluntary institutions. It’s worth noting that 48% of the cases were handled at non-trauma centers. From a geographical standpoint, the South accounted for the largest share of cases at 37%, with the Midwest following at 23% (Table 2).
Table 2.
Hospital Characteristics.
| Hospital Characteristics | % (n) |
|---|---|
| Hospital urban-rural location | |
| large Metropolitan areas with at least 1 million residents | 52% (1,335,647) |
| small Metropolitan areas with less than 1 million residents | 30% (777,428) |
| micropolitan Areas | 9% (231,954) |
| not Metropolitan or micropolitan | 7% (178,426) |
| Hospital Control | |
| government or private | 14% (369,597) |
| government, non-federal, public | 12% (313,520) |
| private, nonprofit, voluntary | 52% (1,320,353) |
| private, invest-own | 11% (275,286) |
| private, collapsed category | 11% (270,188) |
| Hospital region | |
| Northeast | 19% (479,201) |
| Midwest | 23% (593,904) |
| South | 37% (950,756) |
| West | 21% (525,082) |
| Hospital Trauma Center level | |
| Nontrauma center | 48% (1,233,689) |
| Trauma level 1 | 21% (530,180) |
| Trauma level 2 | 17% (435,869) |
| Trauma level 3 | 13% (331,363) |
| Teaching status of hospital | |
| Metropolitan Nonteaching | 20% (512,338) |
| Metropolitan Teaching | 65% (1,656,814) |
| Nonmetropolitan | 15% (384,891) |
Emergency Department Procedures
Predominant ED procedures included evaluation and management level 3, simple repair of superficial facial wounds less than 2.5 cm, and evaluation and management level 2. These are outlined in Tables 3 and 4. Delving deeper into laceration repairs, the most frequent lacerations repaired in the ED were on the face and mucous membranes measuring less than 2.5 cm. This was followed by wounds on the scalp, neck, axillae, external genitalia, trunk, or extremities, and then by simple repairs of superficial facial wounds ranging from 2.6 cm to 5.0 cm (Table 4). Additionally, it is noteworthy to mention that intermediate/complex repairs were not among the most frequent laceration repairs until the fifth to 10th positions in frequency.
Table 3.
Most Common ED Procedures.
| CPT Codes | Description | No. |
|---|---|---|
| 1. 99283 | ED visit for evaluation and management level 3 | 346,483 |
| 2. 12011 | Simple repair of superficial wounds to the face, ears, eyelids, nose, lips, and/or mucous membranes, 2.5 cm or less in size | 292,865 |
| 3. 99282 | ED visit for evaluation and management level 2 | 267,021 |
| 4. 99284 | ED visit for evaluation and management level 4 | 215,885 |
| 5. 70450 | CT scanning, of the head or brain, without contrast | 195,371 |
| 6. 12001 | Simple repair of superficial wounds to the scalp, neck, axillae, external genitalia, trunk, and/or extremities (including the hands and feet), 2.5 cm or less in size | 115,246 |
| 7. 72125 | CT, examination of the cervical spine without contrast | 111,140 |
| 8. 99285 | ED visit for evaluation and management level 5 | 97,250 |
| 9. 12013 | Simple repair of superficial wounds to the face, ears, eyelids, nose, lips and/or mucous membranes, 2.6 to 5.0 cm in size | 76,555 |
| 10. 99281 | ED visit for evaluation and management level 1 | 76,170 |
Table 4.
Most Common Laceration Repairs in the ED.
| CPT Codes | Description | No. |
|---|---|---|
| 1. 12011 | Simple repair of superficial wounds to the face, ears, eyelids, nose, lips, and/or mucous membranes, 2.5 cm or less in size | 292,865 |
| 2. 12001 | Simple repair of superficial wounds to the scalp, neck, axillae, external genitalia, trunk, and/or extremities (including the hands and feet), 2.5 cm or less in size | 115,246 |
| 3. 12013 | Simple repair of superficial wounds to the face, ears, eyelids, nose, lips and/or mucous membranes, 2.6 to 5.0 cm in size | 76,555 |
| 4. 12002 | Simple repair of superficial wounds to the scalp, neck, axillae, external genitalia, trunk, and/or extremities (including the hands and feet), 2.6 to 7.5 cm in size | 62,901 |
| 5. 12051 | Intermediate repair of wounds to the face, ears, eyelids, nose, lips, and/or mucous membranes, 2.5 cm or less in size | 13,765 |
| 6. 12052 | Simple repair of superficial wounds to the scalp, neck, axillae, external genitalia, trunk, and/or extremities (including the hands and feet), 2.6 to 7.5 cm in size | 12,126 |
| 7. 12014 | Simple repair of superficial wounds to the face, ears, eyelids, nose, lips, and/or mucous membranes, 5.1 to 7.5 cm in size | 8354 |
| 8. 12004 | Simple repair of superficial wounds to the scalp, neck, axillae, external genitalia, trunk, and/or extremities (including the hands and feet), 7.6 to 12.5 cm in size | 5954 |
| 9. 12015 | Simple repair of superficial wounds to the face, ears, eyelids, nose, lips, and/or mucous membranes, 7.6 to 12.5 cm in size | 3602 |
| 10. 13132 | Repair, complex, forehead, cheeks, chin, mouth, neck, axillae, genitalia, hands and/or feet | 3454 |
Discussion
Facial lacerations continue to be a common reason for visiting an emergency department in the United States. Previous work has primarily focused on characterizing facial lacerations. Here, we performed a retrospective analysis utilizing the largest emergency department database, the Nationwide Emergency Department Sample, to analyze patient, treatment center, and procedural characteristics between January and December of 2019 to better understand patterns in management. We recorded over 2.5 million cases of facial lacerations during this time interval.
The incidence of facial lacerations is more common amongst males, with rates of 60%–80% commonly reported.2,3,7,12,14,15 Our data reflected this national trend, as 62% of patients were male. While the differential as to why males are more commonly affected may be broad, the answer may lie in behavioral patterns. Eaton et al 16 demonstrated that compared to females, males were more likely to not wear seatbelts or helmets, drive after drinking alcohol, use illicit drugs, carry deadly weapons, and be in physical fights. We did not find a significant difference amongst white, black, hispanic, and asian patients. The percentage of patient laceration races closely resembled population percentages of the US.
When examining patient age, facial lacerations affected a wide range of age groups. Interestingly, the etiology of facial lacerations varies significantly with age. Kim et al 6 demonstrated this in their study which revealed adults aged 65 and greater account for 58% of at-home injuries, with the incidence of at-home accidents increasing with age. Falls, along with the overall most common factor, motor vehicle collisions, remain the most common cause of facial laceration in this population, accounting for approximately 80% of cases. 4 We noted approximately 30% of cases occurred in the pediatric population (age <18 years), which coincides well with published literature. 17 We did not observe a significant discrepancy in facial laceration incidence when comparing the seasons which might be expected given sports and play contribute to pediatric trauma. 17
Our research reveals that assaults contribute to less than 10% of facial laceration cases. This finding aligns with prior studies indicating that deliberate interpersonal violence is responsible for only 10%-15% of such injuries.4,18 Moreover, our study highlights that over half of facial laceration treatments are performed in urban areas with populations exceeding 1 million, and more than 80% of these procedures take place in facilities that serve over fifty thousand individuals.
While many repairs were coded as simple, presentation in the emergency department for over 2.5 million facial lacerations represents a significant burden to the US healthcare system. Over half of the repairs took place in non-profit, private facilities, with an average service charge of nearly $6000. With most encounters (28%) involving 6 or more procedures, the high cost of simple laceration repair is evident. It is salient to consider the balance between outcomes, cost, and patient satisfaction. Most facial laceration repairs occurred in hospitals serving populations of over 50,000 residents. In a busy emergency department, timely management of wound evaluation, washout, and closure may be challenging. Longer ED wait times decrease patient satisfaction.19,20 Most facial lacerations occur in the “T zone” (21%), eyelids (11%), and lips (11%)7; and patients often prefer plastic surgeons over emergency room physicians for repairs for optimal aesthetic, and functional repairs may require higher specialized levels of expertise. 21
In these larger hospitals, it is likely that a plastic surgeon is more accessible. Patient satisfaction decreases with longer wait times, and there are proposed mechanisms to mitigate cost and streamline access to a plastic surgeon.19,20 Recent work by Cullen et al has begun to elucidate an alternative management pathway to that of emergency physician repair. In their prospective study, they found having a dedicated plastic surgery procedural area provided significant savings in cost to the patients and the institution, and decreased hospital length of stay. 22 They demonstrated the feasibility to streamline patients in this fast-track repair pathway and thus decrease the resource burden associated with admission and wait times. Patients seen in this setting with delayed wound closure did not incur higher risks of infection with simple lacerations. 23 While this pathway may result in increased access to plastic surgeon repairs, relevant considerations include the cost of having a specialized practitioner available at-will to perform the procedure, determination of what necessitates that degree of care, and whether or not this could be performed in a different setting. If accessible, this could be transitioned to an office-based setting to further mitigate financial and time cost. These changes may also increase the availability of emergency department providers to other higher acuity encounters. We recognize that historically most laceration repairs have been managed by emergency department staff whose services provide adequate outcomes and have been sustainable for a long time. However, we aim to bring to light the possibility and relevance of changes in these methods. While these alternative treatment systems may not be available at every institution, they merit acknowledgement as creative solutions to common emergency room procedures.
Conclusion
Facial lacerations remain a prevalent cause of emergency department visits across the nation. Given the prolonged patient waiting times, time limitations faced by ED physicians, crowding in emergency departments, and the substantial cost associated with repairs, there is a pressing need for alternative management approaches. One proposed solution involves referral for treatment by a plastic surgeon outside of the emergency department or the establishment of a fast-track in-hospital surgical service for accelerated repairs, particularly in high-volume centers. However, various factors intrinsic to hospital settings, including costs and implementation challenges, must be carefully considered. Thus, we suggest this as a potential alternative management pathway option in specific circumstances.
Appendix A.
Table A1.
ICD 10-CM Codes Used.
| ICD-10 CM Diagnostic Code | Description |
|---|---|
| S01.01XX | Laceration without foreign body of scalp |
| S01.02XX | Laceration with foreign body of scalp |
| S01.11XX | Laceration without foreign body of eyelid and periocular area |
| S01.12XX | Laceration with foreign body of eyelid and periocular area |
| S01.21XX | Laceration without foreign body of nose |
| S01.22XX | Laceration with foreign body of nose |
| S01.31XX | Laceration without foreign body of ear |
| S01.32XX | Laceration with foreign body of ear |
| S01.41XX | Laceration without foreign body of cheek and temporomandibular area |
| S01.42XX | Laceration with foreign body of cheek and temporomandibular area |
| S01.51XX | Laceration of lip and oral cavity without foreign body |
| S01.52XX | Laceration of lip and oral cavity with foreign body |
| S01.81XX | Laceration without foreign body of other part of head |
| S01.82XX | Laceration with foreign body of other part of head |
| S01.91XX | Laceration without foreign body of unspecified part of head |
| S01.92XX | Laceration with foreign body of unspecified part of head |
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Sthefano Araya https://orcid.org/0000-0002-8245-8036
Lindsay Talemal https://orcid.org/0000-0002-5692-6211
Jake Siegel https://orcid.org/0000-0003-2430-9224
References
- 1.Singer AJ, Thode HC, Hollander JE. National trends in ED lacerations between 1992 and 2002. Am J Emerg Med. 2006;24(2):183-188. doi: 10.1016/j.ajem.2005.08.021 [DOI] [PubMed] [Google Scholar]
- 2.Loder RT, Momper L. Demographics and fracture patterns of patients presenting to US emergency departments for intimate partner violence. JAAOS Glob Res Rev. 2020;4(2):e20. doi: 10.5435/JAAOSGlobal-D-20-00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laski R, Ziccardi VB, Broder HL, Janal M. Facial trauma: A recurrent disease? The potential role of disease prevention. J Oral Maxillofac Surg. 2004;62(6):685-688. doi: 10.1016/j.joms.2003.12.008 [DOI] [PubMed] [Google Scholar]
- 4.Roccia F, Bianchi FA, Zavattero E, Baietto F, Boffano P. Etiology and patterns of facial lacerations and their possible association with underlying maxillofacial fractures. J Craniofac Surg. 2011;22(6):e19-e23. doi: 10.1097/SCS.0b013e31822ec934 [DOI] [PubMed] [Google Scholar]
- 5.Hwang K, Huan F, Hwang PJ, Sohn IA. Facial lacerations in children. J Craniofac Surg. 2013;24(2):671-675. doi: 10.1097/SCS.0b013e31828026d8. [DOI] [PubMed] [Google Scholar]
- 6.Kim EJ, Bustos VP, Lee BT. Sources of facial injury across age groups: A Nationwide overview using the national electronic injury surveillance system database. J Craniofac Surg. 2023;34(7):1927-1930. doi: 10.1097/SCS.0000000000009582 [DOI] [PubMed] [Google Scholar]
- 7.Sethi RKV, Kozin ED, Fagenholz PJ, Lee DJ, Shrime MG, Gray ST. Epidemiological survey of head and neck injuries and trauma in the United States. Otolaryngol Neck Surg. 2014;151(5):776-784. doi: 10.1177/0194599814546112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nawar EW, Niska RW, Xu J. National hospital ambulatory medical care survey: 2005 emergency department summary. Adv Data 2007;(386):1-32. [PubMed] [Google Scholar]
- 9.Hollander JE, Singer AJ, Valentine SM, Shofer FS. Risk factors for infection in patients with traumatic lacerations. Acad Emerg Med. 2001;8(7):716-720. doi: 10.1111/j.1553-2712.2001.tb00190.x [DOI] [PubMed] [Google Scholar]
- 10.Haughey RE, Lammers RL, Wagner DK. Use of antibiotics in the initial management of soft tissue hand wounds. Ann Emerg Med. 1981;10(4):187-192. doi: 10.1016/S0196-0644(81)80159-X [DOI] [PubMed] [Google Scholar]
- 11.Patel PR, Miller MA. Postcare recommendations for emergency department wounds. Emerg Med Clin. 2007;25(1):147-158. doi: 10.1016/j.emc.2007.01.006 [DOI] [PubMed] [Google Scholar]
- 12.Quinn J, Wells G, Sutcliffe T, et al. A randomized trial comparing octylcyanoacrylate tissue adhesive and sutures in the management of lacerations. JAMA. 1997;277(19):1527-1530. [PubMed] [Google Scholar]
- 13.Healthcare Cost and Utilization Project (HCUP). HCUP National Emergency DepartmentRockville Sample.MDNEDS. Agency for Healthcare Research and Quality; 2022. [Google Scholar]
- 14.Lee JH, Jeon MS, Lee DL, Shin HK, Seul JH. Analysis of patients with facial lacerations repaired in the emergency room of a provincial hospital. Arch Plast Surg. 2015;42(01):34-39. doi: 10.5999/aps.2015.42.1.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lo S, Aslam N. Mechanisms and pattern of facial lacerations in the Accident Department. Int J Clin Pract. 2004;59(3):333-335. doi: 10.1111/j.1742-1241.2004.00308.x [DOI] [PubMed] [Google Scholar]
- 16.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance--United States, 2007. Morb Mortal Wkly Rep Surveill Summ Wash DC. 2008;57(4):1-131. [PubMed] [Google Scholar]
- 17.Shaikh ZS, Worrall SF. Epidemiology of facial trauma in a sample of patients aged 1–18 years. Injury. 2002;33(8):669-671. doi: 10.1016/S0020-1383(01)00201-7 [DOI] [PubMed] [Google Scholar]
- 18.Khan TU, Rahat S, Khan ZA, Shahid L, Banouri SS, Muhammad N. Etiology and pattern of maxillofacial trauma. PLoS One. 2022;17(9):e0275515. doi: 10.1371/journal.pone.0275515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1-10. doi: 10.1111/j.1553-2712.2008.00295.x [DOI] [PubMed] [Google Scholar]
- 20.Key SJ, Thomas DW, Shepherd JP. The management of soft tissue facial wounds. Br J Oral Maxillofac Surg. 1995;33(2):76-85. doi: 10.1016/0266-4356(95)90204-X [DOI] [PubMed] [Google Scholar]
- 21.Zbar RIS, Monico E, Calise A. Consultation for simple laceration repair when on-call in the emergency department: Potential quagmire. Plast Reconstr Surg - Glob Open. 2017;5(7):e1428. doi: 10.1097/GOX.0000000000001428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cullen S, Wrafter PF, Jones D, et al. Plastic surgery procedure unit: A streamlined care model for minor and intermediate procedures: A cost-benefit analysis. J Plast Reconstr Aesthetic Surg. 2021;74(1):192-198. doi: 10.1016/j.bjps.2020.08.100 [DOI] [PubMed] [Google Scholar]
- 23.Zehtabchi S. The role of antibiotic prophylaxis for prevention of infection in patients with simple hand lacerations. Ann Emerg Med. 2007;49(5):682-689.e1. doi: 10.1016/j.annemergmed.2006.12.014 [DOI] [PubMed] [Google Scholar]