Abstract
Background
To compare the efficacy of the direct anterior approach (DAA) versus the posterolateral approach (PLA) in total hip arthroplasty (THA) in terms of operation time, incision length, intraoperative blood loss, postoperative pain, and incision infection rate.
Methods
We systematically searched databases including China National Knowledge Infrastructure (CNKI), Wanfang Data, VIP Chinese sci-tech journals, Chinese Biomedical Literature Database (CBM), PubMed, and Cochrane Library up to December 2023. We included randomized controlled trials (RCTs) that compared DAA with PLA in THA, with a minimum sample size of 80 and a follow-up of at least 6 months. Studies were screened by two independent researchers, following PRISMA guidelines. Data were extracted using a pre-established feature table, capturing study design, sample size, patient demographics, and outcomes of interest. Meta-analysis was performed using RevMan 5.4.1 software. Heterogeneity was assessed using the Q-value statistical test and I² test. The fixed-effects model was used when heterogeneity was low; otherwise, the random-effects model was applied.
Results
A total of 19 RCTs met the inclusion criteria. The Meta-analysis revealed that DAA was associated with a longer operation time [MD = 5.89, 95%CI(2.26 to 9.51), P = 0.001] but resulted in a smaller incision length [MD = -2.99, 95%CI(-3.76 to -2.22), P < 0.00001], less intraoperative blood loss [MD=-108.36, 95%CI(-131.10 to -85.62), P < 0.00001], lower incidence of postoperative incision infection [OR = 0.39, 95%CI(0.19 to 0.83), P = 0.01], and reduced hip Visual Analog Scale (VAS) scores on the 1st and 3rd days postoperatively [MD=-0.85, 95%CI(-0.96 to -0.74), P < 0.00001; MD=-0.60, 95%CI(-1.13 to -0.07), P = 0.03]. No significant difference was observed in VAS scores on the 7th postoperative day.
Conclusion
The DAA for THA offers advantages over PLA, including reduced incision size, blood loss, and postoperative pain, albeit with a longer operation time. These findings should guide clinical decision-making, considering the benefits and potential increased complexity of the DAA.
Keywords: Direct anterior approach, Posterolateral approach, Total hip arthroplasty, Systematic review, Meta-analysis
Introduction
Total hip arthroplasty (THA) is an effective treatment method for various hip diseases, including hip osteoarthritis, femoral head necrosis, femoral neck fracture, and ankylosis hip joint. It offers significant pain relief, improves hip joint mobility, and enhances patients’ quality of life [8]. Multiple surgical approaches exist for THA, each with its own advantages and disadvantages. The choice of surgical approach influences early rehabilitation outcomes for patients [22, 26]. The posterolateral approach (PLA), the most commonly used approach, is favored due to its simplicity and enhanced posterior hip joint stability [10]. In recent years, the direct anterior approach (DAA) has gained popularity for its advantages of minimizing muscle damage, reducing blood loss during surgery, and promoting faster recovery [6, 24]. Although studies suggest that DAA surgery results in shorter hospital stays and faster early healing, there is insufficient evidence to determine the optimal approach for THA [3, 31].
Consequently, through the review of existing literature, conducting an extensive literature search, and organizing the collected data using the evidence-based medicine approach, this study employs Meta-analysis to compare the surgical duration, length of incision, intraoperative blood loss, incision infection rate, and VAS score between DAA and PLA, thereby offering a solid foundation for clinical management purposes.
Materials and methods
Material sources and retrieval strategies
The databases utilized for information retrieval included China National Knowledge Infrastructure (CNKI), Wanfang Data, VIP Chinese sci-tech journals, Chinese Biomedical Literature Database (CBM), Pubmed, Cochrane Library, and others. The search was conducted until December 2023 on each database. The search terms in Chinese were “total hip arthroplasty”, “direct anterior approach”, “complication”, and their respective synonyms were included. The English keywords used were “TotalhipReplacement”, “DirectForwardApproach”, and “Complications”, and these keywords were combined using the Boolean operator “AND”. The study followed the PRISMA 2020 guidelines.
Criteria for inclusion and exclusion of documents
Inclusion criteria for literature
(1) Patients who underwent THA and were subjected to either DAA or PLA surgical approaches were included. (2) Only randomized controlled trials were considered, with DAA being the experimental group and PLA being the observation group. (3) Studies with a sample size of 80 or more were included. (4) Follow-up time of at least 6 months was required. (5) The observed parameters included operation time, incision length, intraoperative blood loss, incision infection, and VAS score on postoperative days 1, 3, and 7. (6) In the case of multiple reports from the same author, the study with the largest sample size or the newest publication was chosen.
Exclusion criteria for literature
(1) Repetitive or unrelated studies and reviews were excluded. (2) Non-randomized controlled trials were not considered. (3) Studies without clear diagnostic or efficacy criteria were excluded. (4) Studies involving acupuncture treatment in either the experimental or control group were not included. (5) Studies with missing data, incomplete information, or obvious errors were excluded. (6) Studies published before 2020 were not considered.
Literature screening and data extraction
The literature review process involved two researchers from the research team who conducted independent screening. They followed the predetermined criteria for literature inclusion and exclusion, initially reviewing the title and abstract. If necessary, they proceeded to examine the full text and consulted with external experts in cases of disagreement. To gather relevant data, the researchers utilized a pre-established literature feature table. This table allowed them to extract important details such as study design type, overall sample size, sample sizes for the test and control groups, and outcome indicators from the eligible documents.
Document quality evaluation
The quality assessment of the literature included in the study was conducted using the revised Jadad scale. The scale had a maximum score of 7, which encompassed various criteria such as randomization, blinding, and handling of withdrawals and loss of follow-up. A score of 0 indicated exclusion from the study, while scores between 1 and 3 denoted inclusions as a low-quality study. On the other hand, scores ranging from 4 to 7 indicated inclusion as a high-quality study.
Statistical methods
In this study, literature management was conducted using NoteExpress3.2 software, while Excel2003 software was utilized for the collection and extraction of literature data. Meta-analysis was performed using Revman5.4.1 software. The Q-value statistical test and I² test were used to analyze the heterogeneity of the articles. When the P-value of the Q test was greater than 0.1 or I² of the I² test was less than 50% (from the Cochrane Handbook), indicating that there was no statistical heterogeneity in the study, the fixed-effects model (FEM) was used for grouping; otherwise, the random-effects model (REM) was used for analysis. The data was described and analyzed using the odds ratio (OR) and its 95% confidence interval (CI), and a forest map was drawn to illustrate the results. Sensitivity analysis was conducted to examine the stability of the Meta-analysis findings, while publication bias was assessed using a funnel chart. The significance level α was set at 0.05 (two-tailed).
Results
Results of literature retrieval
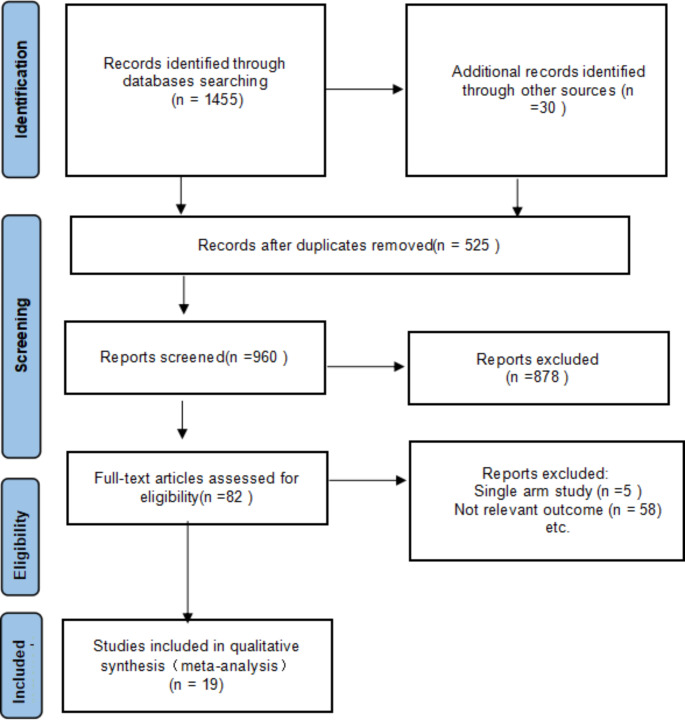
Based on the article retrieval strategy, a total of 1485 relevant articles were initially searched in databases such as China knowledge Network, Wanfang Database, VIP Chinese Sci-tech Journals Database, China Biomedical Database, Pubmed, Cochanelibrary, among others. Afterwards, redundant articles from each database were removed. Subsequently, by carefully reviewing the titles, abstracts, and full texts, a final selection of 19 articles was made. The complete process of literature screening is illustrated in Fig. 1.
Fig. 1.
Flow diagram
Basic characteristics and quality evaluation of literature
Table 1 presents a detailed overview of the first author, year of publication, sample size, age, body mass index (BMI) where available, follow-up time, observation index, and the Jadad score for each study. The observation index includes the specific parameters measured in each study, such as operation time, incision length, intraoperative blood loss, wound infection, and VAS scores at one day, three days, and seven days post-operation. The inclusion of these indices allows for a comprehensive comparison of the outcomes between the DAA and PLA groups. The baseline data primarily consisted of variables such as gender, age, disease duration, treatment strategy, and outcome measures. These variables were crucial in understanding the demographic and clinical characteristics of the patients included in the studies. These parameters were essential in evaluating the efficacy and safety of the surgical approaches. The quality assessment of the 19 studies included in the analysis was conducted using an enhanced version of the Jadad scale, as depicted in Table 1. The Jadad score is a widely accepted tool for evaluating the methodological quality of randomized controlled trials, with higher scores indicating better quality. The scores ranged from 4 to 6, suggesting a generally good quality of the included studies. Studies with a score of 4 were considered to have some methodological weaknesses, while those with scores of 5 and 6 were deemed to be of higher quality, with 6 indicating the highest standard of reporting and methodology.
Table 1.
Basic characteristics and quality evaluation of literature
| First author. | Year of publication. | Sample size (example). | Age. | THA. | BMI. | Follow-up time. | Observation index. | Jadad score. |
||
|---|---|---|---|---|---|---|---|---|---|---|
| Test group. | Control group. | Test group. | Control group. | NA | NA | |||||
| Wang Xiang [29] | 2023 | 30 | 60 | 48.69 ± 5.55 | 48.5 ± 5.82 | NA | NA | 6 months | 1.2.3.4.6. | 4 |
| Sun Jun [25] | 2021 | 60 | 62 | 54 ± 8 | 54 ± 8 | NA | NA | 6 months | 1.2.3.4.5.6.7. | 4 |
| Cui Tao [4] | 2022 | 45 | 48 | 65.85 ± 7.42 | 66.37 ± 7.61 | NA | NA | 6 months | 1.2.3.4.5.6. | 4 |
| Wang Yuanzhou [28] | 2021 | 153 | 145 | 65.47 ± 10.06 | 65.71 ± 10.21 | NA | NA | 1 year | 1.2.3.4. | 4 |
| Lei Tianrun [14] | 2023 | 124 | 124 | 64.72 ± 13.42 | 65.28 ± 10.22 | NA | NA | 1 year | 1.2.3.4.5.6.7. | 4 |
| Li Zheming [17] | 2021 | 59 | 61 | 62.71 ± 9.52 | 59.11 ± 12.02 | NA | NA | 1 year | 1.2.3.4.5.6. | 5 |
| Teng Lichu [27] | 2020 | 40 | 40 | 57.56 ± 6.51 | 56.49 ± 6.53 | NA | NA | 6 months | 1.2.3.4.5.6. | 5 |
| Cui Xiaoguang [5] | 2022 | 53 | 53 | 66.51 ± 2.07 | 67.21 ± 2.10 | NA | NA | 6 months | 1.2.3.4. | 4 |
| Nie Xinpan [21] | 2020 | 49 | 49 | 68.96 ± 2.40 | 69.04 ± 2.37 | NA | NA | 6 months | 1.2.3.4. | 4 |
| Jiang Hongshun [11] | 2020 | 50 | 62 | 59.3 ± 8.3 | 60.2 ± 9.3 | NA | NA | 6 months | 1.2.4. | 4 |
| Ye Dongcheng [30] | 2023 | 45 | 45 | 69.16 ± 2.2 | 70.84 ± 2.3 | NA | NA | 6 months | 1.2.3.4.5.6.7. | 4 |
| Jiang Hailiang [12] | 2023 | 46 | 38 | 53.5 ± 5.2 | 52.3 ± 5.6 | NA | NA | 6 months | 1.3.4. | 4 |
| Ma Chao [19] | 2021 | 48 | 48 | 62∽86 | NA | NA | 1 year | 1 year. | 5 | |
| Li Jinguang [16] | 2021 | 42 | 42 | 64.33 ± 2.35 | 65.61 ± 2.33 | NA | NA | 6 months | 1.2.3.4. | 4 |
| Zhang Xiaomin [32] | 2021 | 52 | 55 | 70.15 ± 6.16 | 70.02 ± 5.86 | NA | NA | 1 year | 1.2.3.4.5.6. | 5 |
| Mund [20] | 2020 | 40 | 40 | 59.6 ± 5.2 | 61.4 ± 4.9 | NA | NA | 1 year | 1.2.3.4. | 4 |
| Chen Yongjie [2] | 2021 | 62 | 62 | 64. 54 ± 6.48 | 67. 46 ± 5. 59 | NA | NA | 6 months | 1.2.3.4. | 4 |
| Zhu Chengxin [33] | 2022 | 40 | 60 | 65. 7 ± 6. 1 | 65. 9 ± 5. 6 | NA | NA | 6 months | 1.2.3.5.6. | 4 |
| Jin Xin [13] | 2023 | 50 | 50 | 51.4 ± 13.6 | 52.3 ± 12.6 | NA | NA | 6 months | 1.2.5.6.7. | 6 |
Note (1) Operation time (min) (2) Incision length (cm) (3) Intraoperative blood loss (ml) (4) Wound infection (5) VAS score 1 day after operation (6) VAS score 3 days after operation (7) VAS score 7 days after operation. NA, which stands for not applicable
Meta analysis results
Operation time
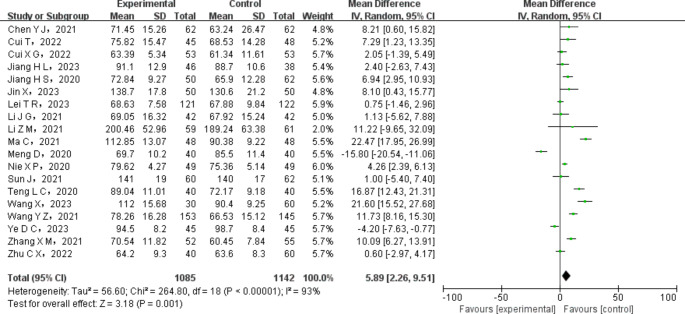
A total of 19 research papers investigated the duration of the operation in both the experimental and control groups. The test group comprised 1085 cases, while there were 1142 cases in the control group. The included literature was assessed for heterogeneity, which revealed statistical heterogeneity among the different studies. Therefore, the random-effects model (REM) was utilized to combine the literature data. The outcomes of the Meta-analysis exhibited that, compared to the control group using PLA, the operation time in the test group with DAA was significantly longer [MD = 5.89, 95%CI (2.26 to 9.51), P = 0.001], as illustrated in Fig. 2.
Fig. 2.
Forest map of comparison of operation time between the experimental group and the control group
Cut length
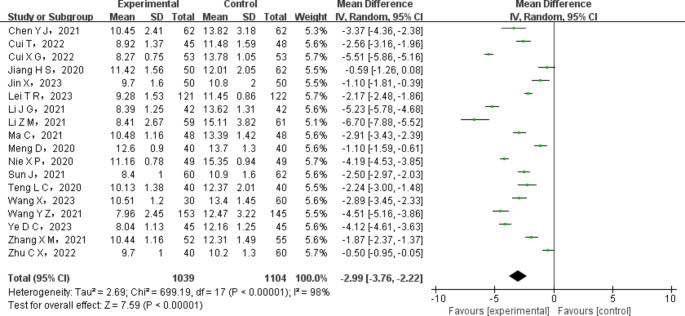
A total of 18 studies analyzed the incision length during surgery between the experimental group and the control group. The test group comprised 1039 cases, while the control group comprised 1104 cases. The included literature was tested for heterogeneity, and the results indicated significant variation among the different studies. Therefore, the random -effects model (REM) was adopted to combine the data from these studies. The Meta-analysis results demonstrated that the length of surgical incision was significantly smaller in the test group (using DAA) compared to the control group (with PLA). The statistical analysis showed a significant difference [MD=-2.99, 95%CI (-3.76 to -2.22), P < 0.00001]. Refer to Fig. 3.
Fig. 3.
Forest map of intraoperative incision length comparison between the experimental group and the control group
Intraoperative bleeding volume
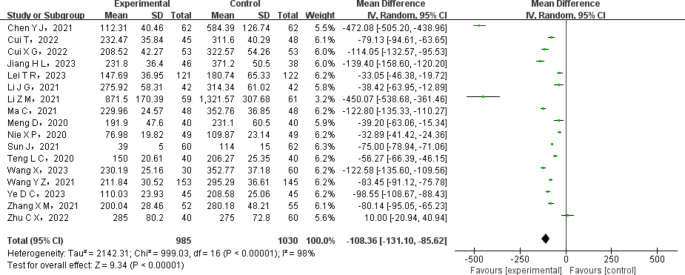
A total of 17 research articles were analyzed to compare the quantity of blood loss between patients in the test group and those in the control group. The test group consisted of 985 cases, while the control group included 1030 cases. The heterogeneity of the selected articles was assessed and statistically significant heterogeneity was detected among different studies. Therefore, the random-effects model (REM) was employed to combine the data from the literature. The results of the Meta-analysis indicated that the test group, which underwent DAA, experienced significantly lower intraoperative blood loss compared to the control group (PLA) [MD=-108.36, 95% CI (-131.10 to -85.62), P < 0.00001]. This is illustrated in Fig. 4.
Fig. 4.
Forest map of comparison of intraoperative blood loss between the experimental group and the control group
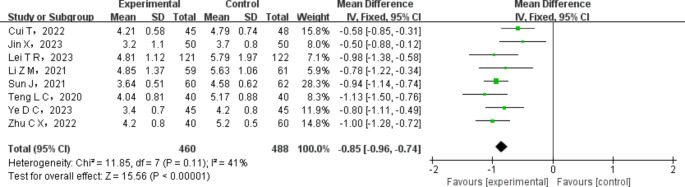
Visual analog pain score (VAS) of hip joint on the first day after operation
A total of 8 studies examined the visual analog pain score (VAS) of the hip joint on the first day after surgery, comparing the experimental group with the control group. The test group consisted of 460 cases, while the control group had 488 cases. To determine the heterogeneity among the included studies, a heterogeneity test was conducted. The results indicated no statistical heterogeneity, implying that the studies were similar. Therefore, the fixed-effects model (FEM) was employed to combine the data from these studies. Meta-analysis results demonstrated that, one day after surgery, the hip joint VAS score was significantly lower in the THA via DAA group compared to the control group. This indicates that patients in the THA via DAA group experienced milder pain symptoms. The difference was statistically significant[MD=-0.85,95%CI(-0.96 to -0.74), P < 0.00001]. Please refer to Fig. 5 for the visualization of these results.
Fig. 5.
Forest map of VAS comparison between the experimental group and the control group on the first day after operation
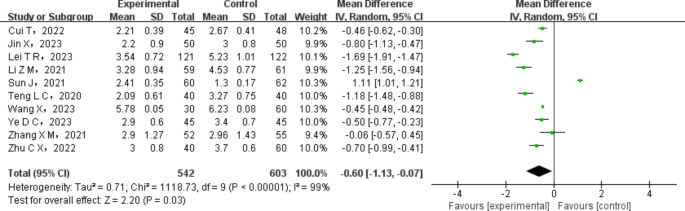
Visual analog pain score (VAS) of hip joint on the 3rd day after operation
In a total of 10 studies, the visual analogue pain score (VAS) of the hip joint on the 3rd day after operation was compared between the experimental and control groups. The test group consisted of 542 cases, while the control group had 603 cases. To assess the heterogeneity of these studies, statistical tests were carried out, which revealed significant heterogeneity among them. To account for this heterogeneity, the random-effects model (REM) was used to combine the data from these studies. The results of the Meta-analysis indicated that, compared to the control group, patients who underwent THA by DAA experienced significantly lower hip joint VAS scores and milder pain symptoms on the 3rd day after the operation [MD=-0.60, 95% CI (-1.13 to -0.07), P = 0.03]. Please refer to Fig. 6 for a visual representation of these findings.
Fig. 6.
Forest map of VAS comparison between the experimental group and the control group on the 3rd day after operation
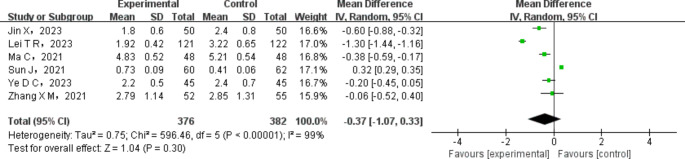
Visual analog pain score (VAS) of hip joint on the 7th day after operation
On the 7th day after the operation, an examination of the visual analog pain score (VAS) of the hip joint was conducted in a total of 6 studies. The experimental group consisted of 376 cases, while the control group had 382 cases. After testing the heterogeneity of the included literature, it was found that there was statistical heterogeneity among different studies. Therefore, the random-effects Model (REM) was used to combine the data from the literature. The results of the Meta-analysis indicated that there was no significant difference in the VAS score of the hip joint between the experimental group and the control group on the 7th day after operation [MD=-0.37, 95%CI (-1.07 to 0.33), P = 0.30]. This is illustrated in Fig. 7.
Fig. 7.
Forest map of VAS comparison between the experimental group and the control group on the 7th day after operation
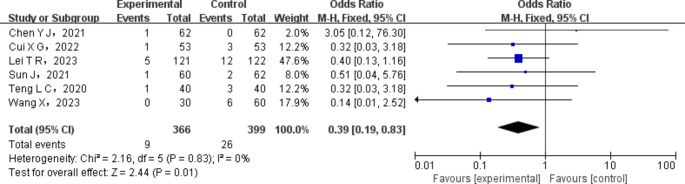
Incisional infection
A total of 8 studies assessed the occurrence of postoperative incision infection in the experimental group compared to the control group. Out of these, 2 studies reported no incision infection in either group, resulting in a final inclusion of 6 studies. The test group comprised 366 cases, while the control group had 399 cases. To evaluate the heterogeneity among the included literature, a statistical test was conducted, revealing no significant heterogeneity across the studies. Therefore, the fixed-effects Model (FEM) was employed to combine the data from the studies. The Meta-analysis results demonstrated a statistically significant decrease in the incidence of incision infection in total hip arthroplasty (THA) using direct anterior approach (DAA) when compared to the control group [OR = 0.39, 95%CI (0.19 to 0.83), P =0.01], as illustrated in Fig. 8.
Fig. 8.
Forest map of postoperative incision infection between the experimental group and the control group
Discussion
Currently, the surgical techniques commonly employed for total hip arthroplasty (THA) include the posterolateral approach (PLA) and the direct anterior approach (DAA). These two approaches differ significantly in their intraoperative procedures, leading to variations in complications such as incisional infections. The incision of PLA is external, and the joint capsule and its wrapped femoral head are exposed layer by layer by layer to bypass the greater trochanter of the femur from the rear during the operation, resulting in a longer surgical incision (generally 10 to 15 cm), while the above process is disassembled.More muscle tissue, which directly increases the amount of intraoperative blood loss, may be one of the important factors leading to the delay of postoperative rehabilitation progress [15, 23]. DAA has emerged with the innovation of new joint replacement surgical instruments, exposing the hip joint from the front through the intermuscular space in minimally invasive conditions, with less damage to the muscle tissue in the joint [1, 7].In this study, we conducted a quantitative analysis and evaluation of the efficacy of the DAA versus the PLA in THA.We examined operation time,incision length,intraoperative blood loss,postoperative pain,and incision infection rate to assess the potential risks and benefits associated with each approach.
The outcomes of the Meta-analysis demonstrated that the experimental group, which underwent DAA, had a longer operation time compared to the control group [MD = 5.89,95%CI (2.26 to 9.51), P =0.001]. Furthermore, the incision length was smaller [MD=-2.99,95%CI (-3.76 to -2.22), P < 0.00001], and there was a reduction in intraoperative bleeding [MD=-108.36,95%CI (-131.10 to -85.62]. On post-operative days 1 and 3, the hip joint VAS score was lower and patients experienced milder pain symptoms (MD =-0.85 and-0.60, respectively). The 95%CI for these values were (− 0.96) and (− 1.13), with P < 0.00001 and P=0.03, respectively. Additionally, the incidence of incision infection in THA patients using DAA was significantly lower than that in the control group [OR = 0.39,95%CI (0.19 to 0.83), P =0.01]. However, there was no significant difference in the hip joint VAS score on the 7th day post-operation [MD=-0.37,95%CI (-1.07 to 0.33), P = 0.30].
Comparing with previous published papers, our study’s focus is on the comparison of postoperative orthopedic complications between the DAA and PLA for primary THA. Singh et al. [24] conducted a systematic review of the DAA for revision THA, examining nine studies with a total of 319 hip joints. Their review found that the DAA for revision THA had a low complication rate and was associated with a variety of indications for revision, including aseptic loosening, prosthetic joint infection, and periprosthetic fractures. While Singh et al. focused on the use of the DAA in revision surgeries, our study concentrated on the DAA for primary THA and compared it with the PLA. Previous studies also compared the DAA and lateral approach (LA) for primary THA. Huang et al. [9] performed a systematic review and Meta-analysis of 13 studies comparing the DAA with the LA for primary THA, involving a total of 24,853 hips. Huang et al. found no significant difference in the rate of surgical site infection, heterotopic ossification, and reoperation between the DAA and LA groups. However, they did observe a lower rate of prosthesis malposition, leg length discrepancy, and Trendelenburg gait in the DAA group, but a higher rate of dislocation, periprosthetic fracture, prosthesis loosening, and nerve injury. Here, our Meta-analysis included a larger number of studies and hips, providing a more robust analysis of the comparative outcomes. Additionally, our study provides a detailed analysis of various postoperative complications, including surgical site infection, prosthesis-related complications, surgical trauma-related complications, dysfunction, and reoperation, which allows for a comprehensive comparison between the two approaches. While our findings are consistent with the advantages of the DAA for THA reported by Singh et al. and Huang et al., such as more precise prosthesis placement and less damage to surrounding hip musculature, our study highlights the need for surgeons to be aware of the higher rates of certain complications, such as dislocation, periprosthetic fracture, prosthesis loosening, and nerve injury, when using the DAA, particularly given the limited exposure and longer learning curve compared to the PLA.
Our study has several limitations that might affect the robustness of our conclusions. First, the small number of included studies could have resulted in high heterogeneity, which may impact the reliability of our pooled estimates. Moreover, due to the limited number of studies, we were unable to perform subgroup analyses or adequately assess publication bias, which are important considerations in Meta-analyses. Second, the lack of hazard ratio data for long-term outcomes limits our understanding of the durability and safety of the direct anterior approach (DAA) compared to the posterior lateral approach (PLA). Hazard ratios provide crucial information about the risk of adverse events over time, and the absence of such data makes it challenging to draw definitive conclusions about the long-term implications of the different surgical approaches. Third, there may be unidentified confounding factors that influenced our results. For instance, differences in patient characteristics, surgeon experience, and surgical techniques across studies could have affected the outcomes. These confounding factors may have biased our results, and therefore, caution is warranted when interpreting the findings. Finally, the studies included in our Meta-analysis varied in design, quality, and reporting standards, which introduces potential sources of bias. Variability in outcome reporting and missing data could have impacted the consistency and comparability of the results. Given these limitations, our findings should be interpreted with caution. Future studies with larger sample sizes, longer follow-up periods, and standardized reporting of outcomes are needed to confirm our results and provide a more comprehensive understanding of the comparative effectiveness and safety of the DAA versus the PLA in total hip arthroplasty.
It is evident that in comparison to PLA, DAA THA exhibits reduced bleeding and smaller incision, thus facilitating a shorter bed rest period, encouraging early mobilization post-surgery, enhancing hip joint functional recovery, and decreasing complications associated with incision infection. However, it should be noted that DAA THA requires a relatively longer operation time, which can be attributed to the smaller incision and heightened surgical exposure complexity [18]. Despite its numerous benefits in THA, DAA also presents certain drawbacks, including a prolonged learning curve and surgical challenges. The findings of this study carry significant implications for clinical practice, advocating for the adoption of the DAA due to its demonstrated benefits. Policymakers should consider integrating DAA training into surgical curricula and promoting its use where feasible. Future research should address the limitations of this study by expanding sample sizes, conducting long-term follow-ups, and assessing economic implications to solidify the evidence base for DAA in total hip arthroplasty.
Conclusion
In summary, in contrast to PLA, DAA offers the benefits of a smaller incision, reduced intraoperative bleeding, and minimized postoperative pain; however, it does require a longer duration for the surgical procedure.
Acknowledgements
The authors are grateful to all participants in the present study.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Kunhao Wang, Tao Zhang, Ruiyang Xia, Jiankai Wang and Jinliang Yu. The first draft of the manuscript was written by Kunhao Wang and Wenbo Wang commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The present study was not supported by any fundings.
Data availability
The data involved in the present study can be provided under reasonable request.
Declarations
Ethics and informed consent
Not applicable.
Competing interests
The authors declare that there is no conflict of interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Brun OL, Månsson L, Nordsletten L (2018) The direct anterior minimal invasive approach in total hip replacement: a prospective departmental study on the learning curve. Hip International: J Clin Experimental Res hip Pathol Therapy 28(2):156–160. 10.5301/hipint.5000542 [DOI] [PubMed] [Google Scholar]
- 2.Chen YJ, Tan L, Zhang HQ, Weng Z, Jiao S, Luo XH, Wu MX, Peng YC, Qiu JB (2021) Comparison of prosthesis position and clinical efficacy after total hip arthroplasty between direct anterior versus classic posterolateral approaches. Guangxi Med J 43(5):556–560. 10.11675/j.issn.0253-4304.2021.05.10 [Google Scholar]
- 3.Cheng TE, Wallis JA, Taylor NF, Holden CT, Marks P, Smith CL, Armstrong MS, Singh PJ (2017) A prospective Randomized Clinical Trial in total hip arthroplasty—comparing early results between the Direct Anterior Approach and the posterior Approach. J Arthroplast 32(3):883–890. 10.1016/j.arth.2016.08.027 [DOI] [PubMed] [Google Scholar]
- 4.Cui T, Tang XJ (2022) Effect of total hip replacement with different approaches on femoral neck fractures of Garden III and IV and and its effect on muscle tissue injury and bone metabolism. Chin Med Innov 19(07):68–72 [Google Scholar]
- 5.Cui XG, Chang JN, Li ZQ (2022) Application of anterior direct approach and posterolateral approach in total hip arthroplasty. Prim Med Forum 26(34):20–22. 10.19435/j.1672-1721.2022.34.007 [Google Scholar]
- 6.Dai HY, Zhu KC, Wang QJ, Zhang XL, Wang Q (2022) Learning curve and short-term clinical outcomes of Mako robotic-assisted direct anterior approach total hip arthroplasty. Chin Med J 102(1):49–55. 10.3760/cma.j.cn112137-20210806-01754 [DOI] [PubMed] [Google Scholar]
- 7.Eguchi Y, Iida S, Suzuki C, Shinada Y, Shoji T, Takahashi K, Ohtori S (2018) Spinopelvic alignment and low back Pain after total hip replacement arthroplasty in patients with severe hip osteoarthritis. Asian Spine J 12(2):325–334. 10.4184/asj.2018.12.2.325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galakatos GR (2018) Direct anterior total hip arthroplasty. Mo Med 115(6):537–541 [PMC free article] [PubMed] [Google Scholar]
- 9.Huang XT, Liu DG, Jia B, Xu YX (2021) Comparisons between Direct Anterior Approach and Lateral Approach for Primary Total Hip Arthroplasty in postoperative Orthopaedic complications: a systematic review and Meta-analysis. Orthop Surg 13(6):1707–1720. 10.1111/os.13101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jia YD, Liu YW, Wang HC, Zhu YJ, Zhang Y, Tang YF, Sun RB, Cai HM (2016) A comparision of direct anterior approach and lateral approach for total hip arthroplasty in the treatment of Crowe I, II type of hip dysplasia. Chin J Bone Joint 5(7):507–510. 10.3969/j.issn.2095-252X.2016.07.007 [Google Scholar]
- 11.Jiang HS, Mao XH, Jin S (2020) Effect of direct anterior and posterolateral approaches on latent blood loss and early hip function during total hip replacement. Zhejiang Practical Med August 25(04):270–271. 10.16794/j.cnki.cn33-1207/r.2020.04.013 [Google Scholar]
- 12.Jiang HL, Liang JM, Chen Q, Yang WC, Jiang HS, Lie L, Xu K (2023) Comparison of early clinical efficacy of direct anterior approach and posterolateral approach for hip replacement. Chin J Bone Joint Surg 16(01):31–36 [Google Scholar]
- 13.Jin X, Chen G, Chen M, Riaz MN, Wang J, Yang S, Xu W (2023) Comparison of postoperative outcomes between bikini-incision via direct anterior approach and posterolateral approach in simultaneous bilateral total hip arthroplasty: a randomized controlled trial. Sci Rep 13(1). 10.1038/s41598-023-29146-2 [DOI] [PMC free article] [PubMed]
- 14.Lei TR, Shang XF, Zhou PH (2023) Early effect of total hip replacement of direct anterior approach under lateral decubitus position. Med J Wuhan Univ 44(4):468–473. 10.14188/j.1671-8852.2021.0440 [Google Scholar]
- 15.Li SL, Yang XT, Tian XB, Sun L (2019) Direct anterior approach and anterolateral approach to the whole hip early functional recovery after arthroplasty. J Peking Univ (Medicine Edition) 51(02):268–272. 10.19723/j.issn.1671-167X.2019.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li JG, Zhang JJ, Nhamujiang B, Li YW, Ai SJ (2021a) Comparison of effects of total hip arthroplasty through direct anterior approach and posterolateral approach in treatment of elderly patients with femoral neck fractures. Med J Chin People’s Health 33(19):129–131 [Google Scholar]
- 17.Li ZM, Bi Q, Yang M, -, -, - - (2021b) Clinical observation of total hip arthroplasty with direct anterior approach in lateral position. Zhejiang Med 43:1111–1114
- 18.Luo ZL, Chen M, Shang XF, -, - - (2016) Clinical efficacy of total hip arthroplasty by direct anterior approach and posterolateral approach. Chin Med J 96(35):2807–2812 [DOI] [PubMed]
- 19.Ma C, Tang HY (2021) Clinical effect of total hip arthroplasty via direct anterior approach and posterolateral approach in the treatment of femoral neck fractures in the elderly. J Trauma Surg 23(02):136–140 [Google Scholar]
- 20.Meng D, Zhu SW, Qi W, Li SZ (2020) Comparison of clinical effects of direct anterior approach and posterolateral approach in total hip arthroplasty. Guangxi Med Sci 42(02):141–146 [Google Scholar]
- 21.Nie XP, Yue ZH (2020) Comparative analysis of clinical efficacy and safety of Direct Anterior Approach and posterior lateral Approach in To-tal hip arthroplasty. Heilongjiang Med Sci 44(5):598–600. 10.3969/j.issn.1004-5775.2020.05.008 [Google Scholar]
- 22.Putananon C, Tuchinda H, Arirachakaran A, Wongsak S, Narinsorasak T, Kongtharvonskul J (2017) Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: network meta-analysis. Eur J Orthop Surg Traumatol 28(2):255–267. 10.1007/s00590-017-2046-1 [DOI] [PubMed] [Google Scholar]
- 23.Salal MH (2017) Transverse Acetabular ligament as an anatomical Landmark for Intraoperative Cup Anteversion in primary total hip replacement. J Coll Physicians Surgeons–Pakistan: JCPSP 27(10):642–644 [PubMed] [Google Scholar]
- 24.Singh G, Khurana A, Gupta S (2021) Evaluation of Direct Anterior Approach for Revision Total hip arthroplasty: a systematic review. Hip Pelvis 33(3):109–119. 10.5371/hp.2021.33.3.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun J, Jiang T, Zhi L (2021) Short-term effects of initial total hip replacement with different approaches in treatment of femoral head necrosis. Chin Med Clin 21(15):2648–2651. 10.11655/zgywylc2021.15.011 [Google Scholar]
- 26.Talia AJ, Coetzee C, Tirosh O, Tran P (2018) Comparison of outcome measures and complication rates following three different approaches for primary total hip arthroplasty: a pragmatic randomised controlled trial. Trials 19(1). 10.1186/s13063-017-2368-7 [DOI] [PMC free article] [PubMed]
- 27.Teng LC, Chen T, Huang S, Chen DX, Wen KW (2020) Comparison of clinical efficacy and postoperative VAS score of direct anterior approach and posterolateral approach in total hip arthroplasty. Hebei Med Sci 26(05):820–825 [Google Scholar]
- 28.Wang YZ, Fu K, Ma CH, Zhuang HX (2021) Effects of different approaches in total hip arthroplasty on postoperative recovery of patients. J Local Surg 30(6):525–528. 10.11659/jjssx.12E020014 [Google Scholar]
- 29.Wang X, Wang H, Wang B, -, -, - - (2023) Comparative study on the short-term efficacy of DAA approach and posterolateral approach for total hip arthroplasty. Henan J Surg 29(04):75–78
- 30.Ye DC, Zhong HX, Li YW, Mo XJ, Zhang S (2023) Clinical study of direct anterior approach total hip replacement in elderly patients with femoral neck fractures. Big Doctor 8(10):54–57. 10.3969/j.issn.2096-2665.2023.10.018 [Google Scholar]
- 31.Yue C, Kang P, Pei F (2015) Comparison of direct anterior and lateral approaches in total hip arthroplasty. Medicine 94(50). 10.1097/md.0000000000002126 [DOI] [PMC free article] [PubMed]
- 32.Zhang XM, Yan TS, Li GQ, Wang XX, Li LJ, Yan XY, Wang Y, Wu Z (2021) Comparison of early effects of total hip arthroplasty with direct anterior approach and posterolateral approach in the treatment of elderly femoral neck fractures. Clin Med Res Pract 6(23):33–35. 10.19347/j.cnki.2096-1413.202123011 [Google Scholar]
- 33.Zhu CX, Xu JZ, Shao S (2022) Comparison of the early efficacy between direct anterior approach and posterolateral approach in total hip arthroplasty and analysis of the risk factors of postoperative persistent pain. J Bengbu Med Coll 47(10):1388–1393. 10.13898/j.cnki.issn.1000-2200.2022.10.013 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data involved in the present study can be provided under reasonable request.